Abstract
This study aimed to investigate the prescribing pattern of antipsychotic medications for schizophrenia using the British National Formulary total daily dose (TDD) online tool. We analysed data from the electronic medical records at King Khalid University Hospital (KKUH) of 272 patients diagnosed with schizophrenia who were prescribed both typical and atypical antipsychotic medications. The results showed that aripiprazole was the most commonly prescribed antipsychotic drug, followed by haloperidol then risperidone. The TDD online tool was used to calculate the TDD of each prescribed antipsychotic medication. Most patients were prescribed doses within the recommended range for each medication, although some were prescribed doses above or below the recommended range. Moreover, a high recommended TDD was associated with the combined use of antipsychotics rather than monotherapy. Additionally, high TDD levels were associated with the following antipsychotics: haloperidol, olanzapine, paliperidone, and quetiapine. Our findings highlight the importance of using evidence-based tools such as the TDD online tool to guide prescribing practices and ensure optimal dosing of antipsychotic medications for patients with schizophrenia.
Keywords: Antipsychotics, Daily Dose online tool, Schizophrenic Patients
1. Introduction
Drug utilisation information plays a key role in understanding, interpreting, evaluating, and improving medication prescribing, administration, and use. Therefore, it is necessary to monitor the use drugs with high-risk side effects, such as antipsychotics, as they contribute to serious and life-threatening conditions.
Schizophrenia is a chronic mental disorder associated with significant disabilities in daily activities. It can influence the patients’ personal, familial, social, educational, and occupational functions. Further, psychosis, which includes hallucinations and delusions, is considered the most common symptom of schizophrenia that should be treated with antipsychotics; statistics show that schizophrenia affects approximately 24 million people or 1 in 300 people (0.32 %) around the world (WHO 2022). Correspondingly, the incidence of schizophrenia in Saudi Arabia is 55.8 % among inpatients and 28.9 % among outpatients (Alosaimi et al., 2017).
There are two main classes of antipsychotic medications: typical (conventional) antipsychotics that act on the dopaminergic system by blocking the dopamine type 2 (D2) receptors, and atypical antipsychotics that work by lowering the affinity and occupancy of the dopaminergic receptors, with a high degree of occupancy toward serotoninergic 5-HT2A receptors (Seeman, 2002). A systematic review concluded that atypical antipsychotics have advantages over typical antipsychotics, mainly due to their better safety profile (Melnik et al., 2010).
The prevalence of antipsychotic medication use has increased significantly (Alessi-Severini et al., 2008), with the global prevalence of antipsychotic medication increasing by 62 %. The most significant diagnoses resulting in antipsychotic prescriptions have been reported to be schizophrenia, dementia, and major depression associated with psychosis. In Saudi Arabia, a study conducted in different hospital settings showed that antipsychotic use was more frequent (6.6 %) than the use of psychotropics. The study results revealed that a larger percentage of inpatients were treated with antipsychotics than outpatients (94.3 % vs. 65.7 %, respectively)(Alosaimi et al., 2017).
The prescribing pattern of antipsychotics should follow guidelines, such as those of the American Psychiatric Association (APA 2020). Guidelines recommend that patients with schizophrenia should be treated with antipsychotic medications and monitored for therapeutic effectiveness and occurrence of side effects (Keepers et al., 2020).
Prescribing high dose antipsychotics has been linked to polypharmacy. Antipsychotic polypharmacy is defined as the prescription of two or more concomitant antipsychotics as standard therapy (Lähteenvuo & Tiihonen, 2021).
The Royal College of Psychiatrists defines a high dose of antipsychotic prescription as prescribing single or several antipsychotics simultaneously when the total daily dose (TDD) exceeds the British National Formulary (BNF) standard or a combination of percentages of a maximum daily dose exceeding 100 % (Royal College of Psychiatrists, 2014).
In addition, combining antipsychotics is a significant contributor to high doses, and studies have shown that high doses of antipsychotics increase mortality and side effects.
In a recent cohort study, the Japan Adverse Drug Events (JADE) recruited psychiatric inpatients administering antipsychotic polypharmacy and experiencing adverse drug events (ADEs).
Atypical antipsychotics were the most common drug class associated with adverse effects (34 %). Central nervous system symptoms, including falls, oversedation, and extrapyramidal symptoms, were the most frequent (44 %), followed by gastrointestinal symptoms, including diarrhoea and constipation (34 %). The median number of ADEs in the antipsychotic polypharmacy group was significantly higher than that in the non-antipsychotic polypharmacy group (Ayani et al., 2021).
According to the Royal College of Psychiatrists (2014), high doses of antipsychotics may lead to extrapyramidal side effects, tardive dyskinesia, postural hypotension, sedation, and some peripheral autonomic effects such as dry mouth, constipation, urine retention, tachycardia, ventricular tachycardia, and sudden death. Further, the rapid escalation of antipsychotic dosage may lead to akathisia and neuroleptic malignant syndrome, whereas hyperprolactinemia is not really dose-related and can occur with many antipsychotics even at low doses (Royal College of Psychiatrists, 2014).
In addition, in a retrospective cohort study of Medicaid in Tennessee enrollees from 1990 to 2005, current users of typical and atypical antipsychotic drugs had higher rates of sudden cardiac death than nonusers of antipsychotic medications with incidence-rate ratios of 1.84 (95 % CI, 1.50–2.26) and 1.99 (95 % CI, 1.61–2.46), respectively, with the risk for current users increasing significantly with an increasing dose for both drug classes.
The incidence rate for a high typical antipsychotic dose was 2.70 (1.90–3.84), and the high atypical antipsychotic dose was 2.69 (1.93–3.73). Consequently, the occurrence of adverse effects associated with antipsychotics requires more attention. Because the risk of these medications increases with increasing dose, the dose should be calculated precisely.
The antipsychotic dose can be calculated in three ways: using the Chlorpromazine dose equivalent (CPZeq), Percentage of BNF maximum, and Defined Daily Dose (DDD). A study conducted in 2011 concluded that all three methods are reliable. The BNF method is an easy and readily available technique, and some investigators have recommended using the BNF instead of the CPZeq method (Sweileh et al., 2014).
In Saudi Arabia, mental health settings have received increasing attention over the years, resulting in better delivery of mental health services. Recently, the Ministry of Health, as part of the KSA's Vision 2030, has been developing a national mental health strategy to address the gap in the current mental health system and design care that ensures quality, accessibility, and integration of care for patients with mental health illnesses. Consequently, implementing an online calculator can help physicians make appropriate prescribing decisions. Expressing the total antipsychotic dose as a percentage of the BNF maximum is easy to understand and calculate. Recent copies of the BNF are widely available, the BNF is updated twice a year, and maximum doses are assumingly accurate and are generally based on toxicity rather than efficacy (Yorston & Pinney, 2000). Therefore, there is an urgent need to focus on the treatment plan in Saudi Arabia and provide innovative applications that keep up with therapeutic decision-making improvement. In addition, reviewing prescription practices helps decision-makers to obtain insights into their decisions and improve patient safety outcomes.
Recently, an online calculator was developed as an accessible method for calculating the total daily antipsychotic dose based on the BNF. According to the authors' objectives, the tool is meant to help clinicians review antipsychotic prescription patterns, enhance decision makers’ options, and improve patient safety outcomes (Northwood et al., 2020).
The online TDD calculator assists in the simple, rapid, and less error-prone calculation of antipsychotic doses containing various typical or atypical antipsychotic medications, as well as different routes of administration, which is of benefit to healthcare professionals, particularly pharmacists.
This study aimed to review the antipsychotic prescription patterns among schizophrenic patients using a TDD calculator and to investigate the need to apply a tool for high-dose antipsychotic prescribing in these patients by determining the prevalence of high-dose antipsychotic prescriptions. Overall, we aimed to elucidate the importance of using online TDD calculators for decision makers and healthcare professionals.
2. Methodology
2.1. Study design and settings
This cross-sectional study was conducted in the primary care psychiatry clinic at King Saud University Medical City (KSUMC) in Riyadh, Saudi Arabia. The study was observational in nature and guided by the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines (Von Elm et al., 2007).
2.2. Participants
Patients who met the following criteria were considered for the study: male or female, 18 years or older, schizophrenic patients defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV), those taking antipsychotic medications that were included in the TDD calculator (Table 1), and patients who received antipsychotics between February 2020–February 2021. Children and patients who were not on any antipsychotic medication or antipsychotic medications not included in the online calculator, as well as newly diagnosed patients were excluded from the study.
Table 1.
Baseline demographics, BNF factor, settings, and antipsychotics of participants.
| N = 272 | N (%), mean (standard deviation-SD), median (interquartile rang-IQR) | |
|---|---|---|
| Age in years, N (%) | 18 | 3 (1.1) |
| 19–39 | 151 (55.5) | |
| 40–69 | 114 (41.9) | |
| >=70 | 4 (1.5) | |
| Gender, N (%) | Male | 112 (41.2) |
| Female | 160 (58.8) | |
| Antipsychotic therapeutic class, N (%) | Atypical | 209 (76.8) |
| Typical | 63 (23.2) | |
| Number of medication, mean (SD) | 2.46 (1.73) | |
| Number of admission days, median (IQR) | 31.00 (27.00–––37.00) | |
| BNF factor, mean (SD) | 0.599 (0.551) | |
| BNF interpretation, N (%) | High | 19 (7.0) |
| Low | 253 (93.0) | |
| Setting, N (%) | Outpatient | 149 (54.8) |
| Inpatient | 123 (45.2) | |
| Aripiprazole, N (%) | 145 (53.3) | |
| Haloperidol, N (%) | 88 (32.4) | |
| Quetiapine, N (%) | 65 (23.9) | |
| Risperidone, N (%) | 64 (23.5) | |
| Olanzapine, N (%) | 58 (21.3) | |
| Amisulpride, N (%) | 22 (8.1) | |
| Clozapine, N (%) | 22 (8.1) | |
| Chloropromazine, N (%) | 9 (3.3) | |
| Paliperidonelnevga, N (%) | 8 (2.9) | |
| Zuclopenthixol, N (%) | 6 (2.2) | |
Bold: indicate higher percent.
2.3. Data source variables and recording
Patient data was obtained from their medical records, and all information was recorded on a predesigned data collection sheet. The data collection sheet was divided into three sections: The first part about participants' demographics, as age and sex; The second section contained information on antipsychotic medications, including drug name, dose, frequency, and duration of treatment; The final part of the sheet was about the TDD factor.
2.4. Assessment tool
The TDD was calculated using an online TDD calculator (Example in Supplementary material Fig. 1) at TDDcalculator.com (https://kornor.github.io/)(Northwood et al., 2020). The calculation was performed by choosing random medical record numbers (MRN) to reduce the risk of sampling bias, then entering antipsychotic medications that are taken at the same interval; doses and single regimen frequencies were submitted and the cumulative TDD factor was calculated (a TDD factor of 1.0 is equivalent to 100 % of the recommended maximum daily dose; a TDD factor exceeding 1 shows that the TDD is higher than that suggested by the TDD for the medication or the medication combination). Based on the TDD factor, we determined the percentage of patients who exceeded the maximum TDD of antipsychotic medications.
2.5. Study sample size
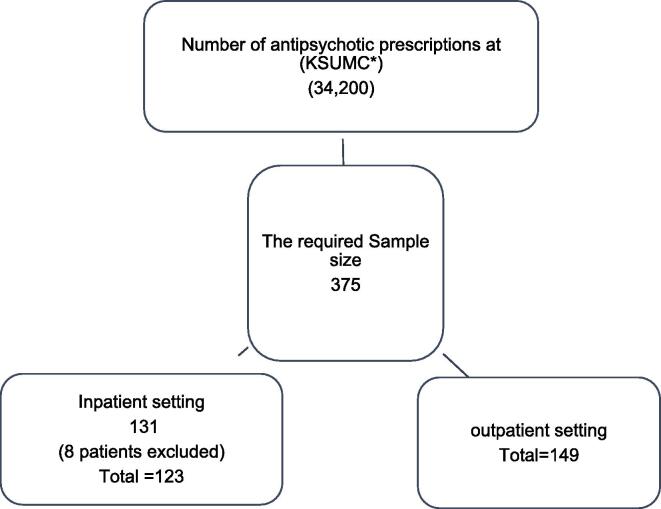
The sample size was computed based on the current number of antipsychotic prescriptions at King Saud University Medical City (KSUMC), which was based on the pharmacy service statistics of the total prescriptions (34,200). The sample size was calculated using an online sample size calculator (https://www.calculator.net/sample-size-calculator.html), considering a 5 % margin of error, 95 % confidence level, and 56 % of the antipsychotic prescriptions reported (Alkhadhari, et al.). The minimum sample size required for the study was 375.
2.6. Statistical methods
Data were coded and entered into IBM Statistical Package for Social Sciences (SPSS) version 25 (IBM Corp., Armonk, USA). Categorical variables were described as numbers and percentages. Continuous variables are conveyed as mean (standard deviation-SD) or median (interquartile range-IQR), depending on the normality of distribution. For comparison, demographics and medications were classified based on the BNF factor as high or low. Differences between high and low categorical variables were calculated using chi squared. Binary logistic regression was used to foresee the odds of a high BNF factor. Statistical significance was set at p < 0.05.
3. Results
Current number of antipsychotic prescriptions at King Saud University Medical City (KSUMC), which was provided based on pharmacy service statistics (34,200). A total of 131 participants were identified from inpatient setting and 149 from outpatient setting. After further file review 8 participants didn’t meet the inclusion criteria and was excluded. Study enrolment Fig. 1.
Fig. 1.
Study enrollment chart, *KSUMC: King Saud University Medical City (KSUMC).
The total number of patients who received antipsychotics and were eligible for study inclusion was 272. Approximately half of the patients (58.8 %, n = 160) were female and 41.2 % (n = 112) were male. Of the patients, 55.5 % (n = 151) were between the ages of 19–39, and 1.5 % (n = 4) were aged 70 years or older. Participants who received mostly atypical antipsychotics (77 %, n = 209) had a mean (SD) number of medications of 2.5 (1.7) and were admitted in the previous year for a median (IQR) of 31 (27–37) days. The mean (SD) BNF-TDD factor was 0.59 (0.55), and of low BNF factor (93 %; n = 253). The most common medication used was aripiprazole (53 %, n = 145), followed by haloperidol (32 %, n = 88) and risperidone (24 %, n = 65). The baseline information of the participants is shown in Table 1.
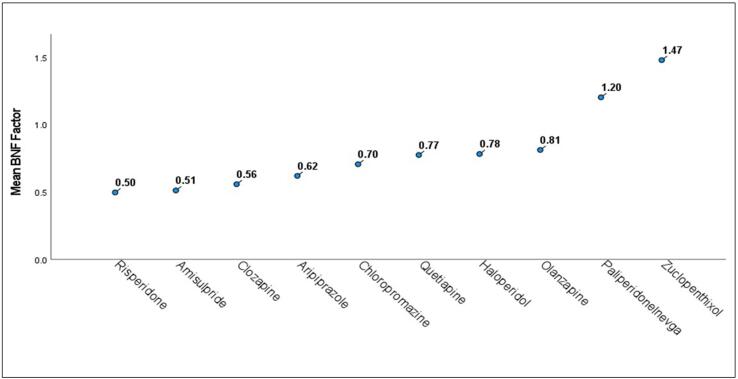
When classified as high or low, participants with a high TDD factor were male (58 %, n = 11),40–69 years of age, and had a greater median (IQR) hospitalisation of 73 (36–111) days; however, all were insignificant. On the other hand, participants with a high BNF factor were more likely to receive typical antipsychotics (42 %, n = 8; p = 0.042) and had a higher median (IQR) of 4 (3–5) days, p < 0.001. Fig. 2 demonstrates the presence of a high BNF factor in the typical antipsychotic group compared to the atypical with a mean (SD) of 0.76 (0.91) versus 0.55 (0.37) respectively p = 0.007. Regarding medication, antipsychotics that were more likely to be prescribed in the high TDD factor group were as follows: haloperidol, 58 % (n = 11), p = 0.014; quetiapine, 47 % (n = 9), p = 0.022; olanzapine, 53 % (n = 10), p = 0.002; and paliperidone, 16 % (n = 3), p = 0.013 (Table 2). Fig. 3 shows mean values of different antipsychotics individually regardless of therapeutic class with highest mean (SD) value of the TDD factor was in individual medications was highest in zuclopenthixol 1.5 (1.6), paliperidone 1.2 (0.69), olanzapine 0.81 (0.68), haloperidol 0.78 (0.82), quetiapine 0.77 (0.76), chlorpromazine 0.70 (0.32), aripiprazole 0.62 (0.39), clozapine 0.56 (0.39), amisulpride 0.51 (0.29) and lowest in risperidone 0.50 (0.32), p = 0.017. Fig. 3.
Fig. 2.
Class of antipsychotic and mean BNF factor with a higher BNF factor in typical versus atypical, p = 0.007.
Table 2.
Difference between high and low BNF factors.
| N = 272 |
High |
Low |
p value | |
|---|---|---|---|---|
| N = 19 | N = 253 | |||
| Age, N (%) | 18 | 0 | 3 (1.2) | 0.415 |
| 19–39 | 8 (42.1) | 143 (56.5) | ||
| 40–69 | 11 (57.9) | 103 (40.7) | ||
| >=70 | 0 | 4 (1.6) | ||
| Gender, N (%) | Male | 11 (57.9) | 101 (39.9) | 0.125 |
| Female | 8 (42.1) | 152 (60.1) | ||
| Antipsychotic therapeutic class, N (%) | Atypical | 11 (57.9) | 198 (78.3) | 0.042* |
| Typical | 8 (42.1) | 55 (21.7) | ||
| Number of medication, mean (SD), count | 4.26 (2.18) | 2.33 (1.62) | <0.001* | |
| Number of admission days, median (IQR), days | 73.00 (36.00–––110.00) | 30.00 (23.00–––36.00) | 0.275 | |
| Aripiprazole | 10 (52.6) | 135 (53.4) | 0.951 | |
| Haloperidol | 11 (57.9) | 77 (30.4) | 0.014* | |
| Quetiapine | 9 (47.4) | 56 (22.1) | 0.022* | |
| Risperidone | 3 (15.8) | 61 (24.1) | 0.578 | |
| Olanzapine | 10 (52.6) | 48 (19.0) | 0.002* | |
| Amisulpride | 1 (5.3) | 21 (8.3) | 1.000 | |
| Clozapine | 2 (10.5) | 20 (7.9) | 0.658 | |
| Chloropromazine | 1 (5.3) | 8 (3.2) | 0.484 | |
| Paliperidone | 3 (15.8) | 5 (2.0) | 0.013* | |
| Zuclopenthixol | 2 (10.5) | 4 (1.6) | 0.059 | |
*significant at p-value < 0.05; bold indicate significantly higher percent or value.
Fig. 3.
Individual antipsychotic and mean BNF factor with a p value of difference of p = 0.017.
The odds ratio of being in the high-TDD group were 2.618 (95 % CI 1.004–6.827, p = 0.049) for typical antipsychotics, 3.166 (95 % CI 1.227–8.172, p = 0.017) for quetiapine, 4.745 (95 % CI 1.828–12.317, p = 0.001) for olanzapine, and 9.300 (95 % CI 2.038–42.437, p = 0.004) for paliperidone. Data obtained using binary regression is presented in Table 3.
Table 3.
Binary logistic regression of factors affecting being in the high BNF factor group.
| B | S.E. | Wald | df | p-value | Odds ratio | 95 % CI |
||
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Female | 0.727 | 0.482 | 2.276 | 1 | 0.131 | 2.069 | 0.804 | 5.323 |
| Typical | 0.962 | 0.489 | 3.874 | 1 | 0.049* | 2.618 | 1.004 | 6.827 |
| Number of medication | −0.423- | 0.107 | 15.719 | 1 | <0.001* | 0.655 | 0.531 | 0.807 |
| Number of admission days | −0.005- | 0.003 | 2.150 | 1 | 0.143 | 0.995 | 0.989 | 1.002 |
| Haloperidol | 1.145 | 0.484 | 5.590 | 1 | 0.018* | 3.143 | 1.216 | 8.121 |
| Quetiapine | 1.152 | 0.484 | 5.675 | 1 | 0.017* | 3.166 | 1.227 | 8.172 |
| Olanzapine | 1.557 | 0.487 | 10.239 | 1 | 0.001* | 4.745 | 1.828 | 12.317 |
| Paliperidonelnevga | 2.230 | 0.775 | 8.290 | 1 | 0.004* | 9.300 | 2.038 | 42.437 |
*Significant at p < 0.05; CI: confidence interval; SE: standard error; df: degrees of freedom.
4. Discussion
The main finding of this study was the significant difference between the use of typical and atypical antipsychotics in terms of the TDD. The results showed that the use of typical antipsychotics was three times higher than that of atypical antipsychotics for the management of schizophrenia symptoms in Saudi patients. Pai et al. proposed a prevalence of 62 % atypical antipsychotics for individuals taking typical antipsychotics in the population(Pai et al., 2022). This is based on the recommendation guidelines of the National Institute for Health and Care Excellence (NICE) on the management of psychosis in patients with schizophrenia. Antipsychotic medications have significant side effects, including weight gain, metabolic disturbances, and movement disorders. Therefore, it is essential to prescribe an appropriate dose to minimise the risk of adverse effects while achieving optimal therapeutic outcomes.
In our study, two or more antipsychotics were prescribed to each patient. Monotherapy may not be effective in all patients, especially in those with severe or treatment-resistant symptoms(Englisch & Zink, 2012). According to the NICE guidelines, antipsychotic drugs can be used to treat patients with schizophrenia as monotherapy or in combinationtherapy (NICE, 2020). A study was conducted to assess the antipsychotic prescription pattern in the Middle East, including Egypt, Kuwait, Saudi Arabia, and the United Arab Emirates. The results showed that for the management of psychosis in patients with schizophrenia, 17 % of the prescribed antipsychotics were monotherapies and 20 % were a combination (Alkhadhari et al., 2015).
In this study, approximately half of the populations received aripiprazole followed by haloperidol and risperidone, which is similar to a study conducted in Korea that investigated high-dose antipsychotic medications that are more likely to be taken in combination rather than alone in patients with schizophrenia, and the most frequently used drugs within combinations of antipsychotics were haloperidol (51.4 %) and quetiapine (48.5 %) (Roh et al., 2014).
TDD calculators have been used to assist complement the BNF method in determining the appropriate dose of antipsychotic medication for patients with schizophrenia. Most patients received recommended daily doses of antipsychotics. However, 7 % of patients exceeded the recommended daily antipsychotic dose. Further, there was a significant correlation between BNF and several factors, including the class of antipsychotic, as well as number and type of medications. To this end, several studies have investigated the importance of using TDD calculators for antipsychotic medications(Stake-Nilsson et al., 2022). A previous study conclude that calculated dose equivalents based on Defined Daily Doses (DDDs) can be a useful resource for pharmacovigilance studies(Leucht et al., 2016).
Our study revealed that the use of haloperidol, olanzapine, paliperidone, and quetiapine significantly exceeded the recommended daily doses. According to the NICE guidelines, haloperidol can be administered intramuscularly to control psychosis associated with schizophrenia symptoms, with high doses being used to control the aggressive symptoms associated with psychosis in schizophrenic patients(Ostinelli et al., 2017). In addition, olanzapine and paliperidone can be used alone or in combination with either oral or injectable dosage forms, which may be the cause of the high daily dose.
The prescribing pattern for olanzapine has evolved over time, as more research has been conducted on its efficacy and safety. Initially, olanzapine was considered a highly effective medication for the treatment of schizophrenia and other psychotic disorders. However, one of the most significant concerns regarding olanzapine is its potential to cause weight gain and metabolic disturbances. Studies have shown that patients taking olanzapine are at an increased risk of developing diabetes, high blood pressure, and other obesity-related health problems. Consequently, many clinicians have become more cautious about prescribing olanzapine and may consider alternative medications or adjunctive therapies to manage these side effects. Despite these concerns, olanzapine remains an important medication for treating certain psychiatric conditions. It is considered one of the most effective medications for treating acute episodes of psychosis in patients with schizophrenia. Additionally, some patients may tolerate olanzapine better than other antipsychotic medications, or may not experience significant side effects. The TDD should be carefully monitored to balance symptom reduction, while minimising side effects. Therefore, TDD can provide regular clinical assessment for patients on antipsychotics(Sørup et al., 2020). Also, TDD assessment can help healthcare providers to closely monitor patients for determine the best treatment plan based on individual needs and preferences(Herzig et al., 2016).
Despite these positive findings, there are some limitations associated with the use of TDD calculators for antipsychotic medications. For instance, these calculators may not consider individual patient factors, such as drug interactions or comorbidities, which may affect dosing requirements(Aburamadan et al., 2021).
Our study has several strengths and limitations. To the best of our knowledge, this is the first antipsychotic-related TDD study conducted in Saudi Arabia. We used an ample period to provide a valid reflection on the current clinical practice. Absolutely, carefully monitoring the Total Daily Dose (TDD) of antipsychotic medications is crucial in balancing the reduction of psychiatric symptoms with the minimization of side effects. Achieving this balance is essential for the effective treatment of conditions such as schizophrenia, which often require long-term antipsychotic medication management. However, the study was limited by its descriptive nature. Therefore, future qualitative studies should investigate the underlying causes of high daily antipsychotic doses in schizophrenia.
In conclusion, the use of TDD calculators for antipsychotic medications is an effective tool for improving prescription practices and patient outcomes. However, healthcare providers should be aware of the limitations of these calculators and should use them in conjunction with clinical judgment and individual patient factors to determine the most appropriate dose of antipsychotic medication.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors would like to thank the Researcher Supporting Project number (RSPD2023R1019), King Saud University, Riyadh, Saudi Arabia. The author also would like to thank Prince Naif Health Research Center, Investigator support Unit for the language editing service provided.
Ethical Consideration
Ethical approval was obtained from the Institutional Review Board of King Saud University (IRB approval no. E-22-0395) and all participants provided written informed consent prior to their participation in the study.
Footnotes
Peer review under responsibility of King Saud University.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jsps.2023.101837.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- Aburamadan H., Sridhar S., Tadross T. Assessment of potential drug interactions among psychiatric inpatients receiving antipsychotic therapy of a secondary care hospital, United Arab Emirates. J. Adv. Pharm. Technol. Res. 2021;12(1):45–51. doi: 10.4103/japtr.JAPTR_110_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alkhadhari, S., al Zain, N., Darwish, T., Khan, S., Okasha, T., Ramy, H., & Tadros, T. M. (2015). Use of second-generation antipsychotics in the acute inpatient management of schizophrenia in the middle east. Neuropsychiatric Disease and Treatment, 11. https://doi.org/10.2147/NDT.S78788. [DOI] [PMC free article] [PubMed]
- Alosaimi F.D., Alzain N., Asiri S., Fallata E., Abalhassan M., Qrmli A., Alhabbad A. Patterns of psychiatric diagnoses in inpatient and outpatient psychiatric settings in Saudi Arabia. Rev. Psiquiatria Clin. 2017;44(3) doi: 10.1590/0101-60830000000124. [DOI] [Google Scholar]
- Ayani N., Morimoto T., Sakuma M., Kikuchi T., Watanabe K., Narumoto J. Antipsychotic polypharmacy is associated with adverse drug events in psychiatric inpatients: The Japan adverse drug events study. J. Clin. Psychopharmacol. 2021;41(4) doi: 10.1097/JCP.0000000000001416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Englisch, S., & Zink, M. (2012). Treatment-resistant schizophrenia: Evidence-based strategies. In Mens Sana Monographs (Vol. 10, Issue 1, pp. 20–32). https://doi.org/10.4103/0973-1229.91588. [DOI] [PMC free article] [PubMed]
- Herzig S.J., Rothberg M.B., Guess J.R., Stevens J.P., Marshall J., Gurwitz J.H., Marcantonio E.R. Antipsychotic use in hospitalized adults: Rates, indications, and predictors. J. Am. Geriatr. Soc. 2016;64(2):299–305. doi: 10.1111/jgs.13943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keepers G.A., Fochtmann L.J., Anzia J.M., Benjamin S., Lyness J.M., Mojtabai R., Servis M., Walaszek A., Buckley P., Lenzenweger M.F., Young A.S., Degenhardt A., Hong S.H. The American psychiatric association practice guideline for the treatment of patients with schizophrenia. Am. J. Psychiatry. 2020;177(9) doi: 10.1176/appi.ajp.2020.177901. [DOI] [PubMed] [Google Scholar]
- Lähteenvuo M., Tiihonen J. Antipsychotic polypharmacy for the management of schizophrenia: Evidence and recommendations. Drugs. 2021;81(11) doi: 10.1007/s40265-021-01556-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leucht S., Samara M., Heres S., Davis J.M. Dose equivalents for antipsychotic drugs: The DDD method. Schizophr. Bull. 2016;42:S90–S94. doi: 10.1093/schbul/sbv167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melnik, T., Soares, B. G., Puga, M. E. dos S., & Atallah, Á. N. (2010). Efficacy and safety of atypical antipsychotic drugs (quetiapine, risperidone, aripiprazole and paliperidone) compared with placebo or typical antipsychotic drugs for treating refractory schizophrenia: Overview of systematic reviews. In Sao Paulo Medical Journal (Vol. 128, Issue 3). https://doi.org/10.1590/s1516-31802010000300007. [DOI] [PMC free article] [PubMed]
- Ostinelli, E. G., Brooke-Powney, M. J., Li, X., & Adams, C. E. (2017). Haloperidol for psychosis-induced aggression or agitation (rapid tranquillisation). In Cochrane Database of Systematic Reviews (Vol. 2017, Issue 7). John Wiley and Sons Ltd. https://doi.org/10.1002/14651858.CD009377.pub3. [DOI] [PMC free article] [PubMed]
- Pai N., Acar M., Juneja P., Kouhkamari M.H., Siva S., Mullan J. Antipsychotic prescribing patterns in Australia: a retrospective analysis. BMC Psychiatry. 2022;22(1) doi: 10.1186/s12888-022-03755-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roh D., Chang J.G., Kim C.H., Cho H.S., An S.K., Jung Y.C. Antipsychotic polypharmacy and high-dose prescription in schizophrenia: A 5-year comparison. Aust. N. Z. J. Psychiatry. 2014;48(1):52–60. doi: 10.1177/0004867413488221. [DOI] [PubMed] [Google Scholar]
- Royal College of Psychiatrists. (2014). Consensus statement on high-dose antipsychotic medication. Royal College of Psychiatrists, October 2005.
- Seeman P. Atypical antipsychotics: Mechanism of action. Can. J. Psychiatry. 2002;47(1) doi: 10.1177/070674370204700106. [DOI] [PubMed] [Google Scholar]
- Sørup F.K.H., Brunak S., Eriksson R. Association between antipsychotic drug dose and length of clinical notes: A proxy of disease severity? BMC Med. Res. Method. 2020;20(1) doi: 10.1186/s12874-020-00993-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stake-Nilsson K., Almstedt M., Fransson G., Masoumi D., Elm A., Toratti-Lindgren M., Björkman A. Medication dosage calculation among nursing students: does digital technology make a difference? A literature review. BMC Nurs. 2022;21(1) doi: 10.1186/s12912-022-00904-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweileh W.M., Odeh J.B., Shraim N.Y., Zyoud S.H., Sawalha A.F., Al-Jabi S.W. Evaluation of Defined Daily Dose, percentage of British National Formulary maximum and chlorpromazine equivalents in antipsychotic drug utilization. Saudi Pharma. J. 2014;22(2) doi: 10.1016/j.jsps.2013.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbrouckef J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Bull. World Health Organization. 2007;85(11):867–872. doi: 10.2471/BLT.07.045120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yorston G., Pinney A. Chlorpromazine equivalents and percentage of British National Formulary maximum recommended dose in patients receiving high-dose antipsychotics. Psychiatr. Bull. 2000;24(4) doi: 10.1192/pb.24.4.130. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.