Abstract
Background
Older adults are at greater risk of medication-related harm than younger adults. The Integrated Medication Management model is an interdisciplinary method aiming to optimize medication therapy and improve patient outcomes.
Objective
We aimed to investigate the cost effectiveness of a medication optimization intervention compared to standard care in acutely hospitalized older adults.
Methods
A cost-utility analysis including 285 adults aged ≥ 70 years was carried out alongside the IMMENSE study. Quality-adjusted life years (QALYs) were derived using the EuroQol 5-Dimension 3-Level Health State Questionnaire (EQ-5D-3L). Patient-level data for healthcare use and costs were obtained from administrative registers, taking a healthcare perspective. The incremental cost-effectiveness ratio was estimated for a 12-month follow-up and compared to a societal willingness-to-pay range of €/QALY 27,067–81,200 (NOK 275,000–825,000). Because of a capacity issue in a primary care resulting in extended hospital stays, a subgroup analysis was carried out for non-long and long stayers with hospitalizations < 14 days or ≥ 14 days.
Results
Mean QALYs were 0.023 [95% confidence interval [CI] 0.022–0.025] higher and mean healthcare costs were €4429 [95% CI − 1101 to 11,926] higher for the intervention group in a full population analysis. This produced an incremental cost-effectiveness ratio of €192,565/QALY. For the subgroup analysis, mean QALYs were 0.067 [95% CI 0.066–0.070, n = 222] and − 0.101 [95% CI − 0.035 to 0.048, n = 63] for the intervention group in the non-long stayers and long stayers, respectively. Corresponding mean costs were €− 824 [95% CI − 3869 to 2066] and €1992 [95% CI − 17,964 to 18,811], respectively. The intervention dominated standard care for the non-long stayers with a probability of cost effectiveness of 93.1–99.2% for the whole willingness-to-pay range and 67.8% at a zero willingness to pay. Hospitalizations were the main cost driver, and readmissions contributed the most to the cost difference between the groups.
Conclusions
According to societal willingness-to-pay thresholds, the medication optimization intervention was not cost effective compared to standard care for the full population. The intervention dominated standard care for the non-long stayers, with a high probability of cost effectiveness.
Clinical Trial Registration
The IMMENSE trial was registered in ClinicalTrials.gov on 28 June, 2016 before enrolment started (NCT02816086).
Supplementary Information
The online version contains supplementary material available at 10.1007/s40266-023-01077-7.
Key Points for Decision Makers
| This is the first cost-utility analysis alongside a clinical trial of an integrated medicine management intervention to be published to date. |
| The intervention was more effective and cost less than standard care with a high probability of cost effectiveness in older adults aged ≥ 70 years with hospital stays up to 14 days. |
| The intervention consistently produced more quality-adjusted life years than standard care and was not costly compared to other care activities. |
Background
Older adults are at greater risk of medication-related harm than younger adults, leading to increased rates of hospitalization and other healthcare resource use, and reduced health-related quality of life [1, 2]. Receiving potentially inappropriate medications, experiencing an adverse drug reaction, or having an adverse drug reaction caused by potentially inappropriate medications is associated with disproportionally high healthcare costs. Improved prescribing quality in older adults may hence potentially improve patient outcomes and associated resource use [3].
The Integrated Medication Management (IMM) model is an interdisciplinary method aiming to optimize medication therapy and improve patient outcomes. The IMM model has previously been shown to reduce healthcare use [4] and increase survival time [5]. However, other studies have been unable to demonstrate similar results [6, 7]. A recent Cochrane review by Bülow et al. investigating the effect of medication reviews on 15,076 hospitalized patients reported that the number needed to treat was 29 to prevent one hospital readmission [8]. The authors pointed out a lack of health-related quality of life (HRQoL) data and the need for cost-effectiveness analyses for such interventions.
The IMMENSE (IMprove MEdicatioN Safety in the Elderly) study was a randomized controlled trial (RCT) designed to investigate the effect of an IMM intervention in acutely hospitalized older adults. The primary outcome was the rate of emergency medical visits (acute readmissions and visits to emergency departments) 12 months after the index hospitalization. Although the study did not demonstrate a statistically significant effect on the primary outcome of the study [9], a cost-utility analysis (CUA) was pre-planned before performing the main analysis of the study. No CUA alongside a clinical trial of an IMM intervention has been published to date, and such analyses can guide resource allocation in healthcare. The aim of this study was to investigate the cost effectiveness of the delivered intervention compared to standard care in acutely hospitalized older adults.
Methods
This trial-based CUA is reported according to the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) [10]. The CHEERS 2022 checklist is included in the Electronic Supplementary Material (ESM). We used an intention-to-treat approach employing data collected during the IMMENSE study and health register data for the included patients. Previous publications from the IMMENSE study include the study protocol [11], the effectiveness evaluation for the primary and secondary outcomes [9], and an intervention fidelity analysis [12].
Study Design and Study Population
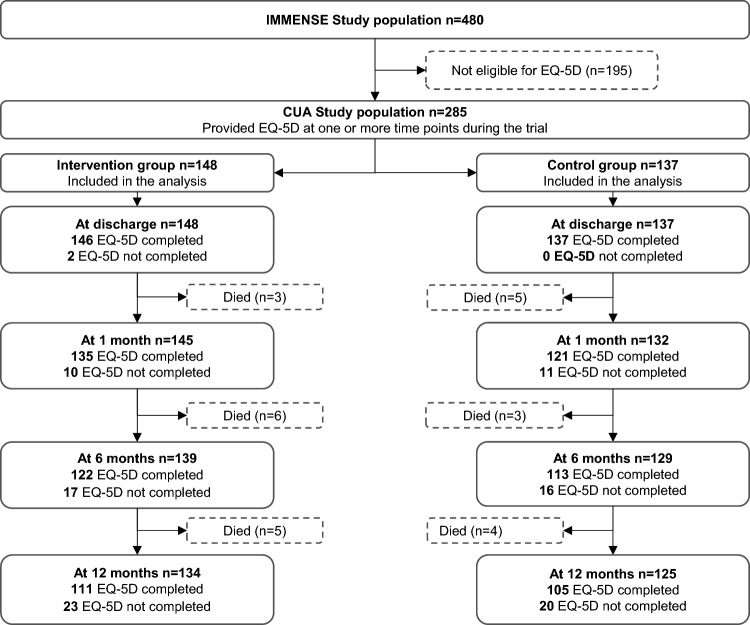
Patients were recruited from September 2016 to December 2019 at two internal medicine wards at the University Hospital of North Norway: one geriatric ward (Ward 1) and one general medicine ward (Ward 2). Patients aged ≥ 70 years acutely admitted to the wards and willing to provide written informed consent (patient or next of kin) were randomized into two groups (1:1). The intervention group received the intervention in addition to standard care, and the control group received standard care only. Follow-up time was 12 months after discharge. According to the study protocol, patients for whom the next of kin provided informed consent were excluded from HRQoL measurements [11]. We have included 285 patients (intervention group, n = 148 and control group, n = 137) of the 480 IMMENSE trial population who were eligible for HRQoL and provided one or more such measurements in the CUA (Fig. 1).
Fig. 1.
Study flowchart showing the EuroQol 5-dimension 3-level questionnaire (EQ-5D-3L) completed or not completed at discharge, 1 month, 6 months, and 12 months in the study follow-up period. CUA cost-utility analysis
The Intervention
The intervention in the IMMENSE study comprised five steps: (i) medication reconciliation at admission; (ii) medication review during the hospital stay; (iii) patient counseling about the use of medicines; (iv) comprehensible and patient-friendly dissemination of the medication list with explanations in discharge summary; and (v) post-discharge phone call to the primary care provider (regular general practitioner or nursing home physician/nurse). The first four steps were completed during the index hospital stay. The fifth step was completed shortly after discharge, aiming to improve the communication of recommendations across care levels.
Health-Related Quality of Life
Health-related quality of life was measured using the EuroQol 5-Dimension 3-Level Health State Questionnaire (EQ-5D-3L) [13]. The five dimensions of the questionnaire are mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each dimension has three possible response levels, namely no problems, moderate problems, or severe problems. A trained study nurse blinded to the study group allocation collected the EQ-5D-3L data at the time of discharge from the index hospital stay and at 1, 6, and 12 months after discharge. The data collection was performed face-to-face with the participants at discharge in Ward 1, while all remaining collections were completed over the phone. We used the three-level version because of cognitive consideration and practicalities (i.e., time to administer the questionnaire).
As recommended by Norwegian authorities owing to a lack of Norwegian tariffs [14], utility values were derived using the UK time-trade-off societal value set, translating the EQ-5D-3L responses for each collection time to a utility value between one for perfect health, zero for death, or below zero for conditions worse than death [15]. This was completed starting with a utility of 1 and subtracting according to the algorithm for each reported problem in each of the five dimensions [15]. Quality-adjusted life years (QALYs) were calculated for each respondent for the 12-month follow-up as the area under the curve combining the utility value for each collection time, assuming a linear change between each timepoint. Because of the acute care setting, the first measurement was performed at discharge after the intervention had been initiated and we consequently did not have a baseline measurement available. However, assuming a common fixed baseline is considered to ensure a minimal bias to the QALY estimation when the first measurement is taken close to the time of baseline and in a series of measurements over a 12-month follow-up [16]. We therefore assumed a baseline utility score for all patients equal to the mean discharge utility for the control group. Patients who died during the follow-up were assigned a utility value of 0 at the collection times following their death. Missing utility values for any collection times were 9.1% and were assumed to be missing at random.
Healthcare Resource Use and Costs
Individual-level resource use and costs were obtained from administrative registers and linked with other trial data using the unique national identity numbers [17]. Hospital resource-use data (index stay and readmissions, inpatient and outpatient hospital care) were obtained from the hospital’s administrative Cost Per Patient register, an activity-based costing register with patient-level costs per episode. Primary care resource-use data (general practitioner, specialist physician, and emergency room visits) were obtained from the Norwegian Control and Payment of Health Reimbursements Database (KUHR), a national administrative database with patient-level costs per episode for all primary healthcare, including patient contributions and healthcare provider reimbursements from the state for treatment and material costs. All costs covered the time horizon from 12 months before inclusion in the study until 12 months after discharge from the index hospitalization. A health provider perspective was taken, including costs of health service use during the trial period. Costs were transformed to 2021 values using the Norwegian inflation index for health [18] and translated to Euros (€) using the 2021 exchange rate (€1 = NOK 10.16) [19].
The intervention cost was estimated based on mean pharmacist salary costs from Statistics Norway [20] adjusted to 2021 values using the Norwegian inflation index for healthcare [18] and social costs (factor 1.4). This produced a cost per hour of €69. We assumed that one clinical pharmacist could deliver the intervention for an average of 30 patients per working week (1.33 hours per patient), based on experience with performing the associated steps in clinical practice. This resulted in an intervention cost of (€ 69*1.33) €92 per patient. For the cost-effectiveness analysis, we assumed that the tasks performed by the study pharmacists were not conducted in standard care and could be performed without additional time spent by the ward staff.
Statistical Analysis
We estimated incremental QALYs (∆QALY) as the mean difference in QALYs per patient between the groups, based on mean utility at each observation point and an area-under-the-curve approach. Mixed-model regression was used to model the multi-level structure of the data in terms of repeated measures on an individual level, as well as missing timepoints [21–24]. The model was fitted with a clustering on the patient level. Clustering on the ward level did not contribute to the model, indicating that the variation between wards was not significant between the study wards and was not included. The model included an interaction term between treatment and time and an unstructured covariance matrix was applied [22]. We adjusted the model for the assumed fixed baseline utility [16, 22, 25]. All other baseline characteristics in Table 1 were tested as covariates, and the following covariates significantly contributed to the model: the total number of medications (continuous), receiving multi-dose dispensed medication (yes/no), home dwelling (yes/no), and receiving home care services (yes/no).
Table 1.
Characteristics of the total population (N = 285), non-long stayers (n = 222), and long stayers (n = 63)
| Total population (n = 285) | Non-long stayers < 14 days (n = 222) |
Long stayers ≥ 14 days (n = 63) |
||||
|---|---|---|---|---|---|---|
| Intervention group (N = 148) | Control group (N = 137) | Intervention group (n = 106) | Control group (n = 116) | Intervention group (n = 42) | Control group (n = 21) | |
| Age included, years mean (SD) | 82.8 (6.0) | 82.1 (5.9) | 82.4 (6.1) | 81.9 (5.9) | 83.9 (5.9) | 82.9 (6.1) |
| Sex, n (%)a | ||||||
| Female | 98 (66.2) | 74 (54.0) | 69 (65.1) | 65 (56.0) | 29 (69.1) | 9 (42.9) |
| Level of education, n (%)a | ||||||
| Low (≤12 years) | 75 (52.8) | 73 (54.1) | 52 (49.1) | 64 (55.2) | 23 (54.8) | 9 (42.9) |
| High (>12 years) | 67 (47.2) | 62 (45.9) | 50 (47.2) | 50 (43.1) | 17 (40.5) | 12 (57.1) |
| Missing | 6 (4.1) | 2 (1.5) | 4 (3.8) | 2 (1.7) | 2 (4.8) | 0 (0) |
| Living status at admission, n (%)a | ||||||
| Home dwelling | 137 (92.6) | 129 (94.2) | 100 (94.3) | 111 (95.7) | 37 (88.1) | 18 (85.7) |
| Living alone | 86 (58.5) | 82 (59.9) | 59 (56.2) | 69 (59.5) | 27 (64.3) | 13 (61.9) |
| Need for assistance, n (%)a | ||||||
| Home care services | 75 (50.7) | 77 (56.2) | 48 (45.3) | 63 (54.3) | 27 (61.3) | 14 (66.7) |
| Multi-dose adherence aid | 43 (29.0) | 48 (35.0) | 27 (25.5) | 38 (32.8) | 16 (38.1) | 10 (47.6) |
| Handling own medications | 77 (52.0) | 64 (46.7) | 59 (55.7) | 58 (50.0) | 18 (42.9) | 6 (28.6) |
| Medication use, mean (SD) | ||||||
| Number of medications regular use | 6.6 (4.0) | 7.4 (4.0) | 6.8 (4.1) | 7.2 (4.0) | 6.4 (3.9) | 8.5 (3.9) |
| Number of medications total | 8.7 (5.1) | 9.6 (5.4) | 8.8 (5.1) | 9.4 (5.4) | 8.5 (5.1) | 10.5 (5.1) |
| Comorbidities in admission notes, n (%)a | ||||||
| Hypertension | 75 (51.0) | 69 (50.4) | 54 (50.4) | 58 (50.0) | 21 (50.0) | 11 (52.4) |
| Asthma or COPD | 44 (29.7) | 38 (27.7) | 34 (32.1) | 33 (28.5) | 10 (23.8) | 5 (23.8) |
| Atrial fibrillation | 37 (25.0) | 42 (30.7) | 15 (23.6) | 36 (31.0) | 12 (28.6) | 6 28.6) |
| Diabetes mellitus | 28 (18.9) | 31 (22.6) | 21 (19.8) | 25 (21.6) | 7 (16.7) | 6 (28.6) |
| Heart failure | 24 (16.2) | 21 (15.3) | 14 (13.2) | 17 (14.7) | 10 (23.8) | 4 (19.1) |
| Renal failure | 24 (16.2) | 21 (15.3) | 14 (13.2) | 16 (13.8) | 10 (23.8) | 5 (23.8) |
| Anxiety/depression | 17 (11.5) | 11 (8.0) | 11 (10.4) | 10 (8.6) | 6 (13.3) | 1 (4.8) |
| Dementia | 7 (4.7) | 4 (2.9) | 3 (2.8) | 4 (3.5) | 4 (9.5) | 0 (0) |
| Study ward, n (%)a | ||||||
| Ward 1 | 117 (79.1) | 103 (75.2) | 80 (75.5) | 85 (73.3) | 37 (88.1) | 18 (85.7) |
| Ward 2 | 31 (21.0) | 34 (24.8) | 26 (24.5) | 31 (26.7) | 5 (11.9) | 3 (14.3) |
| Died during the study period, n (%)a | 14 (9.5) | 12 (8.8) | 7 (6.6) | 10 (8.6) | 7 (16.7) | 2 (9.5) |
| EQ-5D utility score at dischargeb | 0.510 | 0.472 | 0.512 | 0.491 | 0.507 | 0.366 |
| EQ-5D utility score at 1 month follow-upb | 0.522 | 0.500 | 0.568 | 0.530 | 0.398 | 0.328 |
| EQ-5D utility score at 6 months follow-upb | 0.507 | 0.454 | 0.566 | 0.454 | 0.346 | 0.456 |
| EQ-5D utility score at 12 months follow-upb | 0.441 | 0.429 | 0.508 | 0.441 | 0.245 | 0.359 |
| Patients with prolonged hospitalizations (index or readmissions) ≥14 days, n (%)a | 42 (28.3) | 21 (15.3) | N/A | N/A | N/A | N/A |
| Total healthcare costs in previous year, € mean (95% CI)c | 11,085 (8535–13,922) | 11,975 (8835–15,249) | 8409 (6081–11,159) | 12,226 (8813–16,726) | 17,840 (11,721–23,959) | 10,586 (5794–16,807) |
CI confidence interval, COPD chronic obstructive pulmonary disease, N/A not applicable, SD standard deviation
aPercentages were rounded
bAdjusted for common fixed baseline of 0.487
cCIs were bias corrected using bootstrap
Incremental costs (∆C) were reported as the difference in mean total per patient costs between the groups. Cost differences were adjusted for costs in the year before the index hospital stay using linear regression. All costs were described with bias corrected 95% confidence intervals (CIs) calculated by bootstrap, to account for skewed cost data [26].
The incremental cost-effectiveness ratio (ICER) was calculated as the ratio between the incremental cost and incremental QALYs comparing the intervention and control groups, using the following equation: ICER = ∆C/∆QALY. The uncertainty of the ICER was assessed by pairwise bootstrapping of 1000 ICERs plotted in a cost-effectiveness plane. A cost-effectiveness acceptability curve was generated from the 1000 bootstrapped ICERs for several willingness-to-pay (WTP) thresholds, to assess the likelihood that the intervention is cost effective compared to standard care. As the Norwegian societal WTP threshold for gaining 1 year in full health depends on the severity of the condition calculated from absolute shortfall, we report a range of €27,067–81,201 (NOK 275,000–825,000) as recommended by Norwegian authorities [14, 27].
Because of a capacity problem in primary healthcare during the IMMENSE study conduct, hospital stays were extended beyond the patients’ need for hospitalization for some participants; however, the available data do not distinguish between patients who needed extended hospital care and those affected by the capacity problem. Before unblinding the group allocation, we inspected the distribution of extended stays between the study groups. We applied a cut-off for hospitalizations of ≥ 14 days, as this was twice the length of a mean hospital stay in the data material. A post-hoc subgroup analysis was undertaken for patients with at least one hospitalization (index or readmission) of ≥ 14 days, hereafter called long stayers, and those with no such extended hospitalizations, hereafter called non-long stayers.
All statistical analyses were carried out using Stata 17. The analyses were conducted with a 12-month time horizon from discharge, and thus QALYs and costs were not discounted.
Results
Characteristics of the Study Population
Prior to enrolment, the study groups were balanced in terms of age, living arrangements, medication use, medical history, and prior healthcare costs, although there was a higher proportion of women in the intervention group. However, the groups differed in terms of patients with hospitalizations (index or readmission) ≥ 14 days, as there were 42 patients in the intervention group and 21 patients in the control group (Table 1). The characteristics of the total CUA population (n = 285) differed from the full IMMENSE study population (n = 480) with a lower mortality rate and a lower proportion with dementia (Table S1 of the ESM).
Cost Outcomes
Hospitalizations (index and readmissions) had a mean cost of €10,043 [95% CI 9289–10,899]. The mean length of stay for the total population was 7.0 days and 6.2 days in the intervention and control groups, respectively (Table 2). The corresponding incremental cost per patient was €4429 [95% CI − 1101 to 11,926] (Table 3), indicating that the intervention had higher costs compared with standard care. Readmissions contributed the most to the mean cost difference per patient, constituting close to the full cost difference between the groups. However, none of the cost differences between the groups was statistically significant (Table 3).
Table 2.
Quantities and costs (in €) per encounter of healthcare resources used, by cost components
| Cost component | Total population (n = 285) | Non-long stayers <14 days (n = 222) | Long stayers ≥14 days (n = 63) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention group (n = 148) | Control group (n = 137) | Cost per encounter, € | Intervention group (n = 106) | Control group (n = 116) | Cost per encounter, € | Intervention group (n = 42) | Control group (n = 21) | Cost per encounter, € | |
| Encounters | Encounters | Mean (95% CI)a | Encounters | Encounters | Mean (95% CI)a | Encounters | Encounters | Mean (95% CI)a | |
| Hospitalizations (mean length of stay; range) | 351 (7.1; 1–57) | 315 (6.3; 1–88) | 10,043 (9289–10,899) | 205 (4.6; 1–13) | 253 (4.7; 1–13) | 7039 (6617–7448) | 146 (10.5; 1–57) | 62 (12.8; 1–88) | 16,658 (14,627–19,376) |
| Hospital outpatient clinic visits | 1072 | 786 | 356 (332–385) | 648 | 633 | 348 (321–380) | 424 | 153 | 374 (327–431) |
| Emergency room care visits | 262 | 271 | 77 (74–82) | 160 | 207 | 79 (74–84) | 102 | 64 | 73 (67–82) |
| Emergency room, other costsb | 133 | 120 | 9 (9–10) | 71 | 105 | 9 (8–9) | 62 | 15 | 10 (9–12) |
| GP visits | 1392 | 1281 | 46 (44–47) | 1045 | 1084 | 45 (43–46) | 347 | 197 | 49 (46–52) |
| GP, other costs | 2332 | 2218 | 11 (10–11) | 1747 | 1906 | 11 (10–11) | 585 | 312 | 10 (10–11) |
| Specialist physician visits | 71 | 67 | 122 (111–135) | 52 | 60 | 121 (108–137) | 19 | 7 | 126 (109–148) |
| Specialist physician, other costsb | 38 | 27 | 17 (13–23) | 23 | 21 | 17 (12–24) | 15 | 6 | 17 (10–27) |
| Primary care clinic visits | 645 | 528 | 49 (45–54) | 411 | 414 | 52 (48–58) | 234 | 114 | 40 (34–48) |
| Primary care clinic, other costsb | 1133 | 984 | 20 (19–22) | 777 | 823 | 20 (19–22) | 356 | 161 | 20 (18–23) |
| Laboratory work | 55 | 69 | 31 (26–36) | 48 | 58 | 29 (24–34) | 7 | 11 | 44 (29–63) |
| Intervention cost | 148 | N/A | 92 | 106 | N/A | 92 | 42 | N/A | 92 |
CI confidence interval, GP general practitioner, N/A not applicable
aCIs were bias corrected using bootstrap
bCosts for laboratory work, phone call, and use of materials and equipment
Table 3.
Cost-utility analysis (mean cost per patient in €, mean QALYs per patient, and ICER in €/QALY) for the total population, non-long stayers and long stayers
| Total population (n = 285) | Non-long stayers < 14 days (n = 222) | Long stayers ≥ 14 days (n = 63) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention group (n = 148) | Control group (n = 137) | Difference | Intervention group (n = 106) | Control group (n = 116) | Difference | Intervention group (n = 42) | Control group (n = 21) | Difference | |
| Mean (95% CI)a | Mean (95% CI)a | Mean (95% CI)a | Mean (95% CI)a | Mean (95% CI)a | Mean (95% CI)a | Mean (95% CI)a | Mean (95% CI)a | Mean (95% CI)a | |
| Cost, € | Cost, € | Cost, €c | Cost, € | Cost, € | Cost, €c | Cost, € | Cost, € | Cost, €c | |
| Index admissions | 9679 (8428–11,101) | 9663 (8313–11,389) | 55 (− 2161 to 1862) | 7485 (6775–8296) | 7691 (6859–8553) | 1 (− 1135 to 1223) | 15,215 (11,530–19,127) | 20,588 (13,928–29,189) | − 4826 (− 14,545 to 2860) |
| Readmissions | 15,748 (12,308–19,809) | 11,690 (8717–14,985) | 4057 (− 301 to 9930) | 6164 (4504–7995) | 7627 (6056-9936) | − 860 (− 3214 to 1179) | 39,935 (30,542–49,959) | 34,134 (22,147–46,631) | 5496 (− 10,857 to 21,032) |
| Hospital outpatient clinic | 2542 (1813–3539) | 2183 (1637–2822) | 278 (− 706 to 1430) | 1922 (1423–2510) | 2090 (1551–2776) | − 99 (− 884-727) | 3791 (1950–7166) | 2700 (1380–5265) | 1366 (− 1585 to 5499) |
| Emergency room care | 131 (110–160) | 159 (120–203) | − 25 (− 73 to 20) | 119 (94–147) | 142 (110–189) | − 9 (− 50 to 31) | 163 (116–238) | 253 (138–463) | − 103 (− 327 to 23) |
| Emergency room, other costsb | 8 (6–11) | 8 (6–11) | − 0 (− 3 to 4) | 6 (4–9) | 8 (6–10) | − 2 (− 5 to 1) | 14 (7–22) | 9 (4–18) | 1 (− 8 to 9) |
| GP visits | 431 (370–510) | 423 (363–492) | 12 (− 81 to 106) | 433 (383–495) | 426 (336–499) | 20 (− 71 to 108) | 427 (263–683) | 407 (294–551) | − 19 (− 227 to 211) |
| GP, other costsb | 168 (146–191) | 174 (142–215) | − 4 (− 50 to 36) | 173 (148–203) | 180 (147–227) | − 2 (− 52 to 48) | 154 (112–206) | 133 (96–173) | 6 (− 56 to 56) |
| Specialist physician visits | 62 (42–86) | 56 (38–73) | 6 (− 19 to 35) | 64 (42–96) | 58 (41–81) | 5 (− 25 to 39) | 56 (26–100) | 43 (10–91) | 17 (− 50 to 74) |
| Specialist physician, other costsb | 4 (2–8) | 3 (1–6) | 1 (− 3 to 6) | 3 (1–7) | 4 (1–7) | 0 (− 4 to 4) | 7 (1–18) | 2 (0–3) | 6 (− 1 to 17) |
| Primary care clinic | 201 (166–242) | 200 (159–244) | 1 (− 57 to 61) | 194 (150–237) | 196 (156–246) | 4 (− 56 to 67) | 218 (152–310) | 223 (135–346) | 3 (− 153 to 125) |
| Primary care clinic, other costsb | 156 (132–188) | 145 (118–175) | 12 (− 24 to 54) | 158 (127–195) | 136 (109–171) | 24 (− 18 to 73) | 154 (125–187) | 191 (119–290) | − 39 (− 144 to 44) |
| Laboratory work | 14 (9–22) | 13 (6–20) | 1 (− 10 to 11) | 16 (9–25) | 12 (5–22) | 4 (− 10 to 14) | 10 (3–22) | 18 (6–33) | − 7 (− 27 to 7) |
| Intervention cost | 92 | N/A | 92 | 92 | N/A | 92 | 92 | N/A | 92 |
| Total cost, € | 29,147 (25,181–33,654) | 24,717 (21,079–28,957) | 4429 (− 1101 to 11,926) | 16,829 (14,823–18,785) | 18,570 (16,453–21,270) | − 824 (− 3869 to 2066) | 60,235 (51,168–70,976) | 58,672 (45,702–73,872) | 1992 (− 17,964 to 18,811) |
| QALY | QALY | QALY difference | QALY | QALY | QALY difference | QALY | QALY | QALY difference | |
|---|---|---|---|---|---|---|---|---|---|
| QALYs, unadjusted | 0.504 (0.466–0.543) | 0.469 (0.430–0.509) | 0.035 (0.032–0.036) | 0.556 (0.512–0.601) | 0.476 (0.433–0.520) | 0.080 (0.078–0.081) | 0.346 (0.279–0.413) | 0.404 (0.314–0.495) | − 0.058 (− 0.163 to 0.055) |
| QALYs, adjusted | 0.500 (0.468–0.533) | 0.477 (0.443–0.510) | 0.023 (0.022–0.025)d | 0.552 (0.513–0.590) | 0.485 (0.448–0.522) | 0.067 (0.066–0.070)d | 0.332 (0.275–0.389) | 0.433 (0.354–0.511) | − 0.101 (− 0.199 to 0.003)e |
| ICER, €/QALY | 192,565 | Intervention dominates | Intervention dominated |
| ICER | €/QALY | €/QALY | €/QALY | ||||||
|---|---|---|---|---|---|---|---|---|---|
| ICER, €/QALY | 192,565 | Intervention dominates | Intervention dominated |
CI confidence intervals, GP general practitioner, ICER incremental cost-effectiveness ratio, NA not applicable, QALY quality-adjusted life year
aCIs were bias corrected using bootstrap
bCosts for laboratory work, phone call, and use of materials and equipment
cAdjusted for total costs in the previous year
dAdjusted for the total number of medications, multi-dose adherence tool (yes/no), home dwelling (yes/no), and receiving home care services (yes/no) before inclusion
eAdjusted for the total number of medications, multi-dose adherence tool (yes/no), and handling own medications(yes/no) before inclusion
For the non-long stayers, the hospitalizations had a mean cost of €7039 [95% CI 6617–7448] with a mean length of stay of 4.6 and 4.7 days for the intervention and control groups, respectively. The corresponding costs for the long stayers were €16,658 [95% CI 14,627–19,376] with a mean length of stay of 10.5 and 12.8 days for the intervention and control groups, respectively (Table 2). In the subgroup analysis the incremental cost was €− 824 [95% CI − 3869 to 2066] for the non-long stayers and €1992 [95% CI − 17,964–18,811] for the long stayers (Table 3), indicating that the intervention was cost saving compared to standard care for non-long stayers but not for long stayers
Health Outcomes
The incremental QALY for the two groups was 0.023 [95% CI 0.022–0.025] for the total population, representing a statistically significant difference in QALYs. For the subgroup analysis, the incremental QALYs were 0.067 [95% CI 0.066–0.070] and − 0.101 [95% CI − 0.199–0.033] for the non-long and long stayers, respectively, representing a statistically significant increase in the non-long stayers, and a non-significant decrease in the long stayers (Table 3).
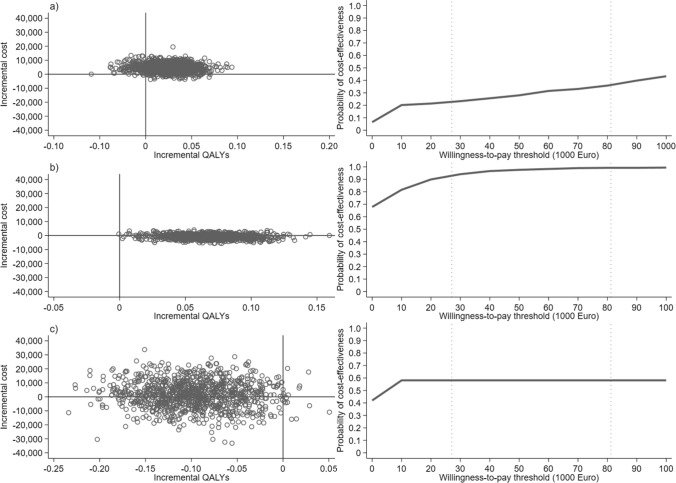
Cost-Effectiveness Analysis
The ICER was €192,565 per QALY for the adjusted main analysis (Table 3). The bootstrapped ICERs were predominantly in the north-east quadrant of the cost-effectiveness plane, indicating that the intervention produced more QALYs and had a higher mean cost than standard care (Fig. 2a). The probability of cost effectiveness was lower for the intervention than for standard care for the whole WTP range of €27,067–81,201 per QALY (Fig. 2a). The intervention dominated standard care for the non-long stayers with a probability of cost effectiveness of 93.1–99.2% for the whole WTP range and 67.8% at zero WTP (Fig. 2b). For the long stayers, the intervention was dominated by standard care (Fig. 2c).
Fig. 2.
Cost-effectiveness plane with 1000 pairwise bootstrapped incremental cost-effectiveness ratios [ICERs] (left side) and the cost-effectiveness acceptability curve showing the probability of cost effectiveness at different willingness-to-pay thresholds for the intervention (right side) for the a full population (percentage of ICERs in the north-east quadrant [NE]: 80.80%, percentage of ICERs in the south-east quadrant [SE]: 6.20%, percentage of ICERs in the north-west quadrant [NW]: 12.70%, percentage of ICERs in the south-west quadrant [SW]: 0.03%), b non-long stayers (NE: 32.20%, SE: 67.80%, NW: 0.01%, SW: 0.00%), and c long stayers (NE: 0.07%, SE: 0.08%, NW: 57.30%, SW: 41.20%), respectively. The dotted lines represent minimum and maximum willingness to pay for the Norwegian setting (€27,067–81,200). QALY quality-adjusted life year
Discussion
Principal Findings
The intervention was not cost effective for the total study population. However, the intervention was more effective and less costly and hence dominated standard care with a high probability of cost effectiveness in the non-long stayer subgroup. In the long stayer subgroup, the intervention was dominated by standard care. Hospitalizations were the main cost driver, and readmissions contributed the most to the cost difference between the groups. The imbalance in long stayers and the high costs of these patients were driving for the cost difference in the total population.
Medication reviews have been implemented in hospital settings in many parts of the world [8], aiming to optimize medication therapy and improve patient outcomes. To our knowledge, this is the first published CUA alongside a clinical trial of an IMM intervention, although several other studies of IMM or similar interventions have been completed [4–7, 28–30]. The probability of cost effectiveness was high for the non-long patient group, and the intervention per se was not costly compared to other care activities, corresponding approximately to the cost of an emergency room visit in the data material. We have assumed that one clinical pharmacist can deliver the intervention for 30 patients per week. It is likely that more time has been spent on the long stayers, while other patients may have required less time than assumed. Employing the number needed to treat of 29 to prevent one hospital readmission reported in the Cochrane review [8] and a mean cost per hospitalization from the current study of €10,043, one could spend €346 (€10,043/29) on the intervention per patient to prevent one readmission. This corresponds to 5.0 hours per patient (346/69), or eight patients per week (40/5.0). Moreover, the assumption that the intervention activities are completely additional to standard care may not be realistic. For example, some activities such as producing a medication list on admission and writing discharge notes are also done in standard care. Consequently, when these tasks are included in the intervention, nurses and physicians may have time for alternative activities. A QALY difference of 0.067 may intuitively seem like a small difference. However, on an individual level, it approximately translates to a full year without transitioning from “no problem” to “moderate problems” in mobility (− 0.069), anxiety/depression (− 0.071), or from “moderate” to “extreme problems” in usual activities (− 0.094 + 0.036 = − 0.058). On a group level, the reported difference translates to 24.5 days (0.067 × 365 days) of perfect health over 1 year, which is significant for patients with a mean QALY of 0.552 and 0.485 for the intervention and control groups, respectively.
Ghatnekar et al. published a probabilistic decision tree model on an IMM intervention in a Swedish setting [31]. The analysis applied dis-utilities from the literature and resource use and unit costs were taken from data collected by the researchers; however, not as a complete RCT. We found a considerably higher incremental QALY than that reported by these authors (0.023 in the full population and 0.069 in the non-long stayers vs 0.005 reported by Ghatnekar et al.). They reported a probability of cost effectiveness of 98% at a zero WTP threshold because of the assumption that some tasks and associated costs of the ward staff were transferred to the study pharmacists as part of the intervention. Another study reported a positive difference in self-rated global HRQoL over 6 months for older patients receiving a similar intervention [32]. Unfortunately, very few clinical trials of IMM or similar interventions have reported HRQoL data, and tend to have a shorter time frame of 90 days [30] or 6 months [29, 32] and focus on the difference in utility scores instead of QALYs [30, 32]. Our study is thus one of the first to contribute to the knowledge gap identified in the recently published Cochrane review [8].
Improving the quality of medication use and sustaining the effect of the intervention for as long as possible should be a goal. We have studied the effect of the intervention delivered at the index hospitalization on costs and QALYs for a follow-up of 12 months in the IMMENSE study. However, there are several factors that may have interfered with the effect of the intervention. First, the intervention was not repeated on readmission. A study by Parekh et al. found that 37% of hospitalized older adults were subject to medication-related harm 8 weeks after discharge, 74% of which was caused by medications initiated during hospitalization [33]. Medication use, including potentially inappropriate medications, often increases during a hospital stay [34]. In the present study, the patients were readmitted on average 1.3 times during the follow-up period. and hence medication changes during readmissions may have counteracted the effect of the intervention in the follow-up period. Second, we do not know to what extent treatment advice resulting from the intervention was acted upon in primary care. Medication changes recommended during the index stay were communicated by phone to primary care givers; however, it was then up to them to decide to implement these in the outpatient setting. Third, around 30% of the patients received a multi-dose dispensed medication, an adherence aid with individually packaged and machine-dispensed disposable sachets with medicines marked with the intended time of intake [35]. There is some evidence that the multi-dose system is resistant to changes in prescribing and hence prone to sustaining potentially inappropriate prescribing patterns [36]. Sustaining the effect of the intervention for a full year after discharge without repeating the intervention may be unrealistic, and the effect of the intervention may have been diluted over time [37–39]. Repeating the intervention when a patient is readmitted may be less time consuming and hence less costly when a previously reconciled medication list and records of previous recommendations are available and could also provide information about the uptake of recommendations in primary care. Further research to study HRQoL, prescribing patterns, and how healthcare costs were distributed during the follow-up period of this study may provide knowledge about the longevity of the intervention effect.
Strength and Limitations of the Study
A strength of this study is the comprehensiveness of the data sources and the consistency of the data collection conducted alongside an RCT. We have included high-quality register data for the costs of all healthcare use for the patients in the analysis, including healthcare use of all care levels. All EQ-5D-3L data were collected by the same trained study nurse blinded to group allocation, and the analysis work was blinded until it was time to interpret the results. Nevertheless, the results must be interpreted with some limitations in mind. First, the capacity problem in primary care to find a bed for patients in a nursing home, or to arrange for home care services, may for a number of patients have led to extended hospital stays even if they were ready for discharge. This is important because hospitalizations were the main cost driver. It was not possible to identify which of the 63 long stayers were affected or how long they were retained, and to what extent this was reflected in the hospitalization costs. Additionally, the group of long stayers was small and there were twice as many patients with long stays in the intervention group compared with the control group. We undertook subgroup analyses for long stayers versus non-long stayers to mitigate overestimation of the cost difference between the groups. However, the intervention may have served as an “early warning system,” leading to identifying problems and subsequently prolonged hospital stays [37], and our analysis would be more reliable if we could identify patients and hospital stays affected. Therefore, it is difficult to conclude on behalf of the long-stayer subgroup. Second, we could only include the patients in the CUA for which EQ-5D-3L data had been collected. The IMMENSE trial was a pragmatic trial and results are generalizable beyond the study population. However, excluding patients who provided consent through the next of kin makes the study population in the CUA less representative of the general older, acutely hospitalized population. Furthermore, the EQ-5D-3L was chosen over the EuroQol 5-Dimension 3-Level Health State Questionnaire, as it was believed to be more feasible to conduct telephone interviews using the three-level scale for patients with some degree of cognitive impairment or hearing loss. Future studies should consider the possibility of performing proxy HRQoL measurements for patients unable to give informed consent, to improve generalizability of the results. Third, having a baseline EQ-5D-3L measurement could have provided a more reliable estimate of the QALY difference between the groups and provide a higher degree of certainty of whether the difference in health status was due to the IMMENSE intervention. Fourth, we were unable to obtain medication costs for medications not administered during hospitalization. However, medication costs are likely to be negligible compared with the hospitalization costs [3] and are thus not likely to substantially influence the cost difference between the groups.
Conclusions
According to societal WTP thresholds, the medication optimization intervention was not cost effective compared with standard care for the full population. The effect and costs of the medication optimization intervention for acutely hospitalized older adults differed for patients who were non-long and long stayers. The intervention dominated standard care for the non-long stayers, with a high probability of cost effectiveness. Further research is needed to facilitate a conclusion on behalf of the long-stayer group. Hospitalization cost was the main cost driver and the intervention was negligible compared to other care activities.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We thank all patients who participated in the IMMENSE study, study nurse Birthe Angermo for data collection, and Frode Skjold for data management.
Declarations
Funding
Open access funding provided by University of Oslo (incl Oslo University Hospital). The IMMENSE study was supported by the Northern Norway Regional Health Authority (grant number HST1314-16). The funding body has supported expenses to cover pharmacist salary and study running costs. They have no part in the collection, management, analysis, or interpretation of the data, nor in the writing and reporting of the study’s conclusions.
Conflict of interest
Eirin Guldsten Robinson, Hanna Gyllensten, Jeanette Schultz Johansen, Kjerstin Havnes, Anne Gerd Granas, Trine Strand Bergmo, Lars Småbrekke, Beate Hennie Garcia, and Kjell H. Halvorsen have no conflicts of interest that are directly relevant to the content of this article.
Ethics approval
This research has been performed in accordance with ethical guidelines stated by the Helsinki declaration. The Norwegian Centre for Research Data and the Norwegian Data Protection Authority granted ethical approval (Project number 41366).
Consent to participate
All participants or next of kin gave written informed consent for study participation.
Consent for publication
Not applicable.
Availability of data and material
The datasets generated and analyzed during the current study are not publicly available because they contain information that can compromise research participants’ privacy/consent but are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Author contributions
EGR provided the study design, performed the statistical analyses, drafted the manuscript, and prepared the tables and illustrations. HG contributed to the statistical analyses. BG, KHH, JSJ, KH, and LS planned and conducted the RCT and collected data. All authors contributed to the study design, writing, reviewing, and editing the manuscript, and have approved the final version.
References
- 1.Hodkinson A, Tyler N, Ashcroft DM, et al. Preventable medication harm across health care settings: a systematic review and meta-analysis. BMC Med. 2020;18:313. doi: 10.1186/s12916-020-01774-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oscanoa TJ, Lizaraso F, Carvajal A. Hospital admissions due to adverse drug reactions in the elderly: a meta-analysis. Eur J Clin Pharmacol. 2017;73:759–770. doi: 10.1007/s00228-017-2225-3. [DOI] [PubMed] [Google Scholar]
- 3.Robinson EG, Hedna K, Hakkarainen KM, Gyllensten H. Healthcare costs of adverse drug reactions and potentially inappropriate prescribing in older adults: a population-based study. BMJ Open. 2022;12:e062589. doi: 10.1136/bmjopen-2022-062589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gillespie U, Alassaad A, Henrohn D, Garmo H, Hammarlund-Udenaes M, Toss H, et al. A comprehensive pharmacist intervention to reduce morbidity in patients 80 years or older: a randomized controlled trial. Arch Intern Med. 2009;169:894–900. doi: 10.1001/archinternmed.2009.71. [DOI] [PubMed] [Google Scholar]
- 5.Lea M, Mowé M, Molden E, Kvernrød K, Skovlund E, Mathiesen L. Effect of medicines management versus standard care on readmissions in multimorbid patients: a randomised controlled trial. BMJ Open. 2020;10:e041558. doi: 10.1136/bmjopen-2020-041558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kempen TGH, Bertilsson M, Hadziosmanovic N, Lindner K-J, Melhus H, Nielsen EI, et al. Effects of hospital-based comprehensive medication reviews including postdischarge follow-up on older patients’ use of health care: a cluster randomized clinical trial. JAMA Netw Open. 2021;4:e216303. doi: 10.1001/jamanetworkopen.2021.6303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ravn-Nielsen LV, Duckert M-L, Lund ML, Henriksen JP, Nielsen ML, Eriksen CS, et al. Effect of an in-hospital multifaceted clinical pharmacist intervention on the risk of readmission: a randomized clinical trial. JAMA Intern Med. 2018;178:375–382. doi: 10.1001/jamainternmed.2017.8274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bülow C, Clausen SS, Lundh A, Christensen M. Medication review in hospitalised patients to reduce morbidity and mortality. Cochrane Database Syst Rev. 2023 doi: 10.1002/14651858.CD008986.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johansen JS, Halvorsen KH, Svendsen K, Havnes K, Robinson EG, Wetting HL, et al. Interdisciplinary collaboration across secondary and primary care to improve medication safety in the elderly (the IMMENSE study): a randomized controlled trial. BMC Health Serv Res. 2022;22:1290. doi: 10.1186/s12913-022-08648-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Husereau D, Drummond M, Augustovski F, et al. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) statement: updated reporting guidance for health economic evaluations. Health Policy Open. 2022;3:100063. doi: 10.1016/j.hpopen.2021.100063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johansen JS, Havnes K, Halvorsen KH, Haustreis S, Skaue LW, Kamycheva E, et al. Interdisciplinary collaboration across secondary and primary care to improve medication safety in the elderly (IMMENSE study): study protocol for a randomised controlled trial. BMJ Open. 2018;8:e020106. doi: 10.1136/bmjopen-2017-020106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johansen JS, Halvorsen KH, Havnes K, Wetting HL, Svendsen K, Garcia BH. Intervention fidelity and process outcomes of the IMMENSE study, a pharmacist-led interdisciplinary intervention to improve medication safety in older hospitalized patients. J Clin Pharm Ther. 2022;47:619–627. doi: 10.1111/jcpt.13581. [DOI] [PubMed] [Google Scholar]
- 13.Brooks R. EuroQol: the current state of play. Health Policy Amst Neth. 1996;37:53–72. doi: 10.1016/0168-8510(96)00822-6. [DOI] [PubMed] [Google Scholar]
- 14.Guidelines for the submission of documentation for single technology assessment (STA) of pharmaceuticals. Available from: https://legemiddelverket.no/Documents/English/Public%20funding%20and%20pricing/Documentation%20for%20STA/Guidelines%2020.05.2020.pdf. Accessed 13 Mar 2023.
- 15.Dolan P. Modeling valuations for EuroQol health states. Med Care. 1998;35:1095–1108. doi: 10.1097/00005650-199711000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Dritsaki M, Achana F, Mason J, Petrou S. Methodological issues surrounding the use of baseline health-related quality of life data to inform trial-based economic evaluations of interventions within emergency and critical care settings: a systematic literature review. Pharmacoeconomics. 2017;35:501–515. doi: 10.1007/s40273-016-0485-x. [DOI] [PubMed] [Google Scholar]
- 17.The Norwegian Tax Administration. National identity numbers. Available from: https://www.skatteetaten.no/en/person/foreign/norwegian-identification-number/national-identity-number/. Accessed 21 Sep 2022.
- 18.Statistics Norway. 03014: Consumer price index, by consumption group, contents and year. Statbank Norway. Available from: https://www.ssb.no/en/system/. Accessed 5 May 2022.
- 19.Norges Bank. Exchange rates. Available from: https://www.norges-bank.no/tema/Statistikk/Valutakurser/. Accessed 17 Oct 2022.
- 20.Statistics Norway. 12407: education broken down by monthly salary and number of years, by completion of education 2015–2019. Available from: http://www.ssb.no/statbankstatbank/table/12407/. Accessed 30 Mar 2020.
- 21.Faria R, Gomes M, Epstein D, White IR. A guide to handling missing data in cost-effectiveness analysis conducted within randomised controlled trials. Pharmacoeconomics. 2014;32:1157–1170. doi: 10.1007/s40273-014-0193-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gabrio A, Plumpton C, Banerjee S, Leurent B. Linear mixed models to handle missing at random data in trial-based economic evaluations. Health Econ. 2022;31:1276–1287. doi: 10.1002/hec.4510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Twisk J, de Boer M, de Vente W, Heymans M. Multiple imputation of missing values was not necessary before performing a longitudinal mixed-model analysis. J Clin Epidemiol. 2013;66:1022–1028. doi: 10.1016/j.jclinepi.2013.03.017. [DOI] [PubMed] [Google Scholar]
- 24.Griffiths A, Paracha N, Davies A, Branscombe N, Cowie MR, Sculpher M. Analyzing health-related quality of life data to estimate parameters for cost-effectiveness models: an example using longitudinal EQ-5D data from the SHIFT randomized controlled trial. Adv Ther. 2017;34:753–764. doi: 10.1007/s12325-016-0471-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ. 2005;14:487–496. doi: 10.1002/hec.944. [DOI] [PubMed] [Google Scholar]
- 26.Thompson SG, Barber JA. How should cost data in pragmatic randomised trials be analysed? BMJ. 2000;320:1197–1200. doi: 10.1136/bmj.320.7243.1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ministry of Health and Care Services. Government. no. Meld. St. 34 (2015–2016). Available from: https://www.regjeringen.no/en/dokumenter/meld.-st.-34-20152016/id2502758/. Accessed 13 Mar 2023.
- 28.Scullin C, Scott MG, Hogg A, McElnay JC. An innovative approach to integrated medicines management. J Eval Clin Pract. 2007;13:781–788. doi: 10.1111/j.1365-2753.2006.00753.x. [DOI] [PubMed] [Google Scholar]
- 29.Bladh L, Ottosson E, Karlsson J, Klintberg L, Wallerstedt SM. Effects of a clinical pharmacist service on health-related quality of life and prescribing of drugs: a randomised controlled trial. BMJ Qual Saf. 2011;20:738–746. doi: 10.1136/bmjqs.2009.039693. [DOI] [PubMed] [Google Scholar]
- 30.Bonnerup DK, Lisby M, Sædder EA, Brock B, Truelshøj T, Sørensen CA, et al. Effects of stratified medication review in high-risk patients at admission to hospital: a randomised controlled trial. Ther Adv Drug Saf. 2020;11:2042098620957142. doi: 10.1177/2042098620957142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ghatnekar O, Bondesson Å, Persson U, Eriksson T. Health economic evaluation of the Lund Integrated Medicines Management Model (LIMM) in elderly patients admitted to hospital. BMJ Open. 2013;3:e001563. doi: 10.1136/bmjopen-2012-001563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wallerstedt SM, Bladh L, Ramsberg J. A cost-effectiveness analysis of an in-hospital clinical pharmacist service. BMJ Open. 2012;2:e000329. doi: 10.1136/bmjopen-2011-000329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Parekh N, Ali K, Stevenson JM, Davies JG, Schiff R, Van der Cammen T, PRIME Study Group et al. Incidence and cost of medication harm in older adults following hospital discharge: a multicentre prospective study in the UK. Br J Clin Pharmacol. 2018;84:1789–1797. doi: 10.1111/bcp.13613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Johansen JS, Halvorsen KH, Svendsen K, Havnes K, Garcia BH. The impact of hospitalisation to geriatric wards on the use of medications and potentially inappropriate medications: a health register study. BMC Geriatr. 2020;20:190. doi: 10.1186/s12877-020-01585-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bell JS, Johnell K, Wimmer BC, Wiese MD. Multidose drug dispensing and optimising drug use in older people. Age Ageing. 2013;42:556–558. doi: 10.1093/ageing/aft080. [DOI] [PubMed] [Google Scholar]
- 36.Josendal AV, Bergmo TS, Granas AG. Potentially inappropriate prescribing to older patients receiving multidose drug dispensing. BMC Geriatr. 2020;20:272. doi: 10.1186/s12877-020-01665-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Elliott RA, Putman K, Davies J, Annemans L. A review of the methodological challenges in assessing the cost effectiveness of pharmacist interventions. Pharmacoeconomics. 2014;32:1185–1199. doi: 10.1007/s40273-014-0197-z. [DOI] [PubMed] [Google Scholar]
- 38.Murray MD, Young J, Hoke S, et al. Pharmacist intervention to improve medication adherence in heart failure: a randomized trial. Ann Intern Med. 2007;146:714–725. doi: 10.7326/0003-4819-146-10-200705150-00005. [DOI] [PubMed] [Google Scholar]
- 39.Denneboom W, Dautzenberg MG, Grol R, De Smet PA. Treatment reviews of older people on polypharmacy in primary care: cluster controlled trial comparing two approaches. Br J Gen Pract. 2007;57:723–731. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.