Abstract
Introduction and importance
Mediastinal teratoma is the most common mediastinal germ cell tumor. Mature mediastinal teratomas are infrequent and often found incidentally.
Case presentation
We report the case of a 14-year-old girl who was presented dyspnea for 2 years. A computed tomography of the chest revealed a 19 cm heterogenous right-sided anterior mediastinal mass suggesting mature teratoma. The mass compressed vital structures. The tumor was considered resectable. By hemiclamshell approach, we punctured the tumor and aspirated its contents. The tumor was totally resected en bloc with a cuff of pericardium, phrenic nerve and azygos vena. The pericardial defect was repaired using Mersilene mesh. Histopathology of the tumor revealed a mature cystic teratoma. Postoperative course was uneventful.
Clinical discussion
Complete surgical excision is the treatment of choice for mediastinal mature teratoma. The choice of incision for removing the tumor depend on the tumor size, location and the relashionships with the associated vital structures. Lengthy incisions were required for the safe mobilization of the tumor. In addition, contents aspiration through a small incision in the giant tumor wall helped improve tumor mobilization.
Conclusion
Appropriate surgical strategy for a well selected case maintains functional status and results total tumor resection.
Keywords: Case report, Giant tumor, Mediastinal tumor, Surgical resection, Teratoma
Highlights
-
•
Complete surgical excision of giant mature teratoma poses a challenge.
-
•
Careful surgical planning and approach must be customized according to the size and extent of mediastinal tumor.
-
•
Our surgical strategy of right hemiclamshell with evacuation of contents of the tumor was effective and resulted in total tumor resection in our case.
1. Introduction and importance
Mediastinal teratoma is the most common mediastinal germ cell tumor. It can be divided into mature and immature teratoma according to the degree of differenciation. Mature mediastinal teratomas represent approximately about 60 to 70 % of mediastinal germ cell tumor. It occurs most frequently in children and young adults. Usually, patients are asymptomatic, but large tumors may cause such symptoms of compression. We report here a case of successful surgical management of a giant mediastinal mature teratoma in a child. This work has been reported in line with the SCARE criteria [1].
2. Case presentation
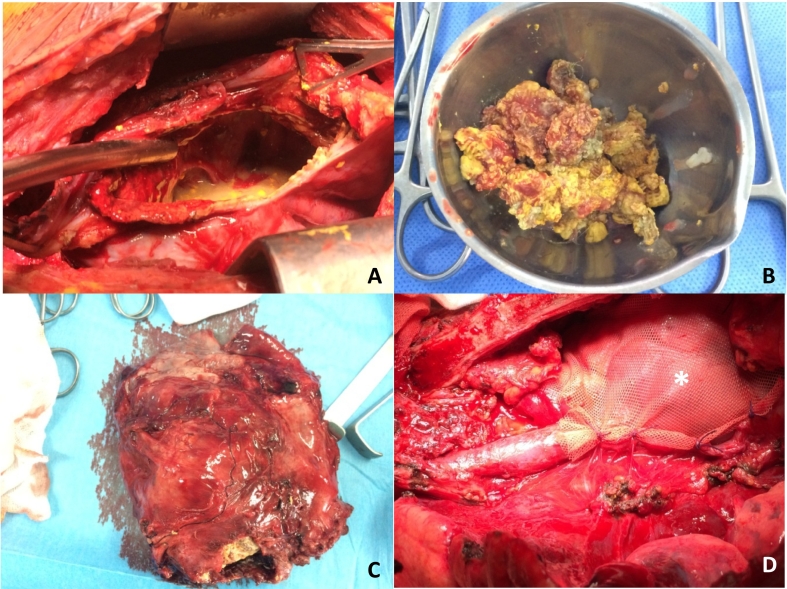
A 14-year- old girl, without comorbidities, has complained of dyspnea for 2 years was admitted to our hospital. The chest examination revealed a right parasternal swelling. The chest X-Ray has showed an homogeneous opacity occupying the middle and the lower zone of the right hemithorax (Fig. 1). A computed tomography of the chest revealed a giant heterogenous right-sided anterior mediastinal mass mesuring 16 × 13 × 19 cm. The mass contained multiple cysts with calcifications and fat, illustrating a mature teratoma which compressed the heart, the superior vena cava, the right pulmonary artery and the pulmonary vena (Fig. 2). Therefore, the tumor has been considered resectable. We have decided to extirpate the tumor by median sternotomy with right anterior thoracotomy extension (hemiclamshell approach). There were widespread adhesions between the tumor, the pericardium and the right phrenic nerve. We have punctured the tumor and we have aspirated its contents (Fig. 3A and B). The tumor was totally resected in bloc along with a cuff of pericardium, phrenic nerve and azygos vena (Fig. 3C). The right pericardial defect has been repaired with Mersilene mesh (Fig. 3D). The histopathology of the tumor revealed a mature cystic teratoma. The postoperative course was uneventful during a 7 day in hospital stay. After 24 month follow-up, the patient denied any shortness of breath, chest pain or limitation on her daily activities with a perfect chest X-Ray (Fig. 4).
Fig. 1.
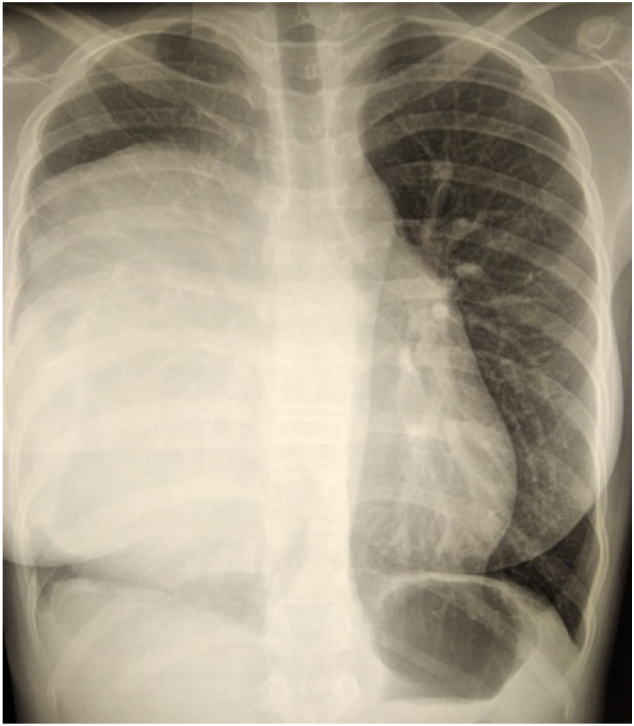
Chest X-Ray showed an homogeneous opacity occupying the middle and the lower zone of the right hemithorax.
Fig. 2.
Computed tomography of the chest revealed a giant heterogenous anterior mediastinal mass mesuring 19 cm of major axis. The mass contained multiple cysts with calcifications and fat, suggesting mature teratoma. It compressed adjacent structures.
Fig. 3.
Intraoperative photograph showing:
(A)(B) The tumor contents; (C) The resected specimen;
(D) Pericardial defect repairation using Mersilene mesh(*).
Fig. 4.

Chest X-Ray after 24 month follow-up.
3. Clinical discussion
Patients who have mediastinal teratoma are usually young and asymptomatic. The chest pain, the coughing, the dyspnea, and the arythmias are examples of such symptoms that patients with tumors compressing the surrounding structures may experience [2]. The complete surgical excision is the treatment of choice for mediastinal mature teratoma [3].
The choice of incision for removing the tumor (median sternotomy, anterolateral thoracotomy, posterolateral thoracotomy, clamshell incision or thoracoscopic surgery) depends on the tumor size, location, the relashionships between the tumor and the associated vital structures. As per the size of provided mass in our case, it has been chosen to have access mainly to the right hemiclamshell and the patient has been placed in a 3/4 position rather than the left lateral decubitus position which could have compressed the heart and resulted in circulatory collapse. These lengthy incisions were required for the safe mobilization of the tumor [4,5].
In addition, contents aspiration through a small incision of the wall related to the giant tumor was helped to improve the visualization as well as the tumor mobilization [6]. A great care shall be taken during dissection because damaging vital structures could result to fatal cardiopulmonary complications [7]. Pointing out that there are previous cases reports of surgeons evacuating cystic fluid safely proposed just prior the resection of tumor [[8], [9], [10]]. A giant mediastinal teratoma with malignant transformation is extremly rare but it is possible that accidental rupture of the mass during the surgery phase could disseminate malignant cells [6,11]. So, we have considered the evacuation of contents is an advantage to a safe extraction.
4. Conclusion
The complete surgical excision of giant mature teratoma poses a challenge tacking into account that a careful surgical planning and approach must be customized according to the size and the extent of mediastinal tumor. The extraction of benign teratoma by a large approach seems to be critical in rare cases, then evacuation of his content is well reasoned. Management of similar cases should consider our experience and make adjustments as appropriate.
Intellectual property
We confirm that we have given due consideration to the protection of intellectual property associated with this work and that there are no impediments to publication, including the timing of publication, with respect to intellectual property. In so doing we confirm that we have followed the regulations of our institutions concerning intellectual property.
Ethical approval
Ethics clearance was not necessary. It is a case report describing a surgical strategy of giant mediastinal mass.
Funding
No funding was received for this work.
Author contribution
The International Committee of Medical Journal Editors (ICMJE) recommends that authorship be based on the following four criteria:
-
1.
Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND
-
2.
Drafting the work or revising it critically for important intellectual content; AND
-
3.
Final approval of the version to be published; AND
-
4.
Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
All those designated as authors should meet all four criteria for authorship, and all who meet the four criteria should be identified as authors. For more information on authorship, please see http://www.icmje.org/recommendations/browse/roles-and-responsibilities/defining-the-role-of-authors-and-contributors.html#two.
All listed authors meet the ICMJE criteria. We attest that all authors contributed significantly to the creation of this manuscript, each having fulfilled criteria as established by the ICMJE.
We confirm that the manuscript has been read and approved by all named authors.
We confirm that the order of authors listed in the manuscript has been approved by all named authors.
Guarantor
Imen Bouassida.
Research registration number
NA.
Contact with the editorial office
The Corresponding Author declared on the title page of the manuscript is:
[Aymen Ben Ayed].
This author submitted this manuscript using his/her account in Editorial Manager.
We understand that this Corresponding Author is the sole contact for the Editorial process (including Editorial Manager and direct communications with the office). That person is responsible for communicating with the other authors about progress, submissions of revisions and final approval of proofs.
We confirm that the email address shown below is accessible by the Corresponding Author, is the address to which Corresponding Author's Editorial Manager account is linked, and has been configured to accept email from the editorial office of Advances in Ophthalmology Practice and Research:
[aymen_ben_ayed@medecinesfax.org].
Parental consent for minors
Written informed consent was obtained from the patient's parents/legal guardian for publication and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Conflict of interest statement
No conflict of interest exists.
We wish to confirm that there are no known conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome.
References
- 1.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., Thoma A., et al. The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. déc 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 2.Asteriou C., Barbetakis N., Kleontas A., Konstantinou D. Giant mediastinal teratoma presenting with paroxysmal atrial fibrillation. Interact. Cardiovasc. Thorac. Surg. 1 févr 2011;12(2):308–310. doi: 10.1510/icvts.2010.253039. [DOI] [PubMed] [Google Scholar]
- 3.Liew W.X. Mediastinal mature teratoma in a child- a case report. Med. J. Malaysia. 2016;71(1) [PubMed] [Google Scholar]
- 4.Kao C., Chou S., Huang C., Lin C., Chiang H., Lee J., et al. Salvage surgery using simultaneous clamshell thoracotomy with median sternotomy for mediastinal growing teratoma syndrome. Thoracic Cancer. mars 2020;11(3):785–788. doi: 10.1111/1759-7714.13297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marta G.M., Aigner C., Klepetko W. Inverse T incision provides improved accessibility to the upper mediastinum. J. Thorac. Cardiovasc. Surg. janv 2005;129(1):221–223. doi: 10.1016/j.jtcvs.2004.04.036. [DOI] [PubMed] [Google Scholar]
- 6.Yokoyama Y., Chen F., Date H. Surgical resection of a giant mediastinal teratoma occupying the entire left hemithorax. Gen. Thorac. Cardiovasc. Surg. avr 2014;62(4):255–257. doi: 10.1007/s11748-013-0239-z. [DOI] [PubMed] [Google Scholar]
- 7.Zhao H., Zhu D., Zhou Q. Complete resection of a giant mediastinal teratoma occupying the entire right hemithorax in a 14-year-old boy. BMC Surg. déc 2014;14(1):56. doi: 10.1186/1471-2482-14-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miyahara R. Successful resection of large mediastinal mature cystic teratoma immediately after evacuation of fluid content. OAS. nov 2010:137. [Google Scholar]
- 9.De Castro M.A., Jr Rosemberg N.P., de Castro M.A., de Castro A.P., Wietzycoscki C., Mespaque C. Mediastinal teratoma mimicking pleural effusion chest X rays. J. Bras. Pnenumol. 2007;33:113–115. doi: 10.1590/s1806-37132007000100021. [DOI] [PubMed] [Google Scholar]
- 10.Shiomi S., Mori S., Shigemori R., Matsudaira H., Ohtsuka T. Avoidance of circulatory collapse by preoperative percutaneous drainage of tumor contents for a giant mediastinal mature cystic teratoma. Gen. Thorac. Cardiovasc. Surg. févr 2021;69(2):401–404. doi: 10.1007/s11748-020-01480-6. [DOI] [PubMed] [Google Scholar]
- 11.Abid H., Neji H., Haddar S., Ammar I., Ayadi L., Msaad S., et al. Tératome médiastinal mature avec transformation maligne spontanée. Rev. Mal. Respir. 1 mai 2013;30(5):424–428. doi: 10.1016/j.rmr.2012.11.006. [DOI] [PubMed] [Google Scholar]