Abstract
Purpose of review:
In this review, we synthesize recent research that has reported associations of a higher sense of purpose in life with reduced risk of developing cardiovascular disease (CVD), and then explore mechanisms that might underlie these associations.
Recent findings:
Accumulating observational and experimental evidence suggests that having a higher sense of purpose might influence CVD risk through three pathways, including: (1) enhancement of other psychological and social resources that buffer against the cardiotoxic effects of overwhelming stress; (2) indirect effects through health behaviors; and (3) direct effects on biological pathways.
Summary:
A sense of purpose in life is emerging as an independent risk factor for incident CVD. A key remaining question is whether purpose causally effects CVD risk; in the future research directions section we focus on work needed to establish causality and provide suggestions for next steps.
Keywords: purpose in life, meaning in life, psychological well-being, cardiovascular disease, health psychology, epidemiology
Introduction
In the United States, nearly half of all U.S. adults (121.5 million) have cardiovascular disease (CVD: which is comprised of coronary heart disease, heart failure, stroke, and a recently revised definition of hypertension); additionally CVD is estimated to cost our economy $351.2 billion each year [1]. Most psychological, biomedical, and public health efforts have focused on reducing harmful risk factors when considering CVD, an approach that has contributed greatly to prevention and treatment programs that have led to steep declines in CVD mortality [1]. However, early signs suggest that this decline is diminishing, and might even be reversing in some groups [2]. Thus, expanding the focus to include upstream psychological assets and resilience factors might help inform the comprehensive and multidisciplinary response that our society needs to make continued progress against CVD.
Emerging evidence suggests that different dimensions of positive psychological well-being (e.g., a sense of purpose in life, optimism, life satisfaction) are independently associated with a healthier profile of CVD-related behaviors and reduced risk of CVD. While some investigators have posited that effects of positive psychological well-being simply reflect the absence of psychological distress, a more recognized risk factor for CVD, studies to date consistently report protective effects of psychological well-being that are independent of psychological distress (e.g., depression) [3–10]. Psychological well-being has been defined in various ways, and although its exact content and contours continue to evolve with new empirical research and theoretical models [11], two main theoretical perspectives have characterized its essential features. First is the hedonic approach, which defines psychological well-being as the pursuit of pleasure and happiness, often characterized by a: (1) high frequency of positive affect, (2) a low frequency of negative affect, and (3) the evaluation of one’s life as satisfying [12]. Second is the eudaimonic approach, which defines psychological well-being as the act of identifying meaningful pursuits and striving toward reaching one’s ultimate potential [8]. Also, there are other psychological constructs that fall under the broad umbrella of psychological well-being but do not fit clearly within either theoretical approach (e.g., optimism).
More recently, a rapidly growing body of evidence suggests that a sense of purpose in life, a component of eudaimonic well-being and one dimension of psychological well-being, might protect against adverse physical health outcomes [8,13,14]. A sense of purpose in life has been conceptualized in various ways [8,15–20], but it can be defined as the extent to which individuals experience life as being directed and motivated by valued life goals. A sense of purpose in life (hereafter: sense of purpose in life, sense of purpose, purpose in life, or purpose) and meaning in life are two terms that some studies have treated interchangeably, i.e., referring to the same underlying construct. However, other studies have differentiated between these terms, considering each as having a unique conceptual definition and antecedents [21]. We recognize the conceptual differences in these constructs and discuss the distinctions between them further in the future research directions section below. However, because the number of studies considering either purpose in life, or meaning in life, in relation to CVD is relatively small and because existing studies often do not provide clear guidance on which construct is being precisely measured, we do not attempt to determine if purpose in life, meaning in life, and other related constructs have differential effects on CVD—an issue we revisit in the future directions section. Further, for this review we consider both constructs without distinguishing them and call them purpose in life studies throughout.
The goal of this review is to provide a broad overview of current knowledge regarding whether and how sense of purpose might influence risk of developing CVD. We start by focusing on studies evaluating links with CVD incidence. Then, we discuss evidence suggesting three key biobehavioral pathways by which a sense of purpose in life might reduce risk of CVD, including: (1) psychological and stress-buffering pathways, (2) behavioral pathways, and (3) biological pathways. We conclude with a discussion of limitations of the existing evidence and recommendations for future research.
Sense of Purpose in Life and Cardiovascular Disease
In 2016, a meta-analysis of 10 prospective studies observed that people with a higher sense of purpose had reduced risk of all-cause mortality [22]. Using the Newcastle-Ottawa Scale—developed to assess the quality of observational epidemiological studies—the quality of studies included in the meta-analysis were rated as excellent with a mean score of 8 out of 9. All of the studies used prospective designs, had reasonable follow-up times, and adequately controlled for key confounders. All of the purpose in life assessments were self-reported and typically used validated multi-item measures, although a few used single-item measures. Among these studies, 5 that specifically evaluated cardiovascular events [22–26], were considered separately (pooled n=124,948; mean follow-up duration, 7.3 years; mean age, 57–72 years), and results showed that the relative risk for cardiovascular events among people with a higher sense of purpose was 0.83 (95% CI: 0.75, 0.92) in models adjusting for a range of key potential confounders, including demographics, conventional cardiovascular risk factors, and psychological distress [22–26].
Since the meta-analysis was published, we are aware of two additional prospective studies evaluating purpose in life in relation to CVD outcomes, and they are highly convergent with findings from the meta-analysis. One study included 453 older U.S. adults (mean age, 84 years) who reported levels of purpose upon enrollment in the study. Followed for an average of 6 years, study participants were autopsied upon their death and assessed by neurologists. The results showed that a higher sense of purpose was associated with lower odds of macroscopic infarcts (OR: 0.54, 95% CI: 0.35, 0.83) but not microinfarcts (OR: 0.78, 95% CI: 0.50, 1.23). These associations persisted after adjusting for a wide range of potential confounders [27]. The second study included 6,985 older adults from the Health and Retirement Study and evaluated cause-specific mortality over the 4-year follow-up period [28]. Compared to those with the highest levels of purpose in life, those with the lowest levels of purpose had increased risk of mortality from heart, circulatory, and blood conditions (HR:2.66, 95% CI: 1.62–4.38), but not other causes of death, after adjusting for sociodemographics and a wide array of health behaviors and several dimensions of psychosocial well-being and distress.
Many studies evaluating purpose in life and CVD outcomes have relatively short follow-up periods with a mean of 7 years of follow-up; this is a concern because of the potential for reverse causality. To help temper this concern, future research should consistently evaluate this question by: 1) using longer follow-up periods, 2) more robustly controlling for indicators of cardiovascular risk at baseline, 3) and considering removing study participants who develop CVD-related outcomes within a few years of baseline as sensitivity analyses. These methodological factors would help reduce the likelihood for reverse causality. However, the majority of studies evaluating the purpose-CVD connection already incorporate some methodological strategies (e.g., adjusting for a range of cardiovascular risk factors at baseline) which can partially address potential concerns about reverse causality. Thus, it seems unlikely that even if future studies consistently account for all of these factors, they will overturn findings from existing studies. That said, causal inference will be more compelling when future studies incorporate longer follow-up periods and remove study participants who develop CVD early in the follow-up. Further, we discuss additional ways that future studies in this area can be further methodologically enhanced in the future directions section. The studies in this section provide suggestive evidence that purpose might reduce CVD risk, but research has yet to clearly identify potential mechanisms underlying the purpose-CVD association.
Mechanisms: Psychological/Stress-Buffering Pathways, Behavioral, and Biological, Pathways
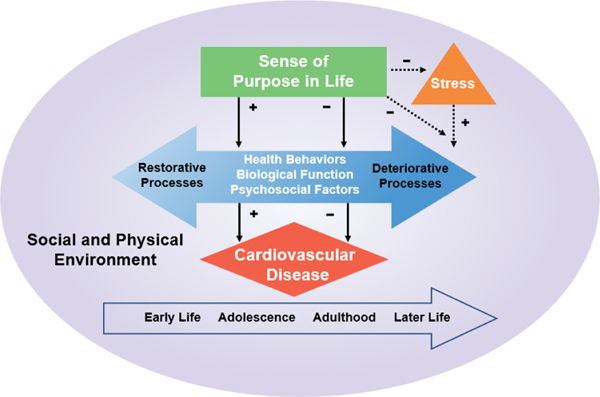
Prior work has proposed a conceptual model suggesting how positive psychological well-being might influence cardiovascular health (see Figure 1). This model suggests a sense of purpose might influence CVD risk through three biobehavioral pathways, including: (1) enhancement of other psychological and social resources that buffer against the cardiotoxic effects of overwhelming stress; (2) indirect effects through health behaviors; and (3) direct effects on biological pathways. For each pathway, a higher sense of purpose might enhance the likelihood of restorative processes (e.g., healthy diet) and decrease the likelihood of deteriorative processes (e.g., smoking and inflammation) [3]. Further, a sense of purpose might help people initially perceive stressors as less difficult (or help them react less to stressors), and it might also foster quicker recovery when stress is experienced (see Figure 1). Additionally, the model recognizes that all of these processes unfold over the life course, and that levels of purpose may ebb and flow over time [8,29–33]. These fluctuations could suggest that age modifies the effect of purpose on CVD. For example, if purpose decreases in older adulthood, the purpose-CVD association might appear somewhat less robust. However, further research is needed to pinpoint the exact nature of the trajectory of purpose in life as individuals age. Further, the model recognizes that these associations are all influenced by our social (e.g., social determinants of health) and physical environments. In the following sections, we summarize findings evaluating purpose in life’s association with each of these potential pathways, emphasizing processes particularly relevant to CVD. Although most existing studies are cross-sectional, some studies have used more rigorous methods (e.g., longitudinal or experimental study design, appropriate adjustment for potential confounders), and we emphasize findings from the methodologically stronger studies when available.
Fig. 1.
This model suggests that a sense of purpose might influence CVD risk through three biobehavioral pathways: (1) enhancement of other psychological and social resources that buffer against the cardiotoxic effects of overwhelming stress; (2) indirect effects through health behaviors; and (3) direct effects on biological pathways. The model recognizes that all of these processes unfold over the life course and are influenced by our social (e.g., social determinants of health) and physical environments. +, positive relationships; −, inverse/negative relationships. Adapted from Kubzansky et al. [3]
Psychological Pathways & Stress Buffering
Research has linked purpose in life with various psychological mechanisms that might underlie CVD risk. People with a higher sense of purpose might experience less cardiotoxic stress because they either (1) perceive stressors as less difficult or are less reactive to stressors or (2), individuals with a higher sense of purpose might be less likely to engage in unhealthy coping behaviors (e.g., smoking), or to activate the stress-linked neurohormonal cascade—all processes that can increase CVD risk. Several studies suggest that people with a higher sense of purpose perceive stressors as less difficult and are also less reactive to stressors when they are perceived, which might result in less frequent stimulation of a potentially cardiotoxic stress axis (i.e., activating sympathetic-adrenal medullary system and hypothalamic-pituitary-adrenocortical axis, or dampening of parasympathetic nervous system). For example, one laboratory study with 253 middle-aged adults assessed links between naturally varying levels of purpose in life and the study participants’ eye-blink startle reflex in response to negative stimuli, a measure of stress reactivity. The researchers observed that people with a higher sense of purpose had a slower eye-blink startle reflex [34], interpreted as evidence of less reactivity to the stressor. Similarly, a separate laboratory study of 29 older adults presented participants with photographs designed to elicit negative affective responses while the participants underwent a functional MRI scan to measure real-time blood flow in the brain [35]. In response to the photographs, participants with a higher sense of purpose displayed relatively less blood flow (or “activation”) in the amygdala, a brain region that helps process threat, fear, and stress, and relatively more “activation” of the ventral anterior cingulate cortex, a brain region involved with emotion regulation.
Other work suggests that individuals with a higher sense of purpose might experience potential stressors as less difficult. For example, a study evaluating the role of purpose in life among 315 older adult caregiving dyads—i.e., a caregiver and an individual for whom the caregiver cares due to functional disability—reported that caregivers with a higher sense of purpose reported fewer difficulties either emotionally or physically with providing care to their spouse. Of note, the association between purpose in life and emotional care-related difficulties was apparent only among women [36]. Moreover, a recent daily diary study of 1,949 middle-aged adults, tracking up to 8 daily assessments of stressors and affect, observed that on days when participants faced increased daily stressors, those with higher purpose displayed less pronounced spikes in negative affect [37]. These findings might add insight to findings from two previous studies observing a weaker association between daily hassles and depressive symptoms when comparing study participants with a higher versus lower sense of purpose [38,39]. In combination, these studies suggest that people with a higher a sense of purpose perceive potential stressors as less stressful to begin with, are less reactive to stressors, and possess an enhanced ability to recover from stressors.
These stress-buffering effects might be partly attributable to healthier coping mechanisms that are associated with a higher sense of purpose. Prior work has linked sense of purpose with greater likelihood of engaging in several healthy coping strategies, including active problem-focused coping (e.g., identifying current stressors and working to reduce their impact instead of ignoring and denying problems) [40–42] and proactive coping (e.g., working to neutralize or mitigate effects of anticipated future stressors) [43–45]. In one illustrative study among 145 adults in their late 20s, participants were given cameras and instructed to take photographs of things that made their lives feel meaningful—a strategy designed to enhance purpose [46]. One month later, increases in purpose were evident and these were also associated with increased proactive coping; an important mediator of this association was the degree to which individuals focused their attention on the future [43]. Thus, individuals with a stronger sense of purpose might self-regulate more effectively, because they are more likely to have a future-oriented perspective—thereby more likely to think about the future, anticipate future consequences, and plan ahead accordingly [47]. This is consistent with at least a few studies reporting that people with a higher sense of purpose display a heightened ability to curb impulsivity and exert self-control [48,49] as well as higher self-efficacy [50,51]. Taken together, these findings might suggest that among individuals experiencing high levels of daily stress, those with a higher sense of purpose might be better able to avoid impulsively indulging in unhealthy behaviors (e.g., binge drinking, smoking, and stress eating) and instead invoke their proactive coping, future temporal focus, and heightened self-efficacy to engage in healthier behaviors for stress relief (e.g., physical activity).
Further, adhering to health behaviors requires the ability to make healthy choices consistently in the midst of competing options. Having a sense of purpose in life might aid in this challenge. For example, one recent functional neuroimaging study suggests people with a higher sense of purpose engage in less conflict-related cognitive processing when shown health messages about physical activity. The study recruited 220 participants who were: on average in their early 30s, overweight or obese, sedentary, and less likely to enjoy physical activity. Participants viewed health messages promoting physical activity while an MRI scanner measured blood flow to various brain regions, including those that tend to be active when people feel conflicted during decision making (e.g., do I take the elevator or stairs today?). Participants with a higher sense of purpose were less likely to show increased blood flow—a proxy for brain activity—in brain regions responsible for conflict processing, and they also reported increased receptivity to health advice [52]. Thus, people with a higher sense of purpose might be able to make a range of healthier behavioral decisions with more cognitive ease. The constellation of psychological resources that people with a higher sense of purpose appear to possess might influence people’s likelihood of starting and adhering to a range of health behaviors.
Behavioral Pathways
Sense of purpose in life might enhance the likelihood that people engage in restorative health behaviors (e.g., physical activity, healthy sleep quality, use of preventive health care services) and also decrease the likelihood that people engage in harmful behaviors (e.g., smoking). In one of the key theories to address why having a greater purpose in life might help individuals live longer, Viktor Frankl suggested higher purpose provides individuals with a greater will to live and this enables them to bear more short-term discomfort or difficulties because they can appreciate why it might be worth it in the long-run [53]. Applying this theory to health behaviors, people with higher purpose may act in healthier ways and take more preventive steps because they have a greater will to live, which gives them more incentive to take preventive measures that may seem time consuming, costly, fear-inducing, or even painful (e.g., colonoscopies).
Most studies in this area have used self-report data to assess both purpose in life and health behaviors. Thus, they cannot rule out concerns regarding common-method bias, or in cross-sectional studies, reverse causality. As such, we highlight studies using longitudinal designs and objective measures whenever available. Both cross-sectional and longitudinal studies have found a higher sense of purpose is associated with more physical activity [50,54–58]. For example, a prospective study of 7,304 older adults in the English Longitudinal Study of Aging (ESLA) observed that a higher sense of purpose was associated with a higher likelihood of engaging in moderate to vigorous physical activity >1x/week and a lower likelihood of sedentary behavior over the four-year follow-up period, after adjusting for sociodemographic covariates, self-rated health status, and depressive symptoms [54]. In another study of 104 community volunteers, study participants reported their levels of purpose upon study enrolment and then wore accelerometers for three consecutive days to measure physical activity. Those with a higher sense of purpose accrued a higher number of objectively-measured steps, after adjusting for sociodemographic variables and self-reported levels of optimism, self-mastery, positive affect, and depressive symptoms [56]. Some work has suggested these effects might be due to enhanced self-efficacy. For example, one recent cross-sectional study among 94 adult women and men of varying ages directly tested this mediation pathway and found support for a model whereby enhanced self-efficacy mediated the purpose and physical activity association [50].
Cross-sectional and prospective studies evaluating sense of purpose in relation to smoking are mixed [54,59–64]. Generally, prospective studies and studies with greater statistical power (i.e., larger studies) observed no association, while cross-sectional studies have observed the opposite. For example, in a prospective study of ~7,000 younger adults from the Growing Up Today study, baseline sense of purpose was not associated with smoking over time after adjusting for sociodemographic variables, depressive symptoms, and smoking status in the prior wave of data collection. Similar findings were observed in a study of 7,304 older adults from the ELSA cohort, which adjusted for the same covariates [54,64]. However, most studies evaluate purpose after individuals have initiated smoking and therefore are considering the association of purpose with likelihood of continuing to smoke. This might be a different question from whether individuals with more purpose are less likely to smoke at the outset. Interestingly, a related and growing body of research has observed that people with a higher sense of purpose have a lower likelihood of misusing both prescription drugs and illegal substances [65–71], and, among users of illicit substances, an increased likelihood of recovering from addiction [72–74]. Given these findings, and with only a small number of studies of smoking, more research is needed to explore the potential impact of purpose in life on smoking status. A small number of studies also suggest purpose in life is associated with higher intake of healthier foods [54,55]. For example, in a prospective study of 7,196 older adults from the ESLA cohort, people with higher purpose were more likely to consume ≥5 servings of fruits and vegetables a day, after adjusting for sociodemographic factors and depressive symptoms [54].
Prospective studies have consistently found positive associations between a higher sense of purpose and healthier sleep quality [54,75–77] but not healthier sleep quantity [64,78]. For example, in a study of 428 Black and 397 White older adults from the Minority Aging Research Study and the Rush Memory and Aging Project, a higher sense of purpose was associated with a lower risk of self-reported sleep apnea and restless leg syndrome over the two-year follow-up period, after adjusting for demographic characteristics [77]. However, not all studies report positive findings across measures of sleep hygiene. For example, in an overnight laboratory study of 130 middle-aged participants who wore a nightcap to monitor REM sleep, body movement, and sleep duration while sleeping, those with a higher sense of purpose displayed less body movement but neither healthier sleep duration nor quantity of REM sleep acquired [78]. A prospective study of ~7,000 younger adults in the Growing Up Today Study did not observe a positive association of purpose with a healthy amount of sleep and instead observed that higher purpose in life was associated with lower self-reported sleep duration after controlling for participants’ sociodemographic characteristics and an array of relevant psychosocial factors [64].
Some research also suggests that purpose in life is associated with increased use of preventive healthcare services [64,79–81]. For example, in a prospective and nationally-representative study of older adults in the U.S.-based Health and Retirement Study (HRS; n = 7,168) that adjusted for sociodemographic factors, baseline health, and depressive symptoms, a higher sense of purpose at baseline was associated with a higher likelihood of obtaining cholesterol tests, colonoscopies, and cancer screenings over the four-year follow-up period—but not flu shots [80]. As people with a high sense of purpose engage in healthier behaviors, it might translate into healthier downstream biological functioning.
Biological Pathways
Purpose in life might influence a number of restorative and deteriorative biological processes linked with CVD risk (see Figure 1), including inflammation, glucose regulation, lipids, cardiac autonomic function, and composite biological risk factors (e.g., metabolic syndrome and allostatic load). Most purpose in life-biological pathway studies are cross-sectional, but one advantage of these studies is that the biological outcomes have been objectively measured, thus reducing concerns about self-report bias.
Existing research evaluating the association between purpose in life and inflammation (or inflammatory-related processes) has reported mixed findings [54,82–85]. However, all such studies are cross-sectional considering the direct association of purpose with inflammatory markers. Longitudinal research might clarify these relationships. Moreover, there is some research suggesting that purpose in life might influence inflammatory processes by “dampening” the effects of factors that seem to cause inflammation (e.g., chronic health conditions, low socioeconomic status, loneliness) or inflammatory processes, thereby serving as an effect modifier. For example, in a pair of cross-sectional studies conducted in about 1,000 middle-aged adults from the Midlife in the United States cohort (MIDUS), lower levels of education and higher numbers of chronic conditions were both associated with higher inflammation; however, among individuals with a higher sense of purpose, these factors were less strongly associated with inflammation, after adjusting for relevant confounders. Another cross-sectional study among 108 community-dwelling older adults evaluated purpose in life in relation to a gene expression pattern identified as a conserved transcriptional response to adversity (CTRA). Investigators have posited the CTRA gene expression pattern results from experiencing stress and the accompanying activation of stress hormones that cause increased transcription of genes involved in inflammation. The study found a strong association between higher purpose in life and down-regulation of CTRA gene expression after adjusting for a range of relevant confounders including health conditions [83]. In related models, researchers observed that loneliness was associated with up-regulation of CTRA gene expression, but when purpose in life was added to the model, the connection between loneliness and CTRA gene expression was no longer apparent, while the association between purpose in life and CTRA gene expression remained [83]. This is further evidence that purpose in life might moderate the effects of various stressors (e.g., loneliness) on inflammation or inflammation-related processes.
Glucose regulation is another possible biological pathway [86–88]. For example, in a study of 3,907 older adults in a national sample from the HRS cohort who had neither prediabetes nor Type 2 diabetes at baseline, participants with a higher sense of purpose had lower odds of developing objectively-measured prediabetes and Type 2 diabetes after adjusting for demographics, baseline physical health, baseline physical function, depression, and psychiatric diagnoses [86]. In contrast to the three studies with positive findings, however, one study among 100 older adults did not observe a direct association between purpose in life and HbA1c over a 2-year follow-up period, but the researchers did observe that purpose in life modified the association between low income and HbA1c, such that low income participants with higher purpose in life exhibited lower levels of HbA1c than low income participants with lower purpose in life [89].
Several studies have evaluated sense of purpose in relation to composite biological risk factors for CVD. For example, one prospective study conducted among 1,205 middle-aged adults from MIDUS observed a higher sense of purpose was marginally associated with having fewer metabolic syndrome components (p=0.06), which include unhealthy waist circumference and unhealthy levels of triglycerides, HDL cholesterol, blood pressure, and fasting plasma glucose, when adjusting for participant sociodemographic characteristics, health behaviors, and their use of relevant medications [90]. However, purpose in life was not associated with a binary (yes/no) diagnosis of metabolic syndrome. Another study among 985middle-aged adults in MIDUS found that baseline purpose in life was associated with a lower allostatic load score assessed 10 years later after adjusting for demographic variables, positive affect, negative affect, and social relations [51]. The allostatic load score included key CVD risk factors, including several markers of inflammation (triglycerides, CRP, IL-6), high lipid counts (HDL and LDL cholesterol), high blood pressure, high BMI, and low heart rate variability.
A small number of studies have evaluated purpose in life in relation to other CVD-relevant biological processes or measures, including lipid counts or measures of cardiac autonomic function. In a cross-sectional sample of 5,097 older adults from ELSA, higher purpose in life was associated with a reduced likelihood of having HDL cholesterol levels below recommended levels and marginally lower fibrinogen levels (p=0.08), after adjusting for sociodemographic variables, self-rated health, and depressive symptoms [54]. In another prospective study of 1,054 middle-aged adults from MIDUS, consistently low levels of purpose in life over a 9- or 10-year period (i.e., low levels of purpose in life at baseline and follow-up) were associated with higher HDL cholesterol levels at follow-up in models that adjusted for demographics and medication use. Moreover, health behaviors appeared to mediate this association [91]. In this same study, purpose in life was not associated with either triglycerides or LDL cholesterol.
There have also been additional important null studies that examined purpose in relation to other potential CVD-related biological pathways. For example, in a cross-sectional study of nearly 967 adults from MIDUS, purpose in life was not associated with high-frequency heart rate variability in any of the four covariate models that were tested, which ranged from basic models to enriched models that included sociodemographic covariates, baseline health, and parasympathetic activity [92]. Additionally, two studies, one conducted cross-sectionally in nearly 485 middle-aged White and Black women from the Study of women’s Health Across the Nation (SWAN) and the other conducted prospectively over a period of 3 years among 149 middle-aged women in the Healthy Women’s Study, observed that sense of purpose was not associated with markers of atherosclerosis, carotid intima thickness, or coronary artery calcification in any covariate models [93,94].
Future Research Directions
When we consider existing gaps in the literature and also attempt to scan the edge of the scientific horizon, we see several exciting future directions that have the potential to provide greater insight into how and why purpose might influence CVD and they include: 1) methodological challenges in existing studies and potential paths forward, 2) alternative study designs, 3) key mechanisms, 4) potential effect modification by key social-structural factors, 5) conceptualization and measurement of purpose in life, and 6) additional outstanding issues. Given that few studies to date can definitively establish causality, perhaps the most critical question to date is whether purpose is truly a causal contributor to CVD onset. Thus, we propose a set of future research directions that can help distinguish causation from association.
1). Methodological challenges in existing studies and potential paths forward.
Key issues include concerns about reverse causality, insufficient accounting for potential confounders, and inadequate accounting for missing data. Among studies that have evaluated the purpose-CVD association, many used longitudinal designs and self-reported CVD, however even in longitudinal studies, self-report measures of CVD can introduce different types of bias such as reverse causality. Thus, there is a need for studies with objectively measured CVD outcomes. Additionally, some prior research did not control for a sufficiently wide array of covariates (especially baseline health and an indicator of psychological distress, such as depression). Future research should evaluate the role of additional relevant variables like education, employment, and religious service attendance, in the purpose-CVD relationship. Given other work demonstrating these factors are associated with CVD as well [95,96], such factors might confound the purpose-CVD association, although many studies to date do adjust for at least some of these factors (e.g., education and employment). It is also possible that purpose might be one pathway through which these factors are linked to CVD, given some work suggesting these variables may serve as upstream factors influencing purpose [64,97]—although the evidence remains mixed for some factors (e.g., education) [98]. As research continues emerging on the factors that influence purpose in life, researchers should evaluate if they are potential confounders of the purpose-CVD relationship. Adequately assessing the role of such variables enhances our ability to assess causality more convincingly. Missing data is another concern as most existing studies used complete-case analysis. However, improperly accounting for missing data can introduce substantial bias in results, and few studies to date have taken advantage of greater accessibility of tools to account for missing data, such as inverse probability weights and/or multiple imputation techniques [99–101]. In light of these limitations, the strength and consistency of estimates across existing studies suggest that the purpose-CVD association is valid—but more research is needed.
2). Alternative study designs.
We encourage researchers to evaluate the coherence of results from observational studies that use different study designs. Several fields, including econometrics, epidemiology, biostatics, and computer science have developed study designs and analytic methods from which causal inference might be drawn based on observational data including the application of counterfactual theory and causal inference methods [102–106].
A sampling of such designs include: (1) regression discontinuity study designs, which use discontinuities in treatment assignment (e.g., there is some evidence that intensive volunteering programs can raise a sense of purpose, however allowing people who are just below eligibility levels to participate in these rigorous volunteering programs is one way to harness this design)); (2) difference in difference designs, which harness differences in trends; (3) interrupted time-series designs, which harness shocks and events (e.g., if future research identifies certain types of professions as sources of meaningful work (working for the United Nations), what effect might policy changes that alter mandatory retirement ages in those professions have on people’s sense of purpose and health?) [105,106]. Further observational work, as described throughout this section, is needed before venturing forth with interventions, but some evidence suggests that volunteering, cognitive behavioral therapy-based methods, and classroom-based modules can enhance a sense of purpose [107–111]. If observational research continues observing strong links between sense of purpose and CVD, and if future work also identifies underlying pathways (e.g., increased physical activity)—the pathways could simultaneously provide proxy targets for interventions studies and increase the scientific plausibility of an association between sense of purpose and CVD. In future work, researchers should consider using experimental methods to evaluate if purpose interventions can alter these pathways and ultimately CVD outcomes.
3). Mechanisms.
Work evaluating potential mechanisms linking purpose in life and CVD risk is already underway, yet existing studies are limited in numerous ways. For example, most health behavior studies have used self-report measures and might be biased by self-report and/or common method bias. Additionally, no prospective studies to our knowledge have formally evaluated whether potential mechanisms mediate the purpose in life-CVD association using formal mediation and causal inference methods. As researchers continue considering mechanisms, they might consider the classic behavioral (smoking, physical inactivity, poor diet) and biological (high cholesterol, high blood pressure, elevated inflammation, diabetes) risk factors for CVD, all of which need further rigorous research. In addition, researchers might also consider investigating: 1) novel biological markers, 2) biological pathways by measuring various -omics (e.g., metabolomics, proteomics), and 3) neural markers that might underlie the purpose-CVD association.
4). Potential effect modification by key social-structural factors.
Currently, all existing evidence on the purpose-CVD association have been conducted in U.S. or Japanese samples, and it remains unclear as to whether the association generalizes to other cultures. Even if the association is not observed in other cultures, it does not invalidate findings from the U.S. or Japan, but does provide interesting insight into boundary conditions. Future research should evaluate if the purpose-CVD association is potentially socially patterned or persists across important social structural factors including: age, sex, socioeconomic status, employment status, race/ethnicity, neighborhoods, and cultures. For example, existing studies provide conflicting evidence regarding the trajectory of purpose in life over the life course, with some studies finding that it appears to decrease [8,29], and others finding it seems to increase [30,31], while still others reporting that it remains stable as people age [32,33]; a further unresolved question is whether age might serve to modify the effect of purpose on CVD. Future research, should continue to evaluating this issue. A structural issue hindering research into links between purpose in life and health is the lack of large epidemiological cohort studies that include diverse populations and repeated measures over time of the participants’ sense of purpose, important potential biological pathways variables, and CVD outcomes. As more cohort studies adopt purpose in life measures, we can evaluate the potential consistency of findings across them and triangulate findings.
5). Conceptualization and measurement of purpose in life.
A key debate in the field is the content and contours of purpose in life when considered in relation to other related constructs. While this review has treated purpose in life and meaning in life as synonymous constructs, emerging theoretical and empirical work has led to the recent development of a tripartite model of meaning in life, which consists of three subconstructs: (1) purpose in life; (2) coherence/comprehension (the degree to which people perceive that their lives as making sense); and (3) significance/mattering (the degree to which people feel their existence is of significance, importance, and value in the world) [15,16]. To date, evidence evaluating CVD risk has been strongest for purpose in life, but this is potentially a byproduct of the fact that it is generally the only facet of the tripartite model assessed in large epidemiological cohorts that have enough statistical power, follow-up duration, CVD measurement, and covariates to conduct rigorous studies. Thus, for the sake of advancing knowledge, and to identify the best potential intervention targets for reducing CVD risk, epidemiological cohorts should also assess the other two facets of meaning in life (i.e., comprehension, mattering).
6). Additional outstanding issues.
Other key questions need further research; for example: is purpose exchangeable with other dimensions of psychological well-being when considered in relation to health outcomes like CVD? In this respect, psychological well-being might be similar to physical activity. For the goal of enhancing health, people engage in a wide variety of activities (e.g., jogging, swimming, biking), and one need not engage in all types of physical activity to benefit health. Similarly, further research might find that to enhance health, only some dimensions of psychological well-being are needed while others are not. Or, purpose in life might turn out to be a key factor needed for reduced risk of CVD, and other facets of psychological well-being might be unable to compensate for low levels of purpose in life. Further research is needed to clarify this point. Finally, another key point that needs additional attention is identifying (1) how much increase in purpose in life might be needed to reduce CVD risk substantially (e.g., a 5%, 10%, 25%, 50% increase in sense of purpose?) and (2) how enduring these effects need to be. After such information is identified, interventionists will have clearer targets to pursue as they consider developing and refining existing purpose interventions.
Conclusions
An exciting body of research suggests that a higher sense of purpose in life is associated with reduced risk of CVD and three biobehavioral pathways underlying this association might be: (1) enhancement of other psychological and social resources that buffer against the cardiotoxic effects of overwhelming stress; (2) indirect effects through health behaviors; and (3) direct effects on biological pathways. More work is needed to evaluate the strength of the purpose-CVD association across social structural factors and also to identify underlying pathways. As evidence accumulates, a sense of purpose in life might emerge as a novel target for interventions, and policies, seeking to enhance cardiovascular health pathways and reduce CVD.
Funding
This work was supported by a grant from the NIH (NIA: K99AG055696).
Footnotes
Conflict of Interest
Eric S. Kim has worked as a consultant with AARP and UnitedHealth Group.
Scott W. Delaney and Laura D. Kubzansky declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Contributor Information
Eric S. Kim, Department of Social & Behavioral Sciences, Harvard T.H. Chan School of Public Health, Boston, MA Lee Kum Sheung Center for Health and Happiness, Harvard T.H. Chan School of Public Health, Boston, MA; Human Flourishing Program, Institute for Quantitative Social Science, Harvard University, Cambridge, MA.
Scott W. Delaney, Department of Social & Behavioral Sciences, Harvard T.H. Chan School of Public Health, Boston, MA
Laura D. Kubzansky, Department of Social & Behavioral Sciences, Harvard T.H. Chan School of Public Health, Boston, MA Lee Kum Sheung Center for Health and Happiness, Harvard T.H. Chan School of Public Health, Boston, MA.
REFERENCES
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139:e56–528. [DOI] [PubMed] [Google Scholar]
- 2.Mensah GA, Wei GS, Sorlie PD, Fine LJ, Rosenberg, Kaufmann PG, et al. Decline in cardiovascular mortality. Circ Res. 2017;120:366–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kubzansky L, Huffman JC, Boehm JK, Hernandez R, Kim ES, Koga HK, et al. Positive psychological well-being and cardiovascular health promotion. J Am Coll Cardiol. 2018;72:1382–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Steptoe A. Happiness and health. Annu Rev Public Health. 2019;40:339–59. [DOI] [PubMed] [Google Scholar]
- 5.Pressman SD, Jenkins BN, Moskowitz JT. Positive affect and health: what do we know and where next should we go? Annu Rev Psychol. 2019;70:627–50. [DOI] [PubMed] [Google Scholar]
- 6.Scheier MF, Carver CS. Dispositional optimism and physical health: a long look back, a quick look forward. 2018;73:1082–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.VanderWeele TJ. On the promotion of human flourishing. Proc Natl Acad Sci. 2017;114:8148–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. ••Ryff CD. Psychological well-being revisited: advances in the science and practice of eudaimonia. Psychother Psychosom. 2014;83:10–28. •• This review provides an overview of the literature evaluating eudaimonic well-being (an umbrella term that encompasses a sense of purpose in life and many other dimensions of psychological well-being) with health and well-being outcomes.
- 9.Seligman MEP. Positive health. Appl Psychol Int Rev. 2008;57:3–18. [Google Scholar]
- 10.Sin NL. The protective role of positive well-being in cardiovascular disease: review of current evidence, mechanisms, and clinical implications. Curr Cardiol Rep. 2016;18:106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kashdan T, Biswas-Diner R, King L. Reconsidering happiness: the costs of distinguishing between hedonics and eudaimonia. J Posit Psychol. 2008;3:219–33. [Google Scholar]
- 12.Diener E, Suh EM, Lucas RE, Smith HL. Subjective well-being: three decades of progress. Psychol Bull. 1999;125:276–302. [Google Scholar]
- 13.Czekierda K, Banik A, Park CL, Luszczynska A. Meaning in life and physical health: systematic review and meta-analysis. Health Psychol Rev. 2017;11:387–418. [DOI] [PubMed] [Google Scholar]
- 14.Roepke AM, Jayawickreme E, Riffle OM. Meaning and health: a systematic review. Appl Res Qual Life. 2014;9:1055–79. [Google Scholar]
- 15. •George LS, Park CL. Meaning in life as comprehension, purpose, and mattering: toward integration and new research questions. Rev Gen Psychol. 2016;20:205–20. •Emerging theoretical and empirical work has led to the recent development of a tripartite model of meaning in life, which consists of three subconstructs: (1) purpose in life; (2) coherence/comprehension; and (3) significance/mattering. This is one of the 2 key papers that discusses this new conceptual model.
- 16. •Martela F, Steger MF. The three meanings of meaning in life: distinguishing coherence, purpose, and significance. J Posit Psychol. 2016;11:531–45. •Emerging theoretical and empirical work has led to the recent development of a tripartite model of meaning in life, which consists of three subconstructs: (1) purpose in life; (2) coherence/comprehension; and (3) significance/mattering. This is one of the 2 key papers that discusses this new conceptual model.
- 17.McKnight PE, Kashdan TB. Purpose in life as a system that creates and sustains health and well-being: an integrative, testable theory. Rev Gen Psychol. 2009;13:242–51. [Google Scholar]
- 18.Heintzelman SJ, King LA. Life is pretty meaningful. Am Psychol. 2014;69:561–74. [DOI] [PubMed] [Google Scholar]
- 19.Scheier MF, Wrosch C, Baum A, Cohen S, Martire LM, Matthews KA, et al. The life engagement test: assessing purpose in life. J Behav Med. 2006;29:291–8. [DOI] [PubMed] [Google Scholar]
- 20.Bronk KC. Purpose in life: A critical component of optimal youth development. 1st ed. Springer Science & Business Media; 2013. [Google Scholar]
- 21.George LS, Park CL. Are meaning and purpose distinct? An examination of correlates and predictors. J Posit Psychol. 2013;8:365–75. [Google Scholar]
- 22. ••Cohen R, Bavishi C, Rozanski A. Purpose in life and its relationship to all-cause mortality and cardiovascular events: a meta-analysis. Psychosom Med. 2016;78:122–33. ••This study meta-analyzed existing evidence around sense of purpose in life with CVD outcomes.
- 23.Tanno K, Sakata K, Ohsawa M, Onoda T, Itai K, Yaegashi Y, et al. Associations of ikigai as a positive psychological factor with all-cause mortality and cause-specific mortality among middle-aged and elderly Japanese people: findings from the Japan Collaborative Cohort Study. J Psychosom Res. 2009;67:67–75. [DOI] [PubMed] [Google Scholar]
- 24.Sone T, Nakaya N, Ohmori K, Shimazu T, Higashiguchi M, Kakizaki M, et al. Sense of life worth living (ikigai) and mortality in Japan: Ohsaki study. Psychosom Med. 2008;70:709–15. [DOI] [PubMed] [Google Scholar]
- 25.Kim ES, Sun JK, Park N, Peterson C. Purpose in life and reduced incidence of stroke in older adults: the health and retirement study. J Psychosom Res. 2013;74:427–32. [DOI] [PubMed] [Google Scholar]
- 26.Kim ES, Sun JK, Park N, Kubzansky LD, Peterson C. Purpose in life and reduced risk of myocardial infarction among older U.S. adults with coronary heart disease: a two-year follow-up. J Behav Med. 2013;36:124–33. [DOI] [PubMed] [Google Scholar]
- 27.Yu L, Boyle PA, Wilson RS, Levine SR, Schneider JA, Bennett DA. Purpose in life and cerebral infarcts in community-dwelling older people. Stroke. 2015;46:1071–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alimujiang A, Wiensch A, Boss J, Fleischer NL, Mondul AM, McLean K, et al. Association between life purpose and mortality among US adults older than 50 years. JAMA Netw Open. 2019;2:e194270–e194270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hill PL, Weston SJ. Evaluating eight-year trajectories for sense of purpose in the health and retirement study. Aging Ment Health. 2019;23:233–7. [DOI] [PubMed] [Google Scholar]
- 30.Reker GT, Peacock EJ, Wong PT. Meaning and purpose in life and well-being: a life-span perspective. J Gerontol. 1987;42:44–9. [DOI] [PubMed] [Google Scholar]
- 31.Damon W, Menon J, Cotton Bronk K. The development of purpose during adolescence. Appl Dev Sci. 2003;7:119–28. [Google Scholar]
- 32.Hill PL, Turiano NA, Spiro A, Mroczek DK. Understanding inter-individual variability in purpose in life: longitudinal findings from the VA Normative Aging Study. Psychol Aging. 2015;30:529–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ko H-J, Hooker K, Geldhof GJ, McAdams DP. Longitudinal purpose in life trajectories: examining predictors in late midlife. Psychol Aging. 2016;31:693–8. [DOI] [PubMed] [Google Scholar]
- 34.Schaefer SM, Morozink Boylan J, van Reekum CM, Lapate RC, Norris CJ, Ryff CD, et al. Purpose in life predicts better emotional recovery from negative stimuli. PLoS ONE. 2013;8:e80329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.van Reekum CM, Urry HL, Johnstone T, Thurow ME, Frye CJ, Jackson CA, et al. Individual differences in amygdala and ventromedial prefrontal cortex activity are associated with evaluation speed and psychological well-being. J Cogn Neurosci. 2007;19:237–48. [DOI] [PubMed] [Google Scholar]
- 36.Polenick CA, Kales HC, Birditt KS. Perceptions of purpose in life within spousal care dyads: associations with emotional and physical caregiving difficulties. Ann Behav Med. 2018;52:77–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hill PL, Sin NL, Turiano NA, Burrow AL, Almeida DM. Sense of purpose moderates the associations between daily stressors and daily well-being. Ann Behav Med. 52:724–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mascaro N, Rosen DH. The role of existential meaning as a buffer against stress. J Humanist Psychol. 46:168–90. [Google Scholar]
- 39.Zika S, Chamberlain K. Relation of hassles and personality to subjective well-being. J Pers Soc Psychol. 1987;53:155–62. [Google Scholar]
- 40.Skrabski A, Kopp M, Rózsa S, Réthelyi J, Rahe RH. Life meaning: an important correlate of health in the Hungarian population. Int J Behav Med. 2005;12:78–85. [DOI] [PubMed] [Google Scholar]
- 41.Smith BW, Zautra AJ. Purpose in life and coping with knee-replacement surgery. Occup Ther J Res. 2000;20:96S–99S. [Google Scholar]
- 42.Peter C, Muller R, Post MWM, van Leeuwen CMC, Werner CS, Geyh S, et al. Depression in spinal cord injury: assessing the role of psychological resources. Rehabil Psychol. 2015;60:67–80. [DOI] [PubMed] [Google Scholar]
- 43.Miao M, Gan Y. How does meaning in life predict proactive coping? The self-regulatory mechanism on emotion and cognition. J Pers. 2019;87:579–92. [DOI] [PubMed] [Google Scholar]
- 44.Miao M, Gan Y. The promotional role of meaning in life in future-oriented coping: positive affect as a mediator. Int J Psychol. 2018; [DOI] [PubMed] [Google Scholar]
- 45.Miao M, Zheng L, Gan Y. Meaning in life promotes proactive coping via positive affect: a daily diary study. J Happiness Stud. 2017;18:1683–96. [Google Scholar]
- 46.Steger M, Shim Y, Barenz J, Shin JY. Through the windows of the soul: a pilot study using photography to enhance meaning in life. J Context Behav Sci. 2013;3. [Google Scholar]
- 47.Hooker SA, Masters KS, Park CL. A meaningful life is a healthy life: a conceptual model linking meaning and meaning salience to health. Rev Gen Psychol. 2018;22:11–24. [Google Scholar]
- 48.Burrow AL, Spreng RN. Waiting with purpose: a reliable but small association between purpose in life and impulsivity. Personal Individ Differ. 2016;90:187–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li J-B, Salcuni S, Delvecchio E. Meaning in life, self-control and psychological distress among adolescents: a cross-national study. Psychiatry Res. 2019;272:122–9. [DOI] [PubMed] [Google Scholar]
- 50.Rush CL, Hooker SA, Ross KM, Frers AK, Peters JC, Masters KS. Brief report: Meaning in life is mediated by self-efficacy in the prediction of physical activity . J Health Psychol. In Press; [DOI] [PubMed] [Google Scholar]
- 51.Zilioli S, Slatcher RB, Ong AD, Gruenewald TL. Purpose in life predicts allostatic load ten years later. J Psychosom Res. 2015;79:451–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kang Y, Strecher VJ, Kim ES, Falk EB. Purpose in life and conflict-related neural responses during health decision making. Health Psychol. 2019;38:545–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Frankl VE. Man’s search for meaning. Boston: Beacon Press; 2006. [Google Scholar]
- 54.Steptoe A, Fancourt D. Leading a meaningful life at older ages and its relationship with social engagement, prosperity, health, biology, and time use. Proc Natl Acad Sci. 2019;116:1207–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hill PL, Edmonds GW, Hampson SE. A purposeful lifestyle is a healthful lifestyle: linking sense of purpose to self-rated health through multiple health behaviors. J Health Psychol. 2017; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hooker SA, Masters KS. Purpose in life is associated with physical activity measured by accelerometer. J Health Psychol. 2016;21:962–71. [DOI] [PubMed] [Google Scholar]
- 57.Holahan CK, Holahan CJ, Suzuki R. Purposiveness, physical activity, and perceived health in cardiac patients. Disabil Rehabil. 2008;30:1772–8. [DOI] [PubMed] [Google Scholar]
- 58.Holahan CK, Holahan CJ, Velasquez KE, Jung S, North RJ, Pahl SA. Purposiveness and leisure-time physical activity in women in early midlife. Women Health. 2011;51:661–75. [DOI] [PubMed] [Google Scholar]
- 59.Morimoto Y, Yamasaki S, Ando S, Koike S, Fujikawa S, Kanata S, et al. Purpose in life and tobacco use among community-dwelling mothers of early adolescents. BMJ Open. 2018;8:e020586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Thege BK, Urbán R, Kopp MS. Four-year prospective evaluation of the relationship between meaning in life and smoking status. Subst Abuse Treat Prev Policy. 2013;8:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Konkolÿ Thege B, Bachner YG, Martos T, Kushnir T. Meaning in life: does it play a role in smoking? Subst Use Misuse. 2009;44:1566–77. [DOI] [PubMed] [Google Scholar]
- 62.Konkolÿ Thege B, Stauder A, Kopp MS. Relationship between meaning in life and intensity of smoking: do gender differences exist? Psychol Health. 2010;25:589–99. [DOI] [PubMed] [Google Scholar]
- 63.Lappan S, Thorne CB, Long D, Hendricks PS. Longitudinal and reciprocal relationships between psychological well-being and smoking. Nicotine Tob Res. 2018; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chen Y, Kim ES, Koh HK, Frazier AL, VanderWeele TJ. Sense of mission and subsequent health and well-being among young adults: an outcome-wide analysis. Am J Epidemiol. 2019;188:664–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Abramoski K, Pierce J, Hauck C, Stoddard S. Variations in adolescent purpose in life and their association with lifetime substance use. J Sch Nurs. 2018;34:114–20. [DOI] [PubMed] [Google Scholar]
- 66.Kinnier RT, Metha AT, Keim JS, Okey JL, et al. Depression, meaninglessness, and substance abuse in “normal” and hospitalized adolescents. J Alcohol Drug Educ. 1994;39:101–11. [Google Scholar]
- 67.Padelford BL. Relationship between drug involvement and purpose in life. J Clin Psychol. 1974;30:303–5. [DOI] [PubMed] [Google Scholar]
- 68.Nicholson T, Higgins W, Turner P, James S, Stickle F, Pruitt T. The relation between meaning in life and the occurrence of drug abuse: a retrospective study. Psychol Addict Behav. 1994;8:24–8. [Google Scholar]
- 69.Shean GD, Fechtmann F. Purpose in life scores of student marihuana users. J Clin Psychol. 1971;27:112–3. [DOI] [PubMed] [Google Scholar]
- 70.Harlow LL, Newcomb MD, Bentler PM. Depression, self-derogation, substance use, and suicide ideation: lack of purpose in life as a mediational factor. J Clin Psychol. 1986;42:5–21. [DOI] [PubMed] [Google Scholar]
- 71.Newcomb MD, Harlow LL. Life events and substance use among adolescents: mediating effects of perceived loss of control and meaninglessness in life. J Pers Soc Psychol. 1986;51:564–77. [DOI] [PubMed] [Google Scholar]
- 72.Krentzman AR, Cranford JA, Robinson EAR. Long-term increases in purpose in life are associated with remission from alcohol dependence. Alcohol Treat Q. 2015;33:252–69. [Google Scholar]
- 73.Martin RA, MacKinnon S, Johnson J, Rohsenow DJ. Purpose in life predicts treatment outcome among adult cocaine abusers in treatment. J Subst Abuse Treat. 2011;40:183–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Roos CR, Kirouac M, Pearson MR, Fink BC, Witkiewitz K. Examining temptation to drink from an existential perspective: associations among temptation, purpose in life, and drinking outcomes. Psychol Addict Behav J Soc Psychol Addict Behav. 2015;29:716–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kim ES, Hershner SD, Strecher VJ. Purpose in life and incidence of sleep disturbances. J Behav Med. 2015;38:590–597. [DOI] [PubMed] [Google Scholar]
- 76.Phelan CH, Love GD, Ryff CD, Brown RL, Heidrich SM. Psychosocial predictors of changing sleep patterns in aging women: a multiple pathway approach. Psychol Aging. 2010;25:858–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Turner AD, Smith CE, Ong JC. Is purpose in life associated with less sleep disturbance in older adults? Sleep Sci Pract. 2017;1:14. [Google Scholar]
- 78.Ryff CD, Singer B, Love GD. Positive health: connecting well–being with biology. Philos Trans R Soc Lond B Biol Sci. 2004;359:1383–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wilson RS, Capuano AW, James BD, Amofa P, Arvanitakis Z, Shah R, et al. Purpose in life and hospitalization for ambulatory care-sensitive conditions in old age. Am J Geriatr Psychiatry. 2018;26:364–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kim ES, Strecher VJ, Ryff CD. Purpose in life and use of preventive health care services. Proc Natl Acad Sci. 2014;111:16331–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Musich S, Wang SS, Kraemer S, Hawkins K, Wicker E. Purpose in life and positive health outcomes among older adults. Popul Health Manag. 2017; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Friedman EM, Hayney M, Love GD, Singer BH, Ryff CD. Plasma interleukin-6 and soluble IL-6 receptors are associated with psychological well-being in aging women. Health Psychol. 2007;26:305–13. [DOI] [PubMed] [Google Scholar]
- 83.Cole SW, Levine ME, Arevalo JMG, Ma J, Weir DR, Crimmins EM. Loneliness, eudaimonia, and the human conserved transcriptional response to adversity. Psychoneuroendocrinology. 2015;62:11–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Friedman EM, Ryff CD. Living well with medical comorbidities: a biopsychosocial perspective. J Gerontol B Psychol Sci Soc Sci. 2012;67:535–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Morozink JA, Friedman EM, Coe CL, Ryff CD. Socioeconomic and psychosocial predictors of interleukin-6 in the MIDUS national sample. Health Psychol. 2010;29:626–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hafez D, Heisler M, Choi H, Ankuda CK, Winkelman T, Kullgren JT. Association between purpose in life and glucose control among older adults. Ann Behav Med. 2018;52:309–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Boylan JM, Tsenkova VK, Miyamoto Y, Ryff CD. Psychological resources and glucoregulation in Japanese adults: findings from MIDJA. Health Psychol. 2017;36:449–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Rasmussen NH, Smith SA, Maxson JA, Bernard ME, Cha SS, Agerter DC, et al. Association of HbA1c with emotion regulation, intolerance of uncertainty, and purpose in life in type 2 diabetes mellitus. Prim Care Diabetes. 2013;7:213–21. [DOI] [PubMed] [Google Scholar]
- 89.Tsenkova VK, Love GD, Singer BH, Ryff CD. Socioeconomic status and psychological well-being predict cross-time change in glycosylated hemoglobin in older women without diabetes. Psychosom Med. 2007;69:777–84. [DOI] [PubMed] [Google Scholar]
- 90.Boylan JM, Ryff CD. Psychological well-being and metabolic syndrome: findings from the midlife in the United States national sample. Psychosom Med. 2015;77:548–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Radler BT, Rigotti A, Ryff CD. Persistently high psychological well-being predicts better HDL cholesterol and triglyceride levels: findings from the Midlife in the U.S. (MIDUS) longitudinal study. Lipids Health Dis. 2018;17:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Sloan RP, Schwarz E, McKinley PS, Weinstein M, Love G, Ryff C, et al. Vagally-mediated heart rate variability and indices of well-being: results of a nationally representative study. Health Psychol. 2017;36:73–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Shahabi L, Karavolos K, Everson-Rose SA, Lewis TT, Matthews KA, Sutton-Tyrrell K, et al. Associations of psychological well-being with carotid intima media thickness in African American and White middle-aged women. Psychosom Med. 2016;78:511–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Low CA, Matthews KA, Kuller LH, Edmundowicz D. Psychosocial predictors of coronary artery calcification progression in postmenopausal women. Psychosom Med. 2011;73:789–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kubota Y, Heiss G, MacLehose RF, Roetker NS, Folsom AR. Association of educational attainment with lifetime risk of cardiovascular disease. JAMA Intern Med. 2017;177:1165–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Li S, Okereke OI, Chang S-C, Kawachi I, VanderWeele TJ. Religious service attendance and lower depression among women-a prospective cohort study. Ann Behav Med. 2016;50:876–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ward SJ, King LA. Work and the good life: how work contributes to meaning in life. Res Organ Behav. 2017;37:59–82. [Google Scholar]
- 98.Sumner R More education, more purpose in life? A comparison of purpose across adults with different levels of education. Appl Res Qual Life. 2017;12:17–34. [Google Scholar]
- 99.Harel O, Mitchell EM, Perkins NJ, Cole SR, Tchetgen Tchetgen EJ, Sun B, et al. Multiple imputation for incomplete data in epidemiologic studies. Am J Epidemiol. 2018;187:576–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Perkins NJ, Cole SR, Harel O, Tchetgen Tchetgen EJ, Sun B, Mitchell EM, et al. Principled approaches to missing data in epidemiologic studies. Am J Epidemiol. 2018;187:568–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Sun B, Perkins NJ, Cole SR, Harel O, Mitchell EM, Schisterman EF, et al. Inverse-probability-weighted estimation for monotone and nonmonotone missing data. Am J Epidemiol. 2018;187:585–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Greenland S, Pearl J, Robins JM. Causal diagrams for epidemiologic research. Epidemiology. 1999;10:37–48. [PubMed] [Google Scholar]
- 103.Glymour MM, Kubzansky LD. Causal inference in psychosocial epidemiology. In: Kivimaki M, Batt DG, Kawachi I, Steptoe A. Routledge International Handbook of Psychosocial Epidemiology. Routledge; 2017. p. 35–60. [Google Scholar]
- 104.VanderWeele TJ, Jackson JW, Li S. Causal inference and longitudinal data: a case study of religion and mental health. Soc Psychiatry Psychiatr Epidemiol. 2016;51:1457–66. [DOI] [PubMed] [Google Scholar]
- 105.Morgan SL, Winship C. Counterfactuals and causal inference. 2nd ed. Cambridge University Press; 2014. [Google Scholar]
- 106.Angrist JD, Pischke J-S. Mostly harmless econometrics: An empiricist’s companion. 1st ed. Princeton University Press; 2009. [Google Scholar]
- 107.Klein N Prosocial behavior increases perceptions of meaning in life. J Posit Psychol. 2017;12:354–61. [Google Scholar]
- 108.Friedman EM, Ruini C, Foy R, Jaros L, Sampson H, Ryff CD. Lighten UP! A community-based group intervention to promote psychological well-being in older adults. Aging Ment Health. 2015;1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Mens MG, Helgeson VS, Lembersky BC, Baum A, Scheier MF. Randomized psychosocial interventions for breast cancer: impact on life purpose. Psychooncology. 2015; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Breitbart W, Rosenfeld B, Pessin H, Applebaum A, Kulikowski J, Lichtenthal WG. Meaning-centered group psychotherapy: an effective intervention for improving psychological well-being in patients with advanced cancer. J Clin Oncol. 2015;33:749–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Rosenfeld B, Cham H, Pessin H, Breitbart W. Why is meaning-centered group psychotherapy (mcgp) effective? Enhanced sense of meaning as the mechanism of change for advanced cancer patients. Psychooncology. 2018;27:654–60. [DOI] [PMC free article] [PubMed] [Google Scholar]