Abstract
Objectives
We describe an automated transcription system that addresses many documentation problems and fits within scheduled clinical hours.
Materials and methods
During visits, the provider listens to the patient while maintaining eye contact and making brief notes on paper. Immediately after the visit conclusion and before the next, the provider makes a short voice recording on a smartphone which is transmitted to the system. The system uses a public domain general language model, and a hypertuned provider-specific language model that is iteratively refined as each produced note is edited by the physician, followed by final automated processing steps to add any templated text to the note.
Results
The provider leaves the clinic having completed all voice files, median duration 3.4 minutes. Created notes are formatted as preferred and are a median of 363 words (range 125-1175).
Discussion
This approach permits documentation to occur almost entirely within scheduled clinic hours, without copy-forward errors, and without interference with patient-provider interaction.
Conclusion
Though no documentation method is likely to appeal to all, this approach may appeal to many physicians and avoid many current problems with documentation.
Keywords: documentation, electronic health records, physicians
Background and significance
Documentation burden is an important contributor to clinician dissatisfaction and may lead physicians to reduce clinical time or retire early.1 Using commercial electronic health records (EHRs) to create notes contributes to this burden.2,3 Resulting notes are criticized for excessive length,4 high percentage of preserved content from one note to the next,5,6 inaccuracy,7,8 and declining quality.9 These problems are partly the result of efforts to speed note writing such as copy-forward and auto-populating templates.10 Use of scribes and voice-to-text technologies have been proposed to address these problems, but cost and privacy concerns limit scribe use,11 and speech recognition workflow in commercial EHRs has not been associated with a decline in documentation time.12–14 New approaches that incorporate multiple microphones and remote transcription, with proposed future replacement by artificial intelligence methods (“ambient clinical documentation”) are touted as possible future solutions.15
Objectives
We describe an automated transcription system (Elliott) we developed that one of us (T.P.), a primary care internal medicine physician, uses that addresses many current documentation problems, and fits within scheduled clinical hours.
Methods
Workflow
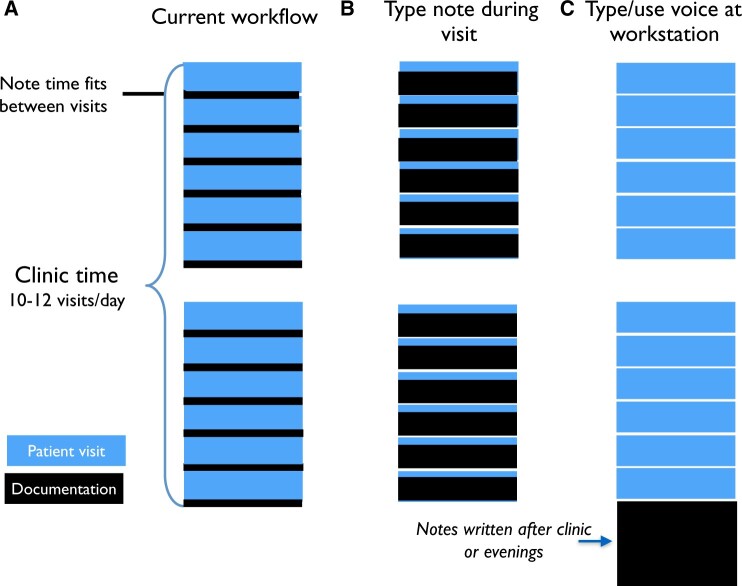
In the exam room, the provider faces and actively listens to the patient while maintaining eye contact and making brief notes on a blank piece of paper. Immediately after the visit conclusion and before seeing the next patient, while in the exam room or nearby, the provider makes a short voice recording on a smartphone (Figure 1), reading in relevant lab results, any outside records, and pertinent information. The recording is made where it is most convenient to do so and does not require the use of a workstation, special microphone, or office, saving the time required to walk to the workstation and back to the next exam room. Recordings do not contain protected health information and are identified by the time stamp and first 2 letters of the patient’s last name. At the end of the clinic day, these completed voice files for each visit which are then compressed, encrypted, and sent via ftp to Elliott.
Figure 1.
Workflow. Clinic schedule showing when documentation occurs relative to patient visits.
Technology
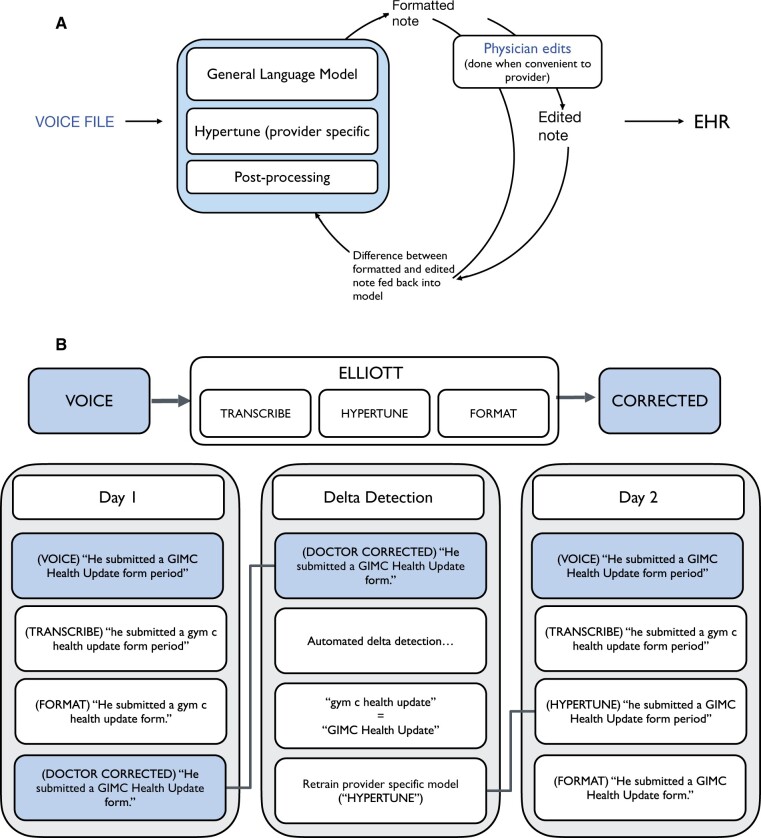
Elliott is speech-to-text software that attempts to fit the note and templating requirements to the doctor instead of the doctor to the template. It has two stages. The first stage (TRANSCRIBE) is an open-source speech-to-text model with some moderate tuning to medical vocabulary. The second stage is made up of a combination of preconfigured rules (FORMATTING) and a highly adaptable model (HYPERTUNE) to adapt the output of the global model to the preferred template of the provider. This idea is similar to how applications such as GitHub’s CoPilot quickly adapt to the nuances of the specific developer to generate code. The key difference here is instead of text generation (which can create realistic but fictitious text [“hallucinations”]), Elliott generates the template and formatting for the content provided by the doctor. To ensure accuracy a human reviews the output.
In the FORMATTING stage, the format of the note is refined and sections are put in the correct order. For example, if the voice file says, at the conclusion of the exam section “Please add to SOCIAL that the patient has a new job in high tech,” this will be added to the SOCIAL section in the correct order. Section headers are changed according to the physician’s preference (in my case, major headers such as EXAM are capitalized and bolded).
The note formatting produced by Elliott places the text in the appropriate sections (eg, PAST MEDICAL HISTORY, EXAM), the sections are placed in the correct order, section headers are formatted (all capitalized, bolded text), punctuation and capitalization of the text and headers accomplished, and required compliance text is added to the note. No EHR template is needed because Elliott provides the section and subsection headers in the correct location rather than requiring the physician to do this manually as is required when Nuance/Dragon is used in the EHR. Within hours, formatted notes in an encrypted file are sent to the provider to be reviewed. The output of Elliott—a completed, properly formatted note—is then pasted (Cntl-C, Cntl-V) into each patient’s EHR record as the clinic note. When the note is in the EHR, sometimes EHR dot phrases are used to enter current medications, vital signs, and the problem list.
Figure 2 shows Elliott’s design. Each note produced by Elliott is reviewed and edited by a physician before it is pasted into the EHR. The edited version is sent back to Elliott where it is compared with the note that Elliott produced. Differences—edits to spelling, correction of proper nouns such as a physician’s name or medication name—are called ‘deltas’ and are stored within Elliott. For example, early in the use of Elliott, the phrase “a bitter old” was corrected by the physician to “albuterol.” Once this was “learned” by Elliott, future corrections were not needed. The differences between the produced and edited notes (delta detection) are used to further tune the provider-specific language model. As a result, the system produces highly accurate, formatted notes that require little editing time by the physician.
Figure 2.
(A) Sequence of Elliott system steps in processing voice file to produce edited note that is placed into EHR. Elliott is iteratively tuned using differences between output of formatted note and note from physician edits. (B) Detail of Elliott architecture showing phonetic and formatting corrections. Delta detection finds differences between the General Language Model output and the formatted note after manual corrections by the physician.
Results
With the 142 most recent voice recordings, median duration is 3.4 minutes. It is always completed between scheduled patient visits. The provider leaves clinic having completed all voice files, and the next morning spends less than an hour for 10-20 notes finishing billing, administrative tasks (click on problem/med list review, enter “copy to” providers), and pasting in completed notes. Created notes (Figure 3) are formatted as preferred and are a median of 363 words (n = 393, range 125-1175). As Figure 4 shows, there is a broad range of note length.
Figure 3.
Example note (deidentified) produced using system described. Three asterisks indicate where patient data may optionally be inserted using a “dot phrase” when note is copied into EHR.
Figure 4.
Histogram of length of notes created using Elliott. Median length is 363 words.
To demonstrate the effect and speed of adaptation of the provider-specific stage of Elliott, we randomly sampled 100 notes to be the test dataset and randomly partitioned the rest of the notes to be the “training” dataset in batches of 11 (a typical number of notes generated in each clinic visit). Figure 5 shows the improvement in the average number of fewer corrections needed (removal/addition/replacements of words) with each additional training dataset batch.
Figure 5.
Effect of iterative training on need for manual edits. Y-axis is the average number of corrected words introduced by the second layer of Elliott (“HYPERTUNE”) on the test dataset. X-axis is the number of training notes. Note the speed at which Elliott adapts to the provider; with only 11 notes it achieves an appreciable difference in quality.
Discussion
The process for creating clinic notes should result in accurate, complete, concise notes, finished during scheduled clinic time, and should not impair physician-patient experience during a visit. Physicians should be proud, or at least satisfied, with the notes they create; as Deming observed, pride in workmanship is important.16 If we fall short of these objectives, we risk adding to patient dissatisfaction and physician burnout. After-hours EHR work, including documentation, is an important contributor to burnout17—spending more than 60 minutes in after-hours clerical work further increases burnout risk.18 The note-writing method described here achieves these objectives because it permits connection with the patient during the visit,19 permits recording the content of the note early to avoid forgetting pertinent details, and avoids after-hours documentation work. The completed notes are nicely formatted and have a professional appearance, which is important to clinicians.20 By reading relevant lab results, we avoid using EHR macros that lengthen notes with long lists of irrelevant results Copying forward notes is not needed, and so the risks of this process, including inaccuracy, are avoided.
How is this different from using Siri or Nuance/Dragon to create text? Both of these are commonly used. However, these technologies convert voice to text but stop there. It’s up to the physician to fit that text into the proper location for a medical note within an EHR template. This process takes time. Sometimes an EHR template is used and the Dragon output is placed within the template by bringing up the template (this requires logging in to a workstation and using a microphone), placing the cursor in the correct section in the template, then speaking so that the created text appears in the correct location. These additional steps mean the process of creating a note extends beyond what can reasonably be fit between patient-scheduled visits. A common sight is physicians using Dragon at a workstation for one note after another at the end of the clinic. In addition, though Nuance/Dragon is remarkably accurate with standard words and medical terms, it leaves it to the physician to correct phrases and words they use that other clinicians do not, for example, names of other physicians and hospitals. It takes a “one-size-fits-all approach” whereas Elliott’s second layer is tailored to the individual, also with remarkable accuracy and achieves this while training itself using corrected notes. Thus, Elliott automates almost all of this scut work.
The frustration and sense of resignation experienced by doctors today with regards to note documentation has little to do with their abilities or the limits of technology. It is simply that current design thinking about the interaction between the health record and the provider has the side effect of forcing the provider to adapt their thinking to the template, instead of the other way around. This cognitive burden, along with the extra clicks required to make note edits and have consistent formatting in a visually pleasing manner, is a major reason many doctors feel frustrated with writing notes.
With Elliott, the physician creates text with rough indications of what the sections are and Elliott converts that into a finished note. No template is needed; it is not necessary to log in to a workstation. The template is fitted to the content, not the other way around. This critical difference means that this can be done easily between patient visits. Corrections and edits are fewer and faster each clinic day because Elliott learns from past edits.
How is our approach different than dictation? Dictation is extremely useful for many physicians and is their preferred method. However, it doesn’t learn from prior notes. It isn’t continuously improving. And the turnaround time means that the dictation process may delay the availability of the note. There is also a cost for transcription that may be a barrier. Table 1 summarizes these differences.
Table 1.
Differences between current method, dictation, commercial EHR voice to text, and typing in the exam room during the visit.
| Current method | Dictation | EHR voice recognition | Type during visit | |
|---|---|---|---|---|
| Full attention devoted to patient during visit |

|

|

|
|
| Turnaround time | Hours | Days | Hours | Minutes |
| Documentation accomplished between patients during clinic |

|

|

|

|
| Not tied to workstation |

|

|
||
| Automatic formatting, grammar correction, spell checking |

|
Possibly | ||
| Improves accuracy over time |

|
Most important is that physician time devoted to documentation is short enough to fit between scheduled patient visits. The physician does not need fit the note content into an EHR template and so is not tied to a workstation, which reduces unnecessary travel time from the exam room and repetitive workstation login and reduces likelihood the physician will forget key details of the patient’s history which may occur if the note is created later. Because recordings occur between visits, notes don’t “pile up” until the end of the workday.
Most importantly the workflow does not interfere with the human connection so crucial to preventing burnout.21,22 Reduced eye contact while typing during a visit may impair the physician-patient relationship during the visit.23–27 There is evidence that patients are less active participants in consultations in which physicians engage in more keyboard activity.28 Nevertheless, some physicians may use workflows that also maintain human connection despite being different from ours.
No single documentation method will appeal to all physicians because habits, aptitudes such as typing speed, practice composition, and workflow vary widely.29,30 However, the workflow described here, with patients scheduled every few minutes, and the provider moves from one room to the next, is common. The Elliott tool could be used in other workflows, for example in an urgent care clinic, hospital rounding, or the emergency room. The ambulatory care workflow used in this report is common: Patients every 10-30 minutes and the provider moves from one room to the next. Our approach is inexpensive, does not require a scribe nor room microphones. Ambient dictation may raise privacy concerns for some patients because it is not clear where recordings travel and are stored.31 Moreover, the thinking of the physician that appears in the note Assessment section may not be part of the digital scribe recording. Ambient dictation may require infrastructure and expense not available to many physicians.
Disadvantages to our approach include that it is not directly supported by EHR vendors (recommendation 3 of the 25 × 5 report addresses this need32) and so at present is manually pasted into the EHR record. Prompts provided by EHR-based template tips aren’t seen, and turnaround time may be longer than other methods. And yet—though clinic days are busy and intense, the author (T.P.) is not burned out and documentation does not contribute to stress. If it works for this author (T.P.), perhaps it may help others.
Acknowledgments
This work was presented in part at the 2020 American College of Medical Informatics Winter Symposium. We thank Stella Dull for assistance with data analysis.
Contributor Information
Thomas H Payne, Department of Medicine, University of Washington School of Medicine, Seattle, WA 98104-2499, United States; Department of Biomedical Informatics & Medical Education, University of Washington School of Medicine, Seattle, WA 98104-2499, United States.
Grace K Turner, Department of Biomedical Informatics & Medical Education, University of Washington School of Medicine, Seattle, WA 98104-2499, United States.
Author contributions
All authors have made substantial contributions to the conception or design of the work and in the acquisition, analysis, or interpretation of data for the work; in drafting the work and revising it critically for important intellectual content; have finally approved the version to be published; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflicts of interest
None declared.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
- 1. Friedberg MW, Chen PG, Van Busum KR, et al. Factors affecting physician professional satisfaction and their implications for patient care, health systems, and health policy. Rand Health Q. 2014. Winter;3(4):1. [PMC free article] [PubMed] [Google Scholar]
- 2. Sinsky C, Colligan L, Li L, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med. 2016;165(11):753-760. [DOI] [PubMed] [Google Scholar]
- 3. Jamoom E, Patel V, King J, Furukawa MF.. Physician experience with electronic health record systems that meet meaningful use criteria: NAMCS physician workflow survey, 2011. NCHS Data Brief. 2013;(129):1-8. [PubMed] [Google Scholar]
- 4. Rule A, Bedrick S, Chiang MF, Hribar MR.. Length and redundancy of outpatient progress notes across a decade at an academic medical center. JAMA Netw Open. 2021;4(7):e2115334. 10.1001/jamanetworkopen.2021.15334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Siegler EL, Adelman R.. Copy and paste: a remediable hazard of electronic health records. Am J Med. 2009;122(6):495-496. [DOI] [PubMed] [Google Scholar]
- 6. Hartzband P, Groopman J.. Off the record—avoiding the pitfalls of going electronic. N Engl J Med. 2008;358(16):1656-1658. 10.1056/NEJMp0802221 [DOI] [PubMed] [Google Scholar]
- 7. Hammond KW, Helbig ST, Benson CC, Brathwaite-Sketoe BM.. Are electronic medical records trustworthy? Observations on copying, pasting and duplication. AMIA Annu Symp Proc. 2003;2003:269-273. [PMC free article] [PubMed] [Google Scholar]
- 8. Yadav S, Kazanji N, K C N, et al. Comparison of accuracy of physical examination findings in initial progress notes between paper charts and a newly implemented electronic health record. J Am Med Inform Assoc. 2017;24(1):140-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Martin SA, Sinsky CA.. The map is not the territory: medical records and 21st century practice. Lancet. 2016;388(10055):2053-2056. 10.1016/S0140-6736(16)00338-X [DOI] [PubMed] [Google Scholar]
- 10. Flanagan ME, Militello LG, Rattray NA, Cottingham AH, Frankel RM.. The thrill is gone: Burdensome electronic documentation takes its toll on physicians’ time and attention. J Gen Intern Med. 2019;34(7):1096-1097. 10.1007/s11606-019-04898-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Walker KJ, Dunlop W, Liew D, et al. An economic evaluation of the costs of training a medical scribe to work in emergency medicine. Emerg Med J. 2016;33(12):865-869. 10.1136/emermed-2016-205934 [DOI] [PubMed] [Google Scholar]
- 12. Hodgson T, Magrabi F, Coiera E.. Evaluating the efficiency and safety of speech recognition within a commercial electronic health record system: a replication study. Appl Clin Inform. 2018;9(2):326-335. 10.1055/s-0038-1649509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dela Cruz JE, Shabosky JC, Albrecht M, et al. Typed versus voice recognition for data entry in electronic health records: emergency physician time use and interruptions. West J Emerg Med. 2014;15(4):541-547. 10.5811/westjem.2014.3.19658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Avendano JP, Gallagher DO, Hawes JD, et al. Interfacing with the electronic health record (her): a comparative review of modes of documentation. Cureus. 2022;14(6):e26330. 10.7759/cureus.26330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Nuance. Reduce documentation time with ambient intelligence. Accessed March 10, 2023. https://www.nuance.com/healthcare/campaign/ppc/nuance-dax-in-action/ambient-intelligence.html
- 16. Deming WE. Out of the Crisis. MIT Press; 2000. [1982]. [Google Scholar]
- 17. Hauer A, Waukau HJ, Welch P.. Physician burnout in Wisconsin: an alarming trend affecting physician wellness. WMJ. 2018;117(5):194-200. [PubMed] [Google Scholar]
- 18. Peccoralo LA, Kaplan CA, Pietrzak RH, Charney DS, Ripp JA.. The impact of time spent on the electronic health record after work and of clerical work on burnout among clinical faculty. J Am Med Inform Assoc. 2021;28(5):938-947. 10.1093/jamia/ocaa349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chen Y, Adler-Milstein J, Sinsky CA.. Measuring and maximizing undivided attention in the context of electronic health records. Appl Clin Inform. 2022;13(4):774-777. 10.1055/a-1892-1437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Payne TH, Patel R, Beahan S, Zehner J.. The physical attractiveness of electronic physician notes. AMIA Annu Symp Proc. 2010;2010:622-626. [PMC free article] [PubMed] [Google Scholar]
- 21. Shanafelt TD, Dyrbye LN, West CP.. Addressing physician burnout: the way forward. JAMA. 2017;317(9):901-902. 10.1001/jama.2017.0076 [DOI] [PubMed] [Google Scholar]
- 22. Haverfield MC, Tierney A, Schwartz R, et al. Can patient-provider interpersonal interventions achieve the quadruple aim of healthcare? A systematic review. J Gen Intern Med. 2020;35(7):2107-2117. 10.1007/s11606-019-05525-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Linder JA, Schnipper JL, Tsurikova R, Melnikas AJ, Volk LA, Middleton B.. Barriers to electronic health record use during patient visits. AMIA Annu Symp Proc. 2006;2006:499-503. [PMC free article] [PubMed] [Google Scholar]
- 24. Ratanawongsa N, Barton JL, Lyles CR, et al. Association between clinician computer use and communication with patients in Safety-Net clinics. JAMA Intern Med. 2016;176(1):125-128. 10.1001/jamainternmed.2015.6186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Toll E. The cost of technology. JAMA. 2012;307(23):2497-2498. [DOI] [PubMed] [Google Scholar]
- 26. Lanier C, Dominicé Dao M, Baer D, Haller DM, Sommer J, Junod Perron N.. How do patients want Us to use the computer during medical encounters?-a discrete choice experiment study. J Gen Intern Med. 2021;36(7):1875-1882. 10.1007/s11606-021-06753-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sinsky CA, Beasley JW.. Texting while doctoring. Ann Intern Med. 2014;160(8):584. 10.7326/L14-5008-9 [DOI] [PubMed] [Google Scholar]
- 28. Street RL Jr, Liu L, Farber NJ, et al. Keystrokes, mouse clicks, and gazing at the computer: How physician interaction with the EHR affects patient participation. J Gen Intern Med. 2018;33(4):423-428. 10.1007/s11606-017-4228-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kalava A, Ravindranath S, Bronshteyn I, Munjal RS, Schianodicola J, Yarmush JM.. Typing skills of physicians in training. J Grad Med Educ. 2014;6(1):155-157. 10.4300/JGME-D-13-00164.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Schuurman AR, Baarsma ME, Wiersinga WJ, Hovius JW.. Digital disparities among healthcare workers in typing speed between generations, genders, and medical specialties: cross sectional study. BMJ. 2022;379:e072784. 10.1136/bmj-2022-072784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Quiroz JC, Laranjo L, Kocaballi AB, Berkovsky S, Rezazadegan D, Coiera E.. Challenges of developing a digital scribe to reduce clinical documentation burden. NPJ Digit Med. 2019;2:114. 10.1038/s41746-019-0190-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hobensack M, Levy DR, Cato K, et al. 25 × 5 symposium to reduce documentation burden: report-out and call for action. Appl Clin Inform. 2022;13(2):439-446. 10.1055/s-0042-1746169 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.