Abstract
This cohort study compares the outcomes of patients with BRCA1 and BRCA-related pancreatic cancers using 2 large data sets.
Introduction
Patients with pancreatic cancer (PDAC) and pathogenic variants (PVs) in BRCA1 or BRCA2 have historically been grouped together.1,2 However, preclinical and clinical data in other BRCA-related tumors suggests that the biological implications of BRCA1 and BRCA2 PVs may be different.3,4,5 To explore this further, we compared outcomes of patients with BRCA1 vs BRCA2-related PDAC using 2 large data sets.
Methods
The institutional review board at the University of Pennsylvania deemed this study exempt and waived informed consent because deidentified data was used. We followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Our cohort was derived from the national Flatiron Health database and from a local University of Pennsylvania database. The study population consisted of adult patients with germline PVs in BRCA1 or BRCA2 and a new diagnosis of PDAC between 2005 to 2021. Only individuals with complete data, including age, sex, ECOG status at diagnosis, resection status, and treatment information were included in the analysis. The primary outcome was overall survival (OS), calculated as the time of diagnosis to date of death or last follow up.
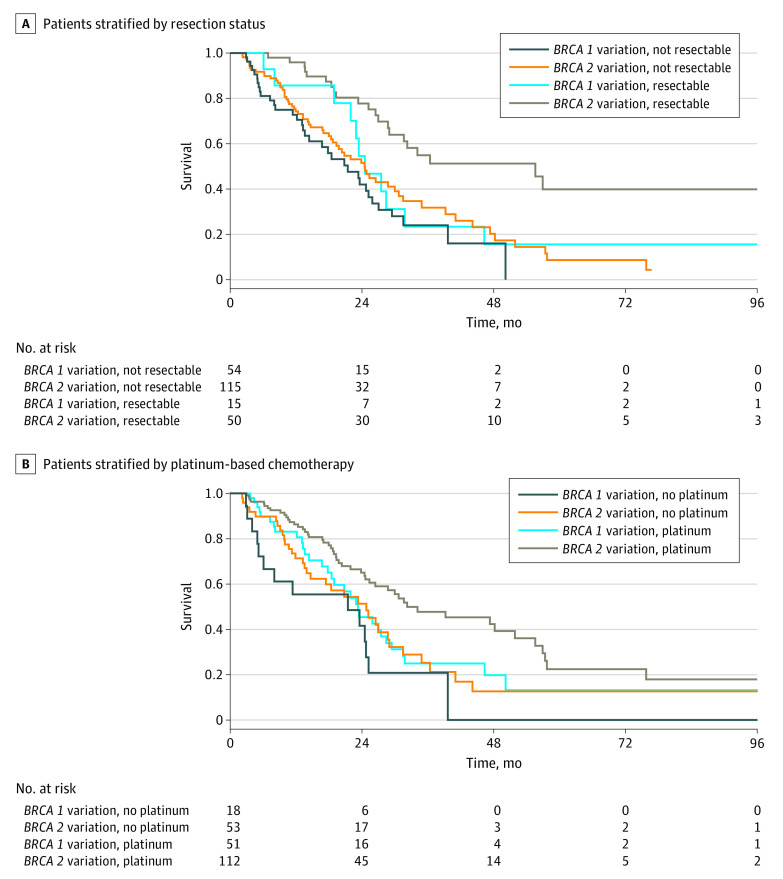
Adjusted hazard ratios (aHRs) and 95% CIs were calculated for comparison of OS between patients with BRCA1 PVs vs BRCA2 PVs using the Cox-proportional-hazards model. Kaplan-Meier curves compared OS between BRCA1 vs BRCA2 PVs, stratified by resection status and use of platinum-based therapies. P ≤ .05 was considered statistically significant. All reported P values are 2-sided. Analyses were performed using Stata version 16 (StataCorp). Data were analyzed from June 2022 to June 2023.
Results
This study included 234 consecutively identified patients with germline BRCA PVs and a diagnosis of PDAC (165 [70.5%] BRCA2; 69 [29.5%] BRCA1). Of patients with BRCA1, 33 of 69 (47.8%) were males with a median (IQR) age of 63 (55-70) years. Of patients with BRCA2, 84 of 165 (50.9%) were males, and the median (IQR) age was 64 (58-70) years. There were no significant differences in age, sex, performance status, year of diagnosis, or rates of exposure to platinum or poly (ADP-ribose) polymerase (PARP) inhibitor therapy between groups. Patients with BRCA2 PVs were more likely to undergo primary tumor resection (50 [30.3%] vs 15 [21.7%]).
Survival outcomes by BRCA status, stratified by stage and platinum exposure, are shown in the Table and Figure. In the total cohort, patients with BRCA2 PV had improved OS compared with patients with BRCA1 (mean [SE], 28.98 [2.53] months vs 23.36 [1.55] months), corresponding to an aHR of 0.64 (95% CI, 0.44-0.94; P = .02). In patients who underwent resection (Figure), BRCA2 PV was associated with improved OS compared with BRCA1 PVs (mean [SE] months, 55.59 [11.95] vs 24.54 [2.70] months; aHR 0.30 [95% CI, 0.13-0.70]; P = .006); in patients not undergoing resection, there were no appreciable differences in survival by BRCA status (24.47 months vs 21.42 months; aHR 0.67; 95% CI, 0.42-1.07). In patients who were exposed to platinum (Figure), BRCA2 PVs were associated with improved survival compared with BRCA1 PVs (mean [SE] OS, 32.26 [7.62] months vs 23.36 [2.89] months; aHR, 0.59 [95% CI, 0.38-0.93]; P = .02). When neither group received platinum, the survival advantage associated with BRCA2 PVs decreased (mean [SE] OS, 24.84 [3.52] months vs 21.42 [5.39] months; aHR 0.44 [95% CI, 0.21-0.92]; P = .03).
Table. Patient Outcomes According to BRCA Status and Stratified by Resection Status and Platinum Exposure.
| Patient Outcomes | HR (95% CI) | Median OS (SE), mo | |
|---|---|---|---|
| Unadjusted | Adjusted | ||
| Resected (early stage) patients | |||
| BRCA2 variant | 0.45 (0.22-0.94) | 0.30 (0.13-0.70) | 55.59 (11.95) |
| BRCA1 variant | 1 [Reference] | 1 [Reference] | 24.54 (2.70) |
| Unresected (locally advanced or metastatic) patients | |||
| BRCA2 variant | 0.75 (0.49-1.15) | 0.67 (0.42-1.07) | 24.48 (2.50) |
| BRCA1 variant | 1 [Reference] | 1 [Reference] | 21.42 (3.86) |
| Platinum exposed patients (all stages) | |||
| BRCA2 variant | 0.60 (0.38-0.94) | 0.59 (0.38-0.93) | 32.26 (7.62) |
| BRCA1 variant | 1 [Reference] | 1 [Reference] | 23.36 (2.89) |
| Nonplatinum exposed patients (all stages) | |||
| BRCA2 variant | 0.65 (0.34-1.22) | 0.44 (0.21-0.92) | 24.84 (3.52) |
| BRCA1 variant | 1 [Reference] | 1 [Reference] | 21.42 (5.39) |
Abbreviations: HR, hazard ratio; OS, overall survival.
Figure. Kaplan-Meier Curves for Overall Survival in Patients With Pancreatic Cancer and BRCA1 vs BRCA2 Variants.
Discussion
In a large cohort of patients with germline BRCA PVs and pancreatic cancer, BRCA2 PVs were associated with better outcomes compared with BRCA1 PVs. This finding appears to be associated with an enhanced benefit from platinum-based therapies and resection in BRCA2 carriers compared with their BRCA1-carrying counterparts. The difference was not statistically significant in the nonresected population.
Biological differences between BRCA1-related tumors and BRCA2-related tumors have been described. While rates of biallelic loss appear to be similar,5 rates of PVs in TP53 are more common in BRCA1-related tumors compared with BRCA2-related tumors (88% vs 53%) and PDAC samples with BRCA2 PVs are more immunogenic than those with BRCA1 PVs.6 This study had limitations including its retrospective nature and the small subgroup of patients with resected PDAC and BRCA1 PV.
Our findings emphasize the need for a better understanding of possible biological differences between pancreatic cancers that develop in patients with BRCA1 PVs vs BRCA2 PVs and consideration of stratification by mutation type in future clinical trials. The association of platinum-based therapies in patients with different BRCA PVs should be evaluated in a separate larger cohort.
Data Sharing Statement
References
- 1.Golan T, Hammel P, Reni M, et al. Maintenance olaparib for germline BRCA-mutated metastatic pancreatic cancer. N Engl J Med. 2019;381(4):317-327. doi: 10.1056/NEJMoa1903387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reiss KA, Mick R, O’Hara MH, et al. Phase II study of maintenance rucaparib in patients with platinum-sensitive advanced pancreatic cancer and a pathogenic germline or somatic variant in BRCA1, BRCA2, or PALB2. J Clin Oncol. 2021;39(22):2497-2505. doi: 10.1200/JCO.21.00003 [DOI] [PubMed] [Google Scholar]
- 3.Chetrit A, Hirsh-Yechezkel G, Ben-David Y, Lubin F, Friedman E, Sadetzki S. Effect of BRCA1/2 mutations on long-term survival of patients with invasive ovarian cancer: the national Israeli study of ovarian cancer. J Clin Oncol. 2008;26(1):20-25. doi: 10.1200/JCO.2007.11.6905 [DOI] [PubMed] [Google Scholar]
- 4.Taza F, Holler AE, Fu W, et al. Differential activity of PARP inhibitors in BRCA1- versus BRCA2-altered metastatic castration-resistant prostate cancer. JCO Precis Oncol. 2021;5:1200-1220. doi: 10.1200/PO.21.00070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Golan T, O’Kane GM, Denroche RE, et al. Genomic features and classification of homologous recombination deficient pancreatic ductal adenocarcinoma. Gastroenterology. 2021;160(6):2119-2132.e9. doi: 10.1053/j.gastro.2021.01.220 [DOI] [PubMed] [Google Scholar]
- 6.Samstein RM, Krishna C, Ma X, et al. Mutations in BRCA1 and BRCA2 differentially affect the tumor microenvironment and response to checkpoint blockade immunotherapy. Nat Cancer. 2021;1(12):1188-1203. doi: 10.1038/s43018-020-00139-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Sharing Statement