Abstract
Background
Cytokines play a potential role in atherosclerosis pathogenesis and progression. We investigated the association of interleukin-6 (IL-6) with the angiographic severity of coronary artery disease (CAD).
Methods
Three hundred ten angiografically diagnosed CAD patients and 210 controls were enrolled in this study. CAD patients were stratified according to IL-6 cut-off value into high levels IL-6 group (≥ 9.5 pg/mL) and low levels IL-6 group (< 9.5 pg/mL). The severity of CAD was assessed according to Gensini score (GS), artery stenosis degree and the number of vessels involved. The mean age was 60.3 ± 11.0 years.
Results
The level of IL-6 in patients was increased compared to controls and ranged from 1.5 to 3640.0 pg/mL. High levels of IL-6 were significantly associated with high levels of GS (> 40) but not with stenosis degree and vessel score. GS levels were significantly more elevated in patients with high levels of IL-6 group than in low IL6 levels patients (60.6 ± 39.5 vs 46.7 ± 37.2; p = 0.027). The analysis of the ROC curve performed in myocardial infarction patients showed that IL-6 (AUC: 0.941 (CI 95% 0.886, 0.997; p < 0.001) could be a powerful predictor marker in evaluating the infarct size after myocardial infarction when compared to myonecrosis biomarkers.
Conclusions
IL-6 levels were associated with the severity of CAD assessed by the GS. Based on the highest levels of IL-6 measured in patients with STEMI, our study strongly suggests that IL-6 could be a powerful marker in evaluating the myocardial necrosis.
Trial registration
ClinicalTrials.gov Number: NCT03075566 (09/03/2017).
Keywords: IL-6, Coronary artery disease, STEMI, Severity, Gensini score
Introduction
Atherosclerosis, an inflammatory process, is characterized by the involvement of multiple risk factors and the complexity of its pathophysiology [1]. The pathogenesis of the disease involves several stages: once stimulated, the damaged vascular endothelial cells secrete various pro-inflammatory molecules that mediate recruitment, migration, cell proliferation and regulation of protein and lipid synthesis. Macrophages internalize oxidized LDL and subsequently differentiate into foam cells [2]. Activation of macrophages causes acute inflammation and secretion of growth factors. Cytokines secreted by activated pro-inflammatory cells induce thickening or rupture of atherosclerotic plaques and arterial thrombosis [3]. The process of atherosclerosis follows well-defined steps and can affect all sites of coronary artery [4]. This pathophysiological mechanism induces the formation of an important lipid necrosis, a cascade of inflammatory reactions [5], alteration of the cascade of coagulation and fibrinolysis [6]. This mechanism causes the release of various cytokines, which are involved in the destruction of the fibrous cap and plaque instability leading to SCA [7]. IL-6, a pleiotropic cytokine intervenes in the acute phase of chronic inflammation response. IL-6, a member of the IL family, plays a proinflammatory role inducing the adhesion and aggregation of inflammatory cells throughout the organism which explains its involvement in the development of atherosclerosis and thrombosis [8]. Blood IL-6 levels are associated with CVD as including endothelial dysfunction, arterial stiffness and atherosclerosis [9]. With regards to CAD risk prediction, we conducted this prospective study to evaluate the association between serum IL-6 levels with the severity of CAD in patients with acute coronary syndrome, as confirmed by elective coronary angiography and Gensini score.
Materials and methods
Methods
Patients
We enrolled 207 blood donors subjects in the blood bank department in the Tahar Sfar University Hospital of Mahdia as controls in this study. Consecutive patients complaining of chest pain who underwent invasive coronary angiography for the diagnosis of CAD. A total of 310 CAD patients recruited from the Department of Cardiology, University Hospital (Monastir, Tunisia) showed by angiography at least one coronary stenosis of more than 50% of the luminal diameter that were included in the study. We followed the methods of Bouzidi N et al. 2020 [10].
The diagnosis of ACS was based on the guidelines of the European Society of Cardiology (ESC) [11]. NSTEMI-Acute coronary syndrome (ACS) included NSTEMI and UA. NSTEMI was defined as elevated cardiac troponin I (cTnI) values without new ST elevation on electrocardiogram with ischemic symptoms. UA was defined as having newly developed and accelerated chest symptoms on exertion or rest angina without the detection of signifcant cTnI increase. STEMI was defined as a persistant electrocardiographic ST-segment elevation associated to high levels of cTnI after chest pain symptoms (> 20 min).
Chronic lung disease, liver disease, kidney disease, concomitant inflammatory diseases such as infections and autoimmune disorders, or malignancy were excluded. The study protocol complied with the Declaration of Helsinki, and this study protocol was reviewed and approved by the National Committee for Medical and Research Ethics of Farhat Hached University Hospital (Sousse, Tunisia). Written informed consent was obtained from each subject.
Angiographic severity
Coronary angiographic data were collected from patient catheterization laboratory records and reviewed independently by interventional cardiologists. The severity of CAD was ascertained by the degree of epicardial coronary artery stenosis and was classified as previously published guidelines, as moderate (50–70% stenosis), and severe (> 70% stenosis) and multivessel disease extent [1, 2 or 3-vessel disease stenosis (> 50%)]. Accordingly, patients were categorized as having one or multi-vessel disease. Multi-vessel CAD was confirmed when at least two of the major coronary arteries had significant atherosclerosis [1].
Coronary lesion severity was assessed in each patient by the Gensini Score (GS) [12], which was calculated by scoring each atherosclerotic lesion according to the degree of coronary artery luminal narrowing and the location of the lesion. The total score was calculated as a sum of the product of the stenosis and location score of each affected lesion.
In this scoring system, 0 indicates no abnormality, 1 represents stenosis of ≤ 25%, 2 represents stenosis of 26–50%, 4 represents stenosis of 51–75%, 16 represents stenosis of 76%–99%, and 32 represents complete occlusion. The score is then multiplied by different factors according to the functional significance of the coronary artery. The evaluation of each segment was performed by multiplying the scores by 5 for the left main trunk, by 2.5 for the proximal left anterior descending (LAD) branch, by 1.5 for the middle LAD, by 1 for the distal LAD, by 1 for the first diagonal branch, by 0.5 for the second diagonal branch, by 2.5 for the proximal LCx, by 1 for the distal LCx and posterior descending branch, and by 0.5 for the posterior branch, while the RCA was performed by multiplying the scores by 1 for the proximal, middle and distal RCA and the posterior descending branch, and by 0.5 for the posterior branch. The final score was calculated by adding the scores of each segment. The patients were then divided according to the median of the total score (GS = 40) [12].
Serum interleukin-6 measurement
Serum interleukin-6 (IL-6) levels were measured by electrochemiluminescence immunoassay (ECLIA) using a Cobas E601 analyzer (Roche Diagnostics, Germany).
Laboratory evaluation
Serum samples were collected from study participants immediately upon admission, and stored in aliquots at -80 °C until use. Triglycerides (TG), total cholesterol (TC), high density lipoprotein-cholesterol (HDL-C), hsCRP, glucose, urae, creatinine, creatine phosphokinase (CPK) and creatine kinase (CK)-MB isoforms were measured using an analyser (Cobas Integra 600, Roche Diagnostic, Germany) for patients upon admission. Low density lipoprotein-cholesterol (LDL-C) was estimated by the Friedewald equation) [10].
Statistical analysis
Data were analyzed using Statistical Package for the Social Sciences (SPSS, version 23.0). Continuous variables were described as mean ± standard deviation (SD) for normally distributed data or medians (minimum—maximum) for non-normally distributed data, as appropriate. Categorical data were summarized as frequencies or percentages. IL-6 was log transformed before analyses because its non-normally distribution. Differences in quantitative parameters between groups were performed using independent-samples T test or Mann–Whitney U test, as appropriate. The predictive values of different biomarkers for the presence of CAD and evaluating infarct size were determined by constructing receiver operating characteristic (ROC) curves and the area under the curve (AUC) was calculated. p value < 0.05 were considered as significant. The cut-off value was determined using the Youden index = maximum (sensitivity + specificity – 1) [12].
Results
Baseline clinical and laboratory characteristics
The baseline clinical and laboratory characteristics of the subjects were shown in Table 1. Patients had 60.3 ± 11.0 years as mean age and were mostly males. As prevalences were high, many risk factors contributed to CAD outcomes development.
Table 1.
Baseline characteristics of the study population
| Characteristics | Controls N = 207 | Patients N = 310 | p |
|---|---|---|---|
| Age, years | 33.2 ± 12.2 | 60.3 ± 11.0 | < 0.001 |
| Male, n (%) | 61(29.5) | 232(74.8) | < 0.001 |
| BMI, Kg/m2 | 25.1 ± 3.6 | 27.5 ± 4.3 | < 0.001 |
| Smoker, % | 8.2 | 41.0 | < 0.001 |
| Menopause, % | 0 | 90.8 | < 0.001 |
| Obesity, % | 0 | 22.6 | < 0.001 |
| Hypertension, % | 0 | 47.1 | < 0.001 |
| Diabetes, % | 0 | 48.4 | < 0.001 |
| Dyslipidemia, % | 0 | 23.5 | < 0.001 |
| Personal history of CAD, % | 0 | 33.2 | < 0.001 |
| Personal history of ACS, % | 0 | 27.4 | < 0.001 |
| Peripheral artery Diseases, % | 0 | 1.6 | < 0.001 |
| History of bypass surgery, % | 0 | 3.2 | < 0.001 |
Data are expressed as mean ± SD or n (%)
ACS Acute coronary syndrome, BMI Body mass index, CAD Coronary artery diseases
Statistical differences between biochemical markers and IL-6 levels
The cutoff value of IL-6 was determined using ROC curve analysis between all patients and controls. Based on IL-6 cutoff value, patients were separately divided into two groups, low- and high IL-6 levels. The biochemical analyses of taken blood samples were compared between both group low- and high IL-6 serum levels. Lipid profile parameters and atherogenic index levels were more elevated in patients with high levels of IL-6. Differences were not statistically significant (Table 2).
Table 2.
Clinical, angiographic and biochemical characteristics of patients
| Characteristics | All N = 310 |
Patients | p | |
|---|---|---|---|---|
| Low < 9.5 pg/mL N = 164 |
High ≥ 9.5 pg/mL N = 146 |
|||
| SBP, cmHg | 13.0 ± 2.2 | 12.8 ± 1.9 | 12.7 ± 2.3 | 0.818 |
| DBP, cmHg | 7.4 ± 1.3 | 7.4 ± 1.1 | 7.4 ± 1.5 | 0.750 |
| Heart rate, b/min | 75.5 ± 15.7 | 73.9 ± 14.4 | 77.1 ± 17.7 | 0.208 |
| Ejection Fraction, % | 49.3 ± 13.7 | 52.9 ± 13.0 | 45.8 ± 13.8 | 0.077 |
| Vessel involved, % | ||||
| LMCA | 6.9 | 45.5 | 54.5 | 0.581 |
| LCx | 48.4 | 53.2 | 46.8 | 0.959 |
| IVA | 73.0 | 53.4 | 46.6 | 0.996 |
| RCA | 47.2 | 56.0 | 44.0 | 0.544 |
| Stenosis, % | 0.723 | |||
| [50–70] | 26.9 | 57.1 | 42.9 | |
| > 70 | 73.1 | 52.6 | 47.4 | |
| Gensini Score categories | 0.022 | |||
| Low (GS < 40) | 42.9 | 50.0 | 50.0 | |
| High (GS > 40) | 57.1 | 34.3 | 65.7 | |
| Vessel Disease, % | 0.344 | |||
| One Vessel | 44.7 | 49.3 | 56.8 | |
| Multi Vessel | 55.3 | 50.7 | 43.2 | |
| Glucose, mmol/L | 7.9 (3.1–42.3) | 8.09 (3.8–21.23) | 7.6 (3.1–41.6) | 0.680 |
| HbA1c, % | 7.9 ± 2.4 | 7.9 ± 2.3 | 7.2(5.3–12.7) | 0.630 |
| Urae, mmol/L | 5.7 (2.5–30.5) | 5.2 (2.5–12.6) | 5.6 (2.3–30.5) | 0.003 |
| Creatinin, µmol/L | 88.0(5–164) | 85(5–148) | 89.5(40–164) | 0.153 |
| Uric Acid, µmol/L | 309.0 (82.0–817.0) | 312.0 (217.0–633.0) | 316.0 (126.0–591.0) | 0.051 |
| TC, mmol/L | 4.4 ± 1.4 | 4.4 ± 1.4 | 4.3 ± 1.4 | 0.542 |
| TG, mmol/L | 1.4 (0.3–12.1) | 1.4 (0.3–12.1) | 1.4 (0.5–4.8) | 0.389 |
| HDL-C, mmol/L | 0.9 (0.23–1.9) | 0.9 (0.23–1.83) | 0.8 (0.33–1.9) | 0.802 |
| LDL-C, mmol/L | 2.7 (0.4–6.0) | 2.4 (0.4–5.0) | 3.0 (0.6–5.0) | 0.056 |
| Lp(a), mg/dL | 11.0 (1.5–123.0) | 10.7 (2.3–123.0) | 10.7 (1.5–110.7) | 0.925 |
| ApoA1, mg/dL | 95.9 (0.0–145.0) | 94.05 (0.0–145.0) | 94.05 (20.1–147.0) | 0.466 |
| ApoB, mg/dL | 72.2(7.2–152.0) | 70.5(22.0–133.0) | 74.5(7.2–152.0) | 0.120 |
| AIP | 0.18(0.58–1.41) | 0.15(0.35–1.41) | 0.19(0.58–0.66) | 0.545 |
| ApoB/ApoA1 | 0.8(0.1–5.1) | 0.7(0.2–3.1) | 0.8(0.1–5.1) | 0.075 |
| HDLc/ApoA1 | 0.9(0.3–2.4) | 1.0(0.3–2.4) | 0.9(0.5–1.8) | 0.378 |
| HDLc/Lp(a) | 7.2(0.7–58.8) | 7.4(0.7–0.9) | 6.5(0.9–41.7) | 0.232 |
| Hcy, µmol/L | 18.9(3.7–50.0) | 15.4(7.7–50.0) | 23.5(3.7–50.0) | 0.125 |
| HGB, g/dL | 13.2(8.1–17.4) | 13.8(8.8–17.3) | 13.0(8.1–17.4) | 0.019 |
| IL-6, pg/mL | 9.0(1.5–3640.0) | 4.6(1.5–9.4) | 24.8(9.6–3640.0) | 0.001 |
| hsCRP, mg/L | 4.9(0.2–1020.0) | 3.2(0.2–100.0) | 14.3(0.3–1020.0) | 0.002 |
| GS | 53.0 ± 38.7 | 46.7 ± 37.2 | 60.6 ± 39.5 | 0.027 |
AIP Atherogenic index of plasma (TG/HDLc), ApoA-1 Apolipoprotein A-1, ApoB Apolipoprotein B, GS Gensini score, HbA1c Gyrated hemoglobin, Hcy Homocysteine, HDL-c High density lipoprotein cholesterol, HGB Hemoglobin, Hs-CRP High sensitivity C-reactive protein, IL-6 Interleukin 6, LDL-c Low density lipoprotein cholesterol, Lp(a) Lipoprotein(a), TC Total cholesterol, TG Triglycerides. Values are expressed as the mean ± SD. ACE Angiotensin converting enzyme inhibitor, DBP Diastolic blood pressure, LAD Left anterior descending, LCx Left circumflex, LDL-c Low density lipoprotein cholesterol, LMCA Left main coronary artery, LVEF Left ventricular ejection fraction, RCA Right coronary artery, SBP Systolic blood pressure. Values are expressed as the mean ± SD or n (%). p < 0.05. p < 0.05
Severity of coronary artery disease
GS levels were significantly more elevated in patients with high levels of IL-6 than in patients with low levels of IL-6 (60.6 ± 39.5 vs. 46.7 ± 37.2; p = 0.027) (Table 2). 64.9% of patients using statins, had IL-6 levels < 9.5 pg/mL. In high levels of IL-6 (≥ 9.5 pg/mL) patient group, 65.7% of patients had GS value > 40 (p = 0.022) (Table 2). High levels of IL-6 were significantly associated with high levels of GS (> 40) (p = 0.027) and not with stenosis degree or vessel score (Table 3).
Table 3.
IL-6 levels distribution according to angiographic profile
| Characteristics | IL-6, pg/mL | p | |
|---|---|---|---|
| Median | Min—Max | ||
| Stenosis | |||
| [50–70] % | 9.1 | 1.8–203.3 | 0.783 |
| > 70% | 7.7 | 1.5–3640.0 | |
| Number of stenotic coronary arteries | |||
| Single vessel diseased | 9.6 | 1.8–1957.0 | 0.274 |
| Multi-vessel diseased | 8.1 | 1.5–3640.0 | |
| Gensini Score categories | |||
| Low (GS < 40) | 7.1 | 2.1–1957.0 | 0.027 |
| High (GS > 40) | 10.9 | 2.2–3640.0 | |
Values are expressed as the mean ± SD. p < 0.05
Abbreviations: GS Gensini score, IL-6 Interleukin 6, Max Maximum value, Min Minimum value
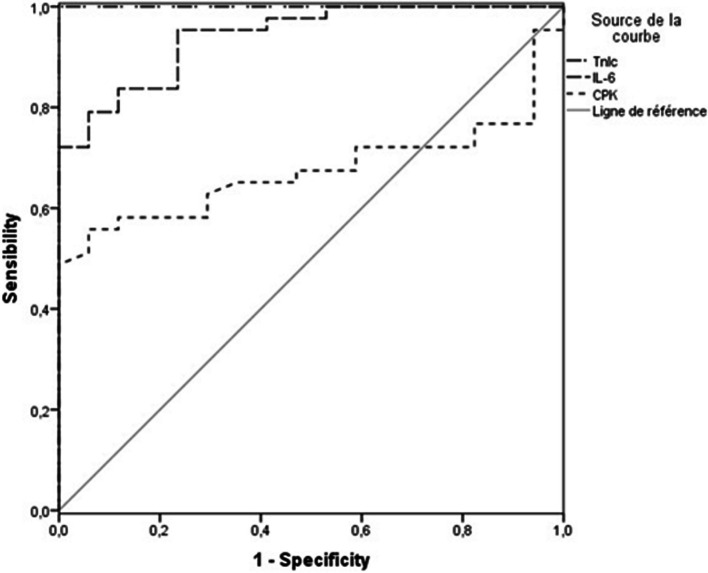
IL-6 was a predictor of CAD severity according to the ROC Analysis performed in patients with GS > 40 [area under the curve (AUC) 0.606; CI: 0.513 – 0.698, p = 0.027] (Fig. 1).
Fig. 1.
ROC analysis for IL-6 levels in predicting CAD severity performed in patients with GS > 40. Area under the ROC curve for IL-6 levels was 0.606; CI: 0.513 – 0.698, p = 0.027
IL-6 levels in different ACS patients subgroups
The subgroup analysis of all patients divided into the NSTE-ACS group, STEMI group and UA showed that serum IL-6 levels in STEMI patients were significantly higher than levels in other patients (19.1 pg/mL vs. 7.5 pg/mL (NSTEMI) and 5.6 pg/mL (UA) (Table 4).
Table 4.
Levels of IL-6 in different clinical groups
| IL-6, pg/mL | Controls N = 207 |
All patients N = 310 |
p | UA N = 107 |
NSTEMI N = 111 |
STEMI N = 92 |
|---|---|---|---|---|---|---|
|
Median V Min; V Max |
3.1 1.1–8.7 |
8.9 1.5–3640.0 |
< 0.001 |
5.6 1.7–855.4 |
7.5 1.5–220.0 |
19.1 2.4–3640.0 |
Abbreviations: IL-6 Interleukin 6, NSTEMI Non ST elevation myocardial infarction, STEMI ST elevation myocardial infarction, UA Unstable Angina, V max Maximum value, V min Minimum value, p (NSTEMI vs UA) = 0.108; p (STEMI vs UA) < 0.001; p (NSTEMI vs STEMI) < 0.001. p values < 0.05 statistical signifiance
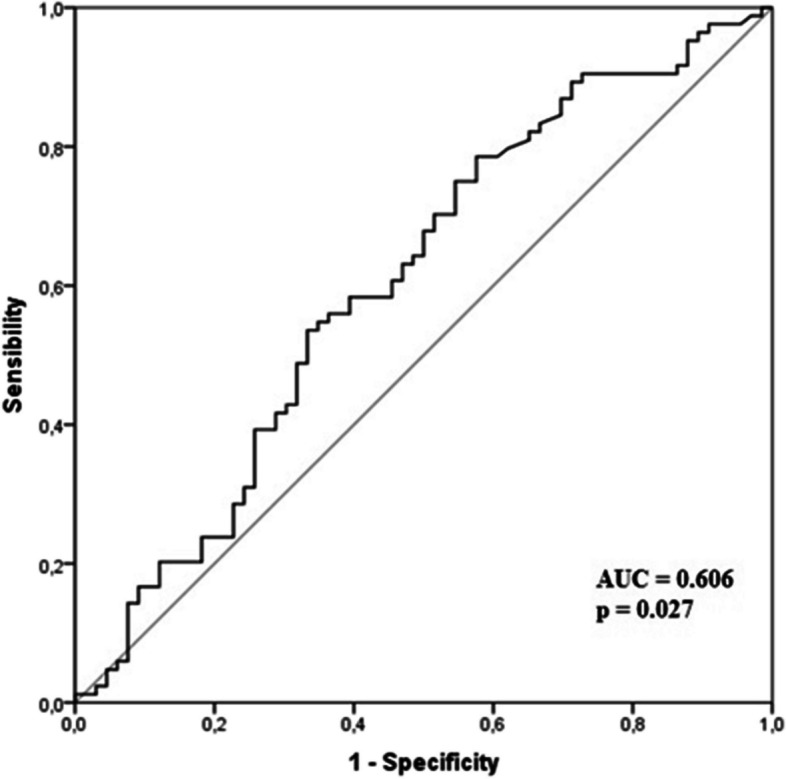
Prediction of infarct size in patients with MI by ROC curve analysis
The analysis by ROC curve for IL-6, TnIc and CPK showed an AUC for IL-6 = 0.941 (CI 95% 0.886, 0.997; p < 0.001); CPK: 0.674 (CI 95% 0.543—0.806; p = 0.036); cTnI 1.00 (CI 95% 1.000, 1.000; p < 0.001) (Fig. 2). These results suggest that IL-6 could be a powerful marker in predicting infarct size in STEMI patients.
Fig. 2.
The analysis by ROC curve for IL-6, TnIc and CPK. AUC for IL-6 = 0.941 (CI 95% 0.886, 0.997; p < 0.001); CPK: 0.674 (CI 95% 0.543–0.806; p = 0.036); cTnI 1.00 (CI 95% 1.000, 1.000; p < 0.001)
Discussion
In this study, we investigated the relationship between serum IL-6 levels and the severity of coronary artery disease (CAD). Our results demonstrated that IL-6 levels were associated with Gensini score in CAD patients. We found that IL-6 levels were significantly elevated in the group of patients with high GS in comparison with low GS group. IL-6 levels, as shown in ROC curve, could be a useful tool in the prediction of CAD.
Our findings were in accordance with other previous studies. In this study, the main results were the significant association between IL-6 and the severity of CAD assessed by GS. A serum IL-6 level above 9.5 pg/mL is highly predictive for severe CAD. Our findings could suggest a different treatment approach between patients on the basis of the CAD severity assessed by GS. Tanindi et al. [13] had found that IL-6 was associated with more extensive and severe CAD as represented by GS. Despite significant association between high levels of IL-6 in single- and multi vessel disease groups as compared with controls, Mokhtar ER et al. [14] findings did not show significant association between IL-6 and GS. Gotsman I et al. [15] reported that there was significant correlations between interleukin-6 with the severity of CAD assessed by the number of obstructed coronary vessels and the lesions severity. Also, Chun-lin L et al. [16] reported that IL-6 could be a useful marker in evaluating the activity of plaque and CAD degree.
Atherosclerosis depends on several well-established risk factors. Several inflammatory markers could stratify patients with high CV risk. Inflammation and the altered release of cytokines are the processes promoting the formation, development and rupture of atherosclerotic plaque which is the essential mechanism causing ACS [17]. IL6 is synthesized by several cell types such as hepatic fibroblasts, macrophages, and monocytes as well as fat cells, vasculature and myocardial cells [18]. A previous study suggests that the important secretion of IL-6 by adipose cells could explain CAD occurrence [19]. It has been shown that in large populations, IL6 compared to other inflammatory markers such as hsCRP and LpPLA2, appears to be the most predictive marker of clinical manifestations even at early stages. Karabağ Y. et al. [20] found that C-Reactive Protein/Albumin Ratio was more tightly associated with the complexity and severity of CAD than CRP and albumin alone and was found to be an independent predictor for intermediate-high Syntax Score patients. High levels of IL-6 suggest a predictor role of major cardiovascular events in CAD patients and healthy subjects [21]. IL-6 levels were associated with cardiovascular complications of MI [22], which support its role as potent activators of local inflammation [23] and could explain high levels of IL6 shown in STEMI patients.
High concentrations of IL-6 have been associated with acute ischemia and may be markers of recurrent CAD [24]. Other studies have shown that IL-6 and its different signaling pathways involve different mechanisms to contribute to the formation and destabilization of atherosclerotic plaques [25]. Once released into the blood, IL-6 molecules activate inflammatory cells, release chemokine and adhesion molecules, and triggers aggregation of these cells to form atherosclerotic plaque. The release of oxygen free radicals and the excessive expression of metalloproteinases by activated inflammatory cells lead to the instability of the atherosclerotic plaque. Secondly, the complement system could be activated also by IL-6 and affect the synthesis of endothelin-1 (ET-1) and nitric oxide altering subsequently the endothelial function. Finally, IL-6 might promote the expression of the tissue factor type I plasminogen activator inhibition factor and intensify its activities, inducing coagulation abnormalities and thrombus formation [26]. High blood levels of IL-6 may have an important role in the transformation of macrophage to foam cells in atherosclerosis in CAD patients.
In the vascular tissue, hypercholesterolemia was associated with the presence of an inflammatory reaction. Oxidized LDL, which is the inflammatory agent [27], had a chemo-attracting power on monocytes, cause their differentiation into macrophages and inhibit their migration [28]. In patients with CAD, statins have been shown to possess anti-inflammatory properties as the decrease of inflammatory cells number by inhibiting adhesion molecules and cytokines as interleukins 6 and 8 [29, 30]. These processes explain high levels of lipids and their ratios in patients with high levels of IL-6. A previous study reported that in AMI patients, IL-6 levels began to increase 14 h (mean; range 8–20 h) after the initial complaints and reached maximal levels of 28 to 250 U/ml (normal values < 10 U/ml) after 36 h (mean; range 24–52 h). This study suggest that a decrease of IL-6 levels 48 h after admission was associated with an uneventful course, and an elevation at this time point was associated with a complicated hospital course [31]. Ikonomidis et al. [32], findings suggested that therapeutic effects of aspirin and statins could explain the decrease of IL-6 level in patients with ACS. These findings could explain the large interval of IL-6 distribution in our patients.
In STEMI patients, circulating levels of IL-6 have been shown to correlate with high levels of cTnI thereafter, with myocardial necrosis size [7]. As shown in ROC curve analysis in this study, IL-6 and necrosis markers were grateful tools in predicting infarct size. Pre-inflammatory cytokines could be involved in reperfusion injury, repair, and healing processes following MI [7].
However, our study also has some limitations. First, coronary angiography detects only coronary luminal narrowing and not systemic atherosclerotic burden; the latter may affect serum levels of inflammatory markers. Second, IL-6 levels were measured in peripheral blood; this does not elucidate the site of origin of inflammatory mediators. Third, despite the common pathophysiology process, CAD outcomes differ in clinical symptoms, which distort results.
Fourth, we did not collect the time of onset of chest pain the samples for IL-6 were taken which may influence the IL-6 levels. Future studies will need to assess the importance of other parameters (i.e., genetic factors, novel risk factors) in angiographic CAD extent prediction. These results apply only to the angiographic assessment of the presence, severity, and extent of CAD; other imaging techniques such as intravascular ultrasound or optical coherence tomography may yield different results.
Conclusions
Our results suggest that IL-6 is useful to be a good biomarker reflecting the severity of CAD assessed by GS and to play a major role in the progression of atherosclerosis. Based on the highest levels of IL-6 measured in patients with STEMI, our study strongly suggests that IL-6 could be a powerful marker in evaluating the necrosis extent and high levels could be related to post MI complication.
Acknowledgements
The authors are grateful to the patients and volunteers for their collaboration, the entire team for collecting blood samples from patients (Cardiology Department, Fattouma Bourguiba University Hospital, Monastir, Tunisia); and the staff members of the Cardiothrombosis Research Laboratory (Monastir, Tunisia) for their technical support.
Abbreviations
- ACS
Acute coronary syndrome
- CAD
Coronary artery disease
- CEI
Conversion enzyme inhibitor
- CK-MB
Creatine kinase isoforms
- CPK
Creatine phosphokinase
- cTnI
Cardiac troponin I
- DBP
Diastolic blood pressure
- ECLIA
Electrochemiluminescence immunoassay
- ESC
European Society of Cardiology
- ET
Endothelin-1
- GS
Gensini score
- HDL-c
High density lipoprotein-cholesterol
- HsCRP
High sensitivity C reactive protein
- IL
Interleukin
- LAD
Left anterior descending
- LCx
Left circumflex
- LDL-c
Low density lipoprotein-cholesterol
- LMCA
Left main coronary artery
- LpPLA2
Lipoprotein-associated phospholipase
- LVEF
Left ventricular ejection fraction
- MI
Myocardial infarction
- NSTEMI
Non-elevation myocardial infarction
- RCA
Right coronary artery
- SBP
Systolic blood pressure
- STEMI
ST-segment elevation myocardial infarction
- TC
Total cholesterol
- TG
Triglycerides
- UA
Unstable angor
Authors’ contributions
All authors contributed to the conception or design and the acquisition, analysis, revising, and approval of the work.
Funding
This work was supported by the research organizations in Tunisia (Ministry of Public Health and Ministry of Higher Education and Scientific Research).
Availability of data and materials
The data used to support the findings of this study are available from the corresponding author upon request.
Declarations
Ethics approval and consent to participate
The study was approved by the local Ethics Committee and was carried out in accordance with the Declaration of Helsinki. Written informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bouzidi N, Betbout F, Maatouk F. Relationship of activin A levels with clinical presentation, extent, and severity of coronary artery disease. Anatol J Cardiol. 2017;18:402–409. doi: 10.14744/AnatolJCardiol.2017.7935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Favero G, Paganelli C, Buffoli B. Endothelium and its alterations in cardiovascular diseases: life style intervention. Biomed Res Int. 2014;2014:801896. doi: 10.1155/2014/801896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ozkaramanli Gur D, Guzel S, Akyuz A. The role of novel cytokines in inflammation: defining peripheral artery disease among patients with coronary artery disease. Vasc Med. 2018;23:428–436. doi: 10.1177/1358863X18763096. [DOI] [PubMed] [Google Scholar]
- 4.Fanola CL, Morrow DA, Cannon CP. Interleukin-6 and the risk of adverse outcomes in patients after an acute coronary syndrome: observations from the SOLID-TIMI 52 (Stabilization of Plaque Using Darapladib—Thrombolysis in Myocardial Infarction 52) trial. J Am Heart Assoc. 2017;6:e005637. doi: 10.1161/JAHA.117.005637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yanjia C, Hui H, Xiaoxiang Y. Tetranectin as a potential biomarker for stable coronary artery disease. Sci Rep. 2015;5:17632. doi: 10.1038/srep17632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vibeke NR, Ingebjørg S, Harald A. IL-6 signalling in patients with acute ST-elevation myocardial infarction. Results Immunol. 2013;14:813. doi: 10.1016/j.rinim.2013.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Simon TG, Trejo MEP, McClelland R. Circulating Interleukin-6 is a biomarker for coronary atherosclerosis in nonalcoholic fatty liver disease: results from the Multi-Ethnic Study of Atherosclerosis. Int J Cardiol. 2018;259:198–204. doi: 10.1016/j.ijcard.2018.01.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang Y, Shao T, Yao L. Effects of tirofban on stent thrombosis, Hs-CRP, IL-6 and sICAM-1 after PCI of acute myocardial infarction. Exp Ther Med. 2018;16:3383–8. doi: 10.3892/etm.2018.6589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bouzidi N, Ben Messaoud M, Maatouk F. Relationship between high sensitivity C-reactive protein and angiographic severity of coronary artery disease. J Geriatr Cardiol. 2020;17:256–263. doi: 10.11909/j.issn.1671-5411.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roffi M, Patrono C, Collet JP. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC) Eur Heart J. 2016;37:267–315. doi: 10.1093/eurheartj/ehv320. [DOI] [PubMed] [Google Scholar]
- 11.Dimitris T, Gerasimos S, Konstantinos M. Serum osteoprotegerin and osteopontin levels are associated with arterial stiffness and the presence and severity of coronary artery disease. Int J Cardiol. 2013;167(5):1924–1928. doi: 10.1016/j.ijcard.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 12.Perkins NJ, Schisterman EF. The youden index and the optimal cut-point corrected for measurement error. Biom J. 2005;47:428–441. doi: 10.1002/bimj.200410133. [DOI] [PubMed] [Google Scholar]
- 13.Tanindi A, Sahinarslan A, Elbeg S. Relation between MMP-1, MMP-9, TIMP-1, IL-6 and risk factors, clinical presentation, extent and severity of atherosclerotic coronary artery disease. Open Cardiovasc Med J. 2011;5:110–6. 10.2174/1874192401105010110. [DOI] [PMC free article] [PubMed]
- 14.Ling Y, Weng H, Tang S. The relationship between IL-6 levels and the angiographic severity of coronary artery disease following percutaneous coronary intervention in acute coronary syndrome patients. BMC Cardiovasc Disord. 2021;21:578. doi: 10.1186/s12872-021-02406-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu CL, Sben DL, Zbu K. Levels of interleukin-33 and interleukin-6 in patients with acute coronary syndrome or stable angina. Clin Invest Med J. 2013;36:E234–241. doi: 10.25011/cim.v36i4.19957. [DOI] [PubMed] [Google Scholar]
- 16.Simon TG, Trejo MEP, McClelland R. Circulating Interleukin-6 is a biomarker for coronary atherosclerosis in nonalcoholic fatty liver disease: Results from the Multi-Ethnic Study of Atherosclerosis. Int J Cardiol. 2018;259:198–204. doi: 10.1016/j.ijcard.2018.01.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shim AL, Aksyonov AA, Mitrokhin VM. Serum interleukin-6: association with circulating cytokine serum levels in patients with sinus arrhythmia and patients with coronary artery disease. Cell Immunol. 2016;310:178–183. doi: 10.1016/j.cellimm.2016.09.007. [DOI] [PubMed] [Google Scholar]
- 18.Nambi V, Hoogeveen RC, Chambless L. Lipoprotein-Associated Phospholipase A2 and High-Sensitivity C Reactive Protein Improve the Stratification of Ischemic Stroke Risk in the Atherosclerosis Risk in Communities (ARIC) Study. Stroke. 2009;40:376–381. doi: 10.1161/STROKEAHA.107.513259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bonda T, Kaminski KA, Kozuch M. Musial Circadian variations of interleukin 6 in coronary circulations of patients with myocardial infarction. Cytokine. 2010;50:204–209. doi: 10.1016/j.cyto.2010.01.007. [DOI] [PubMed] [Google Scholar]
- 20.Karabağ Y, Çağdaş M, Rencuzogullari I, et al. Relationship between C-reactive protein/albumin ratio and coronary artery disease severity in patients with stable angina pectoris. J Clin Lab Anal. 2018;32:e22457. doi: 10.1002/jcla.22457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaminski KA, Kozuch M, Bonda T. Coronary sinus concentrations of interleukin 6 and its soluble receptors are effected by reperfusion and may portend complications in patients with myocardial infarction. Atherosclerosis. 2009;206:581–587. doi: 10.1016/j.atherosclerosis.2009.03.033. [DOI] [PubMed] [Google Scholar]
- 22.Woods A, Brull DJ, Humphries SE. Genetics of inflammation and risk of coronary artery disease: the central role of interleukin-6. Eur Heart J. 2000;21:1574–1583. doi: 10.1053/euhj.1999.2207. [DOI] [PubMed] [Google Scholar]
- 23.Tang JN, Shen DL, Liu CL. Plasma levels of C1q/TNF-related protein 1 and interleukin 6 in patients with acute coronary syndrome or stable angina pectoris. Am J Med Sci. 2015;349:130–136. doi: 10.1097/MAJ.0000000000000378. [DOI] [PubMed] [Google Scholar]
- 24.Wang XH, Liu SQ, Wang YL. Correlation of serum high-sensitivity C-reactive protein and interleukin-6 in patients with acute coronary syndrome. Genet Mol Res. 2014;13:4260–4266. doi: 10.4238/2014. [DOI] [PubMed] [Google Scholar]
- 25.Zhao L, Wang X, Yang Y. Association between interleukin-6 and the risk of cardiac events measured by coronary computed tomography angiography. Int J Cardiovasc Imaging. 2017;33:1237–1244. doi: 10.1007/s10554-017-1098-y. [DOI] [PubMed] [Google Scholar]
- 26.Liao F, Andalibi A, Qiao JH. Genetic evidence for a common pathway mediating oxidative stress, inflammatory gene induction, and aortic Fatty streak formation in mice. J Clin Invest. 1994;94:877–884. doi: 10.1172/JCI117409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Frostegard J, Wu R, Giscombe R. Induction of T-cell activation by oxidized low density lipoprotein. Arterioscle Thromb. 1992;12:461–467. doi: 10.1161/01.atv.12.4.461. [DOI] [PubMed] [Google Scholar]
- 28.Diamantis E, Kyriakos G, Quiles-Sanchez LV. The anti-inflammatory effects of statins on coronary artery disease: an updated review of the literature. Curr Cardiol Rev. 2017;13:209–2016. doi: 10.2174/1573403X13666170426104611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mizuno Y, Jacob RF, Mason RP. Inflammation and the development of atherosclerosis. J Atheroscler Thromb. 2011;18(5):351–358. doi: 10.5551/jat.7591. [DOI] [PubMed] [Google Scholar]
- 30.Triyano T, Pariding J, Sukorini U. Correlation of IL-6 and monocyte count to Troponin I in acute coronary syndrome. Berkala Ilmu kedokteran. 2008;40:189–192. [Google Scholar]
- 31.Biasucci LM, Vitelli A, Liuzzo G, Altamura S, Caligiuri G, Monaco C, Rebuzzi AG, Ciliberto G, Maseri A. Elevated levels of interleukin-6 in unstable angina. Cirotlarion. 1996;94:874–877. doi: 10.1161/01.cir.94.5.874. [DOI] [PubMed] [Google Scholar]
- 32.Ikonomidis I, Andreotti F, Economou E, Stefanadis C, Toutouzas P. Nihoyannopoulos P Increased proinflammatory cytokines in patients with chronic stable angina and their reduction by aspirin. Circulation. 1999;I OO:793–798. doi: 10.1161/01.CIR.100.8.793. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.