Abstract
PURPOSE
Voluntary stopping of eating and drinking (VSED) is a controversial method to hasten death. Little is known about why and how people come to VSED. This study assessed patients’ motives, how patients decide on VSED, and the ways in which they prepare for VSED and involve others.
METHODS
We conducted a qualitative study in the Netherlands of 29 patients; 24 started VSED and 19 died. Thirteen patients were included before or during VSED and 16 afterward. We interviewed 17 patients, 18 relatives, and 10 professional caregivers. Inductive ideal-type analysis was used to describe typologies.
RESULTS
Three patient groups emerged. The first group (12 patients) were older people who felt life was completed, for whom control was important. They prepared well for VSED, but could overlook the need for help and the emotional burden their decision could place on relatives. The second group (11 patients) were older care-dependent patients with a poor quality of life. They sometimes started VSED suddenly, and they relied heavily on (informal) caregivers to prepare and execute their plan. The third group (6 patients) were psychiatric patients with a long-standing but fluctuating death wish, most of whom were younger. They often prepared for VSED in secrecy or started VSED unprepared.
CONCLUSIONS
Patients embarking on a trajectory toward VSED are a very diverse group, with different care needs. Guidance for care during VSED needs to be applicable to all 3 groups.
Key words: voluntarily stopping eating and drinking; VSED; palliative care; pain; suffering; death; aged; aged, 80 and over; elderly; geriatrics; psychiatric illness; end of life; physician-assisted suicide; euthanasia; ethics; primary care
INTRODUCTION
Physicians around the world are confronted with patients who want to hasten death by voluntary stopping of eating and drinking (VSED). Studies showed that 46% of Dutch general practitioners (GPs) and 43% of Swiss GPs provide care to patients during VSED in their career.1,2 In Oregon, 41% of hospice nurses have experience with VSED.3 Studies from the Netherlands and Switzerland estimated 0.5% to 2.1% of people who die do so by VSED.4-6
Patients do not need approval by their physician, or others, to start VSED. With adequate care, VSED can lead to a relatively comfortable death.7,8 Experts stress, however, the importance of involvement of professional and informal caregivers and good preparation.7,8 Some patients do not involve others in VSED.9 In former research, patients informed their GPs in a timely manner in merely 50% of VSED cases, and only a minority involved their GP (21%) or relatives (44%) before their attempt.1 Most physicians and nurses in the western world seem willing to support patients during VSED,1,3,10,11 although they can feel unease over aiding someone to hasten death.7,11-13 Relatives who provide care to a patient during VSED can feel satisfaction as well as a heavy responsibility, exhaustion, and doubts. Their experience is related to their level of acceptance of the patient’s decision.14-16
General practitioners and relatives describe patients’ motives to initiate VSED as diverse. The motives can be related to somatic, psychosocial, and existential suffering; loss of independence; loss of self; and a wish to control the end of life.5,8 Because studies involving patients are lacking, it is unknown why this group with such diverse motives to hasten death choose this method and what happens before they start VSED.17,18
This study aimed to describe why and how patients come to VSED. First, what are their motives and how do they decide on VSED? Second, how do they prepare and in what way do they involve others? Is it a homogenous patient group? To fully explore the subject, we performed a qualitative study and included the perspective of patients, relatives, and professional caregivers.17
This study took place in the Netherlands, where most end-of-life care is provided by GPs, to patients dying at home (33% of nonsudden deaths), in homes providing low-level care, and in hospices (20% of nonsudden deaths).19 Much as in the United States and other western countries, aiding a patient during VSED is legal. According to professional standards, patients are entitled to care to relieve suffering during the process.4 Caregivers can use guidance on care during VSED. In the Netherlands, physician-assisted dying (PAD) or euthanasia can be an alternative for patients with unbearable and incurable (physical or psychological) suffering; however, physicians can decline requests for PAD on personal grounds. Requests for PAD from patients with psychiatric or existential suffering are mostly declined.20
METHODS
Design
We performed a qualitative study using interviews with patients, relatives, and professional caregivers. To be included, individuals had to be (1) people who seriously considered or decided to hasten death by VSED in the near future or recent past, (2) relatives who had a close relationship with a deceased patient who attempted VSED, or (3) professional caregivers (primary treating physicians, nurses, or nursing aids) involved in VSED. When possible, we explored cases from 2 or 3 perspectives. The study protocol was reviewed by the medical ethics committee of the VU University Medical Center, Amsterdam, the Netherlands. We used the Consolidated Criteria for Reporting Qualitative Research (COREQ) for this article.21 The 3 (female) researchers are a practicing GP (E.E.B.), a former nurse and social scientist (R.P.), and a health scientist (B.D.O-P.). Two (R.P. and B.D.O-P.) are experienced qualitative researchers, and 1 (E.E.B.) completed a master’s course on qualitative research. This study followed a quantitative study on VSED that highlighted a need for more in-depth qualitative data on the practice.1
Recruitment and Sampling
Because VSED is rare, we used convenience sampling. We used various sources to recruit participants to increase validity. The sources were a website designed for the project (3 patients); the magazine, newsletter, and helpdesk of NVVE (Nederlandse Vereniging voor Vrijwillige Euthanasie, the Dutch Right-to-Die Association) (16 patients); and professional caregivers (11 patients). General practitioners with special interest in palliative care and hospice physicians were informed about the study at a conference and through personal e-mails. Professional caregivers asked eligible patients and relatives permission for the researchers to contact them. Participants received written and oral information about (the motives for) the study from the researchers before they decided to participate.
The inclusion period lasted 18 months (January 2020-June 2021). We were approached by 27 patients, 49 relatives, and 9 professional caregivers. If the patient gave consent, we invited their relative and professional caregiver to participate after death. In 2 cases, the patient was too weak to participate and their relative gave an interview on their behalf. In many cases, the patient was already deceased at recruitment. We included all of the 12 patients who had an active wish to end life, because they were expected to be the most valuable sources of information. For additional participants, we strove for maximum variation in the sample with respect to source of information, age and sex of the respondent, and source of recruitment.
Setting and Data Collection
We selected 33 cases for an interview, interviewing multiple sources per case when possible. We conducted 54 interviews with 17 patients (with multiple interviews in 6 cases), 18 relatives, 8 physicians, and 2 nurses. One-on-one interviews were conducted face to face at the participant’s chosen location (17 participants, mostly at home) or by telephone (37 participants, because of COVID-19 restrictions) by E.E.B. and R.P. A relative was present during the patient interview in only a single case (case 16). Interviews lasted 29 to 100 minutes and were audio recorded and transcribed verbatim.
Before the interviews, all 3 researchers made a topic list. After 5 interviews, they discussed and adapted the topic list; for instance, questions about burdening relatives and expectations of others were added. The topic list was used as a reminder of issues to be addressed during the semistructured interviews. The interviewer made a mind map and summary directly after the interview and expanded them after reading the interview transcript.
Data collection and data analysis were done simultaneously; new interviews were continued as long as new codes came up. When interviews no longer added new codes, data collection stopped. We excluded 4 cases from analysis because the interviewed patients had not attempted VSED and were not considering it in the near future.
Data Analysis
The data were first analyzed by the principles of inductive thematic analysis.22 Interviews were transcribed and coded using Atlas.ti 8 (Scientific Software Development GmbH). First, E.E.B. familiarized herself with the data by reading 5 interviews and keeping notes. Two interviews were coded inductively by 2 researchers (E.E.B. and R.P.) independently and then discussed by all 3 researchers. Thereafter, codes were refined and an initial coding tree was made by E.E.B. After 5 interviews, the coding tree was discussed by the 3 researchers and adjusted. Two interviews were coded by E.E.B. and R.P. using the new coding tree and discussed. The coding tree was further developed during the study, and interviews already coded were recoded using the new coding tree by E.E.B. Two researchers (R.P. and B.D.O-P.) critically judged the findings.
For this study, the research group further explored the 22 codes involving the period up to VSED and rearranged them into 4 categories: background and motive; considerations and expectations; role of others; and trajectory. In the process of analysis, 3 distinct patient groups emerged from the data, with within-group similarities and between-group differences for each of the 4 categories. From this point onward, we changed our approach to an ideal-type analysis as described by Stapley et al,23 to develop and check typologies.
On the basis of the case summaries and mind maps, and after rereading (parts of) the interviews, each patient’s story was described in a case reconstruction. Key features were systematically compared using color codes in Excel (Microsoft Corp), and the within-group similarities and differences were summarized. Next, we constructed 3 groups that shared fundamental features (ideal cases). Finally, we identified the cases best exemplifying each group (optimal cases). To check credibility, each case reconstruction was reread and outliers were identified.
RESULTS
We included in our analysis 29 cases of patients who used or contemplated VSED. Their characteristics are summarized by group in Table 1 and detailed in Table 2. Nine cases were included before VSED was initiated (of whom 4 made an attempt during the 1-year study period), 4 cases were included during VSED, and 16 cases were included after a VSED attempt. The patients’ ages ranged from 26 to 97 years.
Table 1.
Summary of Patient Characteristics for Each Group (N = 29)
| Characteristic | Group 1: VSED to Remain in Control (n = 12) | Group 2: VSED to Accelerate Natural Death (n = 11) | Group 3: VSED as a More Acceptable Suicide (n = 6) |
|---|---|---|---|
| Age at death/inclusion, median (range), y | 82 (64-93) | 92 (78-97) | 47 (26-82) |
| Sex, female, No. (%) | 5 (41.7) | 7 (63.6) | 5 (83.3) |
| Requested PAD, No. (%) | 9 (75.0) | 7 (63.6) | 5 (83.3) |
| Attempted VSED, No. (%) | 8 (66.7) | 10 (90.9) | 6 (100) |
| Died during VSED attempt, No. (%) | 8 (66.7) | 9 (81.8) | 2 (33.3) |
PAD = physician-assisted dying; VSED = voluntary stopping of eating and drinking.
Table 2.
Detailed Patient Characteristics (N = 29)
| Case No. | Recruitment | Interview Source(s) | Age Decile at Death/Inclusion, y | Sex | Timing of Inclusiona | Request for PAD? | VSED Attempt? | Time Between Attempt and First Interview | Died During Attempt? | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient | Relative | Physician | Nurse | |||||||||
| Group 1: VSED to remain in control (n = 12) | ||||||||||||
| 2 | NVVE | x | 60s | M | After | Yes | Yes | 3 Months after | Yes | |||
| 4 | NVVE | x | x | 80s | M | During | No | Yes | Day 4 of attempt | Yes | ||
| 5 | NVVE | x | x | x | 90s | M | During | Yes | Yes | Day 8 of attempt | Yes | |
| 6 | Other | x | 80s | F | After | No | Yes | 2 Years after | Yes | |||
| 7 | NVVE | x | 80s | M | Before | Yes | No | … | NA | |||
| 10 | NVVE | x | 80s | M | After | Yes | Yes | 1 Year after | Yes | |||
| 11 | NVVE | x | 70s | F | Before | Yes | No | … | NA | |||
| 13 | NVVE | x | 90s | F | After | Yes | Yes | 2 Years after | Yes | |||
| 20 | Other | x | 70s | F | After | Yes | Yes | 4 Years after | Yes | |||
| 21 | Caregiver | x | 70s | F | Before | Yes | Yes | Day 1 of attempt | Yesb | |||
| 25 | NVVE | x | 70s | M | Before | Yes | Noc | (4 Months before PAD) | NA | |||
| 27 | Caregiver | x | 70s | M | After | Yes | Yes | 3 Weeks after | Yes | |||
| Group 2: VSED to accelerate natural death (n = 11) | ||||||||||||
| 8 | NVVE | x | 90s | F | After | Yes | Yes | 8 Months after | Yes | |||
| 9 | NVVE | x | 70s | F | After | No | Yes | 8 Years after | No | |||
| 12 | NVVE | x | 80s | F | After | Yes | Yes | 15 Months after | Yes | |||
| 14 | Caregiver | x | x | x | 90s | F | During | Yes | Yes | Day 1 of attempt | Yes | |
| 15 | Internet | x | x | 80s | F | Before | Yes | Yes | 4 Months before | Yes | ||
| 17 | NVVE | x | 90s | M | After | No | Yes | 10 Months after | Yes | |||
| 18 | Caregiver | x | x | 90s | M | After | No | Yes | 7 Days after | Yes | ||
| 19 | Other | x | 90s | F | After | Yes | Yes | 2 Years after | Yes | |||
| 24 | NVVE | x | 80s | M | Before | Yes | No | … | NA | |||
| 28 | Internet | x | 90s | M | After | Yes | Yes | 4 Months after | Yes | |||
| 29 | Caregiver | x | x | x | 80s | F | Before | No | Yes | Day 9 of attempt | Yes | |
| Group 3: VSED as a more acceptable suicide (n = 6) | ||||||||||||
| 1 | Caregiver | x | x | x | 60s | F | During | Yes | Yes | 2 Days before | Yes | |
| 3 | Other | x | 20s | F | After | Yes | Yes | 4 Days after ending VSED | No | |||
| 16 | NVVE | x | 80s | M | After | No | Yes | 9 Years after | Nob | |||
| 22 | NVVE | x | 30s | F | Before | Yes | No | … | NA | |||
| 23 | NVVE | x | 40s | F | After | No | Yes | 17 Months after | No | |||
| 26 | Internet | x | 30s | F | Before | Yes | Yes | 2 Months before | No | |||
F = female; M = male; NA = not applicable because VSED was not attempted; NVVE = Nederlandse Vereniging voor Vrijwillige Euthanasie (the Dutch Right-to-Die Association); PAD = physician-assisted dying; VSED = voluntary stopping of eating and drinking.
Relative to VSED attempt.
Died by suicide (ingestion of lethal substances).
Died by PAD.
Patient Groups
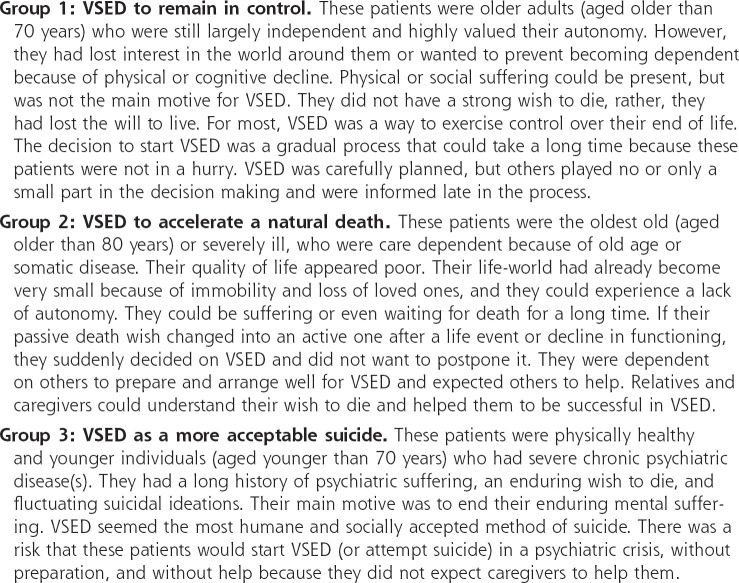
Through ideal-case analysis, we identified 3 groups of patients, each with similar background and motive, considerations and expectations, roles of others, and trajectories: those using VSED to remain in control (group 1), those using it to accelerate a natural death (group 2), and those using it as a more acceptable suicide (group 3). Figure 1 gives narrative descriptions of each group, and Figures 2, 3, and 4 present the cases that best exemplify each group (optimal cases). We discuss each group in detail below, noting supporting quotes from interviews that are given in Table 3.
Figure 1.
Narrative descriptions of the 3 groups.
VSED = voluntary stopping of eating and drinking.
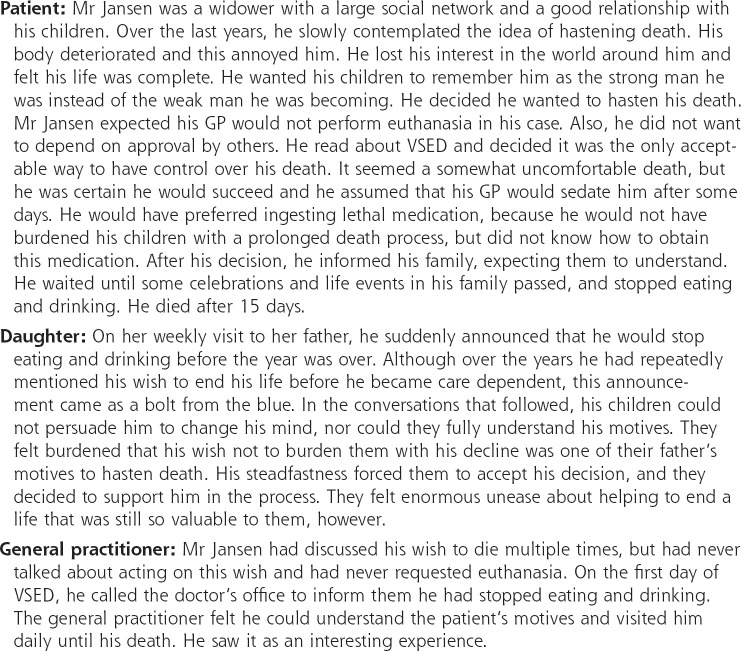
Figure 2.
Optimal case of VSED to remain in control: Mr Jansen, a man in his 90s (case 5).
VSED = voluntary stopping of eating and drinking.
Figure 3.
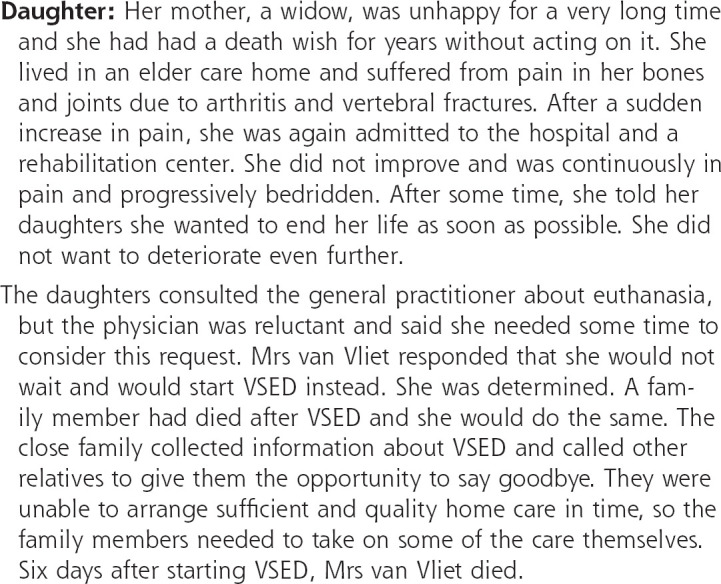
Optimal case of VSED to accelerate a natural death: Mrs van Vliet, a woman in her 80s (case 12).
VSED = voluntary stopping of eating and drinking.
Figure 4.
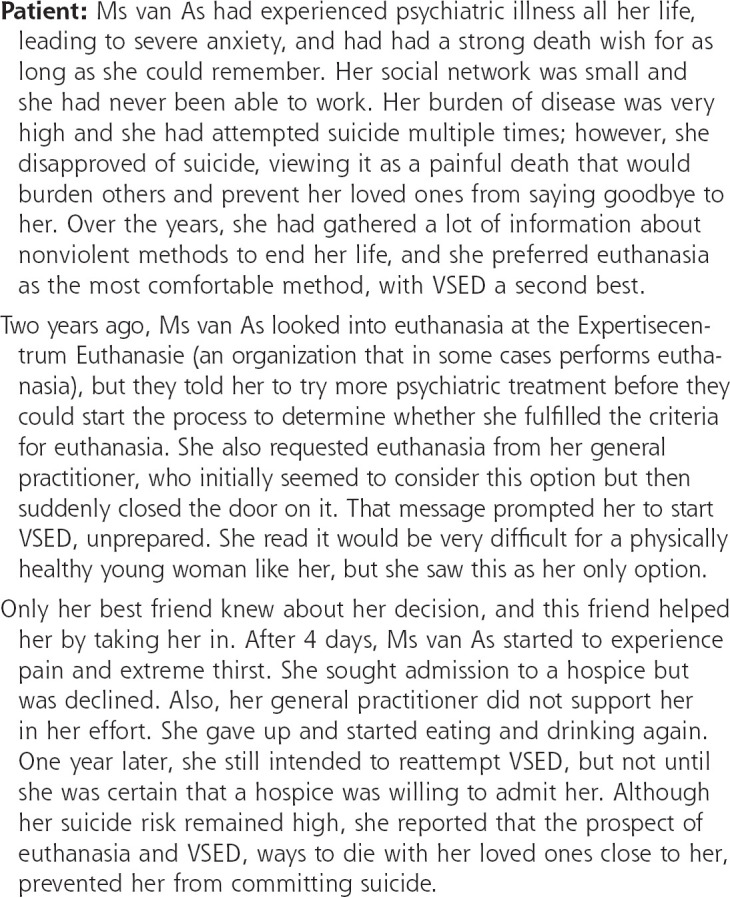
Optimal case of VSED as a more acceptable suicide: Ms van As, a woman in her 20s (case 3).
VSED = voluntary stopping of eating and drinking.
Table 3.
Quotes From Participants in Each Group, by Theme
| Theme | Group 1: VSED to Remain in Control | Group 2: VSED to Accelerate a Natural Death | Group 3: VSED as a More Acceptable Suicide |
|---|---|---|---|
| Background and motive | 1.1. I’m done with it, I’m throwing in the towel. I’m 73. I’ve had a good life. I don’t really feel like having to spend a few years somewhere sitting and watching the credits to what’s been a beautiful film. (case 25, patient) 1.2. My life is beautiful. But I’d rather leave. So that my children will remember a father who is still the father they know. Always a strong man who can do everything, instead of someone who is wasting away.... (case 5, patient) 1.3. During my life, I have always been in control over everything. And that’s exactly what I want at the end of life. (case 11, patient) 1.4 [It is important to me] to remain the same person, and not to wither away. I’ve seen that happening too many times, and I don’t need that. You wither away and you no longer are allowed to decide whether you want to live or die. (case 21, patient) |
2.1. She can’t do her make-up anymore, she can’t style her hair anymore 舢.that deterioration is awful for her. No longer being able to do anything. She can’t write anymore. She loved shopping but that’s no longer possible, or maybe for a little while every now and then. Other than that, she doesn’t really have anything left. (case 15, relative) 2.2. For years my mother has been thinking she wouldn’t mind if it was all over tomorrow. Her health is really bad all the time, so much so that we keep thinking it’s over, and every time she still manages to recover. (case 12, daughter) |
3.1. It’s not that I don’t want to live, it’s that I can’t live. (case 3, patient) 3.2. I haven’t wanted to keep on living for a very long time. Quite a long time, and that thought just became stronger and stronger. (case 23, patient) |
| Considerations and preparations | 1.5. That’s why this method appealed to me: you can do it yourself and aren’t dependent and you don’t have to ask anyone anything. (case 4, patient) 1.6. I also saw how you could collect medicines, you know, but I find that such a hassle. You’re dependent on having to get them, or should you lie? ... And then I think to myself, [in VSED] I’m completely in control here. (case 11, patient) 1.7. I feel like stopping eating and drinking gives you the opportunity to work through a process. A winding-down process. Living with the end in sight, in 1 week or 2. And I can’t prove it, because I’ve not yet experienced it, but I think it’s a good thing. (case 7, patient) 1.8. I can manage that. ... If I’m doing something, then I’ll do it. Then I’m fully behind it. And of course it’s not a spur-of-the-moment thing. (case 25, patient) 1.9. [What you need is] perseverance. And a few people around them who come and check up on them every now and then. (case 5, patient) 1.10. He was so adamant about that: It takes 4 days and then it’s over. And by God I don’t know where he got those 4 days from, but it was so forceful that we all, including him, thought “This takes 4 days.” That wasn’t true. ... And I had an image in my head, from the stories about an Indian sitting down leaning against a tree and his soul flying out. I think I had a bit of a romantic image. (case 6, daughter) |
2.3. She wanted euthanasia. But every time the doctor visited her, she didn’t give a clear signal that she was really ready for euthanasia. She always gave the impression that she was enjoying the small things in life. (case 19, relative) 2.4. He said: “If I don’t get euthanasia, if I don’t get an injection, then this is an option that I still find acceptable and dignified.” (case 28, daughter) 2.5. Her expectations were, because that is what we read, that after 2 days a moment of happiness would arise, and then you calm down and softly fade into unconsciousness. (case 29, daughter) 2.6. At that moment, I don’t think she’d thought further about whether she’d be able to stick with it, she just wanted for it to be over, the end. (case 8, relative) 2.7. She made her announcement very late, so we had to take care of everything in very short order. So yeah, there’s a whole situation first. For us, the hardest thing was that you couldn’t find good home care services at that time. (case 12, daughter) |
3.3. Euthanasia ... in my view that’s still the most humane way. ... I wanted to go back to the end-of-life clinic [for euthanasia], but then I’d have to go back on the waiting list, which is very long. (case 3, patient) 3.4. (About suicide using medicines): My body gets taken over, there’s a lot of hassle, and the family I have, the police, the nurse who gets a shock when she finds me... I just want to do it properly. (case 1, patient) 3.5. Because I’m young, and physically there’s nothing really wrong with me, I’m scared it will take too long. Not the usual average of 2 weeks. But I’m also very scared of delirium. (case 3, patient) |
| Role of others | 1.11. [He said,] “I have a plan and this is what I’m going to do and this is what I’m expecting from you and this is how we’ll do it.” And that’s exactly what he did. (case 4, GP) 1.12. He was very clear, he said there’s no room for discussion. ... “This is my decision.” But he really was willing to explain it to all his children and grandchildren. (case 6, daughter) 1.13. [We said,] “Why are you doing this? There’s nothing wrong with you, you’re healthy!” You try everything to persuade him. ... There’s nothing that convinced us he had to take this step. At some point, my sister and I resigned ourselves to it, because we were fighting a losing battle. But my brother dug his heels in until the very last moment. (case 5, son) |
2.8. Then the doctor came up with the fact that you can also just stop eating and drinking, because that’s not a bad way to go. (case 15, relative) 2.9. We told her, “Mom, if this is what you want, we will be there for you. We will get over this, don’t worry about that.” Because she said, “I don’t want to do this alone, I want to do this together with you.” (case 29, daughter) 2.10. Bizarre. Well, who decides [whether you are eligible for euthanasia]? We were quite annoyed by it. You’ve already been through a lot and then you get that on top of it all. Isn’t it bad enough? Who decides how much someone is suffering and when it’s done? (case 14, daughter) |
3.6. It was around 8 o’clock; he came home and said, “I don’t need dinner, I’m going straight to bed, I’m tired.” For 4 days I didn’t realize that he wasn’t eating or drinking. (case 16, partner) 3.7. [The carers] were also given the freedom to refuse to be involved, but to the great surprise of the head of care they said unanimously that they refused. (case 1, GP) 3.8. I thought I’m not going to drag people into this, they’re not going to support me ... no one is going to support me in this. ... Because I’m too young and because they think I’m going to get better. (case 26, patient) 3.9. The plan was to gradually eat and drink less and lose weight. And then to stop altogether. But the psychiatrist said, if you do that I will have you admitted. So they throw bombs on your plan. (case 22, patient) 3.10. It’s been a whole process to get to the point where I wasn’t trying to stop him anymore, ... it’s been hard to be able to finally say, “I’m with you from now on.” (case 16, partner) |
| Trajectory | 1.14. December, I didn’t think that was a good month to say goodbye because of the Saint Nicholas festivities. ... So I thought January would be a good month. When I had a business, that was the month for clearing up. (case 4, patient) 1.15. Now I’m going to take control. But when you have nobody, you have to arrange things very well. But it doesn’t have to be done on the spot either. (case 11, patient) |
2.11. It’s a battle with myself. On the one hand, I think it’s ... well cowardly to end it, and on the other hand there’s that huge pain where you say, well folks, I’m very sorry, but now I’m going to do what’s right for me. It’s a constant dilemma. (case 24, patient) 2.12. One day, he was sitting at the dinner table, downstairs in the dining hall (of the elderly care home) ..., and he pushed away his plate and said he wanted to go back upstairs. They brought him back to his room and called me [to tell me] that he had stopped eating and drinking. (case 17, relative) 2.13. To everyone’s surprise, she was doing much better [she recovered from a heart attack] ... R. [patient] then immediately says, “Well, but I want to die, give me a shot or whatever.” “No ma’am, this is a hospital, and we don’t do euthanasia in hospitals.” I understand that R. has had a big discussion with the doctor and the nursing staff, saying she wanted to die. And at some point she said, “Then I’ll stop eating and drinking.” (case 8, relative) |
3.11. I really thought oh, I don’t want to go through another winter. Not another ... well, eventually you just keep going or something. (case 23, patient) 3.12. That was in a psychiatric crisis. ... I felt a lot of turmoil inside, about wanting to end it all, and I was somehow trying to stay in control, well then I’d do it this way ... so that I can still say goodbye. (case 26, patient) 3.13. Especially because my GP supports me, my family supports me. Then I don’t really need to commit suicide so to speak. It’s a good source of strength for me. (case 23, patient) |
GP = general practitioner; PAD = physician-assisted dying; VSED = voluntary stopping of eating and drinking.
Group 1: VSED to Remain in Control
Background and motive. The first group consisted of 12 cases, of whom 6 died before study inclusion and 3 died after inclusion. For this group, VSED was a method to maintain a sense of control over life and/or death. These cases were characterized by the absence of severe physical and mental suffering, and the absence of a strong death wish (Table 3, quote 1.1). Participants described physical discomforts related to old age and loss of loved ones, but the main reason they wanted to end their lives was to prevent physical or cognitive decline and loss of independence (quote 1.2). They felt they were already losing parts of their identity: they reported feeling disconnected from the world and a loss of interest in others, describing this interest as an integral part of their identity. Typically, these patients were used to being in charge and wanted to exercise control over their own death (quotes 1.3 and 1.4).
Considerations and expectations. All of the patients in this group had considered PAD and some had discussed it with their GP, but most discarded it as an option. They assumed it was not within reach, and some did not want to depend on, or burden, their physician (Table 3, quote 1.5). Some considered collecting medicine but found it too risky, or discarded it because they did not want to hide their actions (quote 1.6).
Although most preferred a faster and easier death, VSED seemed the most autonomous method. A few patients saw it as an interesting venture or a final challenge, or preferred VSED over PAD as a more gradual and natural death (Table 3, quote 1.7). Patients in this group expected that VSED would not be easy, but were confident that they would succeed (quote 1.8). They did not expect to need much help, and would get help if needed (quote 1.9). Some relatives described afterward how VSED turned out to be harder and lengthier than expected (quote 1.10).
Role of others. Patients in this group rarely included others in their decision making. Most did not inform relatives and caregivers until they had made up their minds and had prepared for VSED by themselves (Table 3, quote 1.11). Relatives could be shocked by the news and have a hard time understanding how the patient came to this decision. The patients were open about their motives (quote 1.12). Both interviewed patients and interviewed relatives described how some relatives tried to talk the patient out of VSED but were unable to do so (quote 1.13).
Trajectory. Patients described their decision making as a gradual process. It started with a growing dread of losing independence, leading to the intention to take matters into their own hands. Patients took their time, and some studiously explored different options to hasten death.
For those who initiated VSED, there was no identifiable trigger for doing so. Rather, patients described how the balance between positive and negative aspects of life had slowly tipped toward the negative. They took a practical approach to planning initiation of VSED, starting after the holiday season or after a family celebration (Table 3, quote 1.14).
Patients took time to prepare. All but 2 prepared well for VSED and their death, and over a longer period of time (Table 3, quote 1.15), and all who started died (although one ultimately died by ingesting lethal substances). Three patients did not start VSED during our 1-year follow-up: 1 died after PAD, 1 was waiting for her cat to die first, and 1 could not say if and when he would want VSED.
Group 2: VSED to Accelerate a Natural Death
Background and motive. The second group consisted of 11 patients who were care dependent because of old age and/or severe disease and had a poor life expectancy. In general, they had had a low quality of life for years. Disability and loss of relatives made their world small (Table 3, quote 2.1). As in the first group, loss of independence played an important role in their motivation to end their lives. But in contrast to the first group, who were still largely independent but feared becoming dependent, patients in this second group had already lost more of their independence than they could bear. These patients had had a passive death wish for a long time, and had been patiently waiting for death until a certain trigger activated them (quote 2.2).
Considerations and expectations. Although most patients in this group preferred PAD, they did not make a formal request, their request was denied, or the process would take too long (Table 3, quote 2.3). Patients wanted to hasten their death as soon as possible, and VSED was seen as the only option within their reach (quote 2.4). Relatives described patients with unrealistic expectations about prognosis or care (quote 2.5). They did not seem to worry about symptoms or problems during VSED (quote 2.6), and trusted their physician to relieve their suffering and their relatives to support them. These patients were described by relatives and caregivers as passive and, as a result, others (relatives and professional caregivers) took over the preparations (quote 2.7).
Role of others. These patients had a strong network of informal caregivers around them and were used to others arranging things for them. In line with this situation, they depended on their relatives and GP to gather information about methods to hasten death. Typically, the decision to start VSED was made together with (and sometimes at the suggestion of) their relative(s) and their GP (Table 3, quote 2.8).
In general, interviewed relatives saw the patients’ suffering and supported the decision (Table 3, quote 2.9). Relatives said they preferred euthanasia, however, because it seemed less burdensome for the patient. This preference could lead to friction between relatives and the physician (quote 2.10).
Trajectory. Patients in this second group had a longstanding death wish but refrained from action for a long time (Table 3, quote 2.11). Factors such as not wanting to hurt relatives or unavailability of home care could lead to postponing or abandoning the idea of VSED. Finally, almost all patients in this group attempted VSED, and all but 1 (a patient with dementia) succeeded.
In this group, patients sometimes suddenly decided not to wait any longer (Table 3, quote 2.12). This abrupt decision could be triggered by a sudden drop in quality of life due to an acute illness or a realization that death was not imminent (quote 2.13). Once they had made up their mind, relatives described how patients were suddenly impatient to initiate VSED. This could lay a heavy burden on relatives, who needed to prepare everything in little time (quote 2.7).
Group 3: VSED as a More Acceptable Suicide
Background and motive. The third group of patients was characterized by a long history of psychiatric problems. They were generally physically healthy and were often young. Because of their lifelong psychiatric problems, they had been unable to build their lives as they would have wished and had a small social network (Table 3, quote 3.1). Patients could have little confidence in professional caregivers, although some had a good relationship with their GP or mental health nurse. They had a long-standing death wish (quote 3.2).
Considerations and expectations. Like the other groups, these patients said they preferred PAD. Some of them requested PAD, but their caregiver denied the request or postponed the decision (Table 3, quote 3.3). The risk of violent suicide seemed high, especially when they were in psychiatric crisis. This patient group preferred VSED over other methods of suicide, because it seemed more morally acceptable, less painful, and less burdensome for others (quotes 3.3 and 3.4).
The younger patients in this group were warned that their physical fitness would make VSED extremely difficult and that they could expect a prolonged dying process with severe physical problems and thirst sensation (Table 3, quote 3.5). This information sometimes led to a decision not to start VSED (yet). Fear of a crisis intervention sometimes led to starting VSED in secret, but without elaborate preparation (quote 3.6). These patients occasionally backed out of their decision because of physical discomfort.
Role of others. Professional caregivers and relatives could disapprove of VSED because of the patient’s young age and a hope for improvement of the psychiatric disease, and could try to prevent the patient from initiating VSED (Table 3, quote 3.7). Some in this group kept their plan a secret because they assumed others would not be supportive (quotes 3.6 and 3.8). Some reported that professional caregivers declared they would intervene if the patient initiated VSED (quote 3.9). When the patient persisted in the death wish, however, some relatives and professional caregivers decided they would help (quote 3.10).
Trajectory. Patients in this group had a persistent death wish and had contemplated methods to hasten death for years. They often described suicide attempts in the past. Their death wish could fluctuate over time, however, and could disappear for longer periods (Table 3, quote 3.11). Some patients in this group showed signs of ambivalence of VSED to their professional caregivers and relatives, and even to the interviewer.
In 5 out of 6 cases, VSED was initiated. One of these patients, the only patient who was supported by a caregiver, died by VSED. The other 4 initiated VSED in a psychiatric crisis, without much preparation and/or without informing others or seeking help (Table 3, quote 3.12). They restarted eating and drinking after some days. They described VSED as a lonely and uncomfortable process. Some reported that they sought help during their attempt, but did not receive the care needed to continue.
This patient group often kept VSED as a back-up plan, however. Some commented that knowing they could hasten death by VSED with help from their relatives and/or physician gave them the strength to keep on going and try another treatment. In this way, the availability of VSED as an option prevented these patients from attempting violent suicides (Table 3, quote 3.13).
Differences and Similarities Between Groups
The 3 groups differed in ways beyond patient demographic and clinical characteristics. The VSED decision-making process ranged from last-minute decisions in response to a trigger (in the second and third groups) to trajectories that were spread out over years (in the first group). Preparations, too, could be spread out over years (first group), be a rush job for caregivers (second group), or be absent in patients who started unprepared (third group). Relatives could be closely involved in the trajectory toward VSED (second group). But involvement was minimal when patients saw no role for relatives (first group) or expected no support (third group).
The groups also had similarities. In all groups, most patients preferred PAD over VSED. Also, patients described VSED as a better, more morally acceptable method to hasten death than ingesting drugs or other methods of suicide.
Some patients had characteristics of multiple groups. For instance, case 1 (third group) had both physical ailments and psychiatric problems. The former made the patient care dependent, whereas the latter was the reason for her death wish. During preparation, she relied heavily on others and trusted others to take care of her, as is described in the second group. Others, however, could not understand her death wish coming from psychiatric suffering, which led to many problems before and during VSED. Case 23 had chronic psychiatric disease, but she started VSED well prepared and out of a wish to retain control, so she fit in the first group. During the process of VSED, however, she described a growing distrust between her and her caregivers, and she committed suicide by ingesting lethal substances (much like patients in the third group).
DISCUSSION
Major Findings
Our study shows that patients considering and/or using VSED are diverse, but we were able to distinguish 3 groups in our patient population. The group seeking to retain control consists of older people who highly value autonomy, a group that is quite visible in the Netherlands as an advocacy group.24,25 The 2 other groups identified in this study are less well represented in the debate on self-termination of life.26 These are (very) old patients who are in poor health and care dependent, and often younger patients with severe psychiatric suffering. These groups seem less well equipped to prepare well for VSED; they likely need the most guidance before and during the process.
Comparison With Existing Literature
Similar to our study, studies among caregivers and relatives have shown that existential and psychosocial suffering are important reasons for VSED.1,6 We are not the first to describe the need to approach VSED as a diverse phenomenon. Stängle et al9 described different types of VSED. They saw concealed VSED in patients who initiated the process in secret because of objections from caregivers, and implicit VSED in patients who reduced food and fluid intake but did not openly state a wish to die.9 We found concealed VSED in our third group, albeit only in cases with psychiatric suffering. We did not come across implicit VSED, possibly because this was not recognized as VSED.
Because we included patients with unsuccessful VSED attempts and even some who never initiated VSED, our sample captured patients who were not included in many previous studies.1,3,4,6,20 In particular, these were often young psychiatric patients.1,6 A Dutch study among people preparing for and seeking demedicalized assistance in suicide (for instance by VSED) included some psychiatric patients.27
VSED in Relation to PAD and Other Methods to Hasten Death
An important similarity across most patients in all 3 groups was the preference for PAD. Only patients in the first group described preferring VSED over PAD. In previous studies, 19% to 49% of patients who died by VSED had requested PAD before they started VSED.1,4,5,20 Our study, as well as the study by Hagens et al,27 indicates that the number of patients preferring PAD is higher. Interestingly, in cases in which we included multiple perspectives, patients or relatives sometimes said that they requested PAD from their GP, but the involved GPs could not remember this request. Possibly, the request for PAD was done more implicitly, or these patients assumed their request would be denied and therefore did not formally make the request.27 This can be especially true for patients with psychiatric or existential suffering, who are least likely to have their request for PAD granted.28-30
In our study, patients with psychiatric suffering often did not succeed in VSED. Explanations found included impulsiveness associated with their disease, a lack of support in their small social network, and objections by professional caregivers. As a result, these patients undertook lonely and poorly prepared VSED attempts. If psychiatric patients with a strong death wish assume they cannot obtain assistance in dying both by PAD and by VSED, they may see no other option than committing suicide by less humane options, such as ingesting lethal substances or using violent methods. In this study, patients described how knowing that VSED was an option helped them to continue living. The same was seen in patients who requested PAD in a study by Pronk et al.31 In their study, however, a request for PAD was sometimes a cry for help, and the same could be true for psychiatric patients who ask for assistance with VSED.
Strengths and Limitations
This study is the first to describe how patients come to VSED, detailing 3 different patient groups. Reducing the patients into 3 groups is a simplification of reality, however, and some patients had characteristics that fit in more than 1 group.
Although we tried to obtain maximum variation, it is possible that we failed to include certain types of patients. Most patients and relatives were recruited via the NVVE (the Dutch Right-to-Die Association). Although this association is large, having 170,000 members, members are more likely than the general population to have overthought their death and methods to hasten death. We therefore put extra effort into recruiting patients via hospices and GPs to find unprepared and younger patients. In all 3 groups, we succeeded in recruiting participants through different sources. Still, we found few patients who stopped eating and drinking without help. It is possible that for these patients, the trajectory toward VSED looks different from the trajectories described in this study. Although we included some cases in which patients were less well prepared by interviewing relatives after the patient’s death, there is a risk of recall bias in these cases because years could have passed between VSED and the interview.
By interviewing some patients at different time points, we were able to better understand the decision-making process. We explored the trajectories toward VSED from the perspective of patients, relatives, and professional caregivers to include a larger variety of cases and gain a more complete picture. In 16 cases, however, the patient perspective was missing. We saw many similarities between the interviews of the patient and of their relatives and caregivers, but there were also inconsistencies. For instance, some patients said that their relatives understood their decision, whereas interviewed relatives said this was not the case.
Although our study took place in the Netherlands, these findings are interesting for readers from other countries as well. Voluntarily stopping eating and drinking may be an even more important topic in countries where PAD is not a legal option. The Netherlands is unique because clinical guidance on VSED is available, published by the Royal Dutch Medical Association and the Dutch Nurses’ Association.7 Although not all professional caregivers are familiar with this guidance, care for patients undertaking VSED in the Netherlands may be better organized than that in other countries.
Practical Implications
Our study illustrates the diversity of patients considering VSED. It is likely that the 3 patient groups have different care needs. We recommend future research to focus on these care needs, as well as the needs of relatives because they can experience a large burden during and after VSED.15,16 These studies could add to the knowledge base needed for clinical guidance for professional caregivers.
There is an increasing call for clinical guidelines for professional caregivers in different countries, similar to the Dutch and American guidelines.7,32-34 In our study, we found a need for guidance among patients and relatives as well. It is important that professional and patient guidelines apply to the full spectrum of patients considering VSED. In overview articles, patients pursuing VSED are described to be mostly old and in poor health (based on quantitative studies, from the perspective of caregivers).18,35 Our study shows that this description does not fit all patients. Moreover, the decision-making and preparatory processes differ distinctly for the different groups of patients. These differences call for a personalized approach to patients considering and initiating VSED.
Acknowledgments
We would like to thank all study participants for sharing their personal stories with us.
Footnotes
Conflicts of interest: authors report none.
Funding support: This study was funded by a grant from the Dutch Research Agenda (NWA), issued by the Dutch Research Council (NWO).
Disclaimer: The views expressed are solely those of the respondents and do not necessarily represent official views of the authors’ affiliated institutions or funder.
Previous presentations: The results of this study were presented as a poster presentation at the NHG wetenschapsdag (Dutch College of General Practitioners Science Day) June 10, 2022, Leiden, The Netherlands (title: Hoe besluiten mensen bewust te stoppen met eten en drinken?/How Do People Consciously Decide to Stop Eating and Drinking?). The results were also presented as a poster presentation at the European Association for Palliative Care 18th World Congress on June 17, 2023, Rotterdam, The Netherlands (title: How Do People Decide to Stop Eating and Drinking to Hasten Death? A Qualitative Interview Study).
References
- 1.Bolt EE, Hagens M, Willems D, Onwuteaka-Philipsen BD.. Primary care patients hastening death by voluntarily stopping eating and drinking. Ann Fam Med. 2015; 13(5): 421-428. 10.1370/afm.1814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stängle S, Schnepp W, Büche D, Häuptle C, Fringer A.. Family physicians’ perspective on voluntary stopping of eating and drinking: a cross-sectional study. J Int Med Res. 2020; 48(8): 300060520936069. 10.1177/0300060520936069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ganzini L, Goy ER, Miller LL, Harvath TA, Jackson A, Delorit MA.. Nurses’ experiences with hospice patients who refuse food and fluids to hasten death. N Engl J Med. 2003; 349(4): 359-365. 10.1056/NEJMsa035086 [DOI] [PubMed] [Google Scholar]
- 4.Hagens M, Pasman HRW, van der Heide A, Onwuteaka-Philipsen BD.. Intentionally ending one’s own life in the presence or absence of a medical condition: a nationwide mortality follow-back study. SSM Popul Health. 2021; 15: 100871. 10.1016/j.ssmph.2021.100871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stängle S, Schnepp W, Büche D, Fringer A.. Voluntary stopping of eating and drinking in Swiss outpatient care. J GeroPsych Geriatric Psy (Bern). 2021; 34(2): 73-81. 10.1024/1662-9647/a000249 [DOI] [Google Scholar]
- 6.Chabot BE, Goedhart A.. A survey of self-directed dying attended by proxies in the Dutch population. Soc Sci Med. 2009; 68(10): 1745-1751. 10.1016/j.socscimed.2009.03.005 [DOI] [PubMed] [Google Scholar]
- 7.KNMG Royal Dutch Medical Association and V&VN Dutch Nurses’ Association . Caring for people who consciously choose not to eat and drink so as to hasten the end of life. Published 2014. Accessed Aug 4, 2023. https://docplayer.net/10054859-Caring-for-people-who-consciously-choose-not-to-eat-and-drink-so-as-to-hasten-the-end-of-life.html
- 8.Quill TE, Ganzini L, Truog RD, Pope TM.. Voluntarily stopping eating and drinking among patients with serious advanced illness-clinical, ethical, and legal aspects. JAMA Intern Med. 2018; 178(1): 123-127. 10.1001/jamainternmed.2017.6307 [DOI] [PubMed] [Google Scholar]
- 9.Stängle S, Schnepp W, Fringer A.. The need to distinguish between different forms of oral nutrition refusal and different forms of voluntary stopping of eating and drinking. Palliat Care Soc Pract. 2019; 13: 1178224219875738. 10.1177/1178224219875738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stängle S, Schnepp W, Büche D, Fringer A.. Long-term care nurses’ attitudes and the incidence of voluntary stopping of eating and drinking: a cross-sectional study. J Adv Nurs. 2020; 76(2): 526-534. 10.1111/jan.14249 [DOI] [PubMed] [Google Scholar]
- 11.Harvath TA, Miller LL, Goy E, Jackson A, Delorit M, Ganzini L.. Voluntary refusal of food and fluids: attitudes of Oregon hospice nurses and social workers. Int J Palliat Nurs. 2004; 10(5): 236-241, discussion 242-243. 10.12968/ijpn.2004.10.5.13072 [DOI] [PubMed] [Google Scholar]
- 12.Koopmans RTCM, Sindram IP, Dekkers WJM.. Bewust weigeren van vocht en voedsel in een verpleeghuis om te overlijden: een zaak voor dokter en patiënt? [Conscious refusal of food and fluids by Dutch nursing home patients in order to hasten death: a matter regarding patient and physician?]. Ned Tijdschr Geneeskd. 2004; 148(11): 536-539. [PubMed] [Google Scholar]
- 13.Koopmans RTCM, Dekkers WJ.. Versterven bij een psychiatrische patiënt: hindernissen voor patiënt, familie en behandelteam. [Refusal of food and fluids of a psychiatric patient in order to hasten death: obstacles for patient, family and care-team]. Tijdschr Gerontol Geriatr. 2012; 43(2): 98-102. [DOI] [PubMed] [Google Scholar]
- 14.Lowers J, Hughes S, Preston N.. Experience of caregivers supporting a patient through voluntarily stopping eating and drinking. J Palliat Med. 2021; 24(3): 376-381. 10.1089/jpm.2020.0223 [DOI] [PubMed] [Google Scholar]
- 15.Lowers J, Scardaville M, Hughes S, Preston NJ.. Comparison of the experience of caregiving at end of life or in hastened death: a narrative synthesis review. BMC Palliat Care. 2020; 19(1): 154. 10.1186/s12904-020-00660-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eppel-Meichlinger J, Stängle S, Mayer H, Fringer A.. Family caregivers’ advocacy in voluntary stopping of eating and drinking: a holistic multiple case study. Nurs Open. 2022; 9(1): 624-636. 10.1002/nop2.1109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ivanović N, Büche D, Fringer A.. Voluntary stopping of eating and drinking at the end of life - a ‘systematic search and review’ giving insight into an option of hastening death in capacitated adults at the end of life. BMC Palliat Care. 2014; 13(1): 1. 10.1186/1472-684X-13-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lowers J, Hughes S, Preston NJ.. Overview of voluntarily stopping eating and drinking to hasten death. Ann Palliat Med. 2021; 10(3): 3611-3616. 10.21037/apm-19-525 [DOI] [PubMed] [Google Scholar]
- 19.PZNL, IKNL . Kerncijfers palliatieve zorg [Key figures for palliative care]. Published 2019. Accessed Aug 4, 2023. https://iknl.nl/getmedia/ec16a960-d5b9-4762-b6c2-b9f360988e03/Kerncijfers_Palliatieve_Zorg_2019_PZNL_IKNL.pdf
- 20.van der Heide A, Legemaate J, Onwuteaka-Philipsen BD, et al. Vierde evaluatie Wet toetsing levensbeëindiging op verzoek en hulp bij zelfdoding [Fourth evaluation of the Termination of Life on Request and Assisted Suicide Review Act]. Published May 30, 2023. Accessed Aug 4, 2023. https://www.rijksoverheid.nl/documenten/rapporten/2023/05/30/pg-1048101-b-vierde-evaluatie-wet-toetsing-levensbeeindiging-op-verzoek-en-hulp-bij-zelfdoding [PubMed]
- 21.Tong A, Sainsbury P, Craig J.. Consolidated Criteria for Reporting Qualitative Research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007; 19(6): 349-357. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 22.Braun V, Clarke C.. Using thematic analysis in psychology. Qual Res Psychol. 2006; 3(2): 77-101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 23.Stapley E, O’Keeffe S, Midgley N.. Developing typologies in qualitative research: the use of ideal-type analysis. Int J Qual Methods. 2022; 21. 10.1177/16094069221100633 [DOI] [Google Scholar]
- 24.van Wijngaarden E, Leget C, Goossensen A.. Ready to give up on life: the lived experience of elderly people who feel life is completed and no longer worth living. Soc Sci Med. 2015; 138: 257-264. 10.1016/j.socscimed.2015.05.015 [DOI] [PubMed] [Google Scholar]
- 25.van Wijngaarden E, Goossensen A, Leget C.. The social-political challenges behind the wish to die in older people who consider their lives to be completed and no longer worth living. J Eur Soc Policy. 2018; 28(4): 419-429. 10.1177/0958928717735064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wil UV. Burgerinitiatief Voltooid Leven [Out of Free Will. Citizens’ Initiative Completed Life]. Burgerinitiatief Voltooid Leven. Accessed Jul 21, 2023. https://uitvrijewil.nu/
- 27.Hagens M, Onwuteaka-Philipsen BD, Pasman HRW.. Trajectories to seeking demedicalised assistance in suicide: a qualitative in-depth interview study. J Med Ethics. 2017; 43(8): 543-548. 10.1136/medethics-2016-103660 [DOI] [PubMed] [Google Scholar]
- 28.Bolt EE, Snijdewind MC, Willems DL, van der Heide A, Onwuteaka-Philipsen BD.. Can physicians conceive of performing euthanasia in case of psychiatric disease, dementia or being tired of living? J Med Ethics. 2015; 41(8): 592-598. 10.1136/medethics-2014-102150 [DOI] [PubMed] [Google Scholar]
- 29.van Tol D, Rietjens J, van der Heide A.. Judgment of unbearable suffering and willingness to grant a euthanasia request by Dutch general practitioners. Health Policy. 2010; 97(2-3): 166-172. 10.1016/j.healthpol.2010.04.007 [DOI] [PubMed] [Google Scholar]
- 30.Onwuteaka-Philipsen BD, Rurup ML, Pasman HR, van der Heide A.. The last phase of life: who requests and who receives euthanasia or physician-assisted suicide? Med Care. 2010; 48(7): 596-603. 10.1097/MLR.0b013e3181dbea75 [DOI] [PubMed] [Google Scholar]
- 31.Pronk R, Willems DL, van de Vathorst S.. Feeling seen, being heard: perspectives of patients suffering from mental illness on the possibility of physician-assisted death in the Netherlands. Cult Med Psychiatry. 2022; 46(2): 475-489. 10.1007/s11013-021-09726-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stängle S, Fringer A.. Perspectives of people accompanying a person during voluntary stopping eating and drinking: a convergent mixed methods study. Ann Palliat Med. 2021; 10(2): 1994-2007. 10.21037/apm-20-1339 [DOI] [PubMed] [Google Scholar]
- 33.Compassion in Dying . Voluntarily stopping eating and drinking (VSED): a call for guidance. Published Nov 2022. Accessed Aug 4, 2023. https://compassionindying.org.uk/resource/voluntarily-stopping-eating-and-drinking-vsed/
- 34.Wechkin H, Macauley R, Menzel PT, Reagan PL, Simmers N, Quill TE.. Clinical guidelines for voluntarily stopping eating and drinking (VSED). J Pain Symptom Manage. 2023: S0885-3924(23)00565-1. 10.1016/j.jpainsymman.2023.06.016 [DOI] [PubMed] [Google Scholar]
- 35.Wax JW, An AW, Kosier N, Quill TE.. Voluntary stopping eating and drinking. J Am Geriatr Soc. 2018; 66(3): 441-445. 10.1111/jgs.15200 [DOI] [PubMed] [Google Scholar]