Abstract
Introduction
Millions of out-of-hospital cardiac arrests (OHCA) occur globally each year. Survival after OHCA can be improved with the use of automated external defibrillators (AED). The main strategy for facilitating bystander defibrillation has been fixed-location public access defibrillators (PADs). New strategies of mobile AEDs depart from the model of static PADs and have the potential to address known barriers to early defibrillation and improve outcomes.
Methods
Mobile AEDs was one of six focus topics for the Wolf Creek XVII Conference held on June 14–17, 2023, in Ann Arbor, Michigan, USA. Conference invitees included international thought leaders and scientists in the field of cardiac arrest resuscitation from academia and industry. Participants submitted via online survey knowledge gaps, barriers to translation and research priorities for each focus topic. Expert panels used the survey results and their own perspectives and insights to create and present a preliminary unranked list for each category that was debated, revised, and ranked by all attendees to identify the top 5 for each category.
Results
Top knowledge gaps center around understanding the impact of mobile AEDs on OHCA outcomes in various settings and the impact of novel AED technologies. Top barriers to translation include questionable public comfort/acceptance, financial/regulatory constraints, and a lack of centralized accountability. Top research priorities focus on understanding the impact of the mobile AED strategies and technologies on time to defibrillation and OHCA outcomes.
Conclusion
This work informs research agendas, funding priorities and policy decisions around using mobile AEDs to optimize prehospital response to OHCA.
Keywords: Mobile AEDs, Early defibrillation, EMS, Community first responders, Drones, Personal AEDs, Wolf Creek Conference
Introduction
Every year, there are approximately 350,000 EMS-treated out-of-hospital cardiac arrests (OHCA) in the United States and millions of OHCA globally.1, 2, 3 OHCA survival has remained largely unchanged at less than 10% for the past three decades, partially due to lack of rapid defibrillation.2, 3, 4, 5, 6 Early AED use is associated with significant increases in survival rates5, 7, 8, 9, 10 and several more productive life-years11 in patients with a shockable initial rhythm.
A defibrillator is most commonly brought to the scene and used by the responding prehospital providers; however, timely ground-based EMS response is challenged by distance, infrastructure, traffic, and geography, among other things. The median time interval from emergency call to scene arrival for EMS in the US is approximately seven minutes; the median time in rural settings doubles to over 14 minutes with nearly 10% of encounters taking 30 minutes or longer.12 These delays contribute to sub-optimal survival rates.13, 14
To mitigate limitations in EMS response time, static public access defibrillator (PADs) programs have been developed. Use of a PAD can improve survival of patients experiencing OHCA in a public area.15, 16 Improved survival has been observed even without AED shock delivery, potentially due to AED-provided CPR instructions.17, 18 Unfortunately, approximately 70% of OHCAs occur in residential settings where PADs are scarce.19 In public settings, time savings often rely on dispatch directing bystanders to the AED location.20 In rural areas, population density and distance limit the impact of PADs.21 As a result of these constraints, PADs are used prior to EMS arrival in less than 5% of OHCA21, 22, 23 and have not been shown to reduce time to first defibrillation at a population level.24
On this basis, it is time to consider the addition of alternate AED delivery methods to achieve earlier defibrillation for people who experience an OHCA. Mobile AED strategies refer to novel models of AED deployment involving portable AEDs, such as AED-equipped community first responders (CFRs), drone AED delivery systems, and personal AEDs.
Methods
Since its inception in 1975, the Wolf Creek Conference has a well-established tradition of providing a unique forum for robust intellectual exchange between thought leaders and scientists from academia and industry that focuses on advancing the science and practice of cardiac arrest resuscitation.25 The Wolf Creek XVII Conference was hosted by the Max Harry Weil Institute for Critical Care Research and Innovation in Ann Arbor, Michigan, USA on June 15–17, 2023.26
“Mobile AEDs” was one of six focus topics for the conference. Meeting invitees included international academic and industry scientists as well as thought leaders in the field of cardiac arrest resuscitation. All participants were required to complete conflict of interest disclosures. Prior to the meeting, all participants were asked via online survey to list up to three knowledge gaps, barriers to translation and research priorities for each topic. Participants were instructed that the topic of mobile AEDs would focus on optimizing the deployment and utilization of AEDs that can be delivered to the scene of an out-of-hospital cardiac arrest without having to be retrieved from a stationary location. Knowledge gaps were defined as areas where our understanding or knowledge is incomplete or limited. These gaps can arise due to various factors, such as lack of research, inadequate information, limited access to data or resources, or simply because the topic is new or complex. Barriers to translation were defined as obstacles that can prevent the successful transfer of knowledge or innovations from research or development settings to practical applications in the real world. Research priorities were defined as the areas of study that are considered most important or urgent by the scientific community or society as a whole. These priorities are often determined by a range of factors such as knowledge gaps, scientific breakthroughs, new challenges, societal needs, or funding opportunities.
Panels made up of experts in each topic used the survey results and their own perspectives and insights to create an initial unranked list of up to ten items for each category. During the conference, expert panelists provided an overview of the current state and potential future state of the field lay the groundwork for an informed debate. This was followed by presentation and initial ranking of the knowledge gaps, barriers to translation, and research priorities by all attendees using electronic voting, discussion and revision by the panel and attendees, and then re-ranking. The top five items in each category underwent final review on the last day of the conference. An overview of the current and potential future state of the field and prioritized results for Mobile AEDs are presented and discussed in this manuscript.
Current state
Community volunteer responder programs
There are two main types of community volunteer responder programs being implemented in various jurisdictions around the world.
The first type of program is built around a crowd-sourcing mobile device app that is downloaded by community members wanting to volunteer for OHCA response. For OHCA incidents within their immediate vicinity, volunteers received alerts with the OHCA location so that they can respond and initiate basic life support prior to EMS arrival. Some apps encourage early AED use by identifying nearby registered AEDs for the user. Examples of this program type include PulsePoint Respond (USA), GoodSAM (UK), and HeartRunner (Sweden). Users can be anonymous or known to the hosting organization. Requirements for prior certification vary by app. For instance, the PulsePoint app requires the user to attest that they are trained in CPR, while the GoodSAM app requires users to provide proof of CPR certification or medical professional licensure. The availability of this technology to enhance community response to OHCA has increased; a recent scoping review identified more than 25 unique mobile phone crowdsourcing technologies from 23 different countries.27 Despite the proliferation of this technology, high quality data on the efficacy of these apps is limited. Some of the most promising data comes out of the HeartRunner program, which has been shown to increase bystander defibrillation in OHCA when used prior to the arrival of EMS in both public and residential locations.28, 29
The second type of approach involves a more formal community volunteer responder program using trained and AED-equipped community members to supplement the EMS response, such as the Sandpiper Trust Wildcat program from Scotland. This program organized rural volunteers into 100 geographically-based teams who were trained on CPR and AED use and provided on-call OHCA coverage for their communities in conjunction with the EMS response. Early data demonstrates a significant improvement in response times with 100% AED application rate and the provision of excellent quality CPR.30 A similar program known as “Neighbors Saving Neighbors” is currently being studied in Ontario, Canada (https://engagefrontenac.ca/neighbours-saving-neighbours).
Drone AED delivery
For maximal efficiency, drones carrying AEDs would need to be automatically deployed from pre-determined locations specifically chosen to optimize regional coverage. Mathematical and geographic analysis suggest that optimally-located drones could result in robust improvements in the time to AED delivery while providing broader geographic AED coverage than traditional ground EMS.31, 32, 33, 34, 35, 36 Machine-based learning techniques can also optimize drone dispatch systems by identifying locations of OHCA where a drone-delivered AED would not arrive prior to a PAD or EMS-delivered AED.37 Computer modeling studies support the financial feasibility and cost-effectiveness of optimized drone delivery systems when compared to EMS-delivered AEDs,38, 39, 40, 41 but a viable drone AED network would require robust funding.41 Both simulated and real-world OHCA studies comparing the time to AED delivery via drone versus ground EMS have generally supported the idea that that drones may shorten AED delivery times.43, 44, 45, 46 Drone delivery of AEDs also results in faster bystander AED application than using PADs in simulated OHCA cases. 24, 47, 48 Current evidence negates that idea that bystanders would not be willing and able to interact successfully with a medical drone delivering an AED.24, 47, 48, 49, 50 There has been one published case a bystander successfully using a drone-delivered AED during a real-life OHCA response.51 In general, interviews with key stakeholders within healthcare and aviation regarding this concept have demonstrated broad support, while highlighting areas of concern such as operationalization of the system, privacy and safety issues, legal and regulatory requirements, technological limitations of current drones, financial liabilities, public buy-in, and the need for further research on the cost-effectiveness of a drone network.42 Fortunately, aviation regulatory bodies are currently working to address regulatory limitations,52, 53 while industry is attempting to improve drone technological capabilities.
Personal AEDs
Advances in defibrillator technology have allowed the development of small, ultra-portable AEDs designed for personal and home use including the CellAED (https://cellaed.io/row), Avive (https://avive.life/), and The Elliot (https://hearthero.com/). These new types of defibrillators aim to make AEDs more ubiquitous and more easily accessible for both public and residential OHCA, hoping to reduce the time to first defibrillation and improve OHCA outcomes when compared to EMS-delivered AEDs and PADs. The FIRST TRIAL is an ongoing cluster-randomized trial in Australia measuring whether a CellAED-equipped GoodSAM responder can improve 30-day hospital survival compared with having a GoodSAM responder without a CellAED (https://anzctr.org.au/Trial/Registration/TrialReview.aspx?id=383697).
Potential future state
A paradigm shift in AED deployment within society is required if we hope to achieve improved OHCA survival outcomes via reductions in time to first defibrillation. The dissemination of more advanced, next-generation defibrillator technology along with novel AED delivery mechanisms will be critical to ensure that an AED is immediately available for all OHCAs.
In the ideal future state, defibrillation technology will be ubiquitous. All AEDs, whether personal/portable AEDs, PADs, AEDs carried by CFRs, drone-based AEDs, or EMS-carried AEDs, will be inventoried, geolocated and remotely monitored for battery life. When 9-1-1 is activated and OHCA recognized, all emergency medical dispatchers (EMDs) will initiate standardized telecommunicator CPR instructions (tCPR) to ensure high quality bystander compressions. While tCPR is ongoing, the computer-aided dispatch (CAD) system will analyze the location of all the AEDs in the system to identify AEDs that could arrive most quickly on scene based on current weather/traffic patterns. By running this algorithm in the background, the CAD-based AED search will free the dispatcher to focus on lifesaving tCPR instructions and emotional support for the bystanders while the AEDs are being obtained, maintaining a patient- and family-centered EMS system.
If there is a personal, portable AED near the patient, the EMD will instruct the bystander on its use. If the AED that could arrive the quickest is carried on a medical drone, the system could auto-launch the drone and provide an estimated time of arrival so the dispatcher could guide bystanders/CFRs through its retrieval and use. The drone could also help the EMD monitor CPR quality via its integrated video feed. If the CAD system identifies that an AED-equipped CFR should be the quickest response, that person would be notified to respond via smartphone/tablet app. Nearby non-AED equipped CFRs would also be notified to retrieve the closest AED, whether a PAD, the drone-delivered AED, or a personal/portable AED. If any activated mechanism within the system could not respond, the software would move down the algorithm, analyzing more AED locations and triggering those AED mechanisms until an AED arrives on scene; this redundancy ensures system reliability. Professional EMS providers would be dispatched as per normal protocols. Although it sounds complex, technology currently used by many EMS systems for dynamic ambulance deployment would easily adapt to this model.
The AEDs used in this ideal system should be smaller, lighter, more portable, and incorporate novel, next-generation AED technology. This technology should perform continuous analysis of the patient’s electrophysiologic waveform during compressions to identify optimal timing and vector of defibrillation. The AEDs should also promote seamless information retrieval across the healthcare system by automatically transmitting waveform data to the monitors of the responding EMS crew and/or directly into EMS electronic health records (EHRs) via mechanisms similar to iPhone AirDrop® (Apple, Cupertino, California). The EMS monitor or EHR should then be linked to the hospital EHR to facilitate early insight into the OHCA (rhythm, duration, CPR quality etc.) by the receiving institution’s resuscitation team, while also enabling the EMS crew to obtain outcome data for quality improvement purposes.
Knowledge gaps
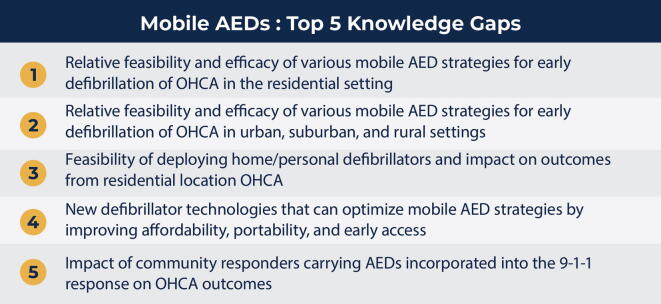
The top five knowledge gaps identified by the conference participants are listed in Fig. 1 and discussed below. Additional knowledge gaps can be found in the supplemental figure.
-
1.
Relative feasibility and efficacy of various mobile AED strategies for early defibrillation of OHCA in the residential setting.
Fig. 1.
Top 5 Knowledge Gaps.
The true feasibility and impact of any mobile AED strategy on patient-centered outcomes from OHCA in the residential setting is yet to be fully explored. The efficacy of CFRs is the most robustly supported by the evidence described above, while medical delivery drones are essentially unstudied in real world residential OHCA. Even less understood is the feasibility and efficacy of integrating multiple mobile AED concepts into a seamless, multidimensional OHCA response framework. The conceptual and theoretical impact of these strategies still waits to be proven through rigorous research and analysis.
-
2.
Relative feasibility and efficacy of various mobile AED strategies for early defibrillation of OHCA in urban, suburban, and rural settings.
It remains unknown whether the various mobile AED strategies are feasible and effective in all rural, suburban, and urban settings, or if specific approaches are best suited to specific settings. A higher population density increases the chance that a CFR is nearby and can respond to an OHCA; however, heavy traffic and high-rise apartments may limit patient access. In low density rural settings, the ability of a medical drone to respond rapidly to the scene may be more effective than a CFR due to low population density. Portable, personal AEDs should theoretically function well in all locations, but the reliance on consumer purchasing habits and technology maintenance could be problematic in lower income areas. In the end, we do not yet understand the feasibility or effectiveness of any of the mobile AED strategies in specific population settings and geographic locations.
-
3.
Feasibility of deploying home/personal defibrillators and impact on outcomes from residential location OHCA.
We do not know if the availability of a personal AEDs in the home would decrease time to first defibrillation at the population level and improve OHCA outcomes. As the HAT trial demonstrated,54 there are important knowledge gaps regarding family member willingness and ability to use AEDs in addition to calling 9-1-1 and starting CPR in residential OHCA. Our lack of knowledge regarding the feasibility and efficacy of portable, personal AEDs in the residential setting must be addressed.
-
4.
New defibrillator technologies that can optimize mobile AED strategies by improving affordability, portability, and early access.
For mobile AED strategies to be successful, AED technology must evolve beyond bulky, heavy AEDs that are cost prohibitive towards AEDs that are smaller, lighter, and more user-friendly with regards to cost. The impact of these personal, portable, high-tech, next-generation AEDs on time to first defibrillation and OHCA outcomes at a population level is unknown but may boost the feasibility and efficacy of all the mobile AED approaches.
-
5.
Impact of community responders carrying AEDs incorporated into the 9-1-1 response on OHCA outcomes.
Although there is some support in the literature reviewed above for the concept of AED-equipped CFRs, there is a lack of robust, convincing evidence supporting a positive impact of AED-equipped CFRs on OHCA survival with good neurological outcome at a population level. We recognize that the feasibility and community acceptance of a non-professional AED-equipped CFR may be influenced by cultural norms.
Dissenting Opinions
There was robust discussion regarding utilizing a just-in-time training app for delivery (Amazon, UPS) and ridesharing (Uber, Lyft) drivers instructed as community responders to increase their comfort with AEDs/CPR and thus enhance the likelihood they will respond. The impact of incentivizing CFRs to respond with monetary rewards and social recognition was also considered. A debate was held regarding the cost-benefit ratio of these systems; specifically, the question arose as to whether the money would be better spent purchasing and deploying more PADs and strengthening current EMS response ability. There was also robust conversation regarding the responsibility of the dispatch center when using mobile AED strategies and how these approaches would be integrated with dispatch centers.
Barriers to translation
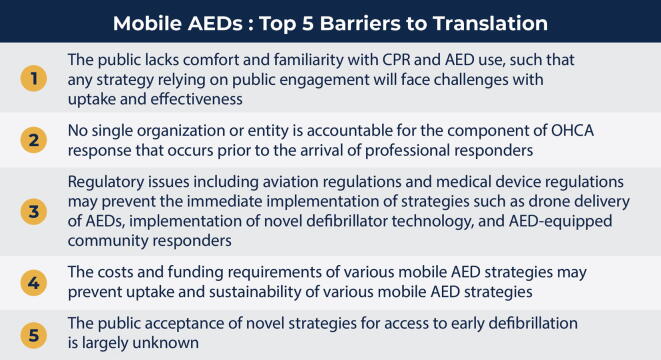
The top five barriers to translation identified by the conference participants are listed in Fig. 2 and discussed below. Additional barriers to translation can be found in the supplemental figure.
-
1.
The public lacks comfort and familiarity with CPR and ARD use, such that any strategy relying on public engagement will face challenges with uptake and effectiveness.
Fig. 2.
Top 5 Barriers to Translation.
In our current system, public knowledge concerning AEDs and CPR is poor and limits our attempt to improve OHCA outcomes via implementation of mobile AED strategies. Layperson discomfort with novel next-generation AED technologies could worsen time to first defibrillation by preventing their use by a layperson. Mistrust or uncertainty regarding non-professional responders may preclude public acceptance of CFR presence and AED use. Delivering an AED to a prehospital scene via drone will not impact OHCA outcomes if the AED is unused or improperly used; bystanders within the community must be willing and able to appropriately use an AED in order for this strategy to be effective.55 Public comfort and knowledge are barriers to translation of these novel strategies and must be addressed for them to be implemented.
-
2.
No single organization or entity is accountable for the component of OHCA response that occurs prior to the arrival of professional responders.
In most communities around the world, there is a general lack of accountability for components of the Chain of Survival that occur prior to the arrival of EMS. While EMS agencies are accountable for paramedic performance and metrics, and hospitals are accountable for the care provided to a cardiac arrest patient in the hospital, no single organization is responsible for the community response to cardiac arrest including bystander CPR and early defibrillation. From one community to another, there is no consistency in organizational responsibility at the local level (e.g., government, EMS, Fire, or community organizations) for minimum standards with respect to early recognition of cardiac arrest, bystander CPR and early defibrillation. This could be addressed with legislative or regulatory tools at the national or regional level to assign accountability to a particular type of organization which could, in turn, lead to rapid, coordinated, and innovative solutions.
-
3.
Regulatory issues including aviation regulations and medical device regulations may prevent the immediate implementation of strategies such as drone delivery of AEDs, implementation of novel defibrillator technology, and AED equipped community responders
We recognize that testing and approval of novel technologies and systems to safeguard public and patient safety is necessary and appropriate. There are significant regulatory limitations that will need to be addressed prior to implementation of the various mobile AED strategies. For CFRs, there are regulatory and legal concerns regarding, licensure requirements, training and compliance standards, and privacy procedures. For next-generation portable, private AED technologies, there exist federal and state regulations regarding certification, transport, and use of novel medical supplies. Specific to drones, aviation regulatory bodies currently limit flight operations in a manner that precludes drone response to the majority of OHCA, creating a barrier to implementation of this mobile AED strategy. Regulatory oversights must evolve to permit rapid adoption of each mobile AED strategy in order to minimize the large number of salvageable lives lost to OHCA each year.
-
4.
The costs and funding requirements of various mobile AED strategies may prevent uptake and sustainability of various mobile AED strategies.
Financial support will be needed to support the research and development of next-generation, personal, portable AED technologies. Stable monetary sources will be required for implementation and maintenance of mobile AED programs, including lobbying for regulatory updates, building needed infrastructure (drone hangers, CFR training programs), streamlining programmatic integration with EMS dispatch, promoting community education, acceptance, and involvement, and maintaining the programs once launched. Funding will be needed to support robust research and clinical trials evaluating the effect of each mobile AED strategy. After program implementation, the financial burden of liability insurance and the cost of iterative quality assurance/quality improvement processes may prove fiscally restrictive. Supporting growth and expansion of the programs will demand further sources of capital. A comprehensive, public–private collaboration may be required to adequately research, execute, sustain, and grow a long-term mobile AED vision. Possible sources include grants, municipal and federal monies, EMS agencies, insurance companies, philanthropic groups, medical professional organizations, and public tax millage.
-
5.
The public acceptance of novel strategies for access to early defibrillation is largely unknown.
Changes to the typical EMS emergency response paradigm may create uncertainty and mistrust in a large portion of the population. Even if the previous four barriers are overcome, the lay community may still simply not understand or accept a change to the typical emergency response for OHCA. A concerted effort and public information campaign to ensure acceptance will likely be required for any of the mobile AED strategies discussed here.
Dissenting Opinions
There were no dissenting opinions articulated after ballot closure.
Research priorities
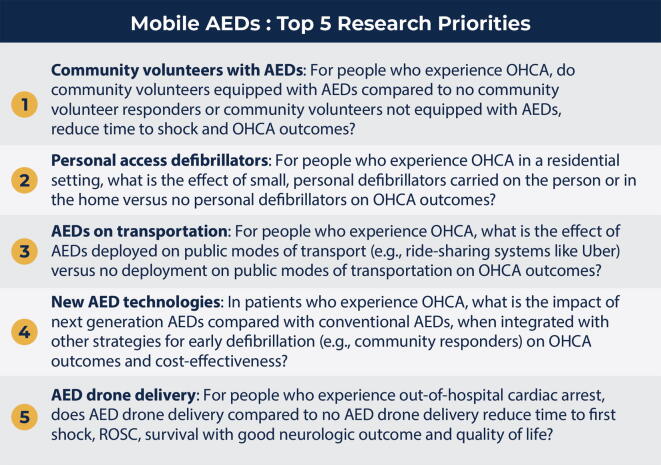
The top five research priorities identified by the conference participants are listed in Fig. 3 and discussed below. Additional research priorities can be found in the supplemental figure.
-
1.
Community volunteers with AEDs: For people who experience OHCA, do community volunteers equipped with AEDs compared to no community volunteer responders or community volunteers not equipped with AEDs, reduce time to shock and OHCA outcomes?
Fig. 3.
Top 5 Research Priorities.
It is unknown whether CFRs with an AED can improve outcomes compared to the current CFR model. AED equipped CFRs eliminate the necessity to retrieve an AED located by the app prior to attending to the patient, resulting in the potential to decrease OHCA response time and time to first shock. This paradigm is currently being assessed in the FIRST trial as noted earlier (https://anzctr.org.au/Trial/Registration/TrialReview.aspx?id=383697), but it will need further large, randomized controlled trials to enhance generalizability.
-
2.
Personal access defibrillators: For people who experience OHCA in a residential setting, what is the effect of small, personal defibrillators carried on the person or in the home versus no personal defibrillators on OHCA outcomes?
Delay to defibrillation in residential settings may be decreased if a family member is able to use a personal, portable AED as soon as the OHCA is recognized. However, ubiquitous AED availability and training may not linearly predict or promote AED use in real-world OHCA,53 emphasizing the need to study the impact of personal, portable AEDs on residential OHCA time to defibrillation and survival outcomes. We must analyze separately the impact of portable AEDs that are carried on the person and the impact of personal AEDs stored in a static location within the home; it is possible that the latter is less effective in part due to the need to retrieve it during an OHCA.
-
3.
AEDs on transportation: For people who experience OHCA, what is the effect of AEDs deployed on public modes of transport (e.g., ride-sharing systems like Uber) versus no deployment on public modes of transportation on OHCA outcomes?
EMS systems that include AED-equipped medical first responders such as police in their 9-1-1 response have usually shown a decrease in time to first defibrillation by increasing the pool of individuals able to intervene.56 The pervasive presence of delivery trucks and ride-sharing-based public transport could be leveraged similarly; by training them as AED-equipped CFRs, a system could employ a crowdsourcing app to notify and divert drivers to the scene of a nearby OHCA, multiplying the pool of first responders in a way that is not currently possible otherwise. It is thus imperative that we prioritize research analyzing the impact of training and equipping drivers of publicly accessible mode of transport with AEDs on the time to first defibrillation and OHCA outcomes at a population level.
-
4.
New AED technologies: In patients who experience OHCA, what is the impact of next generation AEDs compared with conventional AEDs when integrated with other strategies doe early defibrillation (e.g., community responders) on OHCA outcomes and cost-effectiveness?
New generation AEDs that are smaller, simpler, and more portable (pocket-sized) could dramatically impact the frequency of AED use. Improved AED algorithms that employ filtering software that enables earlier determination of VF could also play a role in improving first shock success.57 We should prioritize research that studies next generation AED technology; we must analyze if next generation AEDs that are portable, personal, less expensive and able to identify and intervene on shockable rhythms during active compressions will improve decrease time to first defibrillation and improve OHCA outcomes.
-
5.
AED drone delivery: For people who experience out-of-hospital cardiac arrest, does AED drone delivery compared to no AED drone delivery reduce time to first shock, ROSC, survival with good neurological outcome, and quality of life?
Drone delivery of AED’s is an alluring method to reduce time to first defibrillation, but the real-world impact of drone AED delivery on OHCA outcomes is untested in clinical trials due to regulatory, logistical, operational, and financial constraints. Once these are overcome, we must evaluate the impact of drone delivery of AEDs on the time to first defibrillation in OHCA and OHCA outcomes on a population level. We need to assess how the physical and operational characteristics of various drone models impacts the acceptability of the system to the public and resultant ability of bystanders to utilize the delivered AED. The flight characteristics and capabilities of various drone models may also impact their effectiveness in OHCA response. We should seek to understand the ideal combination of drone/AED by comparing the impact of drone-delivered conventional AEDs to novel next generation AEDs. Then we must pursue real world clinical trials to understand if using drones to deliver AEDs can improve time to first defibrillation and OHCA outcomes at a population level compared to the impact of conventional AED-use models such as PADs and EMS in urban, suburban, and rural areas.
Dissenting Opinions
Given the robust evidence proving the effectiveness of earlier AED application in OHCA as noted previously, some members of the audience questioned the ethical premise of studying the effectiveness of mobile AED strategies in randomized control trials; it was felt that one could not ethically randomize a portion of OHCA cases to not receive an earlier AED. Others highlighted that before these questions could be adequately researched, the resuscitation science community needed to focus on improving the public awareness of what an AED is; otherwise, the accuracy and ability of the studies to demonstrate impact would be limited. Others articulated disappointment in the use of PICO-style questions due to the inherent bias against qualitative research.
Conclusions
As with all innovative concepts, there are significant knowledge gaps with mobile AEDs that must be acknowledged for the technology to progress to reality. The development of prioritized research questions to address these gaps should inform future work in the field. Overcoming the barriers to translation described above will require significant investment and collaborative efforts between clinicians, scientists, researchers, industry, government, and community activists. If these aims can be achieved, mobile AEDs have the potential to significantly decrease the time to first defibrillation in OHCA and achieve substantial improvements in OHCA patient-centered outcomes.
CRediT authorship contribution statement
Christine M. Brent: Conceptualization, Investigation, Writing – original draft, Writing – review & editing, Project administration. Sheldon Cheskes: Conceptualization, Investigation, Writing – original draft, Writing – review & editing. Maaret Castrén: Conceptualization, Investigation, Writing – review & editing. Steve Brooks: Conceptualization, Investigation, Writing – original draft, Writing – review & editing, Supervision.
Declaration of Competing Interest
Dr. Brent has received grant funding from Toyota Motors North America for research into drone delivery of multimodal medical kits for bystander interventions in prehospital emergencies. Dr. Brooks is the Chief Medical Officer for Rapid Response Revival, a defibrillator manufacturer that makes the CellAED. He is also a shareholder in this company. Dr. Brooks has received in-kind support for research from GoodSAM and SaveStation. He receives funding from the Canadian Institutes for Health Research for research on the PulsePoint mobile device app. He also receives funding from the Ontario Ministry of Health for the study of a community volunteer responder program. This study is also supported by Action First Aid, an AED distributor in Canada, through in-kind supply of refurbished defibrillators. The GoodSAM app provided discounted services for use in this study. Dr. Cheskes sits on the Advisory Board of Drone Delivery Canada and has received grant funding from Zoll Medical Inc. for research on the use of drones for time sensitive medical emergencies. Dr. Cheskes has also received grant funding from the Cardiovascular Network of Canada for research into the use of drones in rural and remote cardiac arrest. All other authors report no current relevant financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The study team acknowledges the Weill Critical Care Institute at the University of Michigan for hosting and offering audiovisual support during the Wolff Creek Conference and providing data visualization support in the form of tables.
Footnotes
Supplementary material to this article can be found online at https://doi.org/10.1016/j.resplu.2023.100500.
Contributor Information
Christine M. Brent, Email: martinek@med.umich.edu.
Sheldon Cheskes, Email: sheldon.cheskes@sunnybrook.ca.
Maaret Castrén, Email: maaret.castren@hus.fi.
Steven C. Brooks, Email: Steven.Brooks@kingstonhsc.ca.
Appendix A. Supplementary material
The following are the Supplementary material to this article:
References
- 1.Gräsner J.T., Wnent J., Herlitz J., et al. Survival after out-of-hospital cardiac arrest in Europe—Results of the EuReCa TWO study. Resuscitation. 2020;148:218–226. doi: 10.1016/j.resuscitation.2019.12.042. [DOI] [PubMed] [Google Scholar]
- 2.Zegre-Hemsey J.K., Grewe M.E., Johnson A., Bogle B.M., Arnold E., Rosamond W.D. A feasibility study to assess delivery of automated external defibrillators via drones in simulated cardiac arrest-users’ experiences and the human-drone interaction. Circulation. 2019;140 doi: 10.1161/circ.140.suppl_1.13018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kiguchi T., Okubo M., Nishiyama C., et al. Out-of-hospital cardiac arrest across the World: First report from the International Liaison Committee on Resuscitation (ILCOR) Resuscitation. 2020;152:39–49. doi: 10.1016/j.resuscitation.2020.02.044. [DOI] [PubMed] [Google Scholar]
- 4.Ong M.E.H., Perkins G.D., Cariou A. Out-of-hospital cardiac arrest: prehospital management. Lancet Lond Engl. 2018;391:980–988. doi: 10.1016/S0140-6736(18)30316-7. [DOI] [PubMed] [Google Scholar]
- 5.Bækgaard J.S., Viereck S., Møller T.P., Ersbøll A.K., Lippert F., Folke F. The effects of public access defibrillation on survival after out-of-hospital cardiac arrest: A systematic review of observational studies. Circulation. 2017;136:954–965. doi: 10.1161/CIRCULATIONAHA.117.029067. [DOI] [PubMed] [Google Scholar]
- 6.Sasson C., Rogers M.A.M., Dahl J., Kellermann A.L. Predictors of survival from out-of-hospital cardiac arrest: A systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- 7.Valenzuela T.D., Roe D.J., Cretin S., Spaite D.W., Larsen M.P. Estimating effectiveness of cardiac arrest interventions: a logistic regression survival model. Circulation. 1997;96:3308–3313. doi: 10.1161/01.cir.96.10.3308. [DOI] [PubMed] [Google Scholar]
- 8.Savastano S., Baldi E., Compagnoni S., Fracchia R., Ristagno G., Grieco N. The automated external defibrillator, an underused simple life-saving device: a review of the literature. A joint document from the Italian Resuscitation Council (IRC) and Associazione Italiana di Aritmologia e Cardiostimolazione (AIAC) J Cardiovasc Med Hagerstown Md. 2020;21:733–739. doi: 10.2459/JCM.0000000000001047. [DOI] [PubMed] [Google Scholar]
- 9.Watts D.D. Defibrillation by basic emergency medical technicians: effect on survival. Ann Emerg Med. 1995;26:635–639. doi: 10.1016/s0196-0644(95)70017-x. [DOI] [PubMed] [Google Scholar]
- 10.Blom M.T., Beesems S.G., Homma P.C.M., et al. Improved survival after out-of-hospital cardiac arrest and use of automated external defibrillators. Circulation. 2014;130:1868–1875. doi: 10.1161/CIRCULATIONAHA.114.010905. [DOI] [PubMed] [Google Scholar]
- 11.Rao P., Kern K.B. Improving community survival rates from out-of-hospital cardiac arrest. Curr Cardiol Rev. 2018;14:79–84. doi: 10.2174/1573403X14666180507160555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mell H.K., Mumma S.N., Hiestand B., Carr B.G., Holland T., Stopyra J. Emergency medical services response times in rural, suburban, and urban areas. JAMA Surg. 2017;152:983–984. doi: 10.1001/jamasurg.2017.2230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cui E.R., Beja-Glasser A., Fernandez A.R., Grover J.M., Mann N.C., Patel M.D. Emergency medical services time intervals for acute chest pain in the United States, 2015–2016. Prehospital Emerg Care Off J Natl Assoc EMS Physicians Natl Assoc State EMS Dir. 2020;24:557–565. doi: 10.1080/10903127.2019.1676346. [DOI] [PubMed] [Google Scholar]
- 14.Alanazy A.R.M., Wark S., Fraser J., Nagle A. Factors impacting patient outcomes associated with use of emergency medical services operating in urban versus rural areas: A systematic review. Int J Environ Res Public Health. 2019;16 doi: 10.3390/ijerph16101728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nehme Z., Andrew E., Bernard S., Haskins B., Smith K. Trends in survival from out-of-hospital cardiac arrests defibrillated by paramedics, first responders and bystanders. Resuscitation. 2019;143:85–91. doi: 10.1016/j.resuscitation.2019.08.018. [DOI] [PubMed] [Google Scholar]
- 16.Malta Hansen C., Kragholm K., Pearson D.A., et al. Association of bystander and first-responder intervention with survival after out-of-hospital cardiac arrest in North Carolina, 2010–2013. J Am Med Assoc. 2015;314:255–264. doi: 10.1001/jama.2015.7938. [DOI] [PubMed] [Google Scholar]
- 17.Weisfeldt M., Sitlani C., Ornato J., et al. Survival after application of automatic external defibrillators before arrival of the emergency medical system. J Am Coll Cardiol. 2010;55:1713–1720. doi: 10.1016/j.jacc.2009.11.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pollack R.A., Brown S.P., May S., Rea T., Kudenchuk P.J., Weisfeldt M.L. Bystander automated external defibrillator application in non-shockable out-of-hospital cardiac arrest. Resuscitation. 2019;137:168–174. doi: 10.1016/j.resuscitation.2019.02.007. [DOI] [PubMed] [Google Scholar]
- 19.Virani S.S., Alonso A., Benjamin E.J., et al. Heart disease and stroke statistics-2020 update: A report from the American Heart Association. Circulation. 2020;141:e139–e596. doi: 10.1161/CIR.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 20.Johnson A.M., Cunningham C.J., Zégre-Hemsey J.K., et al. Out-of-hospital cardiac arrest bystander defibrillator search time and experience with and without directional assistance: A randomized simulation trial in a community setting. Simul Healthc J Soc Simul Healthc. 2021 doi: 10.1097/SIH.0000000000000582. Published online June 1, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zègre-Hemsey J.K., Bogle B., Cunningham C.J., Snyder K., Rosamond W. Delivery of automated external defibrillators (AED) by drones: Implications for emergency cardiac care. Curr Cardiovasc Risk Rep. 2018;12 doi: 10.1007/s12170-018-0589-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hawkes C., Booth S., Ji C., et al. Epidemiology and outcomes from out-of-hospital cardiac arrests in England. Resuscitation. 2017;110:133–140. doi: 10.1016/j.resuscitation.2016.10.030. [DOI] [PubMed] [Google Scholar]
- 23.Rosamond W.D., Johnson A.M., Bogle B.M., et al. Drone delivery of an automated external defibrillator. N Engl J Med. 2020;383:1186–1188. doi: 10.1056/NEJMc1915956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cone D.C., Burns K., Maciejewski K., Dziura J., McNally B., Vellano K. Sudden cardiac arrest survival in HEARTSafe communities. Resuscitation. 2020;146:13–18. doi: 10.1016/j.resuscitation.2019.10.029. [DOI] [PubMed] [Google Scholar]
- 25.Neumar R.W. Wolf Creek XVII Part 1: The future of cardiac arrest resuscitation. Resuscitation Plus. 2023;16 doi: 10.1016/j.resplu.2023.100504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Neumar R.W. and Tang W., Wolf Creek XVII Part 2: The origin, evolution and impact of the wolf creek conferences, Resuscitation Plus, 2023;16:100505. 10.1016/j.resplu.2023.100505. [DOI] [PMC free article] [PubMed]
- 27.Valeriano A., Van Heer S., de Champlain F., Brooks C., S. Crowdsourcing to save lives: A scoping review of bystander alert technologies for out-of-hospital cardiac arrest. Resuscitation. 2021;158 doi: 10.1016/j.resuscitation.2020.10.035. [DOI] [PubMed] [Google Scholar]
- 28.Andelius L., Malta Hansen C., Lippert F.K., et al. Smartphone activation of citizen responders to facilitate defibrillation in out-of-hospital cardiac arrest. J Am Coll Cardiol. 2020;76:43–53. doi: 10.1016/j.jacc.2020.04.073. [DOI] [PubMed] [Google Scholar]
- 29.Andelius L., Malta Hansen C., Jonsson M., et al. Smartphone-activated volunteer responders and bystander defibrillation for out-of-hospital cardiac arrest in private homes and public locations. Eur Heart J Acute Cardiovasc Care. 2023;12:87–95. doi: 10.1093/ehjacc/zuac165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Clegg G., Fickling K. The Sandpiper Trust; Edinburgh, Scotland: 2018. The sandpiper wildcat program: Annual report February 2017–February 2018; p. 2018. [Google Scholar]
- 31.Bogle B.M., Rosamond W.D., Snyder K.T., Zègre-Hemsey J.K. The case for drone-assisted emergency response to cardiac arrest: An optimized statewide deployment approach. N C Med J. 2019;80:204–212. doi: 10.18043/ncm.80.4.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Boutilier J.J., Brooks S.C., Janmohamed A., et al. Optimizing a drone network to deliver automated external defibrillators. Circulation. 2017;135:2454–2465. doi: 10.1161/circulationaha.116.026318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pulver A., Wei R., Mann C. Locating AED enabled medical drones to enhance cardiac arrest response times. Prehosp Emerg Care. 2016;20:378–389. doi: 10.3109/10903127.2015.1115932. [DOI] [PubMed] [Google Scholar]
- 34.Schierbeck S., Nord A., Svensson L., et al. National coverage of out-of-hospital cardiac arrests using automated external defibrillator-equipped drones – A geographical information system analysis. Resuscitation. 2021;163:136–145. doi: 10.1016/j.resuscitation.2021.02.040. [DOI] [PubMed] [Google Scholar]
- 35.Ho A.F.W., Pourghaderi A.R., Ong M.E.H. Drone-delivered automated external defibrillators: How to site them? Resuscitation. 2021 doi: 10.1016/j.resuscitation.2021.04.011. [DOI] [PubMed] [Google Scholar]
- 36.Derkenne C., Jost D., Miron De L’Espinay A., et al. Automatic external defibrillator provided by unmanned aerial vehicle (drone) in Greater Paris: A real world-based simulation. Resuscitation. 2021;162:259–265. doi: 10.1016/j.resuscitation.2021.03.012. [DOI] [PubMed] [Google Scholar]
- 37.Chu J., Leung K.H.B., Snobelen P., et al. Machine learning-based dispatch of drone-delivered defibrillators for out-of-hospital cardiac arrest. Resuscitation. 2021;162:120–127. doi: 10.1016/j.resuscitation.2021.02.028. [DOI] [PubMed] [Google Scholar]
- 38.Bauer J., Moormann D., Strametz R., Groneberg D.A. Development of unmanned aerial vehicle (UAV) networks delivering early defibrillation for out-of-hospital cardiac arrests (OHCA) in areas lacking timely access to emergency medical services (EMS) in Germany: a comparative economic study. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-043791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nenni M.E., Di Pasquale V., Miranda S., Riemma S. Development of a drone-supported emergency medical service. Int J Technol. 2020;11:656–666. doi: 10.14716/ijtech.v11i4.3951. [DOI] [Google Scholar]
- 40.Bogle B.M., Rosamond W.D., Snyder K.T., Zègre-Hemsey J.K. Predicted outcomes and cost-effectiveness of optimally designed drone-delivered AED networks in North Carolina: Predicted outcomes and cost-effectiveness. J Electrocardiol. 2019;57:S119–S120. doi: 10.1016/j.jelectrocard.2019.11.023. [DOI] [Google Scholar]
- 41.Lancaster G., Herrmann J.W. Computer simulation of the effectiveness of novel cardiac arrest response systems. Resusc Plus. 2021;7 doi: 10.1016/j.resplu.2021.100153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Starks M.A., Sperling J., Cardenas A., et al. Barriers and opportunities for a drone-delivered AED network in Durham, North Carolina. Circulation. 2020;142 doi: 10.1161/circ.142.suppl_4.151. [DOI] [Google Scholar]
- 43.Claesson A., Bäckman A., Ringh M., et al. Time to delivery of an automated external defibrillator using a drone for simulated out-of-hospital cardiac arrests vs emergency medical services. J Am Med Assoc. 2017;317:2332–2334. doi: 10.1001/jama.2017.3957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Drennan I., Cheskes S., Snobelen P., et al. AED on the fly: A drone delivery feasibility study for rural and remote out-of-hospital cardiac arrest. Can J Emerg Med. 2020;22:S13–S14. doi: 10.1017/cem.2020.75. [DOI] [Google Scholar]
- 45.Cheskes S., McLeod S.L., Nolan M., et al. Improving access to automated external defibrillators in rural and remote settings: A drone delivery feasibility study. J Am Heart Assoc. 2020;9 doi: 10.1161/JAHA.120.016687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schierbeck S., Hollenberg J., Nord A., et al. Automated external defibrillators delivered by drones to patients with suspected out-of-hospital cardiac arrest. Eur Heart J. 2021 doi: 10.1093/eurheartj/ehab498. [DOI] [PubMed] [Google Scholar]
- 47.Rosamond W.D., Johnson A., Bogle B., et al. Aerial drone versus ground search for delivery of an automated external defibrillator (AED) for out-of-hospital cardiac arrest: A comparison of elapsed time and bystander experience in a community setting. Circulation. 2020;141 doi: 10.1161/circ.141.suppl-1.53. [DOI] [Google Scholar]
- 48.Zègre-Hemsey J.K., Grewe M.E., Johnson A.M., et al. Delivery of automated external defibrillators via drones in simulated cardiac arrest: Users’ experiences and the human-drone interaction. Resuscitation. 2020;157:83–88. doi: 10.1016/j.resuscitation.2020.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Starks M.A., Blewer A.L., Sharpe E., et al. Bystander performance during simulated drone delivery of an AED for mock out-of-hospital cardiac arrest. J Am Coll Cardiol. 2020;75 doi: 10.1016/S0735-1097(20)30930-X. [DOI] [Google Scholar]
- 50.Sanfridsson J., Sparrevik J., Hollenberg J., et al. Drone delivery of an automated external defibrillator – a mixed method simulation study of bystander experience. Scand J Trauma Resusc Emerg Med. 2019;27:40. doi: 10.1186/s13049-019-0622-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schierbeck S., Svensson L., Claesson A. Use of a drone-delivered automated external defibrillator in an out-of-hospital cardiac arrest. N Engl J Med. 2022;386:1953–1954. doi: 10.1056/NEJMc2200833. [DOI] [PubMed] [Google Scholar]
- 52.Federal Aviation Administration Unmanned Aircraft System Integration Pilot Program Final Report. US Department of Transportation. Integration Pilot Program – FAA Unmanned Aircraft Systems Accessed 7/16/23.
- 53.Federal Aviation Administration BEYOND Program. US Department of Transportation BEYOND | Federal Aviation Administration (faa.gov) Accessed 7/16/23.
- 54.Bardy G.H., Lee K.L., Mark D.B., et al. Home use of automated external defibrillators for sudden cardiac arrest. NEJM. 2008;24 doi: 10.1056/NEJMoa0801651. [DOI] [PubMed] [Google Scholar]
- 55.Dainty H., Colquitt B., Bhanji F., et al. Understanding the importance of the lay responder experience in out-of-hospital cardiac arrest: A scientific statement from the American Heart Association. Circulation. 2022;145:e852–e867. doi: 10.1161/CIR.0000000000001054. [DOI] [PubMed] [Google Scholar]
- 56.Krammel M., Lobmeyr E., Sulzgruber P., et al. The impact of a high-quality basic life support police-based first responder system on outcome after out-of-hospital cardiac arrest. PLoS One. 2020;15 doi: 10.1371/journal.pone.0233966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Affatato R., Li Y., Ristagno G. See through ECG technology during cardiopulmonary resuscitation to analyze rhythm and predict defibrillation outcome. Curr Opin Crit Care. 2016;22:199–205. doi: 10.1097/MCC.0000000000000297. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.