Abstract
Purpose of Review
This literature review aims to provide a comprehensive overview of the recent advances in prediction models and the deployment of AI and ML in the prediction of cardiopulmonary resuscitation (CPR) success. The objectives are to understand the role of AI and ML in healthcare, specifically in medical diagnosis, statistics, and precision medicine, and to explore their applications in predicting and managing sudden cardiac arrest outcomes, especially in the context of prehospital emergency care.
Recent Findings
The role of AI and ML in healthcare is expanding, with applications evident in medical diagnosis, statistics, and precision medicine. Deep learning is gaining prominence in radiomics and population health for disease risk prediction. There’s a significant focus on the integration of AI and ML in prehospital emergency care, particularly in using ML algorithms for predicting outcomes in COVID-19 patients and enhancing the recognition of out-of-hospital cardiac arrest (OHCA). Furthermore, the combination of AI with automated external defibrillators (AEDs) shows potential in better detecting shockable rhythms during cardiac arrest incidents.
Summary
AI and ML hold immense promise in revolutionizing the prediction and management of sudden cardiac arrest, hinting at improved survival rates and more efficient healthcare interventions in the future. Sudden cardiac arrest (SCA) continues to be a major global cause of death, with survival rates remaining low despite advanced first responder systems. The ongoing challenge is the prediction and prevention of SCA. However, with the rise in the adoption of AI and ML tools in clinical electrophysiology in recent times, there is optimism about addressing these challenges more effectively.
Keywords: Sudden cardiac arrest, Artificial intelligence, Machine learning, Prediction models, Cardiopulmonary resuscitation
Introduction
Sudden cardiac arrest (SCA) remains a prominent global cause of mortality comprising 15–20% of all deaths worldwide, and accounting for 50–100 cases per 100,000 individuals [1••, 2]. Cardiopulmonary resuscitation (CPR) administration and the use of electrical defibrillation are crucial interventions to achieve effective resuscitation in patients experiencing ventricular fibrillation (VF) rhythms and cardiac arrest [3]. Despite the existence of advanced first responder systems for cardiac arrest resuscitation, a recent analysis in North America revealed a meager overall survival rate of 4.6%. Unfortunately, a significant portion of administered shocks remain unsuccessful in achieving the return of spontaneous circulation [4, 5].
Several demographic, clinical, environmental, and genetic factors affect the incidence and survival rates of SCA victims. As for adults, SCA incidence rates are linked with increased age, while survival rates tend to be worse and higher death rates are seen among younger age groups [6, 7]. The prediction and prevention of SCA constitute significant challenges that hinder the effectiveness and cost–benefit of existing methodologies [8]. The utilization of artificial intelligence (AI) tools is on the rise for tackling intricate issues, and they are well-positioned to address the significant unmet requirement in the field of clinical electrophysiology. Consequently, AI tools have become crucial to differentiate the shockable subgroup of sudden cardiac arrest (SCA). There is an urgent demand to discover novel predictors of SCA in individuals [9]. Thus, here we aimed to review the recent advances in prediction models and the deployment of AI and machine learning (ML) in the prediction of CPR success.
Role of AI and ML in Healthcare
AI is a comprehensive term that encompasses the emulation of human intelligence in computer systems programmed to imitate human actions [10]. ML, which falls under the umbrella of AI, can be further classified into supervised and unsupervised learning and can be applied to clinical datasets for creating robust risk models and redefining patients’ classifications [11].
Nowadays, algorithms have already demonstrated superior abilities to detect malignant tumors compared to radiologists and have provided valuable guidance to researchers in constructing cohorts for expensive clinical trials [12]. The most intricate form of ML is deep learning, which encompasses neural network models with multiple levels of features to predict outcomes. These models can unveil thousands of hidden features, due to the accelerated processing capabilities of modern graphics processing units and cloud architectures [13].
The application of deep learning in radiomics, which involves detecting clinically relevant features in imaging data beyond the capabilities of human visual perception, is becoming increasingly prevalent [14]. Figure 1 illustrates the types of application and medical inputs used in deep learing vs. machine learning. Despite accurate predictions, integrating AI-based diagnosis and treatment recommendations into clinical workflows and electronic health record (EHR) systems can present challenges at times.
Fig. 1.
Machine learning vs. deep learning applications in healthcare
AI and ML in Prehospital Emergency Care
ML and AI applications facilitated the accurate prediction of outcomes that may be challenging for other risk-predicting tools to comprehend. Artificial neural networks (ANNs) have been employed to stratify the risk of intricate conditions like syncope in Emergency Care Departments (ED). ANNs are advantageous in this context due to their capability to evaluate complex and non-linear relationships between feature predictors and clinical outcomes [15, 16].
To date, only a limited number of studies have investigated the use of specific ML algorithms for predicting outcomes such as ICU admission or mortality in COVID-19 patients. Considering the potential value of ML-based decision rules and the critical nature of the pandemic, a collaborative endeavor is underway to identify the most effective ML applications for different datasets and diseases [17, 18].
Following the implementation of initiatives aimed at enhancing early recognition, dispatch protocols, bystander action, activation, and post-resuscitation care, several countries have witnessed an increase in survival rates after Out-of-Hospital Cardiac Arrest (OHCA) [19, 20]. In August 2018, a machine learning model was integrated into clinical practice at Copenhagen emergency medical services to enhance the recognition of OHCA. This model analyzed the conversation between the dispatcher and the caller, assisting the dispatcher in real-time to identify OHCA during the conversation. From September 2018 to December 2019, the machine learning model alerted dispatchers when an emergency call indicated a high probability of ongoing OHCA [21, 22].
AI Applications in Prehospital Emergency Care
An automated external defibrillator (AED) is a portable device that delivers the heart with electric shocks in cases of SCA to regain normal rhythm. The European Society for Cardiology (ESC) and European Resuscitation Council (ERC) advocate for the widespread adoption of AEDs by both emergency services and non-medical staff to minimize the time taken for defibrillation [23]. The combination of AED and AI has the potential to further enhance the effectiveness of AEDs and improve outcomes for people experiencing sudden cardiac arrest. One of the applications is improved detection of shockable rhythms that can cause patients’ death if an electrical shock is not immediately delivered [24]. Figuera et al. developed an ML model for the detection of shockable rhythms in AEDs based on surface ECGs and OHCA data which mimics the real-life scenario of the use AEDs [25•].
Previous literature supports the advantages of employing ML models in resuscitation. Specifically, a deep learning model has been developed to achieve more accurate predictions of cardiac arrest and acute respiratory failure in intensive care units, outperforming the National Early Warning Score (NEWS) and the Modified Early Warning Score (MEWS) [26, 27]. The superiority of this deep learning model was attributed to its ability to detect relationships between vital signs and the ability to identify features with high importance and contribution to predicting risk. Despite ML demonstrating superior performance compared to the existing track‐and‐trigger systems, it required the utilization of a greater number of variables for feature learning [28].
The Current State of the Field and Knowledge Gaps
AI has been explored for assessing the quality of CPR during resuscitation efforts. Computer vision algorithms can analyze video data from CPR training sessions or real-life events to provide real-time feedback to rescuers, helping them maintain correct compression depth, rate, and recoil [29]. A pilot study compared augmented reality (AR) CPR training with a standard audio-visual (AV) feedback manikin for healthcare providers and showed similar overall post-simulation CPR quality compared to standard AV feedback CPR training in healthcare providers [30]. In addition, AI algorithms have shown potential in automatically detecting cardiac arrest events in audio and video recordings. This can aid in faster recognition of cardiac arrest incidents and prompt initiation of CPR and AED use [31]. Not to mention the ability of AI in identifying areas with a higher likelihood of cardiac arrest incidents. This information can be used to improve emergency response planning and allocate resources more effectively and optimize the placement and distribution of AEDs in public spaces by analyzing historical cardiac arrest data, population density, and other factors [32–34].
While AI has shown promise in various aspects of healthcare, including medical imaging and diagnosis, its application in CPR and cardiac arrest management had some gaps and challenges. One of these challenges is the inability to adapt quickly to changes in patients’ conditions and provide real-time feedback to medical staff to adjust and enhance CPR [35, 36]. Also, integrating AI systems with existing AEDs and emergency response infrastructure requires careful consideration of data formats, communication protocols, and regulatory compliance [37].
AI-based Prognostic Models in Post-resuscitation Phase
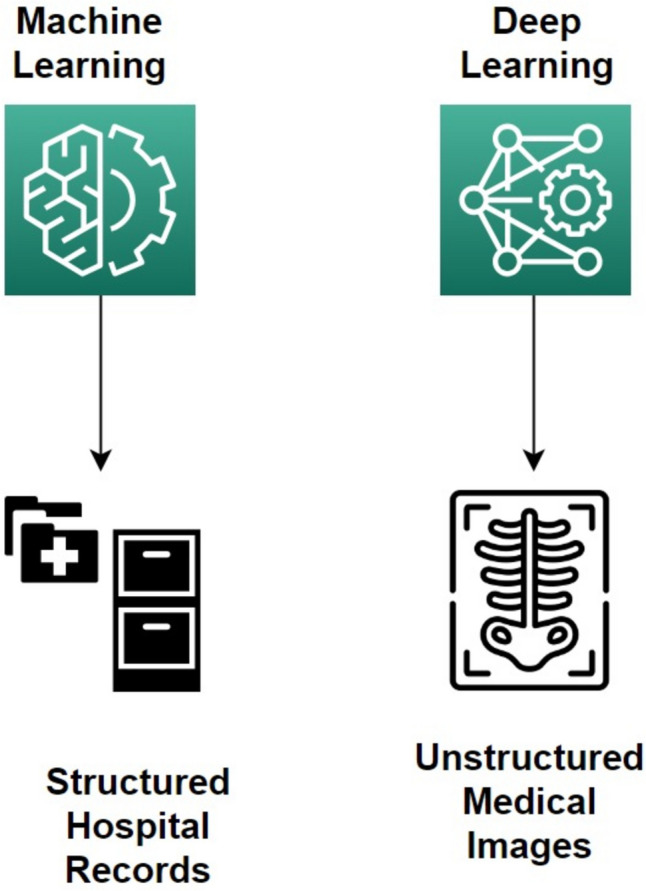
Cheng et al. proposed an ML-based model to predict the 30-day survival rate and survival-to-discharge rate after cardiac arrest of 1071 patients, showing the highest accuracy of 0.87 and 0.83 using the extreme gradient boosting (XGB) model compared to support vector machine (SVM) and logistic regression (LR) [38]. XGB models are a form of decision trees–based models, by combining decision tree models, where trees are incrementally included in the ensemble and trained to rectify the prediction errors of the preceding models. While SVM models implement a hyperplane that can distinctly group and classify samples [39]. Figure 2 shows the differences between XGB and SVM models. Harford et al. used embedded fully convolutional neural networks (EFCN) model to predict outcomes of survival for 2639 out-of-hospital cardiac arrests with 0.83 sensitivity using 27 features [40].
Fig. 2.
XGB vs. SVM model architecture
Use of AI in Predicting Neurological Outcomes After Resuscitation
Kawai et al. implemented an AI-based prognostic model for the prediction of neurological outcomes after 3 h of resuscitation from 321 cardiac arrest patients using CT images, showing better performance than the previous gray-to-white matter ratio (GWR) in terms of precision-recall which accounts for the false-positive predictions, but comparable in terms of area under receiver operating characteristics curve (AUROC) [41]. Mansour et al. established a transfer learning approach to detect hypoxic–ischemic brain injury (HIBI) following cardiac arrests. They used CT scans of normal findings, to detect the outcome on follow-up scans, suggesting that the progression of HIBI can be accurately identified by AI in the early initial scan [42]
AI in Cardio-Oncology Cardiac Arrests
With the co-prevalence of cardiovascular disease and cancer, cardio-oncology is expected to increase due to a globally aging population, and cardiac arrest, the second leading cause of medical death, is likely to be affected [43]. It is expected that the disparities in cardiac arrest observed in the general population would likely persist in the subgroup of patients with active cancer. However, the scarcity of research in this area has hindered effective efforts to address these ongoing disparities. A study by Monlezun et al. conducted a comprehensive analysis of cardio-oncology cardiac arrests, combining clinical, cost, and ethical aspects to improve effectiveness and cost-efficacy in healthcare systems. They developed a cardiac arrest risk prediction score for patients with cancer and introduced a novel clinical predictive model called The Cardiac Arrest Cardio-Oncology Score (CACOS), which can aid in the early prediction and improve resource allocation and health outcomes [44].
Utilizing AI to analyze cardiovascular data obtained from various diagnostic tests has shown promising results in accurately and inexpensively identifying cardiovascular risk, enabling early detection and intervention in cancer patients at risk for cardiovascular complications [45]. This approach has the potential to provide preventive and therapeutic opportunities in cardio-oncology, leading to better patient outcomes [46].
The Use of AI in Defibrillators
In clinical practice, both external defibrillators (EDs) and implantable cardioverter defibrillators (ICDs) employ shock advisory algorithms to determine whether an electrocardiogram (ECG) tracing represents a shockable or non-shockable rhythm. Recently, the use of ML algorithms has been evaluated for shock decision classification, demonstrating a growing level of accuracy in this important task [47]. ICDs are used in individuals at high risk of sudden cardiac death. The crucial factor in delivering an appropriate and potentially life-saving shock from the ICD or AED lies in identifying a shockable rhythm, such as ventricular fibrillation (VF) and ventricular tachycardia (VT) [48]. AI has the potential to make a significant impact by decreasing the time it takes to deliver a shock and enhancing the efficiency of identifying shockable rhythms. This could lead to saving more lives by ensuring timely and appropriate interventions in cases of ventricular fibrillation and ventricular tachycardia.
Research on shock decision algorithms has been framed traditionally as a VF detection problem. Subsequently, ML algorithms such as support vector machines or ensemble methods effectively merged systematic and comprehensive extraction of EKG features with the selection of the most suitable feature subsets for ventricular fibrillation (VF) detection [49].
Limitations of AI in Defibrillators
One of the limitations of AI solutions is that they necessitate large, annotated datasets to fine-tune the numerous trainable network parameters, often numbering in the thousands or even millions. Unfortunately, there is a scarcity of quality-controlled rhythm annotations in out-of-hospital cardiac arrest (OHCA) data. In addition, the use of AI in medical devices, including defibrillators, is subject to rigorous regulatory oversight to ensure safety and efficacy. Complying with these regulations can be time-consuming and resource-intensive [50]. Also, AI models can be vulnerable to adversarial attacks, where maliciously crafted inputs can lead to incorrect or harmful decisions. Securing AI algorithms in defibrillators from potential attacks is essential to maintain patient safety.
Conclusion
In conclusion, SCAs remain a significant global cause of mortality, highlighting the critical need for effective interventions such as cardiopulmonary resuscitation (CPR) and electrical defibrillation. Despite advances in first responder systems, survival rates after out-of-hospital cardiac arrest (OHCA) remain low, and a substantial number of administered shocks do not achieve the desired outcomes. This calls for innovative approaches to improve resuscitation and defibrillation success rates. The application of AI in prehospital emergency care has shown promise in detecting shockable rhythms, predicting resuscitation success, and enhancing CPR quality through real-time feedback. AI’s potential extends to predicting neurological outcomes after resuscitation and even addressing cardio-oncology cardiac arrests, improving risk prediction and resource allocation.
However, AI in defibrillators also faces limitations, including the need for large, annotated datasets, scarce quality-controlled rhythm annotations, regulatory challenges, and vulnerability to adversarial attacks. Future studies are needed to address data quality and biases, advance the interpretability of AI models, and ensure robust security measures. Moreover, further research is needed to validate and integrate AI-based models into clinical workflows and medical devices effectively. Collaboration between researchers, healthcare providers, and regulatory bodies is essential to harness AI's potential fully and drive continuous improvements in cardiac arrest management, ultimately leading to better patient outcomes and increased survival rates.
Acknowledgements
The publication fees of this article were covered thanks to the Qatar National Library (QNL) Open Access Fund.
Funding
Open Access funding provided by the Qatar National Library.
Data Availability
Data is derived from published studies.
Compliance with Ethical Standards
Competing Interests
The authors declare competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.•• Popescu DM, et al. Arrhythmic sudden death survival prediction using deep learning analysis of scarring in the heart. Nat Cardiovasc Res. 2022;1(4):334–43. 10.1038/s44161-022-00041-9. The significance of this study lies in its innovative contribution to addressing the substantial global issue of sudden cardiac death caused by arrhythmia. [DOI] [PMC free article] [PubMed]
- 2.Hayashi M, Shimizu W, Albert CM. The spectrum of epidemiology underlying sudden cardiac death. Circ Res. 2015;116(12):1887. doi: 10.1161/CIRCRESAHA.116.304521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Srinivasan NT, Schilling RJ. Sudden cardiac death and arrhythmias. Arrhythm Electrophysiol Rev. 2018;7(2):111.10.15420/AER.2018:15:2. [DOI] [PMC free article] [PubMed]
- 4.Nichol G, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300(12):1423–1431. doi: 10.1001/JAMA.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fishman GI, et al. Sudden cardiac death prediction and prevention: report from a National Heart. Lung, and Blood Institute and Heart Rhythm Society Workshop, Circulation. 2010;122(22):2335–2348. doi: 10.1161/CIRCULATIONAHA.110.976092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Allan KS, Morrison LJ, Pinter A, Tu JV, Dorian P. Unexpected high prevalence of cardiovascular disease risk factors and psychiatric disease among young people with sudden cardiac arrest. J Am Heart Assoc. 2019;8(2). 10.1161/JAHA.118.010330. [DOI] [PMC free article] [PubMed]
- 7.Atkins DL. Sudden cardiac arrest in a young population: not so unpredictable. J Am Heart Assoc. 2019;8(2). 10.1161/JAHA.118.011700. [DOI] [PMC free article] [PubMed]
- 8.Goldberger JJ, et al. American Heart Association/American College of Cardiology Foundation/Heart Rhythm Society scientific statement on noninvasive risk stratification techniques for identifying patients at risk for sudden cardiac death. A scientific statement from the American Heart Association Council on Clinical Cardiology Committee on Electrocardiography and Arrhythmias and Council on Epidemiology and Prevention, J Am Coll Cardiol. 2008;52(14):1179–1199. doi: 10.1016/j.jacc.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 9.Holmström L, Zhang FZ, Ouyang D, Dey D, Slomka PJ, Chugh SS. Artificial intelligence in ventricular arrhythmias and sudden death. Arrhythm Electrophysiol Rev. 2023;12. 10.15420/AER.2022.42. [DOI] [PMC free article] [PubMed]
- 10.Hamet P, Tremblay J. Artificial intelligence in medicine. Metabolism. 2017;69S:S36–S40. doi: 10.1016/J.METABOL.2017.01.011. [DOI] [PubMed] [Google Scholar]
- 11.Deo RC. Machine learning in medicine. Circulation. 2015;132(20):1920–1930. doi: 10.1161/CIRCULATIONAHA.115.001593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davenport T, Kalakota R. The potential for artificial intelligence in healthcare. Future Healthc J. 2019;6(2):94. doi: 10.7861/FUTUREHOSP.6-2-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sarker IH. Deep learning: a comprehensive overview on techniques, taxonomy, applications and research directions. SN Comput Sci. 2021;2(6):1–20. doi: 10.1007/S42979-021-00815-1/FIGURES/13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vial A, et al. The role of deep learning and radiomic feature extraction in cancer-specific predictive modelling: a review. Transl Cancer Res. 2018;7(3)803–816. 10.21037/TCR.2018.05.02.
- 15.Wang F. Machine learning for predicting rare clinical outcomes-finding needles in a haystack. JAMA Netw Open. 2021;4(5). 10.1001/JAMANETWORKOPEN.2021.10738. [DOI] [PubMed]
- 16.Dipaola F, et al. Multimodal deep learning for COVID-19 prognosis prediction in the emergency department: a bi-centric study. Sci Rep. 2023;13(1):10868. doi: 10.1038/S41598-023-37512-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bolourani S, et al. A machine learning prediction model of respiratory failure within 48 hours of patient admission for COVID-19: model development and validation. J Med Internet Res. 2021;23(2).10.2196/24246. [DOI] [PMC free article] [PubMed]
- 18.Subudhi S, et al. Comparing machine learning algorithms for predicting ICU admission and mortality in COVID-19. NPJ Digit Med. 2021;4(1). 10.1038/S41746-021-00456-X. [DOI] [PMC free article] [PubMed]
- 19.Hasselqvist-Ax I, et al. Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N Engl J Med. 2015;372(24):2307–2315. doi: 10.1056/NEJMOA1405796. [DOI] [PubMed] [Google Scholar]
- 20.Jensen TW, et al. The National Danish Cardiac Arrest Registry for out-of-hospital cardiac arrest - a registry in transformation. Clin Epidemiol. 2022;14:949–957. doi: 10.2147/CLEP.S374788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blomberg SN, et al. Effect of machine learning on dispatcher recognition of out-of-hospital cardiac arrest during calls to emergency medical services: a randomized clinical trial. JAMA Netw Open. 2021;4(1). 10.1001/JAMANETWORKOPEN.2020.32320. [DOI] [PMC free article] [PubMed]
- 22.Blomberg SN, et al. Machine learning as a supportive tool to recognize cardiac arrest in emergency calls. Resuscitation. 2019;138:322–329. doi: 10.1016/J.RESUSCITATION.2019.01.015. [DOI] [PubMed] [Google Scholar]
- 23.Priori SG, et al. ESC-ERC recommendations for the use of automated external defibrillators (AEDs) in Europe. Eur Heart J. 2004;25(5):437–445. doi: 10.1016/J.EHJ.2003.12.019. [DOI] [PubMed] [Google Scholar]
- 24.Hammad M, et al. Automated detection of shockable ECG signals: a review. Inf Sci (N Y) 2021;571:580–604. doi: 10.1016/J.INS.2021.05.035. [DOI] [Google Scholar]
- 25.• Figuera C, et al. Machine learning techniques for the detection of shockable rhythms in automated external defibrillators. PLoS One. 2016;11(7):e0159654. 10.1371/JOURNAL.PONE.0159654. The study underscores the potential of machine learning as a decision support tool for emergency. medical dispatchers. [DOI] [PMC free article] [PubMed]
- 26.Kim J, Chae M, Chang HJ, Kim YA, Park E. Predicting cardiac arrest and respiratory failure using feasible artificial intelligence with simple trajectories of patient data. J Clin Med. 2019;8(9). 10.3390/JCM8091336. [DOI] [PMC free article] [PubMed]
- 27.Kwon JM, Lee Y, Lee Y, Lee S, Park J. An algorithm based on deep learning for predicting in-hospital cardiac arrest. J Am Heart Assoc. 2018;7(13). 10.1161/JAHA.118.008678. [DOI] [PMC free article] [PubMed]
- 28.Churpek MM, Yuen TC, Winslow C, Meltzer DO, Kattan MW, Edelson DP. Multicenter comparison of machine learning methods and conventional regression for predicting clinical deterioration on the wards. Crit Care Med. 2016;44(2):368–374. doi: 10.1097/CCM.0000000000001571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sashidhar D, et al. Machine learning and feature engineering for predicting pulse presence during chest compressions. R Soc Open Sci. 2021;8(11). 10.1098/RSOS.210566. [DOI] [PMC free article] [PubMed]
- 30.Leary M, McGovern SK, Balian S, Abella BS, Blewer AL. A pilot study of CPR quality comparing an augmented reality application vs. a standard audio-visual feedback manikin. Front Digit Health. 2020;2. 10.3389/FDGTH.2020.00001. [DOI] [PMC free article] [PubMed]
- 31.Kwon JM, Kim KH, Jeon KH, Lee SY, Park J, Oh BH. Artificial intelligence algorithm for predicting cardiac arrest using electrocardiography. Scand J Trauma Resusc Emerg Med. 2020;28(1). 10.1186/S13049-020-00791-0. [DOI] [PMC free article] [PubMed]
- 32.Smith CM, et al. Barriers and facilitators to public access defibrillation in out-of-hospital cardiac arrest: a systematic review. Eur Heart J Qual Care Clin Outcomes. 2017;3(4):264–273. doi: 10.1093/ehjqcco/qcx023. [DOI] [PubMed] [Google Scholar]
- 33.Brooks SC, et al. Optimizing outcomes after out-of-hospital cardiac arrest with innovative approaches to public-access defibrillation: a scientific statement from the international liaison committee on resuscitation. Circulation. 2022;145(13):E776–E801. doi: 10.1161/CIR.0000000000001013. [DOI] [PubMed] [Google Scholar]
- 34.Brooks SC, et al. Optimizing outcomes after out-of-hospital cardiac arrest with innovative approaches to public-access defibrillation: a scientific statement from the International Liaison Committee on Resuscitation. Resuscitation. 2022;172:204–228. doi: 10.1016/J.RESUSCITATION.2021.11.032. [DOI] [PubMed] [Google Scholar]
- 35.Santos OC. Training the body: the potential of AIED to support personalized motor skills learning. Int J Artif Intell Educ. 2016;26(2):730–755. doi: 10.1007/S40593-016-0103-2/TABLES/2. [DOI] [Google Scholar]
- 36.Di Mitri D, Schneider J, Drachsler H. Keep me in the loop: real-time feedback with multimodal data. Int J Artif Intell Educ. 2022;32(4):1093–1118. doi: 10.1007/S40593-021-00281-Z/TABLES/3. [DOI] [Google Scholar]
- 37.Sloane EB, Silva RJ. Artificial intelligence in medical devices and clinical decision support systems. Clin Eng Handbook. 2020;556. 10.1016/B978-0-12-813467-2.00084-5.
- 38.Cheng CY, Chiu IM, Zeng WH, Tsai CM, Lin CHR. Machine learning models for survival and neurological outcome prediction of out-of-hospital cardiac arrest patients. Biomed Res Int. 2021;2021. 10.1155/2021/9590131. [DOI] [PMC free article] [PubMed]
- 39.Fan J, et al. Comparison of support vector machine and extreme gradient boosting for predicting daily global solar radiation using temperature and precipitation in humid subtropical climates: a case study in China. Energy Convers Manag. 2018;164:102–111. doi: 10.1016/J.ENCONMAN.2018.02.087. [DOI] [Google Scholar]
- 40.Harford S, et al. A machine learning based model for out of hospital cardiac arrest outcome classification and sensitivity analysis. Resuscitation. 2019;138:134–140. doi: 10.1016/J.RESUSCITATION.2019.03.012. [DOI] [PubMed] [Google Scholar]
- 41.Kawai Y, Kogeichi Y, Yamamoto K, Miyazaki K, Asai H, Fukushima H. Explainable artificial intelligence-based prediction of poor neurological outcome from head computed tomography in the immediate post-resuscitation phase. Sci Rep. 2023;13(1):1–8. 10.1038/s41598-023-32899-5. [DOI] [PMC free article] [PubMed]
- 42.Mansour A, et al. Machine learning for early detection of hypoxic-ischemic brain injury after cardiac arrest. Neurocrit Care. 2022;36(3):974–982. doi: 10.1007/S12028-021-01405-Y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Giza DE, et al. Impact of cardiopulmonary resuscitation on survival in cancer patients: do not resuscitate before or after CPR? JACC CardioOncol. 2020;2(2):359–362. doi: 10.1016/J.JACCAO.2020.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Monlezun DJ, et al. Artificial intelligence-augmented propensity score, cost effectiveness and computational ethical analysis of cardiac arrest and active cancer with novel mortality predictive score. Medicina (B Aires). 2022;58(8). 10.3390/MEDICINA58081039. [DOI] [PMC free article] [PubMed]
- 45.Kostakou PM, Kouris NT, Kostopoulos VS, Damaskos DS, Olympios CD. Cardio-oncology: a new and developing sector of research and therapy in the field of cardiology. Heart Fail Rev. 2019;24(1):91–100. doi: 10.1007/S10741-018-9731-Y. [DOI] [PubMed] [Google Scholar]
- 46.Rhee JW, Ky B, Armenian SH, Yancy CW, Wu JC. Primer on biomarker discovery in cardio-oncology: application of omics technologies. JACC CardioOncol. 2020;2(3):379–384. doi: 10.1016/J.JACCAO.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brown G, et al. Role of artificial intelligence in defibrillators: a narrative review. Open Heart. 2022;9(2):e001976. 10.1136/OPENHRT-2022-001976. [DOI] [PMC free article] [PubMed]
- 48.Priori SG, et al. 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death the Task Force for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death of the European Society of Cardiology (ESC) endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC) EP Europace. 2015;17(11):1601–1687. doi: 10.1093/EUROPACE/EUV319. [DOI] [PubMed] [Google Scholar]
- 49.Jaureguibeitia X, et al. Shock decision algorithms for automated external defibrillators based on convolutional networks. IEEE Access. 2020;8:154746–154758. doi: 10.1109/ACCESS.2020.3018704. [DOI] [Google Scholar]
- 50.Rad AB, et al. ECG-Based classification of resuscitation cardiac rhythms for retrospective data analysis. IEEE Trans Biomed Eng. 2017;64(10):2411–2418. doi: 10.1109/TBME.2017.2688380. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is derived from published studies.