SECTION 1
A 33-year-old woman was admitted to our hospital for treatment of pancytopenia and rash. Her history was notable for systemic lupus erythematosus as well as antiphospholipid antibody syndrome (APS) manifested by prior deep vein thrombosis, pulmonary embolism, and elevated anticardiolipin antibody (95 G phospholipids), β2 glycoprotein immunoglobulin G (IgG) (81 units/mL), and dilute Russell viper venom time (ratio 1.8). She was treated with enoxaparin 1 mg/kg twice daily for her APS. She also had a history of mild bilateral diffuse throbbing headaches occurring every couple of months beginning in her early 20s. Two weeks prior to admission, while vacationing in the Southeastern United States (without exposure to a forest), she developed chills, fatigue, and throbbing headache radiating to the right side of her face, accompanied by a whooshing sound in her right ear. Several days after headache onset, she presented to an outside hospital, where she reportedly had a normal head CT scan and brain MRI scan, but was noted to be pancytopenic (leukocyte count 0.5 × 103/μL, hemoglobin 7.7 mg/dL, and platelets 9 × 103/μL). She underwent a bone marrow biopsy, the results of which were unremarkable. She was discharged with a prednisone taper for suspected lupus flare. Her headache resolved but 2 days later she developed a new erythematous maculopapular rash involving the palms and soles for which she presented to our emergency room. Her complete blood count on admission was again notable for pancytopenia, with a leukocyte count 0.6 × 103/μL (absolute neutrophil count 900/μL), hemoglobin 8.0 mg/dL, and platelets 13 × 103/μL. Her enoxaparin was held given severe thrombocytopenia. The day after her admission, she developed a progressive return of similar quality right-sided headache again accompanied by a whooshing sound. Her headache was made worse by crying, coughing, and physical exertion. She denied any neurologic deficits and her vital signs were normal.
Questions for consideration:
What is the differential diagnosis for progressive and recurrent headache in a patient with APS and new pancytopenia?
What diagnostic workup is indicated at this point?
SECTION 2
The differential diagnosis for progressive headache in our patient includes the primary headache syndromes, such as migraine and tension-type headaches. However, given her thrombocytopenia, use of enoxaparin, APS, immunodeficient status, and viral-type prodrome and rash, she was at risk of several secondary causes of headache, including intracranial hemorrhage, cerebral venous sinus thrombosis (CVST), sinusitis, aseptic meningitis, and both common and opportunistic CNS infections such as tuberculosis, intracerebral abscess formation, cryptococcus, toxoplasmosis, and neoplastic disease.1
With this differential diagnosis in mind, the ideal initial diagnostic battery for this patient includes an emergent noncontrast head CT to rule out an intraparenchymal hemorrhage, MRI with and without gadolinium to evaluate for mass lesions and meningeal enhancement, magnetic resonance venography (MRV) to rule out CVST, and a lumbar puncture to evaluate for opportunistic infections.1,2
Noncontrast head CT performed the day of the patient’s recurrent headache showed no acute abnormality. The medical team initiated workup of her pancytopenia, rash, and viral-like prodrome. Her negative diagnostic workup included Epstein-Barr virus serologies (IgG-positive but immunoglobulin M [IgM]–negative), parvovirus serologies (IgG-positive but IgM- and PCR-negative), HIV, hepatitis A, B, and C, and serologies for Rocky Mountain spotted fever, Ehrlichia, Anaplasma, and peripheral blood smear for intracellular parasites. With her negative infectious workup and laboratory markers of increased lupus activity (elevated anti-double-stranded DNA of 348 international units/mL, decreased C3 complement at 74 mg/dL, and decreased C4 complement at 12 mg/dL), both her rash and pancytopenia were attributed to a lupus flare.
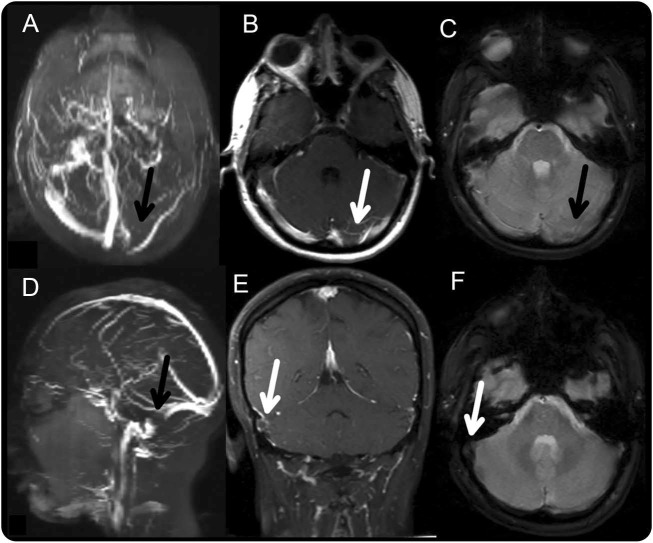
The patient’s headache progressively worsened until the 4th day of admission, when she had 2 episodes of projectile emesis. At that time, an MRI and MRV were performed, demonstrating a thrombosis of the left transverse and sigmoid sinuses and a focal thrombus at the right transverse-sigmoid sinus junction (figure). Upon discovery of her CVST, the neurology service was consulted and she was transferred to the neurologic intensive care unit for treatment and monitoring. The neurologic examination was unremarkable: her neck was supple and direct funduscopic examination revealed normal spontaneous venous pulsations and no evidence of papilledema.
Figure. Cerebral venous sinus thrombosis.
(A) Coronal magnetic resonance venography reconstruction of the patient's cerebral veins, obtained on the fourth day of admission. Absence of flow in the left transverse sinus (black arrow) is shown. (B) Contrast-enhanced T1 MRI demonstrates lack of flow in the left transverse sinus (white arrow). (C) Gradient echo image shows relative decreased susceptibility in the transverse sinus consistent with thrombosis but no hemorrhage. (D) Sagittal magnetic resonance venography reconstruction of the patient's cerebral veins shows absence of flow in the right sigmoid sinus (black arrow). (E) Contrast-enhanced T1 MRI demonstrates absence of contrast filling in the right sigmoid sinus (white arrow). (F) Gradient echo image shows decreased susceptibility in the right sigmoid sinus (white arrow).
Questions for consideration:
What put this patient at risk of CVST?
How did a thrombus form when she was thrombocytopenic and on enoxaparin?
What is the treatment for CVST and how is this complicated by our patient's presentation?
SECTION 3
CVST is an uncommon but serious cause of progressive headache. Headache is sometimes the only presenting sign.2 Interestingly, there is no correlation between the side of the headache and the side of the thrombosis.3 CVST was particularly high on the differential for our patient given her APS and her signs of intracranial hypertension (pulsatile headache worsened with maneuvers that increase intracranial pressure). The most common etiologies of CVST include heritable and acquired thrombophilias, oral contraceptives, pregnancy, malignancy, dehydration, infection, and traumatic head injury.2,4 The most likely etiology in our patient was APS combined with what was likely a lupus flare, exacerbated by the cessation of her enoxaparin on admission due to the severe thrombocytopenia.
It is interesting that our patient developed thrombosis in the setting of severe thrombocytopenia. Cytopenias are common in lupus and pancytopenia in lupus may result from bone marrow failure or macrophage activation syndrome.5 Thrombocytopenia is common in patients with APS, and may be paradoxically associated with an increased risk of thrombosis in patients with APS through an unknown mechanism.6 Furthermore, the fact that our patient's headache began prior to stopping enoxaparin suggests that she may have developed thrombosis in the setting of both thrombocytopenia and therapeutic anticoagulation. The pathogenesis of thrombosis in APS remains poorly understood. One hypothesis involves the antiphospholipid antibody–mediated disruption of annexin-V, an anticoagulant protein that forms a lattice over the surface of phospholipids, blocking their availability for coagulation reactions. When annexin-V is reduced around phospholipids in the cell membranes of vascular endothelial cells, thrombosis may occur.7,8 If this mechanism is independent of the activity of factor Xa and platelets in the coagulation pathway, it may imply a persistent risk of thrombosis in APS despite both anticoagulation and thrombocytopenia.
The acute management of CVST involves controlling elevated intracranial pressure and treating the thrombosis.2 Notably, although CVST occasionally presents with intracranial hemorrhage on head CT, the pathophysiology of these hemorrhages is thought to be related to local increased venous pressure and the presence of hemorrhage in the setting of CVST does not change the recommended treatment of anticoagulation.2 Endovascular therapy may be used when patients clinically or radiographically worsen despite anticoagulant therapy, although there are no published randomized controlled trials evaluating its effectiveness.2 Our patient's thrombocytopenia also put her at increased risk of hemorrhage with anticoagulation. After discussion with hematology, the decision was made to transfuse platelets to above 50 × 103/μL and to start unfractionated heparin; unfractionated heparin was chosen for its quick reversibility in the case of potential intracerebral hemorrhage. Fondaparinux, a synthetic factor Xa inhibitor, has been used for anticoagulation in patients with thrombosis and heparin-induced thrombocytopenia, and may be considered for other patients with concurrent thrombosis and thrombocytopenia.9
Question for consideration:
What is the prognosis for CVST?
SECTION 4
Five percent of patients die in the acute phase of CVST, with the primary cause of death being transtentorial herniation secondary to venous edema and large hemorrhage.10 In the long term, CVST carries a 15% chance of death or dependency. Predictors of poor long-term prognosis include CNS infection, altered mental status, presence of hemorrhage, malignancy, male sex, old age, and thrombosis of the deep venous system.4
After several days of treatment with unfractionated heparin, our patient reported improvement in her headache, and a repeat MRV 1 week later demonstrated decreased thrombus in the left transverse sinus with small persisting thrombus at the left transverse-sigmoid junction. She was transferred out of the neurologic intensive care unit to the wards and continued on a heparin infusion. She had persistent thrombocytopenia for the next several weeks and was treated with methylprednisolone, rituximab, and romiplostim for lupus flare and possible idiopathic thrombocytopenic purpura. She was ultimately discharged on enoxaparin after 1 month once her platelet counts were stably above 50 × 103/μL.
DISCUSSION
We discuss a case of CVST in a woman with APS in the unusual setting of therapeutic anticoagulation and pancytopenia. Her case was particularly challenging given her concurrent hypercoagulable state and thrombocytopenia, which increased her risk of both thrombosis and hemorrhage. CVST is an uncommon but life-threatening and treatable condition that can often be missed, especially when it presents with headache alone, as it did with our patient. The possibility of CVST should be considered in all patients with thrombophilia who present with new headache, whether or not they are managed with therapeutic anticoagulation.
AUTHOR CONTRIBUTIONS
Erin Conrad reviewed the clinical case and wrote the manuscript. James Siegler cowrote the manuscript. Joanna Mattis critically revised the manuscript for intellectual content. Nilan Schnure critically revised the manuscript for intellectual content. Steven Messé critically revised the manuscript for intellectual content.
STUDY FUNDING
No targeted funding reported.
DISCLOSURE
E. Conrad reports no disclosures relevant to the manuscript. J. Siegler is an editorial board member of the Neurology® Resident & Fellow Section and has received financial support from individuals within the private sector, including a representative for Northwestern Mutual, for the production of an educational neurology podcast. J. Mattis and N. Schnure report no disclosures relevant to the manuscript. S. Messé has received compensation from Direct Flow Medical, Inc., for work on the Clinical Event Committee for the SALUS trial; funding from the NIH (U01-DK060990, UM1 HL088957-06, HHSN268200800003C, 1R01HL084375-01A2); and research funding from GlaxoSmithKline, Bayer, and WL Gore & Associates for his work as an investigator in clinical trials. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Ducros A, Bousser MG. Thunderclap headache. BMJ 2013;346:e8557. [DOI] [PubMed] [Google Scholar]
- 2.Saposnik G, Barinagarrementeria F, Brown RD Jr, et al. Diagnosis and management of cerebral venous thrombosis: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011;42:1158–1192. [DOI] [PubMed] [Google Scholar]
- 3.Wasay M, Mohammad W, Suleman K, Dai AI, George B, Zubair S. Headache in cerebral venous thrombosis: incidence, pattern and location in 200 consecutive patients. J Headache Pain 2010;11:137–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ferro JM. Prognosis of cerebral vein and dural sinus thrombosis: results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke 2004;35:664–670. [DOI] [PubMed] [Google Scholar]
- 5.Bashal F. Hematological disorders in patients with systemic lupus erythematosus. Open Rheumatol J 2013;7:87–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Artim-Esen B, Diz-Kucukkaya R, Inanc M. The significance and management of thrombocytopenia in antiphospholipid syndrome. Curr Rheumatol Rep 2015;17:14. [DOI] [PubMed] [Google Scholar]
- 7.Rand JH, Wu XX, Quinn AS, Taatjes DJ. Resistance to annexin A5 anticoagulant activity: a thrombogenic mechanism for the antiphospholipid syndrome. Lupus 2008;17:922–930. [DOI] [PubMed] [Google Scholar]
- 8.Rand JH. Molecular pathogenesis of the antiphospholipid syndrome. Circ Res 2002;90:29–37. [DOI] [PubMed] [Google Scholar]
- 9.Lobo B, Finch C, Howard A, Minhas S. Fondaparinux for the treatment of patients with acute heparin-induced thrombocytopenia. Thromb Haemost 2008;99:208–214. [DOI] [PubMed] [Google Scholar]
- 10.Canhão P, Ferro JM, Lindgren AG, et al. Causes and predictors of death in cerebral venous thrombosis. Stroke 2005;36:1720–1725. [DOI] [PubMed] [Google Scholar]