Key Clinical Message
Remote intracerebral hemorrhage (RICH) is a rare yet highly consequential complication that can occur after a craniotomy performed for the evacuation of an intracerebral hemorrhage (ICH). In this case report, we present the clinical details of a 74‐year‐old female patient who underwent a supratentorial craniotomy to address an ICH, and subsequently developed RICH. A 74‐year‐old woman was admitted to our department with a severe headache, onset of dysarthria, and left‐sided brachio‐crural hemiparesis. The patient had a history of arterial hypertension and a previous cerebral ischemia incident 2 years prior, potentially due to cerebral amyloid angiopathy. Despite the immediate surgical intervention and intensive care, she succumbed to respiratory distress after developing a contralateral ICH. RICH following craniotomy for an intracerebral hematoma is a rare but potentially devastating complication. Close monitoring, prompt recognition of neurological deterioration, and timely intervention are imperative to optimize patient outcomes. Further research is needed to better understand the underlying mechanisms and risk factors associated with this complication, allowing for improved prevention and management strategies in the future.
Keywords: amyloid angiopathy, arterial hypertension, craniotomy, intracerebral hematoma, remote intracerebral hemorrhage
Emblematic images of a contralateral/remote left parietal intracerebral hemorrhage following craniotomy and drainage of a right temporo‐parietal intracerebral hematoma.

1. INTRODUCTION
Remote intracerebral hemorrhage (RICH), occurring remote to the surgical site following craniotomy, is a rare but potentially devastating complication. 1 Although the exact pathophysiology remains unclear, RICH has been attributed to various mechanisms, including reperfusion injury, altered cerebral hemodynamics, and impaired autoregulation. 2 , 3 We present a case of RICH following craniotomy for an intracerebral hematoma, emphasizing the need for vigilance and appropriate management in patients undergoing surgical evacuation.
2. CASE PRESENTATION
A 74‐year‐old female patient presented to our department exhibiting severe headache, onset of dysarthria, and left‐sided brachio‐crural hemiparesis. The patient's medical history was notable for arterial hypertension and a previous episode of cerebral ischemia 2 years prior, potentially linked to cerebral amyloid angiopathy (CAA). Indeed, the patient had undergone brain MRI examination, which clearly demonstrates the characteristic microbleeds associated with CAA in the T2 gradient echo sequences (Figure 1).
FIGURE 1.

Brain MRI axial images in series demonstrating the characteristic microbleeds associated with cerebral amyloid angiopathy in the T2‐weighted gradient echo sequences. Cerebral microhemorrhages, defined as 2–10 mm, round, or ovoid areas of hemorrhage, tend to be cortico‐subcortical (at the gray‐white matter junction) and spare the basal ganglia and pons, in contrast to hypertensive microhemorrhages.
2.1. Initial diagnostic assessment
An immediate brain CT scan revealed an extensive intracerebral hemorrhage in the right temporo‐parietal region, causing a significant mass effect and a leftward shift of median structures by 10 mm. An early right uncal herniation was also observed (Figure 2). Notably, the patient's dysarthria was primarily attributed to brainstem compression resulting from the intracerebral hemorrhage.
FIGURE 2.

Preoperative brain CT axial (A), sagittal (B), and coronal (C) images show an extensive intracerebral hemorrhage in the right temporo‐parietal region, causing a significant mass effect and a leftward shift of median structures by 10 mm. An early right uncal herniation was also documented.
2.2. Clinical findings
During the CT scan, the patient's neurological status worsened, with a Glasgow Coma Scale (GCS) score of 9/15 (E2V2M5). This necessitated immediate surgical intervention.
2.3. Therapeutic intervention
An emergency fronto‐temporo‐parietal right craniotomy was performed to evacuate the intracerebral hematoma and relieve cerebral tension. The pupils remained isochoric and isocyclic even after the surgical procedure. Subsequently, the patient was transferred to the intensive care unit (ICU).
2.4. Follow‐up and outcomes
A postoperative brain CT scan performed 6 h later showed the surgical outcomes and the presence of a contralateral intracerebral hemorrhage in the left parietal region, measuring approximately 50 mm, without shift of median structures (Figure 3). A further brain CT scan conducted 24 h later revealed an additional extension of the contralateral intracerebral hematoma (Figure 4). Despite intensive care and multiparametric monitoring, the patient succumbed to respiratory distress on postoperative Day 3.
FIGURE 3.
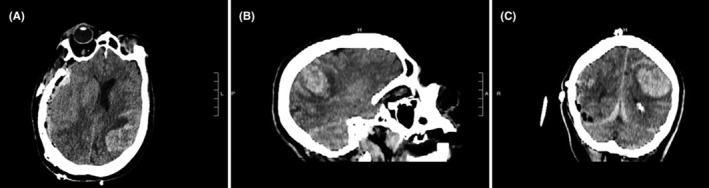
6‐h postoperative brain CT axial (A), sagittal (B), and coronal (C) images show the presence of a contralateral intracerebral hemorrhage in the left parietal region, measuring approximately 50 mm, without shift of median structures.
FIGURE 4.

24‐h postoperative brain CT axial (A), sagittal (B), and coronal (C) images revealed an additional extension of the contralateral intracerebral hematoma.
3. DISCUSSION
RICH following craniotomy for intracerebral hematoma evacuation is an uncommon but serious complication. The reported incidence of remote ICH ranges from 1% to 2% of cases. 4 The exact mechanisms underlying remote ICH are not fully understood, but several theories have been proposed. 2 , 5 , 6 , 7 , 8 , 9 These include altered cerebral hemodynamics, impaired autoregulation, reperfusion injury, and disruption of the blood–brain barrier.
Altered cerebral hemodynamics following craniotomy and hematoma evacuation may contribute to the development of RICH. Surgical manipulation, including retraction of brain tissue and disruption of normal vascular pathways, can lead to changes in blood flow dynamics. This alteration in cerebral perfusion may result in ischemia or hemorrhage in remote regions of the brain. 10 , 11
Impaired autoregulation, the ability of cerebral blood vessels to maintain a constant blood flow despite changes in perfusion pressure, may also play a role. The disruption of autoregulation during the surgical procedure and the subsequent release of increased intracranial pressure after hematoma evacuation can lead to dysregulation of cerebral blood flow, predisposing to remote ICH.
Reperfusion injury is another proposed mechanism. The release of increased intracranial pressure following hematoma evacuation can lead to reperfusion of previously compromised brain tissue. This reperfusion may trigger an inflammatory response, oxidative stress, and disruption of the blood–brain barrier, ultimately resulting in remote hemorrhage. 10
In the context of a RICH following a supratentorial craniotomy, CAA could be a possible cause of hematomas distant from the surgical site, contralateral to the craniotomy. 12 During the craniotomy, the brain is manipulated, and damage to surrounding blood vessels can occur. If a patient has pre‐existing CAA, the vessel fragility caused by amyloid deposition could increase the risk of bleeding both at the surgical site and in other areas of the brain. 13 , 14 However, it is important to note that there could be other causes of hematomas distant from the surgical site after a craniotomy. For example, the use of anticoagulant or antiplatelet medications can increase the risk of bleeding. 15 , 16 Additionally, manipulation of the brain during surgery can cause vessel injury irrespective of the presence of amyloid angiopathy.
However, the association between CAA and RICH following a supratentorial craniotomy is not well‐established. Normally, a remote hematoma occurs because of alterations in intracranial pressure or blood flow, which can arise after brain surgery. It cannot be ruled out that CAA may contribute to such hematomas, particularly if the compromised blood vessels are exposed to stress or changes in pressure.
The diagnosis of remote ICH requires prompt imaging, typically with CT or MRI. These modalities can identify the presence of remote hemorrhage, assess its size and location, evaluate midline shift, and detect associated mass effect. In our case, a repeat CT scan revealed a left‐sided intracerebral hemorrhage, confirming the diagnosis. 5
Management of remote ICH depends on the patient's clinical status, the extent of the hemorrhage, and the presence of mass effect. Surgical intervention, such as hematoma evacuation and decompressive craniectomy, may be necessary to relieve mass effect and prevent further neurological deterioration. Medical management, including blood pressure control and correction of coagulopathy, is also important.
The prognosis of patients with remote ICH varies and depends on factors such as the initial severity of the hemorrhage, the extent of neurological injury, and the timeliness of intervention. Rehabilitation and neurorehabilitation play a crucial role in optimizing functional recovery and improving the patient's quality of life.
4. CONCLUSIONS
RICH following a supratentorial craniotomy for an intracerebral hematoma is a rare but potentially devastating complication. The exact mechanisms remain unclear, but altered cerebral hemodynamics, impaired autoregulation, and reperfusion injury are thought to contribute. Prompt recognition, close monitoring, and timely intervention are essential for optimizing patient outcomes. Further research is needed to improve our understanding of this complication and develop strategies for prevention and management.
AUTHOR CONTRIBUTIONS
Gianluca Scalia: Conceptualization; data curation; methodology; software; validation; writing – original draft; writing – review and editing. Manikon Poullay Silven: Conceptualization; data curation; writing – review and editing. Roberta Costanzo: Data curation; methodology; visualization; writing – review and editing. Bipin Chaurasia: Validation; visualization. Massimo Furnari: Visualization. Domenico Gerardo Iacopino: Supervision. Giovanni Federico Nicoletti: Supervision. Giuseppe Emmanuele Umana: Supervision; validation; writing – review and editing.
FUNDING INFORMATION
No funding was received for this case report.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest related to this case report.
ETHICS STATEMENT
None.
CONSENT
Written informed consent was obtained from the patient's next of kin.
ACKNOWLEDGMENTS
We would like to acknowledge the medical and nursing staff involved in the care of this patient.
Scalia G, Silven MP, Costanzo R, et al. Remote intracerebral hemorrhage following craniotomy for an intracerebral hematoma: A case report. Clin Case Rep. 2023;11:e8271. doi: 10.1002/ccr3.8271
DATA AVAILABILITY STATEMENT
Data sharing not applicable—no new data generated, or the article describes entirely theoretical research.
REFERENCES
- 1. Brisman MH, Bederson JB, Sen CN, Germano IM, Moore F, Post KD. Intracerebral hemorrhage occurring remote from the craniotomy site. Neurosurgery. 1996;39(6):1114‐1122. doi: 10.1097/00006123-199612000-00009 [DOI] [PubMed] [Google Scholar]
- 2. Cohen‐Gadol AA. Remote contralateral intraparenchymal hemorrhage after overdrainage of a chronic subdural hematoma. Int J Surg Case Rep. 2013;4(10):834‐836. doi: 10.1016/j.ijscr.2013.06.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nagasaki H, Yamakawa K, Mochizuki Y, et al. Remote supratentorial hemorrhage following supratentorial craniotomy: a case report. NMC Case Rep J. 2015;3(1):13‐16. doi: 10.2176/nmccrj.cr.2015-0131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Smith ER, Carter BS, Ogilvy CS. Proposed use of prophylactic decompressive craniectomy in poor‐grade aneurysmal subarachnoid hemorrhage patients presenting with associated large sylvian hematomas. Neurosurgery. 2002;51(1):117‐124. [DOI] [PubMed] [Google Scholar]
- 5. Umana GE, Salvati M, Fricia M, et al. A review of remote intracerebral hemorrhage after chronic subdural hematoma evacuation. J Neurol Surg A Cent Eur Neurosurg. 2022;83(4):368‐376. doi: 10.1055/s-0041-1739220 [DOI] [PubMed] [Google Scholar]
- 6. Rusconi A, Sangiorgi S, Bifone L, Balbi S. Infrequent hemorrhagic complications following surgical drainage of chronic subdural hematomas. J Korean Neurosurg Soc. 2015;57(5):379‐385. doi: 10.3340/jkns.2015.57.5.379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rapanà A, Lamaida E, Pizza V. Multiple postoperative intracerebral haematomas remote from the site of craniotomy. Br J Neurosurg. 1998;12(4):364‐368. doi: 10.1080/02688699844916 [DOI] [PubMed] [Google Scholar]
- 8. Landeiro JA, Flores MS, Lapenta MA, Galdino AC, Lázaro BC. Remote hemorrhage from the site of craniotomy. Arq Neuropsiquiatr. 2004;62(3B):832‐834. doi: 10.1590/s0004-282X2004000500017 [DOI] [PubMed] [Google Scholar]
- 9. Waga S, Shimosaka S, Sakakura M. Intracerebral hemorrhage remote from the site of the initial neurosurgical procedure. Neurosurgery. 1983;13(6):662‐665. doi: 10.1227/00006123-198312000-00008 [DOI] [PubMed] [Google Scholar]
- 10. Lee I, Park CW, You CJ, et al. Risk factors of postoperative remote intracerebral hemorrhage after craniotomy for ruptured cerebral aneurysms. J Cerebrovasc Endovasc Neurosurg. 2020;22(2):53‐64. doi: 10.7461/jcen.2020.22.2.53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Xu K, Chen X, Piao J, Yu J. Remote multiple intraparenchymal hemorrhages following aneurysmal clipping of the anterior communicating artery: a case report and literature review. Turk Neurosurg. 2015;25(4):653‐656. doi: 10.5137/1019-5149.JTN.9150-13.0 [DOI] [PubMed] [Google Scholar]
- 12. Ritter MA, Droste DW, Hegedüs K, et al. Role of cerebral amyloid angiopathy in intracerebral hemorrhage in hypertensive patients. Neurology. 2005;64(7):1233‐1237. doi: 10.1212/01.WNL.0000156522.93403.C3 [DOI] [PubMed] [Google Scholar]
- 13. Tseng JH, Hsiao SH, Chang YC. Cerebral amyloid angiopathy with frequent intracerebral hemorrhage: a pitfall for neurosurgeons. Formos J Surg. 2012;45(1):25‐28. doi: 10.1016/j.fjs.2011.11.005 [DOI] [Google Scholar]
- 14. Sigüenza González R, Gómez San Martín E. Amyloid angiopathy as a cause of "intracranial remote hemorrhage" in a patient treated with fibrinolysis. Radiologia (Engl Ed). 2019;61(3):266‐268. doi: 10.1016/j.rx.2018.08.003 [DOI] [PubMed] [Google Scholar]
- 15. Flaherty ML. Anticoagulant‐associated intracerebral hemorrhage. Semin Neurol. 2010;30(5):565‐572. doi: 10.1055/s-0030-1268866 [DOI] [PubMed] [Google Scholar]
- 16. Umana GE, Scalia G, Fricia M, et al. Diamond‐shaped mini‐craniotomy: A new concept in neurosurgery. J Neurol Surg A Cent Eur Neurosurg. 2022;83(3):236‐241. doi: 10.1055/s-0041-1730942 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable—no new data generated, or the article describes entirely theoretical research.


