Abstract
Purpose:
The present study aims to investigate the combined effect of slow breathing exercise (SBE) and progressive muscle relaxation (PMR) technique on blood pressure (BP), heart rate (HR), respiratory rate (RR), and anxiety in patients diagnosed with essential hypertension.
Trial design:
This study was based on a 4-arm parallel-group, randomized control design.
Methods:
Sixty-four participants diagnosed with essential hypertension were randomly allocated into SBE, PMR, SBE-PMR, and Control groups, with 16 subjects each. All 3 groups received different treatments according to their name; however, the Control group received no treatment. Systolic and diastolic BP (SBP and DBP), HR, RR, and anxiety were all evaluated as the study outcomes using a digital sphygmomanometer and perceived stress scale (PSS) at baseline (pretest), 2nd week and 4th weeks post-intervention. A repeated measure analysis of variance test assessed intra-group comparison (overall) analyses across multiple time points. Bonferroni multiple comparison tests were used to analyze the mean differences between the groups. The confidence interval was kept at 95% for all the statistical analyses, that is, P < .05 is considered significant.
Results:
There was a significant change in the HR (F = 239.04, P = .0001), RR (F = 167.74, P = .0001), SBP (F = 266.64, P = .0001), DSP (F = 279.80, P = .0001), and PSS (F = 473.42, P = .0001) as an outcome of baseline measurements versus (vs) the following weeks. There were significant (F = 48.57, P = .001) differences among different training on HR. The SBE vs SBE-PMR showed an insignificant difference (F = 48.54, P = 1.000). The RR showed significant differences (F = 32.05, 0.0001) between the SBE vs PMR, SBE vs Control, PMR vs Control, and SBE-PMR vs Control groups and insignificant differences for the SBE vs SBE-PMR and PMR vs SBE-PMR groups. The SBE vs SBE-PMR groups showed insignificant differences for DPP and SBP. However, PSS showed significant differences (F = 67.12, P = .0001) among the intervention groups except for the PMR and SBE-PMR groups.
Conclusions:
The combined interventions of SBEs and progressive muscle relaxation techniques can effectively reduce the heart rate, respiratory rate, BP, and anxiety in essential hypertensive patients compared to both techniques when given alone.
Keywords: anxiety, blood pressure, heart rate, progressive muscle relaxation, respiratory rate, slow breathing exercise
1. Introduction
Primary hypertension, also called essential hypertension, is a rise in blood pressure (BP) with no identifiable cause.[1] The most prevalent form of hypertension is essential hypertension, which involves 95% of patients with hypertension.[2] People with relatively high BP at early ages are at a higher risk of developing essential hypertension later in life. The prevalence of essential hypertension increases with age. Hypertension stresses various organs, including the kidneys, eyes, and heart, leading them to deteriorate their functions over time.[3] Other risk factors such as smoking, high cholesterol level, family history, obesity, diabetes, coronary artery disease, and other signs of cardiovascular diseases increase the likelihood of complications or rapid progression of hypertension.[3]
Recently, non-pharmaceutical methods of controlling hypertension have grown progressively, with relaxation techniques being the most popular. Relaxation techniques can regulate the hypothalamus response to the parasympathetic nerves, decreasing the heart rate, BP, and respiratory rate and reducing oxygen consumption and muscle tension.[4] Relaxation techniques can diminish the activity of the skeletomuscular neural input and output, which in turn reduces neural reflex function.[5] Several techniques commonly used in relaxation include progressive muscle relaxation (PMR), diaphragmatic breathing exercises, slow breathing exercise (SBE), autogenic training, relaxation response, biofeedback, guided imagery, cognitive behavioral therapy, and transcendental meditation. All these techniques are easy to learn and show good results in patients and healthy subjects.
The progressive muscle relaxation (PMR) technique is learning to relax some groups of muscles while paying attention to the feelings connected with both the tense and relaxed states.[6] It has been proposed that PMR lowers the heart rate,[7] Systolic, and diastolic BP,[8] respiratory rate.[7] and anxiety by reducing neural reflex function, which decreases musculoskeletal neural input and output activity, thus reducing the stress level in hypertensive people. PMR has been used in numerous empirical studies with positive physiological effects in many populations. Many studies have shown that PMR benefits patients with essential hypertension. It can reduce systolic BP,[8,9] the requirement of hypertension medication,[10] adrenaline concentration, and oxygen consumption.[11] PMR reduces stress-related symptoms in the adult population,[12] helps in decreasing anxiety[12] and depression[13] in young adults and reduces anxiety in essential hypertensive patients.[14]
It is generally established that regular slow (deep) breathing exercises enhance respiratory and cardiovascular function by enhancing parasympathetic tone and reducing sympathetic activity, thus reducing BP, heart rate, respiratory rate, and stress levels in hypertensive patients. Although the precise mechanisms are unknown, the autonomic nervous system may play a role in the reduction in BP and pulse rate associated with slow breathing by stimulating arterial baroreceptors, pulmonary stretch receptors, and low-pressure baroreceptors.[15]
Variations in vagal-cardiac activity largely drive changes in heart rate during slow breathing.[16] Slow breathing can increase baroreflex activity in healthy people and patients with congestive heart failure. Slow breathing decreases BP due to a proportional change in vagal activity, sympathetic activity decrease, and afterload reduction.[17] The increase in tidal volume, which compensates for the decreased respiratory rate to maintain minute ventilation, may be responsible for these autonomic changes via a drop-in sympathetic activity or the Hering-Breuer reflex.[18] A similar result was obtained in a clinical trial that used a device-guided breathing exercise, suggesting the involvement of increased sympathetic activity, reduced baroreflex function, and arterial wall compliance.[19]
SBE (about 6 breaths per minute) has many positive effects on the cardiopulmonary system in congestive heart failure patients, including improving ventilation/perfusion mismatch and increasing exercise tolerance by lowering the sensation of dyspnea.[20,21] Moreover, it lowers chemo reflex activation[22] and muscle nerve sympathetic activity.[23] The decrease in BP due to slower and deeper breathing may be due to a reduced afterload, secondary to reduced sympathetic activity.[24] Other studies demonstrated that SBE might influence autonomic functions reducing BP in essential hypertension patients.[18] It is also reported that procedures involving the Control of breathing can positively affect type 2 Diabetes,[25] depression,[26] pain,[27] glucose,[25] and cholesterol levels.[28] The patient's slow breathing pattern is well-tolerated; carbon dioxide is kept within resting standards, and this breathing rate does not stimulate the chemoreflex activity. As it does not induce ventilation, which may be harmful in persons with a tendency to hyperventilate, this pattern can be maintained as spontaneous and trained through the right training.
From the previously published literature, it is obvious that both the SBE and PMR are effective in patients with essential hypertension. However, no studies are available on the combined effect of these 2 techniques. So, the study aims to investigate the combined effect of SBE and PMR techniques on BP, heart rate, respiratory rate, and anxiety in patients diagnosed with essential hypertension.
2. Methods
2.1. Study design
The study was based on a 4-arm parallel-group, repeated measures, randomized controlled trial design to meet the objectives of the study.
2.2. Study setting
The consultant doctor diagnosed the participants with essential hypertension and advised getting cardiopulmonary physiotherapy. The banners were hung in-and-outside the hospital premises to make people aware of the participants. Pamphlets were kept and distributed at the hospital and physiotherapy department outpatient (O.P.D.) reception counter. The study was carried out in the outpatient physiotherapy department of the university hospital. This study was completed over 9 months, starting from February 21, 2019 to October 26, 2019.
2.3. Ethical approval
Before conducting the study, ethical approval was taken from the Ethics Sub-Committee of King Saud University (file ID: RRC-2019-07; dated: 28/01/2019). Furthermore, the study got registered with “ClinicalTrials.gov PRS Protocol Registration and Results Systems (ClinicalTrials.gov ID: NCT05684666; dated: 23/08/2023).” This study was carried out in line with the Principles of the Helsinki Declaration (2013). All the participants were informed in detail regarding the study procedure, potential risks, and benefits. All the participants signed a written informed consent form before the start of the study.
2.4. Sample size calculation
The sample size was calculated with the help of G*Power software (V.3.1.9.4) with a combination of F tests - analysis of variance: repeated measures, between factors analysis: a priori: compute required sample size, Input: Effect size f = 0.4, α err prob = 0.05, Power (1-β err prob) = 0.9, Number of groups = 4, Number of measurements = 4, Correlation among repetitive measures = 0.5, Output: Non-centrality parameter λ = 15.36, Critical F = 2.77, Numerator df = 3.00, Denominator df = 56.00, Total sample size = 60, Actual power = 0.90.
2.5. Study participants
A total of sixty-four hypertensive participants (28 females and 46 males) with an average age of 47.80 ± 6.78years, height of 166.47 ± 8.34cm, weight of 72.64 ± 3.45kg., and Body Mass Index (BMI) of 25.62 ± 3.47kg/m2; willing to participate were screened based on inclusion and exclusion criteria were recruited for the study. They were randomly classified into 4 groups viz. SBE group, Progressive Muscle Relaxation (PMR) group, SBE + PMR group, and Control group by an independent researcher not affiliated with this study. The inclusion criteria were as follows: the participants with essential hypertension, having a diastolic BP between 90 to 109mm of Hg, a systolic BP of more than 140mm of Hg, and aged between 30 to 60 years. The exclusion criteria were participants with secondary hypertension, any physical abnormalities that may disturb the exercise intervention, the participant cannot perform any relaxation or breathing exercises, and showing non-cooperation for the study.
2.6. Experimental tools
A portable electronic self-calibrated stadiometer cum weighing scale (Deteco scale, 750 USA) was used to determine the weight, height, and body mass index. Each participant's systolic, diastolic, and pulse rates were assessed using a portable electronic sphygmomanometer (ORMON HEALTH CARE Co. Ltd. JAPAN). The respiratory rate of each participant was measured manually as the number of breaths a participant takes per minute. The perceived stress was assessed using the perceived stress scale (PSS)[29] with ten items, each with a 5-point Likert scale (where a score of 0 indicates “never,” a score of 1 means “nearly never,” a score of 2 “occasionally,” a score of 3 “very often,” and a score of 4 “often”). This tool was chosen to assess a person perceived degree of stress during the previous month to ascertain whether their stress level impacted their BP.[30] This scale has been shown to be accurate in hypertensive people.[31] The PSS is a widely used measure of global distress.[32] Researchers have discovered that PSS scores are linked to biological markers of stress and risk factors for coronary artery disease.[32]
2.7. Outcome measures
Systolic and diastolic BP (SBP and DBP), heart rate (HR), respiration rate (RR), and anxiety were all evaluated as the study outcomes using a digital sphygmomanometer and PSS at baseline (pre-intervention), 2nd week, and 4th weeks post-intervention. The outcome measures were taken by an assistant physiotherapist who was kept blind to the study group allocation.
2.8. Procedure
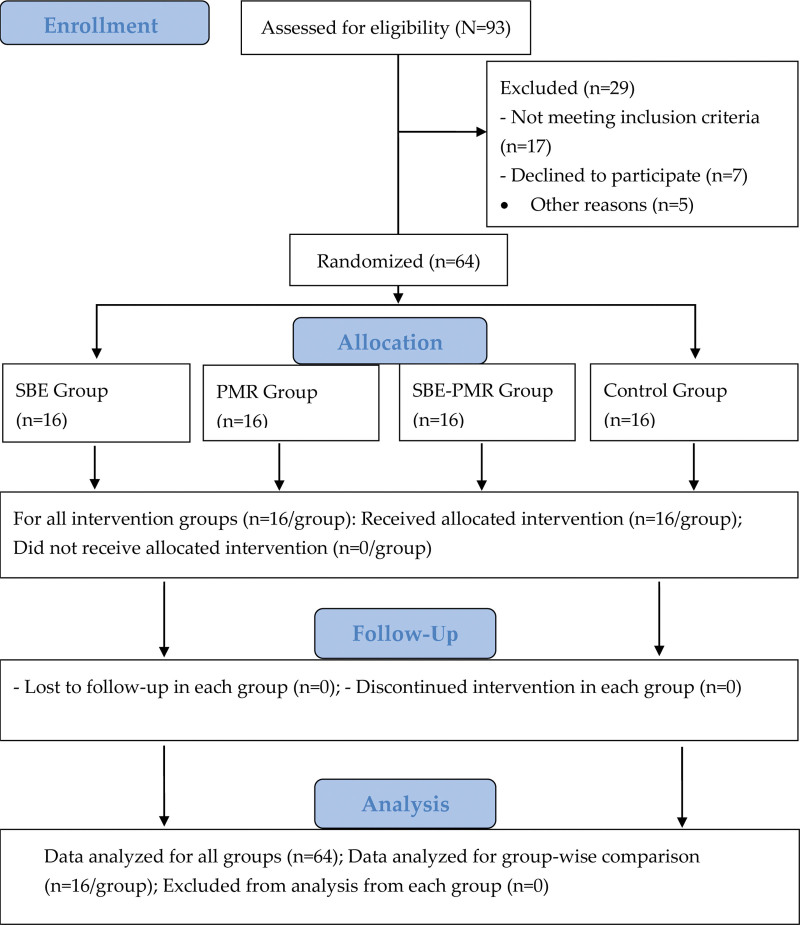
Sixty-four participants signed the informed consent form before the start of the study. The participants were randomly allocated to the respective groups using an online website for the randomization procedure (www.randomization.com). An assistant physiotherapist who kept blind to the participant group allocation carried out the demographic characteristics and baseline measurements for all the study outcomes. The same assessor assessed all the outcomes at different post-intervention time points. For each outcome, at least 2 readings were taken, and the average was recorded for the analysis. A CONSORT (2010) flow diagram depicts the study procedure, including recruitment, randomization, allocation, follow-up, and analysis in Figure 1.
Figure 1.
CONSORT (2010) Flow Diagram presenting the procedures, including enrollment, allocation, follow-up, and study analysis.
2.9. Interventions
The participants from all 4 groups performed/received their stipulated interventions as follows:
2.9.1. SBE group.
The SBE group was instructed to perform a SBE[22,33–35] as follows: All participants were asked to train in slow breathing 3 days before the day of the intervention. Participants received intervention for 30 minutes on all 3 days. The instructions for the SBE group were as follows: commands were used to demonstrate the exercises. Participants learned how to relax their bodies. They were instructed to put their hands down just below the anterior costal border and take calm, slow deep breaths and deeply through the nose. Kept the shoulders relaxed and the upper chest quiet, allowing the abdomen to raise slightly. Further, they were instructed to relax and take slow deep breaths. Participants were asked to make 6 breaths per minute.[22]
The participants were given ten minutes of rest, followed by the intervention.[33] Their position was feet flat, knees flexed with a supine posture[34] on the couch. BP, heart rate, respiratory rate, and perceived stress were measured. The participants were advised to feel the movement with their hands by placing them below the anterior costal margin so that their hands would rise slightly during inspiration and fall during expiration.[36] For 4 weeks, the SBE was performed for 30 minutes at a pace of 6 breaths per minute for each session twice a week.[22]
2.9.2. PMR group.
All participants from the PMR group were called for the PMR technique 3 days prior to the day of the intervention.[35] Participants received intervention for 30 minutes on all 3 days. All participants completed a session of 30 minutes of the PMR technique for 3 days. The participants were then made to sit on the chair with forearm support. The following steps of the PMR technique were taught.[35]
-
•
Step 1:- Make a fist with the dominant hand without involving the upper arm.
-
•
Step 2:- Pushing the elbow of the same arm down against the arm of the chair while keeping the hand relaxed.
-
•
Steps 3 & 4:- the non-dominant arm worked separately.
-
•
Step 5:- Raising the eyebrows.
-
•
Step 6:- Screw up the eyes and wrinkle the nose.
-
•
Step 7:- Clenching the teeth and pull back the mouth corner.
-
•
Step 8: Pull the chin down, press the head against the support, and tense the neck muscles.
-
•
Step 9:- Drawing the shoulders back.
-
•
Step 10:- Tightening the abdominal muscles.
-
•
Step 11:- Tensing the thigh of the dominant leg by contracting the knee flexors and extensors together.
-
•
Step 12:- Pointing the dominant foot down (Plantarflexion).
-
•
Step 13:- Pulling the dominant foot up toward the face (Dorsiflexion)
-
•
Steps 14, 15, 16:- The nondominant leg was worked separately.
A 10 minutes of rest followed by the intervention were given to the participants.[33] The participants were supine on the couch with their knees flexed and their feet flat.[34] Then participants were instructed to sit down and complete all 16 steps of the PMR for 30 minutes twice per week for 4 weeks.
2.9.3. SBE-PMR group.
All participants from the SBE-PMR group were called for SBE and PMR techniques 3 days before the day of the intervention. Participants received intervention for 60 minutes on all 3 days. The instructions for the SBE-PMR group were as follows- SBE and MPR technique for 60 minutes, explained above in the SBE and PMR groups.
The participants were given ten minutes of rest, followed by the intervention.[33] The participants were lying flat on their backs with their knees flexed and their feet flat[34] on the couch. Participants practiced slow breathing and progressive muscle relaxation under the researcher supervision for 60 minutes twice a week for 4 weeks.
2.9.4. Control group.
No intervention was offered to the participants from the control group. On the day of recruitment, baseline diastolic, systolic BP, and heart rate were measured with the help of a sphygmomanometer, and respiratory rate was measured manually, followed by perceived stress. The participants returned after 3 days. They were asked to rest for 30 minutes, and all the measurements were taken. Again, the measurements were taken after the 4th session and after the 8th session for all the groups and compared with baseline measurements.
2.10. Statistical analysis
The statistical package for social sciences (IBM SPSS) (SPSS Inc., Chicago, IL) Version 26.0 was used to statistically analyze the data. Data were reviewed for outliers and missing data before the analysis. The Shapiro–Wilk test was used to determine the normality of the data at a significance level of P > .05. for all outcome measures, while anthropometrical characteristics data and outcome measures were normally distributed, the parametric test was applied. The mean and standard deviation (SD) were used to describe and infer anthropometrical characteristics. The outcome measures were summarized using means differences, standard error, and 95% class interval as Lower Limit (LL) and Upper Limit (UL). The repeated measures analysis of variance test assessed intra-group comparison (overall) of the effect of treatment on systolic and diastolic pressure, heart rate, respiratory rate, and perceived stress between the times. Bonferroni multiple comparison tests were used to analyze the mean differences between the groups. The confidence interval was kept at 95% for all the statistical analyses, that is, P < .05 was considered significant.
3. Results
Tables 1 and 2 represent the gender distribution and anthropometric characteristics of the participants in each group.
Table 1.
Gender distribution in 4 groups (N = 60).
| Groups | Male (%) | Female (%) |
|---|---|---|
| SBE | 6 (10.00) | 10 (16.67) |
| PMR | 9 (15.00) | 7 (11.67) |
| SBE-PMR | 10 (16.67) | 6 (10.00) |
| Control | 11 (18.33) | 5 (8.33) |
| Total | 36 (60.00) | 28 (46.67) |
% = percentage value, PMR = progressive muscle relaxation, SBE = slow breathing exercise.
Table 2.
Anthropometrical characteristics among 4 groups (Mean ± SD).
| Groups | Age (yr) | Height (cm) | Weight (kg) | BMI (kg/m2) |
|---|---|---|---|---|
| SBE | 47.75 ± 7.04 | 160.50 ± 9.75 | 70.50 ± 12.64 | 27.99 ± 3.72 |
| PMR | 47.60 ± 5.38 | 165.56 ± 7.65 | 67.75 ± 10.37 | 24.63 ± 2.21 |
| SBE-PMR | 47.93 ± 7.99 | 167.62 ± 7.80 | 73.31 ± 7.21 | 26.13 ± 2.07 |
| Control | 49 ± 6.76 | 167.87 ± 6.93 | 80.43 ± 23.59 | 26.33 ± 2.18 |
PMR = progressive muscle relaxation, SBE = slow breathing exercise, SD = standard deviation.
Table 3 shows the comparison of HR, RR, SBP, DBP, and PSS scores with Bonferroni analysis between the 3 levels of measurement in all the groups. HR, RR, SBP, DBP, and PSS have been reduced significantly (0.0001) over the period of time. The mean difference in HR score between baseline vs IInd week, IInd week vs IVth week, and baseline vs IVth week were 1.500, 1.031, and 2.531, respectively. The respective standard error was 0.089, 0.103, and 0.120. The mean difference in RR score between baseline vs IInd week, IInd week vs IVth week, and baseline vs IVth week were 1.000, 0.844, and 1.844, respectively. The respective standard error was 0.169, 0.187, and 0.102. The mean difference in SBP score between baseline vs IInd week, IInd week vs IVth week, and baseline vs IVth week were 3.219, 2.875, and 6.094, respectively. The respective standard error was 0.210, 0.172, and 0.265. The mean difference in DBP score between baseline vs IInd week, IInd week vs IVth week, and baseline vs IVth week were 2.438, 1.563, and 4.000, respectively. The respective standard error was 0.147, 0.134, and 0.168. The mean difference in PSS score between baseline vs IInd week, IInd week vs IVth week, and baseline vs IVth week were 2.297, 2.172, and 4.469, respectively. The respective standard error was 0.103, 0.122, and 0.147. The highly significant difference between all 3 levels shows a greater reduction in HR, RR, SBP, DBP, and PSS with the treatment.
Table 3.
Intra group comparison (overall) of the effect of treatment on heart rate, respiratory rate, systolic blood pressure, diastolic blood pressure, and perceived stress between the times.
| Outcomes | Level | Mean difference | Standard error | 95% CI LL–UL | F | Sig. |
|---|---|---|---|---|---|---|
| Heart rate | Baseline vs IInd wk | 1.50 | 0.09 | 1.28–1.72 | 239.04 | 0.0001* |
| IInd wk vs IVth wk | 1.03 | 0.10 | 0.78–1.28 | 0.0001* | ||
| Baseline vs IVth wk | 2.53 | 0.12 | 2.24–2.83 | 0.0001* | ||
| Respiratory rate | Baseline vs IInd wk | 1.00 | 0.17 | 0.58–1.42 | 167.74 | 0.0001* |
| IInd wk vs IVth wk | 0.84 | 0.19 | 0.38–1.31 | 0.0001* | ||
| Baseline vs IVth wk | 1.84 | 0.10 | 1.59–2.09 | 0.0001* | ||
| Systolic blood pressure | Baseline vs IInd wk | 3.22 | 0.21 | 2.70–3.74 | 266.64 | 0.0001* |
| IInd wk vs IVth wk | 2.87 | 0.17 | 2.45–3.31 | 0.0001* | ||
| Baseline vs IVth wk | 6.09 | 0.26 | 5.44–6.74 | 0.0001* | ||
| Diastolic blood pressure | Baseline vs IInd wk | 2.44 | 0.15 | 2.08–2.82 | 279.80 | 0.0001* |
| IInd wk vs IVth wk | 1.56 | 0.13 | 1.23–1.89 | 0.0001* | ||
| Baseline vs IVth wk | 4.00 | 0.17 | 3.59–4.41 | 0.0001* | ||
| Perceived stress scale | Baseline vs IInd wk | 2.29 | 0.10 | 2.04–2.55 | 473.42 | 0.0001* |
| IInd wk vs IVth wk | 2.17 | 0.12 | 1.87–2.47 | 0.0001* | ||
| Baseline vs IVth wk | 4.47 | 0.15 | 4.12–4.83 | 0.0001* |
Highly significant if P < .01. Adjustment for multiple comparisons: Bonferroni. LL = Lower Limit, UL = Upper Limit.
Table 4 shows the comparison of the effect of treatment on HR reduction between the SBE, PMR, SBE-PMR, and Control groups. The mean values were 2.1250, 0.1875, 3.4375, −1.9375, 1.3125, and 3.2500, respectively. There is a significant difference between the groups except for the SBE group and the SBE-PMR group over HR. The standard error was the same for all, i.e., 0.3333.
Table 4.
Inter group comparison of the effect of treatment on heart rate (HR).
| Groups | Mean difference | Standard error | 95% CI LL–UL | F-value | P level |
|---|---|---|---|---|---|
| SBE vs PMR | 2.13 | 0.33 | 1.22 to 3.03 | 48.57 | 0.0001* |
| SBE vs SBE-PMR | 0.19 | 0.33 | −0.72 to 1.11 | 1.0000 | |
| SBE vs Control | 3.44 | 0.33 | 2.53 to 4.35 | 0.0001* | |
| PMR vs SBE-PMR | -1.94 | 0.33 | −2.85 to 1.03 | 0.0001* | |
| PMR vs Control | 1.31 | 0.33 | 0.40 to 2.22 | 0.0001* | |
| SBE-PMR vs Control | 3.25 | 0.33 | 2.34 to 4.16 | 0.0001* |
= Highly Significant. Adjustment for multiple comparisons: Bonferroni. PMR = Progressive muscle relaxation, SBE = Slow breathing exercise.
Table 5 shows the comparison of the effect of treatment on RR reduction between the SBE, PMR, SBE-PMR, and Control groups. The mean values were 1.3125, 0.4375, 2.6250, −0.8750, 1.3125, and 2.1875, respectively. There is a significant difference between the groups except for the SBE group and SBE-PMR group over RR. The standard error was the same for all, i.e., 0.2891.
Table 5.
Inter group comparison of the effect of treatment on respiratory rate (RR).
| Groups | Mean difference | Standard error | 95% CI LL - UL | F-value | P level |
|---|---|---|---|---|---|
| SBE vs PMR | 1.31 | 0.29 | 0.52 to 2.10 | 32.05 | 0.0001* |
| SBE vs SBE-PMR | 0.44 | 0.29 | −035 to 1.23 | 0.8130 | |
| SBE vs Control | 2.63 | 0.29 | 1.84 to 3.41 | 0.0001* | |
| PMR vs SBE-PMR | -0.88 | 0.29 | −1.66 to 0.08 | 0.0222 | |
| PMR vs Control | 1.31 | 0.29 | 0.52 to 2.10 | 0.0001* | |
| SBE-PMR vs Control | 2.19 | 0.29 | 1.39 to 2.97 | 0.0001* |
- Highly Significant if P < .01. Adjustment for multiple comparisons: Bonferroni. PMR = Progressive muscle relaxation, SBE = Slow breathing exercise.
Table 6 shows the comparison of the effect of treatment on SBP reduction between the SBE, PMR, SBE-PMR, and Control groups. The mean values were 4.0000, −0.3750, 6.8750, −4.3750, 2.8750, and 7.2500, respectively. There is a significant difference between the groups except for the SBE group and the SBE-PMR group over SBP. The standard error was the same for all, that is, 0.7048.
Table 6.
Inter group comparison of the effect of treatment on systolic blood pressure (SBP).
| Groups | Mean difference | Standard error | 95% CI LL–UL | F-value | P level |
|---|---|---|---|---|---|
| SBE vs PMR | 4.00 | 0.70 | 2.08–5.93 | 48.09 | 0.0001* |
| SBE vs SBE-PMR | -0.37 | 0.70 | -2.32-1.55 | 1.0000 | |
| SBE vs Control | 6.87 | 0.70 | 4.95–8.81 | 0.0001* | |
| PMR vs SBE-PMR | -4.37 | 0.70 | -6.31-2.45 | 0.0001* | |
| PMR vs Control | 2.87 | 0.70 | 0.95–4.82 | 0.0010* | |
| SBE-PMR vs Control | 7.25 | 0.70 | 5.33–9.17 | 0.0001* |
- Highly Significant. Adjustment for multiple comparisons: Bonferroni. PMR = Progressive muscle relaxation, SBE = Slow breathing exercise.
Table 7 shows the comparison of the effect of treatment on DBP reduction between the SBE, PMR, SBE-PMR, and Control groups. The mean values were 2.3750, 0.3750, 3.7500, −2.0000, 1.3750, and 3.3750, respectively. There is a significant difference between the groups except for the SBE and SBE-PMR groups over DBP. The standard error was the same for all, that is, 0.4884.
Table 7.
Inter Group comparison of the effect of treatment on Diastolic Blood Pressure (DBP).
| Groups | Mean Difference | Standard Error | 95% CI LL–UL | F-value | P level |
|---|---|---|---|---|---|
| SBE vs PMR | 2.38 | 0.49 | 1.04 to 3.71 | 25.93 | 0.0001* |
| SBE vs SBE-PMR | 0.38 | 0.49 | −0.96 to 1.71 | 1.0000 | |
| SBE vs Control | 3.75 | 0.49 | 2.42 to 5.08 | 0.0001* | |
| PMR vs SBE-PMR | -2.00 | 0.49 | −3.33 to 0.67 | 0.0010* | |
| PMR vs Control | 1.37 | 0.49 | 0.04 to 2.71 | 0.0040* | |
| SBE-PMR vs Control | 3.37 | 0.49 | 2.04 to 4.71 | 0.0001* |
- Highly Significant. Adjustment for multiple comparisons: Bonferroni. PMR = Progressive muscle relaxation, SBE = Slow breathing exercise.
Table 8 shows the comparison of the effect of treatment on the PSS between the SBE, PMR, SBE-PMR, and Control groups. The mean values were −1.9375, −1.8750, 3.1875, 0.0625, 5.1250, and 5.0625 respectively. There is a significant difference between the groups except for the PMR and SBE-PMR groups over the PSS. The standard error was the same for all, that is, 0.41.
Table 8.
Inter Group comparison of the effect of treatment on the Perceived Stress Scale (PSS).
| Groups | Mean Difference | Standard Error | 95% CI LL–UL | F value | P level |
|---|---|---|---|---|---|
| SBE vs PMR | -1.94 | 0.41 | −3.07 to −0.81 | 67.12 | 0.0001* |
| SBE vs SBE-PMR | -1.87 | 0.41 | −3.01 to −0.74 | 0.0001* | |
| SBE vs Control | 3.19 | 0.41 | 2.06 to 4.32 | 0.0001* | |
| PMR vs SBE-PMR | 0.06 | 0.41 | −1.07 to 1.19 | 1.0000 | |
| PMR vs Control | 5.13 | 0.41 | 3.99 to 6.26 | 0.0001* | |
| SBE-PMR vs Control | 5.06 | 0.41 | 3.93 to 6.19 | 0.0001* |
- Highly Significant. Adjustment for multiple comparisons: Bonferroni. PMR = Progressive muscle relaxation, SBE = Slow breathing exercise.
4. Discussion
This study aimed to investigate the combined effect of the SBE and PMR techniques on BP, HR, RR, and anxiety in patients diagnosed with essential hypertension. Within-group comparison of HR showed a significant difference in the SBE (Baseline 76.4 ± 1.7 bpm, After 2 weeks 74.2 ± 1.4 bpm, After 4 weeks 72.5 ± 1.1bpm, P < .05), PMR (Baseline 75.1 ± 1.2 bpm, After 2 weeks 74.1 ± 1.3 bpm, After 4 weeks 73.1 ± 1 bpm, P < .05), and SBE-PMR groups (Baseline 76.3 ± 1.5 bpm, After 2 weeks 73.9 ± 1.2 bpm, After 4 weeks 72.4 ± 1.2 bpm, P < .05). Between-group comparison of HR shows a significant difference between SBE and PMR (2.12 bpm, P < .05), SBE and control (3.43 bpm, P < .05), PMR and SBE-PMR (-1.93 bpm, P < .05), PMR and Control (1.31 bpm, P < .05), and SBE-PMR and control groups (3.25 bpm, P < .05). However, no significant difference was found between the SBE and SBE-PMR groups (0.18 bpm, P > .05).
A similar result was reported by Sheu et al[35] in their study on the impact of the progressive muscle relaxation (PMR) approach on individuals with essential hypertension. After employing the PMR technique, they found a statistically significant reduction in pulse rate (from 70.85 bpm to 66.0 bpm, P < .05). In contrast, Pinheiro et al[35] found no statistically significant difference in the resting heart rate (from 74.8 beats per minute to 72.9 beats per minute, P > .05) following the implementation of respiratory retraining. Our study findings suggest a decrease in heart rate (HR) in both the SBE and SBE-PMR groups, which may indicate enhanced parasympathetic activity. The findings of our study are consistent with the research conducted by Jerath et al,[37] which suggests that practicing pranayama breathing can effectively reduce resting heart rate by enhancing vagal tone and decreasing sympathetic discharge.
A comparison of respiratory rate within groups revealed a statistically significant difference in the SBE group (Baseline: 15.1 ± 0.9 breaths, After 2 weeks: 13.4 ± 0.7 breaths, After 4 weeks: 12.2 ± 0.5 breaths, P < .05), the PMR group (Baseline: 14.7 ± 0.9 breaths, After 2 weeks: 13.5 ± 0.8 breaths, After 4 weeks: 13.1 ± 0.8 breaths, P < .05), and the SBE-PMR group (Baseline: 15.4 ± 0.9 breaths, After 2 weeks: 14 ± 0.8 breaths, After 4 weeks: 12.9 ± 0.7 breaths, P < .05). The results of the intergroup comparison of RR indicated statistically significant differences between the SBE and PMR groups (mean difference of 1.3 breaths, P < .05), SBE and control groups (mean difference of 2.6 breaths, P < .05), PMR and SBE-PMR groups (mean difference of −0.8 breaths, P < .05), PMR and control groups (mean difference of 1.31 breaths, P < .05), and SBE-PMR and control groups (mean difference of 2.18 breaths, P < .05). However, no statistically significant difference was observed between the SBE and SBE-PMR groups (mean difference of 0.4 breaths, P > .05).
The findings presented in this study are consistent with the results reported by Pinheiro et al[34] about the impact of SBE on individuals diagnosed with essential hypertension. Pinheiro et al observed a significant decrease in the resting respiratory rate (from 14.60 ± 1.6 breaths/minute to 10.10 ± 1.1 breaths/minute, P < .01) among these patients. Given its association with increased activation of the diaphragm and respiratory muscles, SBE has the potential to enhance exercise capacity by delaying the onset of dyspnea and fatigue.[38] Patients diagnosed with hypertension often exhibit hyperventilation symptoms even during rest periods. This suggests that the cardio-respiratory abnormalities observed in these individuals may be linked to a shared excitatory pattern within the autonomic nervous system. It is possible that adopting a slower breathing rhythm could potentially regulate these abnormalities.[39] The results of our study indicate that both the SBE-PMR group and the SBE group exhibited a statistically significant improvement in RR compared to the PMR group in isolation.
The within-group comparison of systolic blood pressure (SBP) revealed a statistically significant difference in the SBE group (Baseline: 152.2 ± 8.5 mm Hg, After 2 weeks: 147.6 ± 7.4 mm Hg, After 4 weeks: 143.2 ± 6.6 mm Hg, P < .05), the PMR group (Baseline: 149.5 ± 5.3 mm Hg, After 2 weeks: 147 ± 5.2 mm Hg, After 4 weeks: 144.8 ± 5.0 mm Hg, P < .05), and the SBE-PMR group (Baseline: 151.7 ± 5.6 mm Hg, After 2 weeks: 146.8 ± 5.7 mm Hg, After 4 weeks: 143 ± 6.5 mm Hg, P < .05). A group comparison was conducted to examine the SBP levels. The results indicated a significant difference in SBP between the SBE and PMR groups (4 mm Hg, P < .05), SBE and the control group (6.87 mm Hg, P < .05), PMR and SBE-PMR (-4.37 mm Hg, P < .05), PMR and the control group (2.87 mm Hg, P < .05), and the SBE-PMR and control groups (7.25 mm Hg, P < .05). However, there was no significant difference in SBP between the SBE and SBE-PMR groups (-0.3 mm Hg, P > .05).
The findings align with the findings reported by Mori et al,[33] who demonstrated that a single session of slow deep breathing for 30 seconds resulted in a decrease in SBP from an average of 124.0 ± 15.8mmHg to 117.6 ± 14.7mmHg. Furthermore, the research conducted by the authors demonstrated a significant alteration in SBP when comparing the slow, deep breathing group to the control group. Similar results were observed in a study conducted by Yung et al,[40] where they observed a significant decrease in SBP (from 134.6 mm Hg to 125.8 mm Hg, P < .05) among individuals with moderate hypertension. The study authors proposed that relaxation techniques could serve as an adjunctive therapy for individuals with mild hypertension.
A group comparison examined the differences in diastolic blood pressure (DBP) among the SBE, PMR, and SBE-PMR groups. The results indicated a significant decrease in DBP over time for all 3 groups (SBE: Baseline 91.6 ± 1.8 mm Hg, After 2 weeks 88.5 ± 1.8 mm Hg, After 4 weeks 86.1 ± 1.8 mm Hg, P < .05; PMR: Baseline 91 ± 1.2 mm Hg, After 2 weeks 88.7 ± 2 mm Hg, After 4 weeks 87.6 ± 2.2 mm Hg, P < .05; SBE-PMR: Baseline 91 ± 1.7 mm Hg, After 2 weeks 88.1 ± 1.5 mm Hg, After 4 weeks 85.7 ± 1.9 mm Hg, P < .05). The between-group comparison of diastolic blood pressure (DBP) reveals statistically significant differences between the SBE and PMR groups (2.37 mm Hg, P < .05), SBE and control groups (3.75 mm Hg, P < .05), PMR and SBE-PMR groups (−2 mm Hg, P < .05), PMR and control groups (1.37 mm Hg, P < .05), and SBE-PMR and control groups (3.37 mm Hg, P < .05). However, no statistically significant difference is observed between the SBE and SBE-PMR groups (0.37 mm Hg, P > .05).
In the investigation conducted by Bernardi et al,[22] a cohort of 81 individuals diagnosed with congestive heart failure was examined. The study revealed a decrease in diastolic blood pressure (DBP) from an initial value of 62 mm Hg to 59 mm Hg following a 4-minute session of SBE performed at a pace of 6 breaths per minute. The outcomes of this investigation are consistent with the results obtained in our study. SBE, characterized by a respiratory rate of less than ten breaths per minute, are associated with enhanced baroreflex sensitivity. This suggests that SBE induces a shift in autonomic balance, manifested by a decrease in sympathetic activity in absolute terms or relative to parasympathetic tone.
Consequently, this leads to a reduction in SBP and DBP. Notably, the observed decrease in SBP and DBP resulting from SBE is greater than that observed in progressive muscle relaxation (PMR) and significantly higher than in the control group. The process of relaxation can potentially influence the hypothalamus response towards parasympathetic neurons, resulting in a decrease in heart rate, blood pressure, metabolism, and respiratory rate. This state of relaxation also leads to a reduction in oxygen consumption and alleviation of muscle tension.[22]
A comparative analysis was performed on the Perceived Stress Scale (PSS) scores at the Baseline, After 2 weeks, and After 4 weeks of intervention within groups. The results indicate a significant difference in the scores for the SBE group (Baseline: 20.6 ± 4.4, After 2 weeks: 18.6 ± 4.2, After 4 weeks: 16.3 ± 4.3, P < .05), the PMR group (Baseline: 18.9 ± 5.4, After 2 weeks: 15.8 ± 5.3, After 4 weeks: 12.6 ± 5.5 mm Hg, P < .05), and the SBE-PMR group (Baseline: 21.3 ± 3.8, After 2 weeks: 17.9 ± 3.8, After 4 weeks: 15.1 ± 3.8 mm Hg, P < .05). A comparative analysis examined various groups’ differences in Perceived Stress Scale (PSS) scores. The results indicated that there were significant differences in PSS scores between the SBE and PMR groups (−1.93, P < .05), SBE and control groups (3.18, P < .05), SBE and SBE-PMR groups (−1.87, P < .05), PMR and control groups (5.12, P < .05), and SBE-PMR and control groups (5.06, P < .05). However, no significant difference was observed between the PMR and SBE-PMR groups (0.06, P > .05).
A similar result was obtained from Yung et al,[40] wherein they documented a statistically significant decrease in the perceived stress scale (from 19.35 to 15.80, P < .05) after the implementation of progressive muscle relaxation (PMR) intervention. According to Maloh et al,[41] it has been suggested that relaxation techniques have the potential to reduce neural reflex activity, leading to a drop in skeletomuscular neural input and output activity. This reduction in neural activity is believed to contribute to decreased stress levels, as observed in the progressive muscle relaxation (PMR) group. The results of this study exhibit similarities with the SBE-PMR group but diverge from the SBE and control groups. The arterial baroreceptors, pulmonary stretch receptors, and low-pressure baroreceptors, activated by the autonomic nervous system, play a crucial role in decreasing blood pressure and pulse rate induced by slow, deep breathing, as shown by Cohen et al.[36]
4.1. Study limitations
There are a few limitations of the study. The study was conducted to find out the short-term effects of relaxation techniques. The effects of SBE and PMR techniques can be evaluated long-term. All the patients have essential hypertension. So, the study results cannot be generalized to participants with other types of hypertension. Including participants from other hypertension, stages would have been more representative. This study sample size was relatively small due to the convenience sampling technique. Recruiting more samples would have strengthened the result and conclusion. Other techniques like stretch release and cognitive imagery relaxation can also be compared with SBE.
5. Conclusion
Our study leads to the following conclusion: there were significant changes in HR, RR, SBP, DBP, and PSS scores in essential hypertensive patients following SBE, PMR technique alone, and combined SBE plus PMR technique compared to the control group. There was a significant change in PSS score in essential hypertensive patients following the PMR technique and combined SBE plus PMR technique compared to SBE alone. Therefore, the combined treatment of the SBE plus PMR technique can effectively reduce the HR, RR, SBP, DBP, and anxiety in essential hypertensive patients compared to both interventions.
Acknowledgments
The authors are grateful to the Researchers Supporting Project number (RSP2023R382), King Saud University, Riyadh, Saudi Arabia, for funding this research.
Author contributions
Conceptualization: Farhan Khan M. Pathan, Joseley Sunderraj Pandian, Anis I. Shaikh, Mohammad Ahsan, Shibili Nuhmani, Amir Iqbal.
Data curation: Farhan Khan M. Pathan, Joseley Sunderraj Pandian, Anis I. Shaikh.
Formal analysis: Shibili Nuhmani, Amir Iqbal, Ahmad H. Alghadir.
Funding acquisition: Ahmad H. Alghadir.
Methodology: Farhan Khan M. Pathan, Joseley Sunderraj Pandian, Anis I. Shaikh, Shibili Nuhmani, Amir Iqbal.
Supervision: Mohammad Ahsan, Shibili Nuhmani, Ahmad H. Alghadir.
Writing – original draft: Farhan Khan M. Pathan, Joseley Sunderraj Pandian, Anis I. Shaikh, Mohammad Ahsan.
Writing – review & editing: Farhan Khan M. Pathan, Joseley Sunderraj Pandian, Anis I. Shaikh, Mohammad Ahsan, Shibili Nuhmani, Amir Iqbal, Ahmad H. Alghadir.
Abbreviations:
- BP
- blood pressure
- DBP
- diastolic blood pressure
- HR
- heart rate
- PMR
- progressive muscle relaxation
- PSS
- perceived stress scale
- RR
- respiratory rate
- SBE
- slow breathing exercise
- SBP
- systolic blood pressure
Trial registration: ClinicalTrials.gov Identifier: NCT05684666; dated: 23/08/2023.
The study obtained ethical approval from the Ethics Sub-committee (file ID: RRC-2019-04; dated: 16/01/2019) at King Saud University, Saudi Arabia, and was conducted in accordance with the declaration of Helsinki (2010); written informed consent was obtained from the patient(s) to participate in this study.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
The authors have no conflicts of interest to disclose.
The study was funded by the Researchers Supporting Project number (RSP2023R382), King Saud University, Riyadh, Saudi Arabia.
How to cite this article: Pathan FKM, Pandian JS, Shaikh AI, Ahsan M, Nuhmani S, Iqbal A, Alghadir AH. Effect of slow breathing exercise and progressive muscle relaxation technique in the individual with essential hypertension: A randomized controlled trial. Medicine 2023;102:47(e35792).
Contributor Information
Farhan Khan M. Pathan, Email: Farhan_kpathan@yahoo.com.
Joseley Sunderraj Pandian, Email: joseleympt@gmail.com.
Anis I. Shaikh, Email: anisismail_786@yahoo.co.in.
Mohammad Ahsan, Email: mahsan@iau.edu.sa.
Shibili Nuhmani, Email: snuhmani@iau.edu.sa.
Ahmad H. Alghadir, Email: aalghadir@hotmail.com.
References
- [1].Saxena T, Ali AO, Saxena M. Pathophysiology of essential hypertension: an update. Expert Rev Cardiovasc Ther. 2018;16:879–87. [DOI] [PubMed] [Google Scholar]
- [2].Sarkar T, Singh NP. Epidemiology and genetics of hypertension. J Assoc Physicians India. 2015;63:61–98. [PubMed] [Google Scholar]
- [3].Al-Noumani H, Wu JR, Barksdale D, et al. Health beliefs and medication adherence in patients with hypertension: a systematic review of quantitative studies. Patient Educ Couns. 2019;102:1045–56. [DOI] [PubMed] [Google Scholar]
- [4].Verma N, Rastogi S, Chia YC, et al. Non-pharmacological management of hypertension. J Clin Hypertens (Greenwich). 2021;23:1275–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Torales J, O’Higgins M, Barrios I, et al. An overview of jacobson’s progressive muscle relaxation in managing anxiety. Rev Argen de Cli Psicolo. 2020;29:17–23. [Google Scholar]
- [6].Toussaint L, Nguyen QA, Roettger C, et al. Effectiveness of progressive muscle relaxation, deep breathing, and guided imagery in promoting psychological and physiological states of relaxation. Evid Based Complement Alternat Med. 2021;2021:5924040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Kömürkara S, Cengiz Z. Effects of progressive relaxation exercises on vital signs and fatigue in liver transplant patients: a randomized controlled trial. Clin Nurs Res. 2022;31:497–508. [DOI] [PubMed] [Google Scholar]
- [8].Gallego-Gómez JI, Balanza S, Leal-Llopis J, et al. Effectiveness of music therapy and progressive muscle relaxation in reducing stress before exams and improving academic performance in Nursing students: a randomized trial. Nurse Educ Today. 2020;84:104217. [DOI] [PubMed] [Google Scholar]
- [9].Astuti NF, Rekawati E, Wati DNK. Decreased blood pressure among community dwelling older adults following progressive muscle relaxation and music therapy (RESIK). BMC Nurs. 2019;18(Suppl 1):36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Blanchard EB, Mccoy CG, Wittrok D. A controlled comparison of thermal feedback and relaxation training in treatment of essential hypertension: II Effects on cardiovascular reactivity. Health Psychol. 1988;7:19–33. [DOI] [PubMed] [Google Scholar]
- [11].Cottier C, Shapiro K, Julius S. Treatment of mild hypertension with progressive muscle relaxation. Arch Intern Med. 1984;144:1954–8. [PubMed] [Google Scholar]
- [12].Wilczyńska D, Łysak-Radomska A, Podczarska-Głowacka M, et al. Evaluation of the effectiveness of relaxation in lowering the level of anxiety in young adults-a pilot study. Int J Occup Med Environ Health. 2019;32:817–24. [DOI] [PubMed] [Google Scholar]
- [13].Gangadharan MP, Madani MA. Effectiveness of progressive muscle relaxation techniques on depression, anxiety and stress among undergraduate nursing students. Int J Health Sci Res. 2018;8:155–63. [Google Scholar]
- [14].Ermayani M, Prabawati D, Susilo WH. The effect of progressive muscle relaxation on anxiety and blood pressure among hypertension patients in east Kalimantan, Indonesia. Enfermería Clínica. 2020;30:121–5. [Google Scholar]
- [15].Ping KF, Bakar A, Subramaniam S, et al. The impact of music guided deep breathing exercise on blood pressure control-a participant blinded randomised controlled study. Med J Malaysia. 2018;73:233–8. [PubMed] [Google Scholar]
- [16].Gamboa A, Nian H, Smith EC, et al. Twelve weeks of slow breathing exercises reduces blood pressure among healthy normotensive subjects. medRxiv. 2022;30:22279389. [Google Scholar]
- [17].Pal GK, Velkumary S, Madanmohan. Effect of short-term practice of breathing exercises on autonomic functions in normal human volunteers. Indian J Med Res. 2004;120:115–21. [PubMed] [Google Scholar]
- [18].Goso Y, Asanoi H, Ishise H, et al. Respiratory modulation of muscle sympathetic nerve activity in patients with chronic heart failure. Circulation. 2001;104:418–23. [DOI] [PubMed] [Google Scholar]
- [19].Talma R, Ariela A, Endna P, et al. Device-guided breathing exercise reduce blood pressure: ambulatory and home measurements. Am J Hypertens. 2001;14:74–6. [DOI] [PubMed] [Google Scholar]
- [20].Cahalin LP, Arena RA. Breathing exercises and inspiratory muscle training in heart failure. Heart Fail Clin. 2015;11:149–72. [DOI] [PubMed] [Google Scholar]
- [21].Lopes CP, Danzmann LC, Moraes RS, et al. Yoga and breathing technique training in patients with heart failure and preserved ejection fraction: study protocol for a randomized clinical trial. Trials. 2018;19:405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Bernardi L, Porta C, Spicuzza L, et al. Slow breathing increases arterial baroreflex sensitivity in patients with Chronic Heart Failure. Circulation. 2002;105:143–5. [DOI] [PubMed] [Google Scholar]
- [23].Das RR, Sankar J, Kabra SK. Role of breathing exercises in asthma-yoga and pranayama. Indian J Pediatr. 2022;89:174–80. [DOI] [PubMed] [Google Scholar]
- [24].Yau KK, Loke AY. Effects of diaphragmatic deep breathing exercises on prehypertensive or hypertensive adults: a literature review. Complement Ther Clin Pract. 2021;43:101315. [DOI] [PubMed] [Google Scholar]
- [25].Khanum A, Khan S, Kausar S, et al. Effects of diaphragmatic breathing exercises on blood sugar levels in working class females with type-2 diabetes mellitus. Int J Med Res Health Sci. 2019;8:34–42. [Google Scholar]
- [26].Al-Hawamdeh КМ, Vitomska МV, Gavreliuk SV. The influence of breathing exercises on anxiety and depression of cardiosurgical patients within the stationary program of physical therapy. Art Med. 2020:13–20. [Google Scholar]
- [27].Şahin O, Kocamaz D. Effects of diaphragmatic mobilization and diaphragmatic breathing exercises on pain and quality of life in individuals with shoulder pain: a randomized controlled trial. Int J Disabil Sports Health Sci. 2021;4:113–23. [Google Scholar]
- [28].Kang ES, Yook JS, Ha MS. Breathing exercises for improving cognitive function in patients with stroke. J Clin Med. 2022;11:2888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- [30].MacDonald MB, Laing GP, Wilson MP, et al. Prevalence and predictors of white-coat response in patients with treated hypertension. CMAJ. 1999;161:265–9. [PMC free article] [PubMed] [Google Scholar]
- [31].Baum A, Gatchel RJ, Schaeffer MA. Emotional, behavioral, and physiological effects of chronic stress at Three Mile Island. J Consult Clin Psychol. 1983;51:565–72. [DOI] [PubMed] [Google Scholar]
- [32].Labbate LA, Fava M, Oleshansky M, et al. Physical fitness and perceived stress Relationships with coronary artery disease risk factors. Psychosomatics. 1995;36:555–60. [DOI] [PubMed] [Google Scholar]
- [33].Mori H, Yamamoto H, Kuwashima M, et al. How does deep breathing affect office blood pressure and pulse rate? Hypertens Res. 2005;28:499–504. [DOI] [PubMed] [Google Scholar]
- [34].Pinheiro C, Medeiros R, Pinheiro D, et al. Spontaneous respiratory modulation improves cardiovascular control in essential hypertension. Arq Bras Cardiol. 2007;88:576–83. [DOI] [PubMed] [Google Scholar]
- [35].Sheu S, Irvin BL, Lin HS, et al. Effects of progressive muscle relaxation on blood pressure and psychosocial status for clients with essential hypertension in Taiwan. Holist Nurs Pract. 2003;17:41–7. [DOI] [PubMed] [Google Scholar]
- [36].Kisner C, Colby LA. Therapeutic Exercise. 5th Edition. Jaypee Brothers Medical Publishers (P) Ltd. 2007;862–3. [Google Scholar]
- [37].Jerath R, Edry JW, Barnes VA, et al. Physiology of long pranayamic breathing: neural respiratory elements may provide a mechanism that explains how slow deep breathing shifts the autonomic nervous system. Med Hypotheses. 2006;67:566–71. [DOI] [PubMed] [Google Scholar]
- [38].Varvogli L, Darviri C. Stress Management Techniques: evidence-based procedures that reduce stress and promote health. Health Sci J. 2011;5:253–68. [Google Scholar]
- [39].Joseph CN, Porta C, Casucci G, et al. Slow breathing improves arterial baroreflex sensitivity and decreases blood pressure in essential hypertension. Hypertension. 2005;46:714–8. [DOI] [PubMed] [Google Scholar]
- [40].Yung P, French P, Leung B. Relaxation training as complementary therapy for mild hypertension control and the implications of evidence-based medicine. Complement Ther Nurs Midwifery. 2001;7:59–65. [DOI] [PubMed] [Google Scholar]
- [41].Maloh DIA, AlNahar H, AlRahahleh W, et al. The effectiveness of Jacobson’s progressive muscle relaxation technique on fatigue among Jordanian patients with multiple sclerosis during corona epidemic. Clin Schizophr Relat Psychoses. 2022;16S:032822. [Google Scholar]