Abstract
Objectives
Occupation-based intervention (OBI) involves daily and meaningful activities for evaluation and intervention. Recently, the “aid for decision-making in occupation choice for hand” (ADOC-H) was developed to facilitate OBI in patients with hand injuries. We aimed to examine the efficacy of OBI using the ADOC-H combined with physical function-based interventions (PBI) for patients with distal radius fractures (DRF).
Material and methods
Patients with DRF were retrospectively allocated to two groups, ADOC-H group (n = 14) and PBI group (n = 14), and compared.
Results
Improvements in the Pain Catastrophizing Scale magnification and Hospital Anxiety and Depression Scale and Disabilities of the Arm, Shoulder, and Hand questionnaire scores were significantly higher in the ADOC-H group than in the PBI group (p < .05). The groups showed no differences in measure of physical function, such as range of motion and grip strength.
Conclusion
OBI using the ADOC-H combined with PBI is clinically useful for patients with DRF as it promotes use of the injured hand for daily activities in a step-by-step approach, improving psychological difficulties in using the hand.
Keywords: Distal radius fractures, upper extremity, occupation-based intervention, digital decision aids, patient-therapist goals
Introduction
Distal radius fractures (DRF) account for approximately 18% of all fractures (Baron et al., 1996). Post-surgical inactivity, a common cause for prolonged treatment in patients with DRF, contributes to postoperative anxiety and pain catastrophizing, which can lead to complications like complex regional pain syndrome and chronic pain (Dilek et al., 2012; Allen, Galer, & Schwartz, 1999). Patients with DRF have long-standing complaints of inconvenience in meal preparation, shopping, and getting out of a car, suggesting that inactivity immediately after surgery may be prolonged (Edwards et al., 2010). To avoid prolonged treatment after DRF, patients should begin using the injured hand for daily activities in a step-by-step approach from the early post-surgery period.
Postoperative hand therapy for patients with DRF often focuses on physical function-based interventions (PBI), such as range of motion (ROM) exercises. However, the correlation between improvements in wrist ROM and the Jebsen Test of Hand Function (JTHF), which assesses the ability to use the hand, was weak and insignificant in patients with DRF (Tremayne et al., 2002). Improving daily activities in DRF patients requires interventions that consider psychological aspects such as anxiety (Hiraga et al., 2021). These reports suggest the need for interventions that encourage using the injured hand combined with PBI.
Occupation-based intervention (OBI) has attracted attention in the field of hand therapy. OBI is an activity-based intervention consisting of occupations that match patient-identified goals (Fisher, 2013). OBI for patients with hand injuries reportedly reduces difficulties in using the injured hand in daily activities and promotes psychological improvement (Hansen et al., 2020). Although OBI is expected to reduce anxiety and pain catastrophizing if it improves difficulties in daily activities, few studies on the effects of OBI in patients with hand injuries have reported significant improvements in efficacy measures related to psychological aspects (Weinstock-Zlotnick & Mehta, 2019). Therefore, we consider it significant to clarify that OBI combined with PBI reduces difficulties in using the hands in daily activities and improves anxiety and pain catastrophizing.
We developed the aid for decision-making in occupation choice for hand (ADOC-H) as a tool to facilitate OBI (Ohno et al., 2017). ADOC-H is an iPad application tool that helps patients and therapists discuss the use of the injured hand in daily activities through a selection of illustrations (Figure 1) (Ohno et al., 2017).
Figure 1.
Aid for decision-making in occupation choice for hand (ADOC-H). (a) Interview using the ADOC-H (b) Examples of the ADOC-H tablet version Figure 2.
ADOC-H is a decision aid, and decision aids are effective in identifying and clarifying patient-therapist goals (Ohno et al., 2017). This study aimed to examine the efficacy of OBI using ADOC-H for patients with DRF for reducing difficulties in using their hands in daily activities, pain catastrophizing, and anxiety and to examine OBI using ADOC-H combined with PBI (ADOC-H group) and PBI only (PBI group) in a retrospective comparative design. The aim of this study is to propose a specific intervention protocol that combines OBI using the ADOC-H and PBI, and it helps establish evidence for OBI in patients with DRF.
Methods
Study Design
This was a single-center, retrospective, case-control study. The medical institution the first author belongs to conducted PBI for patients with DRF until March 31, 2021. On April 1, 2021, OBI using the ADOC-H combined with PBI was introduced to promote further improvements in patients with DRF, not only in physical function but also in psychological function and disability. Patients with DRF after surgery were retrospectively allocated to the PBI and ADOC-H groups in a non-randomized manner. Data were collected from rehabilitation records after all patient interventions were completed. Ethical approval was obtained from the Ethics Committee of our institution (ref. no. 220020, approval date: July 2022). Informed consent was obtained from all patients once they fully understood the purpose and methodology of the study following the hospital’s ethical guidelines.
Estimating the Sample Size
The power analysis program G*Power 3 (Faul et al., 2007) was used to estimate sample size. The study expected interaction effects by two-way repeated measures analysis of variance (ANOVA) on the outcomes of difficulty using the injured hand in daily activities, pain catastrophizing, and anxiety. Since this was the research hypothesis, the sample size was estimated in terms of interaction effects. The power was set at .8, significance level (α) at .05 (Cohen, 1992), and effect size f at .25, which is the moderate standard for two-way repeated measures ANOVA. Twenty-eight participants were required to ascertain the significant effect of the intervention.
Participants
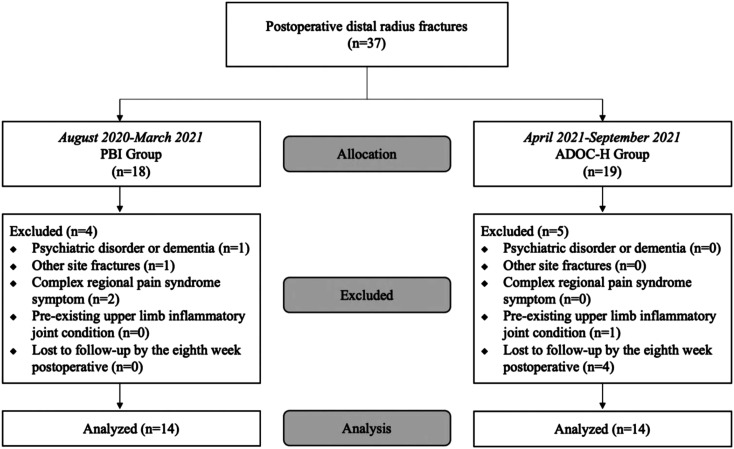
Between August 2020 and September 2021, at the hospital where the first author worked, we recruited 37 patients who underwent open reduction and internal fixation with a volar locking plate following intra-articular or extra-articular DRF and postoperative hand therapy for at least 8 weeks. A total of 28 patients were enrolled following exclusion and allocated to either the ADOC-H (n = 14) or PBI group (n = 14) (Figure 2).
Figure 2.
Flowchart showing patient allocation. PBI = physical function-based interventions; ADOC-H = aid for decision-making in occupation choice for hand.
Intervention Protocol
The intervention protocols for each group are presented in Table 1.
Table 1.
Intervention protocol.
| Days after Surgery | PBI Group (n = 14) | ADOC-H Group (n = 14) | Rehabilitation Intensity |
|---|---|---|---|
| 4th day | Start mild active ROM exercise of the injured hand and fingers. | Inpatient rehabilitation of 40 min once a day. | |
| 7th day | Goal setting was not conducted. | Goal setting using the ADOC-H | |
| 8th–10th day | Discharge to home | Outpatient rehabilitation for 20 min twice a week. | |
| The use of the injured hand in ADL is permitted to the extent that the stress on the fracture is minimal. | |||
| According to guidelines (Valdes et al., 2021), conduct PBI (e.g., ROM exercise). | Based on the goals set in ADOC-H, conduct OBI (e.g., dressing practice) and PBI (e.g., ROM exercise). | ||
| 8th week | The use of the injured hand in ADL is permitted without limitations. | ||
PBI = physical function-based interventions; ADOC-H = aid for decision-making in occupation choice for hand; ROM = range of motion; ADL = activities of daily living; PBI = physical function-based interventions; OBI = occupation-based intervention. The frequency and time of intervention in both groups were comparable.
Hand therapy during hospitalization was encouraged in both groups to move the injured hands and fingers on the fourth postoperative day according to the guidelines for DRF management (Japanese Orthopaedic Association, 2017). Only the ADOC-H group underwent goal-setting using ADOC-H on the seventh postoperative day. Both groups received hand therapy during the outpatient period for 20 min twice a week after discharge. The frequency and time of intervention in both groups were comparable.
PBI Group
Physical exercises such as manual ROM and muscle strengthening exercises were used as hand therapy interventions during outpatient practice in the PBI group according to the guidelines for DRF management (Japanese Orthopaedic Association, 2017). The PBI group was instructed on daily activities that were less stressful on the injured hand. However, the intervention was not designed for the patients’ individual daily activities.
ADOC-H Group
The ADOC-H consists of 130 items within the following 16 categories (Ohno et al., 2017). The ADOC-H goal setting process was performed in several steps. First, the patient selected up to 10 activities using the injured hand from the ADOC-H illustrations and prioritized each illustration. At this point, the therapist suggested several activities to the patient based on the ADOC-H illustrations, considering the patient’s needs and condition of the injured hand. After determining the priority, the patient and therapist discussed the identified problems and measures to overcome them effectively. For example, therapists suggested measures to manage the injured wrists and self-help devices for patients afraid to use their injured hands due to wrist pain and discussed approaches to resume activities gradually. Finally, the patient and therapist set three to five goals based on the prioritized illustrations.
According to the occupation set as the goal, the patient and therapist individually designed interventions for hand therapy during outpatient visits for the ADOC-H group. For example, patients, who selected the illustrations of “front button” and “cuff button” and set the goal of “I want to go out wearing my favorite clothes,” were asked to bring their favorite clothes to the hospital to practice dressing and buttoning. Much of the rehabilitation time was spent conducting OBI with ADOC-H. Additionally, approximately 5 to 10 min of PBI was performed each time to prevent sequelae, depending on the patient’s physical condition.
Measurements
Participant backgrounds, such as age, sex, AO classification, hand dominance, and outcome measures, were obtained from medical records. The outcome measures were performed on the sixth postoperative day (baseline), fourth postoperative week, and eighth postoperative week.
ROM
The ROM measurements were wrist flexion/extension and forearm supination/pronation. ROM was measured using a goniometer. The ROM of the involved side was estimated as a percentage of that of the normal side.
Pain
The numerical rating scale (NRS) was used to evaluate pain. The NRS scores ranged from 0 to 10 (0, no pain; 10, worst imaginable pain) (Jensen et al., 1986). In this study, pain at rest and during motion was assessed using the NRS.
Pain Catastrophizing
The Pain Catastrophizing Scale (PCS) was used to evaluate pain catastrophizing (Osman et al., 2000). The PCS comprises 13 questions divided into three subscales: rumination, helplessness, and magnification. The patients evaluated the time spent in the condition, on a five-point scale (0, not at all; 4, all the time) (Osman et al., 2000). In this study, PCS total scores and subscales were evaluated.
Anxiety and Depression
The Hospital Anxiety and Depression Scale (HADS) was used to assess anxiety and depression (Zigmond & Snaith, 1983). The HADS is composed of 14 questions for each item scored from 0 to 3 (0, not at all; 3, most of the time).
Disabilities of the Arm, Shoulder, and Hand (DASH)
The DASH score was recognized as a patient-reported outcome for measuring upper limb function and symptoms (Gummesson et al., 2003). The DASH consists of 30 items regarding the degree of difficulty in performing daily activities, such as ADLs, IADLs, work, leisure, and social activities. The DASH scores range from 0 to 100; the higher the score, the greater the degree of limited difficulty in performing day-to-day activities (Gummesson et al., 2003).
Grip Strength
Grip strength was measured by using a Jamar dynamometer (Sakai, Tokyo, Japan). The grip strength measurements were evaluated only in the eighth postoperative week for determining the risk of fracture dislocation.
Occupational Goals
Each goal of the ADOC-H group was evaluated in terms of performance and satisfaction. Performance was evaluated on a scale of 1 to 10 (1, not possible; 10, very good). Satisfaction was evaluated on a scale of 1 to 10 (1, not satisfied; 10, very satisfied).
Statistical Analyses
The t-test and Fisher’s exact test were used to analyze differences in patient backgrounds. A two-way repeated measures ANOVA was performed to assess the influence of outcome measures other than grip strength and occupational goals over time. For variables that showed group and time interaction effects in ANOVA, Bonferroni correction for multiple comparisons for differences between groups at each period were performed as post-hoc analysis. The difference in grip strength at the eighth week postoperative was analyzed using the t-tests. Occupational goals were performed with Bonferroni correction for multiple comparisons as a post hoc test of one-way repeated measures ANOVA. All statistical analyses were performed using EZR. The effects were considered significant when the p-value was less than .05.
Results
The patients’ characteristics are shown in Table 2.
Table 2.
Patient characteristics.
| PBI Group (n = 14) | ADOC-H Group (n = 14) | p-value | |
|---|---|---|---|
| Age (years) | 65.1 ± 15.8 | 69.2 ± 19.2 | .611 a |
| Sex (Female), n (%) | 14 (100%) | 13 (92.8%) | .481 b |
| Injured side, n (%) | |||
| Right | 6 (42.8%) | 7 (50.0%) | .704 b |
| Left | 8 (57.2%) | 7 (50.0%) | |
| Dominant side, n (%) | |||
| Dominant | 5 (35.7%) | 7 (50.0%) | .481 b |
| Non-dominant | 9 (64.3%) | 7 (50.0%) | |
| AO classification, n (%) | |||
| A type | 3 (21.5%) | 3 (21.5%) | .43 b |
| B type | 1 (7.1%) | 4 (28.5%) | |
| C type | 10 (71.4%) | 7 (50.0%) | |
AO fracture classification, where A denotes extra-articular, B denotes partial intra-articular, and C denotes intra-articular. PBI = physical function-based intervention; ADOC-H = aid for decision-making in occupation choice for hand. Values are expressed as mean ± standard deviation or n (%).
at-test.
bFisher’s exact test.
The analysis showed no significant differences in the demographic parameters between the groups.
Longitudinal changes (baseline, fourth week postoperative, and eighth week postoperative) in outcome measures and their main effects and interaction are shown in Table 3.
Table 3.
Outcome at Baseline, Week 4, and Week 8 After Surgery by Group.
| PBI Group (n = 21) | ADOC-H Group (n = 20) | Main Effect; Group | Main Effect; Time | Time-by-Group Interaction | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Week 4 | Week 8 | Baseline | Week 4 | Week 8 | F-value | p-value | F-value | p-value | F-value | p-value | η 2 | |
| ROM (%) | |||||||||||||
| Wrist flexion | 48.2 ± 10.1 | 57.6 ± 8.8 | 69.2 ± 9.5 | 51.3 ± 9.5 | 62.1 ± 10.1 | 70.5 ± 8.6 | 2.397 | .126 | 30.855 | <.001** | .288 | .751 | .004 |
| Wrist extension | 57.1 ± 9.1 | 66.5 ± 8.7 | 76.8 ± 9.4 | 56.7 ± 10.9 | 66.1 ± 9.6 | 80.8 ± 8.6 | .221 | .640 | 32.985 | <.001** | .452 | .638 | .006 |
| Forearm supination | 88.5 ± 12.5 | 93.7 ± 8.3 | 96.0 ± 5.3 | 85.7 ± 12.3 | 92.9 ± 7.6 | 94.4 ± 5.1 | .808 | .371 | 5.360 | .007** | .079 | .924 | .002 |
| Forearm pronation | 89.3 ± 10.1 | 94.8 ± 6.1 | 96.0 ± 4.8 | 86.5 ± 10.8 | 92.1 ± 7.1 | 94.0 ± 4.9 | 2.284 | .135 | 5.759 | .005** | .004 | .996 | .000 |
| NRS (points) | |||||||||||||
| Rest pain | .8 ± .9 | .6 ± .9 | .4 ± .7 | 1.1 ± 1.0 | .5 ± .6 | .2 ± .4 | .026 | .872 | 4.224 | .018* | .854 | .429 | .020 |
| Motion pain | 2.4 ± 1.5 | 1.9 ± 1.2 | 1.3 ± 1.0 | 2.2 ± 1.3 | 1.9 ± 1.1 | .8 ± .7 | .619 | .434 | 7.107 | .001** | .301 | .741 | .007 |
| PCS (points) | 14.2 ± 7.4 | 10.5 ± 4.1 | 4.8 ± 2.5 | 12.3 ± 6.7 | 5.2 ± 3.3 | 1.7 ± 1.4 | 10.005 | .002** | 28.452 | <.001** | .853 | .430 | 0.022 |
| Rumination | 9.7 ± 5.4 | 7.2 ± 2.9 | 2.4 ± 1.2 | 7.2 ± 5.7 | 4.2 ± 3.1 | 1.5 ± 1.1 | 6.167 | .015* | 19.240 | <.001** | .531 | .590 | .009 |
| Helplessness | 2.6 ± 1.9 | 2.2 ± 2.0 | 2.4 ± 1.2 | 3.5 ± 2.3 | 1.1 ± .7 | .5 ± .6 | 3.540 | .064 | 7.430 | .001** | 5.120 | .008** | .097 |
| Magnification | 1.7 ± 1.7 | 1.2 ± 1.3 | .5 ± .9 | 1.5 ± 2.7 | .6 ± 1.4 | .3 ± .7 | .597 | .442 | 3.783 | .027* | .171 | .843 | .004 |
| HADS (points) | 11.0 ± 3.1 | 8.4 ± 2.1 | 5.7 ± 1.4 | 12.7 ± 3.8 | 7.9 ± 2.1 | 2.0 ± 1.3 | 1.130 | .291 | 56.170 | <.001** | 7.870 | <.001** | .076 |
| DASH (points) | 70.8 ± 5.9 | 42.5 ± 5.8 | 35.2 ± 5.5 | 73.2 ± 5.8 | 33.5 ± 7.1 | 19.9 ± 2.8 | 32.000 | <.001** | 425.800 | <.001** | 15.900 | <.001** | .032 |
PBI = physical function-based interventions; ADOC-H = aid for decision-making in occupation choice for hand; ROM = range of motion; NRS = numerical rating scale; PCS = pain catastrophizing scale; HADS = Hospital Anxiety and Depression Scale; DASH = disabilities of the arm, shoulder, and hand. Values are expressed as mean ± standard deviation. Two-way repeated measures analysis of variance; *p < .05, **p < .01.
For the main effect; group, the PCS total score (F [1,77] = 10.005, p = .002, η 2 = .069), PCS rumination score (F [1,77] = 6.167, p = .015, η 2 = .050), and DASH score (F [1,77] = 32.000, p < .001, η 2 = .032) had significant main effects. For the main effect; time, we detected significant main effects for all outcome measures (p < .01). There was a significant effect and interaction of time and group on the PCS helplessness score (F [2,77] = 5.120, p = .008, η 2 = .097), HADS score (F [2,77] = 7.870, p < .001, η 2 = .076), and DASH score (F [2,77] = 15.900, p < .001, η 2 = .032).
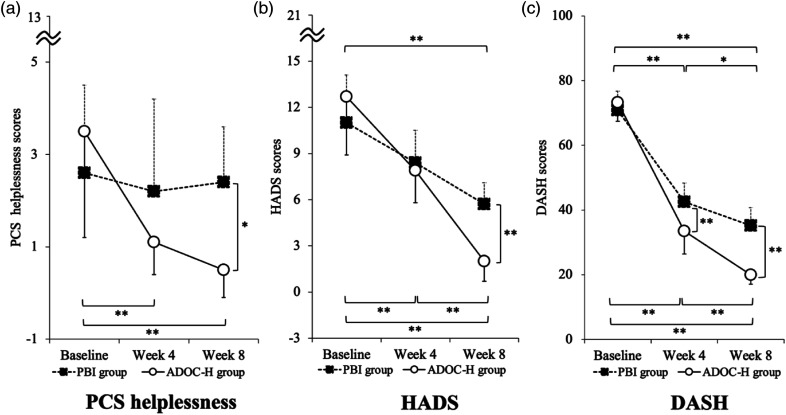
To further analyze the time-course effects and effects of OBI using ADOC-H, we performed Bonferroni correction for multiple comparisons for the outcome measures that showed an interaction. The results of Bonferroni’s multiple comparison tests and the percentage of outcome measures that showed an interaction at the baseline, fourth postoperative week, and eighth postoperative week for all patients are shown in Figure 3.
Figure 3.
Longitudinal changes in outcome measures at baseline and week 4 and week 8 after surgery with respect to the group. (a) PCS helplessness, (b) HADS, (c) DASH. PBI = physical function-based interventions; ADOC-H = aid for decision-making in occupation choice for hand; PCS = pain catastrophizing scale; HADS = Hospital Anxiety and Depression Scale; DASH = disabilities of the arm, shoulder, and hand. Bonferroni test; *significant difference between groups (p < .05); **significant difference between groups (p < .001).
The PCS helplessness scores were not significantly different from baseline to the eighth postoperative week in the PBI group over time, whereas they were significantly different in the ADOC-H group (p < .01). In the eighth postoperative week, there was a difference between groups, with the ADOC-H group showing better results (p = .011). The HADS and DASH scores showed significant improvement over time in both groups. However, a significant difference was observed between the groups at the eighth postoperative week, with the ADOC-H group exhibiting better outcomes (p < .01).
There was no significant difference in grip strength at the eighth postoperative week between the ADOC-H (13.8 ± 2.65 kg) and PBI (13.2 ± 3.37 kg) groups (p = .58).
Significant improvements were observed in both performance scores (baseline vs. fourth postoperative week, p < .001; baseline vs. eighth postoperative week, p < .0019; fourth postoperative week vs. eighth postoperative week postoperatively, p = .039) and satisfaction scores (baseline vs. fourth postoperative week, p < .001; baseline vs. eighth postoperative week, p < .001; fourth postoperative week vs. eighth postoperative week, p < .001) for occupational goals.
Discussion
The results of this study suggest that in patients with DRF, OBI using the ADOC-H combined with PBI has a better effect than PBI alone in improving difficulty using the injured hand in daily activities, pain catastrophizing, and anxiety. This case-control study of 28 patients was compared to a previous case series of eight patients (Ohno et al., 2021); the larger sample size extends the previous findings showing the efficacy of OBI using the ADOC-H for patients with DRF. Most studies on hand therapy for patients with DRF are related to PBI, with few reports on the effects of OBI (Takata et al., 2019). Therefore, we consider the results of this study to be beneficial, as they present a specific intervention protocol for OBI and its effectiveness.
This study showed that the ADOC-H group improved the performance and satisfaction scores of occupational goals over time, as well as in PCS helplessness and HADS. Carpenter et al. reported that improvements in occupational performance were associated with improvements in psychological aspects such as anxiety (Carpenter et al., 2001). One possible reason for the improvement only in helplessness on the PCS may be the difference in trend for each PCS subscale. One study examining the association between PCS subscale and disability in daily activities for patients with DRF reported that only PCS helplessness was associated with disability in daily activities (Kataoka et al., 2018). In other words, the use of the injured hand in daily activities is facilitated in the course of achieving the occupational goals formulated in the ADOC-H, which may lead to improvement of anxiety and pain catastrophizing.
OBI commonly begins with establishing occupational goals initially, as the intervention uses activities consistent with the goals identified by the patient (Fisher, 2013). However, a lack of information after DRF often contributes to discrepancies between therapists and patients, making it challenging to set occupational goals (Stern et al., 2022). Sepucha et al. reported that using decision-making tools during explanations to patients with musculoskeletal disorders can improve their knowledge and facilitate shared decision-making (Sepucha et al., 2017). Information is more easily remembered when presented in illustrations than in words (Shepard, 1967), and ADOC-H, which uses illustrations, can facilitate effective communication between patients and therapists. The ADOC-H has 16 ADL and IADL categories, further subdivided into 130 illustrated items that can be discussed in detail and step-by-step by therapists and patients (Ohno et al., 2017). The use of the ADOC-H in this study allowed the therapist and patient to share occupational goals by identifying activities that were anxious or difficult to perform when using the injured hand (Ohno et al., 2017).
Limitations and Future Directions
This was a retrospective case-control study, in which the two groups were divided according to the timing of the intervention. Therefore, there was no blinding to the intervention and data collection; thus, the possibility of selection and treatment bias cannot be ruled out. To support our results, the effect of OBI using ADOC-H needs to be further investigated in randomized controlled trials with improved design.
Conclusion
The results suggest that OBI using the ADOC-H combined with PBI for patients with DRF encourages the use of the injured hand in daily activities, improves satisfaction, and reduces fear and anxiety regarding pain. Therefore, the ADOC-H may be a clinically useful tool for facilitating OBI in patients with DRF. The overall findings emphasize the need for properly conducted assessor-blinded randomized controlled trials in the future.
Acknowledgments
The authors thank the patients who participated in this study.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Wataru Kukizaki https://orcid.org/0000-0003-4332-5617
References
- Allen G, Galer B.S, Schwartz L. (1999). Epidemiology of complex regional pain syndrome: a retrospective chart review of 134 patients. Pain, 80(3), 539–544. 10.1016/S0304-3959(98)00246-2 [DOI] [PubMed] [Google Scholar]
- Baron J. A., Karagas M., Barrett J., Kniffin W., Malenka D., Mayor M., Keller R. B. (1996). Basic epidemiology of fractures of the upper and lower limb among Americans over 65 years of age. Epidemiology, 7(6), 612–618. 10.1097/00001648-199611000-00008 [DOI] [PubMed] [Google Scholar]
- Carpenter L., Baker G. A., Tyldesley B. (2001). The use of the Canadian occupational performance measure as an outcome of a pain management program. Canadian Journal of Occupational Therapy. Revue Canadienne d’Ergotherapie, 68(1), 16–22. 10.1177/000841740106800102 [DOI] [PubMed] [Google Scholar]
- Cohen J. (1992). A power primer. Psychological Bulletin, 112(1), 155–159. 10.1037//0033-2909.112.1.155 [DOI] [PubMed] [Google Scholar]
- Dilek B., Yemez B., Kizil R., Kartal E., Gulbahar S., Sari O., Akalin E. (2012). Anxious personality is a risk factor for developing complex regional pain syndrome type I. Rheumatology International, 32(4), 915–920. 10.1007/s00296-010-1714-9 [DOI] [PubMed] [Google Scholar]
- Edwards B. J., Song J., Dunlop D. D., Fink H. A., Cauley J. A. (2010). Functional decline after incident wrist fractures—study of osteoporotic fractures: Prospective cohort study. BMJ, 341, c3324. 10.1136/bmj.c3324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faul F., Erdfelder E., Lang A. G., Buchner A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. 10.3758/bf03193146 [DOI] [PubMed] [Google Scholar]
- Fisher A. G. (2013). Occupation-centred, occupation-based, occupation-focused: Same, same or different? Scandinavian Journal of Occupational Therapy, 20(3), 162–173. 10.3109/11038128.2012.754492 [DOI] [PubMed] [Google Scholar]
- Gummesson C., Atroshi I., Ekdahl C. (2003). The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: Longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskeletal Disorders, 4(7765), 11. 10.1186/1471-2474-4-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen A. Ø., Kristensen H. K., Cederlund R., Möller S., Tromborg H. (2020). An occupation-based intervention in patients with hand-related disorders grouped using the sense of coherence scale-A randomized controlled trial. Journal of Hand Therapy, 33(4), 455–469. 10.1016/j.jht.2019.12.009 [DOI] [PubMed] [Google Scholar]
- Hiraga Y., Hisano S., Mizunoe A., Nomiyama K. (2021). The mediating effect of psychological factors on the relationship between pain intensity and wrist joint function: A longitudinal study with mediation analysis. Disability and Rehabilitation, 43(13), 1814–1818. 10.1080/09638288.2019.1676318 [DOI] [PubMed] [Google Scholar]
- Japanese Orthopaedic Association (JOA) . (2017). Clinical practice guideline on the management of distal radius fractures. The Japanese orthopaedic association (2nd ed.). Nabkodo, Co., Ltd. [in Japanese]. [Google Scholar]
- Jensen M. P., Karoly P., Braver S. (1986). The measurement of clinical pain intensity: A comparison of six methods. Pain, 27(1), 117–126. 10.1016/0304-3959(86)90228-9 [DOI] [PubMed] [Google Scholar]
- Kataoka N., Kazuki H., Miyuki I., Hirochika K., Yoshisuke I. (2018). Association between pain catastrophizing and occupational performance in patients with distal radius fractures. Journal of Japan Hand Therapy Society, 11(1), 41–45. [in Japanese]. [Google Scholar]
- Ohno K., Saito K., Matsumoto H., Tomori K., Sawada T. (2021). The clinical utility of a decision-aid to facilitate the use of the hand in real-life activities of patients with distal radius fractures: A case study. Journal of Hand Therapy, 34(3), 341–347. 10.1016/j.jht.2020.03.002 [DOI] [PubMed] [Google Scholar]
- Ohno K., Tomori K., Takebayashi T., Sawada T., Nagayama H., Levack W. M., Domen K., Higashi T. (2017). Development of a tool to facilitate real life activity retraining in hand and arm therapy. British Journal of Occupational Therapy, 80(5), 310–318. 10.1177/0308022617692602 [DOI] [Google Scholar]
- Osman A., Barrios F. X., Gutierrez P. M., Kopper B. A., Merrifield T., Grittmann L. (2000). The pain catastrophizing scale: Further psychometric evaluation with adult samples. Journal of Behavioral Medicine, 23(4), 351–365. 10.1023/a:1005548801037 [DOI] [PubMed] [Google Scholar]
- Sepucha K., Atlas S. J., Chang Y., Dorrwachter J., Freiberg A., Mangla M., Rubash H. E., Simmons L. H., Cha T. (2017). Patient decision Aids improve decision quality and patient experience and reduce surgical rates in routine orthopaedic care: A prospective cohort study. Journal of Bone and Joint Surgery. American Volume, 99(15), 1253–1260. 10.2106/JBJS.16.01045 [DOI] [PubMed] [Google Scholar]
- Shepard R. N. (1967). Recognition memory for words, sentences, and pictures. Journal of Verbal Learning and Verbal Behavior, 6(1), 156–163. 10.1016/S0022-5371(67)80067-7 [DOI] [Google Scholar]
- Stern B. Z., Njelesani J., Howe T. H. (2022). Transitioning from hurting to healing: Self-management after distal radius fracture. Disability and Rehabilitation, 44(21), 1–10. 10.1080/09638288.2021.1962990 [DOI] [PubMed] [Google Scholar]
- Takata S. C., Wade E. T., Roll S. C. (2019). Hand therapy interventions, outcomes, and diagnoses evaluated over the last 10 years: A mapping review linking research to practice. Journal of Hand Therapy, 32(1), 1–9. 10.1016/j.jht.2017.05.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tremayne A., Taylor N., McBurney H., Baskus K. (2002). Correlation of impairment and activity limitation after wrist fracture. Physiotherapy Research International, 7(2), 90–99. 10.1002/pri.245 [DOI] [PubMed] [Google Scholar]
- Weinstock-Zlotnick G., Mehta S. P. (2019). A systematic review of the benefits of occupation-based intervention for patients with upper extremity musculoskeletal disorders. Journal of Hand Therapy, 32(2), 141–152. 10.1016/j.jht.2018.04.001 [DOI] [PubMed] [Google Scholar]
- Zigmond A. S., Snaith R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), 361–370. 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]