Abstract
Objectives
The PMPCA gene encodes the α-subunit of mitochondrial processing peptidase (α-MPP), an enzyme responsible for cleavage of nuclear-encoded mitochondrial precursor proteins after their import into mitochondria. Mutations in this gene have been described in patients with nonprogressive or slow progressive cerebellar ataxia, with variable age at onset and severity. Cerebellar atrophy and striatum changes were found in severe cases.
Methods
The patient was diagnosed using whole exome sequencing. Skin fibroblasts were used for confirmation of α-MPP levels using western blot and mitochondrial morphology assessment of immunofluorescent confocal microscopy images.
Results
Two novel compound heterozygous variants in the PMPCA gene (p.Tyr241Ser and p.Met251Val) were identified in an 8-year-old proband with progressive spastic quadriparesis, delayed psychomotor development, and intellectual disability, with onset at 13 months. The brain imaging showed cortical and cerebellar atrophy, reduced volume of basal ganglia with striatum hyperintensity, and periventricular white matter changes. The patient's fibroblasts showed a decreased α-MPP level and reduced and fragmented mitochondria.
Discussion
The described case contributes to the number of patients with progressive PMPCA-related disease with a severe intermediate phenotype. Moreover, we extend the phenotype to Leigh-like white matter changes that have not been described in previously reported cases.
Introduction
Mitochondrial processing peptidase (MPP) is a heterodimeric enzyme responsible for proteolytic cleavage of targeting presequences of nuclear-encoded mitochondrial precursor proteins after their import into mitochondria.1 The PMPCA gene (9q34.3, MIM#613036) encodes the α-subunit of MPP that is important for substrate recognition.2 In total, 9 different recessive variants have been described to date in 24 patients from 9 families. They have led to a disorder with a spectrum of symptoms from ataxia to multisystemic involvement.1,3-8 Initially, the PMPCA gene mutations were reported to cause nonprogressive autosomal recessive cerebellar ataxia syndrome (SCAR2, MIM#213200), with cerebellar atrophy in 17 patients from 4 families.8 Subsequently, 2 patients from 1 family were reported with a progressive and extremely severe clinical course, with generalized cerebral and cerebellar atrophy, profound developmental delay, optic atrophy, liver failure, respiratory insufficiency, and cardiomyopathy.1 Furthermore, 5 patients with intermediate severity (progressive but without extra-neurological symptoms) were described.3-6 Three of these patients had a combination of cerebellar atrophy and Leigh-like striatum changes in the basal ganglia, which was proposed to represent a hallmark of the PMPCA-associated intermediate phenotype.5
Here we report a boy with 2 novel mutations in the PMPCA gene causing a decreased level of α-MPP and fragmentation of mitochondria. The patient had the intermediate phenotype with a severe course, and the brain imaging also included changes in the periventricular white matter, which has not been previously reported and would thus extend the clinical picture of PMPCA-related encephalopathy.
Methods
DNA Analysis
Whole-exome sequencing (Theragen Etex, South Korea) was performed using SureSelect XT V6 for library preparation and a HiSeq 2000 Sequencer (Illumina). Candidate variants in exon 7 of the PMPCA gene (NM_015160.3) were verified by Sanger sequencing (primers F: 5′GAGAACACAGTTGGCCTCCA3′ and R: 5′TTCCCGCTACTTCACCTTGG3′).
Western Blot
50 ug of whole-cell lysates were separated using SDS-PAGE and transferred to a PVDF membrane. Rabbit anti-PMPCA primary (NBP1-89126, Novus Biologicals, 1:1000 dilution) and anti-rabbit IRDye 680LT secondary (926-68023, LI-COR, 1: 20,000 dilution) antibodies were used. Signals were detected and quantified using the OdysseyXF system and ImageStudioLite (LI-COR). The α-MPP protein levels were normalized to total protein staining (REVERT 700 Total Protein Stain, LI-COR). The statistical differences were determined using one-sample t test.
Immunostaining
The patient and control fibroblasts were fixed with 4% paraformaldehyde and double-stained using a rabbit anti-PMPCA antibody (NBP1-89126, Novus Biologicals, 1:200 dilution) and mouse Total OXPHOS Rodent antibody cocktail (ab110413, Abcam, 1:200 dilution) as primary antibodies; anti-rabbit DyLight™ 488 (35553, Invitrogen, 1:250 dilution) and anti-mouse DyLight™ 550 (SA5-10173, Invitrogen, 1:500 dilution) were used as secondary antibodies. Nuclei were stained with DAPI.
Mitochondrial Morphology
A macro for ImageJ9 software provided by Merrille et al.10 was adapted to measure and count multiple morphological parameters. We analyzed 200 immunostained cells from 3 independent experiments for each patient and a control sample. The plots and t test were performed using the R Statistical Software11 and the rstatix (0.7.0) and ggplot2 (3.3.6) packages.
Ethics Approval and Consent to Participate
The study was conducted according to the guidelines of the Declaration of Helsinki. All individuals or their legal representatives (in participants younger than 18 years) signed informed consent to genetic and fibroblasts studies.
Case Description
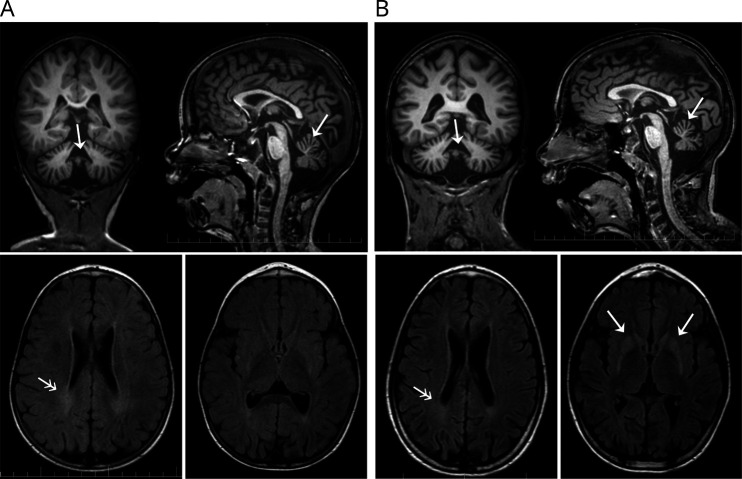
The proband is a boy from Slovakia who is the third child of healthy nonconsanguineous parents born after an uneventful pregnancy and perinatal period. He was sitting at 6 months and walking with support from 12 to 16 months. Regress in skills was noted after overcoming gastroenteritis followed by vaccination at the age of 16 months, and axial hypotony and delayed motoric development were noted. At the age of 21 months, the neurologic examination revealed psychomotor delay and development of spastic quadriparesis with no independent walking. On the MRI at the age of 2.5 years, cerebellar atrophy and nonspecific peritrigonal leukoencephalopathy without acute changes was visible (Figure 1A). At the age of 8 years, his state worsened after febrile illness, and the boy could not talk or sit autonomously. Novel MRI showed significant cortical and cerebellar atrophy, a hyperintense signal and reduced basal ganglia volume and periventricular leukoencephalopathy (Figure 1B). Metabolic investigations during life showed increased lactate in the plasma (8.0 mmol/L) only once during acute deterioration.
Figure 1. Brain MRI of the Patient.
(A) At the age of 3 years—coronal and sagittal T1-weighted images show a reduced infratentorial volume of cerebellar hemispheres and cerebellar atrophy with accentuated gyrification (arrows). On axial FLAIR sequences, increased bilateral peritrigonal white matter changes (double arrow) without acute manifestations were visible. No structural signal changes of the putamen were present. (B) At the age of 8 years—coronal and sagittal T1-weighted images show reduced volume of the vermis and significant atrophy of the cerebellar hemispheres. Axial FLAIR images show persistent increase in the periventricular signal (double arrow) and newly revealed bilateral symmetric hyperintensity in the caput nuclei caudati and putamen. The main radiologic difference at follow-up at the age of 8 years is the increase in the striatal signal abnormality and increasing atrophy of the cerebellar hemispheres.
Results
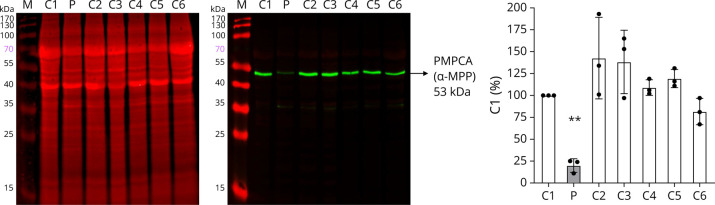
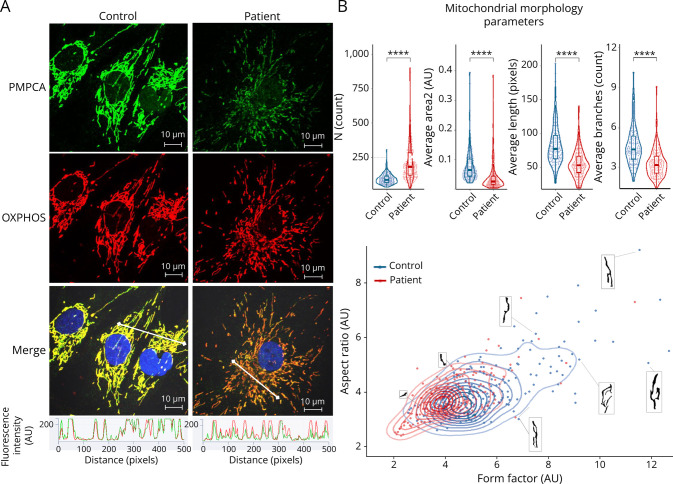
Exome sequencing revealed the presence of 2 novel variants in the PMPCA gene (NM_015160.3) in the proband—c.722A>C, p.(Tyr241Ser) and c.751A>G, p.(Met251Val). Sanger sequencing of the mother's DNA confirmed the presence of heterozygous single variant p.(Met251Val) in mother. Visualization of individual reads performed using IGV (Integrative Genomics Viewer) software confirmed that variants are located in trans (eFigure 1, links.lww.com/NXG/A641). To evaluate the effects of these PMPCA mutations, skin fibroblasts were established from the patient and controls. Western blot revealed significantly decreased level of α-MPP in the patient's fibroblasts (Figure 2). Immunofluorescent labeling confirmed correct localization but a decreased level of α-MPP in mitochondria and showed fragmentation of the mitochondrial network (Figure 3A). Mitochondrial morphometry measurements confirmed the decreased area of the mitochondrial network, a higher mean number of mitochondria per cell, a lower mean number and length of the branches, as well as a lower mean form factor (measure of shape complexity) and aspect ratio (measure of length-to-width ratio) (Figure 3B).
Figure 2. Western Blot Assessment of α-MPP Levels.
α-MPP level is decreased in patient fibroblasts (P) compared with control samples (C1–C6, description in eTable 1, links.lww.com/NXG/A641). A representative image of the western blot membranes is given along with statistics from 3 technical replicates plotted as the ratio of the intensity of the PMPCA signal (green) normalized to total protein (red) and relative to sample C1. Error bars represent SD, **p < 0.01, 1-sample t test. α-MPP = α-subunit of mitochondrial processing peptidase.
Figure 3. Immunofluorescence Staining.
(A) Immunofluorescence staining shows fragmentation of mitochondria in the patient fibroblasts. The α-MPP levels are lower in the patient, but analysis of fluorescence profiles (white line in the merged images) shows the correct localization of α-MPP (green) in mitochondria (red). (B) Mitochondrial morphometry measurements confirm statistically significant differences in the mitochondrial morphology of the patient and control fibroblasts. Each dot represents the average value for a single measured cell. α-MPP = α-subunit of mitochondrial processing peptidase.
Discussion
Our study provides information about a patient with a PMPCA-related disorder, thus increasing the number of reported patients to 25 (from 10 families). So far, 3 severity grades have been described. The milder nonprogressive ataxia in 17 patients from 4 families,8 extremely severe progressive mitochondrial encephalopathy with multisystemic involvement in 2 siblings,1 and an intermediate phenotype of progressive encephalopathy with psychomotor regression, intellectual disability, and spastic ataxia without extra-neurological signs in 8 patients from 6 families,3-6 including this study. However, the course of the disease in our patient is more severe than that of the most patients labeled as intermediate, similar to the patient described in a study,6 who never achieved independent walking. It is probable that patients with a clinical picture across this wide spectrum of severity will be identified in the future.
The authors of a study5 pointed to a specific combination of signs on brain imaging, including cerebellar atrophy and Leigh-like basal ganglia changes, which was present in 3 patients with the intermediate phenotype.4-6 In agreement with this, we observed hyperintensities and reduced volume of basal ganglia in our patient, as well, but only after the disease had progressed in his eighth year of life. Furthermore, the brain MRI showed hyperintensities in the periventricular white matter, which can also be seen in Leigh syndrome cases.12 Hence, our data support the suggestion that cerebellar atrophy and Leigh-like basal ganglia involvement are the hallmarks of the intermediate PMPCA phenotype and further propose that white matter changes may be part of this picture as well.
Mutations in the PMPCA gene often result in a decreased level of α-MPP protein,1,5,8 but increased5 or unaffected levels were seen.3 We confirmed a decreased level of α-MPP in patient fibroblasts in whole-cell lysate (Figure 2), and it was also apparent in the immunostaining images (Figure 3A). In addition, mitochondria in our patient's fibroblasts showed significant fragmentation (Figure 3, A and B), which has not been reported in previous studies. Thus far, none of the studies with patients with the intermediate form performed immunostaining. Previously, swollen mitochondria with α-MPP accumulation were reported in fibroblasts from a patient with the extremely severe form of the disease,1 and no morphological changes or accumulation were seen in a patient with the milder nonprogressive ataxia.8 In agreement with this, patients with the milder form do not show any typical mitochondrial signs, while patients with the intermediate or more severe forms present various degrees of increased lactate and progressive course of the disease.1,5
To assess potential functional effect of variants, we added analyses of the steady-state levels of the mature forms of 2 nuclear-encoded mitochondrial proteins whose processing requires MPP: heat-shock protein 60 (HSP60) and the mitochondrial transcription factor A (TFAM) in patient and controls. In addition, we assessed also levels of VDAC1 that does not undergo cleavage of mitochondrial targeting sequence by MPP. The levels of HSP60 and TFAM appeared similar in patient fibroblasts compared with controls (eFigure 2, links.lww.com/NXG/A641), suggesting that the variants do not alter the steady-state levels of processed forms of these particular proteins. This is, however, in agreement with the authors of a study8 who showed that only 1 of 4 tested targeted proteins, frataxin, revealed presence of unprocessed forms. Moreover, the initial cleavage step from precursor FXN1-210 to intermediate FXN42-210 appeared to be intact, and only the subsequent cleavage to FXN81-210 was impaired. Given the vital biological function of MPP, it is unlikely that mutations that would cause complete loss of MPP would be compatible with life. It is also possible that the reduced MPP function may not manifest itself at the steady-state level, but only under stress conditions, as indicated by the patient's clinical course with worsening of symptoms after intercurrent illnesses.
The described case extends the number of patients with progressive PMPCA-related disease and the severe intermediate form, where a patient is unable to walk independently but has no extra-neurological signs present in the extremely severe form. We show that apart from the typical cerebellar atrophy and Leigh-like striatum changes, the brain imaging can also include white matter changes in patients with progressive PMPCA-related disorder.
Acknowledgment
The authors thank the patient's family for their kind collaboration. The authors thank Dr. Eva Kutejova for kindly providing the HSP60 and TFAM antibodies and control proteins.
Appendix. Authors
| Name | Location | Contribution |
| Vibhuti Rambani, MSc | Institute of Experimental Endocrinology, Biomedical Reserach Center, Slovak Academy of Sciences, Bratislava, Slovakia | Drafting/revision of the manuscript for content, including medical writing for content; major role in the acquisition of data; analysis or interpretation of data |
| Miriam Kolnikova, MD, PhD | Medical Faculty of Comenius University and National Institute of Childern's Diseases, Bratislava, Slovakia | Drafting/revision of the manuscript for content, including medical writing for content; major role in the acquisition of data; analysis or interpretation of data |
| Michal Cagalinec, PhD | Institute of Experimental Endocrinology, Biomedical Reserach Center; Centre of Excellence for Advanced Material Application, Slovak Academy of Sciences, Bratislava, Slovakia | Analysis or interpretation of data |
| Martina Skopkova, PhD | Institute of Experimental Endocrinology, Biomedical Reserach Center, Slovak Academy of Sciences, Bratislava, Slovakia | Drafting/revision of the manuscript for content, including medical writing for content; study concept or design; analysis or interpretation of data |
| Daniela Gasperikova, PhD, DSc | Institute of Experimental Endocrinology, Biomedical Reserach Center, Slovak Academy of Sciences, Bratislava, Slovakia | Drafting/revision of the manuscript for content, including medical writing for content; study concept or design |
Study Funding
This work was supported by APVV-0296-17, VEGA 1/0572/21, APVV-22-0257, ITMS: 313021BZC9, ITMS: 313021T081.
Disclosure
The authors report no relevant disclosures. Go to Neurology.org/NG for full disclosures.
References
- 1.Joshi M, Anselm I, Shi J, et al. Mutations in the substrate binding glycine-rich loop of the mitochondrial processing peptidase-α protein (PMPCA) cause a severe mitochondrial disease. Cold Spring Harb Mol Case Stud. 2016;2(3):a000786. doi: 10.1101/mcs.a000786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gakh O, Obsil T, Adamec J, et al. Substrate binding changes conformation of the α-, but not the β-subunit of mitochondrial processing peptidase. Arch Biochem Biophys. 2001;385(2):392-396. doi: 10.1006/abbi.2000.2167 [DOI] [PubMed] [Google Scholar]
- 3.Choquet K, Zurita-Rendón O, La Piana R, et al. Autosomal recessive cerebellar ataxia caused by a homozygous mutation in PMPCA. Brain. 2016;139(3):e19. doi: 10.1093/brain/awv362 [DOI] [PubMed] [Google Scholar]
- 4.Rubegni A, Pasquariello R, Dosi C, et al. Teaching NeuroImages: Leigh-like features expand the picture of PMPCA-related disorders. Neurology. 2019;92(2):e168-e169. doi: 10.1212/WNL.0000000000006740 [DOI] [PubMed] [Google Scholar]
- 5.Serpieri V, Biagini T, Mazzotta C, et al. Phenotypic definition and genotype-phenotype correlates in PMPCA-related disease. Appl Sci. 2021;11(2):748. doi: 10.3390/app11020748 [DOI] [Google Scholar]
- 6.Takahashi Y, Kubota M, Kosaki R, Kosaki K, Ishiguro A. A severe form of autosomal recessive spinocerebellar ataxia associated with novel PMPCA variants. Brain Dev. 2021;43(3):464-469. doi: 10.1016/j.braindev.2020.11.008 [DOI] [PubMed] [Google Scholar]
- 7.Yoon G, Delague V, Mégarbané A, Isaya G. Reply: autosomal recessive cerebellar ataxia caused by a homozygous mutation in PMPCA. Brain. 2016;139(Pt 3):e20. doi: 10.1093/brain/awv363 [DOI] [PubMed] [Google Scholar]
- 8.Jobling RK, Assoum M, Gakh O, et al. PMPCA mutations cause abnormal mitochondrial protein processing in patients with non-progressive cerebellar ataxia. Brain. 2015;138(Pt 6):1505-1517. doi: 10.1093/brain/awv057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Valente AJ, Maddalena LA, Robb EL, Moradi F, Stuart JA. A simple ImageJ macro tool for analyzing mitochondrial network morphology in mammalian cell culture. Acta Histochem. 2017;119(3):315-326. doi: 10.1016/j.acthis.2017.03.001 [DOI] [PubMed] [Google Scholar]
- 10.Merrill RA, Flippo KH, Strack S. Measuring mitochondrial shape with ImageJ. In: Techniques to Investigate Mitochondrial Function in Neurons, Neuromethods, Vol 123. Springer Protocols. 2017. doi: 10.1007/978-1-4939-6890-9_2 [DOI] [Google Scholar]
- 11.Team RC. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing. R-project.org/ [Google Scholar]
- 12.Topçu M, Saatci I, Apak RA, Söylemezoglu F, Akçören Z. Leigh syndrome in a 3-year-old boy with unusual brain MR imaging and pathologic findings. AJNR Am J Neuroradiol. 2000;21(1):224-227. [PMC free article] [PubMed] [Google Scholar]