Abstract
Introduction
A pseudoaneurysm arising from the superior thyroid artery is extremely rare. To the best of our knowledge, STA Pseudoaneurysm after thyroidectomy has not been reported.
Case presentation
A 21-year-old female presented with anterior neck swelling of two years duration. Physical exam revealed a thyroid mass that measures 10 cm ∗ 8 cm. Neck US showed MNG (TIRADS 3) and FNAC suggested colloid goiter. Near Total Thyroidectomy was performed.
On the 10th postoperative day, she noticed a painless, progressive left-sided neck swelling which is increasing in size with no active bleeding and no compressive symptoms. There is a 6x4cm tense pulsatile left-sided neck swelling adjacent to the thyroid cartilage and anterior to sternocleidomastoid muscle with a healed neck collar incision. CBC and coagulation profile were normal. Head and Neck CTA show aneurysmal dilatation of STA 3.8 cm × 3.2 cm with thrombosis of the posterior part of the lesion.
Clinical discussion
STA Pseudoaneurysms are quite rare events but could lead to catastrophic complications. Clinical manifestations can include pulsating painful mass in the neck, dysphagia, dyspnea, bleeding from the oral cavity, and cerebrovascular symptoms. It should be investigated with Color Doppler ultrasound, MRI and CTA.
Conclusion
In our case, the pseudoaneurysm occurred after thyroidectomy which has not been reported previously. The diagnosis was made by a computed tomography scan and the patient was treated by open STA ligation as endovascular service isn't available in our setup. Clinicians should therefore include pseudoaneurysm of STA or adjacent arteries in their differential diagnosis and intervene early to avoid devastating complications.
Keywords: Pseudoaneurysm, Superior thyroid artery, Thyroidectomy
Highlights
-
•
Iatrogenic Pseudoaneurysm of the Superior Thyroid Artery after Thyroidectomy
-
•
This article teaches all the possible ways of preventing such iatrogenic injury.
-
•
Following critical steps of the procedure has paramount importance.
1. Introduction
A pseudoaneurysm is a pulsating hematoma that results from a tangential injury to an arterial wall that represents a complication after trauma. Though head and neck region pseudoaneurysm are rare they could have catastrophic consequences. Therefore, it must be recognized early to prevent events such as hemorrhage or acute occlusion of the airway.
A pseudoaneurysm arising from the superior thyroid artery (STA) has been reported only in four cases in literature. Two cases of STA pseudoaneurysms have been reported after ultrasound-guided chemical parathyroidectomy and after radiotherapy for hypopharyngeal cancer [1,2]. The other two cases of STA pseudoaneurysm occurred during fine-needle aspiration biopsy of thyroid nodule and after transesophageal echocardiography-guided cardioversion [3,4]. This case is reported in accordance with SCARE criteria [5].
Here we report a case of STA pseudoaneurysm after Thyroidectomy.
2. Presentation of case
A 21 year old female presented to the surgical referral clinic of a comprehensive specialized hospital with a progressively enlarging anterior neck swelling of two years duration. Physical exam revealed a thyroid mass that measures 10 cm ∗ 8 cm. Other physical exams and laboratory evaluations were unremarkable. Neck ultrasound showed MultiNodular Goiter with cystic degeneration (TRIADS 3) and Fine Needle Aspiration Cytology suggested colloid goiter. The patient was admitted and Near Total Thyroidectomy was performed and discharged on her second postoperative day after a smooth postoperative course.
On the 10th postoperative day, she noticed a painless, progressive left-sided neck swelling which is increasing in size with no active bleeding and no compressive symptoms.
Physical examination revealed a 6 cm by 4 cm tense pulsatile left-sided neck swelling adjacent to the thyroid cartilage and anterior to sternocleidomastoid muscle with a healed neck collar incision. She was investigated with CBC and coagulation profiles which were normal. Neck Ultrasound showed a pseudoaneurysm, the origin of which was not clearly visualized and suggested CT angiography.
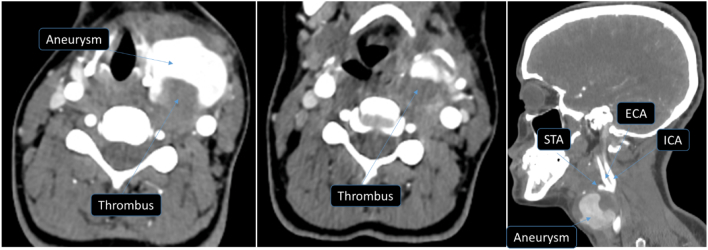
Head and Neck CT angiography revealed an intensely enhancing aneurysmal dilatation in the fossa of the left thyroid lobe measuring 3.8 cm × 3.2 cm with thrombosis of the posterior part of the lesion; the ipsilateral superior thyroid artery is hypertrophied and joins the mass lesion suggestive of partially thrombosed pseudoaneurysm of the superior thyroid artery (Fig. 1).
Fig. 1.

CT-Angiography of the neck illustrating the pseudoaneurysm with peripheral thrombus. The left superior thyroid artery was also hypertrophied.
The Vascular team took over and the patient was operated under General anesthesia and endotracheal intubation (Fig. 2). A longitudinal incision on the anterior border of the left sternocleidomastoid muscle was made to expose and control the common carotid artery and then the superior thyroid artery at its origin (Fig. 3).
Fig. 2.
3D reconstructed image showing the tortuous and hypertrophied left superior thyroid artery and the aneurysm.
Fig. 3.
Left superior thyroid artery (STA) was controlled at its origin and the second revealing the hole in the artery.
There was a 4 cm × 5 cm pulsatile mass arising from the superior thyroid artery just distal to its origin. The STA was also found to be dilated. After control of the STA close to its origin using a vascular clamp, the pseudoaneurysm sac was opened and the hematoma was evacuated. The STA had a hole that seemed to be due to a needle injury.
The superior thyroid artery was ligated at its origin. The distal end of the artery had already been securely ligated. After checking for hemostasis, the wound was closed in layers. The patient was extubated smoothly and had a smooth postoperative course. She was then discharged home on the 2nd postoperative day. Subsequent postoperative follow-up was smooth.
3. Discussion
Pseudoaneurysm, also known as “false aneurysm”, is a hematoma contained by adventitia or perivascular tissue of an artery that results from a tangential injury to the vessel [5]. Most often it is secondary to penetrating trauma [[6], [7], [8]] or surgery. It is also a well-known iatrogenic complication of vascular catheterizations [3,9] and percutaneous procedures like biopsy of solid organs [10].
Pseudoaneurysms of the head and neck region are quite rare events but can lead to catastrophic complications. Clinical manifestations can include pulsating painful mass in the neck, dysphagia, dyspnea, bleeding from the oral cavity, and cerebrovascular symptoms. The differential diagnosis of an expansile cervical mass includes a branchial cleft cyst, neck abscess, and cervical adenitis. Other cervical masses such as tumors, lymphadenopathy, or neurinomas can be excluded by the timing of growth of the mass.
Many imaging techniques are available to differentiate the diagnosis. Color Doppler ultrasound is an excellent technique to detect the presence of an aneurysmal sac and the presence of active bleeding. MRI and CT scans of the neck give information on the involvement of neck anatomical structures. Angiography is the best technique to investigate the morphology of the vessel involved and the source of the aneurysmal sac [4].
Management options for pseudoaneurysm include conservative measures with or without sonographically guided compression therapy [10,11], surgical repair [2], transarterial coil embolization [12], and percutaneous thrombin or alcohol injection [1]. There is no standard treatment protocol because of the rarity of STA pseudoaneurysm. Adequate treatment should be determined on a case-by-case basis.
A fast development of an expanding mass under the angle of the mandible or in the lateral pharyngeal wall following a surgical procedure of the neck, percutaneous biopsy, and neck trauma should always raise a suspicion of an extracranial arterial pseudoaneurysm to prevent complications.
In our case, the pseudoaneurysm occurred after an open thyroidectomy which has not been reported previously. The diagnosis was made by a computed tomography scan and the patient was treated by open STA ligation as endovascular service is not available in our setup. Clinicians should therefore include pseudoaneurysm of STA or adjacent arteries in their differential diagnosis and intervene early to avoid devastating complications.
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
Ethical Approval was provided by the author's institution.
Funding
N/A.
Author contribution
Zekaryas Belete (MD)is the author.
Henok Teklesilassie (MD, Msc) is the author and the leading consultant vascular surgeon who did the procedure.
Abebe Addisie (MD) is assistant surgeon.
Dagim Leykun (MD) is assistant surgeon and editor of the manuscript.
Tesfaye Kebede (MD, SCR, SSBI) has edited the CT scan image.
Guarantor
The author, Zekaryas Belete, is the guarantor.
Research registration number
N/A.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Conflict of interest statement
The authors declare no conflicts of interest.
References
- 1.Perona F., Barile A., Oliveri M., Quadri P., Ferro C. Superior thyroid artery lesion after US-guided chemical parathyroidectomy: angiographic diagnosis and treatment by embolization. Cardiovasc. Intervent. Radiol. 1999;22:249–250. doi: 10.1007/s002709900376. [DOI] [PubMed] [Google Scholar]
- 2.Ernemann U., Herrmann C., Plontke S., Schafer J., Plasswilm L., Skalej M. Pseudoaneurysm of the superior thyroid artery following radiotherapy for hypopharyngeal cancer. Ann. Otol. Rhinol. Laryngol. 2003;112:188–190. doi: 10.1177/000348940311200215. [DOI] [PubMed] [Google Scholar]
- 3.Celik H., Yucel C., Oktar S., et al. Iatrogenic pseudoaneurysm of the superior thyroid artery: color Doppler ultrasonographic diagnosis and treatment approach. J. Ultrasound Med. 2004;23(12):1675–1678. doi: 10.7863/jum.2004.23.12.1675. [DOI] [PubMed] [Google Scholar]
- 4.Canevari F.R., Galla S., Aina E., et al. Superior thyroid artery pseudoaneurysm as a complication of transesophageal echocardiography. J. Otolaryngol. ENT Res. 2015;2(2) (59?61) [Google Scholar]
- 5.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus surgical case report (SCARE) guidelines. Int. J. Surg. 2020;(84):226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 6.Krempl G.A., Noorily A.D. Pseudoaneurysm of the descending palatine artery presenting as epistaxis. Otoloaryngol. Head Neck Surg. 1996;114(3):453–456. doi: 10.1016/S0194-59989670217-6. [DOI] [PubMed] [Google Scholar]
- 7.Han M.H., Sung M.W., Chang K.H., et al. Traumatic pseudoaneurysm of the intracavernous ICA presenting with massive epistaxis: imaging, diagnosis and endovascular treatment. Laryngoscope. 1994;104(3Pt1):370–377. doi: 10.1288/00005537-199403000-00021. [DOI] [PubMed] [Google Scholar]
- 8.Smelt J.L., Alhamarneh O., Dyer J.D., et al. Endovascular coiling of mycotic external carotid artery pseudoaneurysm following pharyngolaryngectomy with a free jejunal graft. J. Laryngol. Otol. 2012;126(2):214–216. doi: 10.1017/S0022215111002866. [DOI] [PubMed] [Google Scholar]
- 9.Parry W., Dhillon R., Salahudeen A. Carotid pseudoaneurysm from inadvertent carotid artery catheterization for haemodialysis. Nephrol. Dial. Transplant. 1996;11(9):1853–1855. [PubMed] [Google Scholar]
- 10.Schaub F., Theiss W., Heinz M., et al. New aspect in ultrasound-guided compression repair of postcatheterization femoral artery injuries. Circulation. 1994;90(4):1861–1865. doi: 10.1161/01.cir.90.4.1861. [DOI] [PubMed] [Google Scholar]
- 11.Walker A.T., Chaloupka J.C., Putman C.M., et al. Sentinal transoral hemorrhage from a pseudoaneyrism of internal maxillary artery: a complication of Ct-giuded biopsy of the masticator space. AJNR Am. J. Neuroradiol. 1996;17(2):377–381. [PMC free article] [PubMed] [Google Scholar]
- 12.Mann G.S., Heran M.K. Percutaneous thrombin injection of a superficial temporal artery pseudoaneurysm. Pediatr. Radiol. 2007;37(6):578–580. doi: 10.1007/s00247-007-0447-8. [DOI] [PubMed] [Google Scholar]