Abstract
The coronavirus disease 2019 (COVID-19) pandemic has spread rapidly worldwide. To prevent its spread, mRNA-based vaccines made by Pfizer/BioNTech (BNT162b1) and Moderna (mRNA-1273) have been widely used, including in Japan. Various adverse events have been reported following the COVID-19 mRNA vaccination, with differences observed among individuals. However, analyses of the genetic background associated with the susceptibility to side effects have been limited. In the present study, we performed genome-wide association studies (GWAS) for self-reported adverse events of the COVID-19 mRNA vaccination in 4545 Japanese individuals and identified 14 associated loci. Among these, 6p21 was associated with 37.5 °C or higher fever, 38 °C or higher fever, and muscle pain. HLA allele association analysis revealed that various HLA alleles were associated with the adverse effects; HLA-DQA1*03:01 and HLA-A*11:01 were more reliably associated with the adverse effects. Our results may enable the preparation and management of adverse effects by identifying the susceptibility to these adverse events. Furthermore, we obtained valuable data that may lead to a better understanding of the mechanisms of action of the COVID-19 mRNA vaccines.
Subject terms: Genetic association study, Genetic markers
Introduction
The novel coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has spread rapidly since its emergence in December 2019 and has affected hundreds of millions of people worldwide1. The development and spread of safe and efficacious vaccines are expected to be the key to controlling the COVID-19 pandemic. According to the World Health Organization, several vaccines have been developed worldwide to prevent the spread of COVID-192. mRNA-based vaccines made by Pfizer/BioNTech (BNT162b1) and Moderna (mRNA-1273) are among the most widely used in Japan and other parts of the world. As of November 29, 2021, the Japanese government estimated that 97.2 million people had been fully vaccinated (received two doses of either vaccine) in Japan, representing 76.7% of the country’s population3.
The most common side effects reported following the COVID-19 mRNA vaccination were injection site reactions, fatigue, headache, and myalgia. These side effects are reported to be mild to moderate and last for a couple of days4. Other local and systemic side effects of the vaccination include swelling, chills, joint pain, fever, redness, itching, nausea, diarrhea, abdominal pain, rash outside the injection site, and vomiting4. Serious side effects such as mild allergic reactions and anaphylaxis are rare but have been reported5,6. Side effects are signs of a common immune response to the vaccine and vary with age, sex, and ethnicity7,8. Interestingly, an elevated risk of myocarditis following the COVID-19 mRNA vaccination was observed in males aged 12–29 years9. HLA alleles have also been reported to be associated with adverse events following the COVID-19 mRNA vaccination10,11. However, to date, the mechanism underlying the development of side effects remains unclear, and there is still a lack of reports from non-European ethnicities.
One crucial challenge is to elucidate the factors that induce adverse events in response to the COVID-19 vaccine to understand its detailed mechanism of action. In this study, we hypothesized that individual differences in response to the COVID-19 vaccine may be explained, in part, by genetic differences. Therefore, to clarify the possible mechanisms by which host genetic variations might affect the COVID-19 vaccine treatment response, a genome-wide association study (GWAS) was performed in the Japanese population.
Materials and methods
Study subjects
The data were obtained through the Japanese direct-to-consumer (DTC) genetic testing services “Genequest ALL” and “Euglena MyHealth”, which are provided by Genequest Inc. (Tokyo, Japan) and Euglena Co., Ltd. (Tokyo, Japan), respectively. We asked subjects who were aged ≥ 18 years and who gave consent to participate in the study to answer internet-based questionnaires about COVID-19 vaccine adverse events. All the participants provided written informed consent for the general use of their genetic data for research. Before participating in this study, information on the study’s aim was sent to the participants and an additional study-specific agreement was obtained by opt-in. The study was conducted in accordance with the principles of the Declaration of Helsinki. The study protocol was approved by the Ethics Committees of Genequest Inc. (IRB no. 2021-0633-4) and Tohoku University Graduate School of Medicine (IRB no. 2021-1-469).
DNA sampling, genotyping, quality control, and genotype imputation
Saliva samples were collected, stabilized, and transported using an Oragene DNA Collection Kit (DNA Genotek Inc., Ottawa, Ontario, Canada) or GeneFix Saliva DNA Collection (Cell Projects Ltd., Harrietsham, Kent, UK). Genotype analysis was performed using the Illumina Infinium Global Screening Array v1 + Customs BeadChip (Illumina, San Diego, CA, USA), which contains 704,589 markers; Infinium Global Screening Array-24 v3.0 + Customs BeadChip, which contains 655,471 markers; HumanCore-12 + Customs BeadChip, which contains 302,073 markers; HumanCore-24 + Customs BeadChip, which contains 309,725 markers; and InfiniumCore-24 + Customs BeadChip, which contains 308,500 markers. Because the analyzed single nucleotide polymorphism (SNP) sets were very different among the genotyping chips used, the subjects were divided into two groups depending on the type of genotyping chip: those analyzed using the former two chips (595,105 common markers) and those analyzed using the latter three chips (289,930 common markers). These are referred to as populations A and B, respectively. Quality control and association analysis procedures were performed separately for each cohort.
For the quality control analysis, we filtered out the SNP markers. The parameters were as follows: call rate per SNP < 0.95; Hardy–Weinberg equilibrium exact test p-value < 1 × 10−6; minor allele frequency < 0.01; SNPs not in autosomes. We also excluded subjects based on the following parameters: inconsistent sex information between the genotype and the questionnaire, call rate per subject < 0.95, closely related pairs determined using the identity-by-descent method (PI_HAT > 0.1875), and estimated non-Japanese ancestry. Quality control analyses were performed using PLINK12,13 (version 1.90b3.42) and Eigensoft14 (version 6.1.3).
Genome-wide genotype imputation was performed using a pre-phasing/imputation stepwise approach implemented in EAGLE215 (version 2.4) and Minimac316 (version 2.0.1). The imputation reference panel was 1000 Genomes Phase 317 (version 5). Variants with low imputation quality (R2 < 0.3) and minor allele frequency (< 0.05) were excluded from further analyses. Finally, we used dosage data for the common 5,930,410 variants for the GWAS in populations A and B.
Adverse events measurement
We provided internet-based questionnaires regarding the COVID-19 vaccine to the study participants. First, they were asked for the manufacturer’s name of the COVID-19 vaccine. Next, they answered questions regarding the local or systemic reactions they experienced after the first and/or second COVID-19 vaccination. The questionnaire provides 53 options of adverse events reported to occur at a frequency of 0.1% or more in the Japanese subjects18; the study participants selected all options that applied to themselves. For each listed adverse event, participants who selected an option were categorized as 'cases', while those who did not select it were categorized ‘controls’. Detailed information on the questionnaires is provided in Table S1.
Genome-wide association and meta-analysis
The association between genotype dosage and the occurrence of COVID-19 vaccine adverse events was examined using a logistic regression model under the assumption of additive genetic effects. For each population, GWAS was performed, with adjustments for age and sex, using PLINK (version 2.00a3).
We combined the statistical data from both populations using a fixed-effects model and the inverse-variance weighting method with the METAL software19 (version 2011-03-25). Variants achieving genome-wide significance (p < 5.0 × 10−8) in the meta-analysis were considered to be associated with the occurrence of COVID-19 vaccine adverse events.
HLA imputation and association analysis
HLA types for A, B, C, DPB1, DQA1, DQB1, and DRB1 were imputed using the HIBAG software20,21 with default recommendations using the HIBAG Asian reference. Posterior probabilities > 0.5 were used as genotype calls. The association between HLA type and the occurrence of COVID-19 vaccine adverse events was examined using the PyHLA software22 (version 1.0.0) with a logistic regression model under the assumption of additive genetic effects with adjustments for age and sex. We performed an HLA association analysis for each population and combined statistical data from both populations using a fixed-effects model and the inverse-variance weighting method with the METAL software19. We analyzed 95 HLA alleles at a frequency > 5%. For the multiple testing correction, HLA alleles achieving p < 5.26 × 10−4 (0.05/95) were considered to be associated with the occurrence of COVID-19 vaccine adverse events.
Results and discussion
Study subjects and the occurrence of COVID-19 vaccine adverse events
The participants’ characteristics are shown in Table 1. The population vaccinated with the mRNA-1273 vaccine was older and had a greater prevalence of females when compared to the population vaccinated with BNT162b1. This difference may be a result of the Japanese vaccination circumstances, where the BNT162b1 vaccine was approved first and administered to vaccination-priority targets such as elderly people and healthcare workers. The occurrence of adverse events following COVID-19 vaccination is shown in Table1 and Table S2. Systemic reactions were more prevalent after the 2nd vaccination dose than after the 1st dose (44% and 71% for BNT162b1 and 57% and 96% for mRNA-1273, for the 1st and 2nd doses, respectively). This is consistent with the results of previous studies8,23. Compared to the report from the Japanese Ministry of Health, Labour, and Welfare18, most of the adverse events had occurrences with a range of difference of ˂ 5%; 88% and 82% for the BNT162b1 vaccine, and 79% and 62% for the mRNA-1273 vaccine, for the 1st and 2nd dose, respectively (Table S2). The adverse event occurrences were very different between BNT162b1 1st dose, 2nd dose and mRNA-1273 1st dose, 2nd dose; the following analyses were performed after stratification by the kind of vaccine and the dose. Table S3–S6 showed that adverse events were correlated with each other and were not independent.
Table 1.
Characteristics of the subjects included in the entire present study.
| BNT162b1 vaccine | mRNA-1273 vaccine | |||
|---|---|---|---|---|
| 1st dose | 2nd dose | 1st dose | 2nd dose | |
| N | 3024 | 2554 | 1521 | 1328 |
| Female (%) | 46.30 | 45.97 | 40.30 | 40.44 |
| Age (mean ± SD) | 52.35 ± 11.54 | 53.55 ± 11.49 | 46.00 ± 11.13 | 46.50 ± 11.22 |
| Local reaction (%) | ||||
| Pain in vaccination site | 86.67 | 82.34 | 86.52 | 80.57 |
| Vaccination site becomes red | 10.35 | 13.78 | 33.99 | 37.65 |
| Swelling of vaccination site | 18.78 | 21.34 | 40.37 | 42.02 |
| Vaccination site becomes hard | 11.71 | 11.82 | 21.04 | 19.73 |
| Itching of vaccination site | 8.80 | 11.39 | 26.89 | 26.05 |
| Vaccination site becomes hot | 17.72 | 17.42 | 37.74 | 38.03 |
| Movement disorder (can’t raise the arm) at the vaccination site | 23.54 | 19.73 | 30.18 | 25.53 |
| Internal bleeding in vaccination site | 1.39 | 0.78 | 0.99 | 1.20 |
| There is nothing that applies in this | 7.28 | 9.98 | 4.01 | 8.28 |
| Systemic reaction (%) | ||||
| 37.5 degrees Celsius or higher fever | 6.58 | 36.22 | 17.75 | 83.21 |
| 38 degrees Celsius or higher fever | 1.55 | 15.94 | 5.85 | 58.81 |
| Fatigue | 24.64 | 48.83 | 35.44 | 70.86 |
| Chills (pathological) | 2.55 | 11.47 | 6.44 | 37.12 |
| Hot flash | 4.83 | 8.89 | 7.30 | 15.44 |
| Peripheral coolness (cold of hands and feet) | 0.56 | 1.33 | 0.72 | 4.74 |
| Numbness | 1.65 | 1.53 | 2.76 | 2.48 |
| Shivering | 0.20 | 1.02 | 1.12 | 4.59 |
| Dizzy | 1.72 | 2.98 | 2.10 | 5.72 |
| Headache | 11.57 | 25.29 | 15.71 | 43.37 |
| Sore throat | 0.69 | 0.74 | 0.72 | 1.96 |
| Mouth and throat discomfort | 1.09 | 1.25 | 1.18 | 2.33 |
| Back pain | 1.22 | 4.46 | 2.96 | 9.56 |
| Swelling of lymph nodes (especially neck, armpit, inguinal part) | 0.73 | 2.51 | 2.24 | 1.96 |
| Pain of lymph nodes (especially neck, armpit, inguinal part) | 1.39 | 4.03 | 3.88 | 5.87 |
| Chest pain | 0.73 | 1.10 | 1.25 | 1.20 |
| Stomach ache | 0.76 | 1.21 | 0.79 | 1.81 |
| Abdominal discomfort | 1.22 | 1.41 | 0.79 | 2.11 |
| Eye pain | 0.40 | 0.55 | 0.46 | 1.43 |
| Joint pain | 3.64 | 11.55 | 5.85 | 23.64 |
| Muscle pain | 9.95 | 12.14 | 13.54 | 19.43 |
| Musculoskeletal discomfort (such as muscle tension) | 1.55 | 3.05 | 1.84 | 3.84 |
| Limb pain | 1.06 | 1.92 | 1.05 | 3.16 |
| Limb discomfort | 0.50 | 1.17 | 0.66 | 1.96 |
| Snot | 1.06 | 0.98 | 0.99 | 1.81 |
| Stuffy nose | 0.66 | 0.55 | 0.53 | 1.20 |
| Nausea | 1.65 | 2.47 | 1.97 | 4.52 |
| Vomiting | 0.23 | 0.43 | 0.59 | 1.13 |
| Loss of appetite | 1.16 | 4.50 | 2.70 | 14.83 |
| Diarrhea | 1.92 | 2.70 | 2.17 | 3.46 |
| Loose stool | 0.83 | 1.61 | 0.72 | 1.58 |
| Constipation | 0.23 | 0.39 | 0.33 | 0.23 |
| Cough | 0.60 | 0.43 | 0.59 | 1.58 |
| Sneeze | 0.33 | 0.35 | 0.46 | 0.45 |
| Dyspnea | 0.17 | 0.04 | 0.20 | 0.38 |
| Muscle weakness | 0.33 | 0.67 | 0.13 | 1.36 |
| Stomatitis | 0.40 | 0.63 | 0.26 | 0.98 |
| Urticaria (rash that disappears within a few hours) | 0.36 | 0.63 | 0.33 | 0.60 |
| Eczema (long-term rash) | 0.17 | 0.43 | 0.72 | 0.53 |
| Blunt feeling | 0.50 | 0.51 | 0.85 | 1.43 |
| Sleepy in the daytime | 5.19 | 8.22 | 4.93 | 9.94 |
| Insomnia | 0.43 | 0.82 | 0.66 | 1.28 |
| Hyperhidrosis | 0.43 | 0.74 | 0.33 | 1.28 |
| There is nothing that applies in this | 56.35 | 29.44 | 43.26 | 4.37 |
SD, standard deviation.
Incidence of COVID-19 vaccine adverse events with respect to sex and age differences
Previous studies7,23 reported that women and younger people have a higher risk of adverse events following COVID-19 vaccination. Consistent with these studies, the present study also showed a higher risk in females (p-value < 0.05; 51% and 63% in BNT162b1, 39% and 53% in mRNA-1273, for the 1st and 2nd doses, respectively) and younger people (p-value < 0.05; 51% and 63% in BNT162b1, 31% and 41% in mRNA-1273, for the 1st and 2nd doses, respectively) (Tables S7 and S8).
GWAS for COVID-19 vaccine adverse events
We performed a GWAS for each population and a meta-analysis of the adverse events. Due to the absence of cases in either population, we were unable to perform GWAS for the following conditions: constipation at BNT162b1 1st dose, dyspnea at BNT162b1 1st and 2nd dose and mRNA-1273 1st dose, eczema at BNT162b1 1st dose, and sneeze at mRNA-1273 1st dose. We identified 14 loci associated with the adverse events in response to the COVID-19 vaccine at the genome-wide significance level (p-value < 5 × 10−8), for the 1st or 2nd dose of the BNT162b1 or mRNA-1273 vaccines (Table 2, Table S9, Figure S1). Associations between rs9266082 and higher fever and rs13279405 and chest pain were found with a p-value < 0.05, for both the BNT162b1 and mRNA-1273 vaccines. However, other variants were differentially associated with the BNT162b1 and mRNA-1273 vaccines. Two hypotheses could explain this: genetic susceptibility to adverse events may differ between the two COVID-19 mRNA vaccines or the populations may have differential statistical power because of differential sample size and adverse event occurrence. In these associated loci, 6p21 (rs551634406, rs183300, rs9266082, rs375726766, rs3135408) was associated with a 37.5 °C or higher fever, 38 °C or higher fever, and muscle pain. Since 37.5 °C or higher fever and 38 °C or higher fever were correlated (Peason correlation coefficients = 0.578, Table S4), the lead variants associated with these two adverse events, despite being different, were located in the same genetic loci.
Table 2.
Loci identified by the meta-analysis of COVID-19 vaccine adverse events.
| reaction | variant | CHR | Position | EA | NEA | EAF | dose | BNT162b1 vaccine | mRNA-1273 vaccine | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | SE | P | OR | SE | P | ||||||||
| Itching at vaccination site | rs10744866 | 12 | 110104688 | A | T | 0.37 | 1st | 0.89 | 0.12 | 0.317 | 0.55 | 0.11 | 2.42 × 10−8 |
| 2nd | 1.10 | 0.11 | 0.404 | 0.88 | 0.11 | 0.239 | |||||||
| Movement disorder at vaccination site | rs146922515 | 10 | 23658821 | CA | C | 0.43 | 1st | 1.13 | 0.07 | 0.0783 | 1.23 | 0.09 | 0.0286 |
| 2nd | 1.03 | 0.08 | 0.738 | 1.80 | 0.11 | 3.69 × 10−8 | |||||||
| Internal bleeding at vaccination site | rs1217097 | 8 | 64623330 | A | G | 0.24 | 1st | 4.12 | 0.24 | 1.79 × 10−9 | 1.11 | 0.41 | 0.797 |
| 2nd | 1.85 | 0.34 | 0.0699 | 0.25 | 0.78 | 0.0768 | |||||||
| 37.5 °C or higher fever | rs551634406 | 6 | 30965800 | (A)15TAT | A | 0.49 | 1st | 0.90 | 0.11 | 0.354 | 0.96 | 0.11 | 0.703 |
| 2nd | 0.66 | 0.07 | 1.09 × 10−9 | 0.84 | 0.12 | 0.127 | |||||||
| 37.5 °C or higher fever | rs183300 | 6 | 33526951 | C | T | 0.46 | 1st | 0.97 | 0.11 | 0.741 | 0.91 | 0.10 | 0.359 |
| 2nd | 0.66 | 0.06 | 3.39 × 10−11 | 0.82 | 0.11 | 0.0736 | |||||||
| 38 °C or higher fever | rs9266082 | 6 | 31320022 | C | T | 0.39 | 1st | 1.31 | 0.21 | 0.201 | 1.39 | 0.16 | 0.0448 |
| 2nd | 1.60 | 0.08 | 4.59 × 10−9 | 1.13 | 0.09 | 0.144 | |||||||
| 38 °C or higher fever | rs375726766 | 6 | 33335716 | C | CA | 0.36 | 1st | 1.04 | 0.23 | 0.856 | 0.90 | 0.18 | 0.556 |
| 2nd | 0.60 | 0.09 | 3.67 × 10−8 | 0.98 | 0.09 | 0.855 | |||||||
| Peripheral coolness | rs10205263 | 2 | 221076324 | C | T | 0.090 | 1st | 13.09 | 0.44 | 7.30 × 10−9 | 1.31 | 0.93 | 0.771 |
| 2nd | 3.61 | 0.41 | 0.00180 | 0.37 | 0.56 | 0.0777 | |||||||
| Dizzy | rs67053119 | 8 | 51750913 | T | A | 0.075 | 1st | 0.52 | 0.63 | 0.300 | 1.25 | 0.63 | 0.726 |
| 2nd | 0.93 | 0.38 | 0.851 | 5.84 | 0.32 | 2.94 × 10−8 | |||||||
| Chest pain | rs13279405 | 8 | 12986585 | T | C | 0.056 | 1st | 17.29 | 0.51 | 2.69 × 10−8 | 7.87 | 0.68 | 0.00225 |
| 2nd | 5.66 | 0.56 | 0.00210 | 4.38 | 1.02 | 0.146 | |||||||
| Abdominal discomfort | rs57177321 | 11 | 33988111 | T | C | 0.10 | 1st | 7.63 | 0.36 | 2.30 × 10−8 | 0.71 | 0.91 | 0.705 |
| 2nd | 1.94 | 0.50 | 0.182 | 0.43 | 0.82 | 0.301 | |||||||
| Joint pain | rs34086990 | 8 | 81791475 | A | AT | 0.19 | 1st | 0.72 | 0.31 | 0.284 | 3.78 | 0.24 | 3.94 × 10−8 |
| 2nd | 1.07 | 0.18 | 0.708 | 1.34 | 0.18 | 0.0962 | |||||||
| Muscle pain | rs3135408 | 6 | 33275013 | C | T | 0.36 | 1st | 0.82 | 0.09 | 0.0392 | 0.84 | 0.11 | 0.111 |
| 2nd | 0.56 | 0.10 | 1.13 × 10−8 | 0.88 | 0.10 | 0.222 | |||||||
| Urticaria | rs2274569 | 1 | 100435079 | C | T | 0.064 | 1st | 3.82 | 0.51 | 0.00811 | 2.94 | 0.79 | 0.170 |
| 2nd | 11.78 | 0.45 | 3.15 × 10−8 | 1.91 | 1.23 | 0.600 | |||||||
Loci that reached genome-wide significance after the meta-analysis following the 1st or 2nd dose of the BNT162b1 or mRNA-1273 vaccines. CHR, chromosome; EA, effect allele; NEA, non-effect allele; EAF, effect allele frequency in the entire our study subjects; OR, odds ratio of effect allele; SE, standard error for beta of effect allele; P, p-value.
Significant values are in bold.
The annotations of the associated variants are listed in Table 324,25. The occurrence of adverse events in response to COVID-19 vaccines was previously reported to differ among ethnicities. The prevalence of fatigue as a reaction to the BNT162b2 vaccine was 59% and 69%, and fever was 16% and 38% in European and Japanese populations, respectively8,18,23. The prevalence of fatigue as a reaction to the mRNA-1273 vaccine was 68% and 80%, and fever was 17% and 77% in European and Japanese populations, respectively8,18,23. In our study, the allele frequencies of eight out of the 14 variants (rs10744866, rs146922515, rs551634406, rs183300, rs375726766, rs13279405, rs34086990, and rs3135408) differed by more than 10% between European and Japanese populations, suggesting the possibility that a difference in genetic backgrounds may influence the occurrence of adverse events in response to COVID-19 vaccines. These loci, especially 6p21, are associated with the expression of many genes, according to the Genotype Tissue-Expression (GTEx) database25. Therefore, these genes may influence the mechanism of action of COVID-19 vaccines. HLA genes’ (HLA-B, C, DPA1) mRNA expressions differed among the genotypes of the associated loci. HLA alleles have also been associated with adverse events following COVID-19 mRNA vaccination10. HLA genes have been reported to be associated with adverse events after the administration of various vaccines26 and drugs27. Increased NOTCH4 expression in the circulating regulatory T cells of COVID-19 patients was associated with disease severity and predicted mortality28. The expression of RPS18 was previously found to increase in isolated T cells upon stimulation with the live influenza virus29. A variant in BAK1 and A haplotypes of MICB have been associated with dengue hemorrhagic fever caused by the dengue virus30,31. A variant in PSORS1C1 has been associated with severe allopurinol-induced adverse reactions32,33. Variants in HSP70, TAPBP, and WDR46 were found to be associated with aspirin-exacerbated respiratory disease34–36.
Table 3.
Allele frequency and expression quantitative trait locus (eQTL) genes of the loci associated with the COVID-19 vaccine adverse events.
| Variant | Associated reaction | Location | Allele frequency | eQTL genes | |
|---|---|---|---|---|---|
| European | Japanese | ||||
| rs10744866 | Itching at vaccination site | 12q24 | 0.20 | 0.37 | MVK, FOXN4, KCTD10 |
| rs146922515 | Movement disorder at vaccination site | 10p12 | 0.35 | 0.43 | None in GTEx |
| rs1217097 | Internal bleeding at vaccination site | 8q12 | 0.28 | 0.24 | RP11-579E24.2, LINC01289 |
| rs551634406 | 37.5 °C or higher fever | 6p21 | 1.00 | 0.49 | None in GTEx |
| rs183300 | 37.5 °C or higher fever | 6p21 | 0.65 | 0.46 | BAK1, COL11A2, DAXX, IP6K3 |
| rs9266082 | 38 °C or higher fever | 6p21 | 0.30 | 0.39 | C4B, CCHCR1, CSNK2B, HCG22, HCG27, HLA-B, HLA-C, HSPA1B, MICB, MIR6891, NOTCH4, POU5F1, PSORS1C1, PSORS1C2, RNF5, SFTA2, TCF19, USP8P1, VARS2, VWA7, WASF5P, XXbac-BPG181B23.7, XXbac-BPG248L24.12, XXbac-BPG299F13.17 |
| rs375726766 | 38 °C or higher fever | 6p21 | 0.60 | 0.36 | None in GTEx |
| rs10205263 | Peripheral coolness | 2q35 | 0.071 | 0.09 | No eQTL genes |
| rs67053119 | Dizzy | 8q11 | 0.12 | 0.075 | No eQTL genes |
| rs13279405 | Chest pain | 8p22 | 0.24 | 0.056 | No eQTL genes |
| rs57177321 | Abdominal discomfort | 11p13 | 0.072 | 0.1 | No eQTL genes |
| rs34086990 | Joint pain | 8q21 | 0.042 | 0.19 | None in GTEx |
| rs3135408 | Muscle pain | 6p21 | 0.54 | 0.36 | B3GALT4, BAK1, DAXX, HCG24, HCG25, HLA-DPA1, RGL2, RPS18, TAPBP, WDR46, ZBTB22 |
| rs2274569 | Urticaria | 1p21 | 0.076 | 0.064 | DBT, LRRC39, MFSD14A, RTCA, SASS6, SLC35A3, TRMT13 |
European allele frequency, the allele frequency of European individuals (non-Finnish) in gnomAD v2,1,1; Japanese allele frequency, allele frequency in this study; eQTL genes, Variants associated with the COVID-19 vaccine adverse events were associated with the gene expression in GTEx (p-value < 0.0005).
HLA association with the COVID-19 vaccine adverse events
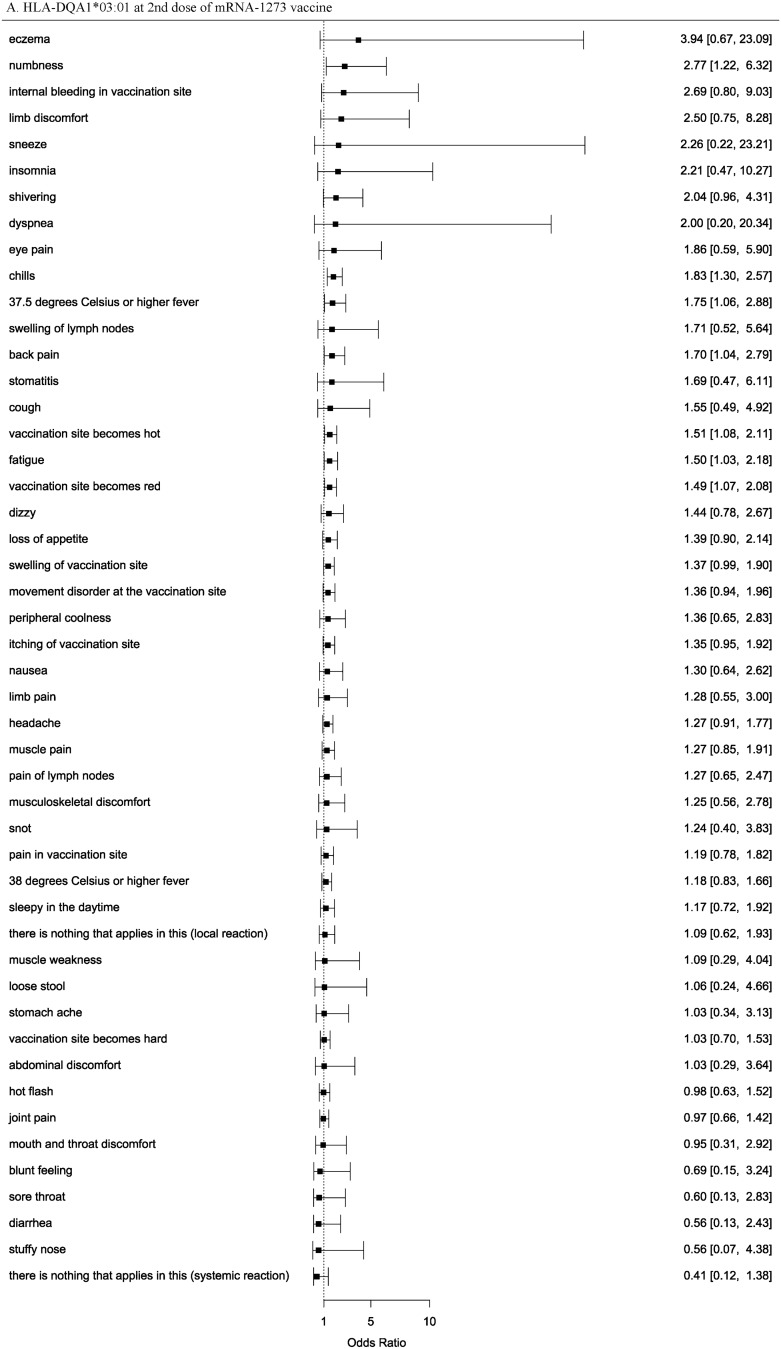
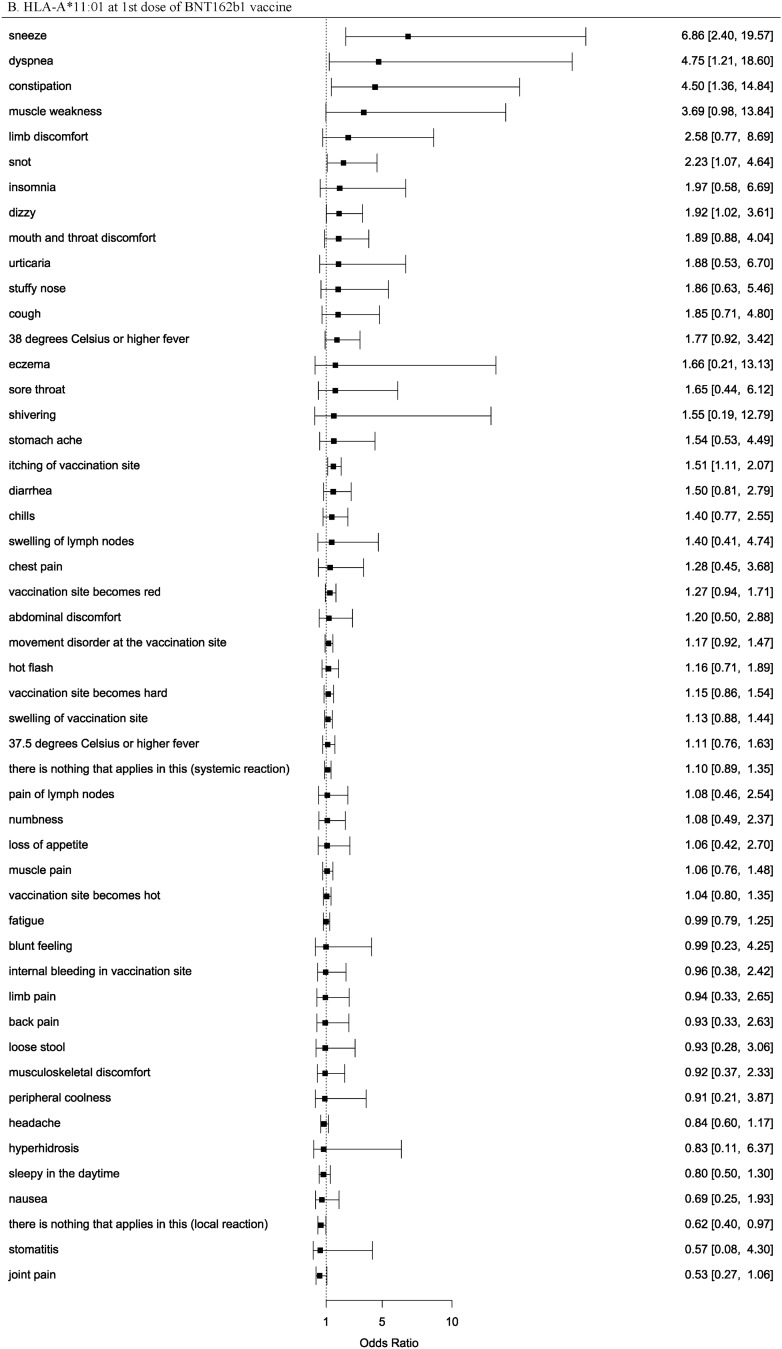
We performed an HLA imputation analysis and used high quality alleles (posterior probabilities > 0.5). The frequency of HLA alleles and sample size in our data were shown in Table S10. Subsequently, we performed an HLA association analysis of the adverse events. We identified 14 HLA alleles associated with the adverse events in response to the COVID-19 vaccine at the significance level (p-value < 5.26 × 10−4), for the 1st or 2nd dose of the BNT162b1 or mRNA-1273 vaccines (Table 4, Table S11). HLA-DQA1*03:01 was associated with chills following the 2nd dose of mRNA-1273 and BNT162b1 in our study and was also reported to be associated with the adverse events of BNT162b1 in a European study11. This allele was considered replicated and more reliably associated. However, our study did not analyze HLA-A*03:01, the top-associated allele in a European study11, because of its low allele frequency (less than 0.005). As allele frequencies are far different between ethnicities, there may have been several alleles that were significantly associated with our study but were not replicated in other ethnicities. HLA-A*11:01 was associated with sneeze following the 1st dose of BNT162b1 and mRNA-1273 in our study and was also reported to be associated with severe COVID-19 in a Japanese study37. The risk allele was shared between the adverse events of the COVID-19 vaccine and severe COVID-19, which suggests that the allele and COVID-19 are strongly related. HLA-B*15:02 and HLA-B*15:35 were associated with adverse events in our study, and HLA-B*15:01 was associated with asymptomatic COVID-19 in a European study38. Therefore, HLA-B*15 might play an important role in COVID-19. However, HLA-B*15:01 was not significantly associated with adverse events in our study (Table S11). We confirmed the association between two reliable HLA alleles (HLA-DQA1*03:01 and HLA-A*11:01) and all adverse events (Fig. 1, Figure S2). The risk for several adverse events were similarly elevated; however, due to the low frequency of the HLA alleles and the infrequent occurrence of adverse events, the associations between the two HLA allele and adverse events had wide confidence intervals and were not statistically significant. To examine whether associated HLA alleles and variants were correlated, we analyzed the correlation coefficients between HLA alleles and variants (Table S12). As a result, these variants and DPB1, DQA1, DQB1 alleles were moderately correlated and the top correlation coefficient was -0.461 between rs375726766 and DPB1*09:01.
Table 4.
HLA alleles identified by the HLA association analysis of the COVID-19 vaccine adverse events.
| Reaction | HLA allele | Dose | BNT162b1 vaccine | mRNA-1273 vaccine | ||||
|---|---|---|---|---|---|---|---|---|
| AF | OR | P | AF | OR | P | |||
| Pain in vaccination site | DQA1*01:01 | 1st | 0.1 | 1.04 | 0.917 | 0.09 | 3.58 | 0.0002932 |
| 2nd | 0.09 | 1.72 | 0.2394 | 0.09 | 1.22 | 0.3588 | ||
| Pain in vaccination site | DQB1*05:01 | 1st | 0.1 | 1.15 | 0.3469 | 0.08 | 3.05 | 0.000443 |
| 2nd | 0.06 | 1.27 | 0.1741 | 0.08 | 1.33 | 0.1802 | ||
| Swelling of lymph nodes (especially neck, armpit, inguinal part) | B*15:02 | 1st | 0.12 | 4.35 | 0.00008469 | NA | NA | NA |
| 2nd | NA | NA | NA | NA | NA | NA | ||
| 37.5 °C or higher fever | DPB1*09:01 | 1st | 0.15 | 0.84 | 0.383 | 0.1 | 0.97 | 0.8852 |
| 2nd | 0.15 | 0.65 | 0.0003488 | 0.1 | 1.04 | 0.8483 | ||
| 37.5 °C or higher fever | B*40:06 | 1st | 0.07 | 1.03 | 0.8866 | 0.06 | 1.22 | 0.4482 |
| 2nd | 0.13 | 0.67 | 0.0002165 | 0.06 | 0.84 | 0.5695 | ||
| 37.5 °C or higher fever | DQB1*06:01 | 1st | 0.19 | 1.11 | 0.7392 | 0.21 | 0.87 | 0.2867 |
| 2nd | 0.13 | 0.62 | 0.000009773 | 0.21 | 0.9 | 0.4149 | ||
| 37.5 °C or higher fever | DRB1*11:01 | 1st | 0.07 | 0.52 | 0.04899 | NA | NA | NA |
| 2nd | 0.14 | 0.63 | 0.0001659 | NA | NA | NA | ||
| 37.5 °C or higher fever | DQA1*06:01 | 1st | NA | NA | NA | NA | NA | NA |
| 2nd | 0.2 | 0.7 | 0.00007333 | NA | NA | NA | ||
| Muscle pain | DRB1*11:01 | 1st | 0.07 | 0.79 | 0.3191 | NA | NA | NA |
| 2nd | 0.14 | 0.47 | 0.0002821 | NA | NA | NA | ||
| Limb pain | DQA1*05:03 | 1st | NA | NA | NA | NA | NA | NA |
| 2nd | 0.07 | 3.27 | 0.0004283 | NA | NA | NA | ||
| Sneeze | A*11:01 | 1st | 0.08 | 6.86 | 0.0003181 | 0.09 | 5.53 | 0.0124 |
| 2nd | 0.11 | 1.53 | 0.5975 | 0.09 | 1.38 | 0.7743 | ||
| Muscle weakness | DQB1*03:01 | 1st | 0.1 | 1.85 | 0.5959 | 0.12 | 5.95 | 0.1866 |
| 2nd | 0.08 | 1.13 | 0.8376 | 0.11 | 4.42 | 0.0001313 | ||
| Sleepy in the daytime | B*15:35 | 1st | NA | NA | NA | NA | NA | NA |
| 2nd | 0.12 | 1.74 | 0.0003864 | NA | NA | NA | ||
| There is nothing that applies in this (systemic reaction) | DQA1*01:02 | 1st | 0.21 | 1.57 | 0.05491 | 0.19 | 1.7 | 0.000006869 |
| 2nd | 0.21 | 1 | 0.9944 | 0.18 | 1.09 | 0.7831 | ||
| Chills (pathological) | DQA1*03:01 | 1st | 0.15 | 0.95 | 0.8494 | 0.1 | 0.9 | 0.7486 |
| 2nd | 0.12 | 1.39 | 0.02235 | 0.1 | 1.83 | 0.0005086 | ||
HLA alleles achieving p < 5.26 × 10−4 (0.05/95) at the 1st or 2nd dose of the BNT162b1 or mRNA-1273 vaccines.
AF, allele frequency; OR, odds ratio of allele; P, p-value.
Significant values are in bold.
Figure 1.
Odds ratios and 95% confidence intervals of the two reliable HLA alleles (HLA-DQA1*03:01 and HLA-A*11:01) for the occurrence of all adverse events.
Limitations
This study had some limitations. Initially, 53 types of adverse events were included; however, multiple test corrections were not performed because the adverse events were correlated. Therefore, the associated loci that we identified could include false positives, and replicate studies are required. Second, our data on the adverse events were based on web-based self-reports and might have been affected by recall bias. Third, our data might include subjects who responded to the questionnaire before experiencing any adverse events. However, the occurrence of adverse events was similar to that reported in a large-scale survey performed in Japan18. Thus, our adverse event data are considered reliable. Finally, our GWAS was based only on the Japanese population. Therefore, our results may not be directly applicable to individuals of other ethnicities.
Conclusions
In this study, we performed GWAS for adverse events following the COVID-19 vaccination. To the best of our knowledge, this study is the first of its kind to focus on East Asian populations. We identified 14 loci associated with the adverse effects of the COVID-19 vaccines in the Japanese population. HLA allele association analysis revealed that various HLA alleles were associated with these adverse effects; HLA-DQA1*03:01 and HLA-A*11:01 were reliably associated with the adverse events. We discovered that genetic background is associated with the susceptibility to experiencing adverse events following the COVID-19 vaccination. Our results may enable the preparation and management of the occurrence of adverse events based on their susceptibility. Furthermore, we obtained valuable basic data that can be used to investigate the mechanisms of action of COVID-19 vaccines.
Supplementary Information
Acknowledgements
We are grateful to “Genequest ALL” and “Euglena MyHealth” participants included in this study. We thank Euglena Co., Ltd. for providing this study with “Euglena MyHealth” data.
Author contributions
K.S. and S.T. designed the experiments. S.N., K.K., M.C., H.K., and K.T. created the questionnaire on the COVID-19 vaccine and reviewed the data. S.N. performed the statistical analyses. S.N. and K.S. wrote the manuscript. H.K. and K.T. interpreted the results and critically reviewed the manuscript. All the authors commented on and approved the manuscript.
Funding
This work was supported by internal funding from Genequest, Inc.
Data availability
The published article and its additional files include all the data analyzed in this study. The summary statistics of the imputed GWASes were deposited on Zenodo (https://doi.org/10.5281/zenodo.8381695). All other data are available from the corresponding author upon reasonable request.
Competing interests
S.N., K.K., and M.C. are employees of Genequest Inc.; K.S. and S.T. are board members of Genequest Inc.; H.K. and K.T. declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-023-47632-5.
References
- 1.Hu B, Guo H, Zhou P, Shi Z-L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2021;19:141–154. doi: 10.1038/s41579-020-00459-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.COVID-19 vaccine tracker and landscape. World Health Organization (WHO).https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines
- 3.Novel coronavirus vaccines. Official Website of the prime minister of Japan and His cabinet. https://www.kantei.go.jp/jp/headline/kansensho/vaccine.html
- 4.Chapin-Bardales J, Gee J, Myers T. Reactogenicity following receipt of mRNA-based COVID-19 vaccines. JAMA. 2021;325:2201–2202. doi: 10.1001/jama.2021.5374. [DOI] [PubMed] [Google Scholar]
- 5.Shimabukuro T, Nair N. Allergic reactions including anaphylaxis after receipt of the first dose of Pfizer-BioNTech COVID-19 vaccine. JAMA. 2021;325:780–781. doi: 10.1001/jama.2021.0600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Klimek L, et al. Practical handling of allergic reactions to COVID-19 vaccines: A position paper from German and Austrian Allergy Societies AeDA, DGAKI, GPA and ÖGAI. Allergo J. Int. 2021;30:79–95. doi: 10.1007/s40629-021-00165-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Menni C, et al. Vaccine side-effects and SARS-CoV-2 infection after vaccination in users of the COVID Symptom Study app in the UK: A prospective observational study. Lancet Infect. Dis. 2021;21:939–949. doi: 10.1016/S1473-3099(21)00224-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Polack FP, et al. Safety and efficacy of the BNT162b2 mRNA covid-19 vaccine. N. Engl. J. Med. 2020;383:2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gargano JW, et al. Use of mRNA COVID-19 vaccine after reports of myocarditis among vaccine recipients: Update from the Advisory Committee on Immunization Practices—United States, June 2021. MMWR Morb. Mortal. Wkly. Rep. 2021;70:977–982. doi: 10.15585/mmwr.mm7027e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The Genetics Behind The Different Reactions to COVID-19 Vaccines. 23andMe Blog (2021). https://blog.23andme.com/23andme-research/reaction-to-covid-vaccine/
- 11.Bolze, A. et al. HLA-A*03:01 is associated with increased risk of fever, chills, and more severe reaction to Pfizer-BioNTech COVID-19 vaccination. 2021.11.16.21266408 10.1101/2021.11.16.21266408v210.1101/2021.11.16.21266408 (2021).
- 12.Second-generation PLINK: Rising to the challenge of larger and richer datasets | GigaScience | Oxford Academic. https://academic.oup.com/gigascience/article/4/1/s13742-015-0047-8/2707533 [DOI] [PMC free article] [PubMed]
- 13.PLINK: A tool set for whole-genome association and population-based linkage analyses. Am. J. Hum. Genet. https://www.cell.com/ajhg/fulltext/S0002-9297(07)61352-4 [DOI] [PMC free article] [PubMed]
- 14.Price AL, et al. Principal components analysis corrects for stratification in genome-wide association studies. Nat. Genet. 2006;38:904–909. doi: 10.1038/ng1847. [DOI] [PubMed] [Google Scholar]
- 15.Loh P-R, et al. Reference-based phasing using the Haplotype Reference Consortium panel. Nat. Genet. 2016;48:1443–1448. doi: 10.1038/ng.3679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Das S, et al. Next-generation genotype imputation service and methods. Nat. Genet. 2016;48:1284–1287. doi: 10.1038/ng.3656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Auton A, et al. A global reference for human genetic variation. Nature. 2015;526:68–74. doi: 10.1038/nature15393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Health status survey after COVID-19 vaccination. Ministry of Health, Labour and Welfare Web site.https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/vaccine_kenkoujoukyoutyousa.html
- 19.Willer CJ, Li Y, Abecasis GR. METAL: Fast and efficient meta-analysis of genomewide association scans. Bioinformatics. 2010;26:2190–2191. doi: 10.1093/bioinformatics/btq340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zheng X, et al. HIBAG–HLA genotype imputation with attribute bagging. Pharmacogenom. J. 2014;14:192–200. doi: 10.1038/tpj.2013.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zheng X. Imputation-based HLA typing with SNPs in GWAS studies. Methods Mol. Biol. Clifton NJ. 2018;1802:163–176. doi: 10.1007/978-1-4939-8546-3_11. [DOI] [PubMed] [Google Scholar]
- 22.Fan Y, Song Y-Q. PyHLA: Tests for the association between HLA alleles and diseases. BMC Bioinform. 2017;18:90. doi: 10.1186/s12859-017-1496-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baden LR, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N. Engl. J. Med. 2020 doi: 10.1056/NEJMoa2035389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Karczewski KJ, et al. The mutational constraint spectrum quantified from variation in 141,456 humans. Nature. 2020;581:434–443. doi: 10.1038/s41586-020-2308-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.THE GTEX CONSORTIUM et al. The genotype-tissue expression (GTEx) pilot analysis: Multitissue gene regulation in humans. Science348, 648–660 (2015). [DOI] [PMC free article] [PubMed]
- 26.Borba V, et al. Classical examples of the concept of the ASIA syndrome. Biomolecules. 2020;10:1436. doi: 10.3390/biom10101436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fan W-L, et al. HLA association with drug-induced adverse reactions. J. Immunol. Res. 2017;2017:e3186328. doi: 10.1155/2017/3186328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harb H, et al. Notch4 signaling limits regulatory T-cell-mediated tissue repair and promotes severe lung inflammation in viral infections. Immunity. 2021;54:1186–1199.e7. doi: 10.1016/j.immuni.2021.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Roy JG, McElhaney JE, Verschoor CP. Reliable reference genes for the quantification of mRNA in human T-cells and PBMCs stimulated with live influenza virus. BMC Immunol. 2020;21:4. doi: 10.1186/s12865-020-0334-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dang TN, et al. Association of BAK1 single nucleotide polymorphism with a risk for dengue hemorrhagic fever. BMC Med. Genet. 2016;17:43. doi: 10.1186/s12881-016-0305-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Luangtrakool P, et al. Major histocompatibility complex class I chain-related A and B (MICA and MICB) gene, allele, and haplotype associations with dengue infections in ethnic thais. J. Infect. Dis. 2020;222:840–846. doi: 10.1093/infdis/jiaa134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cheng L, et al. The minor alleles HCP5 rs3099844 A and PSORS1C1 rs3131003 G are associated with allopurinol-induced severe cutaneous adverse reactions in Han Chinese: A multicentre retrospective case-control clinical study. Br. J. Dermatol. 2018;178:e191–e193. doi: 10.1111/bjd.16151. [DOI] [PubMed] [Google Scholar]
- 33.Maekawa K, et al. Development of a rapid and inexpensive assay for detecting a surrogate genetic polymorphism of HLA-B*58:01: A partially predictive but useful biomarker for allopurinol-related Stevens-Johnson syndrome/toxic epidermal necrolysis in Japanese. Drug Metab. Pharmacokinet. 2012;27:447–450. doi: 10.2133/dmpk.DMPK-11-NT-120. [DOI] [PubMed] [Google Scholar]
- 34.Kooti W, et al. Association of CYP2C19 and HSP70 genes polymorphism with aspirin-exacerbated respiratory disease in a Kurd population. Endocr. Metab. Immune Disord. Drug Targets. 2020;20:256–262. doi: 10.2174/1872214812666190527104329. [DOI] [PubMed] [Google Scholar]
- 35.Cho S, et al. Association analysis of tapasin polymorphisms with aspirin-exacerbated respiratory disease in asthmatics. Pharmacogenet. Genom. 2013;23:341–348. doi: 10.1097/FPC.0b013e328361d4bb. [DOI] [PubMed] [Google Scholar]
- 36.Pasaje CFA, et al. WDR46 is a genetic risk factor for aspirin-exacerbated respiratory disease in a Korean population. Allergy Asthma Immunol. Res. 2012;4:199–205. doi: 10.4168/aair.2012.4.4.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Castro-Santos P, et al. HLA-A*11:01 and HLA-C*04:01 are associated with severe COVID-19. HLA. 2023 doi: 10.1111/tan.15160. [DOI] [PubMed] [Google Scholar]
- 38.Augusto DG, et al. A common allele of HLA is associated with asymptomatic SARS-CoV-2 infection. Nature. 2023;620:128–136. doi: 10.1038/s41586-023-06331-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The published article and its additional files include all the data analyzed in this study. The summary statistics of the imputed GWASes were deposited on Zenodo (https://doi.org/10.5281/zenodo.8381695). All other data are available from the corresponding author upon reasonable request.