Abstract
Background
Social isolation and loneliness are more common in older adults and are associated with a serious impact on their well‐being, mental health, physical health, and longevity. They are a public health concern highlighted by the COVID‐19 pandemic restrictions, hence the need for digital technology tools to enable remotely delivered interventions to alleviate the impact of social isolation and loneliness during the COVID‐19 restrictions.
Objectives
To map available evidence on the effects of digital interventions to mitigate social isolation and/or loneliness in older adults in all settings except hospital settings.
Search Methods
We searched the following databases from inception to May 16, 2021, with no language restrictions. Ovid MEDLINE, Embase, APA PsycInfo via Ovid, CINAHL via EBSCO, Web of Science via Clarivate, ProQuest (all databases), International Bibliography of the Social Sciences (IBSS) via ProQuest, EBSCO (all databases except CINAHL), Global Index Medicus, and Epistemonikos.
Selection Criteria
Titles and abstracts and full text of potentially eligible articles were independently screened in duplicate following the eligibility criteria.
Data Collection and Analysis
We developed and pilot tested a data extraction code set in Eppi‐Reviewer and data were individually extracted and coded based on an intervention‐outcome framework which was also used to define the dimensions of the evidence and gap map.
Main Results
We included 200 articles (103 primary studies and 97 systematic reviews) that assessed the effects of digital interventions to reduce social isolation and/or loneliness in older adults. Most of the systematic reviews (72%) were classified as critically low quality, only 2% as high quality and 25% were published since the COVID‐19 pandemic. The evidence is unevenly distributed with clusters predominantly in high‐income countries and none in low‐income countries. The most common interventions identified are digital interventions to enhance social interactions with family and friends and the community via videoconferencing and telephone calls. Digital interventions to enhance social support, particularly socially assistive robots, and virtual pets were also common. Most interventions focused on reducing loneliness and depression and improving quality of life of older adults. Major gaps were identified in community level outcomes and process indicators. No included studies or reviews assessed affordability or digital divide although the value of accessibility and barriers caused by digital divide were discussed in three primary studies and three reviews. Adverse effects were reported in only two studies and six reviews. No study or review included participants from the LGBTQIA2S+ community and only one study restricted participants to 80 years and older. Very few described how at‐risk populations were recruited or conducted any equity analysis to assess differences in effects for populations experiencing inequities across PROGRESS‐Plus categories.
Authors' Conclusions
The restrictions placed on people during the pandemic have shone a spotlight onto social isolation and loneliness, particularly for older adults. This evidence and gap map shows available evidence on the effectiveness of digital interventions for reducing social isolation or loneliness in older adults. Although the evidence is relatively large and recent, it is unevenly distributed and there is need for more high‐quality research. This map can guide researchers and funders to consider areas of major gaps as priorities for further research.
1. PLAIN LANGUAGE SUMMARY
1.1. Evidence for digital interventions to reduce social isolation and loneliness in older adults is unevenly distributed and most existing reviews are of critically low quality
Mapping the evidence for digital interventions to reduce social isolation and loneliness in older adults shows that many of the systematic reviews are of critically low quality. Most come from high‐income countries, with sparse reporting of community‐level outcomes.
1.2. What is this EGM about?
Social isolation and loneliness are common in older adults and have been highlighted during the COVID‐19 pandemic. Social isolation and loneliness pose a significant concern because of their impact on older adults' well‐being, mental health, physical health and longevity.
Older adults can use digital interventions to maintain existing connections or develop new connections. This was especially evident during the COVID‐19 pandemic, with social distancing and lockdown measures in place. Decisionmakers need to know which digital interventions can reduce social isolation and loneliness in older adults.
1.3. What is the aim of this EGM?
This EGM aims to show available evidence from systematic reviews and primary studies on the effects of digital interventions to reduce social isolation and/or loneliness among older adults in all settings except hospital settings.
1.4. What studies are included?
The EGM includes 200 articles (97 systematic reviews and 103 primary studies) that assessed how digital interventions can reduce social isolation and loneliness in older adults. The studies had to report the effect of digital interventions and could come from any region.
1.5. What are the main findings of this gap map?
The evidence is unevenly distributed geographically, with most from high‐income countries and none from low‐income countries. Over 70% of the systematic reviews have critically low quality and 25% have been published since the pandemic began.
The most common interventions are digital interventions to enhance social interactions with family, friends and the community via videoconferencing and telephone calls. Digital interventions to enhance social support, particularly socially assistive robots and virtual pets, were also common.
Most interventions focus on reducing loneliness and depression and improving quality of life of older adults.
Community level outcomes and process indicators are hardly reported, and no included studies or reviews assess affordability or lack of accessibility, although the value of accessibility and barriers caused by lack of accessibility were discussed in three studies and three reviews. Adverse effects are reported in very few studies and reviews.
Participants from the LGBTQIA2S+ community are not included in any study or review and only one study restricted participants to 80 years and older. Very few studies or reviews describe how at‐risk populations were recruited or conduct any equity analysis to assess differential effects for populations experiencing inequities across PROGRESS‐Plus factors.
1.6. What do the findings of the map mean?
This map is the first step towards identifying which digital interventions are effective for reducing social isolation and loneliness in older adults. The EGM contributes to the longer‐term aim of building an evidence architecture for the field, whereby the use of evidence becomes institutionalized in policy and practice.
Although the evidence is relatively large and recent, it is unevenly distributed and there is need for more high‐quality research. This map can guide researchers and funders to consider areas of major gaps as priorities for further research.
1.7. How up‐to‐date is this EGM?
The authors searched for studies published up to May 2021.
2. BACKGROUND
2.1. Introduction
2.1.1. The problem, condition or issue
A large body of research shows that social isolation and loneliness are associated with a serious impact on older adult's well‐being, mental health, physical health, and longevity (Leigh‐Hunt, 2017; Menec, 2020). Their effect on mortality is comparable to, or even greater, than other well‐established risk factors such as smoking, obesity, and physical inactivity (Holt‐Lunstad, 2015; Ibarra, 2020; Menec, 2020; Windle, 2012).
Social isolation and loneliness are more common in older adults and are described as multidimensional concepts with different methods of measurement leading to variations in the prevalence. The prevalence ranges from 5% to 43% depending on the study and region (Chen, 2016; Donovan, 2020; Ibarra, 2020; Leigh‐Hunt, 2017). Risk factors include living alone, impaired mobility, experiencing a major life transition change (e.g., loss of spouse or other primary network members), limited income or resources, cognitive impairment, inadequate social support, and geographic location (Cohen‐Mansfield, 2015; Donovan, 2020; Findlay, 2003; Ibarra, 2020).
Although they are related, social isolation and loneliness are two distinct concepts and one may occur without the other. Social isolation is the objective state of lack of interactions with others and the wider community or lack of social relationships (Donovan, 2020; Ibarra, 2020; Leigh‐Hunt, 2017; Menec, 2020). Loneliness is the subjective painful feeling of the absence of a social network or a companion or perception of unmet emotional and social needs resulting from a mismatch between the desired and actual experience of the quality or quantity of social relationships (Cacioppo, 2009; Cacioppo, 2014; Menec, 2020; Perlman, 1981; Prohaska, 2020; WHO, 2021). Therefore, an individual can have a social network and be lonely or a socially isolated individual may not feel lonely. An understanding of the differences in these concepts is important for research in the development of appropriate and effective interventions, and standardizing outcome measurements and also to guide the choice of appropriate interventions for socially isolated or lonely individuals (Fakoya, 2020; WHO, 2021).
Social isolation and loneliness among older adults are priority public health problems, as well as national and international policy issues, due to the negative impact on their mental and physical health and longevity (Cattan, 2005; Gardiner, 2018; Shah, 2020; Shah, 2021; WHO, 2020; WHO, 2021). The World Health Organization (WHO) decided, as part of the Decade of Healthy Ageing, to address social isolation and loneliness as a priority issue that cuts across the main action areas of the Decade (WHO, 2020). It is also increasingly being recognized as a public health concern due to the social distancing measures during the COVID‐19 pandemic (Brooke, 2020; Shah, 2020; Shah, 2021; Williams, 2021). For example, the average person's daily number of contacts was reduced by up to 74% and almost one quarter of adults in the UK experienced loneliness when living under lockdown (Williams, 2021). Hence the need for digital technology tools to enable remotely delivered interventions to alleviate the impact of social isolation and loneliness during the COVID‐19 restrictions.
There are challenges associated with access to digital interventions and the use of remotely delivered interventions to reduce social isolation and loneliness. Disparities in access to digital interventions and the use of remotely delivered interventions is a growing concern, especially for older adults and during the COVID‐19 restrictions (Budd, 2020; Jopling, 2020; Watts, 2020; Williams, 2021). Many older adults lack digital skills and the confidence to access online services and support. Other barriers are affordability and accessibility of technology, broadband or Wi‐Fi, data poverty (i.e., lack of accessibility to wireless internet connection), geographic divide (rural and urban, high income and low‐ and middle‐income countries). Concerns with digital technology use have also been raised regarding privacy invasion, legal, ethical and clinical data governance through data sharing and access to information (Budd, 2020; NASEM, 2020). Ethical concerns with any intervention to prevent social isolation and loneliness include issues with accessibility, acceptability, cost, feasibility, autonomy, and informed concern. Privacy concerns may intersect with accessibility issues due to cognitive impairment or involvement of other family members or caregivers. Informed consent provided at the beginning of research may not cover the future use of data created, raising issues with ongoing consent and the ability to withdraw consent. There is also the risk of digital technology exacerbating rather than reducing social isolation, for example, social robots replacing meaningful human contact can result in increased sense of loneliness, deception and infantilization of older adults (NASEM, 2020). Equitable access and support are key in addressing the digital divide.
2.1.2. The intervention
A wide variety of interventions have been developed to reduce social isolation or loneliness among older adults. These interventions use different strategies and target different aspects such as facilitating social connections or service provision. They are implemented at different levels such as one‐on‐one or group focused. Although several systematic reviews have evaluated the effectiveness of different types of interventions for social isolation and loneliness in older adults, their findings have sometimes been conflicting (Cattan, 2005; Cohen‐Mansfield, 2015; Dickens, 2011; Findlay, 2003; Gardiner, 2018; Hagan, 2014; Victor, 2018).
Digital interventions have become a particular focus of interest, due partly to the social distancing and lock‐down measures introduced to combat the COVID‐19 pandemic and to the rapidly increasing role technology – particularly the internet, mobile devices, social media and Internet of things (IoT) – has played in the last 10–15 years in mediating social relations (Boulton, 2020; Brooke, 2020; Budd, 2020; Falk, 2021; Shah, 2020; UCLG, 2020; WHO, 2021; Zanella, 2020). They have been used in different sectors (e.g., health care, social services, the community) and in various ways, including digital epidemiological surveillance, rapid case identification, interruption of community transmission, public communication, and provision of clinical care and income support and livelihood opportunities in the COVID‐19 crisis.
Digital interventions have also been used to mitigate social isolation or loneliness in older adults by facilitating social interaction or by delivering programs or services (Boulton, 2020; Chen, 2016; Chipps, 2017; Findlay, 2003; Ibarra, 2020; Khosravi, 2016; Noone, 2020; Shah, 2021; Thangavel, 2022). They have generally been described as technology‐based interventions to improve communication and social connection among older adults and there is no clear framework for their categorization (Fakoya, 2020). For example, they have been categorized as one‐on‐one or group‐based interventions (Cohen‐Mansfield, 2015; Dickens, 2011; Masi, 2011; Poscia, 2018) or based on four strategies or type (Masi, 2011) as:
interventions for improving social skills (e.g., computer and internet training and use with a focus on reducing social isolation or loneliness, online university of the third age);
interventions for enhancing social support that offer regular contacts, care, or companionship (e.g., telecare with a component to improve social connections, personal reminder information and social management systems (PRISMS), social robots or virtual pets, video games, 3D virtual environments or virtual spaces with trained coaches, conversational agents, or messaging capabilities);
interventions for enhancing social interaction (videoconferencing, supported video communication, internet chat facilities, social networking sites, online discussion groups and forums, telephone befriending)
interventions for social cognitive training (low intensity psychosocial interventions, internet‐delivered cognitive behavioral therapy (CBT), mindfulness interventions).
In mapping the body of available evidence, we categorized interventions by strategies to enable exclusive coding of interventions in categories and subcategories such that an intervention will fit into a single subcategory and not overlap with another on the evidence and gap map.
2.1.3. Why it is important to develop the EGM
Several recent reviews of digital interventions for reducing social isolation and loneliness among older adults indicate there is growing research in this topic area most likely due to the ageing population (Boulton, 2020; Chen, 2016; Chipps, 2017; Findlay, 2003; Ibarra, 2020; Khosravi, 2016; Noone, 2020; Shah, 2021). In addition, the COVID‐19 pandemic restrictions have led to a dramatic expansion in the demand for digital technology interventions by people without access including older adults, for the provision of basic services like healthcare, education, and connections with other people (UCLG, 2020). Although there is a very wide range of such interventions, findings on their effectiveness, have sometimes been inconsistent (WHO, 2021). The body of evidence supporting their use is rapidly expanding, dispersed and uneven with lack of consistent terminology. Therefore, the best use of resources at this point for building the evidence architecture needed would be to develop an evidence and gap map on digital interventions to reduce social isolation and loneliness among older adults. This evidence and gap map will collate the evidence and display clusters of evidence and gaps in evidence that will serve as a resource to guide prioritization of further research and increase the accessibility and use of evidence for informed decision making by stakeholders including citizens, patients, caregivers, health and social care providers, policy makers and researchers.
2.1.4. Existing EGMs and/or relevant systematic reviews
Recent reviews of digital interventions suggest that (a) there is a very wide range of such interventions; (b) findings on their effectiveness, although sometimes positive, are frequently mixed, inconclusive or uncertain; and (c) the technologies involved are developing rapidly (e.g., artificial intelligence, conversational agents, 3D virtual environments, video‐games, social networking tools) (Boulton, 2020; Chen, 2016; Chipps, 2017; Ibarra, 2020; Khosravi, 2016; Noone, 2020; Shah, 2021).
There is an evidence and gap map on specific remotely delivered interventions (i.e., befriending, social support, and low intensity psychosocial interventions) to reduce social isolation and loneliness among older adults (Boulton, 2020). It is based on a rapid review of reviews with systematic review evidence on befriending, social support, and low intensity psychosocial interventions that are delivered remotely to older adults, excluding caregivers. Study‐level evidence is limited to 18 individual studies in the 5 included systematic reviews.
Our evidence and gap map will be more comprehensive with a broader scope of all types of digitial interventions for older adults including older caregivers. It will examine up to date evidence from systematic reviews as well as primary studies and map available evidence to identify gaps and clusters in interventions and outcomes assessed.
3. OBJECTIVES
The aim is to map available evidence on the effects of digital interventions to mitigate social isolation and/or loneliness in older adults in all settings except hospital settings.
Specific objectives are as follows:
-
1.
To identify existing evidence from primary studies and systematic reviews on the effects of digital interventions to reduce social isolation and/or loneliness in older adults.
-
2.
To identify research evidence gaps for new high‐quality primary studies and systematic reviews.
-
3.
To highlight evidence of health equity considerations from included primary studies and systematic reviews.
4. METHODS
We followed the Campbell Collaboration guidance for producing an evidence and gap map (White, 2020) described in the evidence and gap map protocol for this project (Welch, 2022).
4.1. Evidence and gap map: Definition and purpose
Evidence and gap maps are a systematic evidence synthesis product with a visual presentation of existing evidence relevant to a specific research question (Snilstveit, 2013; White, 2020). They display areas with collections or gaps in evidence and the quality of available evidence.
The evidence and gap map is typically a two dimensional matrix with interventions as row headings and outcomes as column headings (Snilstveit, 2016; White, 2020). Each cell within the matrix shows the studies with evidence on the corresponding intervention and outcome. This map identifies areas of evidence as well as any gaps in research related to using digital interventions for social isolation and/or loneliness among older adults.
4.2. Framework development and scope
We developed an intervention‐outcome framework for this evidence and gap map through a consultative process with stakeholders and adaptation of existing frameworks from systematic reviews, conceptual papers, and reports from stakeholder organizations.
A refined version of the WHO Classification of Digital Health Interventions framework (WHO, 2018) was initially considered at the Stakeholder consultation meeting on April 8, 2021. The WHO framework was developed to categorize the different ways in which digital and mobile technologies are used to support healthcare. The stakeholders found the typology of interventions to be too healthcare focused. The consensus was that a more user intuitive typology of interventions was needed to ensure the useability of this evidence and gap map for a larger audience including older adults. A needs‐based approach was preferred as interventions are most effective when they meet the needs and specific circumstances of the older adults (Abdi, 2019; Findlay, 2003; ten Bruggencate, 2019; WHO, 2020).
We identified other relevant frameworks from existing reviews and conceptual papers. We chose two frameworks which used a needs‐based approach (Jopling, 2020) and a strategy‐based approach (Masi, 2011) to address social isolation and loneliness and adapted them for our evidence and gap map.
The needs‐based framework (Jopling, 2020) considers approaches to address loneliness and social isolation that are used in communities to achieve three outcomes: maintain and improve existing relationships or connections, support people to develop new connections, and to change negative thinking about their relationships. The approaches include connector services that reach out to understand the needs of older adults and provide support to meet the needs, gateway infrastructures through which people can connect with others, direct solutions or interventions to reduce loneliness and social isolation, and system‐level approaches that create environments in communities to facilitate tackling loneliness and social isolation (Figure 1).
Figure 1.
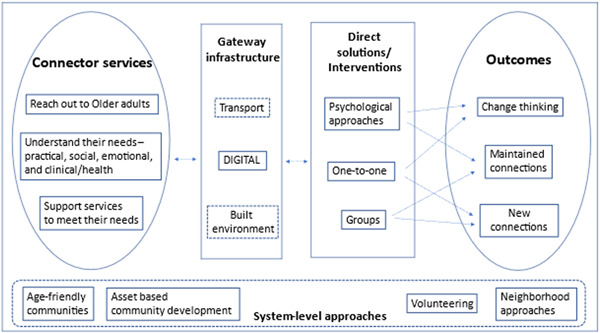
Needs‐based approach framework (Adapted from Jopling et al., 2020).
The intervention categories in this framework do not provide mutually exclusive categorization of digital interventions. For example, many digital interventions such as computer and internet training, video chats, online CBT may be one‐to‐one, or group based. Hence the need for the second framework.
The strategy‐based model (Masi, 2011) describes strategies used in loneliness reduction interventions based on the understanding of the nature of loneliness and social isolation and how they affect people (Figure 2). Interventions were also categorized based on the format or level of delivery (as one‐on‐one or group interventions) or mode of delivery (technology‐based and non‐technology‐based interventions).
Figure 2.
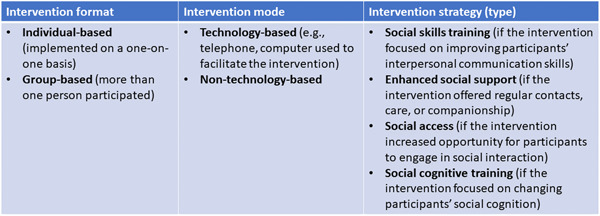
Strategy‐based approach framework (Adapted from Masi et al., 2011).
We used an intervention‐outcome framework where digital interventions of interest will be coded by the strategies to reduce loneliness and social isolation: strategies for (1) improving social skills, (2) enhancing social support, (3) enhancing social interaction, (4) social cognitive training, and (5) multicomponent strategies; as well as by the type of intervention (e.g., computer and internet training to reduce social isolation and loneliness, video chats, telephone befriending, telecare with a component to improve social connections, online CBT). See Supporting Information: Appendix [Link], [Link] for the glossary of key concepts.
Since the framework was bi‐dimensional (interventions and outcomes), the needs of socially isolated and lonely older adults were used as a filter on the map and coded interventions were mapped to the needs.
4.3. Outcomes
The impacts of interventions to prevent social isolation and loneliness have been measured at different levels – individual, community or societal, and process and implementation (Windle, 2012). In our framework, we considered outcomes that have been identified as indicators of social connection and they were categorized based on the impact and level of influence of the interventions:
individual outcomes – loneliness, social isolation, social connectedness, quality of life, anxiety/depression, confidence level, information, communication and technologies (ICT) knowledge and experience, adverse effects;
community outcomes – social support, social engagement, social cohesion, social capital, digital divide (disparities in access to technological interventions);
process indicators – acceptance, adherence, technology use, feasibility, cost‐effectiveness, affordability, barriers.
4.4. Stakeholder engagement
We convened an advisory board of 30 stakeholders from organizations such as the International Red Cross, Canadian Red Cross, Agewell, Canadian Frailty Network, HelpAge, CanAge, Centre for Ageing Better, United Nation Department of Social and Economic Affairs, United Nations Fund for Population Activities (UNFPA), and the WHO. The group of stakeholders included representatives of these key organizations, policymakers, and academics with an interest in mitigating social isolation and loneliness in older adults. The advisory board provided comments on the intervention‐outcome framework. The WHO Classification of Digital Health Interventions framework was considered. Stakeholders suggested a simplified framework to fit the purpose of this evidence and gap map. The framework was revised based on their feedback, and stakeholders were consulted by email for their feedback on the revised framework included in this review.
We consulted with four citizens in two citizen focus groups between June and August 2021. Some iterations were suggested, that is, coding for interventions related to the need of finding purpose in later life, and capturing interventions related to recreation and physical activity. Affordability and access to technology were recommended for consideration as outcomes in the framework.
We created an anonymous survey with four questions and invited stakeholders including citizens by email to respond to the survey questions and provide their feedback on the revised framework and draft map.
4.5. Conceptual framework
Our conceptual framework (Figure 3) was based on the understanding of the needs of older adults, how social isolation and loneliness can occur and how they affect older adults' well‐being. The relationship between these variables can be explained by a potential pathway of effect illustrated in the conceptual framework going from risk factors and needs assessment for older adults to interventions, the mechanisms of change, and process indicators and outcomes.
Figure 3.
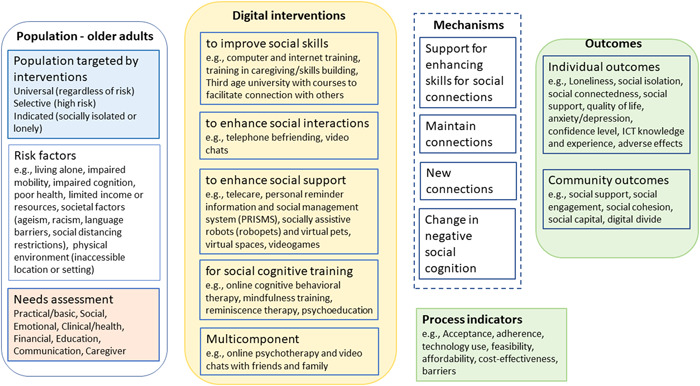
Conceptual framework.
4.5.1. Population targeted by interventions
Older adults are more susceptible to experiencing social isolation and loneliness, but risk exposure may vary with individual contexts. Older adults at risk of isolation and loneliness have been identified by their age, gender, place of residence or other factors (Elder, 2012; Fakoya, 2020; NASEM, 2020). Interventions may target all older adults regardless of their risk (universal) or a subpopulation of older adults who are at risk, for example, those living in nursing homes (selective) or may target those who are socially isolated or lonely (indicated).
4.5.2. Risk factors for social isolation and loneliness
Social isolation and loneliness have been associated with low social support and a disruption in social interactions established with other people at any level (individual, group, community, and societal or system) which can lead to unmet needs (Abdi, 2019; Donovan, 2020; Tomaka, 2006). Major changes in life such as change or loss of social network, social participation or role, physical health, mental health and financial resources can also lead to social isolation and loneliness (Donovan, 2020; Newall, 2019; Victor, 2005). Other risk factors for social isolation and loneliness include living alone, societal factors (racism, language barriers, ageism, social distancing and restrictions) and the physical environment (inaccessible location or community setting) (Berkman, 2000; DeGood, 2011; Donovan, 2020).
4.5.3. Needs assessment for older adults
Ageing is associated with a decline in physical and cognitive health, difficulty with mobility, activities of daily living and household routines which put older adults at risk of experiencing needs that require health and social support. These needs include social and emotional needs (social connections and companionship), civic engagement (meaningfulness and status, the need for having a purpose in later life or being able to contribute usefully to society), healthcare, housing, home modifications and maintenance, domestic assistance, mobility, nutrition and food security, personal care, education (skills development and learning), financial management, respite care, caregiver support, communication (language support or interpreters, information and assistance/referral services) (Abdi, 2019; Bedney, 2010; Henderson, 2008; Jopling, 2020; WHO, 2020).
Support services have been developed to satisfy the needs of older adults and to promote wellbeing and healthy ageing through social networks or relations (Abdi, 2019; Jopling, 2020; ten Bruggencate, 2019; WHO, 2020).
Social isolation and loneliness may be caused by multiple factors and people respond differently depending on their age and coping skills. It is therefore important to reach out to the older adults to understand their circumstances (the risk factors they are facing and their needs) to be able to provide tailored support for social connections or for accessing services as approaches to reduce social isolation and loneliness (Jopling, 2020; ten Bruggencate, 2019).
4.5.4. Digital interventions
Different approaches have been used to reduce social isolation and loneliness including facilitating social connections and providing social support. By providing social support services to meet their needs, opportunities for social connections could be created which could reduce social isolation and loneliness in older adults. Support for social connections and companionship or for accessing services can be provided through digital technology.
Based on the understanding of the nature and impact of social isolation and loneliness, different strategies have been used in digital interventions to mitigate social isolation and loneliness (Masi, 2011). We used these strategies as the typology of intervention categories. Since multiple factors may be involved, multicomponent strategies may also be used to address social isolation and loneliness. The categories include:
-
1.
interventions to improve social skills,
-
2.
interventions to enhance social interactions,
-
3.
interventions to enhance social support,
-
4.
interventions for social cognitive training, and
-
5.
multicomponent interventions.
4.6. Mechanisms
The impact of digital interventions can be achieved by four mechanisms of change:
-
1.
providing support to building skills for social connections (e.g., computer and internet training and use, online university of the third age),
-
2.
maintaining existing connections (e.g., video chat with family and friends, PRISMS to engage family and friends in helping receive care),
-
3.
creating new connections (e.g., telephone befriending programs, social networking sites, robots and virtual pets, videogames), and
-
4.
by changing negative social cognition (e.g., online CBT to teach lonely people to identify and free themselves from negative thoughts and feelings about their relations such as a perception of lack of intimate attachment to their friends or family).
These mechanisms do not map onto the four strategies since some interventions may reduce social isolation or loneliness through more than one mechanism. For example, social networking sites may be used to reduce social isolation and loneliness by maintaining existing connections and by creating new connections. Computer and internet training can be used to maintain connection with family and friends or to create new connections.
4.7. Process indicators and outcomes
The effects of interventions depend on how well the interventions were implemented. Process indicators measure activities or outputs that indicate whether the intervention was implemented as planned (Milstein, 1999). They are preconditions that contribute to the outcomes and are therefore considered proximal indicators of implementation processes or intermediate outcomes (Proctor, 2011).
Different levels of outcome measurements for the effects of digital interventions include:
process indicators – acceptance, adherence, technology use, feasibility, costs, barriers.
individual level outcomes – loneliness, social isolation, social connectedness, quality of life, anxiety/depression, confidence level, information, communication and technologies (ICT) knowledge and experience, adverse effects.
community level outcomes – social support, social engagement, social cohesion, social capital, digital divide (disparities in access to technological interventions).
We used this conceptual framework to define and code the dimensions (categories and subcategories of interventions and outcomes as well as filters) for the evidence and gap map.
4.8. Dimensions
4.8.1. Types of study design
Eligible study designs to be included weree completed or on‐going systematic reviews, and primary studies with any form of control group including randomized controlled trials (RCTs), and evaluative quasi‐experimental designs with a control group.
We included systematic and scoping reviews based on their PICO question if they explicitly described adequate search methods used to identify studies, eligibility criteria for selection of included studies, methods of critical appraisal of included studies and synthesis or analysis of included studies (Moher, 2015).
Quasi‐experimental design studies were considered eligible if the assignment of participants was based on allocation rules such as alternate assignment (quasi‐randomized studies), inclusion of a threshold on a continuous variable (regression discontinuity designs), exogenous variation in the treatment allocation (natural experiments) or other rules including self‐selection by investigators or participants, provided data were collected contemporaneously in a comparison group (non‐equivalent comparison group design), or an interrupted series design with at least three data points both before and after a discrete intervention (six‐period interrupted time series) (Waddington, 2014).
We excluded all studies that used less than six period interrupted time series design, or primary studies without a comparison group design like longitudinal cohort studies with no controls, and cross‐sectional studies. We also excluded literature reviews that were not sysematic reviews. However, systematic reviews which also include studies without a comparison group design will be included.
We did not include qualitative research.
4.8.2. Types of intervention/problem
We defined digital interventions as technology‐based interventions to improve communication and social connection. We considered all types of digital interventions with the aim to reduce social isolation and loneliness. These digital interventions were either one‐to‐one, or group based. They may focus on loneliness, social isolation, or both. We considered any frequency or duration of administration.
We included the following types of digital interventions categorized by strategies.
Interventions to improve social skills: these are interventions that focus on training in interpersonal social skills such as conversational skills with the aim to enable individuals to form and maintain meaningful relationships. Examples are computer and internet training and use to communicate with others, or online university of the third age which includes courses to facilitate communication with others. We excluded studies that assess computer and internet training for digital literacy and do not assess the use of internet to reduce social isolation or loneliness by focusing on improving social skills.
Interventions to enhance social support: these are interventions that offer support (e.g., regular contacts, care, or companionship) and guidance in finding and attending new activities or groups. They aim to help individuals make and maintain social connections. Examples include telecare with a component to improve social connections, PRISMS, online support groups and forums, social robots or virtual pets, video games, 3D virtual environments. We excluded studies that assess interventions for care without a communication component or a component to improve connecting with other people, for example, smart home technologies like sensors for monitoring falls, e‐health for clinical need only, online CBT for dementia care only, online referral systems for healthcare coordination.
Interventions to enhance social interactions: these are interventions that focus on improving the quality of relationships and increase opportunities for social interactions. They aim to promote connections with family/friends or community and include internet chat facilities, social networking sites, online discussion groups and forums or telephone befriending. Although telephone befrienders could also provide social support, we classify telephone befriending as an intervention to enhance social interactions since the main aim for the service is to connect regularly and build friendship with an older person (Boulton, 2020; Gardiner, 2018).
Interventions for social cognitive training: these are interventions that focus on changing negative thinking and feelings about social relationships. They aim to change behaviors, reduce maladaptive cognitions, and increase social connections. Examples include low intensity psychosocial interventions, internet‐delivered CBT, or mindfulness interventions.
See Table 1 for categories and other examples.
Table 1.
Intervention categories.
| Strategy‐based categories and subcategories | Examples |
|---|---|
| Interventions to improve social skills |
|
| |
| Interventions to enhance social interaction |
|
| |
| Interventions to enhance social support |
|
| |
| Social cognitive training interventions |
|
| Multicomponent interventions |
|
Comparators were no interventions, other interventions, or usual care.
4.8.3. Types of population
We included older adults, defined as 60 years of age or older (WHO, 2020). If studies included younger and older adults, we included the studies if data could be disaggregated. If data could not be disaggregated, we included studies if the mean age of all participants was at least 65 years of age. To be inclusive, studies or reviews which stated a focus on older adults without providing the age of participants were included.
4.8.4. Types of outcome measures
Outcomes included loneliness, social isolation, as well as other indicators of social connections. Potential harms such as ethical concerns, privacy violations, liability and cyber‐attacks as well as unintended consequences such as increase in social isolation and loneliness, were also included. Community outcomes such as social support, social engagement, social cohesion, social capital, and digital divide (disparities in access to technological interventions) as well as process indicators (acceptability, adherence, technology use, feasibility, affordability, cost‐effectiveness, and barriers), especially for vulnerable populations, were included (See Table 2).
Table 2.
Outcome categories.
| Outcomes | Acceptable measurements |
|---|---|
| Individual outcomes | |
| Loneliness | UCLA loneliness scale, de Jong‐Gierveld loneliness scale, other scales, for example, Social and Emotional Loneliness Scale, Hughes loneliness scale |
| Social isolation | Lubben's Social Network Scale, Social Network Index, PROMIS social isolation 6‐I scale |
| Social connectedness/interactions/networks or life satisfaction | Lee and Robin's Social Connectedness Scale; Number of contacts; Frequency of social interactions; Satisfaction with interaction; Index of support satisfaction; Support network satisfaction; Companionship scale satisfaction |
| Social support |
Duke‐UNC Functional Social Support Questionnaire; Social support scale by Schuster et al.; Hsiung's Social Support Behaviors Scale; Family and Friendship Contacts Scale; Personal Resource Questionnaire; Interpersonal Support Evaluation List (ISEL); e‐Diabetes Social Support Scale; a bespoke six‐item scale measuring women's perception of emotional and instrumental support |
| Well‐being/Quality of life | MOS SF‐36 Health Survey; Work and Social Adjustment Scale (WSAS); |
| Anxiety/depression | Beck Depression Inventory (BDI); Depression Adjective Check List (DACL) Form E; Geriatric depression scale; The Centre for Epidemiological Studies Depression Scale (CES‐D) |
| Confidence level | Rosenberg Self‐Esteem Scale |
| Information, communication and technology (ICT) knowledge and experience | Questionnaire |
| Adverse effects | Privacy violations, liability, cyber‐attacks, negative effect on well‐being from emotional attachment to devices |
| Community outcomes | |
| Social support | Duke‐UNC Functional Social Support Questionnaire, Social support scale, social Provisions scale |
| Social engagement | Engagement in Meaningful Activities Survey (EMAS) |
| Social cohesion | The Group Cohesion Scale‐Revised; Group Therapy Experience Scale, Group Environment Questionnaire |
| Social capital | The World Bank's integrated questionnaire for the measurement of social capital (SC‐IQ) |
| Digital divide | Lack of affordability/access to technology, lack of affordability/access to broadband or Wi‐Fi, data poverty, lack of digital skills or confidence to access services and support online |
| Process indicators | |
| Acceptability (technology adoption) | Various survey tools to measure acceptability |
| Adherence (training adherence) | Various survey tools to measure adherence |
| Technology use | Frequency of use |
| Feasibility | Various survey tools to measure feasibility |
| Affordability | Various survey tools to measure affordability |
| Cost‐effectiveness | Cost‐effectiveness analysis |
| Barriers | For example, language and cultural barriers, financial accessibility, hearing or vision impairments, personal barriers such as dislike of robopets, digital literacy, lack of familiarity with digital technologies, Lack of confidence in using digital technologies |
Outcomes were not used as eligibility criteria. However, eligible studies and systematic reviews did have a focus on social isolation and loneliness. Studies and reviews assessing interventions with a stated aim to reduce social isolation and loneliness were eligible. Those that assessed the effects of interventions on social isolation and/or loneliness as a primary outcome or considered other indicators of social connections including quality of life, anxiety/depression, social support, social engagement, social cohesion, and social capital were also included.
Studies and reviews assessing the effect of interventions on anxiety or depression with a focus on mental health rather than social isolation or loneliness were excluded.
4.8.5. Other eligibility criteria
Types of location/situation
We included all country settings as defined by the WHO regions (African Region, Region of the Americas, South‐East Asian Region, European Region, Eastern Mediterranean Region, Western Pacific Region) (WHO, 2019) and the World Bank classification by income: low‐income economies, lower‐middle income economies, upper‐middle income economies, high‐income economies (World Bank, 2021).
Primary studies and systematic reviews that did not report the countries were not excluded.
Types of settings
All settings except hospital settings were included, that is, people living in supportive care institutions (nursing home or long‐term care and assisted living facilities) and in the community (residential or personal home).
4.9. Search methods and sources
We designed a search strategy with an information scientist (DS) in consultation with Tomas Allen (WHO information specialist). We searched the following databases from inception to May 16, 2021 with no language restrictions: Ovid MEDLINE, Embase, APA PsycInfo via Ovid, CINAHL via EBSCO, Web of Science via Clarivate, ProQuest (all databases), International Bibliography of the Social Sciences (IBSS) via ProQuest, EBSCO (all databases except CINAHL), Global Index Medicus, and Epistemonikos. The full search strategies are in Supporting Information: Appendix [Link], [Link].
We screened reference lists of all included systematic reviews in Eppi‐Reviewer to identify additional studies. We also contacted stakeholders for information about ongoing studies.
4.10. Analysis and presentation
4.10.1. Report structure
The report has the standard sections: abstract, plain language summary, background, methods, results, discussion, and conclusion.
The report includes the flow of studies, included studies, excluded studies and any studies awaiting assessment, as well as synthesis of included studies. We presented the PRISMA flowchart and conceptual framework. We also included tables and figures that provide a summary of the distribution of primary studies and systematic reviews across the coding categories such as the type of studies, quality of the systematic reviews, types of interventions, needs, types of populations, outcomes, settings, and geographic distribution.
The evidence and gap map has interventions as the row dimension and outcomes as the column dimension. Bubbles of different sizes represent included studies and different colors are used to identify the primary studies and methodological quality of the systematic reviews. The filters used in the map depend on the number of included studies and coded information. See a sample of the map in Figure 4.
Figure 4.
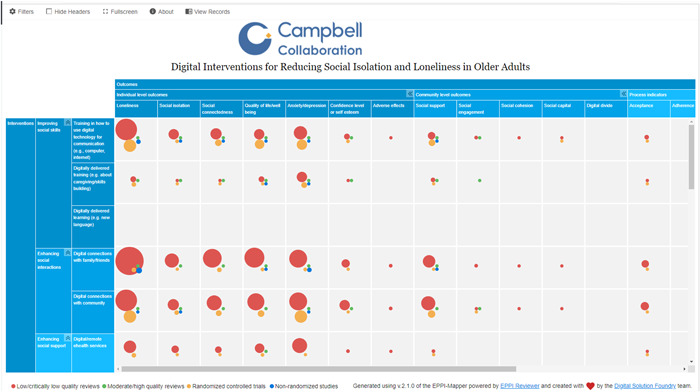
Sample map.
4.10.2. Filters for presentation
Additional dimensions of interest that were used as filters included the publication status of included studies, study design, World Bank classification by income (low‐income economies, lower‐middle income economies, upper‐middle income economies, high income economies), and WHO regions (African Region, Region of the Americas, South‐East Asian Region, European Region, Eastern Mediterranean Region, Western Pacific Region), setting (personal home, independent living/residential home, assisted living, long‐term care/nursing home), health status/condition.
We documented which needs beyond mitigating social isolation and/or loneliness of older adults are being met by digital interventions, using a framework developed from our citizen and stakeholder engagement consultation, which includes social and emotional needs, civic engagement and social participation, healthcare, housing, home modifications and maintenance, domestic assistance, mobility, nutrition and food security, personal care, education, financial management, respite care, caregiver support, communication.
We documented the focus of the intervention as aimed at social isolation, loneliness, or both. We also had filters for the intervention format, how technologies are used, as well as how training on how to use digital technology was delivered.
Equity analysis
We documented whether studies were focused on populations who are at risk or experiencing barriers to health and social care or health inequities across age, gender or sex, ethnicity, income, or other factors. We used the PROGRESS‐Plus acronym to describe factors associated with health inequities (O'Neill, 2014). For these studies, we documented how potentially vulnerable older adults are defined and identified (e.g., using case finding, outreach, screening).
In addition, for each study, we assessed whether studies analyzed differences in effects for populations experiencing inequities, using the PROGRESS factors (Place of residence (urban/rural), Race/ethnicity/culture and language, Occupation, Gender or sex, Religion, Education, Socioeconomic status, Social capital. We also assessed analysis across additional “Plus” factors which are known to be important for older adults, including age, disability, social frailty, health status, being socially isolated or at risk, being lonely or at risk, living situation, and digital literacy.
4.10.3. Dependency
Multiple reports of the same study were treated as one study. A study with multiple interventions or outcomes was shown multiple times on the map (for each intervention or outcome identified). Systematic reviews were mapped to the interventions and outcomes as defined by the question of the systematic review. Primary studies that met the eligibility criteria were mapped as well regardless of whether they are included in one or more systematic reviews.
4.11. Data collection and analysis
4.11.1. Screening and study selection
Titles and abstracts and full text of potentially eligible articles were screened independently following the eligibility criteria in duplicate (by VW, EG, VB, PG, TH, SA, NE, JE, HW and OD) using the Eppi‐Reviewer web‐based software program (Thomas, 2020). We screened systematic reviews based on their PICO questions. Disagreements were resolved by discussion. See Supporting Information: Appendix [Link], [Link] for detailed eligibility criteria.
We used machine learning text mining to support screening at the title and abstract stage. After screening approximately 10% of the titles and abstracts, we used the priority screening function which developed a classifier based on the probability of inclusion determined from the preliminary screening results. We, however, double screened all the search results to ensure all potentially eligible studies were captured for the full text screening stage.
We also screened reference lists of eligible systematic reviews to identify additional studies.
4.11.2. Data extraction and management
We developed and pilot tested a data extraction code set in Eppi‐Reviewer for data collection of the dimensions for the map (see extraction code in Supporting Information: Appendix [Link], [Link]). After the pilot test, members of the team (EG, VB, PG, TH, EB, AW, AA, and SD) individually extracted and coded data. Automation and text mining were not used for coding.
The coding categories included study characteristics (study design, publication status, methodological quality assessment of systematic reviews), intervention categories and subcategories, intervention focus (loneliness, social isolation, or both), intervention format, how technologies are used, how training on how to use digital technology was delivered, outcome domains and subdomains, population characteristics, needs, setting, and location (countries, WHO regions and World Bank classification by income) (Supporting Information: Appendix [Link], [Link]).
We coded the location (country) if it was reported for the primary study or the included studies for reviews. If a review had multiple studies conducted in the same country, it received only one code for the country. For example, a review with six included studies conducted in the USA and two studies conducted in Australia, had only two codes – one for USA and one for Australia.
We coded description of the population characteristics using the PROGRESS‐Plus framework, defined as Place of residence (urban/rural), Race/ethnicity/culture and language, Occupation, Gender/sex, Religion, Education, Socioeconomic status, Social capital (marital status) and additional (plus) factors such as age groups, health status/condition, frailty, disability, living situations, digital literacy, social isolation, and loneliness.
We considered how the study population was selected based on whether they are disadvantaged across any PROGRESS‐Plus factors.
We also coded whether there was any analysis that aimed to understand potential differences across any PROGRESS‐Plus factors.
Given the expected size of the map (over 200 studies), we did not contact organizations or authors of studies and systematic reviews for missing information.
4.11.3. Tools for assessing risk of bias/study quality of included reviews
We assessed the methodological quality of systematic reviews in duplicate (by EG, SD, VB, TH, NE and AW) using the AMSTAR 2 tool (Shea, 2017). Any disagreements were resolved by discussion. As per guidance for evidence maps, primary studies were not assessed for risk of bias or methodological quality (Snilstveit, 2016; White, 2020). A modified AMSTAR2 assessment was conducted for 20 scoping reviews; we did not assess items about risk of bias of included studies since it is optional for scoping reviews (Peters, 2021).
4.11.4. Methods for mapping
We used the EPPI‐Mapping tool (Digital Solution Foundry and EPPI_Centre, 2020) to develop the evidence and gap map.
5. RESULTS
5.1. Description of studies
5.1.1. Results of the search
Our search retrieved 15,324 records from databases and 1829 records from included systematic reviews. After duplicate records were removed, 11,974 articles were screened by title and abstract in duplicate. From this, 633 articles were assessed for eligibility, in duplicate. Two hundred articles were included for the purpose of this EGM. See Figure 5 for the PRISMA flow diagram.
Figure 5.
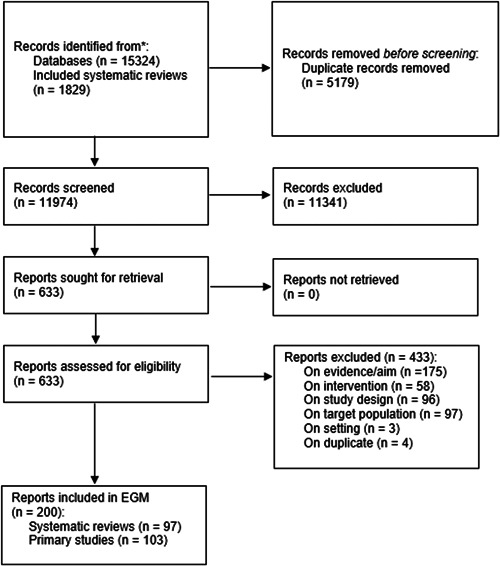
PRISMA flow diagram.
5.1.2. Excluded studies
A total of 433 studies were excluded at the full‐text review phase due to inappropriate evidence/aim (n = 175), inappropriate intervention (n = 58), inappropriate study design (n = 96), inappropriate target population (n = 97), inappropriate setting (n = 3), or duplicate (n = 4). See Figure 5 for the PRISMA flow diagram.
See key excluded studies in the table for Characteristics of excluded studies. Three studies (Bolle, 2015; Clarkson, 2018; Sumner, 2021) were excluded because the aim was not to reduce social isolation or loneliness. Bolle (2015) assessed online health information tools to improve health outcomes. Clarkson (2018) assessed home support interventions to inform dementia care and Sumner (2021) assessed co‐designed interventions to support ageing in place.
Six studies did not assess digital interventions (Dickens, 2011; Gine‐Garriga, 2017; Jones, 2019; Nicholson, 2012; Toh, 2016; Zeppegno, 2018).
Eight studies were excluded for wrong study design; five (Fan, 2016; Forsman, 2018; Gorenko, 2021; Selak, 2019; Winterton, 2011) were not systematic reviews of effectiveness and three were primary studies with no control groups (Perkins, 2012; Preston, 2019; Rebollar, 2015).
Six studies (Burkow, 2015; Cooper, 2014; Dam, 2017; Erfani, 2018; Lara, 2016; Nijman, 2019) included people less than 60 years old and did not provide disaggregated data for people 60 years and older.
5.2. Synthesis of included studies
We included 200 articles that utilized digital interventions to reduce social isolation and/or loneliness; 103 were primary studies and 97 were systematic reviews. See interactive EGM [https://onlinelibrary.wiley.com/pb-assets/assets/18911803/Campbell%20map-Oct5_WITH-1697552065.html].
The primary studies included both RCTs (n = 81) and non‐randomized studies (NRSIs) (n = 22). The systematic reviews included both systematic reviews (n = 77) and scoping reviews (n = 20) that explored the effectiveness of interventions to reduce social isolation and loneliness. Most of the included publications were completed (n = 170, 78 primary studies and 92 reviews) while others were ongoing registered trials and protocols (n = 25, 21 primary studies and 4 reviews). There were five conference abstracts included (n = 5, 4 primary studies and 1 review). See Table 3 (Characteristics of included articles).
Table 3.
Characteristics of included articles.
| Characteristics of included articles | Number of articles | |
|---|---|---|
| Study design |
Primary studies – randomized studies – non‐randomized studies |
103 81 22 |
|
Reviews – systematic reviews – scoping reviews |
97 77 20 |
|
| Publication status |
Completed On‐going Conference abstracts |
78 primary studies/92 reviews 21 primary studies/4 reviews 4 primary studies/1 review |
| Intervention focus |
Social isolation Loneliness Both social isolation and loneliness |
34 primary studies/54 reviews 41 primary studies/23 reviews 34 primary studies/54 reviews |
| Intervention format |
One‐on‐on Group‐based One‐on‐one and group based Unspecified |
29 primary studies/10 reviews 56 primary studies/23 reviews 11 primary studies/28 reviews 7 primary studies/26 reviews |
| Intervention strategies to reduce social isolation and loneliness |
Social cognitive training Improving social skills Enhancing social interactions Enhancing social support Multicomponent |
21 primary studies/19 reviews 37 primary studies/40 reviews 30 primary studies/58 reviews 49 primary studies/81 reviews 16 primary studies/3 reviews |
| Outcomes |
Individual level outcomes Community level outcomes Process indicators |
95 primary studies/96 reviews 40 primary studies/40 reviews 28 primary studies/31 reviews |
| Most reported population sociodemographic characteristics |
Gender/sex Age range (70–80 years old) Education Health condition (dementia) |
83 primary studies/78 reviews 78 primary studies/55 reviews 50 primary studies/6 reviews 16 primary studies/30 reviews |
| Settings |
Personal home Long‐term care (nursing homes) Independent living (residential homes) Assisted living |
36 primary studies/45 reviews 22 primary studies/45 reviews 12 primary studies/23 reviews 5 primary studies/10 reviews |
| Most common locations for included studies |
USA The Netherlands UK Canada Australia |
42 primary studies/44 reviews 8 primary studies/25 reviews 6 primary studies/22 reviews 6 primary studies/16 reviews 5 primary studies/22 reviews |
5.2.1. Interventions
The intervention focus for included publications was on addressing social isolation and loneliness together (n = 88, 34 primary studies and 54 reviews), or on loneliness (n = 64, 41 primary studies and 23 reviews) or social isolation (n = 48, 28 primary studies and 20 reviews) alone.
Included publications reported delivery of interventions as one‐on‐one (n = 79, 56 primary studies and 23 reviews), group‐based (n = 39, 29 primary studies and 10 reviews), or both one‐on‐one and group‐based (n = 49, 11 primary studies and 38 reviews). The mode of delivery was unspecified in some publications (n = 33, 7 primary studies and 26 reviews).
Interventions were categorized based on their strategies to reduce social isolation or loneliness: interventions for social cognitive training (n = 40, 21 primary studies and 19 reviews), improving social skills (n = 77, 37 primary studies and 40 reviews), enhancing social interactions (n = 88, 30 primary studies and 58 reviews), enhancing social support (n = 130, 49 primary studies and 81 reviews), and multicomponent interventions (n = 19, 16 primary studies and 3 reviews) (Figure 6).
Figure 6.
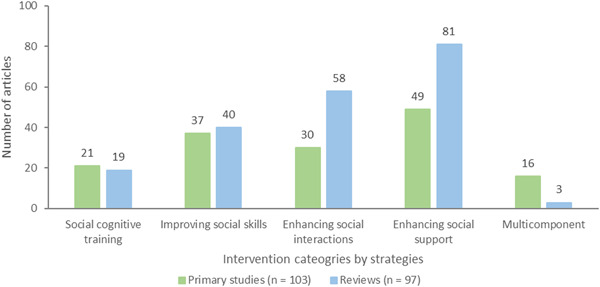
Intervention strategies to reduce social isolation and loneliness.
Each coded intervention category included multiple subcategories. Interventions for social cognitive training consisted of five subcategories: digital CBT (n = 15, 7 primary studies and 8 reviews), digital psychoeducation (n = 12, 5 primary studies and 7 reviews), digital cognitive behavioral coaching (n = 10, 8 primary studies and 2 reviews), digital reminiscence therapy (n = 6, 2 primary studies and 4 reviews), and digital mindfulness training (n = 4, 3 primary studies and 1 review) (Figure 7).
Figure 7.
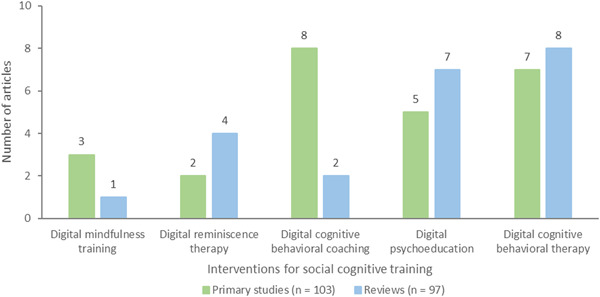
Interventions for social cognitive training.
CBT approaches help individuals recognize and change negative thinking whereas cognitive behavioral coaching approaches help individuals reach their desired goals. Reminiscence therapy involves recalling past events and encourages older adults to communicate and interact with someone in the present. Mindfulness training teaches people to consciously pay attention to their thoughts and feelings and to disengage from negative thoughts, and unhealthy habits that may render them vulnerable. Psychoeducation therapy develops knowledge and understanding of psychological conditions to help individuals cope with them.
Interventions for improving social skills had three subcategories: training in how to use digital technology for communication was most frequent (n = 55, 28 primary studies and 27 reviews), followed by digitally delivered training (n = 23, 9 primary studies and 14 reviews), and no studies or reviews for digitally delivered learning (Figure 8). Training in how to use digital technology was mainly about computer and internet training for communication with family and friends. Half of the primary studies and reviews on digitally delivered training interventions were technology‐based interventions for caregivers of older adults with dementia.
Figure 8.
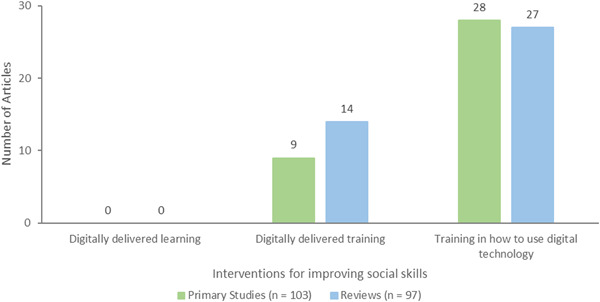
Interventions for improving social skills.
The interventions for enhancing social interactions comprised two subcategories: digital connections with family/friends (n = 57, 13 primary studies and 44 reviews), and digital connections with community including healthcare and social workers and volunteers (n = 61, 22 primary studies and 39 reviews) (Figure 9).
Figure 9.
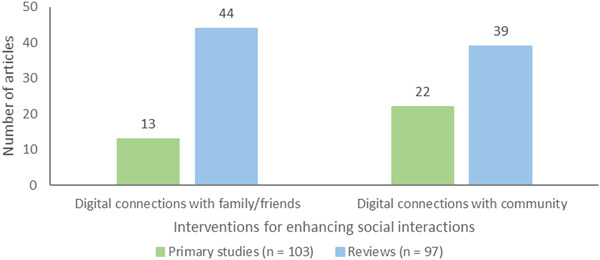
Interventions for enhancing social interactions.
Interventions for enhancing social support had 11 subcategories with most studies involving the following 6 subcategories: socially assistive robots and virtual pets (n = 51, 10 primary studies and 41 reviews), digital games (n = 29, 9 primary studies and 20 reviews, virtual spaces (n = 28, 11 primary studies and 16 reviews), digital/remote e‐health services that also provided companionship or social connections (n = 28, 6 primary studies and 22 reviews), virtual social support groups (n = 27, 10 primary studies and 17 reviews) and digitally delivered activities, mostly physical exercise and exergaming activities (n = 19, 9 primary studies and 20 reviews). Few studies and reviews assessed digital social and healthcare coordination with family/friends (n = 5, 1 primary study and 4 reviews), geolocating/identifying older adults who need services (n = 2 reviews), virtual assistants (n = 3, 1 primary study and 2 reviews), digital intergenerational approaches (n = 3 reviews), and digital coordination of health or social care services (n = 4, 2 primary studies and 2 reviews) (Table 4).
Table 4.
Interventions for enhancing social support.
| Interventions for enhancing social support | Primary studies (n = 103) | Reviews (n = 97) |
|---|---|---|
| Geolocating/identifying older adults who need services | 0 | 2 |
| Digital intergenerational approaches | 0 | 3 |
| Virtual assistants | 1 | 2 |
| Digital social and health care coordination with family/friends | 1 | 4 |
| Digital coordination of health or social care services | 2 | 2 |
| Digital/Remote e‐health services | 6 | 22 |
| Digitally delivered activities | 9 | 10 |
| Digital games | 9 | 20 |
| Virtual social support groups | 10 | 17 |
| Socially assistive robots and virtual pets | 10 | 41 |
| Virtual spaces | 12 | 16 |
5.2.2. Outcomes
Three outcome categories were used to code publications: individual level outcomes (n = 191, 95 primary studies and 96 reviews), community level outcomes (n = 80, 40 primary studies and 40 reviews), and process indicators (n = 59, 28 primary studies and 31 reviews) (Figure 10).
Figure 10.
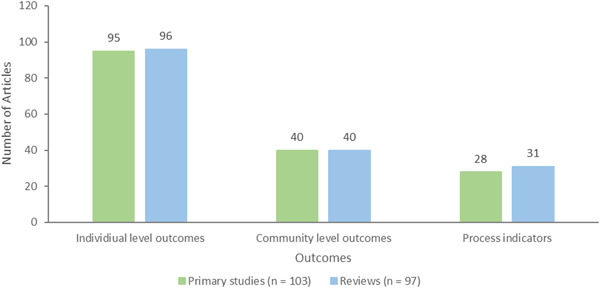
Outcome categories.
Many publications reported multiple outcomes and all outcomes of interest were coded. Individual level outcomes included: loneliness (n = 123, 56 primary studies and 67 reviews), anxiety/depression (n = 112, 57 primary studies and 55 reviews), quality of life/wellbeing (n = 90, 41 primary studies and 49 reviews), social connectedness (n = 54, 17 primary studies and 37 reviews), social isolation (n = 52, 15 primary studies and 37 reviews), confidence level or self‐esteem (n = 23, 8 primary studies and 15 reviews), and adverse effects (n = 8, 2 primary studies and 6 reviews) (Figure 11).
Figure 11.
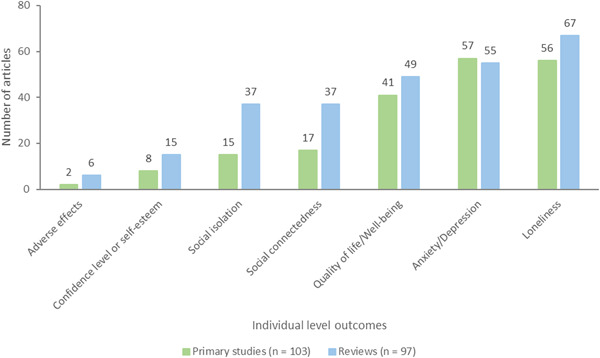
Individual level outcomes.
Adverse effects were mostly privacy and ethical issues reported in three reviews, excessive attachment to robopets with detrimental effects in one review, aggravated musculoskeletal symptoms and fall risks from exergaming in one review, negative impact of adverse media in social networking sites reported in one review, and increase in loneliness in one review. The two primary studies were on‐going and planned to measure adverse effects but did not indicate which ones were anticipated.
Community level outcomes consisted of the following: social support defined as the actual or perceived availability of resources (e.g., tangible, informational, emotional help) from others, typically one's social network (n = 60, 31 primary studies and 29 reviews), social engagement which reflects participation in meaningful activities with others (n = 21, 8 primary studies and 13 reviews), social capital which refers to an appraisal of the social resources or networks people can access in their community (n = 5, 1 primary study and 4 reviews), social cohesion, a measure of mutual community trust and solidarity (n = 1 review). Digital divide, defined as disparities in access to technological interventions (e.g., smartphones, computers, and the internet) which may be due to lack of affordability or access to technology, broadband or Wi‐Fi, data poverty or geographic location, lack of digital skills and the confidence to access online services and support (n = 0) was not measured in any of the included articles (Figure 12). However, one review discussed the barriers caused by digital divide and three primary studies and three reviews each discussed the value of accessibility of digital interventions.
Figure 12.
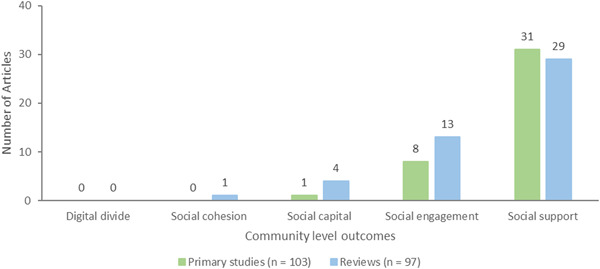
Community level outcomes.
Lastly, process indicators consisted of seven outcomes: acceptance (n = 26, 11 primary studies and 14 reviews), technology use (n = 19, 6 primary studies and 13 reviews), feasibility (n = 15, 6 primary studies and 9 reviews), adherence (n = 14, 10 primary studies and 4 reviews), cost‐effectiveness (n = 9, 1 primary study and 8 reviews), barriers (n = 4 reviews), and affordability (n = 0) which was not measured in any of the included studies or reviews (Figure 13).
Figure 13.
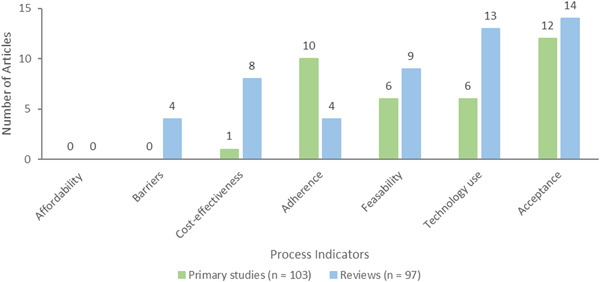
Process indicators.
5.3. Risk of bias in included reviews
Most reviews were classified as critically low quality on the AMSTAR2 Quality Assessment tool due to critical flaws including not reporting prior establishment of a protocol; not providing a list of all excluded studies and justifying the exclusion of each study; as well as not assessing the risk of bias of included studies. The 97 included systematic reviews were classified as follows: critically low (n = 70), low (n = 15), moderate (n = 6), and high (n = 2) quality. Protocols (n = 4) were not assessed (Figure 14).
Figure 14.
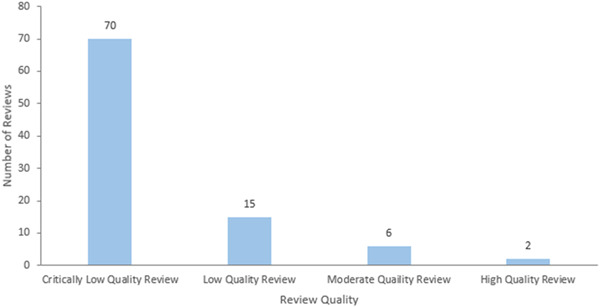
Quality assessment of reviews.
5.4. Additional dimensions
5.4.1. How technologies are used
Technology was used in various ways, and multiple methods were considered in some publications. The most utilized method was videoconferencing (n = 65, 23 primary studies and 42 reviews), followed by telephone calls (n = 55, 20 primary studies and 35 reviews) and robots or virtual companions (n = 51, 10 primary studies and 41 reviews). Mobility tools (n = 1 review), listening to or creating music (n = 3 reviews) and virtual assistants (n = 4, 1 primary study and 3 reviews) were among the least ways in which technology was utilized, and 10 publications (5 primary studies and 5 reviews) did not specify how technologies were used (Table 5).
Table 5.
How technologies are used.
| How technologies are used | Primary studies (n = 103) | Reviews (n = 97) |
|---|---|---|
| Mobility tools | 0 | 1 |
| Listening to or creating Music | 0 | 3 |
| Virtual assistants | 1 | 3 |
| Discussion forums | 3 | 11 |
| Participating in an activity | 15 | 6 |
| Social networking sites | 12 | 16 |
| Digital games | 10 | 20 |
| Messaging | 14 | 17 |
| E‐mail | 13 | 22 |
| Virtual spaces or classrooms with messaging capabilities | 16 | 28 |
| Robots and virtual companions | 10 | 41 |
| Telephone callsa | 20 | 35 |
| Videoconferencing | 23 | 42 |
| Unspecified | 5 | 5 |
Smartphones were specified in 32 of 55 primary studies and systematic reviews. For this EGM, we considered all telephone calls as a strategy for remotely delivered interventions.
5.4.2. Region
Publications included in this EGM come from different countries worldwide. We coded the countries where primary studies were conducted. For reviews, if multiple included studies were conducted in the same country, we coded the country just once. However, if primary studies were included in multiple reviews, the countries where they were conducted were coded multiple times (i.e., once for each review).
Many of the included publications had at least one study conducted in the USA (n = 86, 42 primary studies and 44 reviews) followed by the Netherlands (n = 33, 8 primary studies and 25 reviews), UK (n = 28, 6 primary studies and 22 reviews), Canada (n = 22, 6 primary studies and 16 reviews) and Australia (n = 27, 5 primary studies and 22 reviews). (See geographic heat map for primary studies in Figure 15).
Figure 15.
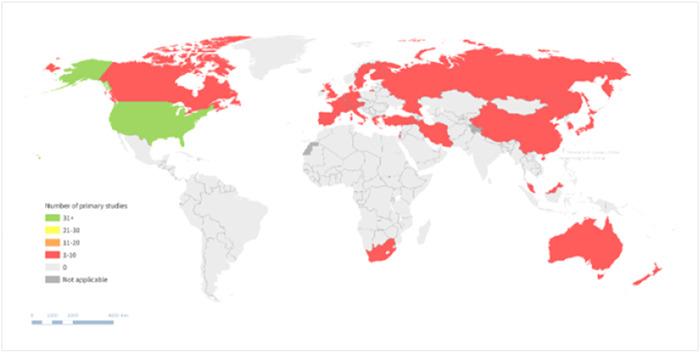
Geographic heat map for primary studies.
In terms of classification by WHO regions (Figure 16) most publications were from the Americas (n = 95, 48 primary studies and 47 reviews), the European Region (n = 77, 33 primary studies and 44 reviews) or Western Pacific Region (n = 58, 20 primary studies and 38 reviews), while very few were from the South‐East Asian (n = 5, 1 primary study and 4 reviews), African (n = 3, 1 primary study and 2 reviews), and Eastern Mediterranean Regions (n = 2 primary studies). Forty reviews did not specify the country where included primary studies were conducted, thus the WHO region and World Bank income region, could not be determined.
Figure 16.
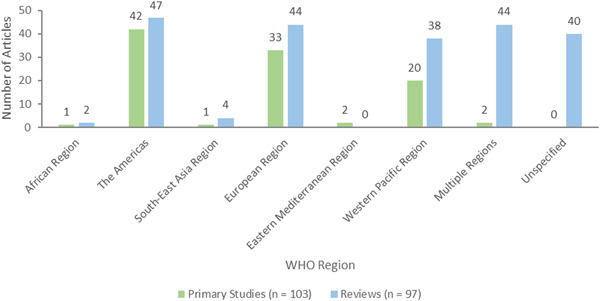
World Health Organization regions.
Following the World Bank income classification, most publications were from high‐income (n = 146, 92 primary studies and 54 reviews) or upper‐middle‐income countries (n = 22, 10 primary and 12 reviews), with none from low‐income countries (Figure 17).
Figure 17.
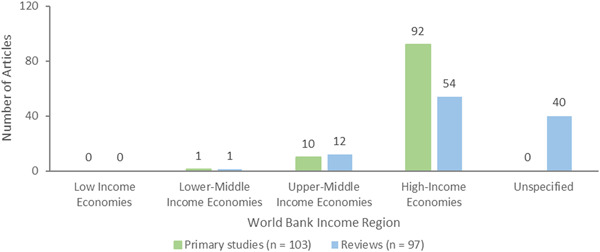
World Bank income classification.
5.4.3. Settings
The setting for most interventions described was the personal home of participants (n = 81, 36 primary studies and 45 reviews), followed by long‐term care/nursing homes (n = 67, 22 primary studies and 45 reviews). Few took place in independent living (n = 35, 12 primary studies and 23 reviews) or assisted living settings (n = 15, 5 primary studies and 10 reviews). Again, some publications included more than one setting for the intervention, and all reported settings were coded as such. Sixty‐eight publications (35 primary studies and 33 reviews) did not specify the setting (Figure 18).
Figure 18.
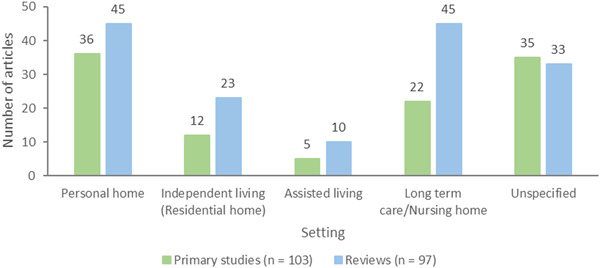
Setting.
5.4.4. Participant needs
Different types of participant needs beyond social isolation and loneliness were identified. Social and emotional needs (n = 191, 97 primary studies and 94 reviews) were the most identified, followed by clinical/health needs (n = 19, 5 primary studies and 14 reviews) and caregiver support (n = 22, 8 primary studies and 14 reviews). Some publications reported interventions targeting more than one need, while no included article targeted participants' accommodation or financial assistance needs (Table 6).
Table 6.
Participant needs.
| Participant needs | Primary studies (n = 103) | Reviews (n = 97) |
|---|---|---|
| Social and emotional needs | 97 | 94 |
| Caregiver support | 8 | 14 |
| Clinical/health needs | 5 | 14 |
| Mobility | 7 | 4 |
| Purpose in Life | 5 | 2 |
| Personal care needs | 1 | 5 |
| Skills development | 2 | 3 |
| Meals | 2 | 0 |
| Respite care | 1 | 2 |
| Communication (language support/interpreters) | 1 | 1 |
| Domestic assistance | 1 | 1 |
| Care navigation support or task orientation | 1 | 0 |
| Learning | 0 | 5 |
| Accommodation | 0 | 0 |
| Financial assistance | 0 | 0 |
5.4.5. Participant characteristics (PROGRESS‐Plus)
Every PROGRESS‐Plus factor was used to describe participants in at least one included article (Figure 19). The PROGRESS acronym stands for Place of residence, Race/ethnicity, Occupation, Gender or sex, Religion, Education, Socioeconomic status, Social capital (marital status). For the purpose of this EGM, we also considered living alone, age group, disability, health condition, and being caregivers as plus factors.
Figure 19.
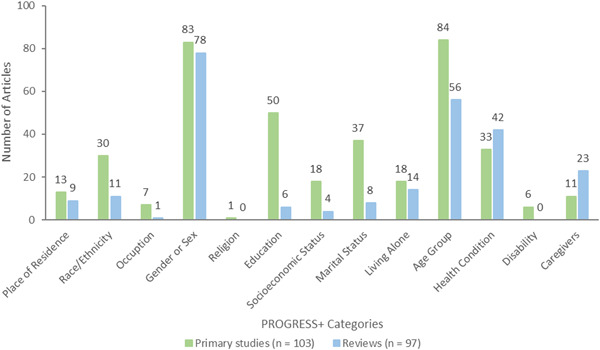
PROGRESS‐Plus categories used to describe participants.
Gender or sex (n = 161, 83 primary studies and 78 reviews) and age (n = 140, 84 primary studies and 56 reviews) were the most reported characteristics, while occupation (n = 8, 7 primary studies and 1 review), and religion (n = 1 primary study) were the least reported.
Of the 161 articles specifying gender or sex, most included male and female participants. Two reviews included some studies with only male participants and 8 reviews included some studies with only female participants; 4 primary studies included only female participants, and gender or sex was unspecified in 39 articles (20 primary studies and 19 reviews). No articles included individuals from the LGBTQIA2S+ (lesbian, gay, bisexual, transgender, queer [or sometimes questioning], and two‐spirited) community.
Of the articles that reported age, the 70–80‐year‐old range was most reported (n = 133, 78 primary studies and 55 reviews), and the age range restricted to older than 80 was least reported (n = 1 primary study). Age of participants was not specified in 67 articles (19 primary studies and 48 reviews) (Figure 20).
Figure 20.
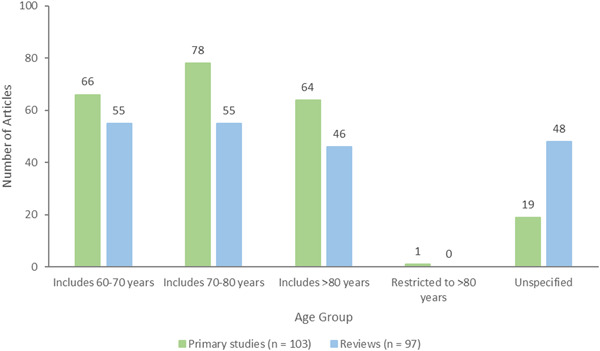
Participant age groups.
5.4.6. Health condition of participants
The health condition of participants was reported in 75 articles (33 primary studies and 42 reviews). Dementia was most common (n = 46, 16 primary studies and 30 reviews), followed by other non‐communicable diseases (n = 13, 8 primary studies and 5 reviews). Included articles did not report on communicable diseases, discharge from hospital, and end‐of‐life/palliative care (Figure 21).
Figure 21.
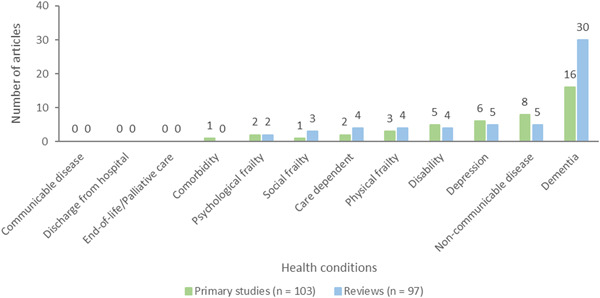
Health conditions of participants.
5.4.7. Equity analysis
Of the 200 included articles, 78 primary studies and 52 reviews focused on recruiting older adults vulnerable across one or more PROGRESS‐Plus factors (Figure 22). Most included articles focused on living situation, that is, older adults living alone or in a nursing home (n = 50, 30 primary studies and 20 reviews), health status (including dementia, depression and other chronic conditions) of older adults (n = 47, 24 primary studies and 23 reviews), socially isolated older adults or at risk of social isolation (n = 20, 13 primary studies and 7 reviews), or lonely older adults or at risk of loneliness (n = 19, 11 primary studies and 8 reviews). Few articles focused on other equity relevant factors including occupation (n = 9, 6 primary studies and 3 reviews), frailty (n = 7, 5 primary studies and 2 reviews), ethnicity (n = 4 primary studies), place of residence, urban or rural (n = 4 primary studies), gender/sex (n = 3 primary studies), digital literacy (n = 3, 2 primary studies and 1 review), disability (n = 2 primary studies), socioeconomic status (n = 2 primary studies), education level (n = 1 primary study), or social capital (n = 1 primary study). No articles focused on religion.
Figure 22.
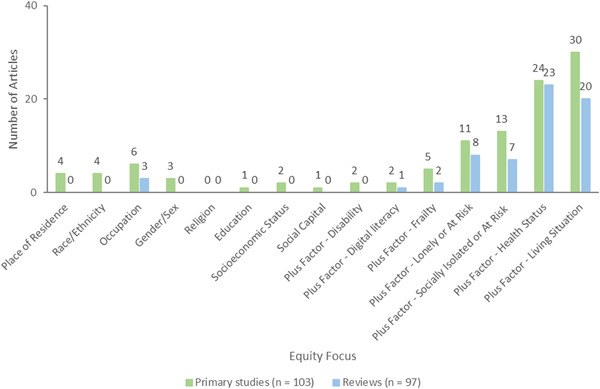
Equity focus of vulnerability across PROGRESS‐Plus factors.
Very few studies focused on multiple vulnerability categories, for example, frail and socially isolated older adults (n = 1), rural isolated family caregivers (n = 1), Chinese socially isolated immigrants (n = 1), low‐income women living alone (n = 1), populations at risk of both social isolation and loneliness (n = 9).
Very few studies described how at‐risk populations were recruited (Figure 23). They were identified through outreach (n = 11, 10 primary studies and 1 review), community‐based programs (n = 11, 8 primary studies and 3 reviews), case finding (n = 7, 6 primary studies and 1 review), or through screening in primary care (n = 3 primary studies). One primary study used all four approaches to identify at‐risk populations.
Figure 23.
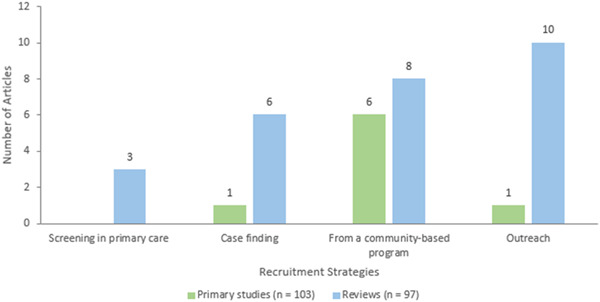
Recruitment strategies for at‐risk populations.
We also assessed whether studies analyzed differences in effects for populations experiencing inequities across PROGRESS‐Plus categories. Despite the large number of articles that considered at least one equity focus, only five articles (4 primary studies and 1 review) assessed the differences in effects across any PROGRESS‐Plus factor including gender or sex (n = 1 study), education level (n = 3 primary studies), age (n = 3 primary studies), living situation (n = 1 primary study), and health status (n = 1 review). No equity analyses were completed for place of residence, race/ethnicity, occupation, religion, socioeconomic status, social capital, frailty, digital literacy, being socially isolated or at risk, being lonely or at risk, or disability (Figure 24).
Figure 24.
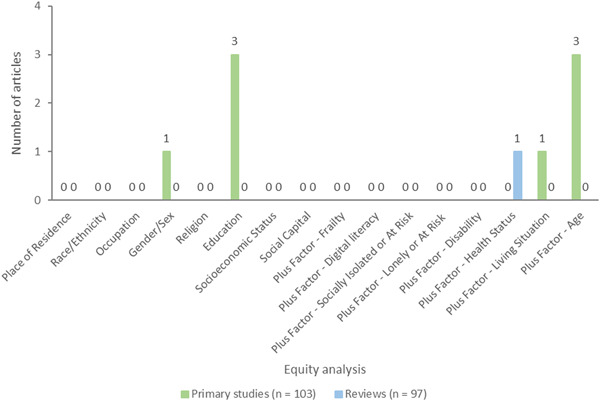
Equity analyses to assess differences in effects across any PROGRESS‐Plus factor.
5.4.8. Stakeholder feedback on framework and draft map
We surveyed 30 people and got 10 (33%) responses. Eight of the 10 (80%) people found that the intervention categories made sense, one (1%) person was neutral and one (1%) disagreed with the category social skills training. We decided to keep social skills training based on the Masi framework (Masi, 2011).
Six (60%) people found the outcome categories made sense, three (30%) were neutral and one (1%) disagreed with including depression/anxiety, quality of life and confidence level as outcomes. We kept these outcomes because they were indicators of social connections (Elder, 2012; Windle, 2012) and were reported in many included articles – 112/200 studies measured anxiety/depression, 90/200 studies measured quality of life, and 23/200 studies measured confidence. Although six (60%) people easily found the information they were looking for on the draft map and one (16.67%) person was neutral, they provided helpful suggestions for knowledge translation activities and improving the usability of the map such as creating a short video of how to use the map.
6. DISCUSSION
6.1. Summary of main results
This evidence and gap map has 200 included articles and there are almost as many primary studies (n = 103) as reviews (n = 97), with most conducted in the Americas, the European and Western Pacific regions. The high ratio of reviews to primary studies indicates a surge in research with over 25% of the reviews conducted since the COVID‐19 pandemic but most reviews are of critically low quality.
The evidence is unevenly distributed across intervention and outcome subcategories with a similar trend across primary studies and reviews. The majority of included primary studies and reviews assessed digital interventions to enhance social interactions with family and friends and the community via videoconferencing and telephone calls. Digital interventions to enhance social support, particularly socially assistive robots, and virtual pets were the next most assessed subcategory of interventions. The social cognitive training strategy was the least assessed of the four intervention strategies although it is considered the most effective (Mann, 2017; Masi, 2011).
The most assessed outcomes were reducing loneliness and depression and improving the quality of life of older adults. Only six reviews reported adverse events and two on‐going primary studies planned to report adverse effects. The most reported age range was 70–80 years old and most common needs addressed were social and emotional needs.
Although many primary studies and reviews focused on recruiting older adults vulnerable across one or more PROGRESS‐Plus factors, very few described how at‐risk populations were recruited or conducted any equity analysis to assess differences in effects for populations experiencing inequities across PROGRESS‐Plus categories.
6.2. Areas of major gaps in the evidence
Major gaps were identified in outcome measures including adverse effects, community level outcomes and process indicators. Only six reviews reported adverse effects. No included studies or reviews assessed affordability or digital divide, which refers to disparities in access to technological interventions, although three primary studies and three reviews discussed the value of accessibility of digital interventions and one of the reviews discussed the barriers caused by digital divide. There were no primary studies or reviews conducted in low‐income countries. Only one primary study restricted participants to 80 years and older and no study or review included participants from the LGBTQIA2S+ community.
6.3. Potential biases in the mapping process
The search strategy was comprehensive and covered published literature until May 16, 2021. We used rigorous methods including duplicate screening of all the identified records and reference lists of included reviews and assessment of methodological quality of reviews. Since our research question is about the effectiveness of digital interventions for social isolation or loneliness, we included only study designs that are appropriate for assessing effectiveness. We did not use outcomes as eligibility criteria. We included studies that assessed the effects of digital interventions on social isolation and loneliness as well as other indicators of social connections such as quality of life, depression.
With the growing research in this area, we may have missed more recent primary studies and reviews. Although there were no language restrictions applied, we may have missed studies and reviews published in non‐English language since mainly English databases were searched.
Mapping the interventions into mutually exclusive categories in the evidence and gap map was challenging due to the lack of consistent terminology and a standardized framework for the classification of interventions for social isolation and loneliness.
6.4. Limitations of the EGM
The map does not include evidence from studies with no control groups or qualitative research. Although these studies might provide useful information about digital interventions for social isolation and loneliness in older adults, they do not assess the effectiveness of interventions.
Most studies and reviews do not focus on reaching the most vulnerable older adults including specific groups such as lonely/socially isolated or at‐risk, low socioeconomic status, low literacy, ethnic minority groups, LGBTQIA2S+ community or populations in low‐income countries where access to digital technology is limited. No included studies or reviews assessed affordability or accessibility of digital interventions, but three primary studies and three reviews discussed the value of accessibility of digital interventions and one of the reviews discussed the barriers caused by digital divide.
6.5. Stakeholder engagement throughout the EGM process
Citizens were involved in the development of this EGM, and they provided constructive and valuable feedback that was incorporated in the process. Only 29% of stakeholders including citizens provided feedback on the framework and draft map.
Although one stakeholder disagreed with social skills training as an intervention category, we decided to keep it since it is included in the Masi framework as interventions that focused on improving interpersonal communication skills (Masi, 2011). One stakeholder disagreed with including depression/anxiety, quality of life and confidence level as outcomes but these outcomes have been described as indicators of social connections (Elder, 2012; Windle, 2012) and were reported in many included articles.
7. AUTHORS' CONCLUSIONS
7.1. Implications for research, practice and/or policy
Social isolation and loneliness are growing public health concerns, which have been highlighted during the COVID‐19 pandemic. This evidence and gap map shows available evidence on effectiveness of digital interventions for reducing social isolation or loneliness in older adults. Over 70% of the systematic reviews have critically low quality, 2% have high quality, and 25% have been published since the pandemic. Clusters of evidence of critically low quality exist mainly for digital interventions to enhance social interactions with family and friends and the community via videoconferencing and telephone calls as well as digital interventions to enhance social support, particularly socially assistive robots, and virtual pets. Most of the digital interventions were focused on reducing loneliness and depression and improving quality of life of older adults.
Major gaps were lack of evidence on equity analysis, community level outcomes and process indicators. Affordability and the digital divide were not assessed in any of the included studies or reviews although barriers caused by the digital divide may increase health inequities and have been key challenges for organizations and governments concerning digital interventions during the COVID‐19 pandemic restrictions. Many studies did not focus on reaching the most vulnerable population groups. The evidence is predominantly from high‐income countries with none in low‐income countries. Other challenges faced by organizations and governments are related to the adverse effects of digital interventions such as privacy and ethical issues. However, very few primary studies and reviews have assessed adverse effects.
This evidence and gap map is the starting point for building the evidence architecture and will guide a future research agenda to standardize definitions of concepts, intervention characteristics, and outcome measurements as well as identify which digital interventions are effective for reducing social isolation and loneliness in older adults taking into consideration their specific needs and contexts.
Although there is proliferation of evidence in recent years, it is unevenly distributed and the systematic reviews are of poor quality highlighting the need for high quality research. Registration of reviews may help to reduce duplication. This map can guide researchers and funders to consider areas of major gaps as priorities for further research.
SOURCES OF SUPPORT
Internal sources
None, Other
External sources
World Health Organization, Switzerland
WHO funding – Purchase Order Number: 202666968
Feedback
CONTRIBUTIONS OF AUTHORS
Content: PH, CM, VW, EG, RS, SB, NH, EB, DK
EGM methods: VW, EG, VB, EB, DK, SD, RD, NE, TH, AW, EBev, PD, JH
Information retrieval: DS
All authors read and approved the review.
DECLARATIONS OF INTEREST
Vivian Welch is editor in chief of the Campbell Collaboration. The editorial process was handled by an independent editor and VW had no input in the editorial process or decisions.
Elisabeth Boulton and Dylan Kneale are joint lead authors of a previous systematic review of systematic reviews which may be eligible for inclusion for the map.
Elizabeth Ghogomu, Victoria Barbeau, Sierra Dowling, Rebecca Doyle, Ella Beveridge, Payaam Desai, Jimmy Huang, Nour Elmestekawy, Tarannum Hussain, Arpana Wadhwani, Sabrina Boutin, Niobe Haitas, Douglas M. Salzwedel, Roger Simard, Paul Hebert, Christopher Mikton have no conflicts of interest.
PLANS FOR UPDATING THE EGM
The EGM will be updated every 2 years.
DIFFERENCES BETWEEN PROTOCOL AND REVIEW
We simplified the conceptual framework in the review.
PUBLISHED NOTES
Characteristics of studies
Characteristics of included studies
| Abbott 2019 |
| Notes |
| Risk of bias table |
| Abdi 2017 |
| Notes |
| Risk of bias table |
| Abdi 2018 |
| Notes |
| Risk of bias table |
| Abou 2020 |
| Notes |
| Risk of bias table |
| Aggarwal 2020 |
| Notes |
| Risk of bias table |
| Ali 2020 |
| Notes |
| Risk of bias table |
| Alves 2020 |
| Notes |
| Risk of bias table |
| Archer 2019 |
| Notes |
| Risk of bias table |
| Baez 2017 |
| Notes |
| Risk of bias table |
| Baker 2018 |
| Notes |
| Risk of bias table |
| Ballesteros 2014 |
| Notes |
| Risk of bias table |
| Banks 2008 |
| Notes |
| Risk of bias table |
| Bedaf 2015 |
| Notes |
| Risk of bias table |
| Beentjes 2020 |
| Notes |
| Risk of bias table |
| Bemelmans 2012 |
| Notes |
| Risk of bias table |
| Beneito‐Montagut 2018 |
| Notes |
| Risk of bias table |
| Bermeja 2018 |
| Notes |
| Risk of bias table |
| Bethell 2019 |
| Notes |
| Risk of bias table |
| Boekhout 2021 |
| Notes |
| Risk of bias table |
| Bornemann 2014 |
| Notes |
| Risk of bias table |
| Boston 2020 |
| Notes |
| Risk of bias table |
| Brodbeck 2019 |
| Notes |
| Risk of bias table |
| Bruce 2020 |
| Notes |
| Risk of bias table |
| Buitenweg 2019 |
| Notes |
| Risk of bias table |
| Cacciata 2019 |
| Notes |
| Risk of bias table |
| Campos 2016 |
| Notes |
| Risk of bias table |
| Casanova 2021 |
| Notes |
| Risk of bias table |
| Cattan 2005 |
| Notes |
| Risk of bias table |
| Chang 2013 |
| Notes |
| Risk of bias table |
| Chen 2016 |
| Notes |
| Risk of bias table |
| Chen 2018 |
| Notes |
| Risk of bias table |
| Chipps 2017 |
| Notes |
| Risk of bias table |
| Chiu 2019 |
| Notes |
| Risk of bias table |
| Choi 2012 |
| Notes |
| Risk of bias table |
| Choi 2020 |
| Notes |
| Risk of bias table |
| Choi 2020a |
| Notes |
| Risk of bias table |
| Choi 2021 |
| Notes |
| Risk of bias table |
| Chua 2013 |
| Notes |
| Risk of bias table |
| Cohen‐Mansfield 2015 |
| Notes |
| Risk of bias table |
| Coll‐Planas 2017 |
| Notes |
| Risk of bias table |
| Courtin 2015 |
| Notes |
| Risk of bias table |
| Czaja 2015 |
| Notes |
| Risk of bias table |
| Czaja 2018 |
| Notes |
| Risk of bias table |
| D'Cunha 2021 |
| Notes |
| Risk of bias table |
| Da‐Eun 2018 |
| Notes |
| Risk of bias table |
| Damant 2017 |
| Notes |
| Risk of bias table |
| Dequanter 2020 |
| Notes |
| Risk of bias table |
| Dermody 2020 |
| Notes |
| Risk of bias table |
| Dichter 2020 |
| Notes |
| Risk of bias table |
| Dickens 2011 a |
| Notes |
| Risk of bias table |
| Dodge 2015 |
| Notes |
| Risk of bias table |
| Dodge 2018 |
| Notes |
| Risk of bias table |
| Duggleby 2020 |
| Notes |
| Risk of bias table |
| El 2020 |
| Notes |
| Risk of bias table |
| Engelbrecht 2015 |
| Notes |
| Risk of bias table |
| Etxeberria |
| Notes |
| Risk of bias table |
| Fakoya 2020 |
| Notes |
| Risk of bias table |
| Feng 2020 |
| Notes |
| Risk of bias table |
| Ferreira 2015 |
| Notes |
| Risk of bias table |
| Fields 2021 |
| Notes |
| Risk of bias table |
| Fokkema 2007 |
| Notes |
| Risk of bias table |
| Forsman 2018 |
| Notes |
| Risk of bias table |
| Francis 2019 |
| Notes |
| Risk of bias table |
| Gardiner 2018 |
| Notes |
| Risk of bias table |
| Godwin 2013 |
| Notes |
| Risk of bias table |
| Gongora 2019 |
| Notes |
| Risk of bias table |
| Gustafson 2019 |
| Notes |
| Risk of bias table |
| Gustafson 2021 |
| Notes |
| Risk of bias table |
| Gustafson 2021a |
| Notes |
| Risk of bias table |
| Haase 2021 |
| Notes |
| Risk of bias table |
| Hagan 2014 |
| Notes |
| Risk of bias table |
| Hartke 2003 |
| Notes |
| Risk of bias table |
| Health Quality Ontario 2008 |
| Notes |
| Risk of bias table |
| Heller 1991 |
| Notes |
| Risk of bias table |
| Hernández‐Ascanio 2020 |
| Notes |
| Risk of bias table |
| Heyn 2001 |
| Notes |
| Risk of bias table |
| Hicken 2017 |
| Notes |
| Risk of bias table |
| Hoang 2021 |
| Notes |
| Risk of bias table |
| Hopwood 2018 |
| Notes |
| Risk of bias table |
| Hung 2019 |
| Notes |
| Risk of bias table |
| Hung 2021 |
| Notes |
| Risk of bias table |
| Ibarra 2020 |
| Notes |
| Risk of bias table |
| Ibrahim 2021 |
| Notes |
| Risk of bias table |
| Iman 2015 |
| Notes |
| Risk of bias table |
| Isabet 2021 |
| Notes |
| Risk of bias table |
| Jackson 2016 |
| Notes |
| Risk of bias table |
| Jarvis 2019 |
| Notes |
| Risk of bias table |
| Jarvis 2020 |
| Notes |
| Risk of bias table |
| Jones 2015 |
| Notes |
| Risk of bias table |
| Jones 2020 |
| Notes |
| Risk of bias table |
| Kachouie 2014 |
| Notes |
| Risk of bias table |
| Kachouie 2017 |
| Notes |
| Risk of bias table |
| Kahlon 2021 |
| Notes |
| Risk of bias table |
| Kamalpour 2020 |
| Notes |
| Risk of bias table |
| kazazi 2021 |
| Notes |
| Risk of bias table |
| Keogh 2014 |
| Notes |
| Risk of bias table |
| Khosravi 2016 |
| Notes |
| Risk of bias table |
| Khosravi 2016a |
| Notes |
| Risk of bias table |
| Koh 2021 |
| Notes |
| Risk of bias table |
| Koh 2021a |
| Notes |
| Risk of bias table |
| Koo 2019 |
| Notes |
| Risk of bias table |
| Kramer 2021 |
| Notes |
| Risk of bias table |
| Kubra 2020 |
| Notes |
| Risk of bias table |
| Lady Lady Davis Institute 2021 |
| Notes |
| Risk of bias table |
| Laganà 2013 |
| Notes |
| Risk of bias table |
| Lai 2020 |
| Notes |
| Risk of bias table |
| Lappalainen 2021 |
| Notes |
| Risk of bias table |
| Larsson 2016 |
| Notes |
| Risk of bias table |
| Lauriks 2007 |
| Notes |
| Risk of bias table |
| Lawson Health Research Institute 2021 |
| Notes |
| Risk of bias table |
| Lee 2021 |
| Notes |
| Risk of bias table |
| Li 2017 |
| Notes |
| Risk of bias table |
| Li 2018 |
| Notes |
| Risk of bias table |
| Liang 2017 |
| Notes |
| Risk of bias table |
| Lin 2020 |
| Notes |
| Risk of bias table |
| Lins 2014 |
| Notes |
| Risk of bias table |
| Lopez‐Hartmann 2012 |
| Notes |
| Risk of bias table |
| Masi 2010 |
| Notes |
| Risk of bias table |
| Matson 2019 |
| Notes |
| Risk of bias table |
| Matz‐Costa 2018 |
| Notes |
| Risk of bias table |
| McKechnie 2014 |
| Notes |
| Risk of bias table |
| Mikkelsen 2019 |
| Notes |
| Risk of bias table |
| Milbury 2020 |
| Notes |
| Risk of bias table |
| Miller 2014 |
| Notes |
| Risk of bias table |
| Mittelman 2006 |
| Notes |
| Risk of bias table |
| Montana 2020 |
| Notes |
| Risk of bias table |
| Morris 2014 |
| Notes |
| Risk of bias table |
| Morton 2018 |
| Notes |
| Risk of bias table |
| Mountain 2014 |
| Notes |
| Risk of bias table |
| Moyle 2017 |
| Notes |
| Risk of bias table |
| Myhre 2015 |
| Notes |
| Risk of bias table |
| Myhre 2017 |
| Notes |
| Risk of bias table |
| Neal 2021 |
| Notes |
| Risk of bias table |
| Nef 2013 |
| Notes |
| Risk of bias table |
| New Study 2 |
| Notes |
| Risk of bias table |
| Nijhof 2009 |
| Notes |
| Risk of bias table |
| Nikitina 2018 |
| Notes |
| Risk of bias table |
| Nilsson 2021 |
| Notes |
| Risk of bias table |
| Noone 2020 |
| Notes |
| Risk of bias table |
| O'Rourke 2018 |
| Notes |
| Risk of bias table |
| Ollevier 2020 |
| Notes |
| Risk of bias table |
| Papadopoulos 2021 |
| Notes |
| Risk of bias table |
| Parkinson 2018 |
| Notes |
| Risk of bias table |
| Pedrozo 2019 |
| Notes |
| Risk of bias table |
| Pepin 2019 |
| Notes |
| Risk of bias table |
| Pereira 2018 |
| Notes |
| Risk of bias table |
| Peres 2021 |
| Notes |
| Risk of bias table |
| Pinto‐Bruno 2017 |
| Notes |
| Risk of bias table |
| Portz 2017 |
| Notes |
| Risk of bias table |
| Poscia 2018 |
| Notes |
| Risk of bias table |
| Pu 2019 |
| Notes |
| Risk of bias table |
| Queiros 2017 |
| Notes |
| Risk of bias table |
| Quinn 2021 |
| Notes |
| Risk of bias table |
| Rainero 2021 |
| Notes |
| Risk of bias table |
| Rienzo 2019 |
| Notes |
| Risk of bias table |
| Robbins 2019 |
| Notes |
| Risk of bias table |
| Robinson 2013 |
| Notes |
| Risk of bias table |
| Robinson 2019 |
| Notes |
| Risk of bias table |
| Ronzi 2018 |
| Notes |
| Risk of bias table |
| Roth 2014 |
| Notes |
| Risk of bias table |
| Salehi |
| Notes |
| Risk of bias table |
| Schulz 2002 |
| Notes |
| Risk of bias table |
| Schwindenhammer 2014 |
| Notes |
| Risk of bias table |
| Sciamanna 2021 |
| Notes |
| Risk of bias table |
| Scoglio 2019 |
| Notes |
| Risk of bias table |
| Shah 2021 |
| Notes |
| Risk of bias table |
| Shapira 2007 |
| Notes |
| Risk of bias table |
| Shapira 2021 |
| Notes |
| Risk of bias table |
| Shapira 2021a |
| Notes |
| Risk of bias table |
| Shishehgar 2018 |
| Notes |
| Risk of bias table |
| Shishehgar 2019 |
| Notes |
| Risk of bias table |
| Smallfield 2018 |
| Notes |
| Risk of bias table |
| Smith 2006 |
| Notes |
| Risk of bias table |
| Smith 2011 |
| Notes |
| Risk of bias table |
| Smith 2017 |
| Notes |
| Risk of bias table |
| Song 2009 |
| Notes |
| Risk of bias table |
| Song 2019 |
| Notes |
| Risk of bias table |
| Sosa 2012 |
| Notes |
| Risk of bias table |
| Su 2020 |
| Notes |
| Risk of bias table |
| Tanaka 2012 |
| Notes |
| Risk of bias table |
| Thodberg 2016 |
| Notes |
| Risk of bias table |
| Tomasino 2017 |
| Notes |
| Risk of bias table |
| Tsai 2010 |
| Notes |
| Risk of bias table |
| Tsai 2011 |
| Notes |
| Risk of bias table |
| Tsai 2020 |
| Notes |
| Risk of bias table |
| Tsai 2020a |
| Notes |
| Risk of bias table |
| Tyack 2017 |
| Notes |
| Risk of bias table |
| University of Texas at Austin 2020 |
| Notes |
| Risk of bias table |
| Uppsala University 2020 |
| Notes |
| Risk of bias table |
| Van Den Heuvel 2019 |
| Notes |
| Risk of bias table |
| Van Houwelingen‐Snippe 2021 |
| Notes |
| Risk of bias table |
| Vanova 2018 |
| Notes |
| Risk of bias table |
| VanRavenstein 2020 |
| Notes |
| Risk of bias table |
| Vazquez 2019 |
| Notes |
| Risk of bias table |
| Wasilewski 2017 |
| Notes |
| Risk of bias table |
| White 1999 |
| Notes |
| Risk of bias table |
| White 2002 |
| Notes |
| Risk of bias table |
| Woodward 2011 |
| Notes |
| Risk of bias table |
| Zaccaria 2020 |
| Notes |
| Risk of bias table |
| Zhao 2020 |
| Notes |
| Risk of bias table |
Characteristics of excluded studies
| Bolle 2015 | |
| Reason for exclusion | Evidence/aim (not to reduce social isolation or loneliness) |
| Burkow 2015 | |
| Reason for exclusion | Target population (included <60 years old, and not disaggregated by age) |
| Clarkson 2018 | |
| Reason for exclusion | Evidence/aim (not to reduce social isolation or loneliness) |
| Cooper 2014 | |
| Reason for exclusion | Target population (included <60 years old, and not disaggregated by age) |
| Dam 2017 | |
| Reason for exclusion | Target population (included <60 years old, and not disaggregated by age) |
| Dickens 2011 | |
| Reason for exclusion | Intervention (not digital) |
| Erfani 2018 | |
| Reason for exclusion | Target population (included <60 years old, and not disaggregated by age) |
| Fan 2016 | |
| Reason for exclusion | Study design (not a systematic review of effectiveness) |
| Forsman 2017 | |
| Reason for exclusion | Study design (not a systematic review of effectiveness) |
| Gine‐Garriga 2017 | |
| Reason for exclusion | Intervention (not digital) |
| Gorenko 2021 | |
| Reason for exclusion | Study design (not a systematic review of effectiveness) |
| Jones 2019 | |
| Reason for exclusion | Intervention (not digital) |
| Lara 2016 | |
| Reason for exclusion | Target population (included <60 years old, and not disaggregated by age) |
| Nicholson 2012 | |
| Reason for exclusion | Intervention (not digital) |
| Nijman 2019 | |
| Reason for exclusion | Target population (included <60 years old, and not disaggregated by age) |
| Perkins 2012 | |
| Reason for exclusion | Study design (not a non‐comparative primary study) |
| Preston 2019 | |
| Reason for exclusion | Study design (not a non‐comparative primary study) |
| Rebollar 2015 | |
| Reason for exclusion | Study design (not a non‐comparative primary study) |
| Selak 2019 | |
| Reason for exclusion | Study design (not a systematic review of effectiveness) |
| Sumner 2021 | |
| Reason for exclusion | Evidence/aim (not to reduce social isolation or loneliness) |
| Toh 2016 | |
| Reason for exclusion | Intervention (not digital) |
| Winterton 2011 | |
| Reason for exclusion | Study design (not a non‐comparative primary study) |
| Zeppegno 2018 | |
| Reason for exclusion | Intervention (not digital) |
Supporting information
Supporting information.
Supporting information.
ACKNOWLEDGMENTS
We acknowledge the contribution of Salman Abdisalam, Priya Grewal, Jinane ElHage, Harry Wang, and Omar Dewidar in screening and coding of articles as well as Tomas Allen for reviewing the search strategies. We gratefully acknowledge the participation of Rheda Adekpedjou and stakeholders in our stakeholder consultation and citizen focus groups. This project was funded by the World Health Organization.
Welch, V. , Ghogomu, E. T. , Barbeau, V. I. , Dowling, S. , Doyle, R. , Beveridge, E. , Boulton, E. , Desai, P. , Huang, J. , Elmestekawy, N. , Hussain, T. , Wadhwani, A. , Boutin, S. , Haitas, N. , Kneale, D. , Salzwedel, D. M. , Simard, R. , Herbert, P. , & Mikton, C. (2023). Digital interventions to reduce social isolation and loneliness in older adults: An evidence and gap map. Campbell Systematic Reviews, 19, e1369. 10.1002/cl2.1369
REFERENCES
- INCLUDED STUDIES
Abbott 2019
- Abbott, R. , Orr, N. , McGill, P. , Whear, R. , Bethel, A. , Garside, R. , Stein, K. , & Thompson‐Coon, J. (2019). How do “robopets” impact the health and well‐being of residents in care homes? A systematic review of qualitative and quantitative evidence. International Journal of Older People Nursing, 14(3), e12239. [DOI] [PMC free article] [PubMed] [Google Scholar]
Abdi 2017
- Abdi, J. , Al‐Hindawi, A. , & Vizcaychipi, M. (2017). Use of socially assistive robot technology in elderly care. Age and Ageing, 46(Supplement 1), i1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Abdi 2018
- Abdi, J. , Al‐Hindawi, A. , Ng, T. , & Vizcaychipi, M. P. (2018). Scoping review on the use of socially assistive robot technology in elderly care. BMJ Open, 8(2), e018815. [DOI] [PMC free article] [PubMed] [Google Scholar]
Abou 2020
- Abou Allaban, A. , Wang, M. Z. , & Padir, T. (2020). A systematic review of robotics research in support of in‐home care for older adults. Information, 11(2), 75. [Google Scholar]
Aggarwal 2020
- Aggarwal, B. , Xiong, Q. , & Schroeder‐Butterfill, E. (2020). Impact of the use of the internet on quality of life in older adults: Review of literature. Primary Health Care Research & Development, 21, e55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ali 2020
- Ali, R. , Hoque, E. , Duberstein, P. , Schubert, L. , Razavi, S. Z. , Kane, B. , Silva, C. , Daks, J. S. , Huang, M. , & Van Orden, K. (2020). Aging and engaging: A pilot randomized controlled trial of an online conversational skills coach for older adults. American Journal of Geriatric Psychiatry, 22, 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Alves 2020
- Alves, G. S. , Bruno Costa, E. , Alves, G. S. , Rodrigues, V. M. , Dourado, M. C. N. , Casali, M. E. , Carrilho, C. G. , Veras, A. B. , Rodrigues, V. M. , & Dourado, M. C. N. (2020). A systematic review of home‐setting psychoeducation interventions for behavioral changes in dementia: Some lessons for the COVID‐19 pandemic and Post‐Pandemic assistance. Frontiers in Psychiatry, 11, 577871. [DOI] [PMC free article] [PubMed] [Google Scholar]
Archer 2019
- Archer, N. , & Aria, R. (2019). Reducing risk from chronic illness with life style changes supported by online health self‐management.
Baez 2017
- Baez, M. , Khaghani Far, I. , Ibarra, F. , Ferron, M. , Didino, D. , & Casati, F. (2017). Effects of online group exercises for older adults on physical, psychological and social wellbeing: A randomized pilot trial. PeerJ, 5, e3150. [DOI] [PMC free article] [PubMed] [Google Scholar]
Baker 2018
- Baker, S. , Warburton, J. , Waycott, J. , Batchelor, F. , Hoang, T. , Dow, B. , Ozanne, E. , & Vetere, F. (2018). Combatting social isolation and increasing social participation of older adults through the use of technology: A systematic review of existing evidence. Australasian Journal on Ageing, 37(3), 184–193. [DOI] [PubMed] [Google Scholar]
Ballesteros 2014
- Ballesteros, S. , Toril, P. , Mayas, J. , Reales Jose, M. , & Waterworth John, A. (2014). An ICT‐mediated social network in support of successful ageing. Gerontechnology, 13(1), 39–48. [Google Scholar]
Banks 2008
- Banks Marian, R. , Willoughby Lisa, M. , & Banks William, A. (2008). Animal‐assisted therapy and loneliness in nursing homes: Use of robotic versus living dogs. Journal of the American Medical Directors Association, 9(3), 173–177. [DOI] [PubMed] [Google Scholar]
Bedaf 2015
- Bedaf, S. , Gelderblom, G. J. , & De Witte, L. (2015). Overview and categorization of robots supporting independent living of elderly people: What activities do they support and how far have they developed. Assistive Technology, 27(2), 88–100. [DOI] [PubMed] [Google Scholar]
Beentjes 2020
- Beentjes, K. M. , Neal, D. P. , Kerkhof, Y. J. F. , Broeder, C. , Moeridjan, Z. D. J. , Ettema, T. P. , Pelkmans, W. , Muller, M. M. , Graff, M. J. L. , & Droes, R. M. (2020). Impact of the FindMyApps program on people with mild cognitive impairment or dementia and their caregivers; an exploratory pilot randomised controlled trial. Disability & Rehabilitation Assistive Technology, 18, 253–265. [DOI] [PubMed] [Google Scholar]
Bemelmans 2012
- Bemelmans, R. , Gelderblom, G. J. , Jonker, P. , & de Witte, L. (2012). Socially assistive robots in elderly care: A systematic review into effects and effectiveness. Journal of the American Medical Directors Association, 13(2), 114–120.e1. [DOI] [PubMed] [Google Scholar]
Beneito‐Montagut 2018
- Beneito‐Montagut, R. , Cassián‐Yde, N. , & Begueria, A. (2018). What do we know about the relationship between internet‐mediated interaction and social isolation and loneliness in later life? Quality in Ageing and Older Adults, 19(1), 14–30. [Google Scholar]
Bermeja 2018
- Bermeja, A. I. , & Ausín, B. (2018). Programas para combatir la soledad en las personas mayores en el ámbito institucionalizado: Una revisión de la literatura científica. Revista Española de Geriatría y Gerontología, 53(3), 155–164. [DOI] [PubMed] [Google Scholar]
Bethell 2019
- Bethell, J. , Babineau, J. , Iaboni, A. , Green, R. , Cuaresma‐Canlas, R. , Karunananthan, R. , Schon, B. , Schon, D. , & McGilton Katherine, S. (2019). Social integration and loneliness among long‐term care home residents: Protocol for a scoping review. BMJ Open, 9(12), e033240. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boekhout 2021
- Boekhout, J. M. , Volders, E. , Bolman, C. A. W. , de Groot, R. H. M. , & Lechner, L. (2021). Long‐term effects on loneliness of a computer‐tailored intervention for older adults with chronic diseases: A randomized controlled trial. Journal of Aging & Health, 33, 865–876. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bornemann 2014
- Bornemann, R. (2014). The impact of information and communication technology (ICT) usage on social isolation including loneliness in older adults. A systematic review. Magdeburg/Stendal University of Applied Sciences. [Google Scholar]
Boston University 2020
- Boston University . (2020). Impact of Covid‐19 on frequent social interaction through communication technologies in the cognitive status of socially‐isolated older adults. clinicaltrials.gov.
Brodbeck 2019
- Brodbeck, J. , Berger, T. , Biesold, N. , Rockstroh, F. , & Znoj, H. J. (2019). Evaluation of a guided internet‐based self‐help intervention for older adults after spousal bereavement or separation/divorce: A randomised controlled trial. Journal of Affective Disorders, 252, 440–449. [DOI] [PubMed] [Google Scholar]
Bruce 2020
- Bruce, M. L. , Pepin, R. , Marti, C. N. , Stevens, C. J. , & Choi, N. G. (2020). One year impact on social connectedness for homebound older adults: A randomized controlled trial of tele‐delivered behavioral activation versus tele‐delivered friendly visits. The American Journal of Geriatric Psychiatry, 28(7), 698–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
Buitenweg 2019
- Buitenweg, IV J. , Van De Ven, R. M. , Ridderinkhof, K. R. , & Murre, J. M. J. (2019). Does cognitive flexibility training enhance subjective mental functioning in healthy older adults? Aging Neuropsychology & Cognition, 26(5), 688–710. [DOI] [PubMed] [Google Scholar]
Cacciata 2019
- Cacciata, M. , Stromberg, A. , Lee, J. A. , Sorkin, D. , Lombardo, D. , Clancy, S. , Nyamathi, A. , & Evangelista, L. S. (2019). Effect of exergaming on health‐related quality of life in older adults: A systematic review. International Journal of Nursing Studies, 93, 30–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Campos 2016
- Campos, W. , Martinez, A. , Sanchez, W. , Estrada, H. , Castro‐Sanchez, N. A. , & Mujica, D. (2016). A systematic review of proposals for the social integration of elderly people using ambient intelligence and social networking sites. Cognitive Computation, 8(3), 529–542. [Google Scholar]
Casanova 2021
- Casanova, G. , Zaccaria, D. , Rolandi, E. , & Guaita, A. (2021). The effect of information and communication technology and social networking site use on older people's well‐being in relation to loneliness: Review of experimental studies. Journal of Medical Internet Research, 23(3), e23588. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cattan 2005
- Cattan, M. , White, M. , Bond, J. , & Learmouth, A. (2005). Preventing social isolation and loneliness among older people: A systematic review of health promotion interventions. Ageing and Society, 25(1), 41–67. [DOI] [PubMed] [Google Scholar]
Chang 2013
- Chang, S. M. , & Sung, H. C. C. (2013). The effectiveness of seal‐like robot therapy on mood and social interactions of older adults: A systematic review protocol. JBI Library of Systematic Reviews, 11(10), 68–75. [Google Scholar]
Chen 2016
- Chen, Y. R. , & Schulz, P. J. (2016). The effect of information communication technology interventions on reducing social isolation in the elderly: A systematic review. Journal of Medical Internet Research, 18(1), e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chen 2018
- Chen, S. C. , Jones, C. , & Moyle, W. (2018). Social robots for depression in older adults: A systematic review. Journal of Nursing Scholarship, 50(6), 612–622. [DOI] [PubMed] [Google Scholar]
Chipps 2017
- Chipps, J. , Jarvis, M. A. , & Ramlall, S. (2017). The effectiveness of e‐interventions on reducing social isolation in older persons: A systematic review of systematic reviews. Journal of Telemedicine & Telecare, 23(10), 817–827. [DOI] [PubMed] [Google Scholar]
Chiu 2019
- Chiu, C. J. , & Wu, C. H. (2019). Information and communications technology as a health promotion method for older adults in assisted‐living facilities: Three‐arm group‐randomized trial. JMIR Aging, 2(1), e12633. [DOI] [PMC free article] [PubMed] [Google Scholar]
Choi 2012
- Choi, M. , Kong, S. , & Jung, D. (2012). Computer and internet interventions for loneliness and depression in older adults: A meta‐analysis. Healthcare Informatics Research, 18(3), 191–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
Choi 2020
- Choi, N. G. , Marti, C. N. , Wilson, N. L. , Chen, G. J. , Sirrianni, L. , Hegel, M. T. , Bruce, M. L. , & Kunik, M. E. (2020). Effect of telehealth treatment by lay counselors vs by clinicians on depressive symptoms among older adults who are homebound: A randomized clinical trial. JAMA Network Open, 3(8), 2574–3805. [DOI] [PMC free article] [PubMed] [Google Scholar]
Choi 2020a
- Choi, N. G. , Pepin, R. , Marti, C. N. , Stevens, C. J. , & Bruce, M. L. (2020). Improving social connectedness for homebound older adults: Randomized controlled trial of tele‐delivered behavioral activation versus tele‐delivered friendly visits. American Journal of Geriatric Psychiatry, 28(7), 698–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
Choi 2021
- Choi, H. K. , & Lee, S. H. (2021). Trends and effectiveness of ICT interventions for the elderly to reduce loneliness: A systematic review. Healthcare, 9(3), 07. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chua 2013
- Chua, P.‐H. , Jung, Y. , Lwin May, O. , & Theng, Y.‐L. (2013). Let's play together: Effects of video‐game play on intergenerational perceptions among youth and elderly participants. Computers in Human Behavior, 29(6), 2303–2311. [Google Scholar]
Cohen‐Mansfield 2015
- Cohen‐Mansfield, J. , & Perach, R (2015). Interventions for alleviating loneliness among older persons: A critical review. American Journal of Health Promotion, 29(3), e109–e125. [DOI] [PubMed] [Google Scholar]
Coll‐Planas 2017
- Coll‐Planas, L. , Nyqvist, F. , Puig, T. , Urrútia, G. , Solà, I. , & Monteserín, R. (2017). Social capital interventions targeting older people and their impact on health: A systematic review. Journal of Epidemiology and Community Health, 71(7), 663–672. [DOI] [PubMed] [Google Scholar]
Courtin 2015
- Courtin, E. , & Knapp, M. (2015). Social isolation, loneliness and health in old age: A scoping review. Health & Social Care in the Community, 25(3), 799–812. [DOI] [PubMed] [Google Scholar]
Czaja 2015
- Czaja, S. J. , Boot, W. R. , Charness, N. , Rogers, W. A. , Sharit, J. , Fisk, A. D. , Lee, C. C. , & Nair, S. N. (2015). The personalized reminder information and social management system (PRISM) trial: Rationale, methods and baseline characteristics. Contemporary Clinical Trials, 40, 35–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
Czaja 2018
- Czaja, S. J. , Boot, W. R. , Charness, N. , Rogers, W. A. , & Sharit, J. (2018). Improving social support for older adults through technology: Findings from the PRISM randomized controlled trial. Gerontologist, 58(3), 467–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
D'Cunha 2021
- D'Cunha, N. M. , Isbel, S. T. , Frost, J. , Fearon, A. , McKune, A. J. , Naumovski, N. , & Kellett, J. (2021). Effects of a virtual group cycling experience on people living with dementia: A mixed method pilot study. Dementia, 20, 1518–1535. [DOI] [PubMed] [Google Scholar]
Da‐Eun 2018
- Da‐Eun, K. , Hyang, K. , Junghee, H. , Hyojin, L. , Hyehyun, S. , Soyoung, B. , Sunghee, H. T. , Yeon‐Hwan, P. , & Ju‐Young, Y. (2018). Interventions using technologies for older adults in long‐term care facilities: A systematic review. Journal of Korean Academy of Community Health Nursing, 29, 170–183. [Google Scholar]
Damant 2017
- Damant, J. , Knapp, M. , Freddolino, P. , & Lombard, D. (2017). Effects of digital engagement on the quality of life of older people. Health & Social Care in the Community, 25(6), 1679–1703. [DOI] [PubMed] [Google Scholar]
Dequanter 2020
- Dequanter, S. , Gagnon, M. P. , Ndiaye, M. A. , Gorus, E. , Fobelets, M. , Giguere, A. , Bourbonnais, A. , & Buyl, R. (2020). The effectiveness of E‐health solutions for ageing with cognitive impairment: A systematic review. Gerontologist, 61, e373–e394. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dermody 2020
- Dermody, G. , Whitehead, L. , Wilson, G. , & Glass, C. (2020). The role of virtual reality in improving health outcomes for community‐dwelling older adults: Systematic review. Journal of Medical Internet Research, 22(6), e17331. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dichter 2020
- Dichter, M. N. , Albers, B. , Trutschel, D. , Strobel, A. M. , Seismann‐Petersen, S. , Wermke, K. , Halek, M. , & Berwig, M. (2020). TALKING TIME: A pilot randomized controlled trial investigating social support for informal caregivers via the telephone. BMC Health Services Research, 20(1), 788. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dickens 2011a
- Dickens, A. P. , Richards, S. H. , Greaves, C. J. , & Campbell, J. L. (2011). Interventions targeting social isolation in older people: A systematic review. BMC Public Health, 11, 647. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dodge 2015
- Dodge, H. H. , Zhu, J. , Mattek, N. , Bowman, M. , Ybarra, O. , Wild, K. , Loewenstein, D. A. , & Kaye, J. A. (2015). Web‐enabled conversational interactions as a means to improve cognitive functions: Results of a 6‐week randomized controlled trial. Alzheimer's & Dementia: Translational Research & Clinical Interventions, 1(1), 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dodge 2018
- Dodge, H. , Goodrich, E. , Lindsley, J. , Hampstead, B. , & Kaye, J. (2018). Behavioral RCT using frequent social interaction to enhance cognitive reserve. Clinical Trials, 15(Supplement 2), 130–131.29361843 [Google Scholar]
Duggleby 2020
- Duggleby, W. , O'Rourke, H. , Swindle, J. , Peacock, S. , McAiney, C. , Baxter, P. , Thompson, G. , Dube, V. , Nekolaichuk, C. , Ghosh, S. , & Holroyd‐Leduc, J. (2020). Study protocol: Pragmatic randomized control trial of my tools 4 care‐ in care (MT4C‐in care) a web‐based tool for family carers of persons with dementia residing in long term care. BMC Geriatrics, 20(1), 285. [DOI] [PMC free article] [PubMed] [Google Scholar]
El Kamali 2020
- El Kamali, M. , Angelini, L. , Caon, M. , Carrino, F. , Rocke, C. , Guye, S. , Rizzo, G. , Mastropietro, A. , Sykora, M. , Elayan, S. , Kniestedt, I. , Ziylan, C. , Lettieri, E. , Abou Khaled, O. , & Mugellini, E. (2020). Virtual coaches for older adults' wellbeing: A systematic review. Ieee Access, 8, 101884–101902. [Google Scholar]
Engelbrecht 2015
- Engelbrecht, R. , & Shoemark, H. (2015). The acceptability and efficacy of using ipads in music therapy to support wellbeing with older adults: A pilot study. The Australian Journal of Music Therapy, 26, 49–70. [Google Scholar]
Etxeberria 2021
- Etxeberria, I. , Salaberria, K. , & Gorostiaga, A. (2021). Online support for family caregivers of people with dementia: A systematic review and meta‐analysis of RCTs and quasi‐experimental studies. Aging & Mental Health, 25(7), 1165–1180. [DOI] [PubMed] [Google Scholar]
Fakoya 2020
- Fakoya Olujoke, A. , McCorry Noleen, K. , & Donnelly, M. (2020). Loneliness and social isolation interventions for older adults: A scoping review of reviews. BMC Public Health, 20(1), 129. [DOI] [PMC free article] [PubMed] [Google Scholar]
Feng 2020
- Feng, Y. , Barakova, E. I. , Yu, S. , Hu, J. , & Rauterberg, G. W. M. (2020). Effects of the level of interactivity of a social robot and the response of the augmented reality display in contextual interactions of people with dementia. Sensors, 20(13), 05. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ferreira 2015
- Ferreira, S. , Torres, A. , Mealha, Ó. , & Veloso, A. (2015). Training effects on older adults in information and communication technologies considering psychosocial variables. Educational Gerontology, 41(7), 482–493. [Google Scholar]
Fields 2021
- Fields, J. , Cemballi, A. G. , Michalec, C. , Uchida, D. , Griffiths, K. , Cardes, H. , Cuellar, J. , Chodos, A. H. , & Lyles, C. R. (2021). In‐home technology training among socially isolated older adults: Findings from the tech allies program. Journal of Applied Gerontology, 40(5), 489–499. [DOI] [PubMed] [Google Scholar]
Fokkema 2007
- Fokkema, T. , & Knipscheer, K. (2007). Escape loneliness by going digital: A quantitative and qualitative evaluation of a Dutch experiment in using ECT to overcome loneliness among older adults. Aging & Mental Health, 11(5), 496–504. [DOI] [PubMed] [Google Scholar]
Forsman 2018
- Forsman, A. K. , Nordmyr, J. , Matosevic, T. , Park, A. L. , Wahlbeck, K. , & McDaid, D. (2018). Promoting mental wellbeing among older people: Technology‐based interventions. Health Promotion International, 33(6), 1042–1054. [DOI] [PubMed] [Google Scholar]
Francis 2019
- Francis, J. , Rikard, R. V. , Cotten, S. R. , & Kadylak, T. (2019). Does ICT use matter? How information and communication technology use affects perceived mattering among a predominantly female sample of older adults residing in retirement communities. Information Communication & Society, 22(9), 1281–1294. [Google Scholar]
Gardiner 2018
- Gardiner, C. , Geldenhuys, G. , & Gott, M. (2018). Interventions to reduce social isolation and loneliness among older people: An integrative review. Health & Social Care in the Community, 26(2), 147–157. [DOI] [PubMed] [Google Scholar]
Godwin 2013
- Godwin, K. M. , Mills, W. L. , Anderson, J. A. , & Kunik, M. E. (2013). Technology‐driven interventions for caregivers of persons with dementia: A systematic review. American Journal of Alzheimer's Disease & Other Dementias, 28(3), 216–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gongora 2019
- Gongora, A. S. , Hamrioui, S. , de la Torre Diez, I. , Motta Cruz, E. , Lopez‐Coronado, M. , & Franco, M. (2019). Social robots for people with aging and dementia: A systematic review of literature. Telemedicine Journal & E‐Health, 25(7), 533–540. [DOI] [PubMed] [Google Scholar]
Gustafson 2019
- Gustafson, D. H. , Gustafson, D. H. , Cody, O. J. , Chih, M. Y. , Johnston, D. C. , & Asthana, S. (2019). Pilot test of a computer‐based system to help family caregivers of dementia patients. Journal of Alzheimer's Disease, 70(2), 541–552. [DOI] [PubMed] [Google Scholar]
Gustafson 2021
- Gustafson, Sr., D. H. , McTavish, F. , Gustafson, Jr., D. H. , Mahoney, J. E. , Johnson, R. A. , Lee, J. D. , Quanbeck, A. , Atwood, A. K. , Isham, A. , Veeramani, R. , Clemson, L. , & Shah, D. (2021). Effect of an eHealth intervention on older adults' quality of life and health‐related outcomes: A randomized clinical trial. Journal of General Internal Medicine, 37, 521–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gustafson 2021a
- Gustafson, Sr., D. H. , Mares, M. L. , Johnston, D. C. , Mahoney, J. E. , Brown, R. T. , Landucci, G. , Pe‐Romashko, K. , Cody, O. J. , Gustafson, Jr., D. H. , & Shah, D. V. (2021). A web‐based ehealth intervention to improve the quality of life of older adults with multiple chronic conditions: Protocol for a randomized controlled trial. JMIR Research Protocols, 10(2), e25175. [DOI] [PMC free article] [PubMed] [Google Scholar]
Haase 2021
- Haase, K. R. , Sattar, S. , Hall, S. , McLean, B. , Wills, A. , Gray, M. , Kenis, C. , Donison, V. , Howell, D. , & Puts, M. (2021). Systematic review of self‐management interventions for older adults with cancer. Psycho‐oncology, 30(7), 989–1008. [DOI] [PubMed] [Google Scholar]
Hagan 2014
- Hagan, R. , Manktelow, R. , Taylor, B. J. , & Mallett, J. (2014). Reducing loneliness amongst older people: A systematic search and narrative review. Aging & Mental Health, 18(6), 683–693. [DOI] [PubMed] [Google Scholar]
Hartke 2003
- Hartke, R. J. , & King, R. B. (2003). Telephone group intervention for older stroke caregivers. Topics in Stroke Rehabilitation, 9(4), 65–81. [DOI] [PubMed] [Google Scholar]
Health Quality Ontario 2008
- Health Quality Ontario . (2008). Social isolation in community‐dwelling seniors: An evidence‐based analysis. Ontario Health Technology Assessment Series, 8(5), 1–49. [PMC free article] [PubMed] [Google Scholar]
Heller 1991
- Heller, K. , Thompson, M. G. , Trueba, P. E. , Hogg, J. R. , & Vlachos‐Weber, I. (1991). Peer support telephone dyads for elderly women: Was this the wrong intervention? American Journal of Community Psychology, 19(1), 53–74. [DOI] [PubMed] [Google Scholar]
Hernández‐Ascanio 2020
- Hernández‐Ascanio, J. , Pérula‐de Torres, L. Á. , Roldán‐Villalobos, A. , Pérula‐de Torres, J. C. , & Rich‐Ruiz, M. (2020). Effectiveness of a multicomponent intervention to reduce social isolation and loneliness in community‐dwelling elders: A randomized clinical trial. Study protocol. Journal of Advanced Nursing, 76(1), 337–346. [DOI] [PubMed] [Google Scholar]
Heyn 2001
- Heyn Billipp, S. (2001). The psychosocial impact of interactive computer use within a vulnerable elderly population: A report on a randomized prospective trial in a home health care setting. Public Health Nursing, 18(2), 138–145. [DOI] [PubMed] [Google Scholar]
Hicken 2017
- Hicken, B. L. , Daniel, C. , Luptak, M. , Grant, M. , Kilian, S. , & Rupper, R. W. (2017). Supporting caregivers of rural veterans electronically (SCORE). Journal of Rural Health, 33(3), 305–313. [DOI] [PubMed] [Google Scholar]
Hoang 2021
- Hoang, P. , Whaley, C. , Thompson, K. , Ho, V. , Rehman, U. , Boluk, K. , & Grindrod, K. A. (2021). Evaluation of an intergenerational and technological intervention for loneliness: Protocol for a feasibility randomized controlled trial. JMIR Research Protocols, 10(2), e23767. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hopwood 2018
- Hopwood, J. , Walker, N. , McDonagh, L. , Rait, G. , Walters, K. , Iliffe, S. , Ross, J. , & Davies, N. (2018). Internet‐based interventions aimed at supporting family caregivers of people with dementia: Systematic review. Journal of Medical Internet Research, 20(6), e216. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hung 2019
- Hung, L. , Liu, C. , Woldum, E. , Au‐Yeung, A. , Berndt, A. , Wallsworth, C. , Horne, N. , Gregorio, M. , Mann, J. , & Chaudhury, H. (2019). The benefits of and barriers to using a social robot PARO in care settings: A scoping review. BMC Geriatrics, 19(1), 232. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hung 2021
- Hung, L. , Chow, B. , Shadarevian, J. , O'Neill, R. , Berndt, A. , Wallsworth, C. , Horne, N. , Gregorio, M. , Mann, J. , Son, C. , & Chaudhury, H. (2021). Using touchscreen tablets to support social connections and reduce responsive behaviours among people with dementia in care settings: A scoping review. Dementia, 20(3), 1124–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ibarra 2020
- Ibarra, F. , Baez, M. , Cernuzzi, L. , & Casati, F. (2020). A systematic review on technology‐supported interventions to improve old‐age social wellbeing: Loneliness, social isolation, and connectedness. Journal of Healthcare Engineering, 2020, 2036842. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ibrahim 2021
- Ibrahim, A. , Chong, M. C. , Khoo, S. , Wong, L. P. , Chung, I. , & Tan, M. P. (2021). Virtual group exercises and psychological status among community‐dwelling older adults during the COVID‐19 pandemic—A feasibility study. Geriatrics, 6(1), 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Iman 2015
- Iman, K. , Far, F. M. , Ibarra, F. , Baez, M. , Tranquillini, S. , Casati, F. , & Doppio, N. (2015). The interplay of physical and social wellbeing in older adults: Investigating the relationship between physical training and social interactions with virtual social environments. PeerJ Computer Science, 1(7), e30. [Google Scholar]
Isabet 2021
- Isabet, B. , Pino, M. , Lewis, M. , Benveniste, S. , & Rigaud, A. S. (2021). Social telepresence robots: A narrative review of experiments involving older adults before and during the COVID‐19 pandemic. International Journal of Environmental Research & Public Health [Electronic Resource], 18(7), 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jackson 2016
- Jackson, D. , Roberts, G. , Wu Min, L. , Ford, R. , & Doyle, C. (2016). A systematic review of the effect of telephone, internet or combined support for carers of people living with Alzheimer's, vascular or mixed dementia in the community. Archives of Gerontology and Geriatrics, 66, 218–236. [DOI] [PubMed] [Google Scholar]
Jarvis 2019
- Jarvis, M. A. , Padmanabhanunni, A. , & Chipps, J. (2019). An evaluation of a low‐intensity cognitive behavioral therapy mHealth‐supported intervention to reduce loneliness in older people. International Journal of Environmental Research & Public Health [Electronic Resource], 16(7), 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jarvis 2020
- Jarvis, M. A. , Padmanabhanunni, A. , Balakrishna, Y. , & Chipps, J. (2020). The effectiveness of interventions addressing loneliness in older persons: An umbrella review. International Journal of Africa Nursing Sciences, 12, 100177. [Google Scholar]
Jones 2015
- Jones, R. B. , Ashurst, E. J. , Atkey, J. , & Duffy, B. (2015). Older people going online: Its value and before‐after evaluation of volunteer support. Journal of Medical Internet Research, 17(5), e122. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jones 2020
- Jones, C. , Liu, D. F. , Murfield, M. J. , & Moyle, P. W. (2020). Effects of non‐facilitated meaningful activities for people with dementia in long‐term care facilities: A systematic review. Geriatric Nursing (New York, N.Y.), 41, 863–871. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kachouie 2014
- Kachouie, R. , Sedighadeli, S. , Khosla, R. , & Chu, M. T. (2014). Socially assistive robots in elderly care: A mixed‐method systematic literature review. International Journal of Human‐Computer Interaction, 30(5), 369–393. [Google Scholar]
Kachouie 2017
- Kachouie, R. , Sedighadeli, S. , & Abkenar, A. B. (2017). The role of socially assistive robots in elderly wellbeing: A systematic review. Cross‐Cultural Design, 10281, 669–682. [Google Scholar]
Kahlon 2021
- Kahlon, M. K. , Aksan, N. , Aubrey, R. , Clark, N. , Cowley‐Morillo, M. , Jacobs, E. A. , Mundhenk, R. , Sebastian, K. R. , & Tomlinson, S. (2021). Effect of layperson‐delivered, empathy‐focused program of telephone calls on loneliness, depression, and anxiety among adults during the COVID‐19 pandemic: A randomized clinical trial. JAMA Psychiatry, 78(6), 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kamalpour 2020
- Kamalpour, M. , Watson, J. , & Buys, L. (2020). How can online communities support resilience factors among older adults. International Journal of Human‐Computer Interaction, 36(14), 1342–1353. [Google Scholar]
Kazazi 2021
- Kazazi, L. , Shati, M. , Mortazavi Seyede, S. , Nejati, V. , & Foroughan, M. (2021). The impact of computer‐based cognitive training intervention on the quality of life among elderly people: A randomized clinical trial. Trials, 22(1), 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Keogh 2014
- Keogh, J. W. , Power, N. , Wooller, L. , Lucas, P. , & Whatman, C. (2014). Physical and psychosocial function in residential aged‐care elders: Effect of Nintendo Wii sports games. Journal of Aging and Physical Activity, 22(2), 235–244. [DOI] [PubMed] [Google Scholar]
Khosravi 2016
- Khosravi, P. , Rezvani, A. , & Wiewiora, A. (2016). The impact of technology on older adults' social isolation. Computers in Human Behavior, 63, 594–603. [Google Scholar]
Khosravi 2016a
- Khosravi, P. , & Ghapanchi, A. H. (2016). Investigating the effectiveness of technologies applied to assist seniors: A systematic literature review. International Journal of Medical Informatics, 85(1), 17–26. [DOI] [PubMed] [Google Scholar]
Koh 2021
- Koh, W. Q. , Felding, S. A. , Toomey, E. , & Casey, D. (2021). Barriers and facilitators to the implementation of social robots for older adults and people with dementia: A scoping review protocol. Systematic Reviews, 10(1), 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
Koh 2021a
- Koh, W. Q. , Ang, F. X. H. , & Casey, D. (2021). Impacts of low‐cost robotic pets for older adults and people with dementia: Scoping review. JMIR Rehabilitation And Assistive Technologies, 8(1), e25340. [DOI] [PMC free article] [PubMed] [Google Scholar]
Koo 2019
- Koo, B. M. , & Vizer, L. M. (2019). Examining mobile technologies to support older adults with dementia through the lens of personhood and human needs: Scoping review. JMIR MHealth and UHealth, 7(11), e15122. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kramer 2021
- Kramer, L. L. , Mulder, B. C. , van Velsen, L. , & de Vet, E. (2021). Use and effect of web‐based embodied conversational agents for improving eating behavior and decreasing loneliness among community‐dwelling older adults: Protocol for a randomized controlled trial. JMIR Research Protocols, 10(1), e22186. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kubra 2020
- Kubra, K. (2020). Telerehabilitation in individuals over 65 years of age having social isolation due to coronavirus (Covid‐19). clinicaltrials.gov.
Lady Davis Institute 2021
- Lady Davis Institute . (2021). Virtual chair yoga for older adults and caregivers: Randomized controlled trial. clinicaltrials.gov.
Laganà 2013
- Laganà, L. , & García James, J. (2013). The mental health impact of computer and internet training on a multi‐ethnic sample of community‐dwelling older adults: Results of a pilot randomised controlled trial. International Journal of Biomedical Sciences, 9(3), 135–147. [PMC free article] [PubMed] [Google Scholar]
Lai 2020
- Lai Daniel, W. L. , Li, J. , Ou, X. , & Li Celia, Y. P. (2020). Effectiveness of a peer‐based intervention on loneliness and social isolation of older Chinese immigrants in Canada: A randomized controlled trial. BMC Geriatrics, 20, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lappalainen 2021
- Lappalainen, P. , Pakkala, I. , Lappalainen, R. , & Nikander, R. (2021). Supported Web‐Based acceptance and commitment therapy for older family caregivers (CareACT) compared to usual care. Clinical Gerontologist, 45, 939–955. [DOI] [PubMed] [Google Scholar]
Larsson 2016
- Larsson, E. , Padyab, M. , Larsson‐Lund, M. , & Nilsson, I. (2016). Effects of a social internet‐based intervention programme for older adults: An explorative randomised crossover study. British Journal of Occupational Therapy, 79(10), 629–636. [Google Scholar]
Lauriks 2007
- Lauriks, S. , Reinersmann, A. , van der Roest, H. G. , Meiland, F. , Davies, R. , Moelaert, F. , Mulvenna, M. , Nugent Chris, D. , & Dröes, R.‐M. (2007). Review of ICT‐based services for identified unmet needs in people with dementia. Ageing Research Reviews, 6(3), 223–246. [DOI] [PubMed] [Google Scholar]
Lawson Health Research Institute 2021
- Lawson Health Research Institute . (2021). SSIPP vs. PST vs. WLC. clinicaltrials.gov.
Lee 2021
- Lee, C. , Kuhn, I. , McGrath, M. , Remes, O. , Cowan, A. , Duncan, F. , Baskin, C. , Oliver, E. J. , Osborn, D. P. J. , Dykxhoorn, J. , Kaner, E. , Walters, K. , Kirkbride, J. , Gnani, S. , & Lafortune, L. (2021). Programme Nihr Sphr Public Mental Health. A systematic scoping review of community‐based interventions for the prevention of mental ill‐health and the promotion of mental health in older adults in the UK. Health & Social Care in the Community, 14, 14. [DOI] [PubMed] [Google Scholar]
Li 2017
- Li, J. , Xu, X. , Pham, T. P. , Theng, Y. L. , Katajapuu, N. , & Luimula, M. (2017). Exergames designed for older adults: A pilot evaluation on psychosocial well‐being. Games for Health Journal, 6(6), 371–378. [DOI] [PubMed] [Google Scholar]
Li 2018
- Li, J. , Erdt, M. , Chen, L. , Cao, Y. , Lee, S.‐Q. , & Theng, Y.‐L. (2018). The social effects of exergames on older adults: Systematic review and metric analysis. Journal of Medical Internet Research, 20(6), e10486. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liang 2017
- Liang, A. , Piroth, I. , Robinson, H. , MacDonald, B. , Fisher, M. , Nater, U. M. , Skoluda, N. , & Broadbent, E. (2017). A pilot randomized trial of a companion robot for people with dementia living in the community. Journal of the American Medical Directors Association, 18(10), 871–878. [DOI] [PubMed] [Google Scholar]
Lin 2020
- Lin, T. Y. , Huang, C. M. , Hsu, H. P. , Liao, J. Y. , Cheng, V. Y. , Wang, S. W. , & Guo, J. L. (2020). Effects of a combination of three‐dimensional virtual reality and hands‐on horticultural therapy on institutionalized older adults' physical and mental health: Quasi‐experimental design. Journal of Medical Internet Research, 22(11), e19002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lins 2014
- Lins, S. , Hayder‐Beichel, D. , Rucker, G. , Motschall, E. , Antes, G. , Meyer, G. , & Langer, G. (2014). Efficacy and experiences of telephone counselling for informal carers of people with dementia. Cochrane Database of Systematic Reviews, 9, CD009126. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lopez‐Hartmann 2012
- Lopez‐Hartmann, M. , Wens, J. , Verhoeven, V. , & Remmen, R. (2012). The effect of caregiver support interventions for informal caregivers of community‐dwelling frail elderly: A systematic review. International Journal of Integrated Care, 12, e133. [DOI] [PMC free article] [PubMed] [Google Scholar]
Masi 2010
- Masi, C. M. , Chen, H.‐Y. , Hawkley Louise, C. , & Cacioppo John, T. (2010). A meta‐analysis of interventions to reduce loneliness. Personality and Social Psychology Review, 15(3), 219–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
Matson 2019
- Matson, T. E. , Anderson Melissa, L. , Renz Anne, D. , Greenwood‐Hickman, M. A. , McClure Jennifer, B. , & Rosenberg Dori, E. (2019). Changes in self‐reported health and psychosocial outcomes in older adults enrolled in sedentary behavior intervention study. American Journal of Health Promotion, 33(7), 1053–1057. [DOI] [PubMed] [Google Scholar]
Matz‐Costa 2018
- Matz‐Costa, C. , Lubben, J. , Lachman, M. E. , Lee, H. , & Choi, Y. J. (2018). A pilot randomized trial of an intervention to enhance the health‐promoting effects of older adults' activity portfolios: The Engaged4Life program. Journal of Gerontological Social Work, 61(8), 792–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
McKechnie 2014
- McKechnie, V. , Barker, C. , & Stott, J. (2014). Effectiveness of computer‐mediated interventions for informal carers of people with dementia—A systematic review. International Psychogeriatrics, 26(10), 1619–1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mikkelsen 2019
- Mikkelsen, A. S. B. , Petersen, S. , Dragsted, A. C. , & Kristiansen, M. (2019). Social interventions targeting social relations among older people at nursing homes: A qualitative synthesized systematic review. Inquiry, 56, 46958018823929. [DOI] [PMC free article] [PubMed] [Google Scholar]
Milbury 2020
- Milbury, K. , Higgins, H. M. , Chen, A. B. , Antonoff, M. , Li, Y. , Tsao, A. S. , & Bruera, E. (2020). Pilot randomized controlled trial (RCT) in women with non‐small cell lung cancer (NSCLC) to assess the feasibility of delivering group‐based psychosocial care via videoconference. Journal of Clinical Oncology, 38(29), 257. [DOI] [PMC free article] [PubMed] [Google Scholar]
Miller 2014
- Miller, K. J. , Adair, B. S. , Pearce, A. J. , Said, C. M. , Ozanne, E. , & Morris, M. M. (2014). Effectiveness and feasibility of virtual reality and gaming system use at home by older adults for enabling physical activity to improve health‐related domains: A systematic review. Age & Ageing, 43(2), 188–195. [DOI] [PubMed] [Google Scholar]
Mittelman 2006
- Mittelman, M. S. , Haley, W. E. , Clay, O. J. , & Roth, D. L. (2006). Improving caregiver well‐being delays nursing home placement of patients with Alzheimer disease. Neurology, 67(9), 1592–1599. [DOI] [PubMed] [Google Scholar]
Montana 2020
- Montana, J. I. , Matamala‐Gomez, M. , Maisto, M. , Mavrodiev, P. A. , Cavalera, C. M. , Diana, B. , Mantovani, F. , & Realdon, O. (2020). The benefits of emotion regulation interventions in virtual reality for the improvement of wellbeing in adults and older adults: A systematic review. Journal of Clinical Medicine, 9(2), 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Morris 2014
- Morris, M. E. , Adair, B. , Ozanne, E. , Kurowski, W. , Miller, K. J. , Pearce, A. J. , Santamaria, N. , Long, M. , Ventura, C. , & Said, C. M. (2014). Smart technologies to enhance social connectedness in older people who live at home. Australasian Journal on Ageing, 33(3), 142–152. [DOI] [PubMed] [Google Scholar]
Morton 2018
- Morton, T. A. , Wilson, N. , Haslam, C. , Birney, M. , Kingston, R. , & McCloskey, L. G. (2018). Activating and guiding the engagement of seniors with online social networking: Experimental findings from the AGES 2.0 project. Journal of Aging & Health, 30(1), 27–51. [DOI] [PubMed] [Google Scholar]
Mountain 2014
- Mountain, G. A. , Hind, D. , Gossage‐Worrall, R. , Walters, S. J. , Duncan, R. , Newbould, L. , Rex, S. , Jones, C. , Bowling, A. , Cattan, M. , Cairns, A. , Cooper, C. , Edwards, R. T. , & Goyder, E. C. (2014). ‘Putting Life in Years’ (PLINY) telephone friendship groups research study: Pilot randomised controlled trial. Trials [Electronic Resource], 15, 141. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moyle 2017
- Moyle, W. , Jones, C. , Murfield, J. , Thalib, L. , Beattie, E. , Shum, D. , O'Dwyer, S. , Mervin, C. , & Draper, B. (2017). Use of a robotic seal as a therapeutic tool to improve dementia symptoms: A cluster‐randomized controlled trial. Journal of the American Medical Directors Association, 18(9), 766–773. [DOI] [PubMed] [Google Scholar]
Myhre 2015
- Myhre, J. W. (2015). Effects of online social networking on the cognitive, social, and emotional health of older adults. Dissertation Abstracts International: Section B: The Sciences and Engineering, 76(1–B(E)). https://repository.arizona.edu/handle/10150/332671 [Google Scholar]
Myhre 2017
- Myhre, J. W. , Mehl, M. R. , & Glisky, E. L. (2017). Cognitive benefits of online social networking for healthy older adults. Journals of Gerontology Series B‐Psychological Sciences & Social Sciences, 72(5), 752–760. [DOI] [PubMed] [Google Scholar]
Neal 2021
- Neal, D. P. , Kerkhof, Y. J. F. , Ettema, T. P. , Muller, M. , Bosmans, J. , Finnema, E. , Graff, M. , Dijkstra, K. , Stek, M. L. , & Droes, R. M. (2021). Evaluation of FindMyApps: Protocol for a randomized controlled trial of the effectiveness and cost‐effectiveness of a tablet‐based intervention to improve self‐management and social participation of community‐dwelling people with mild dementia, compared to usual tablet use. BMC Geriatrics, 21(1), 138. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nef 2013
- Nef, T. , Ganea, R. L. , Muri, R. M. , & Mosimann, U. P. (2013). Social networking sites and older users—A systematic review. International Psychogeriatrics, 25(7), 1041–1053. [DOI] [PubMed] [Google Scholar]
New Study 2
- Panagiota, E. , & Christiana, D. K. (2011). The application of innovative technologies in elderly health care in the community. Cyprus Nursing Chronicles, 12(2), 7–17. [Google Scholar]
Nijhof 2009
- Nijhof, N. , van Gemert‐Pijnen, J. , Dohmen, D. , & Seydel, E. (2009). Dementia and technology: A study of technology interventions in the healthcare for dementia patients and their caregivers. Tijdschrift voor Gerontologie en Geriatrie, 40(3), 113–132. [DOI] [PubMed] [Google Scholar]
Nikitina 2018
- Nikitina, S. , Didino, D. , Baez, M. , Casati, F. , & Feasibility of Virtual Tablet‐Based Group . (2018). Exercise among older adults in Siberia: Findings from two pilot trials. JMIR MHealth and UHealth, 6(2), e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nilsson 2021
- Nilsson, M. Y. , Andersson, S. , Magnusson, L. , & Hanson, E. (2021). Ambient assisted living technology‐mediated interventions for older people and their informal carers in the context of healthy ageing: A scoping review. Health Science Reports, 4(1), e225. [DOI] [PMC free article] [PubMed] [Google Scholar]
Noone 2020
- Noone, C. , McSharry, J. , Smalle, M. , Burns, A. , Dwan, K. , Devane, D. , & Morrissey, E. C. (2020). Video calls for reducing social isolation and loneliness in older people: A rapid review. Cochrane Database of Systematic Reviews, 5, CD013632. [DOI] [PMC free article] [PubMed] [Google Scholar]
O'Rourke 2018
- O'Rourke, H. M. , Collins, L. , & Sidani, S. (2018). Interventions to address social connectedness and loneliness for older adults: A scoping review. BMC Geriatrics, 18(1), 214. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ollevier 2020
- Ollevier, A. , Aguiar, G. , Palomino, M. , & Simpelaere, I. S. (2020). How can technology support ageing in place in healthy older adults? A systematic review. Public Health Reviews, 41(1), 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Papadopoulos 2021
- Papadopoulos, C. , Castro, N. , Nigath, A. , Davidson, R. , Faulkes, N. , Menicatti, R. , Khaliq, A. A. , Recchiuto, C. , Battistuzzi, L. , Randhawa, G. , Merton, L. , Kanoria, S. , Chong, N. Y. , Kamide, H. , Hewson, D. , & Sgorbissa, A. (2021). The CARESSES randomised controlled trial: Exploring the health‐related impact of culturally competent artificial intelligence embedded into socially assistive robots and tested in older adult care homes. International Journal of Social Robotics, 14, 245–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
Parkinson 2018
- Parkinson, L. , Banbury, A. , Livingstone, A. , Gordon, S. , Ray, B. , Byrne, L. , Nancarrow, S. , Doran, C. , McAllister, M. , Petersen, C. , Pedell, S. , & Wood, D. (2018). Caring for carers of people with dementia: A protocol for harnessing innovation through deploying leading edge technologies to enable virtual support groups and services. Studies in Health Technology & Informatics, 246, 29–41. [PubMed] [Google Scholar]
Pedrozo 2019
- Pedrozo, C. A. T. , Souza Bulle de Oliveira, A. , Hudec, R. , Brusque Crocetta, T. , Ferreira de Lima Antao, J. Y. , de Almeida Barbosa, R. T. , Guarnieri, R. , Massetti, T. , Garner, D. M. , & de Abreu, L. C. (2019). Assistive technology for communication of older adults: A systematic review. Aging & Mental Health, 23(4), 417–427. [DOI] [PubMed] [Google Scholar]
Pepin 2019
- Pepin, R. , DiMilia, P. , Choi, N. , & Bruce, M. (2019). Tele‐behavioral activation for social isolation in older home‐delivered meals recipients: Preliminary results from an ongoing randomized controlled trial. American Journal of Geriatric Psychiatry, 27(3), S129–S130. [Google Scholar]
Pereira 2018
- Pereira, L. , Dias, A. , Queiros, A. , & Rocha, N. P. (2018). Technologies for ageing in place: A systematic review of reviews and meta‐analyses. Biomedical Engineering Systems and Technologies, 881, 331–353. [Google Scholar]
Peres 2021
- Peres, K. , Zamudio‐Rodriguez, A. , Dartigues, J. F. , Amieva, H. , & Lafitte, S. (2021). Prospective pragmatic quasi‐experimental study to assess the impact and effectiveness of an innovative large‐scale public health intervention to foster healthy ageing in place: The SoBeezy program protocol. BMJ Open, 11(4), e043082. [DOI] [PMC free article] [PubMed] [Google Scholar]
Peters 2021
- Peters, M. D. , Marnie, C. , Colquhoun, H. , Garritty, C. M. , Hempel, S. , Horsley, T. , Langlois, E. V. , Lillie, E. , O'Brien, K. K. , Tunçalp, Ö. , Wilson, M. G. , Zarin, W. , & Tricco, A. C. (2021). Scoping reviews: Reinforcing and advancing the methodology and application. Systematic Reviews, 10(1), 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pinto‐Bruno 2017
- Pinto‐Bruno, A. C. , Garcia‐Casal, J. A. , Csipke, E. , Jenaro‐Rio, C. , & Franco‐Martin, M. (2017). ICT‐based applications to improve social health and social participation in older adults with dementia. A systematic literature review. Aging & Mental Health, 21(1), 58–65. [DOI] [PubMed] [Google Scholar]
Portz 2017
- Portz, J. D. (2017). A review of web‐based chronic disease self‐management for older adults. Gerontechnology, 16(1), 12–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Poscia 2018
- Poscia, A. , Stojanovic, J. , La Milia, D. I. , Duplaga, M. , Grysztar, M. , Moscato, U. , Graziano, O. , Collamati, A. , Ricciardi, W. , & Magnavita, N. (2018). Interventions targeting loneliness and social isolation among the older people: An update systematic review. Experimental Gerontology, 102, 133–144. [DOI] [PubMed] [Google Scholar]
Pu 2019
- Pu, L. , Moyle, W. , Jones, C. , & Todorovic, M. (2019). The effectiveness of social robots for older adults: A systematic review and meta‐analysis of randomized controlled studies. Gerontologist, 59(1), e37–e51. [DOI] [PubMed] [Google Scholar]
Queiros 2017
- Queiros, A. , Santos, M. , Rocha, N. P. , & Cerqueira, M. (2017). Technologies for ageing in place to support community‐dewlling older adults. In 2017 12th Iberian Conference on Information Systems and Technologies. IEEE. [Google Scholar]
Quinn 2021
- Quinn, K. (2021). Social media and social wellbeing in later life. Ageing and Society, 41(6), 1349–1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rainero 2021
- Rainero, I. , Summers, M. J. , Monter, M. , Bazzani, M. , Giannouli, E. , Aumayr, G. , Burin, D. , Provero, P. , Vercelli, A. E. , My, A. , & HA Consortium . (2021). The My Active and Healthy Aging ICT platform prevents quality of life decline in older adults: A randomised controlled study. Age and Ageing, 50(4), 1261–1267. [DOI] [PubMed] [Google Scholar]
Rienzo 2019
- Rienzo, A. , & Cubillos, C. (2019). Research of gamification techniques and their application in digital games for older Adults. IEEE. [Google Scholar]
Robbins 2019
- Robbins, R. E. (2019). The effect of social interaction on isolated older adults. Dissertation Abstracts International: Section B: The Sciences and Engineering, 80(1–B(E)). https://repository.arizona.edu/handle/10150/630189 [Google Scholar]
Robinson 2013
- Robinson, H. , Macdonald, B. , Kerse, N. , & Broadbent, E. (2013). The psychosocial effects of a companion robot: A randomized controlled trial. Journal of the American Medical Directors Association, 14(9), 661–667. [DOI] [PubMed] [Google Scholar]
Robinson 2019
- Robinson, N. L. , Cottier, T. V. , & Kavanagh, D. J. (2019). Psychosocial health interventions by social robots: Systematic review of randomized controlled trials. Journal of Medical Internet Research, 21(5), e13203. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ronzi 2018
- Ronzi, S. , Orton, L. , Pope, D. , Valtorta, N. K. , & Bruce, N. G. (2018). What is the impact on health and wellbeing of interventions that foster respect and social inclusion in community‐residing older adults? A systematic review of quantitative and qualitative studies. Systematic Reviews, 7(1), 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Roth 2014
- Roth, A. (2014). Engaging older cancer patients in psychotherapy and psychoeducation interventions: Care and vintage readers programs. Psycho‐Oncology, 23, 31. [Google Scholar]
Salehi 2021
- Salehi, A. , Salehi, E. , Mosadeghi‐Nik, M. , Sargeant, S. , & Fatehi, F. (2021). Strengthening positive social pathways via digital social applications in individuals with social skills deficits: A scoping review. International Journal of Social Psychiatry, 67(6), 779–787. [DOI] [PubMed] [Google Scholar]
Schulz 2002
- Schulz, R. , Lustig, A. , Handler, S. , & Martire Lynn, M. (2002). Technology‐based caregiver intervention research: Current status and future directions. Gerontechnology, 2(1), 15–47. [Google Scholar]
Schwindenhammer 2014
- Schwindenhammer, T. M. (2014). Videoconferencing intervention for depressive symptoms and loneliness in nursing home elders.
Sciamanna 2021
- Sciamanna, C. , Ballentine, N. H. , Bopp, M. , Chinchilli, V. M. , Ciccolo, J. T. , Delauter, G. , Fisher, A. , Fox, E. J. , Jan De Beur, S. , Kearcher, K. , Kraschnewski, J. L. , Lehman, E. , McTigue, K. M. , McAuley, E. , Paranjape, A. , Rodriguez‐Colon, S. , Rovniak, L. , Rutt, K. , Smyth, J. M. , Stewart, K. J. , Stuckey, H. L. , & Tsay, A. (2021). Working to increase stability through exercise (WISE): Screening, recruitment, and baseline characteristics. Trials, 22, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Scoglio 2019
- Scoglio, A. A. , Reilly, E. D. , Gorman, J. A. , & Drebing, C. E. (2019). Use of social robots in mental health and well‐being research: Systematic review. Journal of Medical Internet Research, 21(7), e13322. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shah 2021
- Shah, S. G. S. , Nogueras, D. , van Woerden, H. , & Kiparoglou, V. (2021). Evaluation of the effectiveness of digital technology interventions to reduce loneliness in older adults: Systematic review and meta‐analysis. Journal of Medical Internet Research, 23(6), e24712. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shapira 2007
- Shapira, N. , Barak, A. , & Gal, I. (2007). Promoting older adults' well‐being through Internet training and use. Aging & Mental Health, 11(5), 477–484. [DOI] [PubMed] [Google Scholar]
Shapira 2021
- Shapira, S. , Yeshua‐Katz, D. , Goren, G. , Aharonson‐Daniel, L. , Clarfield, A. M. , Sarid, O. , & Evaluation of a Short‐Term Digital Group . (2021). Intervention to relieve mental distress and promote well‐being among community‐dwelling older individuals during the COVID‐19 outbreak: A study protocol. Frontiers in Public Health, 9, 577079. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shapira 2021a
- Shapira, S. , Yeshua‐Katz, D. , Cohn‐Schwartz, E. , Aharonson‐Daniel, L. , Sarid, O. , & Clarfield, A. M. (2021). A pilot randomized controlled trial of a group intervention via Zoom to relieve loneliness and depressive symptoms among older persons during the COVID‐19 outbreak. Internet Interventions, 24, 100368. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shishehgar 2018
- Shishehgar, M. , Kerr, D. , & Blake, J. (2018). A systematic review of research into how robotic technology can help older people. Smart Health, 7–8, 1–18. [Google Scholar]
Shishehgar 2019
- Shishehgar, M. , Kerr, D. , & Blake, J. (2019). The effectiveness of various robotic technologies in assisting older adults. Health Informatics Journal, 25(3), 892–918. [DOI] [PubMed] [Google Scholar]
Smallfield 2018
- Smallfield, S. , & Molitor, W. L. (2018). Occupational therapy interventions supporting social participation and leisure engagement for community‐dwelling older adults: A systematic review. American Journal of Occupational Therapy, 72(4), 7204190020p1–7204190020p8. [DOI] [PubMed] [Google Scholar]
Smith 2006
- Smith, T. L. , & Toseland, R. W. (2006). The effectiveness of a telephone support program for caregivers of frail older adults. Gerontologist, 46(5), 620–629. [DOI] [PubMed] [Google Scholar]
Smith 2011
- Smith, L. J. (2011). The effect of training in internet use on perceived loneliness, depression and well‐being with the African American elderly. Dissertation Abstracts International: Section B: The Sciences and Engineering, 71(12–B), 7354. [Google Scholar]
Smith 2017
- Smith, S. K. , & Astell, A (2017). Independent living functions for the elderly (IN‐LIFE): Supporting communication in dementia. Studies in Health Technology and Infomatics, 242, 16–22. [PubMed] [Google Scholar]
Song 2009
- Song, J. H. (2009). [Effects of a robot pet‐assisted program for elderly people with dementia]. Journal of Korean Academy of Nursing, 39(4), 562–573. [DOI] [PubMed] [Google Scholar]
Song 2019
- Song, Y. , & van der Cammen, T. J. M. (2019). Electronic assistive technology for community‐dwelling solo‐living older adults: A systematic review. Maturitas, 125, 50–56. [DOI] [PubMed] [Google Scholar]
Sosa 2012
- Sosa Giovanni, W. (2012). The impact of a video game intervention on the cognitive functioning, self‐ efficacy, self‐esteem, and video game attitudes of older adults. Dissertation Abstracts International Section A: Humanities and Social Sciences, 73(5–A), 1885. [Google Scholar]
Su 2020
- Su, Z. , Meyer, K. , Li, Y. , McDonnell, D. , Joseph, N. M. , Li, X. , Du, Y. , Advani, S. , Cheshmehzangi, A. , Ahmad, J. , da Veiga, C. P. , Chung, R. Y. , & Wang, J. (2020). Technology‐based interventions for nursing home residents: Implications for nursing home practice amid and beyond the influence of COVID‐19: A systematic review protocol. Research Square, 18, 18. [Google Scholar]
Tanaka 2012
- Tanaka, M. , Ishii, A. , Yamano, E. , Ogikubo, H. , Okazaki, M. , Kamimura, K. , Konishi, Y. , Emoto, S. , & Watanabe, Y. (2012). Effect of a human‐type communication robot on cognitive function in elderly women living alone. Medical Science Monitor, 18(9), CR550–CR557. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thodberg 2016
- Thodberg, K. , Sorensen, L. U. , Christensen, J. W. , Poulsen, P. H. , Houbak, B. , Damgaard, V. , Keseler, I. , Edwards, D. , & Videbech, P. B. (2016). Therapeutic effects of dog visits in nursing homes for the elderly. Psychogeriatrics: The Official Journal of the Japanese Psychogeriatric Society, 16(5), 289–297. [DOI] [PubMed] [Google Scholar]
Tomasino 2017
- Tomasino, K. N. , Lattie, E. G. , Ho, J. , Palac, H. L. , Kaiser, S. M. , & Mohr, D. C. (2017). Harnessing peer support in an online intervention for older adults with depression. American Journal of Geriatric Psychiatry, 25(10), 1109–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tsai 2010
- Tsai, H. H. , Tsai, Y. F. , Wang, H. H. , Chang, Y. C. , & Chu, H. H. (2010). Videoconference program enhances social support, loneliness, and depressive status of elderly nursing home residents. Aging & Mental Health, 14(8), 947–954. [DOI] [PubMed] [Google Scholar]
Tsai 2011
- Tsai, H. H. , & Tsai, Y. F. (2011). Changes in depressive symptoms, social support, and loneliness over 1 year after a minimum 3‐month videoconference program for older nursing home residents. Journal of Medical Internet Research, 13(4), e93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tsai 2020
- Tsai, H. H. , Cheng, C. Y. , Shieh, W. Y. , & Chang, Y. C. (2020). Effects of a smartphone‐based videoconferencing program for older nursing home residents on depression, loneliness, and quality of life: A quasi‐experimental study. BMC Geriatrics, 20(1), 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tsai 2020a
- Tsai, H. H. , Cheng, C. Y. , & Shieh, W. Y. (2020). Effectiveness of laptop‐based versus smartphone‐based videoconferencing interaction on loneliness, depression and social support in nursing home residents: A secondary data analysis. Journal of Telemedicine & Telecare, 29(3), 177–186. [DOI] [PubMed] [Google Scholar]
Tyack 2017
- Tyack Charles, S. M. , & Camic Paul, M. (2017). Touchscreen interventions and the well‐being of people with dementia and caregivers: A systematic review. International Psychogeriatrics, 29(8), 1261–1280. [DOI] [PubMed] [Google Scholar]
University of Texas at Austin 2020
- University of Texas at Austin . (2020). Telephone calls for health for homebound older adults. clinicaltrials.gov.
Uppsala University 2020
- Uppsala University . (2020). Treatment of depressive symptoms in older individuals in isolation during Covid‐19. clinicaltrials.gov.
Van Den Heuvel 2019
- Van Den Heuvel, R. , Lexis, M. , & Daniels, R. (2019). CRDL—Interactive technology eliciting engagement in elderly people with dementia. Technology and Disability, 31(Supplement 1), S114. [Google Scholar]
Van Houwelingen‐Snippe 2021
- Van Houwelingen‐Snippe, J. , Ben Allouch, S. , & Van Rompay, T. J. L. (2021). Virtual reality representations of nature to improve well‐being amongst older adults: A rapid review. Journal of Technology in Behavioral Science, 6, 464–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vanova 2018
- Vanova, M. , Irazoki, E. , Garcia‐Casal, J. A. , Martinez‐Abad, F. , Botella, C. , Shiells, K. R. , & Franco‐Martin, M. A. (2018). The effectiveness of ICT‐based neurocognitive and psychosocial rehabilitation programmes in people with mild dementia and mild cognitive impairment using GRADIOR and ehcoBUTLER: Study protocol for a randomised controlled trial. Trials [Electronic Resource], 19(1), 100. [DOI] [PMC free article] [PubMed] [Google Scholar]
VanRavenstein 2020
- VanRavenstein, K. , Brotherton, S. , & Davis, B. (2020). Investigating the feasibility of using telemedicine to deliver a fall prevention program: A pilot study. Journal of Allied Health, 49(3), 221–227. [PubMed] [Google Scholar]
Vazquez 2019
- Vazquez, F. L. , Torres, A. J. , Otero, P. , Blanco, V. , Lopez, L. , Garcia‐Casal, A. , & Arrojo, M. (2019). Cognitive‐behavioral intervention via interactive multimedia online video game for active aging: Study protocol for a randomized controlled trial. Trials [Electronic Resource], 20(1), 692. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wasilewski 2017
- Wasilewski, M. B. , Stinson, J. N. , & Cameron, J. I. (2017). Web‐based health interventions for family caregivers of elderly individuals: A scoping review. International Journal of Medical Informatics, 103, 109–138. [DOI] [PubMed] [Google Scholar]
White 1999
- White, H. , McConnell, E. , Clipp, E. , Bynum, L. , Teague, C. , Navas, L. , Craven, S. , & Halbrecht, H. (1999). Surfing the net in later life: A review of the literature and pilot study of computer use and quality of life. Journal of Applied Gerontology, 18(3), 358–378. [Google Scholar]
White 2002
- White, H. , McConnell, E. , Clipp, E. , Branch, L. G. , Sloane, R. , Pieper, C. , & Box, T. L. (2002). A randomized controlled trial of the psychosocial impact of providing internet training and access to older adults. Aging & Mental Health, 6(3), 213–221. [DOI] [PubMed] [Google Scholar]
Woodward 2011
- Woodward, A. T. , Freddolino, P. P. , Blaschke‐Thompson, C. M. , Wishart, D. J. , Bakk, L. , Kobayashi, R. , & Tupper, C. (2011). Technology and aging project: Training outcomes and efficacy from a randomized field trial. Ageing International, 36(1), 46–65. [Google Scholar]
Zaccaria 2020
- Zaccaria, D. , Guaita, A. , Vaccaro, R. , Casanova, G. , Abbondanza, S. , Pettinato, L. , Cerati, G. , Rolandi, E. , & Sala, E. (2020). Assessing the impact of social networking site use on older people's loneliness and social isolation. A randomized controlled trial: The Aging in a Networked Society‐Social Experiment Study (ANS‐SE). Contemporary Clinical Trials Communications, 19, 100615. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhao 2020
- Zhao, X. , Wang, L. N. , Ge, C. X. , Zhen, X. T. , Chen, Z. , Wang, J. , & Zhou, Y. Y. (2020). Smartphone application training program improves smartphone usage competency and quality of life among the elderly in an elder university in China: A randomized controlled trial. International Journal of Medical Informatics, 133, 104010. [DOI] [PubMed] [Google Scholar]
EXCLUDED STUDIES Bolle 2015
- * Bolle, S. , van Weert, J. C. , Daams, J. G. , Loos, E. F. , De Haes, H. C. , & Smets, E. M. (2015). Online health information tool effectiveness for older patients: A systematic review of the literature. Journal of Health Communication, 20(9), 1067–1083. [DOI] [PubMed] [Google Scholar]
Burkow 2015
- * Burkow, T. M. , Vognild, L. K. , Johnsen, E. , Risberg, M. J. , Bratvold, A. , Breivik, E. , & Hjalmarsen, A. (2015). Comprehensive pulmonary rehabilitation in home‐based online groups: A mixed method pilot study in COPD. BMC Research Notes, 8(1), 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Clarkson 2018
- * Clarkson, P. , Hughes, J. , Roe, B. , Giebel, C. M. , Jolley, D. , Poland, F. , & Challis, D. (2018). Systematic review: Effective home support in dementia care, components and impacts—Stage 2, effectiveness of home support interventions. Journal of Advanced Nursing, 74(3), 507–527. [DOI] [PubMed] [Google Scholar]
Cooper 2014
- * Cooper, K. , Kirkpatrick, P. , & Wilcock, S. (2014). The effectiveness of peer support interventions for community‐dwelling adults with chronic non‐cancer pain: A systematic review. JBI Evidence Synthesis, 12(5), 319–348. [Google Scholar]
Dam 2017
- * Dam, A. E. , de Vugt, M. E. , van Boxtel, M. P. , & Verhey, F. R. (2017). Effectiveness of an online social support intervention for caregivers of people with dementia: The study protocol of a randomised controlled trial. Trials, 18(1), 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dickens 2011
- * Dickens, A. P. , Richards, S. H. , Hawton, A. , Taylor, R. S. , Greaves, C. J. , Green, C. , & Campbell, J. L. (2011). An evaluation of the effectiveness of a community mentoring service for socially isolated older people: A controlled trial. BMC Public Health, 11(1), 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Erfani 2018
- * Erfani, S. S. , & Abedin, B. (2018). Impacts of the use of social network sites on users’ psychological well‐being: A systematic review. Journal of the Association for Information Science and Technology, 69(7), 900–912. [Google Scholar]
Fan 2016
- Fan, Q. (2016). Utilizing ICT to prevent loneliness and social isolation of the elderly: A literature review. Cuadernos de Trabajo Social, 29(2), 185–200. 10.5209/CUTS.51771 [DOI] [Google Scholar]
Forsman 2017
- * Forsman, A. K. , & Nordmyr, J. (2017). Psychosocial links between Internet use and mental health in later life: A systematic review of quantitative and qualitative evidence. Journal of Applied Gerontology, 36(12), 1471–1518. [DOI] [PubMed] [Google Scholar]
Gine‐Garriga 2017
- * Giné‐Garriga, M. , Coll‐Planas, L. , Guerra, M. , Domingo, À. , Roqué, M. , Caserotti, P. , & Salvà, A. (2017). The SITLESS project: Exercise referral schemes enhanced by self‐management strategies to battle sedentary behaviour in older adults: Study protocol for a randomised controlled trial. Trials, 18(1), 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gorenko 2021
- * Gorenko, J. A. , Moran, C. , Flynn, M. , Dobson, K. , & Konnert, C. (2021). Social isolation and psychological distress among older adults related to COVID‐19: A narrative review of remotely‐delivered interventions and recommendations. Journal of Applied Gerontology, 40(1), 3–13. [DOI] [PubMed] [Google Scholar]
Jones 2019
- * Jones, C. A. , Siever, J. , Knuff, K. , Van Bergen, C. , Mick, P. , Little, J. , & Miller, H. (2019). Walk, Talk and Listen: A pilot randomised controlled trial targeting functional fitness and loneliness in older adults with hearing loss. BMJ Open, 9(4), e026169. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lara 2016
- * Lara, J. , O'Brien, N. , Godfrey, A. , Heaven, B. , Evans, E. H. , Lloyd, S. , & Mathers, J. C. (2016). Pilot randomised controlled trial of a web‐based intervention to promote healthy eating, physical activity and meaningful social connections compared with usual care control in people of retirement age recruited from workplaces. PLoS One, 11(7), e0159703. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nicholson 2012
- * Nicholson, N. R. (2012). A review of social isolation: An important but underassessed condition in older adults. The Journal of Primary Prevention, 33(2), 137–152. [DOI] [PubMed] [Google Scholar]
Nijman 2019
- * Nijman, S. A. , Veling, W. , Greaves‐Lord, K. , Vermeer, R. R. , Vos, M. , Zandee, C. E. , & Pijnenborg, G. H. (2019). Dynamic Interactive Social Cognition Training in Virtual Reality (DiSCoVR) for social cognition and social functioning in people with a psychotic disorder: Study protocol for a multicenter randomized controlled trial. BMC Psychiatry, 19(1), 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Perkins 2012
- * Perkins, E. A. , & LaMartin, K. M. (2012). The Internet as social support for older carers of adults with intellectual disabilities. Journal of Policy and Practice in Intellectual Disabilities, 9(1), 53–62. [Google Scholar]
Preston 2019
- * Preston, C. , & Moore, S. (2019). Ringing the changes: The role of telephone communication in a helpline and befriending service targeting loneliness in older people. Ageing & Society, 39(7), 1528–1551. [Google Scholar]
Rebollar 2015
- * Rebollar, A. M. , & Francisco, W. C. (2015). Correlación entre actividades de interacción social registradas con nuevas tecnologías y el grado de aislamiento social en los adultos mayores. Revista mexicana de ingeniería biomédica, 36(3), 181–190. [Google Scholar]
Selak 2019
- * Selak, Š. , Bacaicoa, O. A. , & Gabrovec, B. (2019). Can we manage frailty at individual level by the use of information and communication technologies: A narrative literature review. Slovenian Medical Journal, 88(5–6), 249–262. [Google Scholar]
Sumner 2021
- * Sumner, J. , Chong, L. S. , Bundele, A. , & Wei Lim, Y. (2021). Co‐designing technology for aging in place: A systematic review. The Gerontologist, 61(7), e395–e409. [DOI] [PMC free article] [PubMed] [Google Scholar]
Toh 2016
- * Toh, H. M. , Ghazali, S. E. , & Subramaniam, P. (2016). The acceptability and usefulness of cognitive stimulation therapy for older adults with dementia: A narrative review. International Journal of Alzheimer's Disease, 2016, 5131570. [DOI] [PMC free article] [PubMed] [Google Scholar]
Winterton 2011
- * Winterton, R. , & Warburton, J. (2011). Models of care for socially isolated older rural carers: Barriers and implications. Rural and Remote Health, 11(3), 203–215. [PubMed] [Google Scholar]
Zeppegno 2018
- * Zeppegno, P. , Gattoni, E. , Mastrangelo, M. , Gramaglia, C. , & Sarchiapone, M. (2019). Psychosocial suicide prevention interventions in the elderly: A mini‐review of the literature. Frontiers in Psychology, 9, 2713. [DOI] [PMC free article] [PubMed] [Google Scholar]
STUDIES AWAITING CLASSIFICATION
- Ongoing studies
- Other references
- Additional references
Abdi 2019
- Abdi, S. , Spann, A. , Borilovic, J. , de Witte, L. , & Hawley, M. (2019). Understanding the care and support needs of older people: A scoping review and categorisation using the WHO international classification of functioning, disability and health framework (ICF). BMC Geriatrics, 19(1), 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bedney 2010
- Bedney Barbara, J. , Goldberg Robert, B. , & Josephson, K. (2010). Aging in place in naturally occurring retirement communities: Transforming aging through supportive service programs. Journal of Housing for the Elderly, 24(3–4), 304–321. [Google Scholar]
Berkman 2000
- Berkman Lisa, F. , Glass, T. , Brissette, I. , & Seeman Teresa, E. (2000). From social integration to health: Durkheim in the new millennium. Social Science & Medicine, 51(6), 843–857. [DOI] [PubMed] [Google Scholar]
Bethell 2019
- Bethell, J. , Babineau, J. , Iaboni, A. , Green, R. , Cuaresma‐Canlas, R. , Karunananthan, R. , Schon, B. , Schon, D. , & McGilton Katherine, S. (2019). Social integration and loneliness among long‐term care home residents: Protocol for a scoping review. BMJ Open, 9(12), e033240. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boulton 2020
- Boulton, E. , Kneale, D. , Stansfield, C. , Heron, P. , Sutcliffe, K. , Hayanga, B. , Hall, A. , Bower, P. , Casey, D. , & Craig, D. (2020). Rapid systematic review of systematic reviews: What befriending, social support and low intensity psychosocial interventions, delivered remotely, are effective in reducing social isolation and loneliness among older adults? How do they work?[version 1; peer review: Awaiting peer review]. F1000Research, 9, 1368. 10.12688/f1000research.27076.2 [DOI] [Google Scholar]
Brooke 2020
- Brooke, J. , & Jackson, D. (2020). Older people and COVID‐19: Isolation, risk and ageism. Journal of Clinical Nursing, 29(13–14), 2044–2046. [DOI] [PubMed] [Google Scholar]
Budd 2020
- Budd, J. , Miller Benjamin, S. , Manning Erin, M. , Lampos, V. , Zhuang, M. , Edelstein, M. , Rees, G. , Emery Vincent, C. , Stevens Molly, M. , & Keegan, N. (2020). Digital technologies in the public‐health response to COVID‐19. Nature Medicine, 26(8), 1183–1192. [DOI] [PubMed] [Google Scholar]
Cacioppo 2009
- Cacioppo, J. T. , Fowler, J. H. , & Christakis, N. A. (2009). Alone in the crowd: The structure and spread of loneliness in a large social network. Journal of Personality and Social Psychology, 97(6), 977. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cacioppo 2014
- Cacioppo, J. T. , Cacioppo, S. , & Boomsma, D. I. (2014). Evolutionary mechanisms for loneliness. Cognition & Emotion, 28(1), 3–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cattan 2005
- Cattan, M. , White, M. , Bond, J. , & Learmouth, A. (2005). Preventing social isolation and loneliness among older people: A systematic review of health promotion interventions. Ageing & Society, 25(1), 41–67. [DOI] [PubMed] [Google Scholar]
Chen 2016
- Chen Yi‐Ru, R. , & Schulz Peter, J. (2016). The effect of information communication technology interventions on reducing social isolation in the elderly: A systematic review. Journal of Medical Internet Research, 18(1), e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chipps 2017
- Chipps, J. , Jarvis Mary, A. , & Ramlall, S. (2017). The effectiveness of e‐interventions on reducing social isolation in older persons: A systematic review of systematic reviews. Journal of Telemedicine and Telecare, 23(10), 817–827. [DOI] [PubMed] [Google Scholar]
Cohen‐Mansfield 2015
- Cohen‐Mansfield, J. , & Perach, R. (2015). Interventions for alleviating loneliness among older persons: A critical review. American Journal of Health Promotion, 29(3), e109–e125. [DOI] [PubMed] [Google Scholar]
DeGood 2011
- DeGood, K. (2011). Aging in place, stuck without options: Fixing the mobility crisis threatening the baby boom generation. http://t4america.org/docs/SeniorsMobilityCrisis.pdf
Dickens 2011
- Dickens Andy, P. , Richards Suzanne, H. , Greaves Colin, J. , & Campbell John, L. (2011). Interventions targeting social isolation in older people: A systematic review. BMC Public Health, 11(1), 1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Digital Solution Foundry and EPPI_Centre 2020
- Eppi‐Mapper [Computer program] . (2020). Digital Solution Foundry and EPPI_Centre. EPPI‐Centre, UCL Social Research Institute, University College London. [Google Scholar]
Donovan 2020
- Donovan, N. J. , & Blazer, D. (2020). Social isolation and loneliness in older adults: Review and commentary of a National Academies Report. The American Journal of Geriatric Psychiatry, 28(12), 1233–1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elder 2012
- Elder, K. , & Retrum, J. (2012). Framework for isolation in adults over 50. AARP Foundation. [Google Scholar]
Fakoya 2020
- Fakoya, O. A. , McCorry, N. K. , & Donnelly, M. (2020). Loneliness and social isolation interventions for older adults: A scoping review of reviews. BMC Public Health, 20(1), 129. [DOI] [PMC free article] [PubMed] [Google Scholar]
Falk 2021
- Falk, W. (2021). The state of virtual care in Canada as of wave three of the COVID‐19 pandemic: An early diagnostique and policy recommendations. Healh Canada, 21–38. https://tinyurl.com/4krrrsmc [Google Scholar]
Findlay 2003
- Findlay, R. A. (2003). Interventions to reduce social isolation amongst older people: Where is the evidence? Ageing & Society, 23(5), 647–658. [Google Scholar]
Gardiner 2018
- Gardiner, C. , Geldenhuys, G. , & Gott, M. (2018). Interventions to reduce social isolation and loneliness among older people: An integrative review. Health & Social Care in the Community, 26(2), 147–157. [DOI] [PubMed] [Google Scholar]
Hagan 2014
- Hagan, R. , Manktelow, R. , Taylor Brian, J. , & Mallett, J. (2014). Reducing loneliness amongst older people: A systematic search and narrative review. Aging & Mental Health, 18(6), 683–693. [DOI] [PubMed] [Google Scholar]
Henderson 2008
- Henderson, E. J. , & Caplan, G. A. (2008). Home sweet home? Community care for older people in Australia. Journal of the American Medical Directors Association, 9(2), 88–94. [DOI] [PubMed] [Google Scholar]
Holt‐Lunstad 2015
- Holt‐Lunstad, J. , Smith Timothy, B. , Baker, M. , Harris, T. , & Stephenson, D. (2015). Loneliness and social isolation as risk factors for mortality: A meta‐analytic review. Perspectives on Psychological Science, 10(2), 227–237. [DOI] [PubMed] [Google Scholar]
Ibarra 2020
- Ibarra, F. , Baez, M. , Cernuzzi, L. , & Casati, F. (2020). A systematic review on technology‐supported interventions to improve old‐age social wellbeing: Loneliness, social isolation, and connectedness. Journal of Healthcare Engineering, 2020, 2036842. 10.1155/2020/2036842 [DOI] [PMC free article] [PubMed] [Google Scholar]
Jopling 2020
- Jopling, K. (2020). Promising approaches revisited: Effective action on loneliness in later life. Campaign to End Loneliness. Accessed June 14, 2021. Available online: https://www.campaigntoendloneliness.org/wp-content/uploads/Promising_Approaches_Revisited_FULL_REPORT.pdf
Kelly 2017
- KellyMichelle, E. , Duff, H. , Kelly, S. , Power Joanna, E. M. H. , Brennan, S. , Lawlor Brian, A. , & Loughrey David, G. (2017). The impact of social activities, social networks, social support and social relationships on the cognitive functioning of healthy older adults: A systematic review. Systematic Reviews, 6(1), 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Khosravi 2016
- Khosravi, P. , Rezvani, A. , & Wiewiora, A. (2016). The impact of technology on older adults' social isolation. Computers in Human Behavior, 63, 594–603. [Google Scholar]
Leigh‐Hunt 2017
- Leigh‐Hunt, N. , Bagguley, D. , Bash, K. , Turner, V. , Turnbull, S. , Valtorta, N. , & Caan, W. (2017). An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health, 152, 157–171. [DOI] [PubMed] [Google Scholar]
Little 2017
- Little, S. G. , Swangler, J. , & Atkin‐Little, A. (2017). Defining social skills. In Matson, J. (Ed.), Handbook of social behavior and skills in children (pp. 9–17). Autism and Child Psychopathology Series. Springer. 10.1007/978-3-319-64592-6_2 [DOI] [Google Scholar]
Mann 2017
- Mann, F. , Bone Jessica, K. , Lloyd‐Evans, B. , Frerichs, J. , Pinfold, V. , Ma, R. , Wang, J. , & Johnson, S. (2017). A life less lonely: The state of the art in interventions to reduce loneliness in people with mental health problems. Social Psychiatry and Psychiatric Epidemiology, 52(6), 627–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
Masi 2011
- Masi, C. M. , Chen, H.‐Y. , Hawkley Louise, C. , & Cacioppo John, T. (2011). A meta‐analysis of interventions to reduce loneliness. Personality and Social Psychology Review, 15(3), 219–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
Menec 2020
- Menec Verena, H. , Newall Nancy, E. , Mackenzie Corey, S. , Shooshtari, S. , & Nowicki, S. (2020). Examining social isolation and loneliness in combination in relation to social support and psychological distress using Canadian Longitudinal Study of Aging (CLSA) data. PLoS One, 15(3), e0230673. [DOI] [PMC free article] [PubMed] [Google Scholar]
Milstein 1999
- Milstein, B. , & Wetterhall, S. F. (1999). Framework for program evaluation in public health. Series: MMWR. Recommendations and reports: Morbidity and mortality weekly report. Recommendations and Reports, 48(RR–11), 1–58. [PubMed] [Google Scholar]
Moher 2015
- Moher, D. , Shamseer, L. , Clarke, M. , Ghersi, D. , Liberati, A. , Petticrew, M. , Shekelle, P. , & Stewart Lesley, A. (2015). Preferred reporting items for systematic review and meta‐analysis protocols (PRISMA‐P) 2015 statement. Systematic Reviews, 4(1), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
NASEM 2020
- National Academies of Sciences, Engineering, and Medicine (NASEM) . (2020). Social isolation and loneliness in older adults: Opportunities for the health care system. National Academy Press. 10.17226/25663 [DOI] [PubMed] [Google Scholar]
Newall 2019
- Newall Nancy, E. G. , & Menec Verena, H. (2019). Loneliness and social isolation of older adults: Why it is important to examine these social aspects together. Journal of Social and Personal Relationships, 36(3), 925–939. [Google Scholar]
Noone 2020
- Noone, C. , McSharry, J. , Smalle, M. , Burns, A. , Dwan, K. , Devane, D. , et al. (2020). Video calls for reducing social isolation and loneliness in older people: A rapid review. Cochrane Database of Systematic Reviews, 5(5), CD013632. 10.1002/14651858.CD013632 [DOI] [PMC free article] [PubMed] [Google Scholar]
O'Neill 2014
- O'Neill, J. , Tabish, H. , Welch, V. , Petticrew, M. , Pottie, K. , Clarke, M. , Evans, T. , Pardo, J. P. , Waters, E. , White, H. , & Tugwell, P. (2014). Applying an equity lens to interventions: Using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. Journal of Clinical Epidemiology, 67(1), 56–64. [DOI] [PubMed] [Google Scholar]
Perlman 1981
- Perlaman, D. , & Peplau, L. A. (1981). Toward a social psychology of loneliness. Personal Relationships, 3, 31–56. [Google Scholar]
Poscia 2018
- Poscia, A. , Stojanovic, J. , La Milia Daniele, I. , Duplaga, M. , Grysztar, M. , Moscato, U. , Onder, G. , Collamati, A. , Ricciardi, W. , & Magnavita, N. (2018). Interventions targeting loneliness and social isolation among the older people: An update systematic review. Experimental Gerontology, 102, 133–144. [DOI] [PubMed] [Google Scholar]
Proctor 2011
- Proctor, E. , Silmere, H. , Raghavan, R. , Hovmand, P. , Aarons, G. , Bunger, A. , Griffey, R. , & Hensley, M. (2011). Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Administration and Policy in Mental Health and Mental Health Services Research, 38(2), 65–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
Prohaska 2020
- Prohaska, T. , Burholt, V. , Burns, A. , Golden, J. , Hawkley, L. , Lawlor, B. , et al. (2020). Consensus statement: Loneliness in older adults, the 21st century social determinant of health? BMJ Open, 10(8), e034967. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shah 2020
- Shah, S. G. S. , Nogueras, D. , Van Woerden, H. C. , & Kiparoglou, V. (2020). The COVID‐19 pandemic: A pandemic of lockdown loneliness and the role of digital technology. Journal of Medical Internet Research, 22(11), e22287. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shah 2021
- Shah, S. G. S. , Nogueras, D. , van Woerden, H. C. , & Kiparoglou, V. (2021). Evaluation of the effectiveness of digital technology interventions to reduce loneliness in older adults: Systematic review and meta‐analysis. Journal of Medical Internet Research, 23(6), e24712. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shea 2017
- Shea Beverley, J. , Reeves Barnaby, C. , Wells, G. , Thuku, M. , Hamel, C. , Moran, J. , Moher, D. , Tugwell, P. , Welch, V. , & Kristjansson, E. (2017). AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non‐randomised studies of healthcare interventions, or both. BMJ, 358, j4008. 10.1136/bmj.j4008 [DOI] [PMC free article] [PubMed] [Google Scholar]
Snilstveit 2013
- Snilstveit, B. , Vojtkova, M. , Bhavsar, A. , & Gaarder, M. (2013). Evidence gap maps—A tool for promoting evidence‐informed policy and prioritizing future research. The World Bank. [DOI] [PubMed] [Google Scholar]
Snilstveit 2016
- Snilstveit, B. , Vojtkova, M. , Bhavsar, A. , Stevenson, J. , & Gaarder, M. (2016). Evidence & gap maps: A tool for promoting evidence informed policy and strategic research agendas. Journal of Clinical Epidemiology, 79, 120–129. [DOI] [PubMed] [Google Scholar]
ten Bruggencate 2019
- ten Bruggencate, T. , Luijkx, K. G. , & Sturm, J. (2019). How to fulfil social needs of older people: Exploring design opportunities for technological interventions. Gerontechnology, 18(3), 156–167. [Google Scholar]
Thangavel 2022
- Thangavel, G. , Memedi, M. , & Hedström, K. (2022). Customized information and communication technology for reducing social isolation and loneliness among older adults: Scoping review. JMIR Mental Health, 9(3), e34221. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thomas 2020
- Thomas, J. , Graziosi, S. , Brunton, J. , Ghouze, Z. , O'Driscoll, P. , & Bond, M. (2020). EPPI‐Reviewer: Advanced software for systematic reviews, maps and evidence synthesis. Eppi‐Centre Software. UCL Social Research Institute. [Google Scholar]
Tomaka 2006
- Tomaka, J. , Thompson, S. , & Palacios, R. (2006). The relation of social isolation, loneliness, and social support to disease outcomes among the elderly. Journal of aging and health, 18(3), 359–384. [DOI] [PubMed] [Google Scholar]
UCLG 2020
- United Cities and Local Governments (UCLG) . (2020). Live Learning Experience: Beyond the immediate response to the outbreak of COVID‐19. Digital Technologies and the COVID‐19 pandemic. Briefing & Learning Note 15.04, 2020. United Cities and Local Governments (UCLG). [Google Scholar]
Valtorta 2016
- Valtorta Nicole, K. , Kanaan, M. , Gilbody, S. , & Hanratty, B. (2016). Loneliness, social isolation and social relationships: What are we measuring? A novel framework for classifying and comparing tools. BMJ Open, 6(4), e010799. [DOI] [PMC free article] [PubMed] [Google Scholar]
Victor 2005
- Victor Christina, R. , Scambler, S. , Bowling, A. N. N. , & Bond, J. (2005). The prevalence of and risk factors for, loneliness in later life: A survey of older people in Great Britain. Ageing and Society, 25(6), 357–375. [Google Scholar]
Victor 2018
- Victor, C. , Mansfield, L. , Kay, T. , Daykin, N. , Lane, J. , Grigsby Duffy, L. , Tomlinson, A. , & Meads, C. (2018). An overview of reviews: The effectiveness of interventions to address loneliness at all stages of the life‐course. What Works Centre for Wellbeing. [Google Scholar]
Waddington 2014
- Waddington, H. , Snilstveit, B. , Hombrados, J. , Vojtkova, M. , Phillips, D. , Davies, P. , & White, H. (2014). Farmer field schools for improving farming practices and farmer outcomes: A systematic review. Campbell Systematic Reviews, 10(1), i‐335. [Google Scholar]
Watts 2020
- Watts, G. (2020). COVID‐19 and the digital divide in the UK. The Lancet Digital Health, 2(8), e395–e396. [DOI] [PMC free article] [PubMed] [Google Scholar]
Welch 2022
- Welch, V. , Tanjong Ghogomu, E. , Barbeau, V. I. , Boulton, E. , Boutin, S. , Haitas, N. , et al. (2022). PROTOCOL: Digital interventions to reduce social isolation and loneliness in older adults: An evidence and gap map. Campbell Campbell Systematic Reviews, 18(3), e1260. 10.1002/cl2.1260 [DOI] [PMC free article] [PubMed] [Google Scholar]
White 2020
- White, H. , Albers, B. , Gaarder, M. , Kornør, H. , Littell, J. , Marshall, Z. , Matthew, C. , Pigott, T. , Snilstveit, B. , & Waddington, H. (2020). Guidance for producing a Campbell evidence and gap map. Campbell Systematic Reviews, 16(4), e1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 2018
- World Health Organization . (2018). Classification of digital health interventions v1. 0: A shared language to describe the uses of digital technology for health. World Health Organization. [Google Scholar]
WHO 2019
- World Health Organization . (2019). World health statistics 2019: Monitoring health for the SDGs, sustainable development goals. World Health Organization. [Google Scholar]
WHO 2020
- World Health Organization . (2020). Decade of healthy ageing: Baseline report. World Health Organization. [Google Scholar]
WHO 2021
- World Health Organization . (2021). Social isolation and loneliness among older people: Advocacy brief. World Health Organization. [Google Scholar]
Williams 2021
- Williams Christopher, Y. K. , Townson Adam, T. , Kapur, M. , Ferreira Alice, F. , Nunn, R. , Galante, J. , Phillips, V. , Gentry, S. , & Usher‐Smith Juliet, A. (2021). Interventions to reduce social isolation and loneliness during COVID‐19 physical distancing measures: A rapid systematic review. PLoS ONE, 16(2), e0247139. [DOI] [PMC free article] [PubMed] [Google Scholar]
Windle 2012
- Windle, K. , Francis, J. , & Coomber, C. (2012). Preventing loneliness and social isolation: Interventions and outcomes. SCIE Research Briefing 39. Social Care Institute for Excellence. [Google Scholar]
World Bank 2021
- World Bank . (2021). World Bank Country and Lending Groups. Country Classification. World Bank Data Help Desk. [Google Scholar]
Zanella 2020
- Zanella, A. , Mason, F. , Pluchino, P. , Cisotto, G. , Orso, V. , & Gamberini, L. (2020). Internet of things for elderly and fragile people. arXiv preprint arXiv:2006.05709.
Zavaleta 2014
- Zavaleta, D. , Samuel, K. , & Mills, C. (2014). OPHI Working Paper No. 67. Social isolation: A conceptual and measurement proposal. Oxford Poverty & Human Development Initiative, University of Oxford. [Google Scholar]
- Other published versions of this review
- Classification pending references
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Supporting information.


