Abstract
In the “boat at the dock” theory, pelvic organ prolapse (POP) may happen when the ropes (uterine supportive ligaments) break and/or the water level drops (pelvic floor muscles). Thus, it causes the boat (uterus and other pelvic organs) to slip from normal position and protrude out of the vagina. Surgical intervention with or without hysterectomy (hystero-preservation) is the most effective treatment for POP. Both hysterectomy and hystero-preservation for POP had a high anatomic and clinical cure rate. There is an increasing trend of hystero-preservation for POP during the past decades. The choices of either hysterectomy or hystero-preservation depend on the surgical factors, psychosocial factors, self-esteem and sexuality factors, and surgeon factors. Pelvic reconstructive surgery, either hysterectomy or hystero-preservation, can be performed via different approaches, including abdominal, laparoscopic, and vaginal routes, with native tissue or with mesh. This review will elucidate their related pros and cons, with further discussion and comparison of hystero-preservation via different routes.
Keywords: Hysterectomy, minimally invasive surgical procedures, pelvic floor disorders, pelvic organ prolapse
INTRODUCTION
Pelvic organ prolapse (POP) describes the condition when the pelvic organs, including uterus, rectum, and bladder, slip from normal position and protrude into or out of the vagina. In the “boat at the dock” theory, the pelvic organs (i.e., bladder, uterus, and rectum) are the boat. The ropes, holding the boat to the dock, are the ligaments (e.g., uterosacral and cardinal ligaments) that support the organs from above. The water is the pelvic floor muscle (e.g., levator ani muscle) that supports the organs from below. If the water level drops (i.e., loss of support or weakness of the pelvic floor muscles), the boat (organs) hangs on the ropes (ligaments). Eventually, the ropes stretch out and break, resulting in the boat (organs) falling down (i.e., prolapse).[1] POP may result from dysfunction of either pelvic muscle and/or supporting ligament.
According to a systemic analysis in 2010 by Vos et al.,[2] POP presents in about 9% of all females worldwide, especially in those who have undergone vaginal deliveries, advanced age, and increased body mass index.[3,4] Given the growing of aging population, the prevalence of POP and the demand of treatment increase over time.[5] POP becomes the leading indication for hysterectomy in postmenopausal women, and accounts for 15%–18% in all-aged women. Although hysterectomy is still the standard intervention of POP patients, more and more people consider uterine-preserving surgery (hystero-preservation).[6,7] Our previous study, based on the National Health Insurance Research Database in Taiwan, found an increasing trend of hystero-preservation for POP during the past decades. Even in the patients who needed reoperation after primary POP surgeries, their tendency of choosing hystero-preservation surgery was still high (30%).[8]
THE CONSERVATIVE TREATMENT BEFORE SURGERY
Treatments for women with POP consist of conservative and surgical management, depending on the severity of symptoms and the demand of the patients.[3,9] Individuals with no or few symptoms may choose conservative options, such as lifestyle modification, laser therapy, or pessary, which are followed by surgical intervention.
Lifestyle modification, including diet control, body weight control, avoidance of heavy lifting work, and discontinuation of smoking, should be considered before surgery;[10] nonetheless, the benefits are not yet established. Evidence indicated a positive effect of pelvic floor muscle training (PFMT) on prolapse symptoms and severity. According to Wiegersma et al., PFMT could significantly improve bladder, bowel, and pelvic floor symptoms after 3-month treatment at a rate of 57% (82/145) versus 13% (18/142) in the watchful waiting group (P < 0.001).[11] Another randomized control trial (RCT) by Hagen et al. further showed the benefit of one-to-one individualized PFMT for reducing prolapse symptoms (i.e. a significantly greater reduction in the POP symptom score) at 12 months than those in the control group.[12]
Biofeedback using electromyography (EMG) and ultrasound is added to recent PFMT treatment for more precise and individualized therapy. An observation study by Liu et al. identified a significant therapeutic effect on overactive bladder and stress urinary incontinence (SUI). However, there is no subjective improvement of POP stage by adding biofeedback with EMG.[13] On the contrary, a RCT by Gu et al. found that PFMT with ultrasound biofeedback attenuated POP severity and strengthened pelvic floor muscles.[14] Related studies on application of biofeedback on PFMT of POP treatment remain inconclusive.
Laser therapy, such as fractional CO2 laser and vaginal erbium-doped yttrium aluminium garnet (Er:YAG) laser, is commonly used for the treatment of genitourinary syndrome of menopause, and thereafter, may play some role in POP treatment.[15,16] A systematic review by Mackova et al. showed that laser therapy significantly improved either urinary incontinence, POP, or both.[17] Nonetheless, there existed huge heterogeneity of laser settings, application, and outcome measurement in these studies. Since there are only RCT and two controlled cohort studies in the review, the efficacy of laser therapy needs improvement, because of weak evidence.
For women who wish to maintain fertility or who are poor surgical candidates, patients may consider pessary use for nonsurgical intervention. Some side effects, such as vaginal erosions, discharge, and other new bowel or bladder symptoms, may still develop. The effects of pessary on sexual functions are still controversial, though most of the complications can be neglected.[18]
THE AFFECTING FACTORS OF CHOOSING HYSTERECTOMY OR HYSTERO-PRESERVATION DURING PELVIC RECONSTRUCTIVE SURGERY
In symptomatic POP patients, who failed conservative treatment, surgical intervention is still inevitable. Although both hysterectomy and hystero-preservation had high anatomic and clinical cure rate, the affecting factors on the outcome of pelvic reconstructive surgery (PRS) are enormous and obscure.[19] The choices, either hysterectomy or hystero-preservation, depend on the surgical factors, psychosocial factors, self-esteem and sex, and surgeon factors.
Surgical factors
Hystero-preservation is less traumatic because of shorter operation time, less intra- and postoperative complications, shortened hospital stay length, less perioperative hemorrhage, blood transfusion rate, urologic injury or fistula, infection, and re-admission rate, than hysterectomy.[20,21,22] Gutman and Maher also unraveled lower rates of postoperative infection risk and mesh erosion in hystero-preservation.[23] These are possibly the main factors in which affect patients’ decision. On the other hand, whether hystero-preservation had a higher recurrence rate is still equivocal. De Oliveira et al. indicated no significant difference in recurrence rates with or without hysterectomy.[21]
The concern of potential subsequent risk of cervical or uterine cancer in hystero-preservation may also affect patients’ decisions. Although the uterine removal can reduce the risk of either cervical or uterine cancer,[24] the risk of subsequent cervical cancer after subtotal hysterectomy (SH) is as low as <0.1%. Due to the potential subsequent risks, long-term surveillance and follow-up of cervical and uterine pathology are therefore essential in patients who received hystero-preservation.
Hysterectomy was found to increase the risk of postoperative SUI as well. Higher postoperative SUI may severely worsen quality of life (QoL), emotional value, and sexual satisfaction.[25] Therefore, those with higher risk of SUI or preoperative SUI symptoms and incontinence surgery such as mid-urethral sling can be considered in combination with PRS to reduce the subsequent postoperative SUI.[26]
Psychosocial and sexual factors
Patients’ characteristics can also predict their preferences for hysterectomy or not.[27] A multicenter cross-sectional study by Korbly et al. found that geographic region and education level also affected the proportion of choosing hystero-preservation.[28] Patients living in the Northeast in the United States or with higher education tended to preserve their uterus than others. Patient age, in a previous nationwide study, was also found to affect the choice to preserve uterus or not. Younger women who were under 50 years old received more hystero-preservation procedures than the older (25.1% vs. 74.9%, P < 0.0001) in Taiwan.[29]
Women are increasingly aware of self-esteem. Therefore, more women prefer to preserve their uterus in PRS. Considerations of hystero-preservation may include maintenance of femininity, integral sexual function, and better mental health.[30] Women who believed uterus as an important sense of self, and those with higher income and education level, tended to prefer hystero-preservation more. Other demographic and social factors, e.g. age, race, prolapsed stage, and previous treatment for POP, did not influence their options.[28] Interestingly, according to Korbly et al.’s study, 21% of women still prefer hystero-preservation, even with the acknowledgment for the potentially inferior outcomes.[28]
Other psychosocial factors that patients primarily ponder upon are the self-body image identity and sexual satisfaction. Since the conscience toward psychological health and sexuality has been growing more and more crucial overtimes, women are more likely to preserve their womb (uterus), which values female identity and remains integral sexual functions. Sexuality, body image, and partnership of the benefit of uterus were all their concerns, and the importance of these concerns differed between races, especially higher in Russia.[31] The effects of uterine removal for POP patients on sexual function, compared with uterine-sparing, are still debatable, since POP per SE is associated with poor sexual function. A RCT by Jeng et al. reported that there was no significant difference in postoperative sexual functioning between patients with and without hysterectomy for PRS after 6-month follow-up.[32] Despite plausible explanations, we cannot exclude the probability that hysterectomy had negative impacts on body image and sexual problems.
Surgeon factors
Besides patients’ preference, surgeons’ personal preference of surgical procedure also showed a strong force behind the choice of hysterectomy or hystero-preservation. As a surgeon or health-care provider, the surgical technical skill relies on apprenticeship during their training courses. The surgeon tends to provide the choices that they are well trained and expert at. Therefore, where the hospital or department the surgeons belong, and who the mentors in the surgeons’ training are, would intensely affect a surgeon’s preference and recommendation to their patients.[33]
In our previous study, surgeons’ age and gender were also affecting factors over choosing hystero-preservation.[29] Younger surgeons (<50 years old) performed more hystero-preservation procedures than the older surgeons (9.3%–10.7% vs. 6.3%–7.5%, P < 0.0001), while female surgeons performed less hystero-preservation procedure than the male surgeons (4.0% vs. 9.9%, P < 0.0001). Moreover, hospital accreditation levels were also impacting factors while local hospitals showed a higher rate of hysterectomy being performed, as compared with a medical center. Overall, more accurate studies are still required in the comparison of hysterectomy versus hystero-preservation for POP. Surgeons may need to get well prepared for the increasing demands of women in selecting uterine-sparing surgery for POP.
COMPARISON BETWEEN HYSTERO-PRESERVATION AND HYSTERECTOMY VIA DIFFERENT APPROACHES
Both hysterectomy and hystero-preservation can be performed via different approaches, including abdominal, laparoscopic, and vaginal routes. They can be done with native tissue (without mesh) or with mesh, which demonstrate related pros and cons. The treatment algorithm chart of POP is shown in Figure 1.
Figure 1.
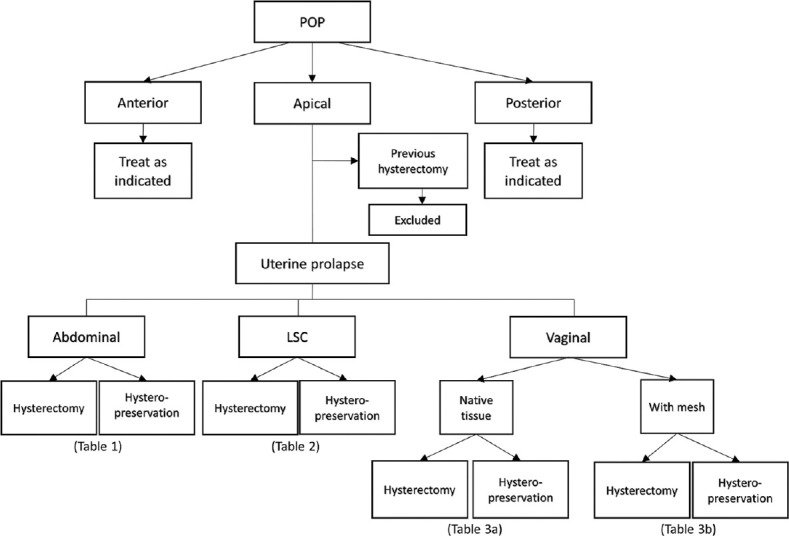
The treatment algorithm chart of POP. POP: Pelvic organ prolapse, LSC: Laparoscopy
Abdominal versus vaginal approaches
PRS can be performed through abdomen or vaginal approach, in which vaginal approach was performed as many as 80%–90% of PRS in epidemiological studies, although no precise statistic estimations.[9,34] According to Maher et al., abdominal route such as sacrocolpopexy was found to be with lower recurrence rate and better anatomic support improvement, as compared with vaginal approach. On the other hand, vaginal routes, including sacrospinous ligament fixation and uterosacral ligament suspension, had shorter operation time, shorter recovery time, as well as lower morbidity.[35] However, there was no significant difference in outcomes among the routes of hysterectomy at long-term follow-up.[36]
Hysterectomy versus hystero-preservation
Illiano et al. and Detollenaere et al. found no differences in outcomes between hysterectomy and hystero-preservation for PRS.[37,38] According to the large population-based cohort study by Dallas et al.,[39] hysterectomy, as compared with hystero-preservation, was found associated with lower risk of repeat PRS, with reoperation rate of 3.0% versus 4.4%, respectively (P < 0.001). Another meta-analysis by de Oliveira et al. showed similar results respecting recurrence (4.23% vs. 6.92%, P = 0.12) and reoperation rate (5% vs. 8.72%, P = 0.02).[21] Nonetheless, Meriwether et al. reported no difference in recurrence rate.[20] Meanwhile, hystero-preservation had shortened operating time, less blood loss, and lower risk of mesh exposure,[20] and fewer visceral injuries were revealed, as compared with hysterectomy.[40,41,42] Here, we further compared and discussed the pros and cons between hysterectomy and hystero-preservation in the same route pattern. The major findings are summarized mainly based on the meta-analysis by de Oliveira et al. and Meriwether et al. [Tables 1-4].[20,21]
Table 1.
Comparison between hysterectomy and hystero-preservation via abdominal route for pelvic organ prolapse
| Abdominal route | Hysterectomy | Hystero-preservation | Favor | Significant | Reference |
|---|---|---|---|---|---|
| Recurrence rate | 1.89% | 4.08% | Hysterectomy | NS | [21] |
| Reoperation rate | 2.83% | 5.1% | Hysterectomy | NS | [21] |
| Operative time (min) | 115-239 | 89-192 | Hystero-preservation | Significant | [20] |
| Blood loss (mL) | 86.77-333 | 52.77-200 | Hystero-preservation | Significant | [20] |
| Voiding dysfunction | 2.86% | 9.09% | Hysterectomy | NS | [21] |
| Length of hospital stay | NA | NA | Equal | NS | [20] |
| Mesh exposure | 7.89% | 0 | Hystero-preservation | NS | [21] |
| Dyspareunia | 6.25% | 6.25% | Equal | NS | [21] |
NS: Not significant, NA: Not available
Table 4.
Overall comparison between hysterectomy and hystero-preservation for pelvic organ prolapse[21]
| Hysterectomy | Hystero-preservation | Favor | Significant | |
|---|---|---|---|---|
| Recurrence rate | 4.23% | 6.92% | Hysterectomy | NS |
| Reoperation rate | 5% | 8.72% | Hysterectomy | Significant |
| Operative time (min) | 104 | 77.78 | Hystero-preservation | Significant |
| Blood loss (mL) | 177.89 | 115.18 | Hystero-preservation | Significant |
| Voiding dysfunction | 7.28% | 8.22% | Equal | NS |
| Duration of catheterization | NA | NA | Equal | NS |
| Length of hospital stay | NA | NA | Equal | NS |
| Mesh exposure | 12.5% | 6.57% | Hystero-preservation | NS |
| Dyspareunia | 4.7% | 3.68% | Equal | NS |
NS: Not significant, NA: Not available
Abdominal approach
Through abdominal approach, hysterectomy had less recurrence, reoperation rate, and less voiding dysfunction but more mesh exposure events than hystero-preservation. On the other hand, hystero-preservation showed significantly shorter operative time and less blood loss than hysterectomy [Table 1].
Laparoscopic approach
As for laparoscopic route, Campagna et al. compared laparoscopic sacral hysteropexy versus laparoscopic sacral colpopexy plus supracervical hysterectomy in a cohort study.[44] Patients in both groups showed high satisfaction for PRS. Hystero-preservation had significant shorter operative time, and less sexual disturbance and less voiding dysfunction without significant difference, as compared with hysterectomy [Table 2].
Table 2.
Comparison between hysterectomy and hystero-preservation via laparoscopic route for pelvic organ prolapse
| Laparoscopic route | Hysterectomy | Hystero-preservation | Favor | Significant | Reference |
|---|---|---|---|---|---|
| Reoperation rate (%) | 2% | 2% | Equal | NS | [44] |
| Operative time (min) | 150 | 120 | Hystero-preservation | Significant | [44] |
| Blood loss (mL) | 30 | 30 | Equal | NS | [44] |
| Voiding dysfunction (%) | 2.5% | 1.9% | Hystero-preservation | NS | [37] |
| Length of hospital stay (day) | 2 | 2 | Equal | NS | [44] |
| Sexual disturbance (%) | 3.7% | 1.9% | Hystero-preservation | NS | [37] |
NS: Not significant
Vaginal approach with native tissue or mesh
Regarding PRS via vaginal approach with native tissue (without mesh), hysterectomy showed lower recurrence rate and lower reoperation rate. On the contrary, hystero-preservation showed shorter operation time, less blood loss, and less voiding dysfunction [Table 3a].
Table 3a.
Comparison between hysterectomy and hystero-preservation via vaginal route with native tissue (no mesh) for pelvic organ prolapse
| Vaginal with native tissue | Hysterectomy | Hystero-preservation | Favor | Significant | Reference |
|---|---|---|---|---|---|
| Recurrence rate | 3.66% | 13.27% | Hysterectomy | Significant | [21] |
| Reoperation rate | 4.88% | 7.14% | Hysterectomy | NS | [21] |
| Operative time (min) | 77 | 51 | Hystero-preservation | Significant | [21] |
| Blood loss (mL) | 135 | 46 | Hystero-preservation | Significant | [21] |
| Visceral injury | 1.61% | 0 | Equal | NS | [21] |
| Voiding dysfunction | 12.66% | 4.17% | Hystero-preservation | NS | [21] |
| Length of hospital stay | NA | NA | Equal | NS | [20] |
| Dyspareunia | 5.13% | 5% | Equal | NS | [21] |
NS: Not Significant, NA: Not available
Surgical mesh is sometimes considered during PRS to reduce recurrent rate and increase surgical success rates. However, the US Food and Drug Administration had released public health notifications in 2008 and 2011, respectively, because of adverse events, especially the common occurrence of postoperative mesh erosion.[43,45] As experts still have different opinions on this issue, the risk–benefit profile of using surgical mesh remains debatable till now. Kato et al. and Iyer and Botros reported that the mesh complication rate can be further decreased by modification and improvement of these prostheses.[46,47] To compare hysterectomy and hystero-preservation procedure via vaginal route with mesh, hysterectomy showed lower recurrence rate and lower reoperation rate [Table 3b]. On the contrary, hystero-preservation showed shorter operation time, less blood loss, and shorter duration of catheterization and shorter hospital stay. Meanwhile, hystero-preservation had less mesh exposure and dyspareunia, though no significant difference [Table 3b].
Table 3b.
Comparison between hysterectomy and hystero-preservation via vaginal route with mesh for pelvic organ prolapse
| Vaginal with mesh | Hysterectomy | Hystero-preservation | Favor | Significant | Reference |
|---|---|---|---|---|---|
| Recurrence rate | 2.02% | 4.85% | Hysterectomy | NS | [21] |
| Reoperation rate | 2.02% | 4.85% | Hysterectomy | NS | [21] |
| Operative time (min) | 125.31 | 90.21 | Hystero-preservation | Significant | [21] |
| Blood loss (mL) | 126.9 | 48.8 | Hystero-preservation | Significant | [21] |
| Voiding dysfunction | 0 | 0 | Equal | NS | [21] |
| Duration of catheterization (day) | 2.7 | 2.4 | Hystero-preservation | Significant | [21] |
| Length of hospital stay (day) | 4.2-7.6 | 1.5-7.7 | Hystero-preservation | Significant | [21] |
| Mesh exposure | 14.29% | 8.74% | Hystero-preservation | NS | [21] |
| Recurrence rate | 2.02% | 4.85% | Hysterectomy | NS | [21] |
NS: Not significant
In summary, due to the lack of high-quality studies and solid data in the comparison between hysterectomy and hystero-preservation for PRS, most of the outcomes are with high bias, resulting in unconvincing and equivocal conclusions. General speaking, hysterectomy showed lower recurrence rate and lower reoperation rate [Table 4]. On the contrary, hystero-preservation showed shorter operation time, less blood loss, and mesh exposure [Table 4]. More studies are still needed to fully understand the advantages and disadvantages between hysterectomy and hystero-preservation in PRS. Nevertheless, the surgeons, as well as patients, may need to keep in mind the potential benefits and drawbacks in various approaches of PRS. Surgeons ought to offer sufficient information and suitable surgical intervention for POP women who are considering surgical options for POP.
CERVICAL PRESERVATION (SUBTOTAL HYSTERECTOMY) AS A PREVENTIVE PROCEDURE IN BENIGN HYSTERECTOMY
Total hysterectomy versus subtotal hysterectomy
When hysterectomy is planned to be performed in patients for benign uterine conditions besides POP, cervical preservation or not may become a concerned issue. Most of the studies comparing total hysterectomy (TH) and SH were conducted via abdominal approach. SH had less blood loss, shorter hospital stay, lower complication rates, shorter operating time, and earlier return to work or baseline activities.[48] On the other hand, TH had fewer cervical stump problems, and less postoperative urinary incontinence risks [Table 5]. Psychological outcome and sexual function improved postoperatively, especially dyspareunia, in both TH and SH, without significant difference.[49,50]
Table 5.
Comparison between total hysterectomy and subtotal hysterectomy with cervical preservation via abdominal approach
| TH | SH | Favor | Significant | Reference | |
|---|---|---|---|---|---|
| Blood loss (mL) | 418.7 | 336.7 | SH | Significant | [48] |
| 370.6 | 302.8 | SH | Significant | [50] | |
| Length of hospital stay | 4.6 | 4.2 | SH | NS | [50] |
| Operative time (min) | 84 | 74 | SH | Significant | [48] |
| 82.1 | 71.8 | SH | Significant | [50] | |
| Complication rates | 21.2% | 19.6% | SH | Significant | [48] |
| Return to normal activities (weeks) | 4.5 | 4.4 | Equal | NS | [50] |
| Sexual function | 9.4% | 8.3% | Equal | NS | [50] |
| Cervical stump problems | NA | 5%-22% | TH | N/A | [48] |
| 0.6% | 13.1% | TH | Significant | [50] | |
| Urinary incontinence | 24.4% | 22.3% | Equal | NS | [48] |
| 5.2% | 7.3% | TH | NS | [50] |
NS: Not significant, NA: Not available, TH: Total hysterectomy, SH: Sub TH
Nonetheless, a practical guideline from the French College of Gynecologists and Obstetricians (CNGOF) is still recommended to remove uterine cervix for hysterectomy, because of subsequent higher risk of cervical cancer and reoperations in cervix preservation.[51] Therefore, SH should be avoided in patients with potential risk or history of cervical dysplasia or cancer. Moreover, cervical stump syndromes, such as cervical bleeding and abnormal Pap smear, are also a concern though uncommon in SH.[48]
Laparoscopic hysterectomy versus laparoscopic subtotal hysterectomy
Literature about the pros and cons of cervical preservation via laparoscopic route is limited.[50,52] The presently available evidence showed shorter recovery time, hospital stay, and return to normal life in laparoscopic subtotal hysterectomy (LSH).[52] However, current studies could not support the benefit of sexual function and psychologic outcome by LSH due to limited researches. In the review by Nesbitt-Hawes, LSH showed less blood loss, operative time, and complication rates for LSH, as compared with laparoscopic hysterectomy without significant difference.[52] Similar to abdominal approach, subsequent higher risk of cervical malignancy still exists after LSH. Therefore, postoperative surveillance of cervical cancer remains mandatory. Furthermore, the potential cyclical bleeding, though only a few cases presented, should always be mentioned and well informed to a patient before undergoing LSH. The symptoms can be bothersome and unacceptable for some women. The American Association of Gynecologic Laparoscopists provided practice guidelines for intraoperative approach, including intraoperative considerations, outcomes, and complications of LSH for clinicians to refer to as practices.[53]
As the current surgical trend becomes more minimally invasive and conservative in consideration of not only organic but also physiologic reasons, surgeons as well as patients rather choose a preserving procedure than an invasive one such as hysterectomy.[54] In light of the clinical preference, better preventive treatments are required, especially for postoperation cervical bleeding and probable prolapse in the future.
CONCLUSION
Women nowadays tend to consider uterus-sparing surgery for POP based on the benefits, including reduced intraoperative blood loss, shorten operative time and hospital stay, and also positively affected self-esteem over female body image and sexuality. As a surgeon, the choice of appropriate procedure for the patients with POP depends on both the surgeon’s experience and skill on specific technique and the patient’s medical and surgical consideration for PRS, comorbidities, and expectation. After all, professional opinions are still the most important factors that affect patients’ decision-making toward hysterectomy.[55] With no inferiority of hystero-preservation in overall outcome and symptom improvement, surgeons should not neglect the patients’ expectation of uterine-sparing. Uterus-sparing surgery, if feasible and suitable for the patients, should be considered for PRS to perform for better QoL. Ultimately, further long-term follow-up studies are still needed to clarify the complications of hystero-preservation, as compared with hysterectomy, for ideal alternatives for PRS choices.
Financial support and sponsorship
Nil.
Conflicts of interest
Prof. Ming-Ping Wu, an editorial board member at Gynecology and Minimally Invasive Therapy, had no role in the peer review process of or decision to publish this article. The other authors declared no conflicts of interest in writing this paper.
REFERENCES
- 1.Hall CM, Brody LT. 2nd ed. Philadelphia: Lippincott Williams &Wilkins; 2005. Therapeutic Exercise:Moving Toward Function. [Google Scholar]
- 2.Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010:A systematic analysis for the global burden of disease study 2010. Lancet. 2012;380:2163–96. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barber MD. Pelvic organ prolapse. BMJ. 2016;354:i3853. doi: 10.1136/bmj.i3853. [DOI] [PubMed] [Google Scholar]
- 4.Vergeldt TF, Weemhoff M, IntHout J, Kluivers KB. Risk factors for pelvic organ prolapse and its recurrence:A systematic review. Int Urogynecol J. 2015;26:1559–73. doi: 10.1007/s00192-015-2695-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu JM, Vaughan CP, Goode PS, Redden DT, Burgio KL, Richter HE, et al. Prevalence and trends of symptomatic pelvic floor disorders in U. S. women. Obstet Gynecol. 2014;123:141–8. doi: 10.1097/AOG.0000000000000057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lin YL, Lo TS, Long CY, Law KS, Ho CH, Wu MP. Time-frame comparison of hystero-preservation in the surgical treatment of uterine prolapse:A population-based nation-wide follow-up descriptive study, 2006-2013 versus 1997-2005. Int Urogynecol J. 2020;31:1839–50. doi: 10.1007/s00192-019-04128-z. [DOI] [PubMed] [Google Scholar]
- 7.Hong MK, Ding DC. Current treatments for female pelvic floor dysfunctions. Gynecol Minim Invasive Ther. 2019;8:143–8. doi: 10.4103/GMIT.GMIT_7_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu MP, Wu CJ, Weng SF. The choice of reoperation after primary surgeries for uterine prolapse:A nationwide study. Gynecol Minim Invasive Ther. 2015;4:120–5. [Google Scholar]
- 9.Jelovsek JE, Maher C, Barber MD. Pelvic organ prolapse. Lancet. 2007;369:1027–38. doi: 10.1016/S0140-6736(07)60462-0. [DOI] [PubMed] [Google Scholar]
- 10.Hagen S, Stark D. Conservative prevention and management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2011;12:CD003882. doi: 10.1002/14651858.CD003882.pub4. [DOI] [PubMed] [Google Scholar]
- 11.Wiegersma M, Panman CM, Kollen BJ, Berger MY, Lisman-Van Leeuwen Y, Dekker JH. Effect of pelvic floor muscle training compared with watchful waiting in older women with symptomatic mild pelvic organ prolapse:Randomised controlled trial in primary care. BMJ. 2014;349:g7378. doi: 10.1136/bmj.g7378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hagen S, Stark D, Glazener C, Dickson S, Barry S, Elders A, et al. Individualised pelvic floor muscle training in women with pelvic organ prolapse (POPPY):A multicentre randomised controlled trial. Lancet. 2014;383:796–806. doi: 10.1016/S0140-6736(13)61977-7. [DOI] [PubMed] [Google Scholar]
- 13.Liu YJ, Ting SW, Hsiao SM, Huang CM, Wu WY. Efficacy of bio-assisted pelvic floor muscle training in women with pelvic floor dysfunction. Eur J Obstet Gynecol Reprod Biol. 2020;251:206–11. doi: 10.1016/j.ejogrb.2020.04.050. [DOI] [PubMed] [Google Scholar]
- 14.Gu X, Yang M, Liu F, Liu D, Shi F. Effects of adding ultrasound biofeedback to individualized pelvic floor muscle training on extensibility of the pelvic floor muscle and anterior pelvic organ prolapse in postmenopausal women. Contrast Media Mol Imaging. 2022;2022:4818011. doi: 10.1155/2022/4818011. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 15.Gambacciani M, Palacios S. Laser therapy for the restoration of vaginal function. Maturitas. 2017;99:10–5. doi: 10.1016/j.maturitas.2017.01.012. [DOI] [PubMed] [Google Scholar]
- 16.Setyaningrum T, Tjokroprawiro BA, Listiawan MY, Santoso B, Prakoeswa CR. Treating vaginal relaxation syndrome using erbium:Yttrium aluminum garnet fractional laser:A retrospective study. Gynecol Minim Invasive Ther. 2022;11:23–7. doi: 10.4103/GMIT.GMIT_141_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mackova K, Van Daele L, Page AS, Geraerts I, Krofta L, Deprest J. Laser therapy for urinary incontinence and pelvic organ prolapse:A systematic review. BJOG. 2020;127:1338–46. doi: 10.1111/1471-0528.16273. [DOI] [PubMed] [Google Scholar]
- 18.Verbeek M, Hayward L. Pelvic floor dysfunction and its effect on quality of sexual life. Sex Med Rev. 2019;7:559–64. doi: 10.1016/j.sxmr.2019.05.007. [DOI] [PubMed] [Google Scholar]
- 19.Haj-Yahya R, Chill HH, Levin G, Reuveni-Salzman A, Shveiky D. Laparoscopic uterosacral ligament hysteropexy versus total vaginal hysterectomy with uterosacral ligament suspension for anterior and apical prolapse:Surgical outcome and patient satisfaction. J Minim Invasive Gynecol. 2020;27:88–93. doi: 10.1016/j.jmig.2019.02.012. [DOI] [PubMed] [Google Scholar]
- 20.Meriwether KV, Antosh DD, Olivera CK, Kim-Fine S, Balk EM, Murphy M, et al. Uterine preservation versus hysterectomy in pelvic organ prolapse surgery:A systematic review with meta-analysis and clinical practice guidelines. Am J Obstet Gynecol. 2018;219:129–46.e2. doi: 10.1016/j.ajog.2018.01.018. [DOI] [PubMed] [Google Scholar]
- 21.de Oliveira SA, Fonseca MC, Bortolini MA, Girão MJ, Roque MT, Castro RA. Hysteropreservation versus hysterectomy in the surgical treatment of uterine prolapse:Systematic review and meta-analysis. Int Urogynecol J. 2017;28:1617–30. doi: 10.1007/s00192-017-3433-1. [DOI] [PubMed] [Google Scholar]
- 22.He L, Feng D, Zha X, Liao XY, Gong ZL, Gu DQ, et al. Hysteropreservation versus hysterectomy in uterine prolapse surgery:A systematic review and meta-analysis. Int Urogynecol J. 2022;33:1917–25. doi: 10.1007/s00192-021-04913-9. [DOI] [PubMed] [Google Scholar]
- 23.Gutman R, Maher C. Uterine-preserving POP surgery. Int Urogynecol J. 2013;24:1803–13. doi: 10.1007/s00192-013-2171-2. [DOI] [PubMed] [Google Scholar]
- 24.Ridgeway BM. Does prolapse equal hysterectomy?The role of uterine conservation in women with uterovaginal prolapse. Am J Obstet Gynecol. 2015;213:802–9. doi: 10.1016/j.ajog.2015.07.035. [DOI] [PubMed] [Google Scholar]
- 25.Kudish BI, Shveiky D, Gutman RE, Jacoby V, Sokol AI, Rodabough R, et al. Hysterectomy and urinary incontinence in postmenopausal women. Int Urogynecol J. 2014;25:1523–31. doi: 10.1007/s00192-014-2422-x. [DOI] [PubMed] [Google Scholar]
- 26.van der Ploeg JM, van der Steen A, Zwolsman S, van der Vaart CH, Roovers J. Prolapse surgery with or without incontinence procedure:A systematic review and meta-analysis. BJOG. 2018;125:289–97. doi: 10.1111/1471-0528.14943. [DOI] [PubMed] [Google Scholar]
- 27.Obut M, Oğlak SC, Akgöl S. Comparison of the quality of life and female sexual function following laparoscopic pectopexy and laparoscopic sacrohysteropexy in apical prolapse patients. Gynecol Minim Invasive Ther. 2021;10:96–103. doi: 10.4103/GMIT.GMIT_67_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Korbly NB, Kassis NC, Good MM, Richardson ML, Book NM, Yip S, et al. Patient preferences for uterine preservation and hysterectomy in women with pelvic organ prolapse. Am J Obstet Gynecol. 2013;209:470.e1–6. doi: 10.1016/j.ajog.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 29.Wu MP, Long CY, Huang KH, Chu CC, Liang CC, Tang CH. Changing trends of surgical approaches for uterine prolapse:An 11-year population-based nationwide descriptive study. Int Urogynecol J. 2012;23:865–72. doi: 10.1007/s00192-011-1647-1. [DOI] [PubMed] [Google Scholar]
- 30.Laughlin-Tommaso SK, Satish A, Khan Z, Smith CY, Rocca WA, Stewart EA. Long-term risk of de novo mental health conditions after hysterectomy with ovarian conservation:A cohort study. Menopause. 2020;27:33–42. doi: 10.1097/GME.0000000000001415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lyatoshinsky P, Fünfgeld C, Popov A, Bezhenar V, Krutova V, Ulrich D, et al. Pelvic organ prolapse patients'attitudes and preferences regarding their uterus:Comparing German and Russian-speaking women. Int Urogynecol J. 2019;30:2077–83. doi: 10.1007/s00192-019-03918-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jeng CJ, Yang YC, Tzeng CR, Shen J, Wang LR. Sexual functioning after vaginal hysterectomy or transvaginal sacrospinous uterine suspension for uterine prolapse:A comparison. J Reprod Med. 2005;50:669–74. [PubMed] [Google Scholar]
- 33.Anglim B, O'Sullivan O, O'Reilly B. How do patients and surgeons decide on uterine preservation or hysterectomy in apical prolapse? Int Urogynecol J. 2018;29:1075–9. doi: 10.1007/s00192-018-3685-4. [DOI] [PubMed] [Google Scholar]
- 34.Jha S, Moran P. The UK national prolapse survey:5 years on. Int Urogynecol J. 2011;22:517–28. doi: 10.1007/s00192-011-1379-2. [DOI] [PubMed] [Google Scholar]
- 35.Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Brown J. Surgery for women with apical vaginal prolapse. Cochrane Database Syst Rev. 2016;10:CD012376. doi: 10.1002/14651858.CD012376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gabriel I, Kalousdian A, Brito LG, Abdalian T, Vitonis AF, Minassian VA. Pelvic organ prolapse after 3 modes of hysterectomy:Long-term follow-up. Am J Obstet Gynecol. 2021;224:496.e1–10. doi: 10.1016/j.ajog.2020.11.008. [DOI] [PubMed] [Google Scholar]
- 37.Illiano E, Giannitsas K, Costantini E. Comparison between laparoscopic sacrocolpopexy with hysterectomy and hysteropexy in advanced urogenital prolapse. Int Urogynecol J. 2020;31:2069–74. doi: 10.1007/s00192-020-04260-1. [DOI] [PubMed] [Google Scholar]
- 38.Detollenaere RJ, den Boon J, Stekelenburg J, IntHout J, Vierhout ME, Kluivers KB, et al. Sacrospinous hysteropexy versus vaginal hysterectomy with suspension of the uterosacral ligaments in women with uterine prolapse stage 2 or higher:Multicentre randomised non-inferiority trial. BMJ. 2015;351:h3717. doi: 10.1136/bmj.h3717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dallas K, Elliott CS, Syan R, Sohlberg E, Enemchukwu E, Rogo-Gupta L. Association between concomitant hysterectomy and repeat surgery for pelvic organ prolapse repair in a cohort of nearly 100,000 women. Obstet Gynecol. 2018;132:1328–36. doi: 10.1097/AOG.0000000000002913. [DOI] [PubMed] [Google Scholar]
- 40.Azadi A, Marchand G, Masoud AT, Sainz K, Govindan M, Ware K, et al. Complications and objective outcomes of uterine preserving surgeries for the repair of pelvic organ prolapse versus procedures removing the Uterus, a systematic review. Eur J Obstet Gynecol Reprod Biol. 2021;267:90–8. doi: 10.1016/j.ejogrb.2021.10.020. [DOI] [PubMed] [Google Scholar]
- 41.Cengiz H, Yildiz S, Alay I, Kaya C, Eren E, Iliman DE. Vaginal-assisted laparoscopic sacrohysteropexy and vaginal hysterectomy with vaginal vault suspension for advanced uterine prolapse:12-month preliminary results of a randomized controlled study. Gynecol Minim Invasive Ther. 2021;10:30–6. doi: 10.4103/GMIT.GMIT_126_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kotani Y, Murakamsi K, Kai S, Yahata T, Kanto A, Matsumura N. Comparison of surgical results and postoperative recurrence rates by laparoscopic sacrocolpopexy with other surgical procedures for managing pelvic organ prolapse. Gynecol Minim Invasive Ther. 2021;10:221–5. doi: 10.4103/GMIT.GMIT_127_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schimpf MO, Abed H, Sanses T, White AB, Lowenstein L, Ward RM, et al. Graft and mesh use in transvaginal Prolapse repair:A systematic review. Obstet Gynecol. 2016;128:81–91. doi: 10.1097/AOG.0000000000001451. [DOI] [PubMed] [Google Scholar]
- 44.Campagna G, Vacca L, Panico G, Rumolo V, Caramazza D, Lombisani A, et al. Laparoscopic sacral hysteropexy versus laparoscopic sacral colpopexy plus supracervical hysterectomy in patients with pelvic organ prolapse. Int Urogynecol J. 2022;33:359–68. doi: 10.1007/s00192-021-04865-0. [DOI] [PubMed] [Google Scholar]
- 45.Glazener CM, Breeman S, Elders A, Hemming C, Cooper KG, Freeman RM, et al. Mesh, graft, or standard repair for women having primary transvaginal anterior or posterior compartment prolapse surgery:Two parallel-group, multicentre, randomised, controlled trials (PROSPECT) Lancet. 2017;389:381–92. doi: 10.1016/S0140-6736(16)31596-3. [DOI] [PubMed] [Google Scholar]
- 46.Kato K, Suzuki S, Ishiyama A, Kawanishi H, Matsui H, Kato T, et al. Mesh exposure after transvaginal mesh prolapse surgery:Out of permissible range? Int J Urol. 2021;28:202–7. doi: 10.1111/iju.14425. [DOI] [PubMed] [Google Scholar]
- 47.Iyer S, Botros SM. Transvaginal mesh:A historical review and update of the current state of affairs in the United States. Int Urogynecol J. 2017;28:527–35. doi: 10.1007/s00192-016-3092-7. [DOI] [PubMed] [Google Scholar]
- 48.Gimbel H. Total or subtotal hysterectomy for benign uterine diseases?A meta-analysis. Acta Obstet Gynecol Scand. 2007;86:133–44. doi: 10.1080/00016340601024716. [DOI] [PubMed] [Google Scholar]
- 49.Persson P, Brynhildsen J, Kjølhede P. Hysterectomy Multicentre Study Group in South-East Sweden. A 1-year follow up of psychological wellbeing after subtotal and total hysterectomy a randomised study. BJOG. 2010;117:479–87. doi: 10.1111/j.1471-0528.2009.02467.x. [DOI] [PubMed] [Google Scholar]
- 50.Lethaby A, Mukhopadhyay A, Naik R. Total versus subtotal hysterectomy for benign gynaecological conditions. Cochrane Database Syst Rev. 2012;4:CD004993. doi: 10.1002/14651858.CD004993.pub3. [DOI] [PubMed] [Google Scholar]
- 51.Millet P, Gauthier T, Vieillefosse S, Dewaele P, Rivain AL, Legendre G, et al. Should we perform cervix removal during hysterectomy for benign uterine disease?Clinical practice guidelines from the French college of gynecologists and obstetricians (CNGOF) J Gynecol Obstet Hum Reprod. 2021;50:102134. doi: 10.1016/j.jogoh.2021.102134. [DOI] [PubMed] [Google Scholar]
- 52.Nesbitt-Hawes EM, Maley PE, Won HR, Law KS, Zhang CS, Lyons SD, et al. Laparoscopic subtotal hysterectomy:Evidence and techniques. J Minim Invasive Gynecol. 2013;20:424–34. doi: 10.1016/j.jmig.2013.01.009. [DOI] [PubMed] [Google Scholar]
- 53.American Association of Gynecologic Laparoscopists. AAGL practice report:Practice guidelines for laparoscopic subtotal/supracervical hysterectomy (LSH) J Minim Invasive Gynecol. 2014;21:9–16. doi: 10.1016/j.jmig.2013.08.001. [DOI] [PubMed] [Google Scholar]
- 54.Wu MP, Huang KH, Long CY, Tsai EM, Tang CH. Trends in various types of surgery for hysterectomy and distribution by patient age, surgeon age, and hospital accreditation:10-year population-based study in Taiwan. J Minim Invasive Gynecol. 2010;17:612–9. doi: 10.1016/j.jmig.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 55.Urdzík P, Kalis V, Blaganje M, Rusavy Z, Smazinka M, Havir M, et al. Pelvic organ prolapse and uterine preservation:A survey of female gynecologists (POP-UP survey) BMC Womens Health. 2020;20:241. doi: 10.1186/s12905-020-01105-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


