Abstract
Purpose of Review
Obesity, generally defined by body mass index (BMI), is an established risk factor for the development of cardiovascular disease (CVD), while cardiorespiratory fitness (CRF) decreases risk. In chronic CVD, an obesity survival paradox in which higher BMI is associated with improved prognosis has been reported. This paper will examine the effect of obesity on CVD risk, explore obesity as a risk factor in patients with established CVD, and investigate the relationship between CRF, obesity, and CVD.
Recent Findings
Through metabolic and hemodynamic changes, obesity increases the risk for CVD and contributes to the development of other cardiovascular risk factors such as diabetes, dyslipidemia, and hypertension. Obesity is associated with metabolic, hormonal, and inflammatory changes that leads to atherosclerosis increasing the risk for coronary artery disease, and myocardial remodeling increasing the risk for heart failure. However, it has also been observed that overweight/obese patients with established CVD have a better prognosis when compared to non-obese individuals termed the obesity paradox. CRF is a vital component of health associated with improved cardiovascular outcomes and furthermore has been shown to markedly attenuate or nullify the relationship between obesity and CVD risk/prognosis.
Summary
Increasing CRF mitigates CVD risk factors and improves overall prognosis in CVD regardless of obesity status.
Keywords: Obesity, Cardiorespiratory fitness, Cardiovascular disease
Introduction
Obesity rates have been increasing in the USA over the past decades and are projected to continue to rise with an estimation that, by 2030, 78% of American adults will be overweight or obese (body mass index [BMI] ≥ 25 kg/m2), including 50% of adults having obesity (BMI ≥ 30 kg/m2) [1•, 2–5]. It is projected that the largest increases in obesity rates will be observed in women, low-income adults, and Hispanic and Black populations [2, 4, 5]. Since obesity is an established risk factor for cardiovascular disease (CVD) [6•, 7–9] and contributes to diabetes, dyslipidemia, and hypertension [3, 6•, 9], a rise in obesity may contribute to cardiovascular health disparities in the USA.
Obesity as a disease is heterogeneous and multi-faceted, with a myriad of potential influences and causes. Lifestyle, socioeconomic, and environmental factors all contribute to obesity [10]. Obesity is traditionally defined by BMI, although a call for alternative methodology to define obesity is rising. Lifestyle factors that have been associated with obesity include diet, physical activity, sleep, and alcohol consumption [10]. Living in poverty, unemployment, housing insecurity, education, and social support are socioeconomic factors that contribute to obesity [10]. Lastly, environmental factors such as food insecurity, access to supermarkets, state and local policies, marketing, and access all are potential influences for the development of obesity [10]. Together, these factors not only influence the likelihood of developing obesity but also may contribute to the overall cardiorespiratory fitness (CRF) of individuals [11].
Cardiorespiratory fitness (CRF) refers to the ability of the circulatory and respiratory systems to supply oxygen to skeletal muscle during prolonged moderate-to-vigorous exercise [11–13]. Clinically, CRF may be reported as Vo2max (mlO2·kg−1·min−1) measured using treadmill or bicycle ergometer exercise tests or reported as metabolic equivalents (METs) [12, 13]. Poor CRF has been associated with increased risk for developing CVD risk factors, including metabolic syndrome, hypertension, dyslipidemia, diabetes, and atrial fibrillation [14–16]. Low CRF is also a predictor of cardiovascular disease development, all-cause mortality, CVD-related mortality, and cancer-related mortality [17••, 18–21]. Despite the importance of CRF on health and long-term mortality, the CRF of adults in the USA and internationally has decreased over the past 40 years, with the largest declines coinciding with the largest increases in adult obesity [22]. In this review, we will discuss obesity and CVD risk, obesity as a risk factor in patients with established CVD, and the relationship between CRF, obesity, and CVD.
Obesity and Cardiovascular Disease Risk
A host of pathophysiologic cardiovascular changes occurs in response to excess body mass in obesity [8]. The cardiac remodeling that occurs is multi-factorial and involves a combination of changes in hemodynamics, neurohormonal signaling, and/or myocardial metabolism [23]. Metabolically, obesity induces myocardial cellular mechanisms such as ectopic cardiac fat deposition, toxic lipid metabolite accumulation, mitochondrial dysfunction, and inflammation that lead to metabolic adaptations [23]. Hemodynamically, the metabolic demand of obesity is associated an increase in intravascular blood volume and cardiac output through an increase in stroke volume and heart rate [8]. This increased workload predisposes the heart to structural remodeling including concentric and eccentric left ventricular hypertrophy [8].
It has been observed that a subset of individuals, despite having obesity, has a normal cardiometabolic profile [24]. Termed metabolically healthy obesity (MHO), it is defined as having a BMI > 30 kg/m2 and meeting none of the metabolic syndrome criteria except waist circumference [24]. Initially, it was thought that MHO individuals had similar CVD risk as compared to normal weight metabolically healthy individuals [25]. However, recent studies have shown that MHO is not a benign condition, and any level of obesity increases the risk for cardiovascular disease [8, 26•, 27–29]. MHO has been associated with coronary artery calcification, impaired vasoreactivity and left ventricular function, and increased carotid intima-media thickness [8, 30–33]. Individuals with MHO are also more quickly and likely to develop metabolic syndrome and have a higher risk of coronary artery disease, heart failure, and all-cause mortality when compared to metabolically healthy, non-obese individuals [34–37]. Thus, the metabolic and hemodynamic changes that occur in obesity, even in the absence of traditional metabolic risk, increase the risk for both coronary artery disease (CAD) and heart failure, as well as arrhythmias such as atrial fibrillation.
Obesity and Coronary Artery Disease
Obesity is an independent risk factor for CAD and contributes to other risk factors for the development of CAD including insulin resistance, hypertension, and dyslipidemia [6•, 9, 26•, 29, 38]. Obesity leads to CAD in part through an inflammatory process that accelerates atherosclerotic plaque formation which may start as early as childhood [6•, 7]. This inflammatory state promotes the oxidation of low-density lipoproteins (LDL) which promotes atherogenesis [7]. Additionally, inflammation and oxidative stress diminishes the availability of nitric oxide leading to endothelial dysfunction [39]. Adipose tissue’s role as an endocrine organ contributes to the relationship between obesity and CAD, which is the role of adipose tissue as an endocrine organ. Adipose tissue has the ability to release adipokines which are bioactive molecules consisting of hormones, chemokines, and cytokines [8, 40]. Adipose tissue dysfunction in obesity leads to a proliferation of pro-inflammatory adipokines [8, 41] which promotes atherosclerosis by inducing insulin resistance, endothelial dysfunction, hypercoagulability, and systemic inflammation [7].
Obesity and Heart Failure
Obesity is a significant risk factor for heart failure with both preserved and reduced ejection fraction [6•, 42]. Obesity leads to heart failure through hemodynamic and metabolic changes that affect the myocardium [7, 9, 23]. Both the renin-angiotensin-aldosterone system and the sympathetic nervous system are upregulated in obesity [7]. Associated metabolic, hormonal, and inflammatory changes in obesity contribute to myocardial remodeling, increasing the risk for heart failure [23]. The obesity-related pro-inflammatory environment promotes atherosclerosis which also may eventually lead to systolic dysfunction and clinical heart failure [9]. Obesity also leads to the deposition of adipokine-releasing epicardial fat [23]. Fat deposition within and around the heart promotes cardiac dysfunction and subsequent heart failure, through metabolic alterations, lipotoxicity, and myocardial fibrosis [23, 43–46]. In summary, the pathophysiology of obesity in heart failure is complex and involves several direct and indirect mechanisms, all of which lead to metabolic, structural, and functional remodeling and ultimately systolic or diastolic heart failure.
The Obesity Paradox
While obesity is associated with a number of established CVD risk factors, it has also been observed that overweight/obese patients with established CVD have a better prognosis when compared to non-obese individuals in some specific populations [9, 24, 27, 29, 47]. This obesity paradox has been observed in several conditions and types of CVD including heart failure, coronary artery disease, and atrial fibrillation (Table 1) [8, 9, 24, 29].
Table 1.
Conditions associated with an obesity paradox
| Coronary heart disease |
| Heart failure |
| Hypertension |
| Pulmonary arterial hypertension |
| Atrial fibrillation |
| Chronic obstructive pulmonary disease |
| End-stage renal disease |
| Rheumatoid arthritis |
| Various cancers |
| HIV |
There are several possible explanations for this obesity survival paradox. Arguments for the obesity paradox include greater metabolic reserve in the setting of the catabolic state of heart failure, protective alterations in cytokines and adipokines, favorable hemodynamic profile due to low levels of circulating B-type natriuretic peptide, anti-inflammatory effects from elevated circulating lipoproteins, attenuated response to renin-angiotensin-aldosterone system activation, the potential for fat as a repository for stem cells to repopulate the myocardium in heart failure, heightened symptoms in obesity leading to earlier presentation, and the ability to tolerate higher doses of cardioprotective blood pressure lowering medications [8, 47]. Others contend that the concept of an obesity paradox may be flawed due to multiple biases and confounders influencing the association between obesity and CVD, the use of BMI as the main measure of obesity rather than accounting for body composition and adipose distribution, and the disappearance of the paradox in individuals with higher cardiorespiratory fitness (CRF) [8, 47, 48].
Overall, despite the numerous studies and analyses that have demonstrated an obesity paradox in patients with CVD, an improved prognosis has been consistently seen in association with increased physical activity, exercise training, and higher levels of cardiorespiratory fitness [24, 27, 38, 49]. Furthermore, CRF has been shown to possibly confound the relationship between obesity and CVD risk. MHO individuals have been shown to have higher levels of CRF when compared to metabolically abnormal obese individuals, with higher fitness levels associated with a reduction in CVD risk [50].
Cardiorespiratory Fitness
Although it has been established that low CRF is associated with a higher risk of CVD and all-cause mortality [13–16, 17••, 18, 20], CRF among adults has been on the decline over the past 40 years [22]. In one of the largest meta-analyses to date, CRF was inversely associated with all-cause mortality, with every 1 metabolic equivalent increase in estimated CRF (eCRF) associated with an 11% reduction in mortality [51, 52]. This inverse relationship has been demonstrated to exist in individuals with and without CVD [53, 54]. Despite this, CRF is not routinely or regularly assessed by physicians as part of an overall health assessment [13, 55, 56]. CRF can be quantified using measures obtained from cardiorespiratory exercise testing (CPX) which provides peak oxygen consumption (Vo2peak) and other parameters, including the minute ventilation/carbon dioxide production (Ve/ Vco2) slope or exercise testing without CPX measurements [13]. Non-exercise measures of CRF include various models that incorporate clinical health indicators, which may be useful in estimating initial CRF [13, 57]. Determinants of CRF, in healthy individuals, include age, BMI, waist circumference, body fat, weight, smoking, and physical activity levels [12].
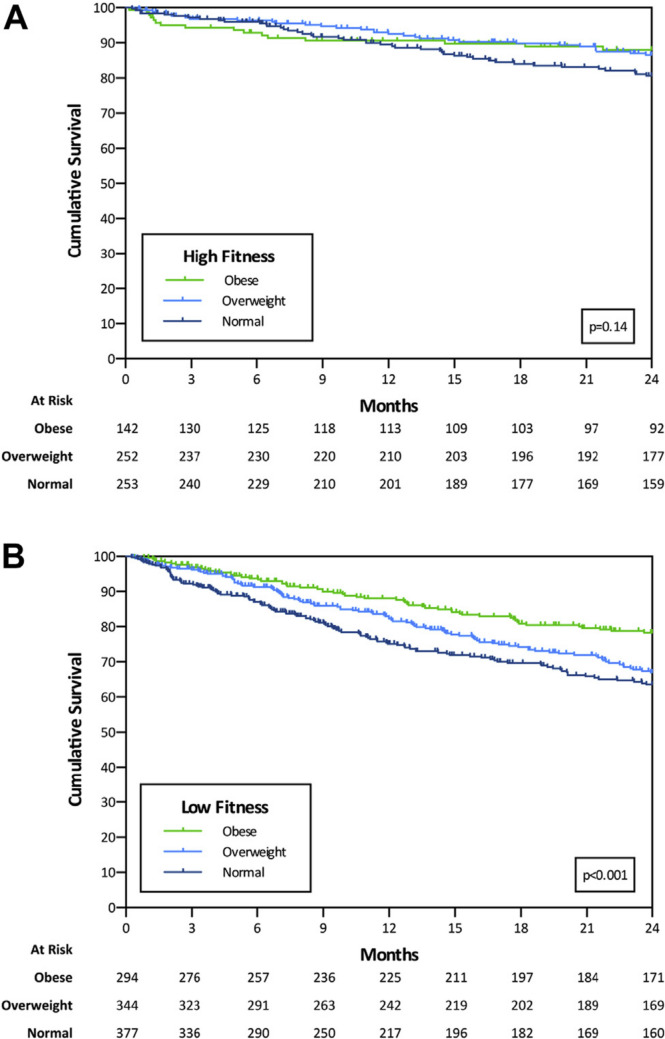
There has been consistent evidence of an association between BMI, waist circumference, and CRF [12]; higher levels of obesity are associated with lower levels of CRF [58]. However, individuals with obesity can have varying levels of CRF [59]. Together, levels of obesity and CRF interact to determine an individual’s CVD risk and CVD prognosis [60]. CRF can mitigate obesity-related CVD risk, as studies have shown an improvement in outcomes among obese individuals with higher levels of CRF [18, 27, 29, 61]. In men with known or suspected coronary heart disease, CRF modified the relationship of adiposity to mortality, with no significant differences in CVD and all-cause mortality risk across BMI, WC, and percent BF categories among men with high fitness levels [62]. Low CRF has been associated with increased risk for heart failure across all BMI categories, with differences in CRF levels serving as an underlying reason for the association between obesity and heart failure [63]. The effect of CRF on CVD prognosis regardless of BMI has been termed the “fat but fit” phenomenon [29, 61]. In patients with systolic heart failure, one study demonstrated an obesity paradox only in those with low CRF, revealing increased mortality in non-obese patients (Fig. 1) [64]. This association between BMI and mortality disappeared in the high CRF group. When BMI and CRF were examined together, individuals with high CRF had the best survival outcomes regardless of BMI, suggesting that improved fitness may attenuate the obesity paradox. While various studies have examined the relationship between obesity, CRF, and CVD, it is important note that obesity is still a significant risk factor for the development of CVD [38]. Overall, fitness and adiposity interact to determine CVD risk, and weight loss when combined with improvements in fitness may lead to the best prognosis in individuals with obesity and CVD [38, 65].
Fig. 1.
Survival at 2 years by BMI in PKVO2 subgroups: A high PKVO2 and B low PKVO2 (adapted from Clark et al. Am J Cardiol 2015;115(2):209–213, with permission from Elsevier) [60]
Increased efforts are needed to improve CRF in individuals with CVD. Cardiac rehabilitation and physical activity interventions have been shown to improve CRF in patients at risk for CVD [8, 12, 13]. Among patients with established CVD, exercise training improves CRF leading to improved prognosis, outcomes, and overall quality of life [49, 66]. Various types of physical activity increase CRF in most adults, with the greater the amount or intensity of physical activity, the greater the increase in CRF [13]. The relationship between physical activity, CRF, obesity, and CVD is complex; however, it is well documented that participating in physical activity increases and allows for the highest possible level of CRF, which, in turn, mitigates CVD risk factors and improves overall prognosis of both CAD and HF [12, 28, 57].
Conclusion
In conclusion, obesity is a significant risk factor for CVD and contributes to the development of other cardiovascular risk factors such as diabetes, dyslipidemia, and hypertension. Obesity-associated changes in hemodynamics, neurohormonal signaling, and myocardial metabolism increase the risk for both CAD and HF. While obesity increases the risk for CVD, it has been observed that overweight/obese patients with established CVD such as heart failure and CAD have a better prognosis when compared to non-obese individuals. While there are many explanations for this paradox, CRF has been shown to markedly attenuate the relationship between obesity/elevated BMI and CVD risk/prognosis. Participating in physical activity increases and allows for the highest possible level of CRF, which is associated with lowered risk of CVD incidence and mortality. Taken together these data suggests that fitness may surpass fatness in determining long-term CVD prognosis.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.• Ogden CL, Fryar CD, Martin CB, Freedman DS, Carroll MD, Gu Q, et al. Trends in obesity prevalence by race and Hispanic origin—1999–2000 to 2017–2018. JAMA. 2020;324(12):1208–10. Public health surveillance of obesity describing changes over time and identifying subgroups at risk of obesity-related consequences. [DOI] [PMC free article] [PubMed]
- 2.Wang Y, Beydoun MA, Min J, Xue H, Kaminsky LA, Cheskin LJ. Has the prevalence of overweight, obesity and central obesity levelled off in the United States? Trends, patterns, disparities, and future projections for the obesity epidemic. Int J Epidemiol. 2020;49(3):810–823. doi: 10.1093/ije/dyz273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hu G, Ding J, Ryan DH. Trends in obesity prevalence and cardiometabolic risk factor control in US adults with diabetes, 1999–2020. Obesity. 2023;31(3):841–851. doi: 10.1002/oby.23652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mohebi R, Chen C, Ibrahim NE, McCarthy CP, Gaggin HK, Singer DE, et al. Cardiovascular disease projections in the United States based on the 2020 census estimates. J Am Coll Cardiol. 2022;80(6):565–578. doi: 10.1016/j.jacc.2022.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ward ZJ, Bleich SN, Cradock AL, Barrett JL, Giles CM, Flax C, et al. Projected US state-level prevalence of adult obesity and severe obesity. N Engl J Med. 2019;381(25):2440–2450. doi: 10.1056/NEJMsa1909301. [DOI] [PubMed] [Google Scholar]
- 6.• Powell-Wiley TM, Poirier P, Burke LE, Després J, Gordon-Larsen P, Lavie CJ, et al. Obesity and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2021;143(21):e984–1010. Comprehensive review on the impact of obesity on the diagnosis, clinical management, and outcomes of atherosclerotic cardiovascular disease, heart failure, and arrhythmias. [DOI] [PMC free article] [PubMed]
- 7.Mandviwala T, Khalid U, Deswal A. Obesity and cardiovascular disease: a risk factor or a risk marker? Curr Atheroscler Rep. 2016;18:1–10. doi: 10.1007/s11883-016-0575-4. [DOI] [PubMed] [Google Scholar]
- 8.Koliaki C, Liatis S, Kokkinos A. Obesity and cardiovascular disease: revisiting an old relationship. Metab Clin Exp. 2019;92:98–107. doi: 10.1016/j.metabol.2018.10.011. [DOI] [PubMed] [Google Scholar]
- 9.Csige I, Ujvárosy D, Szabó Z, Lőrincz I, Paragh G, Harangi M, et al. The impact of obesity on the cardiovascular system. J Diabetes Res. 2018;3407306:2018. [DOI] [PMC free article] [PubMed]
- 10.Safaei M, Sundararajan EA, Driss M, Boulila W, Shapi’i A. A systematic literature review on obesity: understanding the causes & consequences of obesity and reviewing various machine learning approaches used to predict obesity. Comput Biol Med. 2021;136:104754. [DOI] [PubMed]
- 11.Raghuveer G, Hartz J, Lubans DR, Takken T, Wiltz JL, Mietus-Snyder M, et al. Cardiorespiratory fitness in youth: an important marker of health: a scientific statement from the American Heart Association. Circulation. 2020;142(7):e101–e118. doi: 10.1161/CIR.0000000000000866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zeiher J, Ombrellaro KJ, Perumal N, Keil T, Mensink GB, Finger JD. Correlates and determinants of cardiorespiratory fitness in adults: a systematic review. Sports Med Open. 2019;5:1–24. doi: 10.1186/s40798-019-0211-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ross R, Blair SN, Arena R, Church TS, Després J, Franklin BA, et al. Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American Heart Association. Circulation. 2016;134(24):e653–e699. doi: 10.1161/CIR.0000000000000461. [DOI] [PubMed] [Google Scholar]
- 14.Myers J, Kokkinos P, Nyelin E. Physical activity, cardiorespiratory fitness, and the metabolic syndrome. Nutrients. 2019;11(7):1652. doi: 10.3390/nu11071652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sui X, Sarzynski MA, Lee D, Kokkinos PF. Impact of changes in cardiorespiratory fitness on hypertension, dyslipidemia and survival: an overview of the epidemiological evidence. Prog Cardiovasc Dis. 2017;60(1):56–66. doi: 10.1016/j.pcad.2017.02.006. [DOI] [PubMed] [Google Scholar]
- 16.Al-Mallah MH, Sakr S, Al-Qunaibet A. Cardiorespiratory fitness and cardiovascular disease prevention: an update. Curr Atheroscler Rep. 2018;20:1–9. doi: 10.1007/s11883-018-0711-4. [DOI] [PubMed] [Google Scholar]
- 17.•• Han M, Qie R, Shi X, Yang Y, Lu J, Hu F, et al. Cardiorespiratory fitness and mortality from all causes, cardiovascular disease and cancer: dose–response meta-analysis of cohort studies. Br J Sports Med. 2022;56(13):733–9. First meta-analysis to examine the association between CRF and CVD mortality. [DOI] [PubMed]
- 18.Kokkinos P, Faselis C, Samuel IBH, Pittaras A, Doumas M, Murphy R, et al. Cardiorespiratory fitness and mortality risk across the spectra of age, race, and sex. J Am Coll Cardiol. 2022;80(6):598–609. doi: 10.1016/j.jacc.2022.05.031. [DOI] [PubMed] [Google Scholar]
- 19.Mandsager K, Harb S, Cremer P, Phelan D, Nissen SE, Jaber W. Association of cardiorespiratory fitness with long-term mortality among adults undergoing exercise treadmill testing. JAMA Netw Open. 2018;1(6):e183605. [DOI] [PMC free article] [PubMed]
- 20.Imboden MT, Harber MP, Whaley MH, Finch WH, Bishop DL, Kaminsky LA. Cardiorespiratory fitness and mortality in healthy men and women. J Am Coll Cardiol. 2018;72(19):2283–2292. doi: 10.1016/j.jacc.2018.08.2166. [DOI] [PubMed] [Google Scholar]
- 21.Harber MP, Kaminsky LA, Arena R, Blair SN, Franklin BA, Myers J, et al. Impact of cardiorespiratory fitness on all-cause and disease-specific mortality: advances since 2009. Prog Cardiovasc Dis. 2017;60(1):11–20. doi: 10.1016/j.pcad.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 22.Lamoureux NR, Fitzgerald JS, Norton KI, Sabato T, Tremblay MS, Tomkinson GR. Temporal trends in the cardiorespiratory fitness of 2,525,827 adults between 1967 and 2016: a systematic review. Sports Med. 2019;49:41–55. doi: 10.1007/s40279-018-1017-y. [DOI] [PubMed] [Google Scholar]
- 23.Haidar A, Taegtmeyer H. Strategies for imaging metabolic remodeling of the heart in obesity and heart failure. Curr Cardiol Rep. 2022;24(4):327–335. doi: 10.1007/s11886-022-01650-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ortega FB, Lavie CJ, Blair SN. Obesity and cardiovascular disease. Circ Res. 2016;118(11):1752–1770. doi: 10.1161/CIRCRESAHA.115.306883. [DOI] [PubMed] [Google Scholar]
- 25.Hamer M, Stamatakis E. Metabolically healthy obesity and risk of all-cause and cardiovascular disease mortality. J Clin Endocrinol Metab. 2012;97(7):2482–2488. doi: 10.1210/jc.2011-3475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.• Elagizi A, Kachur S, Carbone S, Lavie CJ, Blair SN. A review of obesity, physical activity, and cardiovascular disease. Curr Obes Rep. 2020;9:571–81. Comprehensive review summarizing the pathophysiological changes associated with obesity, recommendations for interventions such as diet, increased physical activity, and weight loss according to current literature and guidelines, and the critical importance of cardiorespiratory fitness (CRF). [DOI] [PubMed]
- 27.Lavie CJ, De Schutter A, Milani RV. Healthy obese versus unhealthy lean: the obesity paradox. Nat Rev Endocrinol. 2015;11(1):55–62. doi: 10.1038/nrendo.2014.165. [DOI] [PubMed] [Google Scholar]
- 28.Lavie CJ, Milani RV, Ventura HO. Disparate effects of metabolically healthy obesity in coronary heart disease and heart failure. J Am Coll Cardiol. 2014;63(11):1079–1081. doi: 10.1016/j.jacc.2013.10.080. [DOI] [PubMed] [Google Scholar]
- 29.Elagizi A, Kachur S, Lavie CJ, Carbone S, Pandey A, Ortega FB, et al. An overview and update on obesity and the obesity paradox in cardiovascular diseases. Prog Cardiovasc Dis. 2018;61(2):142–150. doi: 10.1016/j.pcad.2018.07.003. [DOI] [PubMed] [Google Scholar]
- 30.Khan UI, Wang D, Thurston RC, Sowers M, Sutton-Tyrrell K, Matthews KA, et al. Burden of subclinical cardiovascular disease in “metabolically benign” and “at-risk” overweight and obese women: the Study of Women’s Health Across the Nation (SWAN) Atherosclerosis. 2011;217(1):179–186. doi: 10.1016/j.atherosclerosis.2011.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chang Y, Kim B, Yun KE, Cho J, Zhang Y, Rampal S, et al. Metabolically-healthy obesity and coronary artery calcification. J Am Coll Cardiol. 2014;63(24):2679–2686. doi: 10.1016/j.jacc.2014.03.042. [DOI] [PubMed] [Google Scholar]
- 32.Park J, Kim SH, Cho G, Baik I, Kim NH, Lim HE, et al. Obesity phenotype and cardiovascular changes. J Hypertens. 2011;29(9):1765–1772. doi: 10.1097/HJH.0b013e32834a50f3. [DOI] [PubMed] [Google Scholar]
- 33.Lind L, Siegbahn A, Ingelsson E, Sundström J, Ärnlöv J. A detailed cardiovascular characterization of obesity without the metabolic syndrome. Arterioscler Thromb Vasc Biol. 2011;31(8):e27–e34. doi: 10.1161/ATVBAHA.110.221572. [DOI] [PubMed] [Google Scholar]
- 34.Hwang YC, Hayashi T, Fujimoto WY, Kahn SE, Leonetti DL, McNeely MJ, et al. Visceral abdominal fat accumulation predicts the conversion of metabolically healthy obese subjects to an unhealthy phenotype. Int J Obes. 2015;39(9):1365–1370. doi: 10.1038/ijo.2015.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mongraw-Chaffin M, Foster MC, Anderson CA, Burke GL, Haq N, Kalyani RR, et al. Metabolically healthy obesity, transition to metabolic syndrome, and cardiovascular risk. J Am Coll Cardiol. 2018;71(17):1857–1865. doi: 10.1016/j.jacc.2018.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Caleyachetty R, Thomas GN, Toulis KA, Mohammed N, Gokhale KM, Balachandran K, et al. Metabolically healthy obese and incident cardiovascular disease events among 3.5 million men and women. J Am Coll Cardiol. 2017;70(12):1429–37. [DOI] [PubMed]
- 37.Ortega FB, Cadenas-Sanchez C, Migueles JH, Labayen I, Ruiz JR, Sui X, et al. Role of physical activity and fitness in the characterization and prognosis of the metabolically healthy obesity phenotype: a systematic review and meta-analysis. Prog Cardiovasc Dis. 2018;61(2):190–205. doi: 10.1016/j.pcad.2018.07.008. [DOI] [PubMed] [Google Scholar]
- 38.Lavie CJ, Arena R, Alpert MA, Milani RV, Ventura HO. Management of cardiovascular diseases in patients with obesity. Nat Rev Cardiol. 2018;15(1):45–56. doi: 10.1038/nrcardio.2017.108. [DOI] [PubMed] [Google Scholar]
- 39.Engin A. Endothelial dysfunction in obesity. Obesity Lipotoxicity. 2017;345–79. [DOI] [PubMed]
- 40.Kershaw EE, Flier JS. Adipose tissue as an endocrine organ. J Clin Endocrinol Metab. 2004;89(6):2548–2556. doi: 10.1210/jc.2004-0395. [DOI] [PubMed] [Google Scholar]
- 41.Nakamura K, Fuster JJ, Walsh K. Adipokines: a link between obesity and cardiovascular disease. J Cardiol. 2014;63(4):250–259. doi: 10.1016/j.jjcc.2013.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bozkurt B, Aguilar D, Deswal A, Dunbar SB, Francis GS, Horwich T, et al. Contributory risk and management of comorbidities of hypertension, obesity, diabetes mellitus, hyperlipidemia, and metabolic syndrome in chronic heart failure: a scientific statement from the American Heart Association. Circulation. 2016;134(23):e535–e578. doi: 10.1161/CIR.0000000000000450. [DOI] [PubMed] [Google Scholar]
- 43.Piché M, Poirier P. Obesity, ectopic fat and cardiac metabolism. Expert Rev Endocrinol Metab. 2018;13(4):213–221. doi: 10.1080/17446651.2018.1500894. [DOI] [PubMed] [Google Scholar]
- 44.Ferrara D, Montecucco F, Dallegri F, Carbone F. Impact of different ectopic fat depots on cardiovascular and metabolic diseases. J Cell Physiol. 2019;234(12):21630–21641. doi: 10.1002/jcp.28821. [DOI] [PubMed] [Google Scholar]
- 45.Sletten AC, Peterson LR, Schaffer JE. Manifestations and mechanisms of myocardial lipotoxicity in obesity. J Intern Med. 2018;284(5):478–491. doi: 10.1111/joim.12728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Iacobellis G. Local and systemic effects of the multifaceted epicardial adipose tissue depot. Nat Rev Endocrinol. 2015;11(6):363–371. doi: 10.1038/nrendo.2015.58. [DOI] [PubMed] [Google Scholar]
- 47.Horwich TB, Fonarow GC, Clark AL. Obesity and the obesity paradox in heart failure. Prog Cardiovasc Dis. 2018;61(2):151–156. doi: 10.1016/j.pcad.2018.05.005. [DOI] [PubMed] [Google Scholar]
- 48.Kokkinos P, Faselis C, Franklin B, Lavie CJ, Sidossis L, Moore H, et al. Cardiorespiratory fitness, body mass index and heart failure incidence. Eur J Heart Fail. 2019;21(4):436–444. doi: 10.1002/ejhf.1433. [DOI] [PubMed] [Google Scholar]
- 49.Pandey A, Parashar A, Kumbhani DJ, Agarwal S, Garg J, Kitzman D, et al. Exercise training in patients with heart failure and preserved ejection fraction: meta-analysis of randomized control trials. Circ Heart Fail. 2015;8(1):33–40. [DOI] [PMC free article] [PubMed]
- 50.Ortega FB, Lee D, Katzmarzyk PT, Ruiz JR, Sui X, Church TS, et al. The intriguing metabolically healthy but obese phenotype: cardiovascular prognosis and role of fitness. Eur Heart J. 2013;34(5):389–397. doi: 10.1093/eurheartj/ehs174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Laukkanen JA, Isiozor NM, Kunutsor SK. Objectively assessed cardiorespiratory fitness and all-cause mortality risk: an updated meta-analysis of 37 cohort studies involving 2,258,029 participants. Mayo Clin Proc. 2022;97(6):1054–1073. doi: 10.1016/j.mayocp.2022.02.029. [DOI] [PubMed] [Google Scholar]
- 52.Lavie CJ, Arena R, Kaminsky LA. Making the case to measure and improve cardiorespiratory fitness in routine clinical practice. Mayo Clin Proc. 2022;97(6):1038–1040. doi: 10.1016/j.mayocp.2022.04.011. [DOI] [PubMed] [Google Scholar]
- 53.Kokkinos P, Faselis C, Samuel IB, Lavie CJ, Zhang J, Vargas JD, et al. Changes in cardiorespiratory fitness and survival in patients with or without cardiovascular disease. J Am Coll Cardiol. 2023;81(12):1137–1147. doi: 10.1016/j.jacc.2023.01.027. [DOI] [PubMed] [Google Scholar]
- 54.Kaminsky LA, Imboden MT, Ozemek C. It’s time to (again) recognize the considerable clinical and public health significance of cardiorespiratory fitness. J Am Coll Cardiol. 2023;81(12):1148–1150. doi: 10.1016/j.jacc.2023.02.004. [DOI] [PubMed] [Google Scholar]
- 55.Kaminsky LA, Arena R, Ellingsen Ø, Harber MP, Myers J, Ozemek C, et al. Cardiorespiratory fitness and cardiovascular disease-the past, present, and future. Prog Cardiovasc Dis. 2019;62(2):86–93. doi: 10.1016/j.pcad.2019.01.002. [DOI] [PubMed] [Google Scholar]
- 56.Kaminsky LA, Arena R, Beckie TM, Brubaker PH, Church TS, Forman DE, et al. The importance of cardiorespiratory fitness in the United States: the need for a national registry: a policy statement from the American Heart Association. Circulation. 2013;127(5):652–662. doi: 10.1161/CIR.0b013e31827ee100. [DOI] [PubMed] [Google Scholar]
- 57.DeFina LF, Haskell WL, Willis BL, Barlow CE, Finley CE, Levine BD, et al. Physical activity versus cardiorespiratory fitness: two (partly) distinct components of cardiovascular health? Prog Cardiovasc Dis. 2015;57(4):324–329. doi: 10.1016/j.pcad.2014.09.008. [DOI] [PubMed] [Google Scholar]
- 58.Kaze AD, Da Agoons D, Santhanam P, Erqou S, Ahima RS, Echouffo-Tcheugui JB. Correlates of cardiorespiratory fitness among overweight or obese individuals with type 2 diabetes. BMJ Open Diabetes Res Care. 2022;10(1):e002446. [DOI] [PMC free article] [PubMed]
- 59.Takken T, Hulzebos HJ. Is BMI Associated with cardiorespiratory fitness? A cross-sectional analysis among 8470 apparently healthy subjects aged 18–94 years from the Low-Lands Fitness Registry. J Sci Sport Exerc. 2022;4(3):283–289. doi: 10.1007/s42978-021-00143-z. [DOI] [Google Scholar]
- 60.Henriksson H, Henriksson P, Tynelius P, Ekstedt M, Berglind D, Labayen I, et al. Cardiorespiratory fitness, muscular strength, and obesity in adolescence and later chronic disability due to cardiovascular disease: a cohort study of 1 million men. Eur Heart J. 2020;41(15):1503–1510. doi: 10.1093/eurheartj/ehz774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Oktay AA, Lavie CJ, Kokkinos PF, Parto P, Pandey A, Ventura HO. The interaction of cardiorespiratory fitness with obesity and the obesity paradox in cardiovascular disease. Prog Cardiovasc Dis. 2017;60(1):30–44. doi: 10.1016/j.pcad.2017.05.005. [DOI] [PubMed] [Google Scholar]
- 62.McAuley PA, Artero EG, Sui X, Lee D, Church TS, Lavie CJ, et al. The obesity paradox, cardiorespiratory fitness, and coronary heart disease. Mayo Clin Proc. 2012;87(5):443–451. doi: 10.1016/j.mayocp.2012.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Pandey A, Cornwell WK, Willis B, Neeland IJ, Gao A, Leonard D, et al. Body mass index and cardiorespiratory fitness in mid-life and risk of heart failure hospitalization in older age: findings from the Cooper Center Longitudinal Study. JACC Heart Fail. 2017;5(5):367–74. [DOI] [PubMed]
- 64.Clark AL, Fonarow GC, Horwich TB. Impact of cardiorespiratory fitness on the obesity paradox in patients with systolic heart failure. Am J Cardiol. 2015;115(2):209–213. doi: 10.1016/j.amjcard.2014.10.023. [DOI] [PubMed] [Google Scholar]
- 65.Tutor AW, Lavie CJ, Kachur S, Milani RV, Ventura HO. Updates on obesity and the obesity paradox in cardiovascular diseases. Prog Cardiovasc Dis. 2023;78:2–10 [DOI] [PubMed]
- 66.Tutor A, Lavie CJ, Kachur S, Dinshaw H, Milani RV. Impact of cardiorespiratory fitness on outcomes in cardiac rehabilitation. Prog Cardiovasc Dis. 2022;70:2–7. doi: 10.1016/j.pcad.2021.11.001. [DOI] [PubMed] [Google Scholar]