Abstract
Background
Neonatal hypoglycaemia is a common condition that can be associated with brain injury. Current practice usually includes early identification of at‐risk infants (e.g. infants of diabetic mothers; preterm, small‐ or large‐for‐gestational‐age infants), and prophylactic measures are advised. However, these measures often involve use of formula milk or admission to the neonatal unit. Dextrose gel is non‐invasive, inexpensive and effective for treatment of neonatal hypoglycaemia. Prophylactic dextrose gel can reduce the incidence of neonatal hypoglycaemia, thus potentially reducing separation of mother and baby and supporting breastfeeding, as well as preventing brain injury.
This is an update of a previous Cochrane Review published in 2021.
Objectives
To assess the effectiveness and safety of oral dextrose gel in preventing hypoglycaemia before first hospital discharge and reducing long‐term neurodevelopmental impairment in newborn infants at risk of hypoglycaemia.
Search methods
We searched CENTRAL, MEDLINE, Embase and Epistemonikos in April 2023. We also searched clinical trials databases and the reference lists of retrieved articles.
Selection criteria
We included randomised controlled trials (RCTs) and quasi‐RCTs comparing oral dextrose gel versus placebo, no intervention, or other therapies for the prevention of neonatal hypoglycaemia. We included newborn infants at risk of hypoglycaemia, including infants of mothers with diabetes (all types), high or low birthweight, and born preterm (< 37 weeks), age from birth to 24 hours, who had not yet been diagnosed with hypoglycaemia.
Data collection and analysis
Two review authors independently extracted data and assessed the risk of bias. We contacted investigators to obtain additional information. We used fixed‐effect meta‐analyses. We used the GRADE approach to assess the certainty of evidence.
Main results
We included two studies conducted in high‐income countries comparing oral dextrose gel versus placebo in 2548 infants at risk of neonatal hypoglycaemia. Both of these studies were included in the previous version of this review, but new follow‐up data were available for both. We judged these two studies to be at low risk of bias in 13/14 domains, and that the evidence for most outcomes was of moderate certainty.
Meta‐analysis of the two studies showed that oral dextrose gel reduces the risk of hypoglycaemia (risk ratio (RR) 0.87, 95% confidence interval (CI) 0.79 to 0.95; risk difference (RD) ‐0.06, 95% CI ‐0.10 to ‐0.02; 2548 infants; high‐certainty evidence). Evidence from two studies showed that there may be little to no difference in the risk of major neurological disability at two years of age after oral dextrose gel (RR 1.00, 95% CI 0.59 to 1.68; 1554 children; low‐certainty evidence).
Meta‐analysis of the two studies showed that oral dextrose gel probably reduces the risk of receipt of treatment for hypoglycaemia during initial hospital stay (RR 0.89, 95% CI 0.79 to 1.00; 2548 infants; moderate‐certainty evidence) but probably makes little or no difference to the risk of receipt of intravenous treatment for hypoglycaemia (RR 1.01, 0.68 to 1.49; 2548 infants; moderate‐certainty evidence). Oral dextrose gel may have little or no effect on the risk of separation from the mother for treatment of hypoglycaemia (RR 1.12, 95% CI 0.81 to 1.55; two studies, 2548 infants; low‐certainty evidence).
There is probably little or no difference in the risk of adverse effects in infants who receive oral dextrose gel compared to placebo gel (RR 1.22, 95% CI 0.64 to 2.33; two studies, 2510 infants; moderate‐certainty evidence), but there are no studies comparing oral dextrose with other comparators such as no intervention or other therapies.
No data were available on exclusive breastfeeding after discharge.
Authors' conclusions
Prophylactic oral dextrose gel reduces the risk of neonatal hypoglycaemia in at‐risk infants and probably reduces the risk of treatment for hypoglycaemia without adverse effects. It may make little to no difference to the risk of major neurological disability at two years, but the confidence intervals include the possibility of substantial benefit or harm. Evidence at six to seven years is limited to a single small study.
In view of its limited short‐term benefits, prophylactic oral dextrose gel should not be incorporated into routine practice until additional information is available about the balance of risks and harms for later neurological disability. Additional large follow‐up studies at two years of age or older are required. Future research should also be undertaken in other high‐income countries, low‐ and middle‐income countries, preterm infants, using other dextrose gel preparations, and using comparators other than placebo gel. There are three studies awaiting classification and one ongoing study which may alter the conclusions of the review when published.
Keywords: Child; Female; Humans; Infant; Infant, Newborn; Brain Injuries; Glucose; Hypoglycemia; Hypoglycemia/prevention & control; Infant, Low Birth Weight; Infant, Premature
Plain language summary
Oral dextrose gel for prevention of low blood glucose levels in newborn babies
Review question
Is oral dextrose gel effective and safe in preventing low blood glucose levels and reducing long‐term disability in newborn babies at risk of low blood glucose levels?
Key messages
‐ Current evidence is based on two studies in 2548 at‐risk babies in high income countries with outcome assessments in newborns, at two years and six to seven years of age.
‐ Oral dextrose gel is safe and effective in reducing low blood glucose levels in newborn babies at risk of low blood glucose levels.
‐ It is uncertain whether oral dextrose gel increases or decreases disability at two years or older.
Why are low blood glucose levels important?
Low blood sugar (glucose) levels are important because they are common and are associated with brain injury in newborn babies. Up to 39 of every 100 babies will have low blood glucose levels over the first few days after they are born, and as many as half of babies who are at higher risk (those born preterm, or smaller or larger than usual, or whose mothers have diabetes).
Low blood glucose levels can cause problems with academic achievement and development during childhood. Some evidence suggests that even one episode of low blood glucose or episodes that are undetected can contribute to these problems. Therefore, it would be useful to prevent low glucose levels from occurring. Additionally, treatments for low glucose levels often include formula milk or admission to the neonatal unit, leading to the separation of mother and baby. The treatments and the separation may both impair breastfeeding.
How could dextrose gel prevent low blood glucose levels?
Oral dextrose (sugar) gel can be rubbed on the inside of a baby's mouth, where the sugar can be absorbed and thus potentially help prevent low glucose levels.
What did we want to find out?
We wanted to understand whether babies given oral dextrose gel after birth are less likely to:
‐ have low blood sugar levels
‐ have major disability at two years or older
We also wanted to know if oral dextrose gel had any unwanted effects such as vomiting or choking.
What did we do?
We searched for studies that investigated whether oral dextrose gel, compared to another treatment or no treatment, was safe and effective in preventing low blood sugar levels and major disability later in childhood. We also looked at additional clinically important outcomes.
What did we find?
We found two studies, both in high‐income countries, including a total of 2548 at‐risk infants. Both studies assessed the health outcomes of participating children at two years of age, and one also assessed them at six to seven years of age. From reviewing these studies, we are confident that preventative oral dextrose gel reduces the risk of low blood glucose levels in newborn infants at risk. However, we are uncertain whether oral dextrose gel alters the risk of major disability at two years or older, as one study in 360 children showed disability was possibly reduced, while the other study in 2149 children showed it was possibly increased.
Evidence from two studies suggests that infants given oral dextrose gel are not at a higher risk of adverse effects (harms) such as choking or vomiting compared with infants given placebo gel, but there was no information to assess whether oral dextrose gel is safer than no treatment or other therapies. Oral dextrose gel also probably reduces the need for treatment for low blood sugar levels. It may have little to no effect on separation from the mother for treatment of hypoglycaemia, but we have little confidence in this finding because of variation between the two studies. No data were available on exclusive breastfeeding after discharge.
What are the limitations of the evidence?
The two studies were conducted in high‐income countries only, and the findings may not be applicable to other settings. The findings may also not be applicable to preterm infants or other preparations of dextrose gel. Where we were not confident in the evidence was generally because there were only two studies that did not allow us to be certain about the results. Also, there may have been too few events (e.g. adverse effects) to make a conclusion with certainty.
How up‐to‐date is this evidence?
This review updates our previous review, published in 2021. The evidence is up‐to‐date to April 2023.
Summary of findings
Summary of findings 1. Dextrose gel compared with placebo for prevention of hypoglycaemia in newborn infants.
| Dextrose gel compared with placebo for prevention of hypoglycaemia in newborn infants | ||||||
| Patient or population: newborn infants at risk of neonatal hypoglycaemia Setting: New Zealand and Australia Intervention: dextrose gel Comparison: placebo gel | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with placebo | Risk with dextrose gel | |||||
| Hypoglycaemia (investigator‐defined) | 433 per 1000 | 377 per 1000 (342 to 411) | RR 0.87 (0.79 to 0.95) |
2548 (2 RCTs) |
⊕⊕⊕⊕ HIGH | |
| Major neurological disability at 2 years of age (Defined as any of the following: legal blindness, sensorineural deafness requiring hearing aids, moderate or severe cerebral palsy or developmental delay/intellectual impairment (developmental quotient or intelligence quotient lower than 2 SD below the mean)) |
33 per 1000 | 32 per 1000 (19 to 54) | RR 1.00 (0.59 to 1.68) | 1554 (2 RCTs) | ⊕⊕⊝⊝ LOWab |
|
| Receipt of treatment for hypoglycaemia during initial hospital stay (investigator‐defined, any treatment ‐ oral dextrose gel, intravenous dextrose, or other drug therapy) during initial hospital stay (yes/no) |
316 per 1000 | 281 per 1000 (249 to 316) | RR 0.89 (0.79 to 1.00) | 2548 (2 RCTs) | ⊕⊕⊕⊝ MODERATEc | |
| Receipt of intravenous treatment for hypoglycaemia (yes/no) |
37 per 1000 | 37 per 1000 (25 to 55) | RR 1.01 (0.68 to 1.49) | 2548 (2 RCTs) | ⊕⊕⊕⊝ MODERATEa | |
| Adverse events# (e.g. choking or vomiting at time of administration) | 10 per 1000 | 12 per 1000 (6 to 24) |
RR 1.22 (0.64 to 2.33) |
2510 (2 RCTs) |
⊕⊕⊕⊝ MODERATEa | |
| Separation from mother for treatment of hypoglycaemia (infant nursed in an environment that is not in the same room as the mother, e.g. for NICU admission or the like) (yes/no) |
50 per 1000 | 56 per 1000 (40 to 77) | RR 1.12 (0.81 to 1.55) |
2548 (2 RCTs) |
⊕⊕⊝⊝ LOWab |
|
| Breastfeeding (exclusive after discharge) ‐ not reported (WHO 2008 definition (yes/no)) |
‐ | ‐ | ‐ | ‐ | ‐ | No data were reported for this outcome. |
| *The risk in the intervention group (and its 95% confidence interval) is based on assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI); #Placebo gel was the comparator. CI: confidence interval; NICU: neonatal intensive care unit; OR: odds ratio; RR: risk ratio; SD: standard deviations | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect | ||||||
aDowngraded one level for serious imprecision (due to the wide CI and low event rates)
bDowngraded one level for serious inconsistency (due to the high I2 value of > 75%)
cDowngraded one level for serious imprecision (due to the CI including the possibility of benefit and harm)
Background
Description of the condition
Hypoglycaemia is the commonest metabolic disorder of the newborn (Harris 2012; Hay 2009). Up to 39% of newborn infants will have low blood glucose concentrations (Harris 2020). The rate is higher in infants with risk factors: those whose mothers have diabetes (Agrawal 2000; Maayan‐Metzger 2009), large for gestational age (Weissmann‐Brenner 2012), small for gestational age (Hawdon 1993), or preterm (Kerstjens 2012). Fifty per cent of these infants will develop at least one episode of hypoglycaemia (Harris 2012). Additional risk factors for neonatal hypoglycaemia include perinatal asphyxia (Salhab 2004), prolonged labour, hypothermia, sepsis, and maternal medications such as beta‐agonists (Kurtoglu 2005), beta‐blockers (de Bruin 2022; Daskas 2013), and antenatal corticosteroids (Deshmukh 2021).
Severe symptomatic and prolonged neonatal hypoglycaemia can cause both brain damage (Burns 2008; Duvanel 1999; Kerstjens 2012; Koh 1988), and death (Achoki 2010; Cornblath 1965; Nadjm 2013; Willcox 2010). Early magnetic resonance imaging (MRI) studies reported the commonest site of damage is in the occipital cortex (Alkalay 2005; Spar 1994). However, more widespread MRI changes may also be seen in the temporoparietal region, cerebral cortex, and basal ganglia/thalamus (Burns 2008). MRI changes in the subcortical grey matter, occipital lobe, caudate and thalamus in 9‐to 10‐year‐old children have more recently been reported after neonatal hypoglycaemia (Nivins 2022).
The effect of less severe neonatal hypoglycaemia on longer‐term outcomes is not yet well‐defined. A retrospective population study of transient hypoglycaemia (defined as a single initial blood glucose concentration of less than 2.6 mmol/L, followed by a repeat result above this) demonstrated an association between low initial blood glucose concentration and lower academic test scores at 10 years of age (Kaiser 2015). However, in a cohort of babies at risk of neonatal hypoglycaemia, half of whom became hypoglycaemic and were treated to maintain blood glucose concentrations ≥ 2.6 mmol/L, there was no difference in neurodevelopmental outcome at two years (McKinlay 2015) or at 9 to10 years (Shah 2022), between those who did and did not experience neonatal hypoglycaemia, although those who experienced hypoglycaemia were at increased risk of executive and visual‐motor dysfunction at 4.5 years (McKinlay 2017).
The definition of neonatal hypoglycaemia remains controversial, with various definitions used in publications (Agrawal 2000; Burns 2008; Kerstjens 2012; Maayan‐Metzger 2009), and suggested as thresholds for intervention in current guidelines (Adamkin 2011; BAPM 2017; Narvey 2019). A widely accepted definition is < 2.6 mmol/L (Adamkin 2011; Harris 2014; Narvey 2019). This is heavily influenced by the description of abnormal sensory evoked potentials in infants who had blood glucose concentrations of < 2.6 mmol/L (Koh 1988), and of a relationship between the number of days on which blood glucose measurements of < 2.6 mmol/L were recorded in preterm infants and neurodevelopmental impairment at 18 months (Lucas 1988), and at seven to eight years (Lucas 1999).
Treatment of neonatal hypoglycaemia commonly requires admission to a newborn intensive care unit (NICU) or special care baby unit (SCBU), separating mothers and infants and interfering with the establishment of breastfeeding, thus incurring a high social and financial cost. The World Health Organization, in its publication on neonatal hypoglycaemia, states “… an approach aimed first at the prevention of hypoglycaemia, second at its reliable detection in infants at risk and third at appropriate treatment which will not be deleterious to breastfeeding is … of global importance” (WHO 1997). The American Academy of Pediatrics recommends “… early identification of the at‐risk infant and institution of prophylactic measures to prevent neonatal hypoglycaemia” (Adamkin 2011).
Widely accepted clinical monitoring of infants at risk of neonatal hypoglycaemia involves:
early identification of pertinent risk factors;
early feeding;
pre‐feed blood glucose concentration measurement to determine blood glucose concentrations at the time when it is most at risk of being low;
monitoring during the period of highest risk until blood glucose concentration is demonstrated to remain above the chosen threshold for intervention (Adamkin 2011; Narvey 2019; NICE 2008; UNICEF 2013; WHO 1997).
Despite these recommendations to prevent neonatal hypoglycaemia, there is little evidence of any effective interventions to achieve this.
Antenatal expression of colostrum is considered to potentially increase the colostrum supply available for infants following birth, reduce the time taken to establish breastfeeding and decrease formula use (Cox 2006). One small retrospective study of mothers with diabetes who expressed colostrum antenatally reported that they gave birth one week earlier, and the rates of admission of their infants to the NICU were increased compared with mothers with diabetes who did not express (Soltani 2012). However, in a randomised trial involving women with diabetes allocated to antenatal expression or no expression, there was no change in the incidence of neonatal hypoglycaemia or admission to NICU (Forster 2017).
Early initiation of breastfeeding within 30 minutes following birth has no effect on the blood glucose concentration at one and two hours after birth in infants without risk factors for neonatal hypoglycaemia (Sweet 1999; Zhou 2017). However, early feeding (within 30 minutes of birth) of infants of mothers with diabetes was reported to decrease the incidence of subsequent neonatal hypoglycaemia, and these infants maintained a higher mean blood glucose concentration than those who received their first feed later (Chertok 2009). Other studies on early feeding plus skin‐to‐skin contact have reported similar findings (Boundy 2016; Dalsgaard 2019; Moore 2016), but these studies are small and of poor quality.
Supplementation or substitution of breastfeeding with fluid or foods other than expressed breast milk may reduce the duration of breastfeeding (Becker 2016; Blomquist 1994). Therefore, the commonly accepted practice is to advise exclusive breastfeeding (Eidelman 2012; UNICEF 2013). Healthy newborn infants will usually maintain their blood glucose concentration despite the small‐volume, low‐energy food source provided by colostrum. However, colostrum alone cannot be relied upon to meet the essential energy needs of infants with additional risk factors for neonatal hypoglycaemia. Thus, infants at risk of hypoglycaemia frequently receive supplemental or complementary feeding during establishment of feeding (Blomquist 1994; Harris 2013).
Powdered sugar has been used as an addition to formula in an attempt to prevent neonatal hypoglycaemia. Two randomised trials in India compared formula with formula plus added powdered sugar for the prevention of subsequent hypoglycaemia in infants at risk of hypoglycaemia (small for gestational age and large for gestational age). Both studies reported a significant reduction in the incidence of subsequent hypoglycaemia in the infants who received formula plus powdered sugar (Singhal 1991; Singhal 1992). In contrast, a more recent randomised trial comparing oral sucrose solution plus feeding versus feeding alone for preventing neonatal hypoglycaemia in at‐risk infants reported similar blood glucose concentrations within six hours after birth in both groups (Surachaidungtavil 2020).
The ideal intervention would be effective in preventing hypoglycaemia, reduce the need for artificial formula, improve breastfeeding rates, reduce costs, as well as potentially reduce the risk of later adverse outcomes. Oral dextrose given as 200 mg/kg (0.5 mL/kg) of 40% dextrose gel has been shown to be effective and safe in treating neonatal hypoglycaemia (Gupta 2022; Harris 2013), and is cost‐effective (Glasgow 2018). A separate Cochrane Review, “Oral dextrose gel for the treatment of hypoglycaemia in newborn infants” was published in 2022. In comparison to placebo, oral dextrose gel was found to probably increase correction of hypoglycaemic events and probably increase exclusive breastfeeding after discharge (Edwards 2022).
Description of the intervention
This review assesses the use of oral dextrose gel in the prevention of neonatal hypoglycaemia.
Dextrose gel is a non‐proprietary, low‐cost, simple carbohydrate in concentrated thickened aqueous solution, which can be administered by direct application to the oral mucosa ‐ either buccal or sublingual. Administration via these highly vascularised, thin mucous membranes allows rapid access to the circulation. Some of the administered gel may be swallowed and absorbed from the gastrointestinal tract.
Commercially manufactured gel costs approximately NZD 86 per 100 mL. Alternatively, gel can be prepared in hospital pharmacies (Harris 2013). Ingredients will vary by pharmaceutical manufacturer but commonly include water, glucose, a gelling agent and preservative(s). Some preparations include flavourings and colourings, and the concentrations of glucose may vary (Solimano 2019). Suitability of the gel for use in neonates should be assessed on an individual basis. The difference in effectiveness of various formulations is unknown.
How the intervention might work
Dextrose gel administered to the oral mucosa will enter the systemic circulation via the lingual vein and the internal jugular vein. This is in comparison to oral‐gastrointestinal administration, where the first pass effect of the portal circulation may minimise any change in systemic blood glucose concentrations. Prevention of neonatal hypoglycaemia by providing additional glucose during the period of the neonatal metabolic transition may reduce the medical prescription of artificial formula feeds, reduce admission to the NICU for intravenous dextrose, and prevent the neurodevelopmental impairment associated with neonatal hypoglycaemia. There is no evidence of possible differences in effect in different populations.
Why it is important to do this review
Neonatal hypoglycaemia is important because it is common, and it may be associated with brain injury in newborn infants. There are known risk factors for neonatal hypoglycaemia, so specific groups of infants are routinely targeted for screening (i.e. those who are infants of mothers with diabetes, high or low birth weight, preterm and those with poor feeding). These infants are frequently treated with supplemental formula milk or admitted to neonatal units for intravenous dextrose. Supplemental formula may impair establishment of breastfeeding and intravenous treatment is expensive, not always available in resource‐poor settings and usually requires separation of the mother and infant.
Oral dextrose gel is simple to administer and inexpensive. Therefore, if it is effective in preventing neonatal hypoglycaemia, it would have many advantages, particularly in low‐resource settings.
The results of this review may help to inform those preparing clinical practice guidelines, such as those currently available to guide the care of babies at risk of neonatal hypoglycaemia (Adamkin 2011; BAPM 2017; UNICEF 2013; Wight 2021).
Objectives
To assess the effectiveness and safety of oral dextrose gel in preventing hypoglycaemia before first hospital discharge and reducing long‐term neurodevelopmental impairment in newborn infants at risk of hypoglycaemia.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) and quasi‐RCTs, including cluster‐randomised trials, were considered for inclusion. Cross‐over trials were excluded because they would require each infant to act as its own control, which is inappropriate in this context. We included both published and unpublished studies. We included unpublished studies and studies published only as abstracts when assessment of study quality was possible and if other criteria for inclusion were fulfilled.
Types of participants
Newborn infants at risk of hypoglycaemia, including infants of mothers with diabetes (all types), high or low birthweight, and born preterm (< 37 weeks), age from birth to 24 hours, who had not yet been diagnosed with hypoglycaemia (blood glucose concentration below normal range, investigator‐defined) or had treatment for hypoglycaemia. If study authors reported on only a subset of relevant participants, they were contacted for data from the full study sample.
Types of interventions
Dextrose gel, of any concentration and at any dose or number of doses, given orally compared with placebo, no treatment or standard care, or other therapies (such as antenatal expression of colostrum, early initiation of breastfeeding, supplementation or substitution of breastfeeding with formula milk), for the prevention of hypoglycaemia at any gestational age and commenced within the first 24 hours following birth.
Types of outcome measures
Primary outcomes
Hypoglycaemia ‐ investigator‐defined
Major neurological disability at two years of age or older, defined as any of the following: legal blindness, sensorineural deafness requiring hearing aids, moderate or severe cerebral palsy, or developmental delay/intellectual impairment (developmental quotient or intelligence quotient lower than two standard deviations below the mean)
Secondary outcomes
Hypoglycaemia (any blood glucose concentration < 2.6 mmol/L) during initial hospital stay ‐ Harris 2014 definition (yes/no);
Receipt of treatment for hypoglycaemia (investigator‐defined, any treatment ‐ oral dextrose gel, intravenous dextrose, or other drug therapy) during initial hospital stay (yes/no);
Separation from mother for treatment of hypoglycaemia (infant being nursed in an environment that is not in the same room as the mother, e.g. neonatal unit) (yes/no);
Receipt of intravenous treatment for hypoglycaemia (yes/no);
Adverse effects (e.g. choking or vomiting at time of administration) (yes/no);
Exclusive breastfeeding after discharge ‐ WHO 2008 definition (yes/no);
Developmental disability at two years of age or greater ‐ investigator‐defined (yes/no);
Receipt of oral dextrose gel treatment for hypoglycaemia (yes/no);
Receipt of any medications for hypoglycaemia, such as glucagon, diazoxide, or corticosteroids (yes/no);
Number of episodes of hypoglycaemia ‐ investigator‐defined (total number per infant);
Neonatal seizures (yes/no);
Abnormal MRI of the brain in the neonatal period (yes/no);
Duration of initial hospital stay (days);
Breastfeeding (any) after discharge (yes/no);
Exclusive breastfeeding at six months of age ‐ WHO 2008 definition (yes/no);
Visual impairment and severity of impairment at two years of age or older;
Hearing impairment and severity of impairment at two years of age or older;
Cerebral palsy and severity of disorder at two years of age or older;
Developmental delay/intellectual impairment and severity of impairment at two years of age or older;
Executive dysfunction and severity of dysfunction at two years of age or older;
Behavioural problems and severity of problems at two years of age or older;
Abnormal MRI of the brain at two years of age or older;
Costs associated with the intervention ‐ investigator‐defined.
Search methods for identification of studies
The Neonatal Group Information Specialist developed a draft search strategy for Ovid MEDLINE (Appendix 1). This strategy was translated for other databases, using appropriate syntax and controlled vocabulary, then peer reviewed by a Medical Librarian.
A population filter developed by Cochrane Neonatal was used to limit retrieval, and methodological filters were used to identify randomised controlled and quasi‐randomised studies and systematic reviews. Searches for eligible trials were conducted without language, publication year, publication type, or publication status restrictions. Searches were documented in sufficient detail to inform a study flow (PRISMA) diagram (Figure 1), (Liberati 2009; Moher 2009).
1.
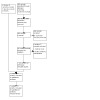
Study flow diagram
Electronic searches
We conducted a comprehensive search including:
Cochrane Central Register of Controlled Trials (CENTRAL) Issue 4 of 12, April 2023;
Ovid MEDLINE (from 1946 to 26 April 2023);
Ovid Embase (from 1980 to 26 April 2023);
Epistemonikos (to 26 April 2023).
We have included the search strategies for each database in Appendix 1. Previous search methods are available in Appendix 2.
Searching other resources
Trial registration records were identified using CENTRAL and by independent searches of:
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (clinicaltrials.gov);
World Health Organization International Clinical Trials Registry Platform (ICTRP);
ISRCTN registry;
Australian New Zealand Clinical Trials Registry (ANZCTR).
Conference abstracts were identified using CENTRAL and the following websites:
Pediatric Academic Societies (PAS);
Eastern Society for Pediatric Research (ESPR);
Perinatal Society of Australia and New Zealand (PSANZ).
We searched the reference lists of included studies and approached well‐known researchers in this clinical area to identify any unpublished or ongoing research.
Data collection and analysis
We collected information regarding the setting, method of randomisation, blinding, and intervention for each included study. We noted information regarding trial participants including maternal diabetes status, infant weight category, ethnic group, and other hypoglycaemia risk factors. We analysed the clinical outcomes noted above under Types of outcome measures.
Selection of studies
Two review authors (LR, LL) independently assessed the eligibility of each study for inclusion. We did not encounter any disagreements.
Data extraction and management
Two review authors (LR, LL) independently extracted data from the eligible studies. We did not encounter any disagreements. One review author (LR) entered consensus data into Review Manager Web (RevMan Web 2023). This data was validated by the second review author (LL).
Assessment of risk of bias in included studies
Two review authors (LR, LL) independently assessed the risk of bias (low, high, or unclear) in all included studies using the Cochrane ‘Risk of bias 1’ tool (Higgins 2011), for these domains:
sequence generation (selection bias);
allocation concealment (selection bias);
blinding of participants and personnel (performance bias);
blinding of outcome assessment (detection bias);
incomplete outcome data (attrition bias);
selective reporting (reporting bias);
any other bias.
Any disagreements were resolved by discussion or by a third assessor. See Appendix 3 for a more detailed description of the risk of bias for each domain
Measures of treatment effect
We used the numbers of events in control and intervention groups of each study to calculate risk ratios (RRs) for dichotomous data. We calculated mean differences (MDs) between treatment groups when outcomes were measured in the same way for continuous data. We reported risk differences (RDs) and, when a significant effect was found, we calculated numbers needed to treat for an additional beneficial outcome (NNTB) or numbers needed to treat for an additional harmful outcome (NNTH). We reported 95% confidence intervals (CIs) for all outcomes.
Unit of analysis issues
We planned to include cluster‐randomised trials in analyses along with individually randomised trials, but we did not identify any cluster‐randomised trials for inclusion.
Dealing with missing data
We carried out analyses on an intention‐to‐treat basis for all outcomes. We contacted the original investigators to request missing data, when possible.
Assessment of heterogeneity
We considered whether clinical and methodological characteristics of the included studies were sufficiently similar for meta‐analysis to provide a clinically meaningful summary by assessing statistical heterogeneity using the Chi2 test and the I2 statistic, considering an I2 value of less than 25% to be none, 25% to 49% low, 50% to 74% moderate, and 75% or greater to be high heterogeneity. We took an I2 value greater than 50% and a low P value (< 0.10) from the Chi2 test for heterogeneity to indicate substantial heterogeneity (Higgins 2022). If we detected substantial heterogeneity, we planned to explore possible explanations by performing sensitivity or subgroup analyses, but we were unable to do this given the small number of eligible trials. We took statistical heterogeneity into account when interpreting results, especially when we noted variation in the direction of effect.
Assessment of reporting biases
Reporting biases arise when dissemination of research findings is influenced by the nature and direction of results. Some types of reporting bias (e.g. publication bias, multiple publication bias, language bias) reduce the likelihood that all studies eligible for a review will be retrieved. If all eligible studies are not retrieved, the review may be biased. We conducted a comprehensive search for eligible studies and were alert for duplication of data. We were unable to assess publication bias by visually inspecting a funnel plot because we did not identify 10 or more trials to make such an inspection valid. Two review authors (LR, LL) examined the methods of each study for prespecified outcomes and, if all prespecified outcomes were reported in the results, we considered the study carried low risk of bias. If any prespecified outcome was not reported in the results, we considered the study to carry a higher risk of bias.
Data synthesis
We evaluated studies for potential clinical diversity and planned to restrict meta‐analysis to situations in which clinical consistency was apparent. We evaluated studies for bias, as above, and restricted meta‐analysis if bias would have been compounded. We used a fixed‐effect model to combine data when it was reasonable to assume that studies were estimating the same underlying treatment effect. If we found evidence of clinical heterogeneity, we planned to try to explain this on the basis of different study characteristics and subgroup analyses.
Subgroup analysis and investigation of heterogeneity
We planned to carry out the following subgroup analyses using a fixed‐effect model.
Reason for risk of hypoglycaemia (infant of diabetic mother, preterm, small or large for gestational age, other);
Gestational age at birth (term and post‐term versus late preterm 35 to 36 weeks versus moderately preterm 30 to 34 weeks versus extremely preterm < 30 weeks);
Actual mode of feeding (formula versus breast milk versus mixed);
Method of administration of gel (rubbed into buccal mucosa versus sublingual versus other);
Dose of dextrose gel per administration (≤ 200 mg/kg versus > 200 mg/kg);
Number of dextrose gel doses administered (one dose versus > one dose);
Time of administration of first dose of gel (within one hour of age versus after one hour of age versus after two hours of age).
Sensitivity analysis
We planned to conduct sensitivity analysis by examining only trials considered to have a low risk of bias across all domains as determined by the Cochrane ‘Risk of bias 1’ tool (Higgins 2011). We planned to report results of sensitivity analyses for primary outcomes only. However, we did not conduct the planned sensitivity analyses because the included trials had a low risk of bias.
Summary of findings and assessment of the certainty of the evidence
We used the GRADE approach, as outlined in the GRADE Handbook (Schünemann 2013), to assess the certainty of evidence for the following (clinically relevant) outcomes:
hypoglycaemia;
major neurological disability at two years of age or older;
receipt of treatment for hypoglycaemia during initial hospital stay;
separation from the mother for treatment of hypoglycaemia;
receipt of intravenous treatment for hypoglycaemia;
adverse effects; and
exclusive breastfeeding after discharge.
Two review authors (LR, LL) independently assessed the certainty of evidence for each of the outcomes. We considered evidence from randomised controlled trials as high certainty but downgraded the evidence by one level for serious (or two levels for very serious) limitations on the basis of the following: design (risk of bias), consistency across studies, directness of evidence, precision of estimates, and presence of publication bias. We used the (GRADEpro GDT), Guideline Development Tool to create ‘Table 1’ to report the certainty of evidence.
The GRADE approach results in an assessment of the certainty of a body of evidence as one of four grades.
High certainty: further research is very unlikely to change our confidence in the estimate of effect.
Moderate certainty: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
Low certainty: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low certainty: we are very uncertain about the estimate.
We justified all decisions to downgrade the certainty of the evidence using footnotes and made comments to aid the reader's understanding of the review where necessary.
Results
Description of studies
We included two studies in this update: both of which were identified in the previous Cochrane Review (Edwards 2021), and had new follow‐up data.
Results of the search
See Characteristics of included studies, Characteristics of excluded studies, Characteristics of studies awaiting classification, and Characteristics of ongoing studies.
Our search in April 2023 identified 390 records, of which 91 were automatically removed as duplicates. After screening the titles and abstracts of 299 records, we excluded 250 because they were not relevant and manually removed 31 duplicates. Upon review of the full text of 18 records (see Figure 1), we excluded six primary and one secondary reference(s) (Bourchier 1992; Burch 2021; Coors 2018; Gupta 2022; Retbi 2013; Van Loghum 2014). One relevant study is ongoing (NCT04353713); and three are awaiting classification (CTRI/2017/11/010645; NCT04185766; TCTR20190805003).
Included studies
Participants
We identified two eligible randomised, blinded, placebo‐controlled trials (Harding 2021; Hegarty 2016a), associated with 13 records, that enrolled a total of 2548 late preterm and term infants born at risk of neonatal hypoglycaemia. At‐risk infants included infants born to mothers with diabetes, late preterm (35 to 36 weeks' gestation), or small (< 2.5 kg or < 10th percentile) or large birthweight (> 4.5 kg or > 90th percentile). The included studies recruited from 18 maternity hospitals in New Zealand and Australia (Harding 2021) and from two hospitals in New Zealand (Hegarty 2016a).
Interventions
In one study, at‐risk infants were randomised to receive a single dose of 40% dextrose gel or placebo gel (Harding 2021). In the other study, infants were randomised in a 2:1 ratio to one of the following dose regimens of 40% dextrose gel or placebo: 0.5 mL/kg once, 1 mL/kg once, 0.5 mL/kg for four doses, and 1 mL/kg once followed by 0.5 mL/kg for three additional doses (Hegarty 2016a). In both studies, the gel was massaged into the buccal mucosa at one hour after birth followed by breastfeeding. Blood glucose concentration was measured using the glucose oxidase method at two hours after birth, and subsequent measurements were performed according to local hospital protocol.
Outcome assessment
The primary outcomes were hypoglycaemia (blood glucose concentration < 2.6 mmol/l) in Hegarty 2016a and admission to neonatal intensive care or special care in Harding 2021, and were assessed in all 2548 infants. Of the 1722 children eligible for health outcomes assessment at two years' corrected age, 1557 children (90%) were assessed. One study additionally assessed 315 of 392 eligible children (80%) at six to seven years' corrected age (Hegarty 2016a).
See Characteristics of included studies for further information about the included studies.
Studies awaiting classification
Three studies are awaiting classification as it is unclear whether they meet the inclusion criteria for this review since their findings are not yet publicly available (CTRI/2017/11/010645, NCT04185766, TCTR20190805003). Authors of these three studies were contacted in May 2023, and we received no confirmation of publication. See Characteristics of studies awaiting classification for more information about these studies.
Ongoing studies
One study is classified as ongoing (NCT04353713) since it meets the inclusion criteria of our review, but its findings are not yet publicly available. See Characteristics of ongoing studies for more information about this study.
Excluded studies
We excluded six studies (seven records) for the following reasons:
Three studies were commentaries which evaluated dextrose gel as a treatment for neonatal hypoglycaemia (Bourchier 1992; Retbi 2013; Van Loghum 2014).
One study was a randomised controlled trial which evaluated dextrose gel as a treatment for neonatal hypoglycaemia (Gupta 2022).
One study (two records) was a non‐randomised study which investigated oral dextrose gel as prophylaxis against transient neonatal hypoglycaemia in at‐risk infants (Coors 2018).
One study was a Cochrane clinical answer that investigated oral dextrose gel application for the prevention of neonatal hypoglycaemia in at‐risk infants (Burch 2021).
See Characteristics of excluded studies for further details.
Risk of bias in included studies
Refer to Figure 2 and Figure 3 for a summary of the risk of bias assessment and Characteristics of included studies for more details.
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Allocation
Both studies reported using computer‐generated block randomisation with variable block sizes (Harding 2021; Hegarty 2016a). Allocation was concealed by a central randomisation system which assigned infants to a numbered trial pack containing identical‐looking syringes of either dextrose or placebo gel. We judged these studies to be at a low risk of selection bias.
Blinding
Both studies reported that clinicians, families and all study personnel were masked to treatment allocation (Harding 2021; Hegarty 2016a). The two‐year and six to seven‐year follow‐up reports stated that follow‐up assessors were unaware of the infant’s treatment allocation (Harding 2021; Hegarty 2016a). We judged these studies to be at low risk of performance and detection bias.
Incomplete outcome data
Both studies included all randomised infants in the intention‐to‐treat analysis of neonatal outcomes (Harding 2021; Hegarty 2016a). Hegarty 2016a assessed 90% of those eligible at two years' corrected age (dextrose 243/271 and placebo 117/130) and 87% of those randomised (dextrose 243/277 and placebo 117/138). The same study assessed 80% of those eligible at six to seven years' of age (315/392) and 76% of those randomised (315/415). Harding 2021 assessed 91% (1197/1321) of those eligible at two years' corrected age and 56% (1197/2149) of those randomised. In both studies, maternal and child characteristics were similar in those who were and were not assessed at two years. However, those assessed at six to seven years of age were born slightly earlier and had older mothers who were more likely to have received tertiary education upon entry to the trial. We judged these studies to be at low risk of attrition bias.
Selective reporting
Both studies reported data for all outcomes prespecified in the trial registration documentation (Harding 2021; Hegarty 2016a). We judged these studies to be at low risk of reporting bias.
Other potential sources of bias
Both studies reported that the demographic and prognostic characteristics of infants in each trial arm were balanced at baseline (Harding 2021; Hegarty 2016a). One study, however, noted an imbalance between characteristics of those assessed and those not assessed at two years' and six to seven years of age (Hegarty 2016a). It is unclear whether this imbalance would result in bias. We did not identify any other potential sources of bias. We judged these studies to be at low (Harding 2021) and unclear (Hegarty 2016a) risk of other bias.
Effects of interventions
See: Table 1
Primary outcomes
Hypoglycaemia ‐ investigator‐defined
Meta‐analysis showed that oral dextrose gel reduces the risk of neonatal hypoglycaemia (defined as a blood glucose concentration < 2.6 mmol/L) compared with placebo gel (RR 0.87, 95% CI 0.79 to 0.95; two studies, 2548 infants; high‐certainty evidence; Analysis 1.1). The RD was ‐0.06 (95% CI ‐0.10 to ‐0.02) and, on average, 17 infants would have to receive prophylactic dextrose gel to prevent one additional case of neonatal hypoglycaemia.
1.1. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 1: Hypoglycaemia
Major neurological disability at two years or older
Meta‐analysis showed that there may be little to no difference in the risk of major neurological disability at two years of age after oral dextrose gel compared with placebo gel (RR 1.00, 95% CI 0.59 to 1.68; two studies, 1554 children; low‐certainty evidence; Analysis 1.2). There is substantial heterogeneity for this outcome (I2 = 85%, P = 0.009), with the direction of effect suggesting benefit in one study (Hegarty 2016a), and possible harm in the other, larger study (Harding 2021).
1.2. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 2: Major neurological disability at two years of age
Evidence from one study (Hegarty 2016a) showed that oral dextrose gel probably does not reduce the risk of major neurological disability at six to seven years of age compared with placebo gel (RR 0.72, 95% CI 0.49 to 1.06; one study; 308 children; Analysis 1.3).
1.3. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 3: Major neurological disability at six to seven years of age
Data from one study (Harding 2021) found no evidence that the effect of oral dextrose gel on major neurological disability at two years of age differed in children of mothers with diabetes (RR 1.10, 95% CI 0.54, 2.23; one study; 900 children; Analysis 1.4), compared to children with other risk factors for neonatal hypoglycaemia (RR 3.95, 95% CI 0.85, 18.27; one study; 294 children; Analysis 1.4) (subgroup effect P = 0.14, I² = 54.4%).
1.4. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 4: Major neurological disability at two years of age ‐ by risk factor
Secondary outcomes
Hypoglycaemia (any blood glucose concentration less than 2.6 mmol/L) during initial hospital stay ‐ Harris 2014 definition
Meta‐analysis showed that oral dextrose gel reduces the risk of neonatal hypoglycaemia (defined as a blood glucose concentration < 2.6 mmol/L in the first 48 hours) compared to placebo gel (RR 0.87, 95% CI 0.79 to 0.95; two studies, 2548 infants; high‐certainty evidence; Analysis 1.1). The RD was ‐0.06 (95% CI ‐0.10 to ‐0.02) and, on average, 17 infants would have to receive prophylactic dextrose gel to prevent one additional case of neonatal hypoglycaemia.
Receipt of treatment (investigator‐defined, any treatment ‐ oral dextrose gel, intravenous dextrose or other drug therapy) for hypoglycaemia during initial hospital stay
Meta‐analysis showed that oral dextrose gel probably reduces the risk of receipt of treatment for neonatal hypoglycaemia compared with placebo gel (RR 0.89, 95% CI 0.79 to 1.00; two studies, 2548 infants; moderate‐certainty evidence; Analysis 1.5). The RD was ‐0.03 (95% CI ‐0.07 to 0.00) and, on average, 33 infants would have to receive prophylactic dextrose gel to prevent one receiving treatment for hypoglycaemia during the initial hospital stay.
1.5. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 5: Receipt of treatment for hypoglycaemia during initial hospital stay
Separation from the mother for treatment of hypoglycaemia (infant being nursed in an environment that is not in the same room as the mother, e.g. neonatal unit)
Meta‐analysis showed that oral dextrose gel may not reduce separation of the infant from the mother for treatment of neonatal hypoglycaemia compared to placebo gel (RR 1.12, 95% CI 0.81 to 1.55; two studies, 2548 infants; low‐certainty evidence; Analysis 1.6). There is substantial heterogeneity for this outcome (I2 = 83%, P = 0.02), with the direction of effect suggesting benefit in one study (Hegarty 2016a), and possible harm in the other, larger study (Harding 2021).
1.6. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 6: Separation from mother for treatment of hypoglycaemia (admission to NICU for hypoglycaemia)
Receipt of intravenous treatment for hypoglycaemia
Meta‐analysis including additional data from the authors of one study (Harding 2021), showed that oral dextrose gel probably does not reduce receipt of intravenous treatment for hypoglycaemia compared to placebo gel (RR 1.01, 95% CI 0.68 to 1.49; two studies, 2548 infants; moderate‐certainty evidence; Analysis 1.7).
1.7. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 7: Receipt of intravenous treatment for hypoglycaemia
Adverse effects e.g. choking or vomiting at the time of administration
Meta‐analysis including additional data from the authors of one study (Harding 2021) showed that oral dextrose gel probably does not increase the risk of adverse effects compared to placebo gel (RR 1.22, 95% CI 0.64 to 2.33; two studies, 2510 infants; moderate‐certainty evidence; Analysis 1.8).
1.8. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 8: Adverse effects (e.g. choking or vomiting at time of administration)
Exclusive breastfeeding after discharge ‐ WHO 2008 definition
No data were available for this outcome.
Developmental disability at two years of age or greater
Meta‐analysis showed that oral dextrose gel may not reduce the risk of any developmental disability compared to placebo gel at two years of age (RR 1.03, 95% CI 0.84 to 1.26; two studies; 1553 children; Analysis 1.9) or at six to seven years of age (RR 0.85, 95% CI 0.68 to 1.07; one study; 308 children; Analysis 1.10).
1.9. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 9: Developmental disability at two years of age
1.10. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 10: Developmental disability at six to seven years of age
Data from one study (Harding 2021) found no evidence that the effect of oral dextrose gel on any developmental disability at two years of age was different amongst children of mothers with diabetes (RR 1.12, 95% CI 0.87 to 1.46; 900 children; Analysis 1.11), compared to children with other risk factors for neonatal hypoglycaemia (RR 1.07, 95% CI 0.65 to 1.75; 294 children; Analysis 1.11), (subgroup effect P = 0.85, I² = 0%).
1.11. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 11: Any neurological disability at two years of age ‐ by risk factor
Data from one study (Hegarty 2016a) found no evidence that the effect of oral dextrose gel on any developmental disability at six to seven years of age was different amongst children of mothers with diabetes (RR 0.80, 95% CI 0.63 to 1.02; 219 children; Analysis 1.12), compared to children with other risk factors for neonatal hypoglycaemia (RR 0.99, 95% CI 0.59 to 1.68; 89 children; Analysis 1.12) (subgroup effect P = 0.46, I² = 0%). Data from the same study found no evidence that the effect of oral dextrose gel on any developmental disability at six to seven years of age was different amongst children who received a single dose of gel (RR 0.82, 95% CI 0.61 to 1.10; 167 children; Analysis 1.13), compared to those who received multiple doses (RR 0.90, 95% CI 0.64 to 1.27; 141 children; Analysis 1.13), (subgroup effect P = 0.68, I² = 0%).
1.12. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 12: Any neurological disability at six to seven years of age ‐ by risk factor
1.13. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 13: Any neurological disability at six to seven years of age ‐ by single or multiple gel dose
Receipt of oral dextrose gel treatment for hypoglycaemia
Meta‐analysis showed that prophylactic oral dextrose gel may not reduce the receipt of oral dextrose gel for treatment of hypoglycaemia compared to placebo gel (RR 0.90, 95% CI 0.79 to 1.01; two studies, 2548 infants; Analysis 1.14).
1.14. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 14: Receipt of oral dextrose gel treatment for hypoglycaemia
Receipt of any medications for hypoglycaemia, such as glucagon, diazoxide or corticosteroids
Additional data received from the authors of both studies showed that no infants in either the dextrose gel or placebo groups received any medication for hypoglycaemia, such as glucagon, diazoxide, or corticosteroids (Analysis 1.15).
1.15. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 15: Receipt of any medications for hypoglycaemia such as glucagon or corticosteroids
Number of episodes of hypoglycaemia ‐ investigator‐defined (total number per infant)
Data from one study (Hegarty 2016a) showed that there may be no difference in the number of episodes of hypoglycaemia per infant after oral dextrose gel compared to placebo gel (MD ‐0.18, 95% CI ‐0.55 to 0.19; one study, 186 infants; Analysis 1.16).
1.16. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 16: Number of episodes of hypoglycaemia (glucose oxidase method) (total number per infant)
Neonatal seizures
Only one event of neonatal seizures was reported in the dextrose gel group in Hegarty 2016a and one event of neonatal seizures was reported in the placebo group in Harding 2021 (RR 0.69, 95% CI 0.08 to 5.69; two studies, 2548 infants; Analysis 1.17). Both studies reported that the seizures were unrelated to neonatal hypoglycaemia.
1.17. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 17: Neonatal seizures
Abnormal MRI of the brain in the neonatal period
No data were available for this outcome.
Duration of initial hospital stay (days)
We received additional data from the authors of both studies which showed that oral dextrose gel probably makes little or no difference to the mean duration of initial hospital stay (days) (MD 0.06, 95% CI ‐0.13 to 0.24; two studies, 2537 infants; Analysis 1.18).
1.18. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 18: Duration of initial hospital stay (days)
Breastfeeding (any) after discharge
Data from both studies showed that there is little to no difference in breastfeeding (full or exclusive) after discharge after oral dextrose gel compared to placebo gel (RR 1.01, 95% CI 0.98 to 1.05; two studies, 2323 infants; Analysis 1.19).
1.19. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 19: Breastfeeding (any) after discharge
Exclusive breastfeeding at six months of age – WHO 2008 definition
No data were available for this outcome.
Visual impairment and severity at two years of age or greater
At two years of age, only two events of visual impairment were reported in the placebo gel group (2/703; 0.3%) and none in the dextrose gel group across two studies. Due to low event numbers, it is very uncertain whether dextrose gel alters the rate of visual impairment compared to placebo gel (RR 0.19, 95% CI 0.01 to 4.03; two studies; 1551 children; Analysis 1.20). There was no information related to the severity of visual impairment.
1.20. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 20: Visual impairment at two years of age
Hearing impairment and severity at two years of age or greater
At two years of age, hearing impairment was reported in one child in the dextrose gel group (1/848; 0.1%) and three children in the placebo gel group (3/703; 0.4%) across two studies. Due to low event numbers, it is very uncertain whether dextrose gel alters the rate of hearing impairment compared to placebo gel (RR 0.32, 95% CI 0.05 to 2.05; two studies, 1551 children; Analysis 1.21). No data were available regarding the severity of hearing impairment.
1.21. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 21: Hearing impairment at two years of age
Cerebral palsy and severity at two years of age or greater
At two years of age, one child in the dextrose gel group had mild cerebral palsy (1/844; 0.2%) and two children in the placebo gel group had moderate or severe cerebral palsy (2/699; 0.3%) across the two studies. Due to low event numbers, it is very uncertain whether dextrose gel alters the rate of cerebral palsy compared to placebo gel (RR 0.49, 95% CI 0.04 to 5.33; two studies, 1543 children; Analysis 1.22).
1.22. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 22: Cerebral palsy at two years of age
Developmental delay/intellectual impairment and severity at two years of age or greater
Meta‐analysis showed that oral dextrose gel may have little to no effect on the risk of developmental delay/intellectual impairment at two years of age compared to placebo gel (RR 1.07, 95% CI 0.86 to 1.32; two studies, 1546 children; Analysis 1.23). Data from one study (Harding 2021), showed that oral dextrose gel had little to no effect on developmental delay that was mild (RR 1.08, 95% CI 0.82 to 1.43; 1187 children; Analysis 1.24) or moderate‐to‐severe (RR 1.87, 95% CI 0.94 to 3.72; 1187 children; Analysis 1.25).
1.23. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 23: Developmental delay/intellectual impairment at two years of age
1.24. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 24: Developmental delay/intellectual impairment at two years of age ‐ mild (70 to 84)
1.25. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 25: Developmental delay/intellectual impairment at two years of age ‐ moderate or severe (< 70)
Data from one study (Hegarty 2016a) showed that, at six to seven years of age, oral dextrose gel may decrease the risk of motor impairment compared to placebo (RR 0.25, 95% CI 0.10 to 0.59; one study, 308 children; Analysis 1.26). The RD was ‐0.10 (95% CI ‐0.17 to ‐0.03) and, on average, 10 infants would have to receive prophylactic dextrose gel to prevent one case of motor impairment in mid‐childhood. Data from the same study suggest oral dextrose gel may have little to no effect on the risk of language impairment at six to seven years of age (RR 0.69, 95% CI 0.41 to 1.17; one study; 308 children; Analysis 1.26).
1.26. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 26: Developmental delay/intellectual impairment at six to seven years of age
Data from one study (Harding 2021), found no evidence that the effect of oral dextrose gel on developmental delay/intellectual impairment at two years of age was different amongst children of mothers with diabetes (RR 1.12, 95% CI 0.87 to 1.46; 900 children; Analysis 1.27), compared to children with other risk factors for neonatal hypoglycaemia (RR 1.07, 95% CI 0.65 to 1.75; one study; 294 children; Analysis 1.27) (subgroup effect P = 0.85, I² = 0%).
1.27. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 27: Developmental delay/intellectual impairment at two years of age ‐ by risk factor
Executive dysfunction and severity at two years of age or greater
Meta‐analysis showed that oral dextrose gel may have little to no effect on the risk of executive dysfunction at two years of age (RR 0.79 95% CI 0.54 to 1.16; two studies; 1544 children; Analysis 1.28) or six to seven years of age (RR 0.65, 95% CI 0.35 to 1.19; one study, 308 children; Analysis 1.29), compared to placebo gel. No data were available regarding the severity of executive dysfunction.
1.28. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 28: Executive dysfunction at two years of age
1.29. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 29: Executive dysfunction at six to seven years of age
Data from one study (Hegarty 2016a) showed that oral dextrose gel may reduce the risk of executive dysfunction at six to seven years of age amongst those given a single dose of gel (RR 0.41, 95% CI 0.20 to 0.84; 167 children; Analysis 1.30), but not amongst those given multiple doses (RR 2.34, 95% CI 0.54 to 10.26; one study; 141 children; Analysis 1.30), (subgroup effect P = 0.04, I² = 77.1%). Amongst those given a single dose, the RD was ‐0.15 (95% CI ‐0.27 to ‐0.02) and, on average, seven infants would have to receive a single dose of prophylactic dextrose gel to prevent one case of executive dysfunction in mid‐childhood.
1.30. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 30: Executive dysfunction at six to seven years of age ‐ by single or multiple gel dose
Data from one study (Harding 2021), found no evidence that the effect of oral dextrose gel on executive dysfunction at two years of age was different amongst children of mothers with diabetes (RR 0.80, 95% CI 0.47 to 1.35; 895 children; Analysis 1.31), compared to children with other risk factors for neonatal hypoglycaemia (RR 1.67, 95% CI 0.62 to 4.47; 292 children; Analysis 1.31), (subgroup effect P = 0.20, I² = 39.7%). Data from one study (Hegarty 2016a) also found no evidence that the effect of oral dextrose gel on executive dysfunction at six to seven years of age was different amongst children of mothers with diabetes (RR 0.74, 95% CI 0.38 to 1.45; 219 children; Analysis 1.32), compared to children with other risk factors for neonatal hypoglycaemia (RR 0.28, 95% CI 0.05 to 1.45; 89 children; Analysis 1.32) (subgroup effect P = 0.28, I² = 14.1%).
1.31. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 31: Executive dysfunction at two years of age ‐ by risk factor
1.32. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 32: Executive dysfunction at six to seven years of age ‐ by risk factor
Behavioural problems and severity at two years of age or greater
Data from one study (Hegarty 2016a) showed that oral dextrose gel may have little to no effect on the risk of emotional‐behavioural difficulty at six to seven years compared to placebo gel (RR 0.62, 95% CI 0.33 to 1.18; 228 children; Analysis 1.33). No data were available regarding the severity of emotional‐behavioural difficulty.
1.33. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 33: Emotional‐behavioural difficulty at six to seven years of age
The same study found no evidence that the effect of oral dextrose gel on emotional‐behavioural difficulty at six to seven years of age was different amongst children of mothers with diabetes (RR 0.55, 95% CI 0.26 to 1.14; 160 children; Analysis 1.34), compared to children with other risk factors for neonatal hypoglycaemia (RR 0.85, 95% CI 0.22 to 3.25; one study; 68 children; Analysis 1.34), (subgroup effect P = 0.57, I ² = 0%).
1.34. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 34: Emotional‐behavioural difficulty at six to seven years of age ‐ by risk factor
The same study also found no evidence that the effect of oral dextrose gel on emotional‐behavioural difficulty at six to seven years of age was different amongst children who received a single dose of gel (RR 0.42, 95% CI 0.18 to 1.01; 121 children; Analysis 1.35), compared to those who received multiple doses (RR 1.02, 95% CI 0.35 to 2.96; 107 participants; Analysis 1.35), (subgroup effect P = 0.21, I² = 36.9%).
1.35. Analysis.

Comparison 1: Dextrose gel versus control, Outcome 35: Emotional‐behavioural difficulty at six to seven years of age ‐ by single or multiple gel dose
Abnormal MRI of the brain at two years of age or greater
No data were available for this outcome.
Costs associated with the intervention ‐ investigator‐defined
No data were available for this outcome.
Discussion
Summary of main results
This updated review included two studies that evaluated oral dextrose gel compared with placebo gel for preventing neonatal hypoglycaemia in 2548 at‐risk infants (Harding 2021; Hegarty 2016a).
High‐certainty evidence from the two studies showed that oral dextrose gel reduces the risk of neonatal hypoglycaemia. On average, 17 at‐risk infants would need to be treated with oral dextrose gel to prevent one additional case of neonatal hypoglycaemia (95% CI 10 to 50). There was low‐certainty evidence from two studies including 1554 infants that oral dextrose gel compared with placebo gel may not reduce the risk of major neurological disability at two years of age or older, and moderate‐certainty evidence from one study including 308 infants that oral dextrose gel compared with placebo gel probably does not alter this outcome at six to seven years of age (see Table 1).
Oral dextrose gel probably reduces the risk of receipt of treatment for hypoglycaemia during the initial hospital stay (NNTB 33) but makes little or no difference to intravenous or oral dextrose gel treatment during the initial hospital stay, may have little or no effect on separation of the mother from the infant for treatment of hypoglycaemia, and probably does not result in increased adverse events compared with placebo gel. Oral dextrose gel probably also has little or no effect on the number of hypoglycaemic episodes during the initial hospital stay, neonatal seizures, whether an infant is breastfed after discharge, or the duration of initial hospital stay.
While oral dextrose gel probably has little or no effect on developmental delay/intellectual impairment at two years of age, evidence from one study suggests it may reduce the risk of motor impairment (NNTB 10), but not language impairment, at six to seven years of age. Subgroup analysis suggests that oral dextrose gel may also reduce the risk of executive dysfunction at six to seven years of age when given as a single dose (NNTB 7), but not when given as multiple doses. Oral dextrose gel probably has little to no effect on visual impairment, hearing impairment, cerebral palsy, or behavioural problems, all at two years of age or greater.
Overall completeness and applicability of evidence
Since the previous version of this review, more data have become available on neurodevelopmental outcomes at two years of age from one large study (Harding 2021), and new data at six to seven years of age from one small study (Hegarty 2016a). No data were available for the following prespecified secondary outcomes: abnormal MRI of the brain in the neonatal period and at two years of age or greater; exclusive breastfeeding after discharge or at six months of age; and costs associated with the intervention. Both included studies compared a single preparation of oral dextrose gel with placebo in late preterm and term infants in two high‐income countries in the same geographical region with likely similar practices (Australia and New Zealand). Therefore, the applicability of these findings to other preparations of gel, extremely and moderately preterm infants and other healthcare settings remains unknown. There were no randomised trials that compared oral dextrose gel with no treatment, standard care or other therapies (such as antenatal expression of colostrum, early initiation of breastfeeding and the supplementation of breastfeeding with formula milk).
Quality of the evidence
We assessed both included studies as having low risk of bias across all but one domain, with one study having unclear risk of bias due to baseline imbalances at follow‐up. The certainty of evidence assessed by GRADE was moderate for most outcomes, except for the co‐primary outcomes of hypoglycaemia, which was graded as high certainty, and co‐primary outcome of major neurological disability at two years of age or older and secondary outcome of separation of mother and infant, which were graded as low certainty (see Table 1). The most common reason for downgrading the evidence was imprecision due to wide confidence intervals and low event rates.
For the co‐primary outcome of major neurological disability at two years of age or older, data were available from two studies with the effect estimates in opposite directions, resulting in substantial unexplained heterogeneity and wide confidence intervals including the possibility of important benefit or harm, so we graded the certainty of this evidence as low. Additional studies are needed to clarify this finding.
We downgraded one secondary outcome (separation from the mother for treatment of hypoglycaemia) to low certainty because of imprecision and substantial unexplained heterogeneity. We were unable to further explore this with planned subgroup analyses because there were only two studies. However, it is possible that this heterogeneity may be due to variations between hospitals in policies for admission to the NICU.
We downgraded the outcome of adverse events to moderate certainty because of imprecision due to low event rates. Thus, there is moderate‐certainty evidence that dextrose gel does not increase the risk of an infant choking or vomiting during administration compared to those who received placebo gel, and that the risk is low (< 1% in both groups), but there is no evidence about whether receipt of oral dextrose gel may increase the risk of these events or other harms compared with no treatment or other therapies such as formula feeding.
We downgraded the outcome of receipt of treatment for hypoglycaemia during the initial hospital stay due to imprecision since the confidence interval included one. We downgraded the outcome of receipt of intravenous treatment for hypoglycaemia to moderate certainty due to low event rates and wide confidence intervals.
Potential biases in the review process
We believe that we have made every effort to minimise bias in the review process. We conducted a systematic search of the literature for randomised controlled trial evidence, not restricted by language or date of publication. When necessary, we contacted authors of primary studies to obtain additional outcome data. We adhered to the Cochrane methods of searching and performing data extraction and analysis. While three authors of the included studies co‐authored this review (JA, TE, JH), we minimised potential bias by involving them in the write‐up of this review but not in data extraction, bias assessment, or assessment of certainty in the findings, which were undertaken by two independent review authors not involved in the included studies (LR, LL).
Agreements and disagreements with other studies or reviews
This update includes the same two studies and agrees with the first (Hegarty 2017) and second versions of this review (Edwards 2021), which reported that prophylactic oral dextrose gel compared with placebo reduced the risk of neonatal hypoglycaemia in at‐risk infants and probably reduced the risk of receipt of treatment for hypoglycaemia during the initial hospital stay. Similar to the findings of previous versions of this review, there was no evidence of adverse events. However, the previous version of this review reported a reduction in the risk of major neurological disability at two years of age after oral dextrose gel when compared with placebo gel, based on data from a single small study (Hegarty 2016a). This review includes additional follow‐up data from the second larger study (Harding 2021), that have changed these findings to no reduction in the risk of major neurological disability at two years, but with confidence intervals including the possibility of important benefit or harm. Additional evidence from Hegarty 2016a also suggests dextrose gel probably does not alter this outcome at six to seven years.
The Cochrane Review, “Oral dextrose gel for the treatment of hypoglycaemia in newborn infants", (Edwards 2022), reported that treatment of hypoglycaemia with oral dextrose gel was associated with a reduction in separation of the mother and infant and increased likelihood of full breastfeeding after discharge. Edwards 2022 also found no evidence of adverse events of dextrose gel during the neonatal period or at two years' corrected age.
Authors' conclusions
Implications for practice.
The available evidence suggests that giving prophylactic oral dextrose gel to 100 at‐risk late preterm and term infants will prevent approximately six cases of neonatal hypoglycaemia and three babies being treated for neonatal hypoglycaemia, without increasing the risk of adverse events or altering separation from the mother or breastfeeding outcomes. Prophylactic oral dextrose gel compared to placebo probably makes little to no difference to the risk of major neurological disability at two years, but the confidence intervals include the possibility of substantial benefit or harm. Evidence at six to seven years of age is limited to a single small study.
A cost‐utility analysis (not reported in this review) has reported that prophylactic oral dextrose gel is likely to be cost‐effective, reducing healthcare costs while improving quality of life (Glasgow 2018).
In view of its limited short‐term benefits, prophylactic oral dextrose gel should not be incorporated into routine practice until additional information is available about the balance of possible risks and harms for later neurological disability.
Implications for research.
Further data are required from large randomised trials about the effects of prophylactic oral dextrose gel on later neurodevelopmental outcomes. An update of this review when data become available from an ongoing follow‐up study of one of the included studies will help clarify the certainty of this evidence. Additional data are also required on the effects of prophylactic dextrose gel on exclusive or any breastfeeding after discharge, and if the effects on the separation of mother from infant differ in hospitals with different NICU admission policies.
There is no evidence about the effects of prophylactic oral dextrose gel in other high‐income countries, in low‐ and middle‐income countries or on extremely and moderately preterm infants and using other dextrose gel preparations. However, the results of three studies awaiting classification set in India (CTRI/2017/11/010645), Thailand (TCTR20190805003), and Italy (NCT04185766), and an ongoing study in very preterm infants (NCT04353713), may help to address these knowledge gaps. Future research should also compare prophylactic oral dextrose gel with other active therapies and assess adverse events compared with no treatment.
What's new
| Date | Event | Description |
|---|---|---|
| 28 November 2023 | New citation required and conclusions have changed | There has been a change in authorship. Outcomes at two years of age include the possibility of substantial benefit or harm. |
| 28 November 2023 | New search has been performed | An updated search was conducted with a new search strategy in April 2023. Additional follow‐up data were available for the two studies included in the previous review. There are a further three studies ongoing and one study awaiting classification. These studies were all identified in the earlier review. |
History
Protocol first published: Issue 4, 2016 Review first published: Issue 7, 2017
| Date | Event | Description |
|---|---|---|
| 19 October 2020 | New citation required but conclusions have not changed | There has been a change in authorship. One trial reported on long‐term neurodevelopmental and disability outcomes at two years of age or greater. |
| 19 October 2020 | New search has been performed | The literature was searched in October 2020 using a new search strategy which we ran without date limits. One new published study, one ongoing study and three studies awaiting classification were identified. |
Acknowledgements
We acknowledge the contributions of Julie Brown, Joanne Hegarty, and Caroline Crowther, who were co‐authors of the protocol and earlier versions of this Cochrane Review (Hegarty 2016b; Hegarty 2017; Edwards 2021).
The methods section of this review is based on a standard template used by Cochrane Neonatal. The database and trials searches were designed and run by Lily Roberts and Luling Lin.
We would like to thank Cochrane Neonatal: Jane Cracknell and Michelle Fiander, Managing Editors; and Roger Soll and Bill McGuire, Co‐coordinating Editors, who provided editorial and administrative support.
We are grateful to the following peer reviewers for their time and comments: Daniela Dinu Associate Professor Baylor College of Medicine, Houston, Texas, USA and Nai Ming Lai, School of Medicine, Taylor's University, Malaysia.
We thank Anne Lethaby for copy editing.
Appendices
Appendix 1. 26th April 2023 search methods
The RCT filters have been created using Cochrane's highly sensitive search strategies for identifying randomised trials (Higgins 2022). The neonatal filters were created and tested by the Cochrane Neonatal Information Specialist.
CENTRAL via CRS Web:
| Term category | Term no. | Term | Results |
| Neonatal population [LR1] | #1 | MeSH descriptor: [Infant, Newborn] explode all trees | 20,484 |
| #2 | MeSH descriptor: [Intensive Care, Neonatal] this term only | 375 | |
| #3 | MeSH descriptor: [Intensive Care Units, Neonatal] this term only | 1025 | |
| #4 | MeSH descriptor: [Gestational Age] this term only | 3956 | |
| #5 | ("babe" or "babes" or baby* or "babies" or "gestational age" or "gestational ages" or infant? or "infantile" or infancy or "low birth weight" OR "low birth weights" or "low birthweight" or "low birthweights" or neonat* or "neo‐nat*" or newborn* or "new born?" or "newly born" or "premature" or "pre‐mature" or "pre‐matures" or prematures or prematurity or "pre‐maturity" or "preterm" or "preterms" or "pre term?" or "preemie" or "preemies" or "premies" or "premie" or "VLBW" or "VLBWI" or "VLBW‐I" or "VLBWs" or "LBW" or "LBWI" or "LBWs" or "ELBW" or "ELBWI" or "ELBWs" or "NICU" or "NICUs"):ti,ab,kw | 108,579 | |
| #6 | #1 OR #2 OR #3 OR #4 OR #5 | 110,331 | |
| Hypoglycaemia | #7 | MeSH descriptor: [Hypoglycemia] explode all trees | 4072 |
| #8 | hypogly*:ti,ab,kw | 22,141 | |
| #9 | #7 OR #8 | 22,144 | |
| Dextrose gel | #10 | MeSH descriptor: [Glucose] explode all trees | 22,064 |
| #11 | MeSH descriptor: [Sweetening Agents] explode all trees | 859 | |
| #12 | dextrose* or glucose* or sweetening agent*:ti,ab,kw | 80,233 | |
| #13 | (“corn sugar*” or “grape sugar*” or “starch sugar*”):ti,ab,kw | 15 | |
| #14 | #10 OR #11 OR #12 OR #13 | 80,453 | |
| #15 | MeSH descriptor: [Gels] explode all trees | 2998 | |
| #16 | gel or gels:ti,ab,kw | 17,797 | |
| #17 | #15 OR #16 | 18,135 | |
| #18 | #6 AND #9 AND #14 AND #17 | 69 |
MEDLINE via Ovid:
| Term category | Term no. | Term | Results |
| Neonatal population | #1 | exp infant, newborn/ or Intensive Care, Neonatal/ or Intensive Care Units, Neonatal/ or Gestational Age/ | 719,935 |
| #2 | (babe or babes or baby* or babies or gestational age? or infant? or infantile or infancy or low birth weight or low birthweight or neonat* or neo‐nat* or newborn* or new born? or newly born or premature or pre‐mature or pre‐matures or prematures or prematurity or pre‐maturity or preterm or preterms or pre term? or preemie or preemies or premies or premie or VLBW or VLBWI or VLBW‐I or VLBWs or LBW or LBWI or LBWs or ELBW or ELBWI or ELBWs or NICU or NICUs).ti,ab,kw,kf. | 1,036,143 | |
| #3 | #1 OR #2 | 1,347,076 | |
| Hypoglycaemia | #4 | exp Hypoglycemia | 31,355 |
| #5 | hypogly*.mp | 131,108 | |
| #6 | #4 OR #5 | 131,746 | |
| Dextrose gel | #7 | exp Glucose/ | 336,179 |
| #8 | exp Sweetening Agents/ | 255,200 | |
| #9 | (dextrose* or glucose* or sweetening agent*).ti,ab,kw,kf. | 563,629 | |
| #10 | (corn or grape or starch adj2 (sugar*)).ti,ab,kw,kf. | 1867 | |
| #11 | #7 OR #8 OR #9 OR #10 | 734,767 | |
| #12 | exp Gels/ | 66,417 | |
| #13 | (gel or gels).mp. | 495,300 | |
| #14 | #12 OR #13 | 521,597 | |
| RCT filter | #15 | Randomi*ed controlled trial.pt. | 591,543 |
| #16 | controlled clinical trial.pt. | 95,283 | |
| #17 | Randomi*ed.ti,ab,kw. | 777,011 | |
| #18 | placebo.ti,ab.kw. | 244,308 | |
| #19 | drug therapy.fs. | 2,584,521 | |
| #20 | randomly.ti,ab,kw. | 407,785 | |
| #21 | trial.ti,ab,kw. | 748,385 | |
| #22 | groups.ti,ab,kw. | 2,535,557 | |
| #23 | #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 | 5,728,115 | |
| #24 | (quasirandom* or quasi‐random* or random*).ti,ab,kw,kf. | 1,414,655 | |
| #25 | (control* adj2 (group? or trial? or study)).ti,ab,kw,kf. | 1,078,425 | |
| #26 | #24 OR #25 | 2,005,428 | |
| #27 | exp animals/ not humans/ | 5,115,959 | |
| #28 | #23 OR #26 | 6,245,661 | |
| #29 | #3 AND #6 AND #11 AND #14 AND #28 NOT #27 | 52 |
Embase via Ovid:
| Term category | Term no. | Term | Results |
| Neonatal population | #1 | newborn/ or prematurity/ or newborn intensive care/ or newborn care/ or gestational age/ | 418,859 |
| #2 | (babe or babes or baby* or babies or gestational age? or infant? or infantile or infancy or low birth weight or low birthweight or neonat* or neo‐nat* or newborn* or new born? or newly born or premature or pre‐mature or pre‐matures or prematures or prematurity or pre‐maturity or preterm or preterms or pre term? or preemie or preemies or premies or premie or VLBW or VLBWI or VLBW‐I or VLBWs or LBW or LBWI or LBWs or ELBW or ELBWI or ELBWs or NICU or NICUs).ti,ab,kw,kf. | 701,410 | |
| #3 | #1 OR #2 | 828,422 | |
| Hypoglycaemia | #4 | Hypoglycaemia/ | 45,464 |
| #5 | hypogly*.mp | 70,887 | |
| #6 | #4 OR #5 | 70,887 | |
| Dextrose gel | #7 | Glucose/ | 235,185 |
| #8 | Sweetening Agent/ | 2904 | |
| #9 | (dextrose* or glucose* or sweetening agent*).ti,ab,kw,kf. | 410,882 | |
| #10 | (corn or grape or starch adj2 (sugar*)).ti,ab,kw,kf. | 709 | |
| #11 | #7 OR #8 OR #9 OR #10 | 450,723 | |
| #12 | Gel/ | 14,462 | |
| #13 | (gel or gels).mp. | 292,452 | |
| #14 | #12 OR #13 | 292,452 | |
| RCT filter | #15 | Randomized controlled trial/ or Controlled clinical study/ | 552,534 |
| #16 | random*.ti,ab,kw. | 1,051,081 | |
| #17 | Randomization/ | 66,145 | |
| #18 | placebo.ti,ab,kw. | 225,637 | |
| #19 | ((double or single or doubly or singly) adj (blind or blinded or blindly)).ti,ab,kw. | 169,331 | |
| #20 | double blind procedure/ | 117,766 | |
| #21 | (controlled adj7 (study or design or trial)).ti,ab,kw. | 237,908 | |
| #22 | parallel group$1.ti,ab. | 17,728 | |
| #23 | ((assign$ or match or matched or allocation) adj5 (alternate or group$1 or intervention$1 or patient$1 or subject$1 or participant$1)).ti,ab. | 235,732 | |
| #24 | (open adj label).ti,ab. | 69,187 | |
| #25 | (quasirandom* or quasi‐random* or random*).ti,ab,kw,kf. | 1,051,533 | |
| #26 | (control* adj2 group?).ti,ab,kw,kf. | 464,523 | |
| #27 | #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 | 1,816,633 | |
| #32 | #3 AND #6 AND #11 AND #14 AND #27 | 26 |
Epistemonikos:
| Term category | Term no. | Term | Results |
| #1 | (title:((title:(hypoglycaemia AND dextrose AND randomised) OR abstract:(hypoglycaemia AND dextrose AND randomised))) OR abstract:((title:(hypoglycaemia AND dextrose AND randomised) OR abstract:(hypoglycaemia AND dextrose AND randomised)))) | 21 |
ISRCTN:
| Search no. | Term | Results |
| #1 | Interventions: dextrose Participant age range: Neonate |
2 |
| #2 | Interventions: glucose Participant age range: Neonate |
18 |
| #3 | Interventions: sweetening agent Participant age range: Neonate |
0 |
| #4 | Text search: dextrose Participant age range: Neonate |
2 |
| #5 | Text search: glucose Participant age range: Neonate |
31 |
| #6 | Text search: sweetening agent Participant age range: Neonate |
0 |
| #7 | Condition: hypoglycaemia Interventions: dextrose |
1 |
| #8 | Condition: hypoglycemia Interventions: dextrose |
0 |
| #9 | Condition: hypoglycaemia Interventions: glucose |
4 |
| #10 | Condition: hypoglycemia Interventions: glucose |
1 |
| 59 in total 36 imported to Covidence after removing duplicates |
ANZCTR:
| Search no. | Term | Results |
| #1 | Health condition or problem studied: hypoglycaemia Description of intervention/exposure: dextrose Allocation to intervention: randomised Age group: Child |
4 |
| #2 | Health condition or problem studied: hypoglycaemia Description of intervention/exposure: glucose Allocation to intervention: randomised Age group: Child |
4 |
| #3 | Health condition or problem studied: hypoglycaemia Description of intervention/exposure: sweetening agent Allocation to intervention: randomised Age group: Child |
0 |
| 8 in total 7 imported to Covidence after removing duplicates |
ICTRP:
| Term no. | Term | Results |
| #1 | hypoglycaemia OR dextrose OR hypoglycemia OR glucose [in the Title] | 30 |
| #2 | hypoglycaemia OR hypoglycemia [in the Condition with synonyms] | |
| #3 | dextrose* OR glucose* OR "sweetening agent" [in the Intervention with synonyms] | |
| #4 | Search for clinical trials in children | |
| #5 | Recruitment status is ALL |
ClinicalTrials.gov:
| Term category | Term no. | Term | Results |
| Condition or disease | #1 | Hypoglycaemia [and synonyms Hypoglycaemic syndrome, Low blood sugar] | 126 |
| Other terms | #2 | Dextrose [and synonyms Glucose, D Glucose, Dex4, Dextrosa, Glucosa] | |
| Age | #3 | Child (birth‐17) | |
| Study type | #4 | Interventional (Clinical Trial) |
Appendix 2. Previous search methods
Review authors conducted a comprehensive search that included the Cochrane Central Register of Controlled Trials (CENTRAL 2020, Issue 10) in the Cochrane Library; and Ovid MEDLINE(R) and Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Daily and Versions(R) on 19 October 2020 and did not apply language restrictions.
The following search strategy was used:
CENTRAL: (((MESH DESCRIPTOR Hypoglycemia EXPLODE ALL AND CENTRAL:TARGET) OR (hypogly* AND CENTRAL:TARGET)) AND ((MESH DESCRIPTOR Glucose EXPLODE ALL AND CENTRAL:TARGET) OR (MESH DESCRIPTOR Sweetening Agents EXPLODE ALL AND CENTRAL:TARGET) OR (dextrose* or glucose* or sweetening agent* AND CENTRAL:TARGET)) AND ((MESH DESCRIPTOR Gels EXPLODE ALL AND CENTRAL:TARGET) OR (gel or gels AND CENTRAL:TARGET) AND ((MESH DESCRIPTOR Infant, Newborn EXPLODE ALL AND CENTRAL:TARGET) OR (infant or infants or infant's or "infant s" or infantile or infancy or newborn* or "new born" or "new borns" or "newly born" or neonat* or baby* or babies or premature or prematures or prematurity or preterm or preterms or "pre term" or premies or "low birth weight" or "low birthweight" or VLBW or LBW or ELBW or NICU AND CENTRAL:TARGET))
MEDLINE: ((exp Hypoglycemia/ OR hypogly*.mp.) AND ((exp Glucose/) OR (exp Sweetening Agents/) OR (dextrose* or glucose* or sweetening agent*.mp.)) AND ((exp Gels/) OR ((gel or gels).mp.) AND ((exp infant, newborn/) OR ((newborn* or new born or new borns or newly born or baby* or babies or premature or prematurity or preterm or pre term or low birth weight or low birthweight or VLBW or LBW or infant or infants or 'infant s' or infant's or infantile or infancy or neonat*).ti,ab.)) AND ((randomized controlled trial.pt.) OR (controlled clinical trial.pt.) OR (randomized.ab.) OR (placebo.ab.) OR (drug therapy.fs.) OR (randomly.ab.) OR (trial.ab.) OR (groups.ab.)) NOT exp animals/ not humans.sh. AND ((randomi?ed.ti,ab.) OR (randomly.ti,ab.) OR (trial.ti,ab.) OR (groups.ti,ab.) OR (((single or doubl* or tripl* or treb*) and (blind* or mask*)).ti,ab.) OR (placebo*.ti,ab.) AND (limit 33 to yr="2018 ‐Current")
They searched clinical trial registries for ongoing or recently completed trials. These included the World Health Organization’s International Clinical Trials Registry Platform (ICTRP) (www.who.int/ictrp/search/en/) and the US National Library of Medicine’s ClinicalTrials.gov (clinicaltrials.gov) via Cochrane CENTRAL. They also searched the ISRCTN Registry (www.isrctn.com) and the ANZCTR Registry (www.anzctr.org.au) for any unique trials not found through the Cochrane CENTRAL search.
Appendix 3. Risk of Bias tool
Sequence generation (checking for possible selection bias). Was the allocation sequence adequately generated?
For each included study, we categorised the method used to generate the allocation sequence as:
low risk (any truly random process e.g. random number table; computer random number generator);
high risk (any non‐random process e.g. odd or even date of birth; hospital or clinic record number); or
unclear risk.
Allocation concealment (checking for possible selection bias). Was allocation adequately concealed?
For each included study, we categorised the method used to conceal the allocation sequence as:
low risk (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
high risk (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth); or
unclear risk.
Blinding of participants and personnel (checking for possible performance bias). Was knowledge of the allocated intervention adequately prevented during the study?
For each included study, we categorised the methods used to blind study participants and personnel from knowledge of which intervention a participant received. Blinding was assessed separately for different outcomes or class of outcomes. We categorised the methods as:
low risk, high risk or unclear risk for participants; and
low risk, high risk or unclear risk for personnel.
Blinding of outcome assessment (checking for possible detection bias)
For each included study, we categorised the methods used to blind outcome assessment. Blinding was assessed separately for different outcomes or class of outcomes. We categorised the methods as:
low risk for outcome assessors;
high risk for outcome assessors; or
unclear risk for outcome assessors.
Incomplete outcome data (checking for possible attrition bias through withdrawals, dropouts, protocol deviations). Were incomplete outcome data adequately addressed
For each included study and for each outcome, we described the completeness of data including attrition and exclusions from the analysis. We noted whether attrition and exclusions were reported, the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported or supplied by the trial authors, we re‐included missing data in the analyses. We categorised the methods as:
low risk (< 20% missing data);
high risk (≥ 20% missing data); or
unclear risk.
Selective reporting bias. Are reports of the study free of suggestion of selective outcome reporting?
For each included study, we described how we investigated the possibility of selective outcome reporting bias and what we found. For studies in which study protocols were published in advance, we compared prespecified outcomes versus outcomes eventually reported in the published results. If the study protocol was not published in advance, we contacted study authors to gain access to the study protocol. We assessed the methods as:
low risk (where it is clear that all of the study's prespecified outcomes and all expected outcomes of interest to the review have been reported);
high risk (where not all the study's prespecified outcomes have been reported; one or more reported primary outcomes were not prespecified outcomes of interest and are reported incompletely and so cannot be used; study fails to include results of a key outcome that would have been expected to have been reported); or
unclear risk.
Other sources of bias. Was the study apparently free of other problems that could put it at a high risk of bias?
For each included study, we described any important concerns we had about other possible sources of bias (for example, whether there was a potential source of bias related to the specific study design or whether the trial was stopped early due to some data‐dependent process). We assessed whether each study was free of other problems that could put it at risk of bias as:
low risk;
high risk; or
unclear risk.
If needed, we explored the impact of the level of bias through undertaking sensitivity analyses.
Data and analyses
Comparison 1. Dextrose gel versus control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Hypoglycaemia | 2 | 2548 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.79, 0.95] |
| 1.2 Major neurological disability at two years of age | 2 | 1554 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.59, 1.68] |
| 1.2.1 Major neurological disability at two years of age | 2 | 1554 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.59, 1.68] |
| 1.3 Major neurological disability at six to seven years of age | 1 | 308 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.49, 1.06] |
| 1.4 Major neurological disability at two years of age ‐ by risk factor | 1 | 1194 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.45 [0.78, 2.71] |
| 1.4.1 Child of mother with diabetes | 1 | 900 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.54, 2.23] |
| 1.4.2 Other risk factor | 1 | 294 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.95 [0.85, 18.27] |
| 1.5 Receipt of treatment for hypoglycaemia during initial hospital stay | 2 | 2548 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.79, 1.00] |
| 1.6 Separation from mother for treatment of hypoglycaemia (admission to NICU for hypoglycaemia) | 2 | 2548 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.81, 1.55] |
| 1.7 Receipt of intravenous treatment for hypoglycaemia | 2 | 2548 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.68, 1.49] |
| 1.8 Adverse effects (e.g. choking or vomiting at time of administration) | 2 | 2510 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.64, 2.33] |
| 1.9 Developmental disability at two years of age | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.9.1 Developmental disability at two years of age | 2 | 1553 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.84, 1.26] |
| 1.10 Developmental disability at six to seven years of age | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.10.1 Developmental disability at six to seven years of age | 1 | 308 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.68, 1.07] |
| 1.11 Any neurological disability at two years of age ‐ by risk factor | 1 | 1194 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.88, 1.40] |
| 1.11.1 Child of mother with diabetes | 1 | 900 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.87, 1.46] |
| 1.11.2 Other risk factor | 1 | 294 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.65, 1.75] |
| 1.12 Any neurological disability at six to seven years of age ‐ by risk factor | 1 | 308 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.68, 1.05] |
| 1.12.1 Child of mother with diabetes | 1 | 219 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.63, 1.02] |
| 1.12.2 Other risk factor | 1 | 89 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.59, 1.68] |
| 1.13 Any neurological disability at six to seven years of age ‐ by single or multiple gel dose | 1 | 308 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.68, 1.07] |
| 1.13.1 Single dose | 1 | 167 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.61, 1.10] |
| 1.13.2 Multiple dose | 1 | 141 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.64, 1.27] |
| 1.14 Receipt of oral dextrose gel treatment for hypoglycaemia | 2 | 2548 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.79, 1.01] |
| 1.15 Receipt of any medications for hypoglycaemia such as glucagon or corticosteroids | 2 | 2548 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 1.16 Number of episodes of hypoglycaemia (glucose oxidase method) (total number per infant) | 1 | 186 | Mean Difference (IV, Fixed, 95% CI) | ‐0.18 [‐0.55, 0.19] |
| 1.17 Neonatal seizures | 2 | 2548 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.08, 5.69] |
| 1.18 Duration of initial hospital stay (days) | 2 | 2537 | Mean Difference (IV, Fixed, 95% CI) | 0.06 [‐0.13, 0.24] |
| 1.19 Breastfeeding (any) after discharge | 2 | 2323 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.98, 1.05] |
| 1.19.1 Breastfeeding (full or exclusive) after discharge | 2 | 2323 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.98, 1.05] |
| 1.20 Visual impairment at two years of age | 2 | 1551 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.01, 4.03] |
| 1.21 Hearing impairment at two years of age | 2 | 1551 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.05, 2.05] |
| 1.22 Cerebral palsy at two years of age | 2 | 1543 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.04, 5.33] |
| 1.23 Developmental delay/intellectual impairment at two years of age | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.23.1 Developmental delay/intellectual impairment at two years of age | 2 | 1546 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.86, 1.32] |
| 1.24 Developmental delay/intellectual impairment at two years of age ‐ mild (70 to 84) | 1 | 1187 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.82, 1.43] |
| 1.25 Developmental delay/intellectual impairment at two years of age ‐ moderate or severe (< 70) | 1 | 1187 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.87 [0.94, 3.72] |
| 1.26 Developmental delay/intellectual impairment at six to seven years of age | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.26.1 Developmental delay/intellectual impairment at six to seven years of age ‐ motor impairment | 1 | 308 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.10, 0.59] |
| 1.26.2 Developmental delay/intellectual impairment at six to seven years of age ‐ language impairment | 1 | 308 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.41, 1.17] |
| 1.27 Developmental delay/intellectual impairment at two years of age ‐ by risk factor | 1 | 1194 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.88, 1.40] |
| 1.27.1 Child of mother with diabetes | 1 | 900 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.87, 1.46] |
| 1.27.2 Other risk factor | 1 | 294 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.65, 1.75] |
| 1.28 Executive dysfunction at two years of age | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.28.1 Executive dysfunction at two years of age | 2 | 1544 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.54, 1.16] |
| 1.29 Executive dysfunction at six to seven years of age | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.29.1 Executive dysfunction at six to seven years of age | 1 | 308 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.35, 1.19] |
| 1.30 Executive dysfunction at six to seven years of age ‐ by single or multiple gel dose | 1 | 308 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.36, 1.21] |
| 1.30.1 Single dose | 1 | 167 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.20, 0.84] |
| 1.30.2 Multiple dose | 1 | 141 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.34 [0.54, 10.26] |
| 1.31 Executive dysfunction at two years of age ‐ by risk factor | 1 | 1187 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.60, 1.50] |
| 1.31.1 Child of mother with diabetes ‐ at two years of age | 1 | 895 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.47, 1.35] |
| 1.31.2 Other risk factor ‐ at two years of age | 1 | 292 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.67 [0.62, 4.47] |
| 1.32 Executive dysfunction at six to seven years of age ‐ by risk factor | 1 | 308 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.35, 1.16] |
| 1.32.1 Child of mother with diabetes ‐ at six to seven years of age | 1 | 219 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.38, 1.45] |
| 1.32.2 Other risk factor ‐ at six to seven years of age | 1 | 89 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.28 [0.05, 1.45] |
| 1.33 Emotional‐behavioural difficulty at six to seven years of age | 1 | 228 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.33, 1.18] |
| 1.34 Emotional‐behavioural difficulty at six to seven years of age ‐ by risk factor | 1 | 228 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.32, 1.17] |
| 1.34.1 Child of mother with diabetes | 1 | 160 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.26, 1.14] |
| 1.34.2 Other risk factor | 1 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.22, 3.25] |
| 1.35 Emotional‐behavioural difficulty at six to seven years of age ‐ by single or multiple gel dose | 1 | 228 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.32, 1.19] |
| 1.35.1 Single dose | 1 | 121 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.18, 1.01] |
| 1.35.2 Multiple dose | 1 | 107 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.35, 2.96] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Harding 2021.
| Study characteristics | ||
| Methods | Randomised parallel controlled trial | |
| Participants | 2149 infants were randomised (16 infants randomised in error). Of 1321 children eligible for follow‐up at two years' corrected age (774 randomised in Australia, 16 randomised in error, 3 died, 35 declined), 1197 (91%) were assessed (68 overseas, 49 declined, 7 lost to follow‐up). Inclusion criteria: infants born to a mother with diabetes, late preterm (35 to 36 weeks' gestation) or small (< 2.5 kg or < 10th percentile) or large birthweight (> 4.5 kg or > 90th percentile); < 1 hour old; no indication for NICU admission; unlikely to require NICU admission for other reasons; mother intended to breastfeed. Exclusion criteria: major congenital abnormality; previous formula feeding or intravenous fluids; previous diagnosis of hypoglycaemia; admitted to NICU; imminent admission to NICU Setting: multi‐centre Timing: Recruitment: January 2015 to May 2019 Follow‐up: January 2017 to July 2021 |
|
| Interventions | 40% dextrose gel massaged into buccal mucosa as a single dose (0.5 mL/kg) 1 hour after birth (n = 1070) vs Placebo gel massaged into buccal mucosa using the same protocol as the intervention (n = 1063) For both groups, gel administration was followed by a breast feed. Blood glucose concentration was measured at 2 hours after birth and then according to standard hospital practice. Babies who became hypoglycaemic were treated according to standard hospital practice. |
|
| Outcomes |
Primary outcomes • Hypoglycaemia (any blood glucose concentration < 2.6 mmol/L in first 48 hours) ‐ significantly lower incidence in oral dextrose gel group • Neurosensory impairment at ≥ 2 years (includes blindness, deafness, cerebral palsy, developmental delay (Bayley‐III cognitive, language, or motor composite score < 85), or performance‐based executive function total score more than 1.5 SD below the cohort mean) ‐ no significant difference between oral dextrose and placebo groups Secondary outcomes • Receipt of treatment (any including intravenous, oral dextrose gel, medications) for hypoglycaemia during initial hospital stay (yes/no) ‐ no significant difference between oral dextrose and placebo groups • Admission to NICU (defined as admission to NICU (or special care baby unit (SCBU) for hospitals using that name) for > 4 hours) ‐ no significant difference between oral dextrose and placebo groups • Admission to NICU for hypoglycaemia ‐ no significant difference between oral dextrose and placebo groups • Hyperglycaemia (any blood glucose concentration > 10 mmol/L) ‐ no cases • Breastfeeding at discharge from hospital (full or exclusive) ‐ no significant difference between oral dextrose and placebo groups • Receipt of any formula before discharge from hospital ‐ no significant difference between oral dextrose and placebo groups • Formula feeding at 6 weeks of age ‐ no significant difference between oral dextrose and placebo groups • Developmental delay at ≥ 2 years ‐ no significant difference between oral dextrose and placebo groups except in moderate or severe (< 70) cognitive delay and motor delay which were significantly higher in the oral dextrose gel group • Hearing impairment at ≥ 2 years ‐ no significant difference between oral dextrose and placebo groups • Cerebral palsy at ≥ 2 years ‐ no significant difference between oral dextrose and placebo groups • Executive dysfunction at ≥ 2 years ‐ no significant difference between oral dextrose and placebo groups • Cost of care until primary discharge home ‐ reported separately • Maternal satisfaction (via telephone questionnaire at 6 weeks) ‐ high • Adverse events (i.e. choking or vomiting at time of gel administration) ‐ no significant difference between oral dextrose and placebo groups |
|
| Notes |
Funding The trial and follow‐up studies were funded by the Health Research Council of New Zealand (15/216; 13/131), the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) of the National Institutes of Health (NIH; grant R01HD091075), and the Aotearoa Foundation (9909494). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. Declarations of Interest During the conduct of the study, Jane Alsweiler, Jane Harding and Caroline Crowther received grants from the Health Research Council of New Zealand; Gregory Gamble received grants from the Liggins Institute. Jane Harding received an unrestricted research grant from Biomed Auckland, who manufacture dextrose gel. That sponsor was said to have no involvement in the study. No other disclosures were reported. Trials registration: ACTRN12614001263684. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote from Harding 2021: "Staff at the study sites accessed a centralized internet‐based randomization service within the first hour after the birth to receive a study number that corresponded to a study treatment pack containing a single pre‐packaged syringe of 40% dextrose gel or identical‐appearing 2% hydroxymethylcellulose placebo gel (1:1 ratio).” |
| Allocation concealment (selection bias) | Low risk | Quote from Harding 2021: "Staff at the study sites accessed a centralized internet‐based randomization service within the first hour after the birth to receive a study number that corresponded to a study treatment pack containing a single pre‐packaged syringe of 40% dextrose gel or identical‐appearing 2% hydroxymethylcellulose placebo gel (1:1 ratio).” |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quotes from Harding 2021: "Families, study and site staff and investigators were all blinded to treatment allocation". However, “some families appear to have become aware of group allocation as more parents whose babies were randomised to dextrose gel correctly guessed the contents of the gel, and would participate in a similar study in the future… however, all study staff remained blinded to treatment allocation, and there is no reason to think that the detection of the primary and secondary outcome would be likely to be differentially affected by parents’ belief about their baby’s treatment group allocation”. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote from Harding 2021: "...study and site staff and investigators were all blinded to treatment allocation". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote from Harding 2021: "All analyses were pre‐specified and carried out using a modified intention‐to‐treat approach in which babies randomised in error (did not meet eligibility criteria at randomisation) were excluded, but all other babies were analysed in the groups which they were allocated". |
| Selective reporting (reporting bias) | Low risk | Yes, all outcomes mentioned in the protocol were published. |
| Other bias | Low risk | Groups were well‐balanced for maternal and demographic variables. The authors concluded that the study was not at risk of other bias. |
Hegarty 2016a.
| Study characteristics | ||
| Methods | 2 centre randomised, double‐blind, placebo‐controlled trial | |
| Participants | 416 infants were randomised (1 infant randomised in error). Of 401 children eligible for follow‐up at two years' corrected age (13 withdrawals, one death, one incorrectly randomised), 360 (90%) were assessed (12 declined, 26 overseas, 3 lost to follow‐up). At six to seven years' corrected age, 392 of the 415 correctly randomised children were eligible for follow‐up (22 withdrawals, one death) and 315 (80%) were assessed (40 declined, 37 lost to follow‐up). Inclusion criteria: infants born to mothers with diabetes, late preterm (35 to 36 weeks' gestation) or small (< 2.5 kg or < 10th percentile) or large birthweight (> 4.5 kg or > 90th percentile), or other risk factors for hypoglycaemia; ≥ 35 weeks gestation; birthweight ≥ 2.2 kg; < 1 hour old; no apparent indication for admission to NICU, unlikely to require admission to NICU for other reasons; mother intended to breastfeed Exclusion criteria: major congenital abnormality, previously fed by formula or received intravenous fluid, previous diagnosis of hypoglycaemia, admission to NICU or imminent admission to NICU Setting: 2 hospitals providing maternity and neonatal services (Auckland City Hospital and Waitakere Hospital) in Auckland, New Zealand Timing: Recruitment: August 2013 to November 2014 Follow‐up: August 2015 to February 2017 Follow‐up: dates not stated |
|
| Interventions | 40% dextrose gel massaged into the buccal mucosa as a single dose (0.5 mL/kg or 1 mL/kg at 1 hour) or multiple doses (additional 0.5 mL/kg 3 times pre‐feed in first 12 hours) (n = 277) vs Placebo gel massaged into the buccal mucosa using the same protocol and volume as the intervention (n = 138) In both groups, babies were breastfed after the intervention and their blood glucose concentration was measured using the glucose oxidase method at 2 hours after birth. Subsequent blood glucose measurements were performed according to local hospital protocol. Babies who developed hypoglycaemia were managed according to the standard clinical practice at each hospital. |
|
| Outcomes |
Primary outcome
Secondary outcomes at neonatal stage
Secondary outcomes at two years of age
Secondary outcomes at six to seven years of age
|
|
| Notes |
Funding This trial was funded by the A+ Trust (www.adhb.govt.nz; A+5696); Auckland Medical Research Foundation (www.medicalresearch.org.nz; 1113012); Cure Kids (www.curekids.org.nz; 3537); and Lottery Health Research (http://www.communitymatters.govt.nz; 326844), and by philanthropic donations to the University of Auckland Foundation (www.auckland.ac.nz). The two‐year follow‐up studies were also funded by grants from the Health Research Council of New Zealand (13/131. 15/216), Lottery Health Research (241266), Cure Kids (3561), Gravida, National Centre for Growth and Development (SCH‐14‐14 Hegarty) and the Eunice Kennedy Shriver National Institute of Child Health & Human Development, National Institutes of Health (R01HD091075). The six to seven year follow‐up study was funded by the Health Research Council of New Zealand (19/960) and the Eunice Kennedy Shriver National Institute of Child Health & Human Development, National Institutes of Health (R01HD091075). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. Declarations of interest Jane Harding received an unrestricted research grant from Biomed Auckland, who manufacture dextrose gel. That sponsor was said to have no involvement in the study. No other disclosures were reported. Other primary authors reported no competing interests. Australian New Zealand Clinical Trials Registry ACTRN12613000322730 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote from Hegarty 2016: "We used computer‐generated blocked randomisation with variable block sizes to assign babies to one of eight treatment arms". |
| Allocation concealment (selection bias) | Low risk | Centralised allocation. Quote from Hegarty 2016: "Research staff entered demographic and entry criteria data into an online randomisation website that provided a number corresponding to a numbered trial pack". |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote from Hegarty 2016: "Clinicians, families, and all study investigators were masked to treatment group allocation throughout the study and remain so for planned follow‐up". |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote from Hegarty 2016: "At 24 months’ corrected age, children underwent a comprehensive assessment of neurodevelopment, growth and general health by doctors trained in all assessments who were unaware of the child’s randomisation group". Quote from Wei: “Assessors were blinded to trial allocation and the neonatal glycemic history of the child.” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote from Hegarty 2016: “All other babies had primary outcome data available and were included in the intention‐to‐treat analysis”. |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes were reported except for cost of care which was reported separately. |
| Other bias | Unclear risk | The study was not terminated early. Co‐interventions were similar across arms. Quote from Hegarty 2016: “There was no difference between placebo and dextrose gel groups in timing of gel administration or in volume of gel administered”. Quote from Wei: “Of those assessed [at six‐to‐seven years follow‐up], there was potential imbalance in several baseline prognostic variables between treatment groups, including lower maternal BMI and nulliparity and fewer females among those allocated to dextrose gel 1000 mg/kg, and fewer children of Māori and Pacific ethnicity among those allocated to dextrose gel 400 mg/kg and dextrose gel 1000 mg/kg (Table 1).” Intervention delivery was compliant with protocol. Follow‐up assessments were conducted at the same time points across arms. The authors concluded that the study was not at risk of other bias. |
aRR: adjusted risk ratio BMI: body mass index DCCS: Dimensional Change Card Sort logMAR: Logarithm of the Minimum Angle of Resolution NICU: neonatal intensive care unit SCBU: special care baby unit SD: standard deviation vs: versus
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bourchier 1992 | The intervention was oral dextrose gel as a treatment for neonatal hypoglycaemia. |
| Burch 2021 | Not a randomised controlled trial |
| Coors 2018 | Not a randomised controlled trial |
| Gupta 2022 | The intervention was oral dextrose gel as a treatment for neonatal hypoglycaemia. |
| Retbi 2013 | The intervention was oral dextrose gel as a treatment for neonatal hypoglycaemia. |
| Van Loghum 2014 | The intervention was oral dextrose gel as a treatment for neonatal hypoglycaemia. |
Characteristics of studies awaiting classification [ordered by study ID]
CTRI/2017/11/010645.
| Methods | Randomised parallel controlled trial |
| Participants | 611 infants Inclusion criteria: infants of diabetic mothers, > 35 weeks’ gestation and birthweight > 2 kg Exclusion criteria: major congenital malformation or requiring admission to NICU before randomisation for any of the following: < 35 weeks’ gestation, birthweight < 2 kg, respiratory distress, major lethal congenital malformation, antenatal ultrasound findings with absent/reversal of diastolic mesenteric flow, Rh negative mother with DCT positive baby and indication suggested by consultants Setting: India |
| Interventions | 40% dextrose gel (0.5 ml/L) massaged into the buccal mucosa after birth followed by a breast feed within 30 minutes after birth vs Breast feed within 30 minutes after birth |
| Outcomes |
Primary outcome
Secondary outcomes
|
| Notes | Trial registration: CTRI/2017/11/010645. Trial completed but unpublished ‐ authors contacted in May 2023 for additional information. |
NCT04185766.
| Methods | Randomised parallel controlled trial |
| Participants | 172 infants Inclusion criteria: late preterm and term infants (34 to 42 weeks’ gestation), small (< 10th centile) or large‐for‐gestational age (> 90thcentile), natural birth, rooming‐in and body temperature between 36.5 to 37.5 degrees. Mother intends to breastfeed and has a BMI between 19 and 24. Exclusion criteria: major congenital malformations, blood glucose concentration < 47 mg/dL (2.6 mmol/L), NICU admission, milk intake in formula, intravenous infusion of 10% glucose solution, metabolic and respiratory acidosis (pH: 7.28 to 7.38) or mother taking medications during pregnancy Setting: Poliambulanza Foundation Hospital Institute, Brescia, Italy |
| Interventions | 40% destrogel as a single dose (0.5 mL/kg or 1 mL/kg) massaged into the buccal mucosa at one hour after birth (n = 86) vs Placebo gel massaged into the buccal mucosa using the same protocol and volume as the intervention (n = 86) |
| Outcomes |
Primary outcome
Secondary outcomes
|
| Notes | Trial registration: NCT04185766. Trial completed but unpublished ‐ authors contacted in May 2023 for additional information |
TCTR20190805003.
| Methods | Randomised double‐blind, placebo‐controlled trial |
| Participants | 600 infants Inclusion criteria: late preterm (34 to 37 weeks' gestation), small (< 10th centile) or large‐for‐gestational age (> 90th centile), infants of diabetic mothers, low birthweight (< 2500 g) or macrosomia (> 4000 g) Exclusion criteria: received oral feed or intravenous treatment for hypoglycaemia, congenital abnormality, admission to NICU, birthweight < 1800 grams Setting: Thailand |
| Interventions | 40% dextrose gel (0.5 ml/L) applied into the buccal mucosa within 48 hours after birth vs Arboxymethyl cellulose placebo gel massaged into the buccal mucosa using the same protocol as the intervention |
| Outcomes |
Primary outcome
Secondary outcomes
|
| Notes | Trial registration: TCTR20190805003. Trial completed but unpublished ‐ authors contacted in May 2023 for additional information |
BMI: body mass index DCT: Direct Coombs Test NICU: neonatal intensive care unit Rh: rhesus vs: versus
Characteristics of ongoing studies [ordered by study ID]
NCT04353713.
| Study name | Gel for early hypoglycaemia prevention in preterm infants |
| Methods | Multi‐centre, randomised double‐blind, placebo‐controlled trial |
| Participants | 534 infants Inclusion criteria: Infants ≤ 32 weeks’ gestation Exclusion criteria: planned comfort care (palliative approach) after delivery Setting: Ireland |
| Interventions | 40% oral dextrose gel (0.5 ml/L) massaged into the buccal mucosa immediately after stabilisation or resuscitation at birth prior to in‐house transport from the delivery ward to the NICU vs 2% hydroxymethylcellulose placebo gel massaged into the buccal mucosa using the same protocol and volume as the intervention |
| Outcomes |
Primary outcome
Secondary outcomes
|
| Starting date | 1 July 2020 |
| Contact information | jkelleher@coombe.ie |
| Notes | Trial registration: NCT04353713 |
NICU: neonatal intensive care unit vs: versus
Differences between protocol and review
The original protocol for this review was published in 2016 (Hegarty 2016). For the 2021 review update, a new search strategy was developed and run without date limits (Edwards 2021). This new search strategy excluded Embase, CINAHL, ClinicalTrials.gov, and the World Health Organization’s International Clinical Trials Registry Platform (ICTRP) in line with Cochrane Neonatal’s latest guidance. The term ‘adverse effects’ was changed to ‘adverse events’.
In consultation with a Cochrane Neonatal Information Specialist, the 2023 review followed a revised search strategy to increase search sensitivity. In addition to the databases searched in the 2021 review update, this review included searches of: Embase, Epistemonikos, ClinicalTrials.gov, and the World Health Organization’s International Clinical Trials Registry Platform (ICTRP).
Population and RCT filters updated by Cochrane Neonatal in 2022 were used in the updated review.
Contributions of authors
2023 update
LR:
screened studies for eligibility and extracted data;
prepared the first draft and revised subsequent drafts under the supervision of Jane Harding and Luling Lin;
contributed to subsequent drafts and approved the final version.
LL:
screened studies for eligibility and extracted data;
contributed to subsequent drafts and approved the final version.
JA:
contributed to subsequent drafts and approved the final version.
TE:
contributed to subsequent drafts and approved the final version.
GL:
contributed to subsequent drafts and approved the final version.
JH:
supervised the first draft and revised subsequent drafts; and
approved the final version.
Sources of support
Internal sources
-
Liggins Institute, University of Auckland, New Zealand
University appointments for Jane Harding and Jane Alsweiler
-
Aotearoa Foundation, New Zealand
Undergraduate Clinical Research Internship for Gordon Liu and research fellowship for Luling Lin
External sources
-
Vermont Oxford Network, USA
Cochrane Neonatal Reviews are produced with support from Vermont Oxford Network, a worldwide collaboration of health professionals dedicated to providing evidence‐based care of the highest quality for newborn infants and their families
-
Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, USA
Contribution to salary support for Jane Harding
Declarations of interest
LR has no interest to declare. She was an independent reviewer who extracted data and assessed bias and certainty of evidence for both included studies.
LL has no interest to declare. She was an independent reviewer who extracted data and assessed bias and certainty of evidence for both included studies.
JA is an author of the included studies (Harding 2021; Hegarty 2016a). She has published opinions in medical journals relevant to the interventions in the work. The studies were funded by Auckland Medical Research Foundation and Health Research Council of New Zealand.
TE is an author of an included study (Harding 2021). The study was funded by Health Research Council of New Zealand (HRC) (grant 15/216) and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) of the National Institutes of Health (NIH; grant R01HD091075).
GL has no interest to declare.
JH is an author of the included studies (Harding 2021; Hegarty 2016a). She is the principal investigator of the pre‐hPOD trial and follow‐up studies, funded from: A+ Trust (A+5696); Auckland Medical Research Foundation (1113012); Cure Kids (3537, 3561); Lottery Health Research (241266, 326844); philanthropic donations to the University of Auckland Foundation (F‐ILG‐LRSR); Health Research Council of New Zealand (15/216, 19/690); Gravida, National Centre for Growth and Development (SCH‐14‐14 Hegarty); and Eunice Kennedy Shriver National Institute of Child Health & Human Development, National Institutes of Health (R01HD091075). She is also the principal investigator of the hPOD trial and follow‐up studies, funded from: Health Research Council of New Zealand (13/131, 15/216), Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health (R01HD091075). She received partial salary support for research with results included in this review and during the writing of this review from Eunice Kennedy Shriver National Institute of Child Health and Human Development. She has given multiple lectures and published some review articles which relate to the material included in this review, none directly reporting the contents of the review.
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Harding 2021 {published and unpublished data}
- ACTRN12614001263684. hPOD - Hypoglycaemia Prevention in newborns with Oral Dextrose. anzctr.org.au/Trial/Registration/TrialReview.aspx?id=367361&isReview=true (first received 17 november 2014). [ANZCTR TRIAL REGISTRATION: https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=367361]
- Edwards T, Alsweiler JM, Crowther CA, Edlin R, Gamble GD, Hegarty JE, et al. Prophylactic oral dextrose gel and neurosensory impairment at 2-year follow-up of participants in the hPOD randomized trial. JAMA 2022;327(12):1149-57. [DOI: 10.1001/jama.2022.2363] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards T, Alsweiler JM, Crowther CA, Edlin R, Gamble GD, Hegarty JE, et al. Two-year outcomes after prophylactic oral dextrose gel: the hypoglycaemia prevention with oral dextrose (hpod) randomised trial. Journal of Paediatrics and Child Health 2022;58:157-9. [DOI: 10.1111/jpc.15947] [DOI]
- Harding JE, Hegarty JE, Crowther CA, Edlin R, Gamble GD, Alsweiler JM. Randomised trial of neonatal hypoglycaemia prevention with oral dextrose gel (hPOD): study protocol. BMC Pediatrics 2015;15:120. [DOI: 10.1186/s12887-015-0440-6] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harding JE, Hegarty JE, Crowther CA, Edlin R, Gamble GD, Alsweiler JM, hPOD Study Group. Evaluation of oral dextrose gel for prevention of neonatal hypoglycemia (hPOD): A multicenter, double-blind randomized controlled trial. PLoS Medicine 2021;18(1):e1003411. [DOI: 10.1371/journal.pmed.1003411] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- St Clair SL, Harding JE, O'Sullivan JM, Gamble GD, Alsweiler JM, Vatanen T, hPOD Study Group. Effect of prophylactic dextrose gel on the neonatal gut microbiome. Archives of Disease in Childhood - Fetal and Neonatal Edition 2022;107(5):501-7. [DOI: 10. 1136/archdischild-2021- 322757] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hegarty 2016a {published and unpublished data}
- ACTRN12613000322730. Hypoglycaemia prevention in newborns with oral dextrose: the dosage trial [In newborn infants at risk of hypoglycaemia does prophylactic oral dextrose gel compared to placebo reduce the incidence of hypoglycaemia (any blood glucose concentration < 2.6 mM)]. trialsearch.who.int/Trial2.aspx?TrialID=ACTRN12613000322730 (first received 22 March 2013). [CENTRAL: CN-02443606]
- Griffith RJ, Hegarty JE, Alsweiler JM, Gamble GD, May R, McKinlay CJ, et al. Two-year outcomes after dextrose gel prophylaxis for neonatal hypoglycaemia. Archives of Disease in Childhood - Fetal and Neonatal Edition 2021;206(3):278-85. [DOI: 10.1136/archdischild-2020-320305] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hegarty JE, Alsweiler JM, Gamble GG, Crowther CA, Harding JE. Effect of prophylactic dextrose gel on continuous measures of neonatal glycemia: secondary analysis of the pre-hpod trial. Journal of Pediatrics 2021;245:107-15.e.4. [DOI: 10.1016/j.jpeds.2021.03.057] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hegarty JE, Harding JE, Gamble GD, Crowther CA, Edlin R, Alsweiler JM. Preventing neonatal hypoglycaemia with oral dextrose gel: a randomised controlled trial. Journal of Perinatal Medicine. Abstracts 12th World Congress of Perinatal Medicine; 2015 November 3 - 6; Madrid 2015;43(s1):O-0119. [DOI: 10.1515/jpm-2015-2002] [DOI]
- Hegarty JE, Harding JE, Gamble GD, Crowther CA, Edlin R, Alsweiler JM. Prophylactic oral dextrose gel for newborn babies at risk of neonatal hypoglycaemia: a randomised controlled dose-finding trial (the Pre-hPOD Study). PLOS Medicine 2016;13(10):e1002155. [DOI: 10.1371/journal.pmed.1002155] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei X, Franke N, Alsweiler JM, Brown GTL, Gamble GD, McNeill A, et al. Dextrose gel prophylaxis for neonatal hypoglycemia and neurocognitive function at early-school-age: a randomized dosage trial. Unpublished. [DOI] [PMC free article] [PubMed]
- Wei X, Harding JE, Gamble GD, Alsweiler JM, Franke N, Rogers JA, et al. Dextrose gel prophylaxis for neonatal hypoglycaemia and neurocognitive function at early-school-age: a randomised dosage study. Perinatal Society of Australia and New Zealand (PSANZ) 2023 Annual Congress “Laneways to Better Perinatal Outcomes”, 2023 5–8 March; Melbourne Convention Centre, Melbourne, Victoria. Journal of Paediatrics and Child Health 2023;59:4-54. [DOI: 10.1111/jpc.16356] [DOI]
References to studies excluded from this review
Bourchier 1992 {published data only}
- Bourchier D, Weston P, Heron P. Hypostop for neonatal hypoglycaemia. New Zealand Medical Journal 1992;105(926):22. [PMID: ] [PubMed] [Google Scholar]
Burch 2021 {published data only}
- Burch J, Tort S. What are the effects of oral dextrose for preventing hypoglycemia in at‐risk neonates? Cochrane Clinical Answers 2021. [DOI: 10.1002/cca.3727] [DOI]
Coors 2018 {published data only}
- Coors S, Cousin J, Hagan J, Kaiser J. Prophylactic dextrose gel does not prevent neonatal hypoglycemia: a quasi-experimental pilot study. Journal of Pediatrics 2018;198:156-61. [DOI: 10.1016/j.jpeds.2018.02.025] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Hagan J, Coors SM, Cousin J, Kaiser JR. Prophylactic dextrose gel does not prevent neonatal hypoglycemia: a pilot study. In: Pediatric Academic Societies Annual Meeting; 2017 May 06 - 09. San Francisco (CA), 2017. [DOI] [PubMed]
- NCT02523222. Prophylactic dextrose gel for newborns at high-risk for hypoglycemia. clinicaltrials.gov/show/NCT02523222 (first received 14 August 2015). [CENTRAL: CN-02033884]
Gupta 2022 {published data only}
- Gupta K, Prakash A, Umamaheswari B, Ashok C, Thangaraj A, Usha D. Dextrose gel for neonates at risk with asymptomatic hypoglycemia: a randomized clinical trial. Pediatrics 2022;149(6):e2021050733. [DOI: 10.1542/peds.2021-050733] [PMID: ] [DOI] [PubMed] [Google Scholar]
Retbi 2013 {published data only}
- Retbi J-M. Glucose gel for hypoglycaemia in the newborn. Soins Pediatrie, Puericulture 2013;275:8. [PMID: ] [PubMed] [Google Scholar]
Van Loghum 2014 {published data only}
- Van Loghum BS. Oral dextrose gel is effective in the treatment of neonatal hypoglycemia [Orale dextrose-gel is effectief in de behandeling van neonatale hypoglykemie]. Tijdschrift Voor Kindergeneeskunde 2014;82:147-8. [DOI: 10.1007/s12456-014-0029-2] [DOI] [Google Scholar]
References to studies awaiting assessment
CTRI/2017/11/010645 {published data only}
- CTRI/2017/11/010645. Prevention of low blood sugar by 40% oral dextrose gel in newborn infant of diabetic mother [Role of 40% oral dextrose gel on prevention of hypoglycemia in newborn Infants of Diabetic Mother (IDM). A randomized controlled trial]. who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2017/11/010645 (first received 27 November 2017). [CENTRAL: CN-01887712]
NCT04185766 {published data only}
- NCT04185766. Prevention of hypoglycaemia by oral 40% destrogel [Use of oral 40% destrogel to prevent hypoglycaemia in late‐term births and SGA or LGA term newborns]. clinicaltrials.gov/show/NCT04185766 (first received 4 December 2019). [CENTRAL: CN-02052900]
TCTR20190805003 {published data only}
- TCTR20190805003. Oral dextrose gel for management of neonates at risk for hypoglycemia. who.int/trial2.aspx?TrialID=TCTR20190805003 (first received 3 August 2019). [CENTRAL: CN-02071790]
References to ongoing studies
NCT04353713 {published data only}
- NCT04353713. Gel for early hypoglycaemia prevention in preterm infants (GEHPPI) [Oral dextrose gel to prevent early hypoglycaemia in very preterm infants]. clinicaltrials.gov/ct2/show/NCT04353713 (first received 20 April 2020). [CENTRAL: CN-02103289]
Additional references
Achoki 2010
- Achoki R, Opiyo N, English M. Mini-review: management of hypoglycaemia in children aged 0–59 months. Journal of Tropical Pediatrics 2010;56(4):227-4. [DOI: 10.1093/tropej/fmp109] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Adamkin 2011
- Adamkin DH, Committee on Fetus and Newborn. Postnatal glucose homeostasis in late-preterm and term infants. Pediatrics 2011;127(3):575-9. [DOI: 10.1542/peds.2010-3851] [PMID: ] [DOI] [PubMed] [Google Scholar]
Agrawal 2000
- Agrawal RK, Lui K, Gupta JM. Neonatal hypoglycaemia in infants of diabetic mothers. Journal of Paediatrics and Child Health 2000;36(4):354–6. [DOI: 10.1046/j.1440-1754.2000.00512.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Alkalay 2005
- Alkalay AL, Flores-Sarnat L, Sarnat HB, Moser FG, Simmons CF. Brain imaging findings in neonatal hypoglycemia: case report and review of 23 cases. Clinical Pediatrics 2005;44(9):783–90. [DOI: 10.1177/000992280504400906] [PMID: ] [DOI] [PubMed] [Google Scholar]
BAPM 2017
- British Association of Perinatal Medicine (BAPM). Identification and Management of Neonatal Hypoglycaemia in the Full Term Infant – A Framework for Practice. bapm.org/resources/40-identification-and-management-of-neonatal-hypoglycaemia-in-the-full-term-infant-2017 (accessed 1 May 2023). [DOI] [PubMed]
Becker 2016
- Becker GE, Remmington S, Remmington T. Early additional food and fluids for healthy breastfed full-term infants. Cochrane Database of Systematic Reviews 2016, Issue 8. Art. No: CD006462. [DOI: 10.1002/14651858.CD006462.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Blomquist 1994
- Blomquist HK, Jonsbo F, Serenius F, Persson LA. Supplementary feeding in the maternity ward shortens the duration of breast feeding. Acta Paediatrica 1994;83(11):1122-6. [DOI: 10.1111/j.1651-2227.1994.tb18263.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Boundy 2016
- Boundy EO, Dastjerdi R, Spiegelman D, Fawzi WW, Missmer SA, Lieberman E, et al. Kangaroo mother care and neonatal outcomes: a meta-analysis. Pediatrics 2016;137(1):e20152238. [DOI: 10.1542/peds.2015-2238] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Burns 2008
- Burns CM, Rutherford MA, Boardman JP, Cowan FM. Patterns of cerebral injury and neurodevelopmental outcomes after symptomatic neonatal hypoglycemia. Pediatrics 2008;122(1):65-74. [DOI: 10.1542/peds.2007-2822] [PMID: ] [DOI] [PubMed] [Google Scholar]
Chertok 2009
- Chertok IR, Raz I, Shoham I, Haddad H, Wiznitzer A. Effects of early breastfeeding on neonatal glucose levels of term infants born to women with gestational diabetes. Journal of Human Nutrition & Dietetics 2009;22(2):166-9. [DOI: 10.1111/j.1365-277X.2008.00921.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Cornblath 1965
- Cornblath M, Reisner SH. Blood glucose in the neonate and its clinical significance. New England Journal of Medicine 1965;273(7):378-81. [DOI: 10.1056/nejm196508122730707] [PMID: ] [DOI] [PubMed] [Google Scholar]
Cox 2006
- Cox SG. Expressing and storing colostrum antenatally for use in the newborn period. Breastfeeding Review 2006;14(3):11-6. [PMID: ] [PubMed] [Google Scholar]
Dalsgaard 2019
- Dalsgaard BT, Rodrigo-Domingo M, Kronborg H, Haslund H. Breastfeeding and skin to-skin contact as non-pharmacological prevention of neonatal hypoglycemia in infants born to women with gestational diabetes; a Danish quasi-experimental study. Sexual & Reproductive Healthcare 2019;19:1-8. [DOI: 10.1016/j.srhc.2018.10.003] [PMID: ] [DOI] [PubMed] [Google Scholar]
Daskas 2013
- Daskas N, Crowne E, Shield JP. Is labetalol really a culprit in neonatal hypoglycaemia? Archives of Disease in Childhood. Fetal & Neonatal Edition 2013;98(2):F185. [DOI: 10.1136/archdischild-2012-303057] [PMID: ] [DOI] [PubMed] [Google Scholar]
de Bruin 2022
- Bruin R, Dalen SL, Franx SJ, Ramaswamy VV, Simons SH, Flint RB, et al. The risk for neonatal hypoglycemia and bradycardia after beta-blocker use during pregnancy or lactation: A systematic review and meta-analysis. International Journal of Environmental Research and Public Health 2022;19(9616):1-43. [DOI: 10.3390/ijerph19159616] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Deshmukh 2021
- Deshmukh M, Patole S. Antenatal corticosteroids for impending late preterm (34-36+ 6 weeks) deliveries—A systematic review and meta-analysis of RCTs. PLoS ONE 2021;16(3):e0248774. [DOI: 10.1371/journal.pone.0248774] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Duvanel 1999
- Duvanel CB, Fawer CL, Cotting J, Hohlfeld P, Matthieu JM. Long-term effects of neonatal hypoglycemia on brain growth and psychomotor development in small-for-gestational-age preterm infants. Journal of Pediatrics 1999;134(4):492-8. [DOI: 10.1016/s0022-3476(99)70209-x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Edwards 2022
- Edwards T, Liu G, Battin M, Harris DL, Hegarty JE, Weston PJ, et al. Oral dextrose gel for the treatment of hypoglycaemia in newborn infants. Cochrane Database of Systematic Reviews 2022, Issue 3. Art. No: CD011027. [DOI: 10.1002/14651858.CD011027.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Eidelman 2012
- Eidelman AI. Breastfeeding and the use of human milk: an analysis of the American Academy of Pediatrics 2012 Breastfeeding Policy Statement. Breastfeeding Medicine 2012;7(5):323-4. [DOI: 10.1089/bfm.2012.0067] [PMID: ] [DOI] [PubMed] [Google Scholar]
Forster 2017
- Forster DA, Moorhead AM, Jacobs SE, Davis PG, Walker SP, McEgan KM, et al. Advising women with diabetes in pregnancy to express breastmilk in late pregnancy (Diabetes and Antenatal Milk Expressing [DAME]): a multicentre, unblinded, randomised controlled trial. Lancet 2017;389(10085):2204–13. [DOI: 10.1016/S0140-6736(17)31373-9] [PMID: ] [DOI] [PubMed] [Google Scholar]
Glasgow 2018
- Glasgow MJ, Harding JE, Edlin R, Children with Hypoglycemia and Their Later Development (CHYLD) Study Team. Cost analysis of treating neonatal hypoglycaemia with dextrose gel. Journal of Paediatrics and Child Health 2018;198(S1):21-2. [DOI: 10.1111/jpc.13882_51] [PMID: 29625731] [DOI] [Google Scholar]
GRADEpro GDT [Computer program]
- GRADEpro GDT. Version accessed 24 May 2023. Hamilton (ON): McMaster University (developed by Evidence Prime). Available at gradepro.org.
Gupta 2022
- Gupta K, Amboiram P, Balakrishnan U, Askok C, Abiramalatha T, Devi U. Dextrose gel for neonates at risk with asymptomatic hypoglycemia: a randomized clinical trial. Pediatrics 2022;149(6):e2021050733. [DOI: 10.1542/peds.2021-050733] [PMID: ] [DOI] [PubMed] [Google Scholar]
Harris 2012
- Harris DL, Weston PJ, Harding JE. Incidence of neonatal hypoglycemia in babies identified as at risk. Journal of Pediatrics 2012;161(5):787-91. [DOI: 10.1016/j.jpeds.2012.05.022] [PMID: ] [DOI] [PubMed] [Google Scholar]
Harris 2013
- Harris DL, Weston PJ, Signal M, Chase JG, Harding JE. Dextrose gel for neonatal hypoglycaemia (the Sugar Babies Study): a randomised, double-blind, placebo-controlled trial. Lancet 2013;382(9910):2077-83. [DOI: 10.1016/S0140-6736(13)61645-1] [PMID: ] [DOI] [PubMed] [Google Scholar]
Harris 2014
- Harris DL, Weston PJ, Battin MR, Harding JE. A survey of the management of neonatal hypoglycaemia within the Australian and New Zealand Neonatal Network. Journal of Paediatrics and Child Health 2014;50(10):E55-62. [DOI: 10.1111/j.1440-1754.2009.01599.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Harris 2020
- Harris DL, Weston PJ, Gamble GD, Harding JE. Glucose profiles in healthy term infants in the first 5 days: the glucose in well babies (GLOW) study. Journal of Pediatrics 2020;223:34-41.e4. [DOI: 10.1016/j.jpeds.2020.02.079] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hawdon 1993
- Hawdon JM, Aynsley-Green A, Bartlett K, Ward Platt MP. The role of pancreatic insulin secretion in neonatal glucoregulation. II. Infants with disordered blood glucose homoeostasis. Archives of Disease in Childhood 1993;68(3 Spec No):280-5. [DOI: 10.1136/adc.68.3_spec_no.280] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hay 2009
- Hay WW Jr, Raju TN, Higgins RD, Kalhan SC, Devaskar SU. Knowledge gaps and research needs for understanding and treating neonatal hypoglycemia: workshop report from Eunice Kennedy Shriver National Institute of Child Health and Human Development. Journal of Pediatrics 2009;155(5):612-7. [DOI: 10.1016/j.jpeds.2009.06.044] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Altman DG, Sterne JA, editor(s). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Churchill R, Chandler J, Cumpston MS, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). Cochrane, 2011. Available fromhandbook-5-1.cochrane.org.
Higgins 2022
- Higgins JP, Li T, Deeks JJ. Chapter 6: Choosing effect measures and computing estimates of effect. In: Higgins JP, Thomas J Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (updated February 2022). Cochrane, 2022. Available from training.cochrane.org/handbook.
Kaiser 2015
Kerstjens 2012
- Kerstjens JM, Bocca-Tjeertes IF, Winter AF, Reijneveld SA, Bos AF. Neonatal morbidities and developmental delay in moderately preterm-born children. Pediatrics 2012;130(2):e265-72. [DOI: 10.1542/peds.2012-0079] [PMID: ] [DOI] [PubMed] [Google Scholar]
Koh 1988
- Koh TH, Aynsley-Green A, Tarbit M, Eyre JA. Neural dysfunction during hypoglycaemia. Archives of Disease in Childhood 1988;63(11):1353-8. [DOI: 10.1136/adc.63.11.1353] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kurtoglu 2005
- Kurtoglu S, Akcakus M, Keskin M, Ozcan A, Hussain K. Severe hyperinsulinaemic hypoglycaemia in a baby born to a mother taking oral ritodrine therapy for preterm labour. Hormone Research 2005;64(2):61-3. [DOI: 10.1159/000087471] [PMID: ] [DOI] [PubMed] [Google Scholar]
Liberati 2009
- Liberati A, Altman DG, TetzlaM J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Medicine 2009;6(7):e1000100. [DOI: 10.1136/bmj.b2700] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lucas 1988
- Lucas A, Morley R, Cole TJ. Adverse neurodevelopmental outcome of moderate neonatal hypoglycaemia. BMJ 1988;297(6659):1304-8. [DOI: 10.1159/000087471] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lucas 1999
- Lucas A, Morley R. Authors' reply to Cornblath - outcome of neonatal hypoglycaemia. Complete data are needed. BMJ 1999;318(7177):195. [DOI: 10.1136/bmj.318.7177.194a] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Maayan‐Metzger 2009
- Maayan-Metzger A, Lubin D, Kuint J. Hypoglycemia rates in the first days of life among term infants born to diabetic mothers. Neonatology 2009;96(2):80-5. [DOI: 10.1159/000203337] [PMID: ] [DOI] [PubMed] [Google Scholar]
McKinlay 2015
- McKinlay CJ, Alsweiler JM, Ansell JM, Anstice NS, Chase JG, Gamble GD, et al, CHYLD Study Group. Neonatal glycemia and neurodevelopmental outcomes at 2 years. New England Journal of Medicine 2015;373(16):1507-18. [DOI: 10.1056/NEJMoa1504909] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
McKinlay 2017
- McKinlay CJ, Alsweiler JM, Anstice NS, Burakevych N, Chakraborty A, Chase JG, et al, Children with hypoglycemia and their later development (CHYLD) study team. Association of neonatal glycemia with neurodevelopmental outcomes at 4.5 years. JAMA Pediatrics 2017;171(10):972–983. [DOI: 10.1001/jamapediatrics.2017.1579] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moher 2009
- Moore ER, Bergman N, Anderson GC, Medley N. Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database of Systematic Reviews 2016, Issue 11. Art. No: CD003519. [DOI: 10.1002/14651858.CD003519.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moore 2016
- Moore ER, Bergman N, Anderson GC, Medley N. Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database of Systematic Reviews 2016, Issue 11. Art. No: CD003519. [DOI: 10.1002/14651858.CD003519.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nadjm 2013
- Nadjm B, Mtove G, Amos B, Hildenwall H, Najjuka A, Mtei F, et al. Blood glucose as a predictor of mortality in children admitted to the hospital with febrile illness in Tanzania. American Journal of Tropical Medicine & Hygiene 2013;89(2):232-7. [DOI: 10.4269/ajtmh.13-0016] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Narvey 2019
- Narvey MR, Marks SD. The screening and management of newborns at risk for low blood glucose. Paediatrics & Child Health 2019;24(8):536-44. [DOI: 10.1093/pch/pxz134] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
NICE 2008
- National Institute for Health and Clinical Excellence (NICE) UK. Diabetes in Pregnancy; March 2008. Available at www.nice.org.uk/guidance/cg63.
Nivins 2022
- Nivins S, Kennedy E, Thompson B, Gamble GD, Alsweiler JM, Metcalfe R, et al Children with hypoglycaemia and their later development study group. Associations between neonatal hypoglycaemia and brain volumes, cortical thickness and white matter microstructure in mid-childhood: an MRI study. NeuroImage. Clinical 2022;33:102943. [DOI: 10.1016/j.nicl.2022.102943] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan Web 2023 [Computer program]
- Review Manager Web (RevMan Web). Version 5.6.0. The Cochrane Collaboration, 2023. Available at revman.cochrane.org.
Salhab 2004
- Salhab WA, Wyckoff MH, Laptook AR, Perlman JM. Initial hypoglycemia and neonatal brain injury in term infants with severe fetal acidemia. Pediatrics 2004;114(2):361-6. [DOI: 10.1542/peds.114.2.361] [PMID: ] [DOI] [PubMed] [Google Scholar]
Schünemann 2013
- Schünemann H, Brożek J, Guyatt G, Oxman A, editor(s). Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach (updated October 2013). GRADE Working Group, 2013. Available from gdt.guidelinedevelopment.org/app/handbook/handbook.html.
Shah 2022
- Shah R, Dai DWT, Alsweiler JM, Brown GTL, Chase JG, Gamble GD, et al, Children with hypoglycaemia and their later development (CHYLD) study team. Association of neonatal hypoglycemia with academic performance in mid-childhood. JAMA 2022;327(12):1158-70. [DOI: 10.1001/jama.2022.0992] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Singhal 1991
- Singhal PK, Singh M, Paul VK, Malhotra AK, Deorari AK, Ghorpade MD. A controlled study of sugar-fortified milk feeding for prevention of neonatal hypoglycaemia. Indian Journal of Medical Research 1991;94:342-5. [PMID: ] [PubMed] [Google Scholar]
Singhal 1992
- Singhal PK, Singh M, Paul VK, Lamba IM, Malhotra AK, Deorari AK, et al. Prevention of hypoglycemia: a controlled evaluation of sugar fortified milk feeding in small-for-gestational age infants. Indian Pediatrics 1992;29(11):1365-9. [PMID: ] [PubMed] [Google Scholar]
Solimano 2019
- Solimano A, Kwan E, Osiovich H, Dyer R, Elango R. Dextrose gels for neonatal transitional hypoglycemia: What are we giving our babies?. Paediatrics 2019;24(2):115-8. [DOI: 10.1093/pch/pxy185] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Soltani 2012
- Soltani H, Scott AM. Antenatal breast expression in women with diabetes: outcomes from a retrospective cohort study. International Breastfeeding Journal 2012;7(1):18. [DOI: 10.1186/1746-4358-7-18] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Spar 1994
- Spar JA, Lewine JD, Orrison WW Jr. Neonatal hypoglycemia: CT and MR findings. American Journal of Neuroradiology 1994;15(8):1477-8. [PMID: ] [PMC free article] [PubMed] [Google Scholar]
Surachaidungtavil 2020
- Surachaidungtavil S, Chanvorachote P, Suksumek N. A randomized control trial of oral sucrose solution for prevention of hypoglycemia in high risk infants. In Vivo 2020;34(3):1493-7. [DOI: ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sweet 1999
- Sweet DG, Hadden D, Halliday HL. The effect of early feeding on the neonatal blood glucose level at 1-hour of age. Early Human Development 1999;55(1):63-6. [DOI: 10.1016/s0378-3782(99)00004-3] [PMID: ] [DOI] [PubMed] [Google Scholar]
UNICEF 2013
- UNICEF UK - The Baby Friendly Initiative. Guidance on the development of policies and guidelines for the prevention and management of hypoglycaemia of the newborn; July 2013. Available at www.unicef.org.uk/babyfriendly/wp-content/uploads/sites/2/2010/10/hypo_policy.pdf.
Weissmann‐Brenner 2012
- Weissmann-Brenner A, Simchen MJ, Zilberberg E, Kalter A, Weisz B, Achiron R, et al. Maternal and neonatal outcomes of large for gestational age pregnancies. Acta Obstetricia et Gynecologica Scandinavica 2012;91(7):844-9. [DOI: 10.1111/j.1600-0412.2012.01412.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
WHO 1997
- World Health Organization. Hypoglycaemia of the newborn; 1997. Available at www.who.int/maternal_child_adolescent/documents/chd_97_1/en/.
WHO 2008
- World Health Organization. Indicators for assessing infant and young child feeding practices - part I: definition. 2008. Available at http://whqlibdoc.who.int/publications/2008/9789241596664_eng.pdf?ua=1.
Wight 2021
- Wight NE, Academy of Breastfeeding Medicine. ABM Clinical Protocol #1: Guidelines for glucose monitoring and treatment of hypoglycemia in term and late preterm neonates, revised 2021. Breastfeeding Medicine 2021;16(5):353-65. [DOI: 10.1089/bfm.2021.29178.new] [PMID: ] [DOI] [PubMed] [Google Scholar]
Willcox 2010
- Willcox ML, Forster M, Dicko MI, Graz B, Mayon-White R, Barennes H. Blood glucose and prognosis in children with presumed severe malaria: is there a threshold for 'hypoglycaemia'? Tropical Medicine & International Health 2010;15(2):232-40. [DOI: ] [PMID: ] [DOI] [PubMed] [Google Scholar]
Zhou 2017
- Zhou Y, Bai S, Bornhorst JA, Elhassan NO, Kaiser JR. The effect of early feeding on initial glucose concentrations in term newborns. Journal of Pediatrics 2017;181:112-5. [DOI: 10.1016/j.jpeds.2016.10.032] [DOI: ] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Edwards 2021
- Edwards T, Liu G, Hegarty JE, Crowther CA, Alsweiler J, Harding JE. Oral dextrose gel to prevent hypoglycaemia in at‐risk neonates. Cochrane Database of Systematic Reviews 2021, Issue 5. Art. No: CD012152. [DOI: 10.1002/14651858.CD012152.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hegarty 2016b
- Hegarty JE, Harding JE, Crowther CA, Brown J, Alsweiler J. Oral dextrose gel for the prevention of hypoglycaemia in newborn infants. Cochrane Database of Systematic Reviews 2016, Issue 4. Art. No: CD012152. [DOI: 10.1002/14651858.CD012152] [DOI] [Google Scholar]
Hegarty 2017
- Hegarty JE, Harding JE, Crowther CA, Brown J, Alsweiler J. Oral dextrose gel to prevent hypoglycaemia in at-risk neonates. Cochrane Database of Systematic Reviews 2017, Issue 7. Art. No: CD012152. [DOI: 10.1002/14651858.CD012152.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]


