Abstract
Objective
To compare access to caregiving between men and women with Parkinson disease (PD).
Methods
This was a cross-sectional and longitudinal study among participants with PD enrolled in the National Parkinson Foundation Parkinson's Outcomes Project from 2009 to 2014 at 21 international sites. The primary outcome measures were presence of a caregiver at the baseline visit, caregiver burden as measured by the Multidimensional Caregiver Strain Index (MCSI) at baseline, and time to first paid caregiver.
Results
A total of 7,209 participants (63% men, 37% women) with PD were evaluated. Men had a mean age of 66.0 (SD 9.8) years, and women had a mean age of 66.9 (SD 9.7) years. More men than women had a caregiver (88.4% vs 79.4%, p < 0.0001). Caregivers of men reported greater strain than those of women (MCSI score 19.9 vs 16.4, p < 0.0001). These differences persisted after controlling for age, disease stage, number of comorbidities, cognitive and mobility measures, and health-related quality of life. In addition, the odds of caregiver accompaniment at baseline visit were lower for women compared to men (odds ratio 0.76, 95% confidence interval [CI] 0.67–0.86), and women had a faster rate to using a paid caregiver than men (hazard ratio 1.76, 95% CI 1.35–2.28) after controlling for potential confounders.
Conclusions
Informal caregiving resources are lower for women than men with PD, despite the finding that their caregivers report less strain than those of men. In addition, women are more likely to use formal, paid caregivers. Strategies to improve access to caregiving, particularly for women, are needed.
Parkinson disease (PD) impairs movement, cognition, and psychiatric function, directly and indirectly affecting the ability to perform activities of daily living, to participate in social activities, to access medical care, and to adhere to treatment regimens. With disease progression, formal (paid) and informal (unpaid) caregivers help provide necessary physical, psychosocial, and cognitive support to patients with PD. However, provision of this type of care is extremely costly. A 20-year-old, small study based in North Carolina showed that caregivers provided an average of 22 hours per care a week for people with PD, and when monetized, this was the second largest source of economic burden on a family after income loss.1 Unfortunately, while caregiving is an integral and valuable part of PD treatment,2 there has been little study of caregiving patterns and needs in PD.
There is evidence that women may be at higher risk of not receiving this care. In a landmark national study from 2000, Katz and colleagues3 showed that disabled women from any condition receive about one-third fewer hours of caregiving than similarly disabled men. In addition, women are more likely to perceive that caregivers might be unavailable if they were to need one.4
Lack of access to caregiving has enormous potential implications in PD. Prior studies in other conditions such as dementia and schizophrenia show that the presence of an informal caregiver improves health outcomes, including improving treatment adherence and quality of health care and delaying time to institutionalization.5–8 On the other hand, providing care for a person with PD can also lead to increased feelings of burden and strain for the caregiver, and there is some evidence that this strain may be higher among female caregivers of men with PD.9,10
Therefore, we sought to study patterns of caregiving among patients with PD and to test whether patient sex is associated with specific outcomes, including caregiver accompaniment to visits, paid caregiving, and caregiver strain, in a large, observational, international cohort of participants with PD and their caregivers seen at National Parkinson Foundation (NPF) Centers of Excellence.
Methods
Standard protocol approvals, registrations, and patient consents
Approval from the Institutional Review Board at each site was obtained before the start of participant recruitment. We obtained written informed consent from all participants (patients and caregivers).
Study design and sample
We conducted a cross-sectional and longitudinal study using patients drawn from an ongoing, prospective, observational study of PD. The NPF Parkinson's Outcomes Project (NPF-POP) annually assesses health outcomes among participants with PD and their caregivers. The study is conducted at 21 NPF Centers of Excellence located in Canada, Netherlands, Israel, and the United States.11 Participant enrollment began in 2009, and new participants continue to be enrolled every year. For this analysis, participants were followed up until 2014. Only participants who were living at home at baseline and had a physician diagnosis of idiopathic PD and at least 1 follow-up visit after the baseline visit were included in the analysis. The study is designed as a brief additional assessment that is administered before, during, or after the participant's regularly scheduled clinical visit.
Measures
The NPF-POP collects annual patient and caregiver data from study participants. Patient data include demographics, medications, disease duration, Hoehn & Yahr (H & Y) stage, 5-word recall and verbal fluency,12,13 Timed Up and Go (TUG), and Parkinson's Disease Questionnaire-39 (PDQ-39), a disease-specific health-related quality of life scale in which higher scores indicate worse quality of life.14 The TUG scores were standardized to z scores for analysis. From the caregiver, we collect presence at visit, type of caregiver (response options: none, spouse/partner, other relative, paid caregiver, other), and Multidimensional Caregiver Strain Index (MCSI), which is an 18-item questionnaire. Participants respond on a 5-point Likert scale about their feelings regarding the physical, social, interpersonal, and financial strain, time constraints, and elder demanding/manipulative behavior that may arise with caregiving. Higher scores indicate greater strain.15
Analysis
Descriptive statistics were used to characterize the sample. Next, we used t tests for continuous variables and χ2 tests for categorical variables to compare demographic, clinical, and caregiving characteristics by patient sex at baseline. We compared the 2 sex groups on time to first paid caregiver using a Kaplan-Meier survival curve. Then, we used backward selection with a p value cutoff of 0.10 for inclusion of covariates to run the following regression models: logistic regression of caregiver presence at baseline, linear regression of caregiver burden (MCSI) at baseline, and Cox regression of time to first paid caregiver. As a secondary analysis, we ran a final linear regression model with patient-reported health-related quality of life (PDQ-39) at baseline as the dependent variable.
Results
Patient characteristics
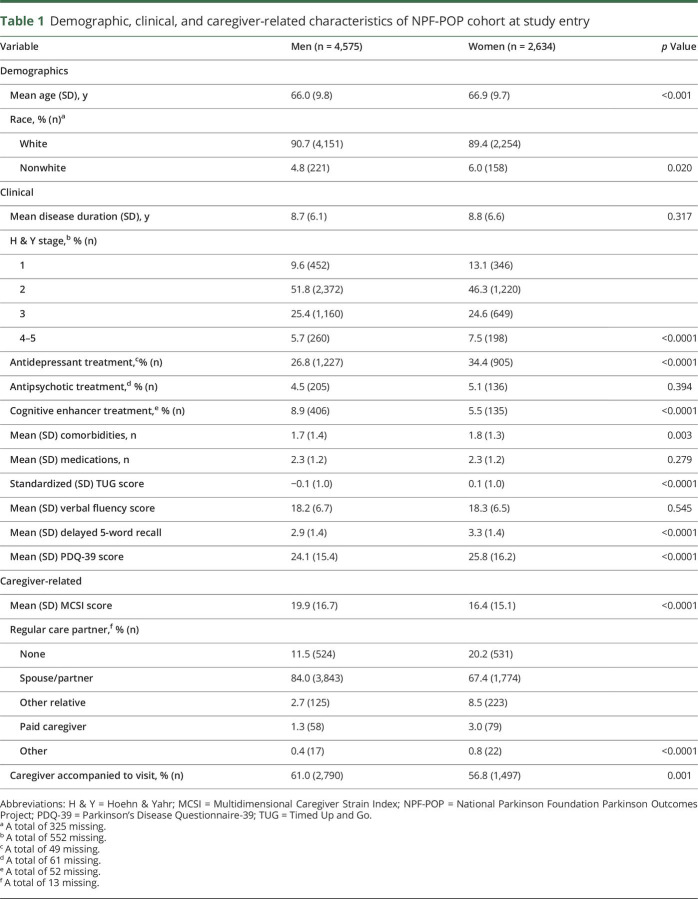
A total of 7,209 participants (63% men and 37% women) provided baseline data to the NPF-POP. Figure 1 shows the flow of study participants over 5 years of rolling enrollment and longitudinal data collection. Table 1 shows the baseline demographic and clinical characteristics of the cohort by sex. On average, women were slightly older than men (66.9 [SD 9.7] vs 66.0 [SD 9.8] years). There were sex differences in the distribution of disease stage wherein greater proportions of women with PD were in the earliest stages (H & Y stage 1) and latest stages (H & Y stage 4–5). The majority of participants were white, consistent with known racial differences in PD diagnosis16 and racial disparities in the use of specialty care for PD.17 Years (mean) of disease duration (men 8.7 [SD 6.1], women 8.8 [SD 6.6]; t test, p = 0.317) and total number of prescription medications (men 2.3 [SD 1.2], women 2.3 [SD 1.2]; t test, p = 0.279) did not differ by sex. Antidepressants were the second most common prescription drug class (after anti-Parkinson medications) reported by study participants; women were more frequently prescribed antidepressant medications (34.4% vs 26.8% in men; χ2, p < 0.0001). Only 7.5% of participants (n = 541) reported taking cognitive enhancer or antidementia drugs at baseline, but men were the majority of users (75.0%, n = 406). Men and women had similar use of antipsychotic medications (men 4.5%, women 5.1%; χ2, p = 0.394). Women performed worse at baseline on the mobility measure (TUG) and health-related quality of life (PDQ-39) than men. However, in secondary analysis, patient sex was no longer associated with health-related quality of life after controlling for age, disease duration, number of comorbidities, and PD-related mobility and cognitive measures. While there were no significant sex differences in verbal fluency, women performed better on delayed recall than men.
Figure 1. Flow of study participants in NPF-POP.
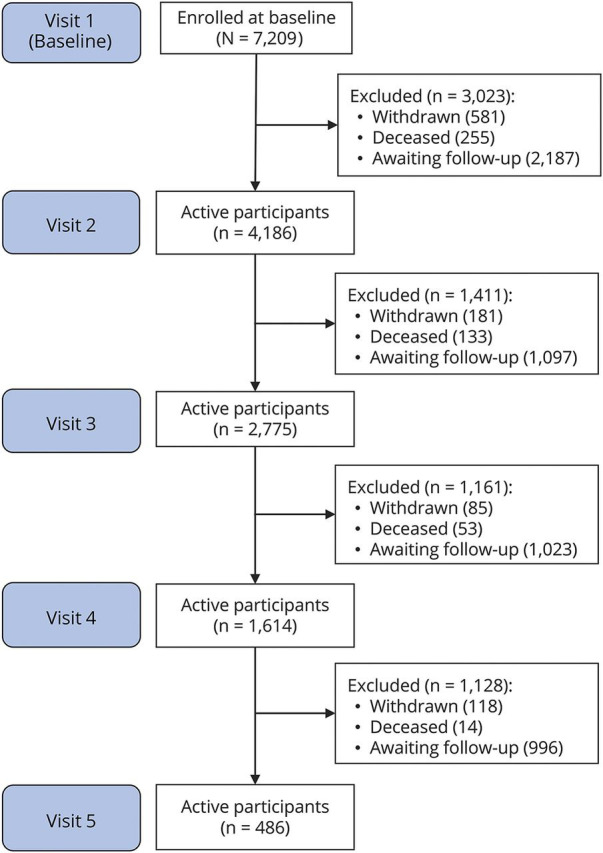
NPF-POP = National Parkinson Foundation Parkinson Outcomes Project.
Table 1.
Demographic, clinical, and caregiver-related characteristics of NPF-POP cohort at study entry
Caregiver characteristics
On study entry, men more frequently reported having a regular caregiver (88.4% vs 79.4%; χ2, p < 0.0001) and more frequently had their caregiver accompany them at their visit (61.0% vs 56.8%; χ2, p = 0.001). A little over 20% of women reported having no care partner at all (table 1). The spouse was identified as the primary caregiver for 84.0% of men compared to only 67.4% of women (χ2, p < 0.0001). Women were twice as likely as men to have a paid caregiver (women 3.0% vs men 1.3%). Caregivers of women reported lower strain than those of men (mean MCSI score: women 16.4 [SD 15.1] vs men 19.9 [SD 16.7]; t test, p < 0.0001).
Cross-sectional analyses
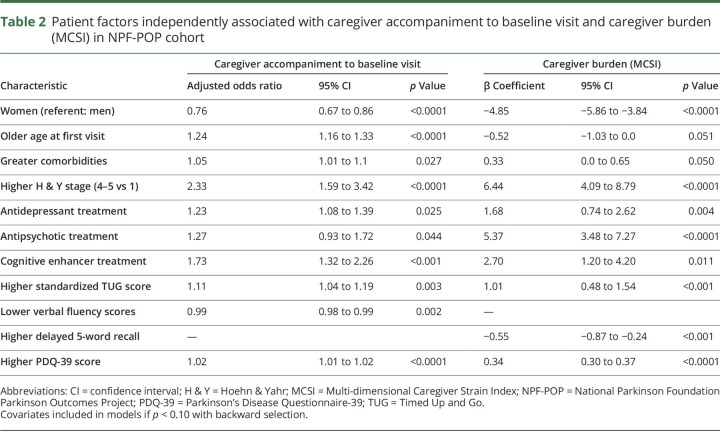
Compared to men, women had a lower odds of having a caregiver accompany them at the baseline visit (odds ratio 0.76, 95% confidence interval 0.67–0.86) after adjustment for differences in demographic and clinical variables with the backward selection method (p < 0.10) for inclusion of covariates in the model. Factors independently associated with greater caregiver burden included greater comorbidity burden, higher disease stage, worse TUG score, and worse quality of life. As shown in table 2, caregivers of women and patients with higher delayed recall scores also reported lower caregiver burden.
Table 2.
Patient factors independently associated with caregiver accompaniment to baseline visit and caregiver burden (MCSI) in NPF-POP cohort
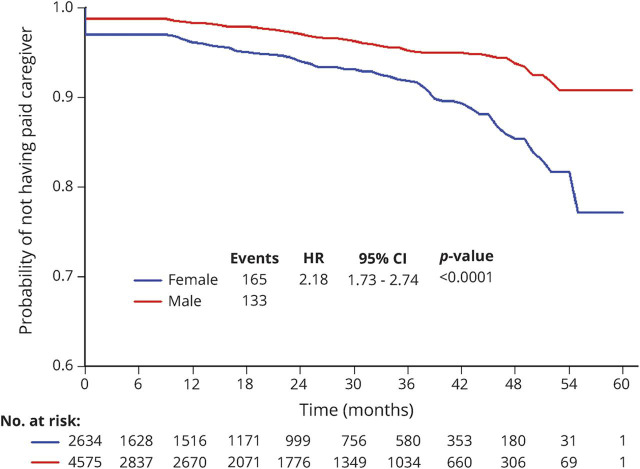
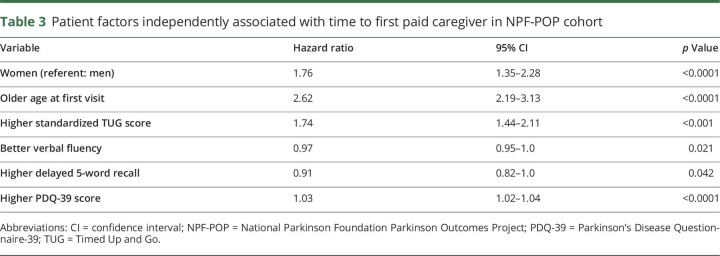
Time to first paid caregiver
Finally, a longitudinal analysis was applied to determine which patient factors were associated with time to first paid caregiver. Survival analysis of time to first paid caregiver demonstrated that, over 60 months, men were less likely than women to have a paid caregiver (figure 2). After adjustment for potential demographic and clinical confounders, women still progressed at a faster rate to having a paid caregiver (hazard ratio 1.76, 95% confidence interval 1.35–2.28, p < 0.0001) (table 3).
Figure 2. Time to first paid caregiver by patient sex.
CI = confidence interval; HR = hazard ratio.
Table 3.
Patient factors independently associated with time to first paid caregiver in NPF-POP cohort
Discussion
In this large, international cohort study of patients seen at NPF Centers of Excellence, women with PD have fewer informal caregiving resources and are more likely to use formal, paid caregivers than men. These differences in receipt of caregiving differ by patient sex even after adjustment for potential clinical characteristic differences. Furthermore, caregivers of men with PD report greater strain than those of women.
Prior studies show that sex differences in the epidemiology of PD exist. Both incidence and prevalence of PD are 1.5 to 2 times higher in men than women, but women are diagnosed at later stages with PD.18,19 Furthermore, there is conflicting evidence of whether the clinical phenotype differs between men and women. Large multicenter studies suggest that women may perform better on tests of cognitive function than men.20,21 Single-center studies report a range of sex differences, including more frequent levodopa-induced dyskinesias and a different distribution of nonmotor symptoms among women compared to men.19,22–25 However, even after adjustment for small but statistically significant clinical differences present in this cohort, there are notable differences in receipt of caregiving between men and women with PD.
There are several potential reasons for these observed sex difference in caregiving receipt. Unfortunately, we did not collect data on the sex of the caregiver. However, women have shouldered the overwhelming burden of caregiving duties throughout history.26 While the demographics of caregiving may be changing, even data collected as recently as 2015 by the National Caregiver Alliance and the American Association of Retired People across all patient health conditions show that women are more likely to be caregivers than men.27 Because the largest proportion of caregiver type in this cohort was the spouse/partner, a married woman with PD might be less likely to receive care from a male spouse. This idea is supported by the finding that married women with disability receive fewer hours of informal caregiving than married men with disability.3 Same-sex couples encounter additional unique challenges in their caregiving experience.28 In addition, women have a longer life expectancy and are more likely to be living alone than men.29,30 Taken together, these findings indicate that it is possible that women with PD are more likely to have outlived their male spouse/partner than men with PD, which would necessitate other options for caregiving. Lastly, men represent a larger proportion of the paid labor force compared to women (65.7% of men 55–64 years and 18.4% of men >65 years of age compared to 50.8% of women 55–64 years and 9.7% of women >65 years of age).30 Again, this may result in women being accompanied less often to a visit by a male spouse because he may be less able to take time off from a paid position during physician office hours because of job restrictions and loss of wages.
Although caregivers of men with PD reported significantly higher burden, this did not translate to faster time to paid caregiving. Indeed, women with PD had a faster time to using a paid caregiver. Several prior studies have shown higher caregiving burden among female caregivers compared to men in cancer, palliative care, and dementia populations, in addition to PD.31–35 Potential explanations for these differences are different coping styles, levels of support from friends/family, and feelings of hope between female and male caregivers.31,32 In PD, 1 study suggested that low mutuality (quality of the relationship) between female spouse caregivers and male patients contributed to greater strain over time.35 Caregiver strain is especially important to screen for and to address because it is linked to worse health outcomes, including higher rates of depression and morbidity.36–38
Paid caregiving, although expensive, can alleviate burden on an informal caregiver or may be a necessity if there are no family members or friends available to provide care. One study empirically demonstrated that having a paid caregiver provide some support improved the well-being of the informal caregiver.39 Overall, a relatively small proportion of patients with PD in this cohort used formal caregiving, particularly compared to formal caregiving use in other countries. For example, in Portugal and Austria, ≈14% and 12% of participants paid for formal caregiving.40 Quantifying the number of hours of care provided and the out-of-pocket costs for paid caregiving is an important next step to help health policy makers develop long-term care programs for people with PD.
There were several limitations to this analysis. NPF-POP does not contain detailed caregiver data such as sex, family characteristics, years of education, caregiver changes over time, or caregiver comorbidities to begin to analyze underlying causes of sex differences in caregiving receipt. In addition, patients with PD may be caregivers themselves, which likely influences their own receipt of caregiving; however, this information was not obtained. All participants were seen at specialty PD centers, which primarily care for individuals of higher socioeconomic status; this will limit the generalizability of these findings. Lastly, 3.1% to 8.3% of participants withdrew from the NPF-POP every year. It is possible that these participants had different caregiving characteristics that led to the inability to continue to be seen for follow-up at the center or to participate in the study, which would bias the results. Overall, a retention rate >90% is excellent for a longitudinal observational study of older adults with a disabling condition.
Because caregivers are an important part of the treatment team for a patient with PD, it is imperative that caregivers are provided early and adequate support to prevent the development of burden and to be successful. We present new data on sex differences in access to caregiving for PD. Future studies to understand the underlying mechanisms of the observed sex disparities in receipt of caregiving are underway with the goal of developing tailored interventions to support caregivers and, in particular, to design innovative programs to improve outcomes for women with PD. However, it is important to note that sex disparities in caregiving access are systemic and long-standing and cross multiple conditions.3 Changes in health policy to better support older women with disability are urgently needed.
Glossary
- H & Y
Hoehn & Yahr
- MCSI
Multidimensional Caregiver Strain Index
- NPF
National Parkinson Foundation
- PD
Parkinson disease
- PDQ-39
Parkinson's Disease Questionnaire-39
- POP
Parkinson's Outcomes Project
- TUG
Timed Up and Go
Author contributions
Nabila Dahodwala: study concept and design, draft of the manuscript, analysis and interpretation of data. Krunal Shah: acquisition of data, critical revision of manuscript for intellectual content. Ying He and Samuel S. Wu: analysis and interpretation of data, critical revision of manuscript for intellectual content. Peter Schmidt: study concept and design, acquisition of data, analysis and interpretation of data, study supervision. Fernando Cubillos: acquisition of data, study supervision. Allison W. Willis: critical revision of manuscript for intellectual content.
Study funding
This study was funded by the NPF.
Disclosure
N. Dahodwala received research support from the NIH, the NPF, the Parkinson Council, Biotie, and Abbvie. K. Shah, Y. He, and S. Wu report no disclosures relevant to the manuscript. P. Schmidt and F. Cubillos are employed by the NPF. A. Willis received research support from the NIH (K23NS081087), the Patient Centered Outcomes Research Institute, the St. Louis Chapter of the American Parkinson Disease Association, the University of Pennsylvania, Walter and Connie Donius, and The Robert Renschen Fund. Go to Neurology.org/N for full disclosures.
References
- 1.Whetten-Goldstein K, Sloan F, Kulas E, Cutson T, Schenkman M. The burden of Parkinson's disease on society, family, and the individual. J Am Geriatr Soc 1997;45:844–849. [DOI] [PubMed] [Google Scholar]
- 2.Hassan A, Wu SS, Schmidt P, et al. What are the issues facing Parkinson's disease patients at ten years of disease and beyond? Data from the NPF-QII study. Parkinsonism Relat Disord 2012;18(suppl 3):S10–S14. [DOI] [PubMed] [Google Scholar]
- 3.Katz SJ, Kabeto M, Langa KM. Gender disparities in the receipt of home care for elderly people with disability in the United States. JAMA 2000;284:3022–3027. [DOI] [PubMed] [Google Scholar]
- 4.Roth DL, Haley WE, Wadley VG, Clay OJ, Howard G. Race and gender differences in perceived caregiver availability for community-dwelling middle-aged and older adults. Gerontologist 2007;47:721–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DiMatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol 2004;23:207. [DOI] [PubMed] [Google Scholar]
- 6.Vickrey BG, Mittman BS, Connor KI, et al. The effect of disease management intervention on quality and outcomes of dementia care. Ann Intern Med 2006;145:713–726. [DOI] [PubMed] [Google Scholar]
- 7.Wolff JL. Family matters in health care delivery. JAMA 2012;308:1529–1530. [DOI] [PubMed] [Google Scholar]
- 8.Severson MA, Smith GE, Tangalos EG, et al. Patterns and predictors of institutionalization in community-based dementia patients. J Am Geriatr Soc 1994;42:181–185. [DOI] [PubMed] [Google Scholar]
- 9.Schrag A, Hovris A, Morley D, Quinn N, Jahanshahi M. Caregiver-burden in Parkinson's disease is closely associated with psychiatric symptoms, falls, and disability. Parkinsonism Relat Disord 2006;12:35–41. [DOI] [PubMed] [Google Scholar]
- 10.Oguh O, Kwasny M, Carter J, Stell B, Simuni T. Caregiver strain in Parkinson's disease: National Parkinson Foundation Quality Initiative Study. Parkinsonism Relat Disord 2013;19:975–979. [DOI] [PubMed] [Google Scholar]
- 11.Okun MS, Siderowf A, Nutt JG, et al. Piloting the NPF data-driven quality improvement initiative. Parkinsonism Relat Disord 2010;16:517–521. [DOI] [PubMed] [Google Scholar]
- 12.Chou KL, Amick MM, Brandt J, et al. A recommended scale for cognitive screening in clinical trials of Parkinson's disease. Mov Disord 2010;25:2501–2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nasreddine ZS, Phillips NA, Bedirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 2005;53:695–699. [DOI] [PubMed] [Google Scholar]
- 14.Peto V, Jenkinson C, Fitzpatrick R. PDQ-39: a review of the development, validation and application of a Parkinson's disease quality of life questionnaire and its associated measures. J Neurol 1998;245(suppl 1):S10–S14. [DOI] [PubMed] [Google Scholar]
- 15.Stull DE. The Multidimensional Caregiver Strain Index (MCSI): its measurement and structure. J Clin Geropsychol 1996;2:175–196. [Google Scholar]
- 16.Van Den Eaden SK, Tanner CM, Bernstein AL, et al. Incidence of Parkinson's disease: variation by age, gender, and race/ethnicity. Am J Epidemiol 2003;157:1015–1022. [DOI] [PubMed] [Google Scholar]
- 17.Willis AW, Schootman M, Evanoff BA, Perlmutter JS, Racette BA. Neurologist care in Parkinson disease: a utilization, outcomes, and survival study. Neurology 2011;77:851–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wooten GF, Currie LJ, Bovbjerg VE, Lee JK, Patrie J. Are men at greater risk for Parkinson's disease than women? J Neurol Neurosurg Psychiatry 2004;75:637–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Haaxma CA, Bloem BR, Borm GF, et al. Gender differences in Parkinson's disease. J Neurol Neurosurg Psychiatry 2007;78:819–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Augustine EF, Perez A, Dhall R, et al. Sex differences in clinical features of early, treated Parkinson's disease. PLoS One 2015;10:e0133002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dahodwala N, Pei Q, Schmidt P. Sex differences in the clinical progression of Parkinson's disease. J Obstet Gynecol Neonatal Nurs 2016;45:749–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baba Y, Putzke JD, Whaley NR, Wszolek ZK, Uitti RJ. Gender and the Parkinson's disease phenotype. J Neurol 2005;252:1201–1205. [DOI] [PubMed] [Google Scholar]
- 23.Lyons KE, Hubble JP, Troster AI, Pahwa R, Koller WC. Gender differences in Parkinson's disease. Clin Neuropharmacol 1998;21:118–121. [PubMed] [Google Scholar]
- 24.Picillo M, Amboni M, Erro R, et al. Gender differences in non-motor symptoms in early, drug naive Parkinson's disease. J Neurol 2013;260:2849–2855. [DOI] [PubMed] [Google Scholar]
- 25.Solla P, Cannas A, Ibba FC, et al. Gender differences in motor and non-motor symptoms among Sardinian patients with Parkinson's disease. J Neurol Sci 2012;323:33–39. [DOI] [PubMed] [Google Scholar]
- 26.Sommers T, Shields L, MacLean J. Women Take Care: The Consequences of Caregiving in Today's Society. Gainesville: Triad Publishing Co; 1987. [Google Scholar]
- 27.NAC and AARP Public Policy Institute. Caregiving in the US [online]. Available at: caregiving.org/wp-content/uploads/2015/05/2015_CaregivingintheUS_Final-Report-June-4_WEB.pdf. Accessed February 21, 2017.
- 28.Hash K. Caregiving and post-caregiving experiences of midlife and older gay men and lesbians. J Gerontol Soc Work 2006;47:121–138. [DOI] [PubMed] [Google Scholar]
- 29.Barford A, Dorling D, Davey Smith G, Shaw M. Life expectancy: women now on top everywhere. BMJ 2006;332:808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.We the people: women and men in the United States [online]. Available at: census.gov/prod/2005pubs/censr-20.pdf. Accessed July 16, 2015.
- 31.Schrank B, Ebert-Vogel A, Amering M, et al. Gender differences in caregiver burden and its determinants in family members of terminally ill cancer patients. Psycho Oncol 2016;25:808–814. [DOI] [PubMed] [Google Scholar]
- 32.Brazil K, Thabane L, Foster G, Bedard M. Gender differences among Canadian spousal caregivers at the end of life. Health Soc Care Commun 2009;17:159–166. [DOI] [PubMed] [Google Scholar]
- 33.Barusch AS, Spaid WM. Gender differences in caregiving: why do wives report greater burden? Gerontologist 1989;29:667–676. [DOI] [PubMed] [Google Scholar]
- 34.Gibbons C, Creese J, Tran M, et al. The psychological and health consequences of caring for a spouse with dementia: a critical comparison of husbands and wives. J Women Aging 2014;26:3–21. [DOI] [PubMed] [Google Scholar]
- 35.Lyons KS, Stewart BJ, Archbold PG, Carter JH. Optimism, pessimism, mutuality, and gender: predicting 10-year role strain in Parkinson's disease spouses. Gerontologist 2009;49:378–387. [DOI] [PubMed] [Google Scholar]
- 36.Aarsland D, Larsen JP, Karlsen K, Lim NG, Tandberg E. Mental symptoms in Parkinson's disease are important contributors to caregiver distress. Int J Geriatr Psychiatry 1999;14:866–874. [PubMed] [Google Scholar]
- 37.Dura JR, Haywood-Niler E, Kiecolt-Glaser JK. Spousal caregivers of persons with Alzheimer's and Parkinson's disease dementia: a preliminary comparison. Gerontologist 1990;30:332–336. [DOI] [PubMed] [Google Scholar]
- 38.Schulz R, Beach SR. Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. JAMA 1999;282:2215–2219. [DOI] [PubMed] [Google Scholar]
- 39.Verbakel E, Metzelthin SF, Kempen GI. Caregiving to older adults: determinants of informal caregivers' subjective well-being and formal and informal support as alleviating conditions. J Gerontol Ser B Psychol Sci Soc Sci 2016:gbw047. [DOI] [PubMed] [Google Scholar]
- 40.von Campenhausen S, Winter Y, Rodrigues e Silva A, et al. Costs of illness and care in Parkinson's disease: an evaluation in six countries. Eur Neuropsychopharmacol 2011;21:180–191. [DOI] [PubMed] [Google Scholar]