Abstract
Background
In 2016, two Canadian hospitals participated in a quality improvement (QI) program, the International Acute Care for Elders (ACE) Collaborative, and sought to adapt and implement a transition coach intervention (TCI). Both hospitals were challenged to provide optimal continuity of care for an increasing number of older adults. The two hospitals received initial funding, coaching, educational materials, and tools to adapt the TCI to their local contexts, but the QI project teams achieved different results. We aimed to compare the implementation of the ACE TCI in these two Canadian hospitals to identify the factors influencing the adaptation of the intervention to the local contexts and to understand their different results.
Methods
We conducted a retrospective multiple case study, including documentary analysis, 21 semi-structured individual interviews, and two focus groups. We performed thematic analysis using a hybrid inductive-deductive approach.
Results
Both hospitals met initial organizational goals to varying degrees. Our qualitative analysis highlighted certain factors that were critical to the effective implementation and achievement of the QI project goals: the magnitude of changes and adaptations to the initial intervention; the organizational approaches to the QI project implementation, management, and monitoring; the organizational context; the change management strategies; the ongoing health system reform and organizational restructuring. Our study also identified other key factors for successful care transition QI projects: minimal adaptation to the original evidence-based intervention; use of a collaborative, bottom-up approach; use of a theoretical model to support sustainability; support from clinical and organizational leadership; a strong organizational culture for QI; access to timely quality measures; financial support; use of a knowledge management platform; and involvement of an integrated research team and expert guidance.
Conclusion
Many of the lessons learned and strategies identified from our analysis will help clinicians, managers, and policymakers better address the issues and challenges of adapting evidence-based innovations in care transitions for older adults to local contexts.
Keywords: care transition, frailty, older adults, transition coach, implementation evaluation, multiple case study, quality improvement collaborative
INTRODUCTION
Frail older Canadians have complex health and social needs.(1,2) Frailty is a common geriatric syndrome characterized by age-associated declines in physiologic reserve and function across multiple organ systems, leading to increased vulnerability for adverse health outcomes when exposed to endogenous or exogenous stressors.(2,3) Frail older adults are at high risk of hospitalization(2,4) and are more likely to experience organizational failures in access, integration and, especially, coordination and continuity of care.(2,5) In particular, care transitions are high-risk moments in the care continuum that expose frail older adults to avoidable adverse events, threatening their autonomy and lives.(6–8)
The Acute Care for Elders (ACE) program(9) is a widely recognized evidence-informed quality improvement care model that addresses the many issues facing older adults across the continuum of care. In 2010, Sinai Health in Toronto, Canada, developed a context-adapted ACE strategy guideline.(10) Their ACE strategy is a multicomponent intervention within the continuum of care to reduce functional decline, hospital readmissions, emergency room visits, functional disability, and long-term care (LTC) admissions. The ACE strategy includes 1) emergency department (ED) care components; 2) inpatient care components; and 3) community-based interventions.(10) To improve post-discharge care, inpatient care components include care transition interventions involving a “transition coach”—an advanced practice nurse who educates and helps hospitalized patients develop self-management skills.(11) After implementing the ACE strategy, Sinai Health significantly improved overall care quality, reduced inappropriate resource use, and lowered costs.(10)
In 2015, the Canadian Foundation for Health Improvement (CFHI) (now Healthcare Excellence Canada) partnered with the Canadian Frailty Network (CFN) and Sinai Health to launch the International Acute Care for Elders (ACE) Collaborative, a twelve-month quality improvement (QI) program to help implement effective practices leading to better patient outcomes. The CFHI-CFN-Sinai Health partnership provided 18 improvement teams (17 in Canada and 1 in Iceland) with funding (CAD $40,000), coaching, educational materials, and tools to adapt Sinai Health’s ACE strategy to their local contexts. Two francophone hospitals participated: Hôpital Montfort (HM) in Ottawa, Ontario, and Hôtel-Dieu de Lévis (HDL), in Lévis, Québec. Both hospitals aimed to improve their hospital-to-community care transitions for a growing frail elderly population. Both hospitals chose to implement a Transition Coach Intervention (TCI) based on Sinai Health’s ACE strategy. The HM team successfully implemented the TCI, introduced practice changes, and achieved positive organizational outcomes, while the HDL team experienced many challenges and failed to move beyond the pre-implementation phase.
One of the implementation barriers limiting the spread of evidence-based innovations is the difficulty of adapting knowledge tools (e.g., practice guidelines) to other cultural and organizational contexts.(6) How to effectively adapt the ACE strategy TCI component to different cultural and provincial contexts is still poorly understood. Although a previous study has been conducted to determine the effectiveness of the ACE strategy at Mount Sinai Hospital,(10) to our knowledge, no study has previously analyzed the process of adaptation and implementation of the TCI in other Canadian contexts. This study was also the first to be conducted in two francophone hospital settings which adds an additional challenge to translate knowledge implementation material from one language to another.
We aimed to compare the implementation of the ACE TCI in these two Canadian hospitals to identify the factors influencing the adaptation of the intervention to the local contexts and to understand their different results. This study provides a unique opportunity to learn more about the process of implementing and adapting the ACE TCI to different settings and cultural backgrounds.
METHODS
We conducted comparative analyses to highlight the strengths and weaknesses of each implementation process. We used a retrospective evaluation approach with a multiple case study design, following Yin’s methodology,(12) to identify factors influencing the TCI implementation and adaptation, and to understand the different outcomes in both contexts. According to Yin, case study methodology allows us to use multiple data sources, both qualitative and quantitative, to explore complex relationships between contexts, processes, and outcomes of interventions.(12) Sites selected represented two Canadian provinces with different health systems but many similar characteristics. Both hospitals 1) selected the same ACE TCI; 2) shared a common cultural and linguistic background; 3) were university-teaching hospitals; 4) received the same support and funding. The ethics committees of both hospitals approved our study. We used the Revised Standards for Quality Improvement Reporting Excellence (SQUIRE 2.0) to report our findings.(13)
Theoretical Framework
We used the Strategic Framework for a Useful and Used Evaluation(14) to analyze the following key elements: 1) stakeholders; 2) issues identified for different stages and levels (local, regional, provincial); 3) strategies for implementation and knowledge-sharing; and 4) contexts and environments that influenced the project’s implementation. This framework also analyzes the theoretical approaches, methods, and strategies tailored to complex projects.(14)
Data Collection and Analysis
We conducted 1) a documentary analysis (e.g., progress and final reports, CFHI documents); 2) semi-structured interviews until thematic saturation; and 3) two focus groups to validate interview findings. Documentary analysis helped document the project (history, context, actors, decisions, and outcomes), identify organizational and environmental factors, and better plan and understand interviews and focus groups.(12)
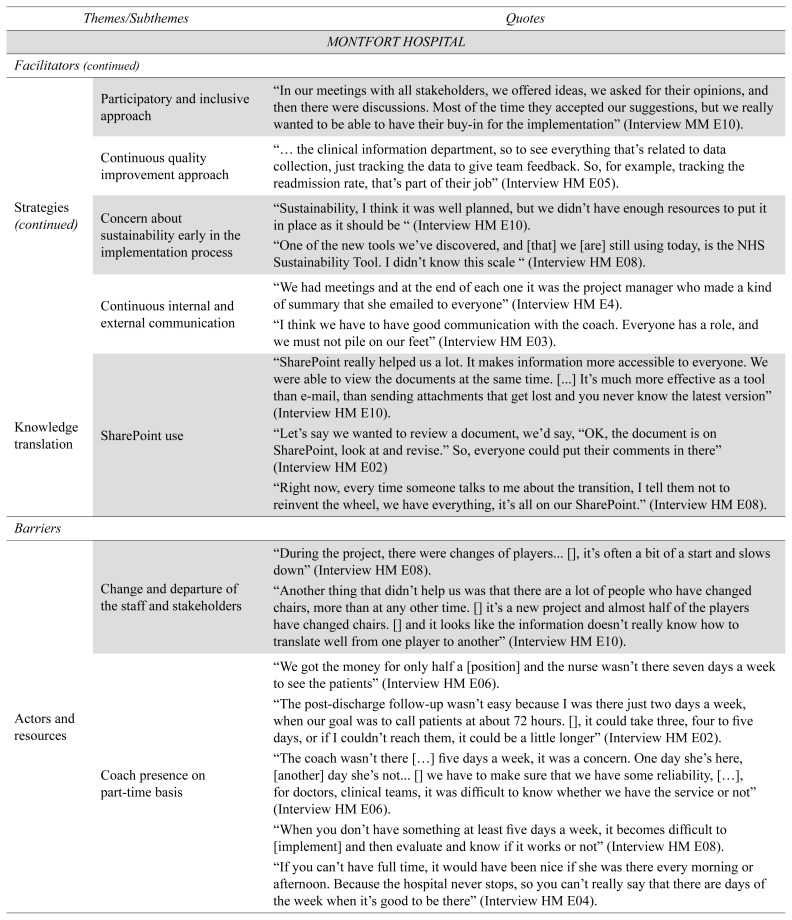
Quantitative data were obtained through documentary analysis. Both hospitals identified measures that allowed them to monitor activities and identify areas for improvement. HM selected 6 indicators, while HDL selected 3. Only the 30-day hospital readmission rate was common to both organizations (Table 1). Management teams, supported by the organization’s data analysis specialists, led the ongoing collection and analysis of field measurements.
Table 1.
ACE project organizational target achievement
| Organization | Measurement | Baseline Measures a | Target | Value Measured b c |
|---|---|---|---|---|
| Hôpital Montfort | Hospital readmission rate | 6% | 4.5% (reduction of 25%) | 3.42% (Mean) (43% Relative Risk Reduction) |
| Rate of compliance with the comparative review of drugs on discharge | 88.1% | 90% | N/Ad | |
| NRC Picker Surveye: Patients answering “YES” to the question as to whether “Families have sufficient information about recovery” | 52.5% | 60% | N/Ad | |
| Number of scheduled appointments with a family doctor or specialist | No baseline data (new measurement) | 100% | 88% | |
| Number of consultations with the Community Care Centre program (patients/month) | 3.6 | 7.2 | 4 (11% Relative Risk Increase) | |
| Patient satisfaction with their care transition (CTM-3f, Mean score) | No baseline data (new measurement) | > or = 3.5/5 | 3.8 | |
|
| ||||
| Hôtel-Dieu de Lévis (HDL) | Hospital readmission rate | 14% | 12% | 12% (14% Relative Risk Reduction) |
| Rate of emergency room visits within 30 days of hospital discharge | 22% | 20% | 20.5% (7% Relative Risk Reduction) | |
| Enrolling patients with a high risk of readmission to the telemonitoring service | No baseline data (new measurement) | 50% | 4% (1/24)g | |
Measured at baseline in 2015.
Value measured after the project started in 2016 or at the end of the ACE project in 2017.
Reported values represent absolute intervention effect and relative risk reductions (RRR) or increase (RRI) are presented in parentheses.
Missing data
NRC Picker Survey: National Research Corporation Picker Survey (https://nrchealth.com/)
CTM-3: Three-item Care Transition Measure (https://caretransitions.org/wp-content/uploads/2019/09/CTM-3.pdf)
Twenty-four patients agreed to participate in the ACE project and provide personal information (e.g., sociodemographic data), but only one person accepted the telemonitoring service.
We conducted qualitative interviews and focus groups with key stakeholders identified by each local ACE team leader, including clinicians, patient partners, and managers. We developed the interview guides based on our theoretical framework. Interviews and focus group discussions were recorded and transcribed verbatim. We simultaneously collected and analyzed the data using an iterative approach. This helped in refining our interview guide.
Two independent researchers (EKG and SB) performed thematic analysis according to Braun et al.(15) using Nvivo 12.0 (QSR International, Victoria, Australia). We used a hybrid inductive-deductive approach to identify themes based on our theoretical framework. The researchers developed a coding structure with themes based on the framework and refined it as new themes emerged.(12) We used a descriptive and interpretive approach to assign codes before grouping similar codes into broader themes and theme categories. Disagreements were resolved by discussion (EKG, SB, PA, LB).
RESULTS
Both sites adapted the ACE TCI based on their local contexts and various organizational goals.
Documentary Analysis Results
The documentary analysis allowed us to describe the context, document the QI project governance decisions and adjustments, access the reported quantitative data, and examine how each organization implemented the project. Documentation supporting this and all analyses is available on request.
ACE Transition Coach Intervention Adaptation to Local Contexts
The Director of Medicine, Rehabilitation, Geriatrics, Therapeutic Services, Palliative Care and Discharge Planning supported the project at HM. HM slightly modified the original intervention to fit the local context. The HM team hired an advanced practice nurse to serve as a transition coach. Her role focused on pre-discharge patient education, chronic disease self-management, and coordinating post-discharge follow-up. The intervention targeted people aged ≥65 years, scoring 3–7 on the Clinical Frailty Scale(16) scheduled for discharge from an acute medical unit to the community, and able to attend health and medication management education sessions. Patients discharged to a nursing home, rehabilitation unit, intensive care unit, psychiatric unit, or palliative care unit were excluded. The ACE project was integrated into Montfort’s Senior Friendly Hospital strategy and managed by two teams: (1) an implementation team responsible for the project’s local planning and implementation; and (2) a project management team.
At HDL, the ACE project was initiated by an embedded clinician researcher and supported by the Director of Nursing, the Chief Executive Officer, and the Director of the Support for Elderly Autonomy Program. The HDL team did not hire a transition coach. Discharge planning and coordination were already initiated by nurse discharge coordinators. Instead, the team offered patients access to a telemonitoring service managed by a nonprofit, community-based organization (Télésurveillance-Santé-Chaudière-Appalaches), in partnership with Info-Santé-811, a free province-wide telephone helpline. Telemonitoring connects older patients or their family members with a nurse for non-emergency health or social issues 24 hours a day, seven days a week for a monthly fee (CAD $25/month in 2017). To meet eligibility criteria for the telemonitoring service, the HDL intervention targeted patients aged 50 years and older, at high risk for 30-day hospital readmission determined by a modified LACE Index Score (7/12 or higher),(17) able to give consent or have a caregiver who could provide proxy consent. Patients were excluded if they did not speak French or English, or were transferred to a long-term care home or to palliative care.
Since 2013, HDL had been implementing Quebec’s Specialized Approach to Senior Hospital Care (SASHC), aiming to improve the quality of hospital care of older adults.(18) Quebec’s SASHC is heavily influenced by the ACE strategy and included seven objectives overlapping with Ontario’s Senior Friendly Hospital Strategy.(19) HDL’s ACE project was seen as another lever for Quebec’s SASHC and was managed through two subcommittees: (1) an executive committee responsible for designing and implementing the local ACE initiative; and (2) an extended committee involving hospital executives, managers, and advisors.
ACE Projects Comparative Organizational Target Achievements at Both Sites
Each hospital set measurable targets to assess the effectiveness of its respective TCI. Table 1 compares how the two hospitals achieved these targets.
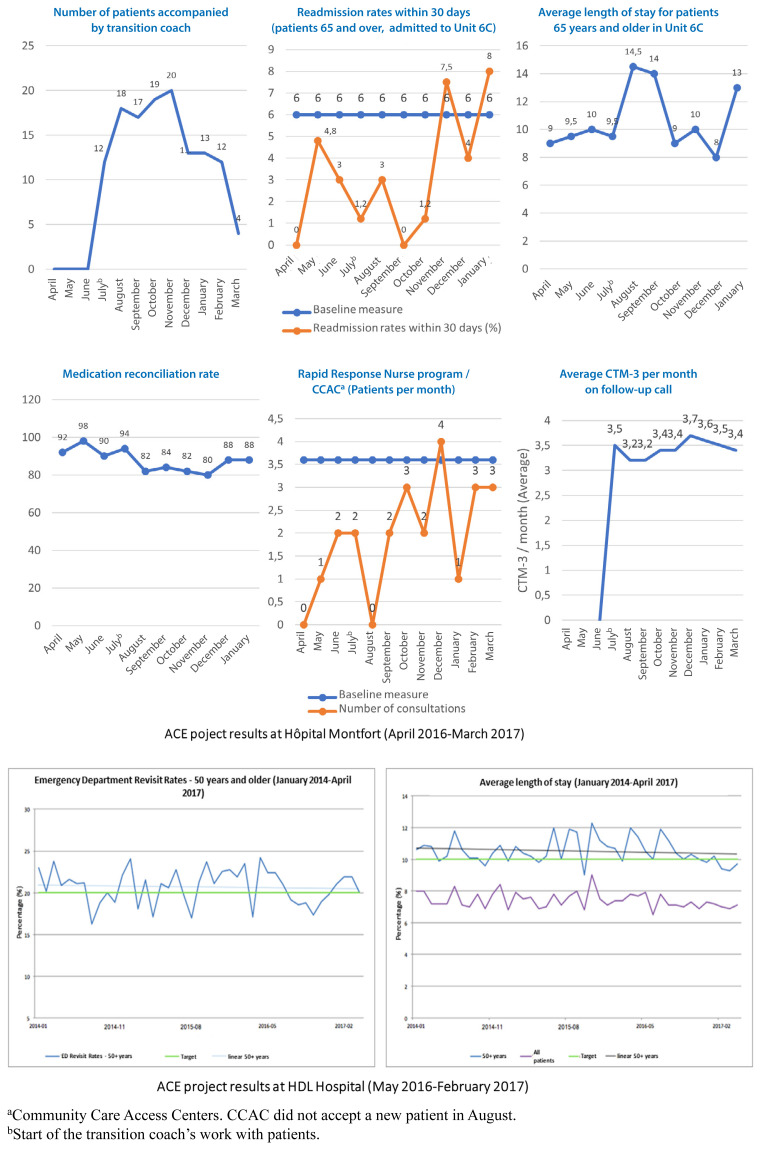
At HM, over a nine-month period (July 1, 2016, to March 31, 2017), the transition coach accompanied 128 patients (14.2 patients per month), whereas the initial goal was 20 patients per month. The transition coach dedicated the last month of the project (March 2017) to knowledge transfer activities to transfer her knowledge to the new discharge management team. HM met three of its six goals: reducing hospital readmission rates by 24%, reaching 88% of patients with a scheduled follow-up appointment with a family doctor or specialist, and exceeding its goal for patient satisfaction measured by the three-item Care Transition Measure (CTM-3) (mean score 3.8). The average length of stay for frail seniors in the care unit was stable. Medication reconciliation worsened; however, the small sample size analyzed does not allow for a robust analysis. The Transition Coach referred several patients to the Rapid Response Nurse Program—Community Care Access Centers (CCACs) (average of 2.6 patients/month). This service was almost unused before hiring the Transition Coach (average 0.9 patients/month, 2014–2015). The CTM-3 was used to monitor patient satisfaction after discharge. This self-report measure was administered by the coach during the follow-up call within 24–48 hours after discharge. The team achieved the CTM-3 target early and it remained stable until the end of the project. HDL achieved two of its three targets: reducing emergency department visits within 30 days of hospital discharge from 22% to 20.5% and hospital readmissions from 14% to 12%. Figure 1 summarizes the ACE project results.
FIGURE 1.
ACE Project Results at the Two Hospitals
aCommunity Care Access Centers. CCAC did not accept a new patient in August.
bStart of the transition coach’s work with patients.
Results of Qualitative Studies
The next sections summarize the characteristics of the participants interviewed, their initial expectations and perceptions, and the factors that contributed to the difference in achieving the two hospitals initial goals.
Participants Profile
A single interviewer conducted 13 semi-directed individual phone interviews with HM key informants (May–September 2018; length: 40 to 90 minutes); and eight semi-directed individual phone interviews with HDL key informants (November 2018–April 2019; length: 40 to 75 minutes). We also conducted a focus group in each hospital to validate our interview findings and to gather additional information. Table 2 summarizes the characteristics of key informants at both hospitals.
TABLE 2.
Individual interview and focus group participants’ characteristics
| Hôpital Montfort | Hôtel-Dieu de Lévis | |||
|---|---|---|---|---|
|
| ||||
| Individual interviews (N=13) | Focus group (N=10) | Individual interviews (N=8) | Focus group (N=9) | |
|
| ||||
| N (%) | N (%) | N (%) | N (%) | |
| Sex | ||||
| Male | 1 (8) | 1 (10) | 1 (12.5) | 1 (11) |
| Female | 12 (92) | 9 (90) | 7 (87) | 8 (89) |
|
| ||||
| Age | ||||
| 30–39 | 3 (23) | 2 (20) | 1 (12.5) | 1 (11) |
| 40–49 | 4 (30) | 4 (40) | 4 (50) | 4 (44) |
| 50–59 | 6 (46) | 4 (40) | 3 (37.5) | 4 (44) |
|
| ||||
| Occupation | ||||
| Health professionals | 6 (62) | 5 (50) | 2 (25) | 1 (11) |
| Physician | 1 (8) | 1 (10) | - | 1 (11) |
| Pharmacist | 1 (8) | - | - | |
| Advanced practice nurse | 2 (15) | 2 (20) | - | - |
| Registered nurse | 2 (15) | 2 (20) | 2 (25) | - |
| Researchers | - | - | 1 (12.5) | 1 (11) |
| Decision makers | 2 (15) | 2 (20) | 2 (25) | 3 (33) |
| Managers | 2 (15) | 2 (20) | 2 (25) | 3 (33) |
| Patient partners | 1 (8) | - | - | - |
| Others | 2 (15) | 1 (1) | - | - |
| Information technology specialist | 1(8) | 1 (10) | - | - |
| Administrative assistant | 1(8) | - | - | - |
|
| ||||
| Job Experience (years) | ||||
| Mean [min–max] | 18 [2.5–30] | 18.3 [2.5–30] | 21 [15–33] | 20.7 [15–33] |
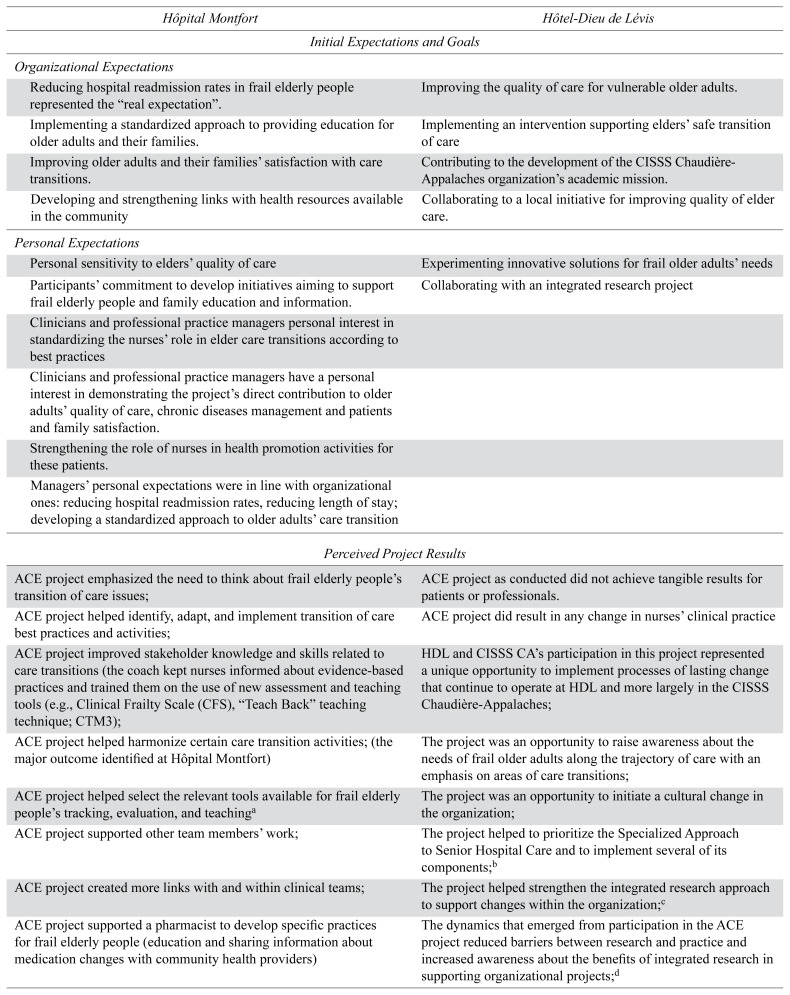
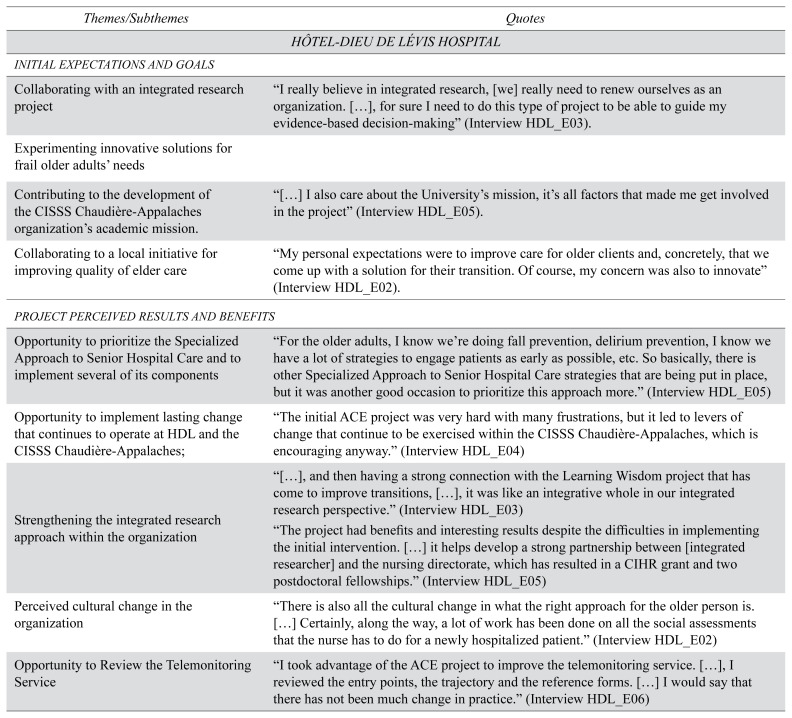
Initial Expectations and Perceived Results in Both Hospitals
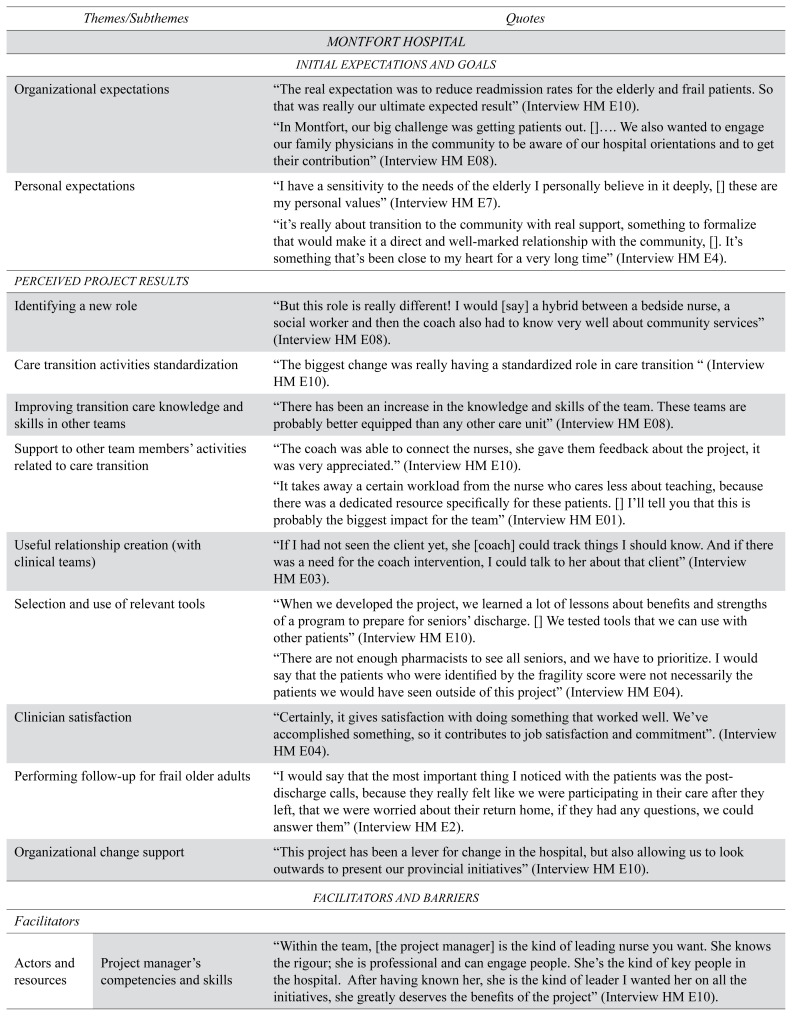
Main initial organizational expectations at both hospitals were implementing a standardized approach supporting safe transitions of care, improving the quality of care, and reducing hospital readmissions; improving elderly people and families’ satisfaction; and developing and strengthening links with community health resources. Actors were committed to developing QI initiatives to support older adults and families. At HM, clinicians expressed interest in strengthening the nurses’ role in elder care transitions. At HDL, participants wanted to collaborate on an integrated research project that was led by the senior author (PA) and the CISSS-CA Director of Nursing (JR) who proposed evidence-based strategies to assist decision makers in adapting and implementing the TCI.(6) Integrated research (a.k.a. embedded research) assumes that knowledge that is collected and generated in the field, through daily interaction and negotiation with clinicians, decision-makers and patients, provides better insight into the issues affecting these stakeholders, is more relevant to the local context, and is thus more easily translated into practice.(20,21) This is also the concept underlying the creation of Learning Health Systems, which was the basis for this project.(6) Appendix A summarizes both hospitals’ organizational and personal expectations and perceived ACE strategy results.
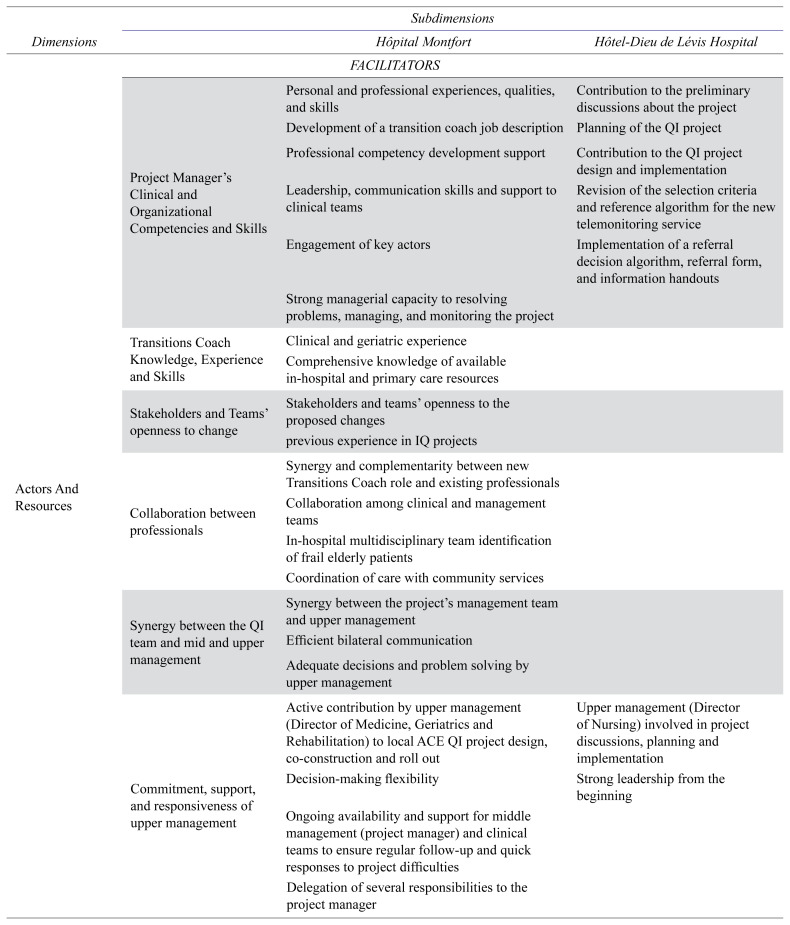
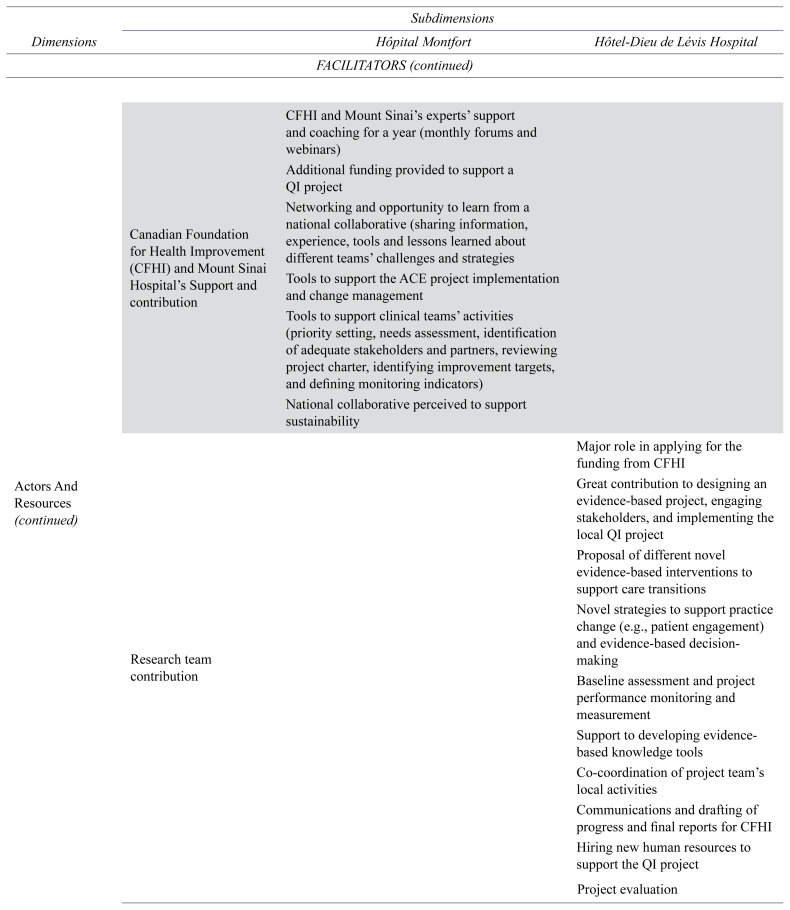
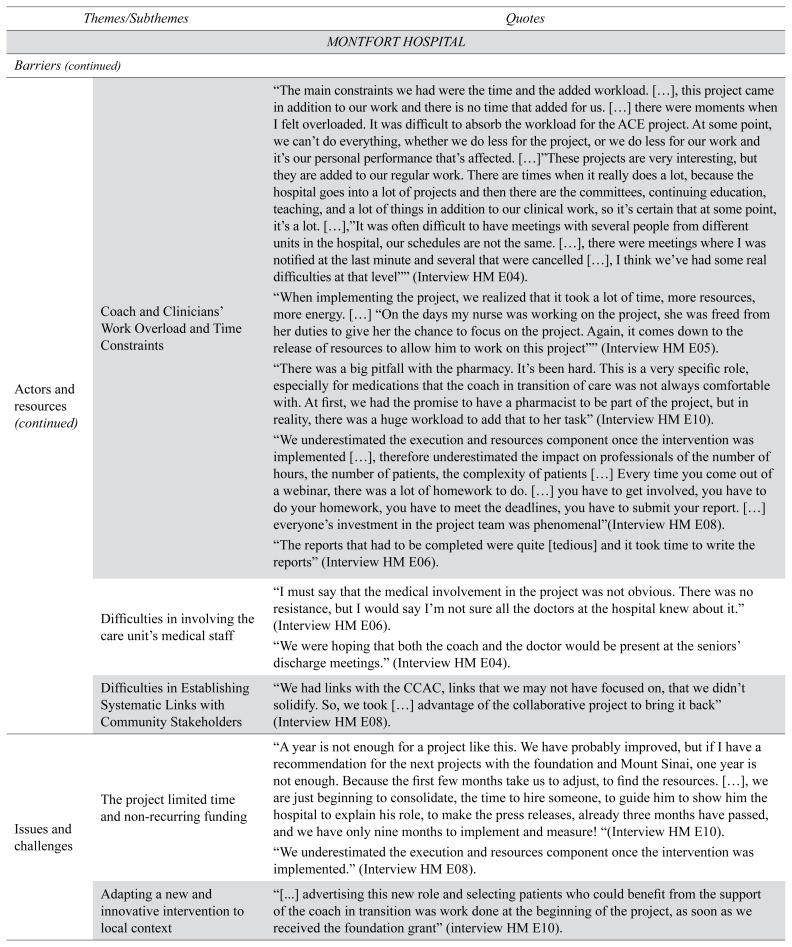
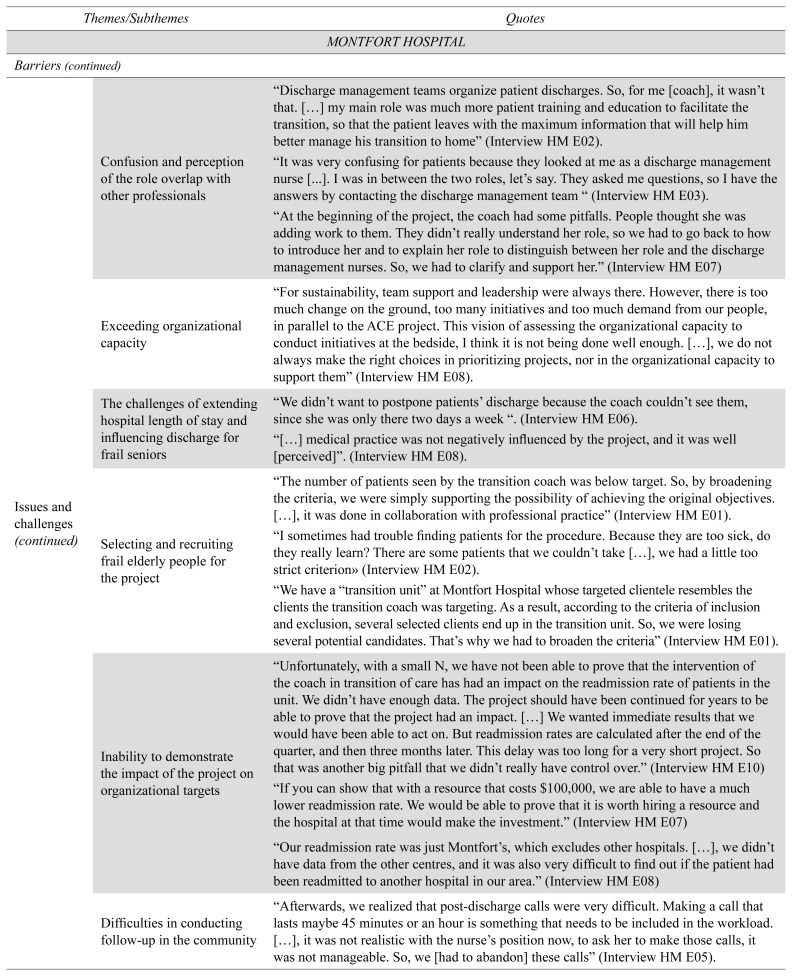
Facilitators and Barriers
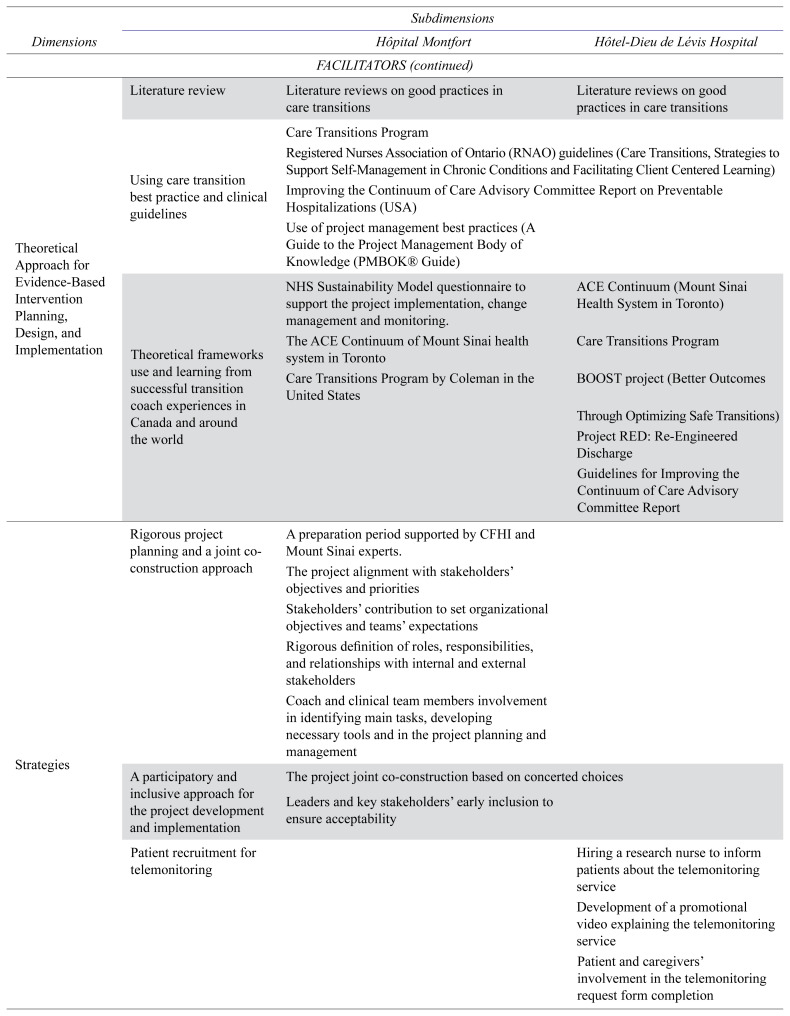
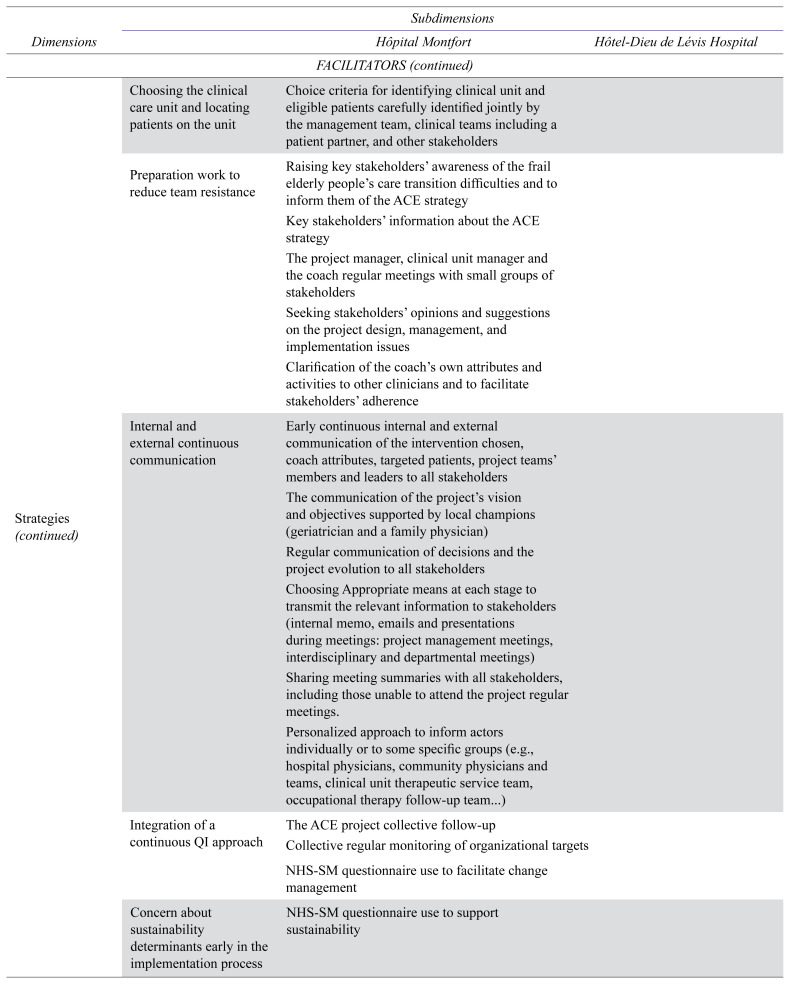
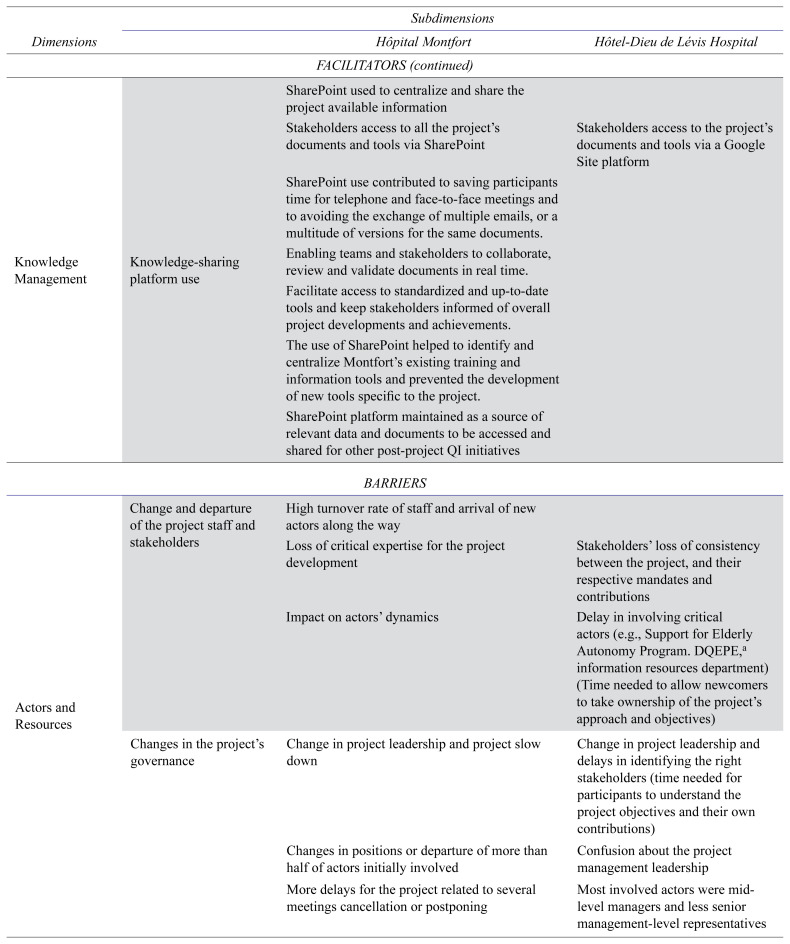
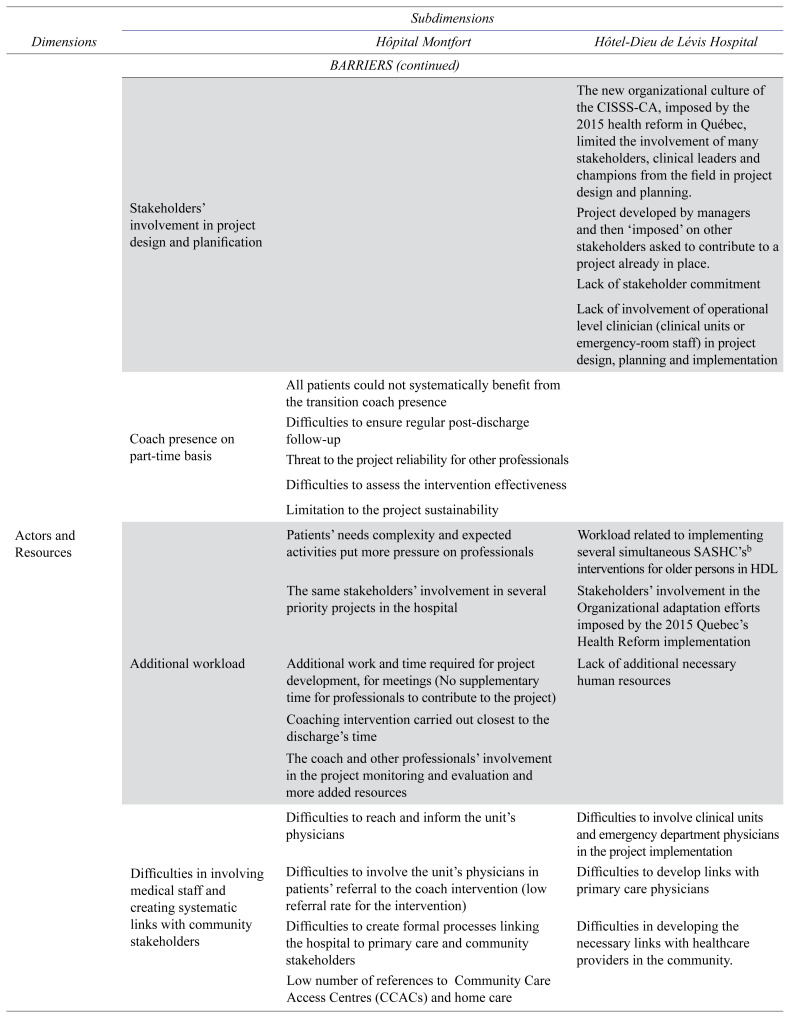
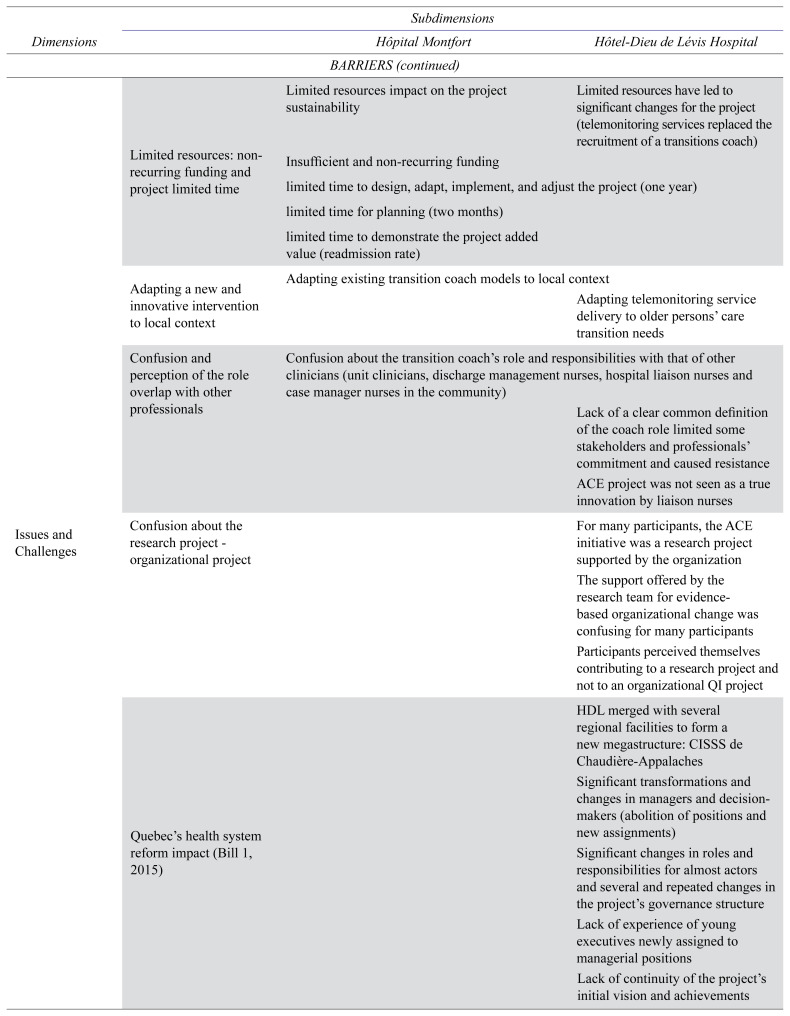
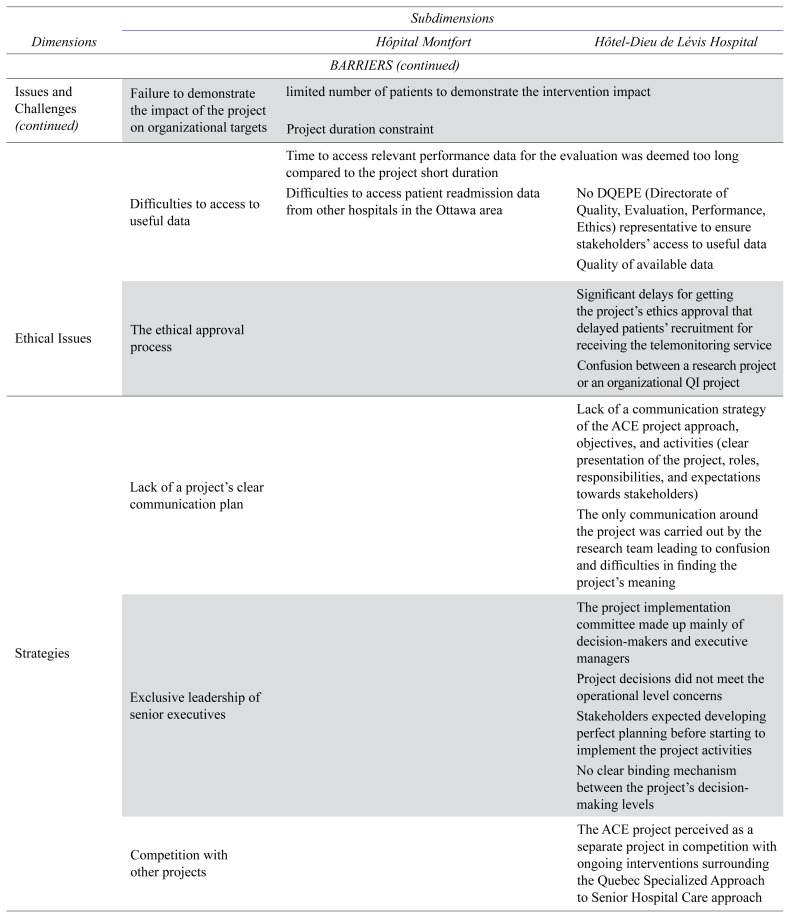
We analyzed the project facilitators and barriers according to our framework: actors and resources, theoretical approaches, issues and challenges, strategies, and knowledge transfer approaches.(14) Key barriers and facilitators are detailed in Appendix B. Appendix C provides citations for the dimensions and sub-dimensions of barriers and facilitators identified in our analysis.
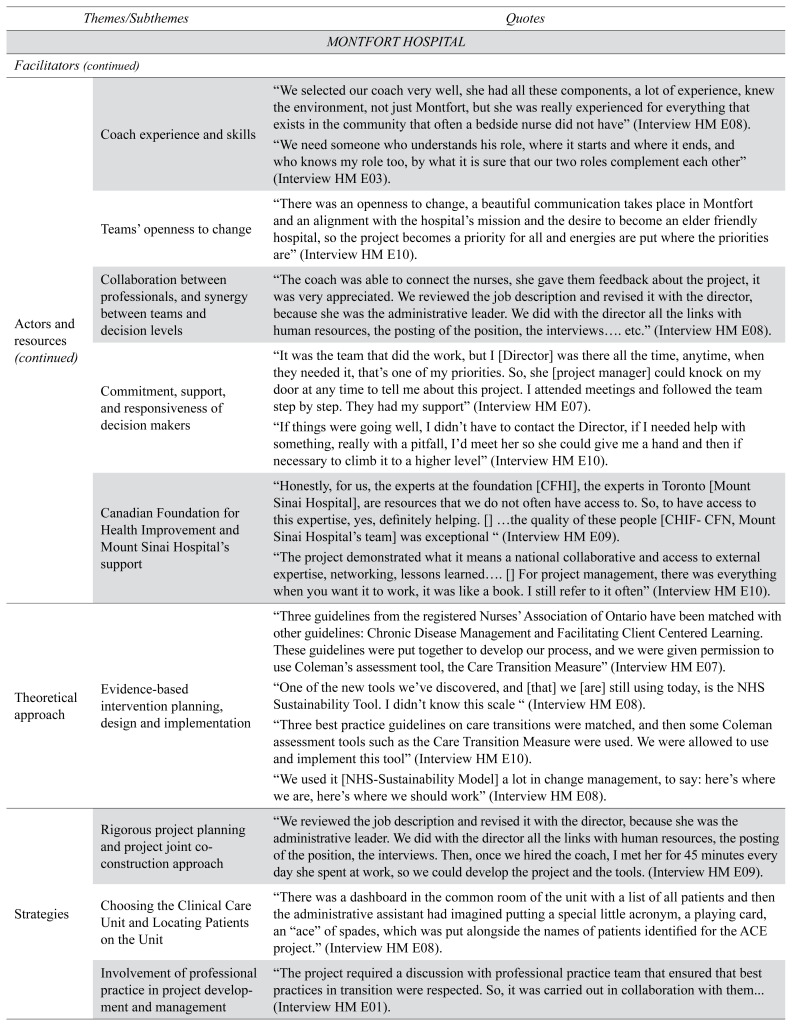
Facilitators at Hôpital Montfort
We identified the following facilitators, actors and resources: (1) the project manager’s clinical and organizational competencies, which facilitated project planning and implementation; (2) the transition coach’s clinical experience, skills, and knowledge; (3) the clinical and management teams’ openness to change; (4) the collaboration among clinicians and managers; (5) the decision-makers’ commitment, support, and responsiveness; and (6) the support and contributions of the CFHI, CFN and of Sinai Health. Theoretical approaches: Both the evidence-based ACE TCI and project management supported by the NHS Sustainability Model (NHS-SM) supported implementation. Strategies: Effective change strategies included (1) participative co-design and implementation; (2) mitigation of resistance to change; (3) continuous internal and external communication; (4) continuous QI approach; and (5) early focus on sustainability. Knowledge transfer approaches: The team used SharePoint (Microsoft, Redmond, CA, USA), a collaborative authoring and knowledge management platform that saved time and facilitated the sharing of data and documents.
Barriers at Hôpital Montfort
We identified the following barriers for actors and resources: (1) high human resource turnover (more than half of the initial team members changed positions); (2) the transition coach was only part-time; (3) additional workload for clinicians and team members; and (4) difficulty engaging medical staff and establishing community-based linkages (Community Care Access Centre (CCAC) home care providers). Issues and challenges: We found that: (1) the ACE project was limited in time and hampered by insufficient and non-recurrent funding; (2) adapting the intervention to local context proved challenging; (3) the transition coach’s role overlapped with the responsibilities of other professionals; (4) time constraints undermined the efforts of many stakeholders to help design and implement the project; (5) clinicians faced challenges in identifying frail elderly people; and (6) the project failed to demonstrate the impact on some organizational goals.
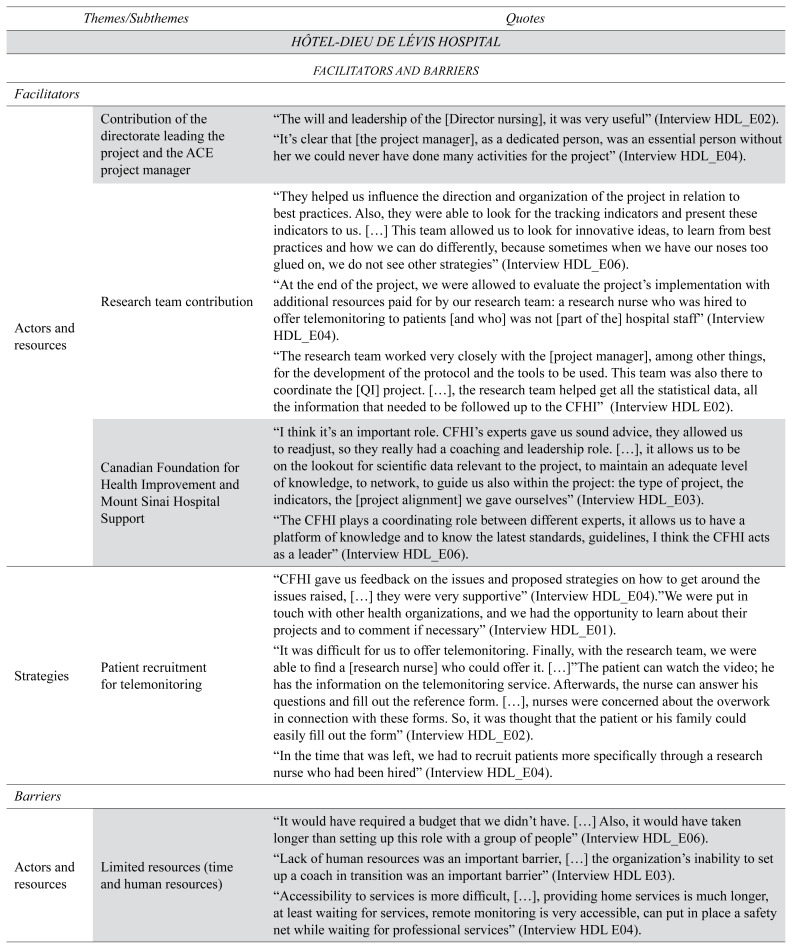
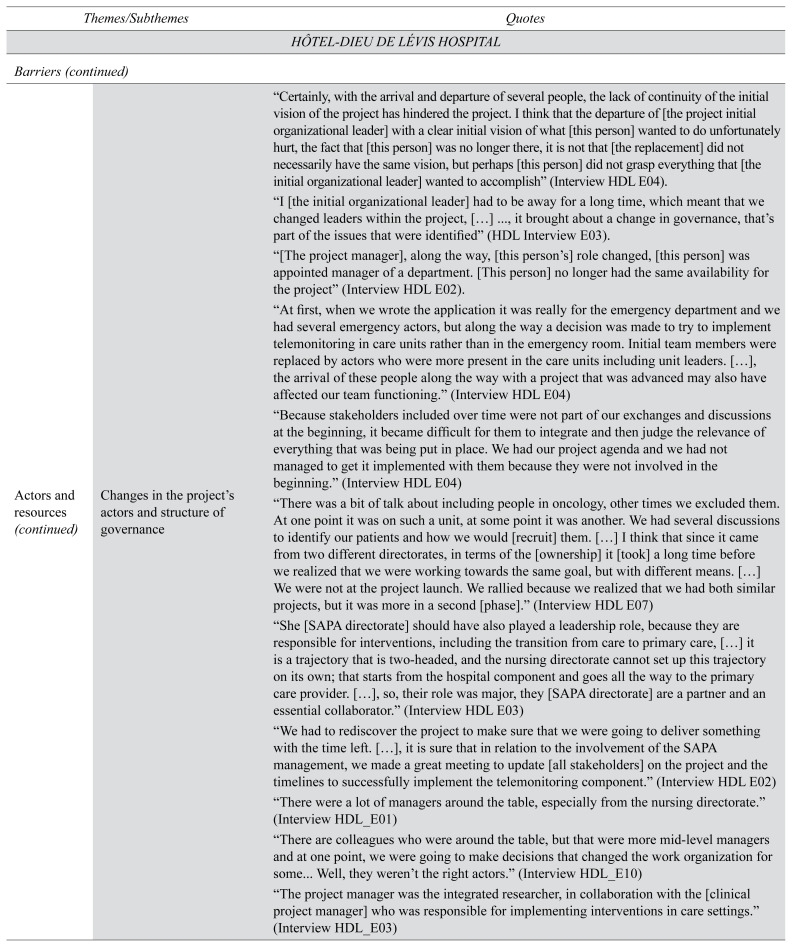
Facilitators at HDL Hospital
We identified the following facilitators regarding actors and resources: (1) nursing director and skilled project manager; (2) integrated research team; and (3) CFHI-CFN-Sinai Health financial support and mentorship. Theoretical approaches: We found that developing a guideline-based transition pathway (i.e., using the Registered Nurses’ Association of Ontario Care Transition Guideline(22)) facilitated local acceptability. Strategies: (1) Hiring a research nurse facilitated patient recruitment; (2) telemonitoring referrals; and (3) patient/caregiver completion of the telemonitoring referral form. Developing a video explaining the telemonitoring service was another helpful strategy. Knowledge transfer approaches: Using a Google Sites collaborative writing platform to support team knowledge management and document sharing facilitated the implementation of the ACE care transition component.
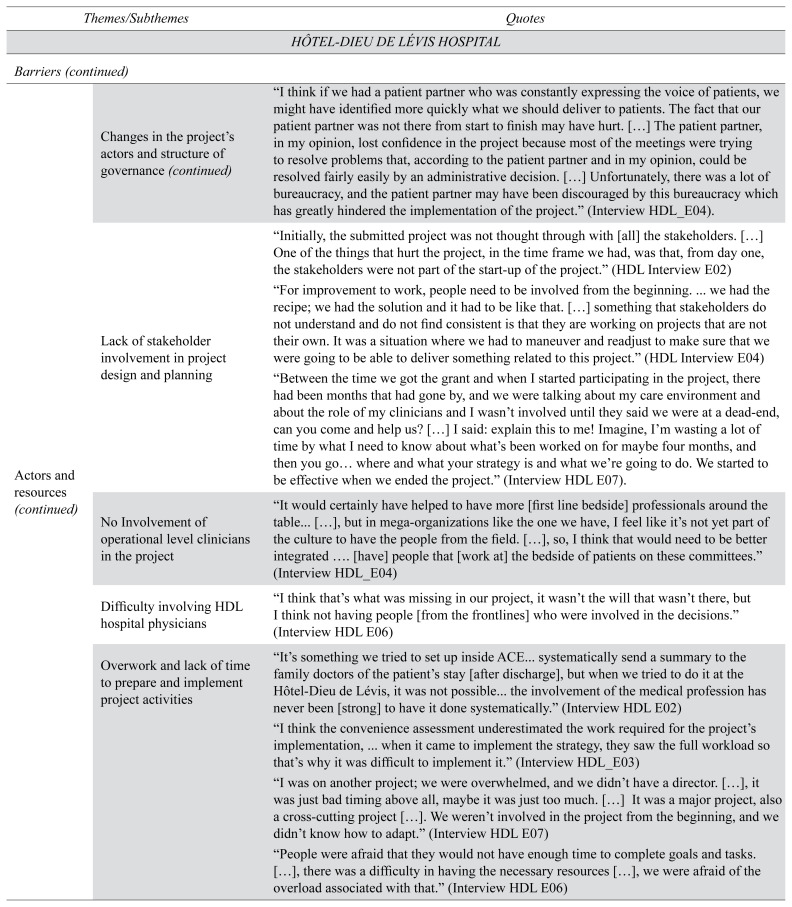
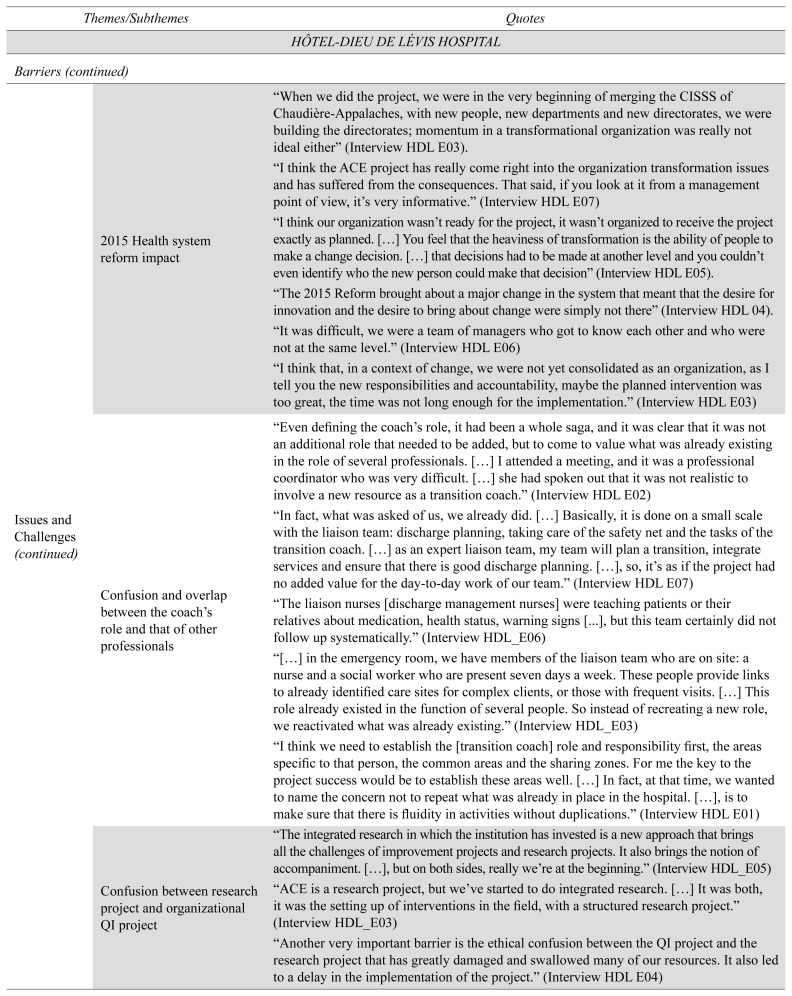
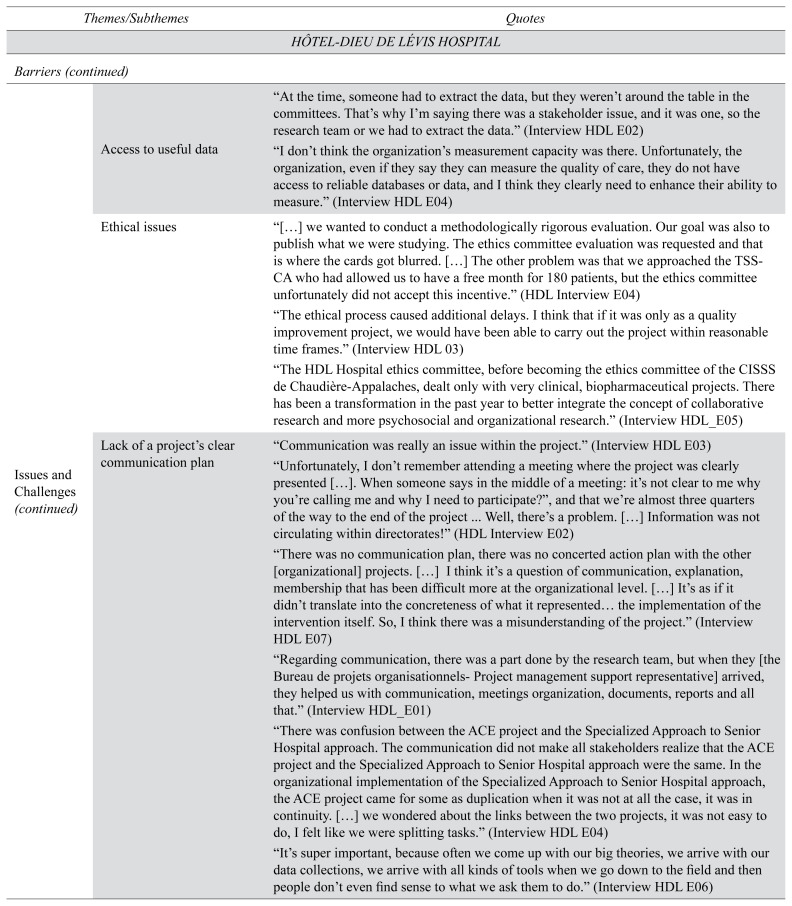
Barriers at HDL Hospital
The HDL team faced several difficulties that led to significant delays. Actors and resources: Major obstacles included: (1) limited human and financial resources; (2) changes in organizational leadership; (3) frequent turnover in key management roles; (4) changing governance structure; (5) lack of stakeholder involvement in project design and planning; (6) lack of involvement of frontline clinicians and physicians; (7) work overload from other concurrent initiatives; and (8) change in the intervention implementation site (the emergency department was changed to a regular medical ward). Issues and challenges: Quebec’s 2015 health-care reform (Quebec, Bill 1)(23) negatively impacted the project. Merging all Chaudière-Appalaches hospitals, community services and long-term care homes into one large health organization while eliminating many management positions created uncertainty and disorganization. Many newly appointed managers were not empowered to fully support the ACE project many months after the reform. There was also perceived overlap with the Quebec Specialized Approach to Senior Hospital Care, and existing liaison nurses’ duties. The lack of access to timely performance data was another barrier. There was also confusion about whether the project was a research project or a QI project. The ethics committee also struggled to understand the dual integrated research and QI status of the project, thus delaying the approval of the project. Finally, using Google Sites as the team’s knowledge-sharing platform raised cybersecurity risk issues. Strategies: Participants identified the following barriers: (1) lack of clear communication; (2) lack of clinical champions; (3) lack of communication between departments involved in the dysfunctional care transitions (e.g., hospital care to community care); (4) poor project planning to address clinical and operational concerns; and (5) selecting a technology-based intervention (i.e., telemonitoring) with complex care coordination challenges, access, and cost issues.
Conditions for Success and Sustainability
Table 3 shows the main conditions for success and determinants of sustainability for both QI projects identified through our qualitative analysis based on the theoretical framework. The findings are based on direct interviews with participants regarding their perceptions of the success and sustainability of the TCI.
TABLE 3.
Main conditions for success and sustainability for both quality improvement projects
| Conditions of Success | |
|---|---|
| External support | QI project supported by credible organizations and credentialed experts |
|
| |
| Organizational factors | Organizational stability and openness to change |
| Shared history of organizational change | |
| QI project based on clinical and organizational needs and in alignment with organizational, regional, and departmental priorities | |
| Accurate diagnosis of the problem and strategic selection of the solution to address it | |
|
| |
| Actors’ dynamics | Shared vision, developed with all stakeholders, of a common organizational QI project |
| Confirmed clinical leadership and solid support and responsiveness from the senior management team | |
| Actor dynamics aimed at changing practices and building consensus | |
|
| |
| Implementation strategies | Progressive/iterative approach supports incremental implementation |
|
| |
| Project management strategies | Plan, implement and manage projects based on evidence and successful experiences elsewhere |
| Integration of QI project governance into organizational decision-making process | |
| Collaborative, regular monitoring and ongoing communication of project progress | |
|
| |
| Determinants of Sustainability | |
|
| |
| Resources | Financial and human resources |
| Using relevant theoretical models and tools to systematically identify project sustainability conditions | |
|
| |
| Organizational factors | Developing interoperable information systems to support information continuity |
| Using knowledge management platforms | |
| Access to patient-level data and to performance indicators | |
| Access to the project financial cost-efficacy data | |
| Demonstrating the value and impact of QI interventions | |
|
| |
| Actors | Clinical leadership |
| Involvement of the physicians | |
| Developing more connections to increase awareness/involvement and partnerships with community stakeholders | |
DISCUSSION
In both hospitals, the ACE project demonstrated alignment with clinical and organizational priorities. Stakeholders at both hospitals cited access to external support, CFHI/Sinai Health experts, learning sessions, and access to knowledge tools and evidence-based strategies as facilitating factors for improvement. Participation in a national collaborative project allowed stakeholders to network, learn from other organizations, and discover the challenges different teams face and their strategies for overcoming them. Both hospitals used a collaborative approach to project development and implementation. Although the two projects had different outcomes, both teams learned numerous QI best practices and strategies. These continue to support sustainable change at both organizations. Understanding the key facilitating conditions and strategies used in both hospitals will benefit other centres planning the implementation of complex care transition interventions.
HM’s implementation strategies provided timely and effective guidance. HM undertook minor adjustments to the TCI design and implementation. In providing telemonitoring services to support older adults care transitions, HDL had to make significant project adjustments. Local stakeholders underestimated the complexity of new care transition projects especially when new technology is introduced.(24)
Both hospitals favoured a bottom-up approach to driving change. Adopting a bottom-up or top-down approach can make a big difference in driving clinical improvements in collaborative improvement projects.(25) To engage stakeholders, HM management team worked collaboratively and frequently communicated. Discussing evidence was key for ensuring project acceptability.(26) Senior management and CFHI experts helped HM overcome local barriers.(27) HM also used iterative implementation cycles.(28,29) Project milestones and accepted quality indicators were regularly tracked by all stakeholders. A recent review identified this as a facilitating factor.(30)
Prior to the ACE project, HM had a strong innovation and QI culture, all important in improving elder care transitions.(26,30,31) Like HM, HDL also embraced innovation and change. However, HDL’s efforts were focused elsewhere due to a major health reform (Quebec, Bill 1) and organizational restructuring. With high staff turnover and changing roles and responsibilities, many managers didn’t have enough time to fully understand their new roles or engage clinical leadership, a critical success factor for QI initiatives.(28) Establishing a governance structure and team composition took many months. Such systemic changes and team member instability disrupt QI projects.(28)
The ACE project was also one of HDL’s first experiences with an innovative form of integrated research supporting evidence-based organizational change. The integrated research team played a major role in engaging stakeholders, and in designing and implementing the ACE project. Involving an embedded clinician-researcher was confusing to some professionals who felt they were contributing to research rather than organizational QI. Although integrated research promises to support learning health-care organizations, many challenges remain, including creating a collaborative research/clinical culture where stakeholders work together in a trusting and open relationship to sustainably improve health system outcomes.(32) This first integrated research experience provided a strong, sustainable foundation for future integrated research. Several ongoing spin-off projects continue the work started during the ACE project.(6,33)
Finally, sustainability was an early concern for CFHI leaders. MH used the NHS-SM to monitor and manage change.(34) Addressing sustainability early helps participants avoid wasted effort and highlight the collective benefits of QI initiatives.(29,34) In both centres, three issues limited organizational capacity to measure sustainability: (1) barriers to accessing timely data; (2) lack of data systems for project performance monitoring and data analysis; and (3) lack of interoperable information systems to measure care continuity across transitions.
Our results complement the conclusions of the Acute Care for Elders Strategy Sustainment and Sustainability Study (ACES-SSS).(35) Similar to our study, ACES-SSS compared the sustainability of two different in-patient ACE interventions at two other ACE Collaborative intervention sites: a rural and remote community hospital (Whitehorse General Hospital) and an academic-affiliated hospital (Thunder Bay Regional Health Sciences Centre). Our study differed from ACES-SSS because we only focused on a TCI in two different hospitals with similar academic backgrounds, while ACES-SSSS studied the sustainment and sustainability of two in-patient care interventions in two different academic settings: the Braden Skin Assessment at the Thunder Bay Regional Health Sciences Centre and an ACE unit to offer optimal evidence-based in-patient acute care for older adults at the Whitehorse General Hospital. The ACES-SSSS found that adaptations to evidence-based interventions which respect as much as possible the fidelity of the original intervention are more likely to be sustainable. We also found this to be the case at HDL, where the TCI was adapted to the point that it differed significantly from the TCI implemented at HM and quite differently from the original TCI developed by Coleman et al.,(11) ultimately leading to successful sustainability at HM compared to HDL. Similar to Rappon,(35) we also found that frequent staff turnover and rapidly changing organizational priorities were major barriers to sustainability in both HM and HDL study sites. A common facilitator identified in both studies was the highly valued support of CFHI and Sinai Health experts in the form of additional funding, clinical expertise, and change management expertise. Our study adds to the ACES-SSS and existing implementation science literature by suggesting several facilitators to consider when adapting an evidence-based innovation to new organizations with different provincial contexts and change management cultures: minimal adaptation to the original evidence-based intervention; use of a collaborative, bottom-up approach; use of a theoretical model to support sustainability; support from clinical and organizational leadership; a strong organizational culture for QI; access to timely quality measures; financial support; use of a knowledge management platform; and involvement of an integrated research team and expert guidance.
Our study has several strengths. First, we interviewed a large sample of key participants representing a range of clinical, policy, and managerial stakeholders. We also included the patient perspective by involving a patient partner from HM. We used rigorous qualitative analysis methods, including focus group validation of our findings. Our rigorous approach and large sample size support generalizability to other Canadian francophone hospitals.
We also acknowledge some limitations. First, our retrospective analysis could be exposed to recall bias. Second, we were only able to report on the perspective of a single patient partner. Finally, analyzing other ACE Collaborative sites’ experiences, including international sites, would have provided more diverse and generalizable results.
CONCLUSION
We compared the implementation of a care transition intervention in two French-Canadian hospitals participating in an Acute Care for Elders QI collaborative. Emerging lessons and strategies will help clinicians, managers, and policymakers better address the challenges of implementing complex evidence-based care transition interventions. Notably, minimizing adaptations to original evidence-based interventions, using a bottom-up collaborative approach supported by strong clinical and organizational leadership, strong organizational culture for quality improvement, access to timely quality indicators, financial support, use of a knowledge management platform, and involvement of an integrated research team and expert guidance are key factors to successful care transition quality improvement projects.
ACKNOWLEDGEMENTS
The authors would like to thank the two hospitals for supporting this study, as well as everyone who agreed to participate as key informants. We would also like to thank Thérèse Antoun and Linda Lessard for their assistance with access to key informants and the relevant data, and Denis Roy for supporting the first author and feeding our reflections during the writing of the manuscript.
APPENDIX A. ACE project initial expectations and perceived results
| Hôpital Montfort | Hôtel-Dieu de Lévis |
|---|---|
| Initial Expectations and Goals | |
| Organizational Expectations | |
| Reducing hospital readmission rates in frail elderly people represented the “real expectation”. | Improving the quality of care for vulnerable older adults. |
| Implementing a standardized approach to providing education for older adults and their families. | Implementing an intervention supporting elders’ safe transition of care |
| Improving older adults and their families’ satisfaction with care transitions. | Contributing to the development of the CISSS Chaudière-Appalaches organization’s academic mission. |
| Developing and strengthening links with health resources available in the community | Collaborating to a local initiative for improving quality of elder care. |
| Personal Expectations | |
| Personal sensitivity to elders’ quality of care | Experimenting innovative solutions for frail older adults’ needs |
| Participants’ commitment to develop initiatives aiming to support frail elderly people and family education and information. | Collaborating with an integrated research project |
| Clinicians and professional practice managers personal interest in standardizing the nurses’ role in elder care transitions according to best practices | |
| Clinicians and professional practice managers have a personal interest in demonstrating the project’s direct contribution to older adults’ quality of care, chronic diseases management and patients and family satisfaction. | |
| Strengthening the role of nurses in health promotion activities for these patients. | |
| Managers’ personal expectations were in line with organizational ones: reducing hospital readmission rates, reducing length of stay; developing a standardized approach to older adults’ care transition | |
| Perceived Project Results | |
| ACE project emphasized the need to think about frail elderly people’s transition of care issues; | ACE project as conducted did not achieve tangible results for patients or professionals. |
| ACE project helped identify, adapt, and implement transition of care best practices and activities; | ACE project did result in any change in nurses’ clinical practice |
| ACE project improved stakeholder knowledge and skills related to care transitions (the coach kept nurses informed about evidence-based practices and trained them on the use of new assessment and teaching tools (e.g., Clinical Frailty Scale (CFS), “Teach Back” teaching technique; CTM3); | HDL and CISSS CA’s participation in this project represented a unique opportunity to implement processes of lasting change that continue to operate at HDL and more largely in the CISSS Chaudière-Appalaches; |
| ACE project helped harmonize certain care transition activities; (the major outcome identified at Hôpital Montfort) | The project was an opportunity to raise awareness about the needs of frail older adults along the trajectory of care with an emphasis on areas of care transitions; |
| ACE project helped select the relevant tools available for frail elderly people’s tracking, evaluation, and teachinga | The project was an opportunity to initiate a cultural change in the organization; |
| ACE project supported other team members’ work; | The project helped to prioritize the Specialized Approach to Senior Hospital Care and to implement several of its components;b |
| ACE project created more links with and within clinical teams; | The project helped strengthen the integrated research approach to support changes within the organization;c |
| ACE project supported a pharmacist to develop specific practices for frail elderly people (education and sharing information about medication changes with community health providers) | The dynamics that emerged from participation in the ACE project reduced barriers between research and practice and increased awareness about the benefits of integrated research in supporting organizational projects;d |
| ACE project created more links with the primary care providers and resources in the community (formal hospital discharge summary including discharge medication reconciliation; letter reminding family doctors to schedule a follow-up appointment); | ACE project was an opportunity to activate a “notice of admission” alert developed by the Support for Elderly Autonomy Program Directorate (SEAP) and Nursing Directorate, to inform Local Community Service Center (“CLSC”) professionals about an elderly patient’s hospital admission or emergency room visit; |
| The project helped establish some links with Community Care Access Centers’ (CCAC) (Rapid Response Nurses (RRN)e program for home visits and follow-up in the community. | The project was an opportunity to review the telemonitoring service referral and care trajectory processes; |
| The project contributed to improving clinicians’ satisfaction towards activities supporting the quality-of-care transitions and teamwork; | The project was an opportunity to review and harmonize the referral form allowing telemonitoring nurses to properly identify frail elderly people and helping liaison nurses identify and refer these people to the telemonitoring service. |
These changes remained on the unit after the end of the project.
For example, the implementation of the Emergency Geriatric Nurse Project (GEM Nurse), the design of a project to assess the impact of telemonitoring use for older persons with high use of emergency rooms.
The integrated research team obtained, in collaboration with the Director of Nursing, funding from CIHR to conduct a second phase of the ACE project, on a larger scale in the CISSS CA (Learning Wisdom Project(6)). Also, a team member was able to obtain a CIHR Postdoctoral Health System Impact Fellowship (https://cihr-irsc.gc.ca/e/51211.html).
Several partnerships have been developed between the research team and two CISSS Chaudière-Appalaches Directorates, whose managers are currently acting as co-investigators and knowledge users in several research projects. Collaborative links were also noted between researchers, managers and clinicians from emergency departments and some care units.
The Rapid Response Nursing program is a dedicated team of Registered Nurses providing a variety of intensive in-home services to patients with complex care needs and their families to support smooth and safe transitions from hospital to the patient’s home (http://healthcareathome.ca/centraleast/en/care/patient/Documents/Rapid-Response-Nurses-Fact-Sheet.pdf).
APPENDIX B. Facilitators and barriers to the implementation of the ACE projects at Hôpital Montfort and Hôtel-Dieu de Lévis
| Dimensions | Subdimensions | ||
|---|---|---|---|
|
| |||
| Hôpital Montfort | Hôtel-Dieu de Lévis Hospital | ||
| Actors And Resources | FACILITATORS | ||
|
| |||
| Project Manager’s Clinical and Organizational Competencies and Skills | Personal and professional experiences, qualities, and skills | Contribution to the preliminary discussions about the project | |
| Development of a transition coach job description | Planning of the QI project | ||
| Professional competency development support | Contribution to the QI project design and implementation | ||
| Leadership, communication skills and support to clinical teams | Revision of the selection criteria and reference algorithm for the new telemonitoring service | ||
| Engagement of key actors | Implementation of a referral decision algorithm, referral form, and information handouts | ||
| Strong managerial capacity to resolving problems, managing, and monitoring the project | |||
|
| |||
| Transitions Coach Knowledge, Experience and Skills | Clinical and geriatric experience | ||
| Comprehensive knowledge of available in-hospital and primary care resources | |||
|
| |||
| Stakeholders and Teams’ openness to change | Stakeholders and teams’ openness to the proposed changes | ||
| previous experience in IQ projects | |||
|
| |||
| Collaboration between professionals | Synergy and complementarity between new Transitions Coach role and existing professionals | ||
| Collaboration among clinical and management teams | |||
| In-hospital multidisciplinary team identification of frail elderly patients | |||
| Coordination of care with community services | |||
|
| |||
| Synergy between the QI team and mid and upper management | Synergy between the project’s management team and upper management | ||
| Efficient bilateral communication | |||
| Adequate decisions and problem solving by upper management | |||
|
| |||
| Commitment, support, and responsiveness of upper management | Active contribution by upper management (Director of Medicine, Geriatrics and Rehabilitation) to local ACE QI project design, co-construction and roll out | Upper management (Director of Nursing) involved in project discussions, planning and implementation | |
| Decision-making flexibility | Strong leadership from the beginning | ||
| Ongoing availability and support for middle management (project manager) and clinical teams to ensure regular follow-up and quick responses to project difficulties | |||
| Delegation of several responsibilities to the project manager | |||
|
| |||
| Canadian Foundation for Health Improvement (CFHI) and Mount Sinai Hospital’s Support and contribution | CFHI and Mount Sinai’s experts’ support and coaching for a year (monthly forums and webinars) | ||
| Additional funding provided to support a QI project | |||
| Networking and opportunity to learn from a national collaborative (sharing information, experience, tools and lessons learned about different teams’ challenges and strategies | |||
| Tools to support the ACE project implementation and change management | |||
| Tools to support clinical teams’ activities (priority setting, needs assessment, identification of adequate stakeholders and partners, reviewing project charter, identifying improvement targets, and defining monitoring indicators) | |||
| National collaborative perceived to support sustainability | |||
|
| |||
| Research team contribution | Major role in applying for the funding from CFHI | ||
| Great contribution to designing an evidence-based project, engaging stakeholders, and implementing the local QI project | |||
| Proposal of different novel evidence-based interventions to support care transitions | |||
| Novel strategies to support practice change (e.g., patient engagement) and evidence-based decision-making | |||
| Baseline assessment and project performance monitoring and measurement | |||
| Support to developing evidence-based knowledge tools | |||
| Co-coordination of project team’s local activities | |||
| Communications and drafting of progress and final reports for CFHI | |||
| Hiring new human resources to support the QI project | |||
| Project evaluation | |||
|
| |||
| Theoretical Approach for Evidence-Based Intervention Planning, Design, and Implementation | Literature review | Literature reviews on good practices in care transitions | Literature reviews on good practices in care transitions |
|
| |||
| Using care transition best practice and clinical guidelines | Care Transitions Program | ||
| Registered Nurses Association of Ontario (RNAO) guidelines (Care Transitions, Strategies to Support Self-Management in Chronic Conditions and Facilitating Client Centered Learning) | |||
| Improving the Continuum of Care Advisory Committee Report on Preventable Hospitalizations (USA) | |||
| Use of project management best practices (A Guide to the Project Management Body of Knowledge (PMBOK® Guide) | |||
|
| |||
| Theoretical frameworks use and learning from successful transition coach experiences in Canada and around the world | NHS Sustainability Model questionnaire to support the project implementation, change management and monitoring. | ACE Continuum (Mount Sinai Health System in Toronto) | |
| The ACE Continuum of Mount Sinai health system in Toronto | Care Transitions Program | ||
| Care Transitions Program by Coleman in the United States | BOOST project (Better Outcomes | ||
| Through Optimizing Safe Transitions) | |||
| Project RED: Re-Engineered Discharge | |||
| Guidelines for Improving the Continuum of Care Advisory Committee Report | |||
|
| |||
| Strategies | Rigorous project planning and a joint co-construction approach | A preparation period supported by CFHI and Mount Sinai experts. | |
| The project alignment with stakeholders’ objectives and priorities | |||
| Stakeholders’ contribution to set organizational objectives and teams’ expectations | |||
| Rigorous definition of roles, responsibilities, and relationships with internal and external stakeholders | |||
| Coach and clinical team members involvement in identifying main tasks, developing necessary tools and in the project planning and management | |||
|
| |||
| A participatory and inclusive approach for the project development and implementation | The project joint co-construction based on concerted choices | ||
| Leaders and key stakeholders’ early inclusion to ensure acceptability | |||
|
| |||
| Patient recruitment for telemonitoring | Hiring a research nurse to inform patients about the telemonitoring service | ||
| Development of a promotional video explaining the telemonitoring service | |||
| Patient and caregivers’ involvement in the telemonitoring request form completion | |||
|
| |||
| Choosing the clinical care unit and locating patients on the unit | Choice criteria for identifying clinical unit and eligible patients carefully identified jointly by the management team, clinical teams including a patient partner, and other stakeholders | ||
|
| |||
| Preparation work to reduce team resistance | Raising key stakeholders’ awareness of the frail elderly people’s care transition difficulties and to inform them of the ACE strategy | ||
| Key stakeholders’ information about the ACE strategy | |||
| The project manager, clinical unit manager and the coach regular meetings with small groups of stakeholders | |||
| Seeking stakeholders’ opinions and suggestions on the project design, management, and implementation issues | |||
| Clarification of the coach’s own attributes and activities to other clinicians and to facilitate stakeholders’ adherence | |||
|
| |||
| Internal and external continuous communication | Early continuous internal and external communication of the intervention chosen, coach attributes, targeted patients, project teams’ members and leaders to all stakeholders | ||
| The communication of the project’s vision and objectives supported by local champions (geriatrician and a family physician) | |||
| Regular communication of decisions and the project evolution to all stakeholders | |||
| Choosing Appropriate means at each stage to transmit the relevant information to stakeholders (internal memo, emails and presentations during meetings: project management meetings, interdisciplinary and departmental meetings) | |||
| Sharing meeting summaries with all stakeholders, including those unable to attend the project regular meetings. | |||
| Personalized approach to inform actors individually or to some specific groups (e.g., hospital physicians, community physicians and teams, clinical unit therapeutic service team, occupational therapy follow-up team...) | |||
|
| |||
| Integration of a continuous QI approach | The ACE project collective follow-up | ||
| Collective regular monitoring of organizational targets | |||
| NHS-SM questionnaire use to facilitate change management | |||
|
| |||
| Concern about sustainability determinants early in the implementation process | NHS-SM questionnaire use to support sustainability | ||
|
| |||
| Knowledge Management | Knowledge-sharing platform use | SharePoint used to centralize and share the project available information | |
| Stakeholders access to all the project’s documents and tools via SharePoint | Stakeholders access to the project’s documents and tools via a Google Site platform | ||
| SharePoint use contributed to saving participants time for telephone and face-to-face meetings and to avoiding the exchange of multiple emails, or a multitude of versions for the same documents. | |||
| Enabling teams and stakeholders to collaborate, review and validate documents in real time. | |||
| Facilitate access to standardized and up-to-date tools and keep stakeholders informed of overall project developments and achievements. | |||
| The use of SharePoint helped to identify and centralize Montfort’s existing training and information tools and prevented the development of new tools specific to the project. | |||
| SharePoint platform maintained as a source of relevant data and documents to be accessed and shared for other post-project QI initiatives | |||
|
| |||
| BARRIERS | |||
|
| |||
| Actors and Resources | Change and departure of the project staff and stakeholders | High turnover rate of staff and arrival of new actors along the way | |
| Loss of critical expertise for the project development | Stakeholders’ loss of consistency between the project, and their respective mandates and contributions | ||
| Impact on actors’ dynamics | Delay in involving critical actors (e.g., Support for Elderly Autonomy Program. DQEPE,a information resources department) (Time needed to allow newcomers to take ownership of the project’s approach and objectives) | ||
|
| |||
| Changes in the project’s governance | Change in project leadership and project slow down | Change in project leadership and delays in identifying the right stakeholders (time needed for participants to understand the project objectives and their own contributions) | |
| Changes in positions or departure of more than half of actors initially involved | Confusion about the project management leadership | ||
| More delays for the project related to several meetings cancellation or postponing | Most involved actors were mid-level managers and less senior management-level representatives | ||
|
| |||
| Stakeholders’ involvement in project design and planification | The new organizational culture of the CISSS-CA, imposed by the 2015 health reform in Québec, limited the involvement of many stakeholders, clinical leaders and champions from the field in project design and planning. | ||
| Project developed by managers and then ‘imposed’ on other stakeholders asked to contribute to a project already in place. | |||
| Lack of stakeholder commitment | |||
| Lack of involvement of operational level clinician (clinical units or emergency-room staff) in project design, planning and implementation | |||
|
| |||
| Coach presence on part-time basis | All patients could not systematically benefit from the transition coach presence | ||
| Difficulties to ensure regular post-discharge follow-up | |||
| Threat to the project reliability for other professionals | |||
| Difficulties to assess the intervention effectiveness | |||
| Limitation to the project sustainability | |||
|
| |||
| Additional workload | Patients’ needs complexity and expected activities put more pressure on professionals | Workload related to implementing several simultaneous SASHC’sb interventions for older persons in HDL | |
| The same stakeholders’ involvement in several priority projects in the hospital | Stakeholders’ involvement in the Organizational adaptation efforts imposed by the 2015 Quebec’s Health Reform implementation | ||
| Additional work and time required for project development, for meetings (No supplementary time for professionals to contribute to the project) | Lack of additional necessary human resources | ||
| Coaching intervention carried out closest to the discharge’s time | |||
| The coach and other professionals’ involvement in the project monitoring and evaluation and more added resources | |||
|
| |||
| Difficulties in involving medical staff and creating systematic links with community stakeholders | Difficulties to reach and inform the unit’s physicians | Difficulties to involve clinical units and emergency department physicians in the project implementation | |
| Difficulties to involve the unit’s physicians in patients’ referral to the coach intervention (low referral rate for the intervention) | Difficulties to develop links with primary care physicians | ||
| Difficulties to create formal processes linking the hospital to primary care and community stakeholders | Difficulties in developing the necessary links with healthcare providers in the community. | ||
| Low number of references to Community Care Access Centres (CCACs) and home care | |||
|
| |||
| Issues and Challenges | Limited resources: non-recurring funding and project limited time | Limited resources impact on the project sustainability | Limited resources have led to significant changes for the project (telemonitoring services replaced the recruitment of a transitions coach) |
| Insufficient and non-recurring funding | |||
| limited time to design, adapt, implement, and adjust the project (one year) | |||
| limited time for planning (two months) | |||
| limited time to demonstrate the project added value (readmission rate) | |||
|
| |||
| Adapting a new and innovative intervention to local context | Adapting existing transition coach models to local context | ||
| Adapting telemonitoring service delivery to older persons’ care transition needs | |||
|
| |||
| Confusion and perception of the role overlap with other professionals | Confusion about the transition coach’s role and responsibilities with that of other clinicians (unit clinicians, discharge management nurses, hospital liaison nurses and case manager nurses in the community) | ||
| Lack of a clear common definition of the coach role limited some stakeholders and professionals’ commitment and caused resistance | |||
| ACE project was not seen as a true innovation by liaison nurses | |||
|
| |||
| Confusion about the research project - organizational project | For many participants, the ACE initiative was a research project supported by the organization | ||
| The support offered by the research team for evidence-based organizational change was confusing for many participants | |||
| Participants perceived themselves contributing to a research project and not to an organizational QI project | |||
|
| |||
| Quebec’s health system reform impact (Bill 1, 2015) | HDL merged with several regional facilities to form a new megastructure: CISSS de Chaudière-Appalaches | ||
| Significant transformations and changes in managers and decision-makers (abolition of positions and new assignments) | |||
| Significant changes in roles and responsibilities for almost actors and several and repeated changes in the project’s governance structure | |||
| Lack of experience of young executives newly assigned to managerial positions | |||
| Lack of continuity of the project’s initial vision and achievements | |||
| Failure to demonstrate the impact of the project on organizational targets | limited number of patients to demonstrate the intervention impact | ||
| Project duration constraint | |||
|
| |||
| Difficulties to access to useful data | Time to access relevant performance data for the evaluation was deemed too long compared to the project short duration | ||
| Difficulties to access patient readmission data from other hospitals in the Ottawa area | No DQEPE (Directorate of Quality, Evaluation, Performance, Ethics) representative to ensure stakeholders’ access to useful data | ||
| Quality of available data | |||
|
|
|||
| Ethical Issues | The ethical approval process | Significant delays for getting the project’s ethics approval that delayed patients’ recruitment for receiving the telemonitoring service | |
| Confusion between a research project or an organizational QI project | |||
|
| |||
| Strategies | Lack of a project’s clear communication plan | Lack of a communication strategy of the ACE project approach, objectives, and activities (clear presentation of the project, roles, responsibilities, and expectations towards stakeholders) | |
| The only communication around the project was carried out by the research team leading to confusion and difficulties in finding the project’s meaning | |||
|
| |||
| Exclusive leadership of senior executives | The project implementation committee made up mainly of decision-makers and executive managers | ||
| Project decisions did not meet the operational level concerns | |||
| Stakeholders expected developing perfect planning before starting to implement the project activities | |||
| No clear binding mechanism between the project’s decision-making levels | |||
|
| |||
| Competition with other projects | The ACE project perceived as a separate project in competition with ongoing interventions surrounding the Quebec Specialized Approach to Senior Hospital Care approach | ||
|
| |||
| Implementing telemonitoring as a “complex” technological innovation | Challenges associated with the telemonitoring service implementation as a complex technology for care and services delivery (need to review the telemonitoring recruitment and referral processes) | ||
| Need for revising actors’ roles and responsibilities and for establishing a new trajectory involving hospital units, emergency department and community healthcare providers | |||
| Technological issues related to the equipment availability, patient acceptance and consent. | |||
| The challenges of technology cost and use for older persons. | |||
|
| |||
| Knowledge Management | Knowledge-sharing platform use | Google Sites platform blocked by the organization’s Information Resources Directorate for security issues | |
| Limited access and sharing of useful information and documents | |||
A Directorate of Quality, Evaluation, Performance, Ethics.
Quebec’s Specialized Approach to Senior Hospital Care.
APPENDIX C. Key themes related to initial expectations and goals, facilitators and barriers, and related verbatim quotes
| Themes/Subthemes | Quotes | |
|---|---|---|
| MONTFORT HOSPITAL | ||
|
| ||
| INITIAL EXPECTATIONS AND GOALS | ||
|
| ||
| Organizational expectations | “The real expectation was to reduce readmission rates for the elderly and frail patients. So that was really our ultimate expected result” (Interview HM E10). | |
|
| ||
| “In Montfort, our big challenge was getting patients out. []…. We also wanted to engage our family physicians in the community to be aware of our hospital orientations and to get their contribution” (Interview HM E08). | ||
|
| ||
| Personal expectations | “I have a sensitivity to the needs of the elderly I personally believe in it deeply, [] these are my personal values” (Interview HM E7). | |
| “it’s really about transition to the community with real support, something to formalize that would make it a direct and well-marked relationship with the community, []. It’s something that’s been close to my heart for a very long time” (Interview HM E4). | ||
|
| ||
| PERCEIVED PROJECT RESULTS | ||
|
| ||
| Identifying a new role | “But this role is really different! I would [say] a hybrid between a bedside nurse, a social worker and then the coach also had to know very well about community services” (Interview HM E08). | |
|
| ||
| Care transition activities standardization | “The biggest change was really having a standardized role in care transition “ (Interview HM E10). | |
|
| ||
| Improving transition care knowledge and skills in other teams | “There has been an increase in the knowledge and skills of the team. These teams are probably better equipped than any other care unit” (Interview HM E08). | |
|
| ||
| Support to other team members’ activities related to care transition | “The coach was able to connect the nurses, she gave them feedback about the project, it was very appreciated.” (Interview HM E10). | |
| “It takes away a certain workload from the nurse who cares less about teaching, because there was a dedicated resource specifically for these patients. [] I’ll tell you that this is probably the biggest impact for the team” (Interview HM E01). | ||
|
| ||
| Useful relationship creation (with clinical teams) | “If I had not seen the client yet, she [coach] could track things I should know. And if there was a need for the coach intervention, I could talk to her about that client” (Interview HM E03). | |
|
| ||
| Selection and use of relevant tools | “When we developed the project, we learned a lot of lessons about benefits and strengths of a program to prepare for seniors’ discharge. [] We tested tools that we can use with other patients” (Interview HM E10). | |
| “There are not enough pharmacists to see all seniors, and we have to prioritize. I would say that the patients who were identified by the fragility score were not necessarily the patients we would have seen outside of this project” (Interview HM E04). | ||
|
| ||
| Clinician satisfaction | “Certainly, it gives satisfaction with doing something that worked well. We’ve accomplished something, so it contributes to job satisfaction and commitment”. (Interview HM E04). | |
|
| ||
| Performing follow-up for frail older adults | “I would say that the most important thing I noticed with the patients was the post-discharge calls, because they really felt like we were participating in their care after they left, that we were worried about their return home, if they had any questions, we could answer them” (Interview HM E2). | |
|
| ||
| Organizational change support | “This project has been a lever for change in the hospital, but also allowing us to look outwards to present our provincial initiatives” (Interview HM E10). | |
|
| ||
| FACILITATORS AND BARRIERS | ||
|
| ||
| Facilitators | ||
|
| ||
| Actors and resources | Project manager’s competencies and skills | “Within the team, [the project manager] is the kind of leading nurse you want. She knows the rigour; she is professional and can engage people. She’s the kind of key people in the hospital. After having known her, she is the kind of leader I wanted her on all the initiatives, she greatly deserves the benefits of the project” (Interview HM E10). |
|
| ||
| Coach experience and skills | “We selected our coach very well, she had all these components, a lot of experience, knew the environment, not just Montfort, but she was really experienced for everything that exists in the community that often a bedside nurse did not have” (Interview HM E08). | |
| “We need someone who understands his role, where it starts and where it ends, and who knows my role too, by what it is sure that our two roles complement each other” (Interview HM E03). | ||
|
| ||
| Teams’ openness to change | “There was an openness to change, a beautiful communication takes place in Montfort and an alignment with the hospital’s mission and the desire to become an elder friendly hospital, so the project becomes a priority for all and energies are put where the priorities are” (Interview HM E10). | |
|
| ||
| Collaboration between professionals, and synergy between teams and decision levels | “The coach was able to connect the nurses, she gave them feedback about the project, it was very appreciated. We reviewed the job description and revised it with the director, because she was the administrative leader. We did with the director all the links with human resources, the posting of the position, the interviews…. etc.” (Interview HM E08). | |
|
| ||
| Commitment, support, and responsiveness of decision makers | “It was the team that did the work, but I [Director] was there all the time, anytime, when they needed it, that’s one of my priorities. So, she [project manager] could knock on my door at any time to tell me about this project. I attended meetings and followed the team step by step. They had my support” (Interview HM E07). | |
| “If things were going well, I didn’t have to contact the Director, if I needed help with something, really with a pitfall, I’d meet her so she could give me a hand and then if necessary to climb it to a higher level” (Interview HM E10). | ||
|
| ||
| Canadian Foundation for Health Improvement and Mount Sinai Hospital’s support | “Honestly, for us, the experts at the foundation [CFHI], the experts in Toronto [Mount Sinai Hospital], are resources that we do not often have access to. So, to have access to this expertise, yes, definitely helping. [] …the quality of these people [CHIF-CFN, Mount Sinai Hospital’s team] was exceptional “ (Interview HM E09). | |
| “The project demonstrated what it means a national collaborative and access to external expertise, networking, lessons learned…. [] For project management, there was everything when you want it to work, it was like a book. I still refer to it often” (Interview HM E10). | ||
|
| ||
| Theoretical approach | Evidence-based intervention planning, design and implementation | “Three guidelines from the registered Nurses’ Association of Ontario have been matched with other guidelines: Chronic Disease Management and Facilitating Client Centered Learning. These guidelines were put together to develop our process, and we were given permission to use Coleman’s assessment tool, the Care Transition Measure” (Interview HM E07). |
| “One of the new tools we’ve discovered, and [that] we [are] still using today, is the NHS Sustainability Tool. I didn’t know this scale “ (Interview HM E08). | ||
| “Three best practice guidelines on care transitions were matched, and then some Coleman assessment tools such as the Care Transition Measure were used. We were allowed to use and implement this tool” (Interview HM E10). | ||
| “We used it [NHS-Sustainability Model] a lot in change management, to say: here’s where we are, here’s where we should work” (Interview HM E08). | ||
|
| ||
| Strategies | Rigorous project planning and project joint co-construction approach | “We reviewed the job description and revised it with the director, because she was the administrative leader. We did with the director all the links with human resources, the posting of the position, the interviews. Then, once we hired the coach, I met her for 45 minutes every day she spent at work, so we could develop the project and the tools. (Interview HM E09). |
|
| ||
| Choosing the Clinical Care Unit and Locating Patients on the Unit | “There was a dashboard in the common room of the unit with a list of all patients and then the administrative assistant had imagined putting a special little acronym, a playing card, an “ace” of spades, which was put alongside the names of patients identified for the ACE project.” (Interview HM E08). | |
|
| ||
| Involvement of professional practice in project development and management | “The project required a discussion with professional practice team that ensured that best practices in transition were respected. So, it was carried out in collaboration with them... (Interview HM E01). | |
|
| ||
| Participatory and inclusive approach | “In our meetings with all stakeholders, we offered ideas, we asked for their opinions, and then there were discussions. Most of the time they accepted our suggestions, but we really wanted to be able to have their buy-in for the implementation” (Interview MM E10). | |
|
| ||
| Continuous quality improvement approach | “… the clinical information department, so to see everything that’s related to data collection, just tracking the data to give team feedback. So, for example, tracking the readmission rate, that’s part of their job” (Interview HM E05). | |
|
| ||
| Concern about sustainability early in the implementation process | “Sustainability, I think it was well planned, but we didn’t have enough resources to put it in place as it should be “ (Interview HM E10). | |
| “One of the new tools we’ve discovered, and [that] we [are] still using today, is the NHS Sustainability Tool. I didn’t know this scale “ (Interview HM E08). | ||
|
| ||
| Continuous internal and external communication | “We had meetings and at the end of each one it was the project manager who made a kind of summary that she emailed to everyone” (Interview HM E4). | |
| “I think we have to have good communication with the coach. Everyone has a role, and we must not pile on our feet” (Interview HM E03). | ||
|
| ||
| Knowledge translation | SharePoint use | “SharePoint really helped us a lot. It makes information more accessible to everyone. We were able to view the documents at the same time. [...] It’s much more effective as a tool than e-mail, than sending attachments that get lost and you never know the latest version” (Interview HM E10). |
| “Let’s say we wanted to review a document, we’d say, “OK, the document is on SharePoint, look at and revise.” So, everyone could put their comments in there” (Interview HM E02) | ||
| “Right now, every time someone talks to me about the transition, I tell them not to reinvent the wheel, we have everything, it’s all on our SharePoint.” (Interview HM E08). | ||
|
| ||
| Barriers | ||
|
| ||
| Actors and resources | Change and departure of the staff and stakeholders | “During the project, there were changes of players... [], it’s often a bit of a start and slows down” (Interview HM E08). |
| “Another thing that didn’t help us was that there are a lot of people who have changed chairs, more than at any other time. [] it’s a new project and almost half of the players have changed chairs. [] and it looks like the information doesn’t really know how to translate well from one player to another” (Interview HM E10). | ||
|
| ||
| Coach presence on part-time basis | “We got the money for only half a [position] and the nurse wasn’t there seven days a week to see the patients” (Interview HM E06). | |
| “The post-discharge follow-up wasn’t easy because I was there just two days a week, when our goal was to call patients at about 72 hours. [], it could take three, four to five days, or if I couldn’t reach them, it could be a little longer” (Interview HM E02). | ||
| “The coach wasn’t there […] five days a week, it was a concern. One day she’s here, [another] day she’s not... [] we have to make sure that we have some reliability, […], for doctors, clinical teams, it was difficult to know whether we have the service or not” (Interview HM E06). | ||
| “When you don’t have something at least five days a week, it becomes difficult to [implement] and then evaluate and know if it works or not” (Interview HM E08). | ||
| “If you can’t have full time, it would have been nice if she was there every morning or afternoon. Because the hospital never stops, so you can’t really say that there are days of the week when it’s good to be there” (Interview HM E04). | ||
|
| ||
| Coach and Clinicians’ Work Overload and Time Constraints | “The main constraints we had were the time and the added workload. […], this project came in addition to our work and there is no time that added for us. […] there were moments when I felt overloaded. It was difficult to absorb the workload for the ACE project. At some point, we can’t do everything, whether we do less for the project, or we do less for our work and it’s our personal performance that’s affected. […]”These projects are very interesting, but they are added to our regular work. There are times when it really does a lot, because the hospital goes into a lot of projects and then there are the committees, continuing education, teaching, and a lot of things in addition to our clinical work, so it’s certain that at some point, it’s a lot. […],”It was often difficult to have meetings with several people from different units in the hospital, our schedules are not the same. […], there were meetings where I was notified at the last minute and several that were cancelled […], I think we’ve had some real difficulties at that level”“ (Interview HM E04). | |
| “When implementing the project, we realized that it took a lot of time, more resources, more energy. […] “On the days my nurse was working on the project, she was freed from her duties to give her the chance to focus on the project. Again, it comes down to the release of resources to allow him to work on this project”“ (Interview HM E05). | ||
| “There was a big pitfall with the pharmacy. It’s been hard. This is a very specific role, especially for medications that the coach in transition of care was not always comfortable with. At first, we had the promise to have a pharmacist to be part of the project, but in reality, there was a huge workload to add that to her task” (Interview HM E10). | ||
| “We underestimated the execution and resources component once the intervention was implemented […], therefore underestimated the impact on professionals of the number of hours, the number of patients, the complexity of patients […] Every time you come out of a webinar, there was a lot of homework to do. […] you have to get involved, you have to do your homework, you have to meet the deadlines, you have to submit your report. […] everyone’s investment in the project team was phenomenal”(Interview HM E08). | ||
| “The reports that had to be completed were quite [tedious] and it took time to write the reports” (Interview HM E06). | ||
|
| ||
| Difficulties in involving the care unit’s medical staff | “I must say that the medical involvement in the project was not obvious. There was no resistance, but I would say I’m not sure all the doctors at the hospital knew about it.” (Interview HM E06). | |
| “We were hoping that both the coach and the doctor would be present at the seniors’ discharge meetings.” (Interview HM E04). | ||
|
| ||
| Difficulties in Establishing Systematic Links with Community Stakeholders | “We had links with the CCAC, links that we may not have focused on, that we didn’t solidify. So, we took […] advantage of the collaborative project to bring it back” (Interview HM E08). | |
|
| ||
| Issues and challenges | The project limited time and non-recurring funding | “A year is not enough for a project like this. We have probably improved, but if I have a recommendation for the next projects with the foundation and Mount Sinai, one year is not enough. Because the first few months take us to adjust, to find the resources. […], we are just beginning to consolidate, the time to hire someone, to guide him to show him the hospital to explain his role, to make the press releases, already three months have passed, and we have only nine months to implement and measure! “(Interview HM E10). |
| “We underestimated the execution and resources component once the intervention was implemented.” (Interview HM E08). | ||
|
| ||
| Adapting a new and innovative intervention to local context | “[...] advertising this new role and selecting patients who could benefit from the support of the coach in transition was work done at the beginning of the project, as soon as we received the foundation grant” (interview HM E10). | |
| Confusion and perception of the role overlap with other professionals | “Discharge management teams organize patient discharges. So, for me [coach], it wasn’t that. […] my main role was much more patient training and education to facilitate the transition, so that the patient leaves with the maximum information that will help him better manage his transition to home” (Interview HM E02). | |
| “It was very confusing for patients because they looked at me as a discharge management nurse [...]. I was in between the two roles, let’s say. They asked me questions, so I have the answers by contacting the discharge management team “ (Interview HM E03). | ||
| “At the beginning of the project, the coach had some pitfalls. People thought she was adding work to them. They didn’t really understand her role, so we had to go back to how to introduce her and to explain her role to distinguish between her role and the discharge management nurses. So, we had to clarify and support her.” (Interview HM E07) | ||
|
| ||
| Exceeding organizational capacity | “For sustainability, team support and leadership were always there. However, there is too much change on the ground, too many initiatives and too much demand from our people, in parallel to the ACE project. This vision of assessing the organizational capacity to conduct initiatives at the bedside, I think it is not being done well enough. […], we do not always make the right choices in prioritizing projects, nor in the organizational capacity to support them” (Interview HM E08). | |
|
| ||
| The challenges of extending hospital length of stay and influencing discharge for frail seniors | “We didn’t want to postpone patients’ discharge because the coach couldn’t see them, since she was only there two days a week “. (Interview HM E06). | |
| “[…] medical practice was not negatively influenced by the project, and it was well [perceived]”. (Interview HM E08). | ||
|
| ||
| Selecting and recruiting frail elderly people for the project | “The number of patients seen by the transition coach was below target. So, by broadening the criteria, we were simply supporting the possibility of achieving the original objectives. […], it was done in collaboration with professional practice” (Interview HM E01). | |
| “I sometimes had trouble finding patients for the procedure. Because they are too sick, do they really learn? There are some patients that we couldn’t take […], we had a little too strict criterion» (Interview HM E02). | ||
| “We have a “transition unit” at Montfort Hospital whose targeted clientele resembles the clients the transition coach was targeting. As a result, according to the criteria of inclusion and exclusion, several selected clients end up in the transition unit. So, we were losing several potential candidates. That’s why we had to broaden the criteria” (Interview HM E01). | ||
|
| ||
| Inability to demonstrate the impact of the project on organizational targets | “Unfortunately, with a small N, we have not been able to prove that the intervention of the coach in transition of care has had an impact on the readmission rate of patients in the unit. We didn’t have enough data. The project should have been continued for years to be able to prove that the project had an impact. […] We wanted immediate results that we would have been able to act on. But readmission rates are calculated after the end of the quarter, and then three months later. This delay was too long for a very short project. So that was another big pitfall that we didn’t really have control over.” (Interview HM E10) | |
| “If you can show that with a resource that costs $100,000, we are able to have a much lower readmission rate. We would be able to prove that it is worth hiring a resource and the hospital at that time would make the investment.” (Interview HM E07) | ||
| “Our readmission rate was just Montfort’s, which excludes other hospitals. […], we didn’t have data from the other centres, and it was also very difficult to find out if the patient had been readmitted to another hospital in our area.” (Interview HM E08) | ||
|
| ||
| Difficulties in conducting follow-up in the community | “Afterwards, we realized that post-discharge calls were very difficult. Making a call that lasts maybe 45 minutes or an hour is something that needs to be included in the workload. […], it was not realistic with the nurse’s position now, to ask her to make those calls, it was not manageable. So, we [had to abandon] these calls” (Interview HM E05). | |
|
| ||
| HÔTEL-DIEU DE LÉVIS HOSPITAL | ||
|
| ||
| INITIAL EXPECTATIONS AND GOALS | ||
|
| ||
| Collaborating with an integrated research project | “I really believe in integrated research, [we] really need to renew ourselves as an organization. […], for sure I need to do this type of project to be able to guide my evidence-based decision-making” (Interview HDL_E03). | |
|
| ||
| Experimenting innovative solutions for frail older adults’ needs | ||
|
| ||
| Contributing to the development of the CISSS Chaudière-Appalaches organization’s academic mission. | “[…] I also care about the University’s mission, it’s all factors that made me get involved in the project” (Interview HDL_E05). | |
|
| ||
| Collaborating to a local initiative for improving quality of elder care | “My personal expectations were to improve care for older clients and, concretely, that we come up with a solution for their transition. Of course, my concern was also to innovate” (Interview HDL_E02). | |
|
| ||
| PROJECT PERCEIVED RESULTS AND BENEFITS | ||
|
| ||
| Opportunity to prioritize the Specialized Approach to Senior Hospital Care and to implement several of its components | “For the older adults, I know we’re doing fall prevention, delirium prevention, I know we have a lot of strategies to engage patients as early as possible, etc. So basically, there is other Specialized Approach to Senior Hospital Care strategies that are being put in place, but it was another good occasion to prioritize this approach more.” (Interview HDL_E05) | |
|
| ||
| Opportunity to implement lasting change that continues to operate at HDL and the CISSS Chaudière-Appalaches; | “The initial ACE project was very hard with many frustrations, but it led to levers of change that continue to be exercised within the CISSS Chaudière-Appalaches, which is encouraging anyway.” (Interview HDL_E04) | |
|
| ||
| Strengthening the integrated research approach within the organization | “[…], and then having a strong connection with the Learning Wisdom project that has come to improve transitions, […], it was like an integrative whole in our integrated research perspective.” (Interview HDL_E03) | |
| “The project had benefits and interesting results despite the difficulties in implementing the initial intervention. […] it helps develop a strong partnership between [integrated researcher] and the nursing directorate, which has resulted in a CIHR grant and two postdoctoral fellowships.” (Interview HDL_E05) | ||
|
| ||
| Perceived cultural change in the organization | “There is also all the cultural change in what the right approach for the older person is. […] Certainly, along the way, a lot of work has been done on all the social assessments that the nurse has to do for a newly hospitalized patient.” (Interview HDL_E02) | |
|
| ||
| Opportunity to Review the Telemonitoring Service | “I took advantage of the ACE project to improve the telemonitoring service. […], I reviewed the entry points, the trajectory and the reference forms. […] I would say that there has not been much change in practice.” (Interview HDL_E06) | |
|
| ||
| FACILITATORS AND BARRIERS | ||
|
| ||
| Facilitators | ||
|
| ||
| Actors and resources | Contribution of the directorate leading the project and the ACE project manager | “The will and leadership of the [Director nursing], it was very useful” (Interview HDL_E02). |
| “It’s clear that [the project manager], as a dedicated person, was an essential person without her we could never have done many activities for the project” (Interview HDL_E04). | ||
|
| ||
| Research team contribution | “They helped us influence the direction and organization of the project in relation to best practices. Also, they were able to look for the tracking indicators and present these indicators to us. […] This team allowed us to look for innovative ideas, to learn from best practices and how we can do differently, because sometimes when we have our noses too glued on, we do not see other strategies” (Interview HDL_E06). | |
| “At the end of the project, we were allowed to evaluate the project’s implementation with additional resources paid for by our research team: a research nurse who was hired to offer telemonitoring to patients [and who] was not [part of the] hospital staff” (Interview HDL_E04). | ||
| “The research team worked very closely with the [project manager], among other things, for the development of the protocol and the tools to be used. This team was also there to coordinate the [QI] project. […], the research team helped get all the statistical data, all the information that needed to be followed up to the CFHI” (Interview HDL E02). | ||
|
| ||
| Canadian Foundation for Health Improvement and Mount Sinai Hospital Support | “I think it’s an important role. CFHI’s experts gave us sound advice, they allowed us to readjust, so they really had a coaching and leadership role. […], it allows us to be on the lookout for scientific data relevant to the project, to maintain an adequate level of knowledge, to network, to guide us also within the project: the type of project, the indicators, the [project alignment] we gave ourselves” (Interview HDL_E03). | |
| “The CFHI plays a coordinating role between different experts, it allows us to have a platform of knowledge and to know the latest standards, guidelines, I think the CFHI acts as a leader” (Interview HDL_E06). | ||
|
| ||
| Strategies | Patient recruitment for telemonitoring | “CFHI gave us feedback on the issues and proposed strategies on how to get around the issues raised, […] they were very supportive” (Interview HDL_E04).”We were put in touch with other health organizations, and we had the opportunity to learn about their projects and to comment if necessary” (Interview HDL_E01). |
| “It was difficult for us to offer telemonitoring. Finally, with the research team, we were able to find a [research nurse] who could offer it. […]”The patient can watch the video; he has the information on the telemonitoring service. Afterwards, the nurse can answer his questions and fill out the reference form. […], nurses were concerned about the overwork in connection with these forms. So, it was thought that the patient or his family could easily fill out the form” (Interview HDL_E02). | ||
| “In the time that was left, we had to recruit patients more specifically through a research nurse who had been hired” (Interview HDL_E04). | ||
|
| ||
| Barriers | ||
|
| ||
| Actors and resources | Limited resources (time and human resources) | “It would have required a budget that we didn’t have. […] Also, it would have taken longer than setting up this role with a group of people” (Interview HDL_E06). |
| “Lack of human resources was an important barrier, […] the organization’s inability to set up a coach in transition was an important barrier” (Interview HDL E03). | ||
| “Accessibility to services is more difficult, […], providing home services is much longer, at least waiting for services, remote monitoring is very accessible, can put in place a safety net while waiting for professional services” (Interview HDL E04). | ||
| Changes in the project’s actors and structure of governance | “Certainly, with the arrival and departure of several people, the lack of continuity of the initial vision of the project has hindered the project. I think that the departure of [the project initial organizational leader] with a clear initial vision of what [this person] wanted to do unfortunately hurt, the fact that [this person] was no longer there, it is not that [the replacement] did not necessarily have the same vision, but perhaps [this person] did not grasp everything that [the initial organizational leader] wanted to accomplish” (Interview HDL E04). | |
| “I [the initial organizational leader] had to be away for a long time, which meant that we changed leaders within the project, […] ..., it brought about a change in governance, that’s part of the issues that were identified” (HDL Interview E03). | ||
| “[The project manager], along the way, [this person’s] role changed, [this person] was appointed manager of a department. [This person] no longer had the same availability for the project” (Interview HDL E02). | ||
| “At first, when we wrote the application it was really for the emergency department and we had several emergency actors, but along the way a decision was made to try to implement telemonitoring in care units rather than in the emergency room. Initial team members were replaced by actors who were more present in the care units including unit leaders. […], the arrival of these people along the way with a project that was advanced may also have affected our team functioning.” (Interview HDL E04) | ||
| “Because stakeholders included over time were not part of our exchanges and discussions at the beginning, it became difficult for them to integrate and then judge the relevance of everything that was being put in place. We had our project agenda and we had not managed to get it implemented with them because they were not involved in the beginning.” (Interview HDL E04) | ||
| “There was a bit of talk about including people in oncology, other times we excluded them. At one point it was on such a unit, at some point it was another. We had several discussions to identify our patients and how we would [recruit] them. […] I think that since it came from two different directorates, in terms of the [ownership] it [took] a long time before we realized that we were working towards the same goal, but with different means. […] We were not at the project launch. We rallied because we realized that we had both similar projects, but it was more in a second [phase].” (Interview HDL E07) | ||
| “She [SAPA directorate] should have also played a leadership role, because they are responsible for interventions, including the transition from care to primary care, […] it is a trajectory that is two-headed, and the nursing directorate cannot set up this trajectory on its own; that starts from the hospital component and goes all the way to the primary care provider. […], so, their role was major, they [SAPA directorate] are a partner and an essential collaborator.” (Interview HDL E03) | ||
| “We had to rediscover the project to make sure that we were going to deliver something with the time left. […], it is sure that in relation to the involvement of the SAPA management, we made a great meeting to update [all stakeholders] on the project and the timelines to successfully implement the telemonitoring component.” (Interview HDL E02) | ||
| “There were a lot of managers around the table, especially from the nursing directorate.” (Interview HDL_E01) | ||
| “There are colleagues who were around the table, but that were more mid-level managers and at one point, we were going to make decisions that changed the work organization for some... Well, they weren’t the right actors.” (Interview HDL_E10) | ||
| “The project manager was the integrated researcher, in collaboration with the [clinical project manager] who was responsible for implementing interventions in care settings.” (Interview HDL_E03) | ||
| “I think if we had a patient partner who was constantly expressing the voice of patients, we might have identified more quickly what we should deliver to patients. The fact that our patient partner was not there from start to finish may have hurt. […] The patient partner, in my opinion, lost confidence in the project because most of the meetings were trying to resolve problems that, according to the patient partner and in my opinion, could be resolved fairly easily by an administrative decision. […] Unfortunately, there was a lot of bureaucracy, and the patient partner may have been discouraged by this bureaucracy which has greatly hindered the implementation of the project.” (Interview HDL_E04). | ||
|
| ||
| Lack of stakeholder involvement in project design and planning | “Initially, the submitted project was not thought through with [all] the stakeholders. […] One of the things that hurt the project, in the time frame we had, was that, from day one, the stakeholders were not part of the start-up of the project.” (HDL Interview E02) | |
| “For improvement to work, people need to be involved from the beginning. … we had the recipe; we had the solution and it had to be like that. […] something that stakeholders do not understand and do not find consistent is that they are working on projects that are not their own. It was a situation where we had to maneuver and readjust to make sure that we were going to be able to deliver something related to this project.” (HDL Interview E04) | ||
| “Between the time we got the grant and when I started participating in the project, there had been months that had gone by, and we were talking about my care environment and about the role of my clinicians and I wasn’t involved until they said we were at a dead-end, can you come and help us? […] I said: explain this to me! Imagine, I’m wasting a lot of time by what I need to know about what’s been worked on for maybe four months, and then you go… where and what your strategy is and what we’re going to do. We started to be effective when we ended the project.” (Interview HDL E07). | ||
|
| ||
| No Involvement of operational level clinicians in the project | “It would certainly have helped to have more [first line bedside] professionals around the table... […], but in mega-organizations like the one we have, I feel like it’s not yet part of the culture to have the people from the field. […], so, I think that would need to be better integrated …. [have] people that [work at] the bedside of patients on these committees.” (Interview HDL_E04) | |
|
| ||
| Difficulty involving HDL hospital physicians | “I think that’s what was missing in our project, it wasn’t the will that wasn’t there, but I think not having people [from the frontlines] who were involved in the decisions.” (Interview HDL E06) | |
|
| ||
| Overwork and lack of time to prepare and implement project activities | “It’s something we tried to set up inside ACE... systematically send a summary to the family doctors of the patient’s stay [after discharge], but when we tried to do it at the Hôtel-Dieu de Lévis, it was not possible... the involvement of the medical profession has never been [strong] to have it done systematically.” (Interview HDL E02) | |
| “I think the convenience assessment underestimated the work required for the project’s implementation, … when it came to implement the strategy, they saw the full workload so that’s why it was difficult to implement it.” (Interview HDL_E03) | ||
| “I was on another project; we were overwhelmed, and we didn’t have a director. […], it was just bad timing above all, maybe it was just too much. […] It was a major project, also a cross-cutting project […]. We weren’t involved in the project from the beginning, and we didn’t know how to adapt.” (Interview HDL E07) | ||
| “People were afraid that they would not have enough time to complete goals and tasks. […], there was a difficulty in having the necessary resources […], we were afraid of the overload associated with that.” (Interview HDL E06) | ||
| Issues and Challenges | 2015 Health system reform impact | “When we did the project, we were in the very beginning of merging the CISSS of Chaudière-Appalaches, with new people, new departments and new directorates, we were building the directorates; momentum in a transformational organization was really not ideal either” (Interview HDL E03). |
| “I think the ACE project has really come right into the organization transformation issues and has suffered from the consequences. That said, if you look at it from a management point of view, it’s very informative.” (Interview HDL E07) | ||
| “I think our organization wasn’t ready for the project, it wasn’t organized to receive the project exactly as planned. […] You feel that the heaviness of transformation is the ability of people to make a change decision. […] that decisions had to be made at another level and you couldn’t even identify who the new person could make that decision” (Interview HDL E05). | ||
| “The 2015 Reform brought about a major change in the system that meant that the desire for innovation and the desire to bring about change were simply not there” (Interview HDL 04). | ||
| “It was difficult, we were a team of managers who got to know each other and who were not at the same level.” (Interview HDL E06) | ||
| “I think that, in a context of change, we were not yet consolidated as an organization, as I tell you the new responsibilities and accountability, maybe the planned intervention was too great, the time was not long enough for the implementation.” (Interview HDL E03) | ||
|
| ||
| Confusion and overlap between the coach’s role and that of other professionals | “Even defining the coach’s role, it had been a whole saga, and it was clear that it was not an additional role that needed to be added, but to come to value what was already existing in the role of several professionals. […] I attended a meeting, and it was a professional coordinator who was very difficult. […] she had spoken out that it was not realistic to involve a new resource as a transition coach.” (Interview HDL E02) | |
| “In fact, what was asked of us, we already did. […] Basically, it is done on a small scale with the liaison team: discharge planning, taking care of the safety net and the tasks of the transition coach. […] as an expert liaison team, my team will plan a transition, integrate services and ensure that there is good discharge planning. […], so, it’s as if the project had no added value for the day-to-day work of our team.” (Interview HDL E07) | ||
| “The liaison nurses [discharge management nurses] were teaching patients or their relatives about medication, health status, warning signs [...], but this team certainly did not follow up systematically.” (Interview HDL_E06) | ||
| “[…] in the emergency room, we have members of the liaison team who are on site: a nurse and a social worker who are present seven days a week. These people provide links to already identified care sites for complex clients, or those with frequent visits. […] This role already existed in the function of several people. So instead of recreating a new role, we reactivated what was already existing.” (Interview HDL_E03) | ||
| “I think we need to establish the [transition coach] role and responsibility first, the areas specific to that person, the common areas and the sharing zones. For me the key to the project success would be to establish these areas well. […] In fact, at that time, we wanted to name the concern not to repeat what was already in place in the hospital. […], is to make sure that there is fluidity in activities without duplications.” (Interview HDL E01) | ||
|
| ||
| Confusion between research project and organizational QI project | “The integrated research in which the institution has invested is a new approach that brings all the challenges of improvement projects and research projects. It also brings the notion of accompaniment. […], but on both sides, really we’re at the beginning.” (Interview HDL_E05) | |
| “ACE is a research project, but we’ve started to do integrated research. […] It was both, it was the setting up of interventions in the field, with a structured research project.” (Interview HDL_E03) | ||
| “Another very important barrier is the ethical confusion between the QI project and the research project that has greatly damaged and swallowed many of our resources. It also led to a delay in the implementation of the project.” (Interview HDL E04) | ||
|
| ||
| Access to useful data | “At the time, someone had to extract the data, but they weren’t around the table in the committees. That’s why I’m saying there was a stakeholder issue, and it was one, so the research team or we had to extract the data.” (Interview HDL E02) | |
| “I don’t think the organization’s measurement capacity was there. Unfortunately, the organization, even if they say they can measure the quality of care, they do not have access to reliable databases or data, and I think they clearly need to enhance their ability to measure.” (Interview HDL E04) | ||
|
| ||
| Ethical issues | “[…] we wanted to conduct a methodologically rigorous evaluation. Our goal was also to publish what we were studying. The ethics committee evaluation was requested and that is where the cards got blurred. […] The other problem was that we approached the TSS-CA who had allowed us to have a free month for 180 patients, but the ethics committee unfortunately did not accept this incentive.” (HDL Interview E04) | |
| “The ethical process caused additional delays. I think that if it was only as a quality improvement project, we would have been able to carry out the project within reasonable time frames.” (Interview HDL 03) | ||
| “The HDL Hospital ethics committee, before becoming the ethics committee of the CISSS de Chaudière-Appalaches, dealt only with very clinical, biopharmaceutical projects. There has been a transformation in the past year to better integrate the concept of collaborative research and more psychosocial and organizational research.” (Interview HDL_E05) | ||
|
| ||
| Lack of a project’s clear communication plan | “Communication was really an issue within the project.” (Interview HDL E03) | |
| “Unfortunately, I don’t remember attending a meeting where the project was clearly presented […]. When someone says in the middle of a meeting: it’s not clear to me why you’re calling me and why I need to participate?”, and that we’re almost three quarters of the way to the end of the project … Well, there’s a problem. […] Information was not circulating within directorates!” (HDL Interview E02) | ||
| “There was no communication plan, there was no concerted action plan with the other [organizational] projects. […] I think it’s a question of communication, explanation, membership that has been difficult more at the organizational level. […] It’s as if it didn’t translate into the concreteness of what it represented… the implementation of the intervention itself. So, I think there was a misunderstanding of the project.” (Interview HDL E07) | ||
| “Regarding communication, there was a part done by the research team, but when they [the Bureau de projets organisationnels-Project management support representative] arrived, they helped us with communication, meetings organization, documents, reports and all that.” (Interview HDL_E01) | ||
| “There was confusion between the ACE project and the Specialized Approach to Senior Hospital approach. The communication did not make all stakeholders realize that the ACE project and the Specialized Approach to Senior Hospital approach were the same. In the organizational implementation of the Specialized Approach to Senior Hospital approach, the ACE project came for some as duplication when it was not at all the case, it was in continuity. […] we wondered about the links between the two projects, it was not easy to do, I felt like we were splitting tasks.” (Interview HDL E04) | ||
| “It’s super important, because often we come up with our big theories, we arrive with our data collections, we arrive with all kinds of tools when we go down to the field and then people don’t even find sense to what we ask them to do.” (Interview HDL E06) | ||
| An emphasis on planning instead of implementation | “It’s multifactorial obviously, but maybe having clear, precise mandates, with specific timelines, and with the establishment of very specific roles and responsibilities for the actors. And perhaps target the necessary actors, the actors who would be most relevant by their role, their function, etc.” (Interview HDL E01) | |
| “On project planning; I want to say that there would have been place for improvement, it was more at the “now that I’ve heard, now that I’ve consulted, I do what with it and I use it in what way?” (Interview HDL E07) | ||
| “We wanted to set up a project that was too perfect to start with. However, it is important to start somewhere with small steps that are easy to implement, measure and study changes, and act: do simple and fast PDSA cycles, evaluate and move forward!” (Interview HDL E04) | ||
|
| ||
| Lack of project planning | “I think we should have had a more operational committee to help us implement the strategy […], people are more there, and we talk more in the how with the teams. […] Of course, it’s important to have the leaders be able to make policy decisions, but the operational part should have really been there.” (Interview HDL E03) | |
| “There were a department head who was in the project, but [the person] didn’t understand that [the person] had to make the connection with the director, and I realized after a few weeks, a few months, that the director was not aware of the project, so I don’t know if the role of the people who were on the committee was clear to them and their responsibility and accountability within the project.” (HDL Interview E05) | ||
|
| ||
| Competition with other projects | “Since there were several projects simultaneously running in the CISSS surrounding the Specialized Approach to Senior Hospital approach, confusion also developed, namely what was one project versus another.” (HDL Interview E02) | |
| “We all had a common goal, but sometimes it lacked a bit of clarity. We often gathered the same actors around the different tables for each of the “pieces”, I would say different projects. […] I find that there was a lot of confusion between our project and the ACE project, although everyone agreed on the objective.” (Interview HDL E07) | ||
|
| ||
| Attempting to Implement Telemonitoring as a “Complex” Technological Innovation | “It had several organizational barriers … we thought that remote monitoring would be easy to install, finally it was not so easy. […] …for telemonitoring reference, who was going to do the screening? Who will show, discuss and present this service to patients? After that, who’s going to make the reference? There were really a lot of questions as people thought it still took time to present and offer the service.” (HDL Interview E06) | |
|
| ||
| Telemonitoring service cost | “Unfortunately, most of the patients who were offered telemonitoring refused it because it cost [money]. There were several reasons in fact that the research nurse documented. […] 3 out of 29 patients who were approached finally accepted it, so a large refusal rate.” (Interview HDL E04) | |
|
| ||
| Google Site’s knowledge-sharing platform security issues | “Even just wanting to use a new platform to improve communication was difficult. […] because there were a lot of technological barriers to sharing and access to the platform that was blocked by the hospital firewall that prevented people from having access to the platform. […] It was necessary to bring in the Information Technology (IT) Department to see how to develop the tool.” (Interview HDL E04) | |
ACE = Acute Care for Elders; CCAC = Community Care Access Centre; CFHI = Canadian Foundation for Healthcare Improvement; CFN = Canadian Frailty Network; CISSS = Centre Intégré de Santé et de services sociaux; PDSA = Plan, Do, Study, Act; SASHA = Specialized Approach to Senior Hospital (Quebec).
Funding Statement
El Kebir Ghandour received a CIHR Health System Impact Fellowship Award from the Canadian Institutes of Health Research (CIHR) in collaboration with the Centre intégré de santé et de services sociaux de Chaudière-Appalaches, from 2017 to 2018 (#388533). Patrick Archambault received a CIHR Embedded Clinician Researcher Award (#370937) and a Fonds de recherche du Québec—Santé (FRQS) Clinical Scholar Award (#283211). This project was supported by an Institut du Savoir Montfort—Pilot Project Grant (2017-10).
Footnotes
CONFLICT OF INTEREST DISCLOSURES
We have read and understood the Canadian Geriatrics Journal’s policy on conflicts of interest disclosure and declare we have none.
FUNDING
El Kebir Ghandour received a CIHR Health System Impact Fellowship Award from the Canadian Institutes of Health Research (CIHR) in collaboration with the Centre intégré de santé et de services sociaux de Chaudière-Appalaches, from 2017 to 2018 (#388533). Patrick Archambault received a CIHR Embedded Clinician Researcher Award (#370937) and a Fonds de recherche du Québec—Santé (FRQS) Clinical Scholar Award (#283211). This project was supported by an Institut du Savoir Montfort—Pilot Project Grant (2017-10). The Institut du Savoir Montfort had no role in the design and conduct of the study, in the analysis and interpretation of the data, or in the approval of the manuscript and the decision to submit the manuscript for publication.
REFERENCES
- 1. Kuluski K, Ho JW, Hans PK, Nelson M. Community care for people with complex care needs: bridging the gap between health and social care. Int J Integr Care. 2017 Jul;17(4):2. doi: 10.5334/ijic.2944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Canadian Frailty Network. Frailty matters. a growing health system challenge [Internet] Kingston, ON: CFN; 2018. [cited 2020 October 20]. Available from: https://www.cfn-nce.ca/frailty-matters/#1574890408921-bde36ff7-f581. [Google Scholar]
- 3. Chen X, Mao G, Leng SX. Frailty syndrome: an overview. Clin Intervent Aging. 2014 Mar;19:433–41. doi: 10.2147/CIA.S45300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tran K, Wright MD. Senior friendly hospital care: a review of guidelines [Internet]. [Internet] Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; 2019. [cited 2020 November 05]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542755/ [PubMed] [Google Scholar]
- 5.Canadian Medical Association (CMA) The state of seniors health care in Canada [Internet] Ottawa, ON: CMA; Sep, 2016. [cited 2022 August 13]. Available from: https://www.cma.ca/sites/default/files/2018-11/the-state-of-seniors-health-care-in-canada-september-2016.pdf. [Google Scholar]
- 6. Archambault PM, Rivard J, Smith PY, Sinha S, Morin M, LeBlanc A, et al. Learning integrated health system to mobilize context-adapted knowledge with a Wiki platform to improve the transitions of frail seniors from hospitals and emergency departments to the community (LEARNING WISDOM): protocol for a mixed-methods implementation study. JMIR Res Protoc. 2020 Aug 5;9(8):e17363. doi: 10.2196/17363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kahn JM, Angus DC. Going home on the right medications: prescription errors and transitions of care. JAMA. 2011 Aug 24;306(8):878–79. doi: 10.1001/jama.2011.1209. [DOI] [PubMed] [Google Scholar]
- 8. Le Berre M, Maimon G, Sourial N, Gueriton M, Vedel I. Impact of transitional care services for chronically ill older patients: a systematic evidence review. J Am Geriatr Soc. 2017 Jul;65(7):1597–608. doi: 10.1111/jgs.14828. [DOI] [PubMed] [Google Scholar]
- 9. Palmer RM, Landefeld CS, Kresevic D, Kowal J. A medical unit for the acute care of the elderly. J Am Geriatr Soc. 1994 May;42(5):545–52. doi: 10.1111/j.1532-5415.1994.tb04978.x. [DOI] [PubMed] [Google Scholar]
- 10. Sinha SK, Bennett J, Ramsden R, Bon J, Chalk T. Delivering improved patient and system outcomes for hospitalized older adults through an Acute Care for Elders Strategy. Healthc Manage Forum. 2018 Jul;31(4):126–32. doi: 10.1177/0840470418773108. [DOI] [PubMed] [Google Scholar]
- 11. Coleman EA, Parry C, Chalmers S, Min S. The care transitions intervention: Results of a randomized controlled trial. Arch Intern Med. 2006 Sep 25;166(17):1822–28. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 12.Yin RK. Case study research: design and methods. 5th ed. Thousand Oaks, CA: SAGE Publications; 2013. [Google Scholar]
- 13. Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): revised publication guidelines from a detailed consensus process. BMJ Qual Saf. 2016 Dec;25(12):986–992. doi: 10.1136/bmjqs-2015-004411. Epub 2015 Sep 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fortin J-P, Gagnon M-P, Lamothe L, editors. Evaluation of health care information and communication technologies: a framework to support decision-making. Proceedings of the IADIS International Conference e-Society; 2004; Avila, Spain. Available from: https://www.iadisportal.org/e-society-2004-proceedings. [Google Scholar]
- 15. Braun V, Clarke V, Terry G, Rohleder P, Lyons A. Qualitative research in clinical and health psychology. Qual Res Psychol. 2014 Oct 24;3(2):77–101. [Google Scholar]
- 16. Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. Can Med Assoc J. 2005 Aug 30;173(5):489–95. doi: 10.1503/cmaj.050051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. van Walraven C, Dhalla IA, Bell C, Etchells E, Stiell IG, Zarnke K, et al. Derivation and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. Can Med Assoc J. 2010 Apr 6;182(6):551–57. doi: 10.1503/cmaj.091117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ministère de la Santé et des Services sociaux (MSSS) Plan stratégique du ministère de la Santé et des Services sociaux 2015–2020—Mise à jour 2017 [Internet] Québec, QC: Canada Ministère de la Santé et des Services Sociaux (Québec); 2017. [cited 2018 October 20]. Available from: https://cdn-contenu.quebec.ca/cdn-contenu/adm/min/sante-services-sociaux/publications-adm/plan-strategique/PL_17-717-01W_MSSS.pdf. [Google Scholar]
- 19.Wong K, Ryan D, Liu B. Senior friendly hospital care across Ontario: summary report and recommendations [Internet] Ontario Local Health Integration Network; 2011. Sept, [cited 2019 March 10]. Available from: https://www.rgptoronto.ca/wp-content/uploads/2018/01/SFH_Provincial_Report-Summary_and_Recommendations_2011.pdf. [Google Scholar]
- 20. Vindrola-Padros C, Pape T, Utley M, Fulop NJ. The role of embedded research in quality improvement: a narrative review. BMJ Qual Saf. 2017 Jan 1;26(1):70–80. doi: 10.1136/bmjqs-2015-004877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wye L, Cramer H, Beckett K, Farr M, le May A, Carey J, et al. Collective knowledge brokering: the model and impact of an embedded team. Evidence & Policy. 2020 Aug 25;16(3):429–52. [Google Scholar]
- 22.Registered Nurses’ Association of Ontario (RNAO) Care Transitions [Internet] Toronto, ON: Registered Nurses’ Association of Ontario RNAO; 2014. Mar 20, [cited 2017 December 08]. Available from: https://rnao.ca/media/3167/download. [Google Scholar]
- 23.Gouvernement du Québec. Act to Modify the Organization and Governance of the Health and Social Services Network, in Particular by Abolishing the Regional Agencies, Chapter 0.7.2. [Internet] Québec, QC, Canada: Ministère de la Santé et des Services Sociaux (Québec); 2015. [updated January 1, 2023]. Available from: https://www.legisquebec.gouv.qc.ca/en/pdf/cs/O-7.2.pdf. [Google Scholar]
- 24. Christensen JKB. The emergence and unfolding of telemonitoring practices in different healthcare organizations. Int J Environ Res Public Health. 2018 Jan;15(1):61. doi: 10.3390/ijerph15010061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sathyamoorthy G.How a ‘bottom-up’ approach to innovation is making service improvements easier. Health Serv J (HSJ) [Internet] 2012. Feb 1, [cited 2021 February 10]. Available from: https://www.hsj.co.uk/efficiency/how-a-bottom-up-approach-to-innovation-is-making-service-improvements-easier/5040805.article.
- 26. Hesselink G, Vernooij-Dassen M, Pijnenborg L, Barach P, Gademan P, Dudzik-Urbaniak E, et al. Organizational culture: an important context for addressing and improving hospital to community patient discharge. Med Care. 2013 Jan 1;51(1):90–98. doi: 10.1097/MLR.0b013e31827632ec. [DOI] [PubMed] [Google Scholar]
- 27. Klundert JV, de Korne D, Yuan S, Wang F, van Wijngaarden J. ‘Hybrid’ top down bottom up health system innovation in rural China: a qualitative analysis. PLoS One. 2020 Oct 7;15(10):e0239307. doi: 10.1371/journal.pone.0239307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Dixon-Woods M, McNicol S, Martin G. Ten challenges in improving quality in healthcare: lessons from the Health Foundation’s programme evaluations and relevant literature. BMJ Qual Saf. 2012 Oct 1;21(10):876–84. doi: 10.1136/bmjqs-2011-000760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Jones B, Vaux E, Olsson-Brown A. How to get started in quality improvement. BMJ. 2019 Jan 17;364:k5408. doi: 10.1136/bmj.k5437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Fakha A, Groenvynck L, de Boer B, van Achterberg T, Hamers J, Verbeek H. A myriad of factors influencing the implementation of transitional care innovations: a scoping review. Implement Sci. 2021 Dec;16(1):21. doi: 10.1186/s13012-021-01087-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Devos G, Buelens M, Bouckenooghe D. Contribution of content, context, and process to understanding openness to organizational change: two experimental simulation studies. J Soc Psychol. 2007 Dec 1;147(6):607–30. doi: 10.3200/SOCP.147.6.607-630. [DOI] [PubMed] [Google Scholar]
- 32. Lamontagne F, Rowan KM, Guyatt G. Integrating research into clinical practice: challenges and solutions for Canada. Can Med Assoc J. 2021 Jan 25;193(4):E127–E131. doi: 10.1503/cmaj.202397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cabinet de la ministre responsable des Ainés et des Proches aidants. Maladie d’Alzheimer et autres troubles neurocognitifs majeurs—Un financement de 5 M$ pour soutenir la recherche [Internet] Ministère de la Santé et des Services Sociaux (Québec); mars 15, 2022. [cited 2022 March 30]. Available from: https://www.newswire.ca/fr/news-releases/maladie-d-alzheimer-et-autres-troubles-neurocognitifs-majeurs-un-financement-de-5-m-pour-soutenir-la-recherche-819933955.html. [Google Scholar]
- 34.Maher L, Gustafson D, Evans A. NHS sustainability model and guide [Internet] Institute for Innovation and Improvement; 2010. [cited 2018 March 12]. Available from: https://webarchive.nationalarchives.gov.uk/20160805122935/http://www.nhsiq.nhs.uk/media/2757778/nhs_sustainability_model_-_february_2010_1_.pdf. [Google Scholar]
- 35.Rappon T. The sustainment and sustainability of quality improvement initiatives for the health care of older adults [Doctoral thesis] Toronto: University of Toronto (Canada); 2021. [Google Scholar]