Abstract
Background:
Recent advances have begun to identify the nonphysical factors facilitating successful return to sport (RTS) after shoulder instability surgery, yet little is currently known regarding psychological factors and RTS.
Purpose/Hypothesis:
The purposes of this study were to (1) identify psychological factors associated with RTS, (2) evaluate the prognostic utility of various psychological factors, and (3) evaluate the available metrics used to assess psychological RTS readiness. It was hypothesized that psychological factors would be identified as critical elements influencing a patient's RTS.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
Clinical studies reporting on the psychological determinants of RTS for patients who had surgery for shoulder instability between 1996 and 2022 were identified from MEDLINE, Embase, and Cochrane databases. Demographic, clinical, and psychometric properties were extracted for pooled weighted analysis.
Results:
Of the 969 studies screened, 24 (2.5%) met inclusion criteria. Overall, 2135 patients were included (mean age, 26.0 years; range, 17.4-35.5 years; 84.7% male). The mean time to RTS was 6.8 months (range, 3.7-11.9 months). There was a 76.3% rate of any RTS; of the 1212 patients who reported level of play at return, 305 (25.2%) were unable to perform at their prior level. Psychological reasons were cited by 85% (n = 360) of patients who did not RTS. Fear of reinjury was the most common reason (n = 154; 42.8%); other psychological factors included lack of confidence (n = 46; 12.8%), anxiety (n = 45; 12.5%), depression (n = 44; 12.2%), psychosocial factors (n = 48; 13.3%), and lack of motivation (n = 23; 6.4%). The Shoulder Instability Return to Sport after Injury, Western Ontario Shoulder Instability Index, Quick Inventory of Depressive Symptoms Self Report, Degree of Shoulder Involvement in Sports, Tampa Scale of Kinesiophobia-11, and Veterans Rand 12-Item Health Survey were reported measures for assessing psychology and RTS.
Conclusion:
Fear of reinjury was found to be the most commonly reported impediment to RTS. The psychological characteristics identified through this review may be incorporated into future RTS protocols seeking to address resilience and nonphysical factors associated with RTS.
Keywords: shoulder instability, sport psychology, psychological readiness, return to sport, return to play
Surgical intervention for shoulder instability is commonly performed for patients with the goals of restoring shoulder function and stability while facilitating timely return to preinjury levels of activity. Glenohumeral instability is a diagnosis that ranges from apprehension and microinstability to frank dislocation and occurs with an incidence of 0.12 injuries per 1000 athletes. Further, shoulder instability is a significant cause of missed time from sport.34,54 Currently available data regarding rates of return to sport (RTS) vary with estimates ranging by surgical technique, injury mechanism, and patient-specific factors; however, estimates for RTS rates after shoulder surgery often range between 70% and 95%.31-43 However, the estimates of the rate of return to preinjury levels of activity and competition are currently limited, potentially due to a lack of activity-level assessment standardization.22,30,37 A recent meta-analysis identifying studies reporting RTS after surgery for shoulder instability found that, on average, 73% of people returned to any sport and 65% returned to their preinjury level of sport. 41 Factors currently known to influence RTS include age, sex, surgical technique, traumatic injury pattern, contact and collision sports, and overhead sports participation.18,21,35,49,56
RTS after shoulder surgery is of paramount importance to both athletes and their treating physicians. Despite the numerous advances in the treatment of shoulder instability, recent studies have begun to identify discrepancies between objective functional data and patient perceptions of their injury and readiness to RTS.20,33,42 Factors affecting RTS after shoulder instability surgery are multifactorial, and psychosocial factors affecting RTS after shoulder instability surgery are not yet well described in the current literature.
The purpose of this systematic review was to identify psychological factors associated with RTS after surgical treatment of glenohumeral instability and evaluate the prognostic utility of various psychological factors. Further, we sought to assess the currently available metrics used to assess psychological RTS readiness. We hypothesized that psychological factors would be reported in the literature as critical elements influencing a patient's RTS.
Methods
Study Population and Design
A systematic review of the MEDLINE (PubMed), Embase, and Cochrane databases was performed to identify studies from 1996 to March 2022 reporting RTS after shoulder instability surgery. The following search term was constructed: (((shoulder instability return sport) OR (shoulder instability return play)) OR (shoulder instability surgery return sport)) OR (shoulder instability surgery return play))). The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines with the PRISMA checklist were appropriately applied. Following the PICO framework, we sought to investigate (Population) athletes with anterior shoulder instability, treated with (Intervention) surgical stabilization, to assess (Comparison) the influence of psychology on (Outcome) RTS rates. 9
Two authors (D.G. and N.M.) independently screened abstracts and manuscripts for clinical studies reporting on the psychological determinants of RTS. If there was a disagreement regarding study inclusion between the first 2 reviewers, a third independent arbitrator (C.H. or R.R.) would review the studies in question and facilitate a decision. The primary search resulted in 743 studies from MEDLINE (PubMed), 635 studies from Embase, and 28 studies from Cochrane. Each article was reviewed for inclusion with the following criteria: English language, studies related to clinical outcomes of shoulder instability surgery, >5 patients included, and assessment of RTS and reports on the impact of psychological factors on RTS (Figure 1).
Figure 1.
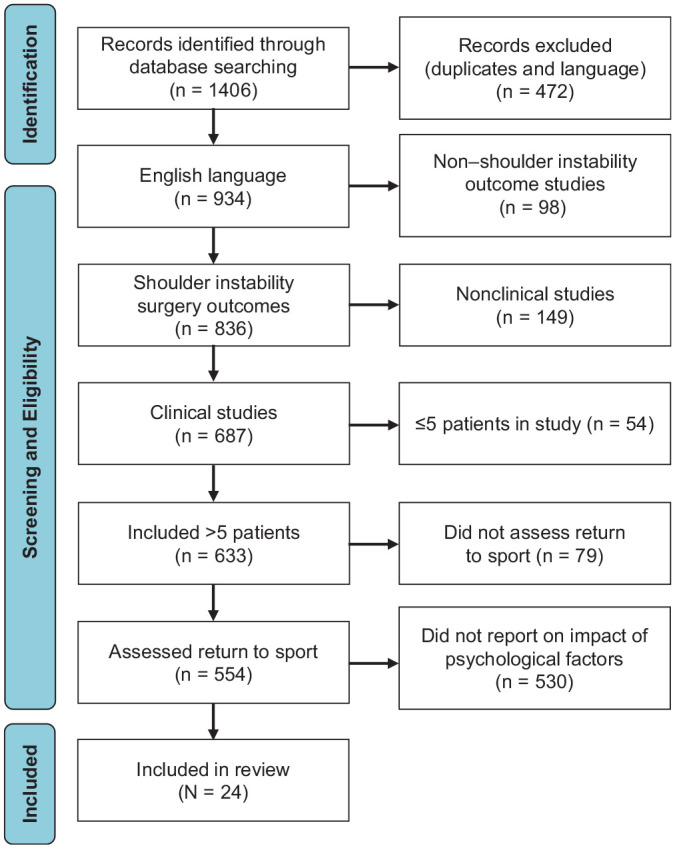
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart of study inclusion and exclusion.
Extracted data from each study included the following: journal and author name, time of publication, level of evidence, number of patients, patient sex, patient age, type of instability surgery, mean follow-up time as well as whether patients returned to sport, the time until RTS, and the level at which they returned. The method of psychological measurement utilized by the studies, psychological reasons reported by patients who did not RTS, and number of patients who cited these reasons were also recorded. Measures of psychological readiness and psychological rationale for not returning to sport were recorded descriptively, as presented by the included studies. Psychosocial factors included closely related yet distinct concepts such as fear of recurrent injury, anxiety, self-efficacy, loss of confidence, hesitancy, motivation, coping strategies, social support, and performance expectations.32,51 In studies in which these specific factors were not further delineated, psychosocial reasons was recorded as the psychological rationale. Rates of RTS and return to prior level were recorded quantitatively as presented in the results of the included studies.
The quality of each study was assessed with the methodological index for nonrandomized studies (MINORS) criteria, a validated scoring tool for nonrandomized studies that includes a 24-point scale for comparative studies and a 16-point scale for noncomparative studies. 47 Random-effects weighted proportion meta-analysis was conducted to quantify the rates of RTS and return to prior level across included studies.
Results
Characteristics of Included Studies and Patients
Of the 969 identified studies, 24 studies § (2.5%) met the formal inclusion criteria. Of these studies, 12 were level 3 evidence and 12 were level 4 evidence. The mean MINORS score was 15.3 (range, 8-24) from the included studies (Table 1). 47 Included studies were primarily cohort studies, as randomized controlled trials assessing psychological factors and RTS were not currently available and case series with ≤5 patients were excluded.
Table 1.
Characteristics of the Included Studies (N = 24) a
| Characteristic | Value |
|---|---|
| Level of evidence | |
| 1 or 2 | 0 (0.0) |
| 3 | 12 (50.0) |
| 4 | 12 (50.0) |
| Mean MINORS score | 15.3 |
| Journal | |
| American Journal of Sports Medicine | 3 |
| Arthroscopy | 2 |
| European Society of Sports Traumatology | 1 |
| Joints | 1 |
| Journal of Shoulder and Elbow Surgery | 1 |
| Journal of Shoulder and Elbow Surgery International | 1 |
| Journal of Sport Rehabilitation | 1 |
| Knee Surgery, Sports Traumatology, Arthroscopy | 2 |
| Orthopaedic Journal of Sports Medicine | 9 |
| Scandinavian Journal of Medicine & Science in Sports | 1 |
| Sports Health | 1 |
| The Surgeon | 1 |
Data are presented as n or n (%) unless otherwise indicated. MINORS, methodological index for non-randomized studies.
A total of 2135 patients were pooled from the included studies. The mean age from these patients was 26.0 years, and 1809 (84.7%) were male. The mean number of dislocations before surgical intervention was 3.6 (range, 0-6), and the mean clinical follow-up was 38.9 months (range, 12-86.2 months) (Table 2).
Table 2.
Clinical and Demographic Characteristics of Included Patients (N = 2135) a
| Characteristic | Value |
|---|---|
| Age, y | 26.0 (17.4-35.5) |
| Sex | |
| Male | 1809 (84.7) |
| Female | 306 (14.3) |
| Not reported | 20 (1.0) |
| Dislocations before surgery | 3.6 (0-6) |
| Type of surgery | |
| Arthroscopic labral repair | 1105 (51.8) |
| Open labral repair/capsular shift | 129 (6.0) |
| Open bone block (Latarjet) | 672 (31.5) |
| Not specified | 229 (10.7) |
| Follow-up time, mo | 38.9 (12-86.2) |
Data are presented as n (%) or mean (range).
Influence of Psychology on RTS
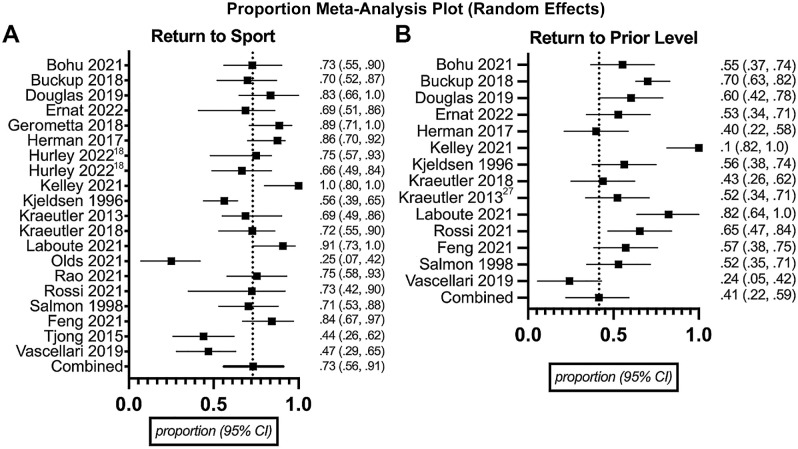
Of the 24 studies, there were 20 studies ‖ (n = 1784 patients) that reported RTS rates and were utilized for formal pooled RTS analysis; the remaining 4 studies14,25,53,55 were included because they further validated the role of psychological assessment in instability recovery. The mean reported time until RTS from these studies was 6.8 months (range, 3.7-11.9 months). Of the 1784 patients, 1361 (76.3%) achieved RTS successfully and 423 (23.7%) were unable to RTS. There were 14 studies ¶ (n = 1212 patients) that assessed return to prior activity level. Overall, there was a 76.3% rate of RTS at any level, and of the 1212 patients who reported the degree to which they returned, 305 (25.2%) were unable to perform at their prior level.The rate of RTS within a specific surgical procedure was reported in 16 studies # (n = 1532 patients) and was 76.3%, 67.9%, and 73.6% after arthroscopic labral repair, open labral repair, and Latarjet, respectively. Four studies13,33,45,53 reported surgical characteristics with only cumulative cohort RTS rates and were subsequently excluded from this surgery-specific RTS subgroup analysis (Table 3). Proportion weighed meta-analysis demonstrated an overall RTS rate of 73% and a 40.7% rate of return to prior level among the studies that assessed psychological factors associated with RTS (Figure 2).
Table 3.
Summary of Study Findings on Psychological Factors and RTS a
| Reported Finding | Value |
|---|---|
| Time to RTS, mo, mean (range) | 6.8 (3.7-11.9) |
| Studies reporting RTS rate (n = 20 studies; 1784 patients) | |
| Patients who achieved RTS | 1361 (76.3) |
| Patients who did not achieve RTS | 423 (23.7) |
| Patients with psychological reason for no RTS | 360 (85.1) |
| Studies reporting return to prior level (n = 14 studies; 1212 patients) | |
| Patients who achieved RTS but not at prior level | 305 (25.2) |
| Studies reporting surgery-specific RTS rate (n = 16 studies; 1532 patients) b | |
| RTS after arthroscopic labral repair | 703/921 (76.3) |
| RTS after open labral repair or capsular shift | 57/84 (67.9) |
| RTS after open bone block (Latarjet) | 388/527 (73.6) |
Data are presented as No. of patients (%) unless otherwise indicated. RTS, return to sport.
Values separated by virgule are No. of patients/No. in the surgery-specific subcohort (percentage).
Figure 2.
Results of meta-analysis of the included studies that (A) assessed for any return to sport and (B) assessed for return to prior activity level.
Among the 423 patients who were unable to RTS, 360 (85.1%) cited a psychological reason. Fear of reinjury was cited by 154 patients (42.8%) as their primary reason for not returning to their sport. Psychosocial factors otherwise not categorized were cited by 48 patients (13.3%). Lack of confidence (n = 46; 12.8%), anxiety (n = 45; 12.5%), depression (n = 44; 12.2%), and lack of motivation (n = 23; 6.4%) were other psychological factors cited as reasons for not returning to their sport (Table 4).
Table 4.
Patient-Cited Factors Affecting RTS a
| Factors Affecting RTS | Patients (n = 360) | Studies (n = 15) |
|---|---|---|
| Anxiety | 45 (12.5) | 2 (13.3) |
| Depression | 44 (12.2) | 1 (6.7) |
| Fear of reinjury | 154 (42.8) | 8 (53.3) |
| Lack of confidence | 46 (12.8) | 4 (26.7) |
| Lack of motivation | 23 (6.4) | 3 (20.0) |
| Psychosocial | 48 (13.3) | 6 (40.0) |
Data are presented as n (%). RTS, return to sport.
Objective psychological assessment tools frequently utilized to assess psychology and RTS included the Shoulder Instability Return to Sport after Injury (SIRSI),3,13 Western Ontario Shoulder Instability Index (WOSI),20,33 Quick Inventory of Depressive Symptoms Self Report (QIDS-SR16), 55 Degree of Shoulder Involvement in Sports (DOSIS), 2 Tampa Scale of Kinesiophobia-11 (TSK-11), 53 and Veterans Rand 12-Item Health Survey (VR-12). 42 Preoperative factors associated with RTS included perceived social support, mood (anxiety, depression), and the patient's expectations of surgery as well as the preoperative WOSI emotion. Postoperative factors influencing RTS included risk-taking behavior and the subjective sense of stability and confidence in one's shoulder, along with objective measures of psychological readiness for RTS that included SIRSI, TSK-11, WOSI, DOSIS, VR-12 mental health, and QIDS-SR16.
Discussion
The most important finding from our review was that among studies assessing psychological factors and shoulder instability, 85.1% of athletes who did not RTS had a psychological reason for not returning. The success of shoulder instability treatment is typically defined by the lack of recurrent dislocation after surgery. For competitive athletes, an additional measure for the success of surgery is RTS and return to preinjury sport level. It should be noted that if a patient does not RTS, his or her risk of redislocation will be inherently low. There is an increasing body of evidence demonstrating excellent RTS outcomes after surgical intervention for shoulder instability.6,7,28,38,39 Despite advances in surgical technique and rehabilitation, there is a persistent cohort of patients who are unable to achieve a full RTS after shoulder surgery. 12 We posit that psychological factors are a key contributor among this cohort of patients.
Rossi et al 42 reported in their study on arthroscopic Bankart repair that 74% of patients who did not RTS cited reasons independent of shoulder function. Their finding, along with the 85.1% reported in the current review, was higher than rates previously cited in other sports injury literature such as anterior cruciate ligament (ACL) reconstruction, where 64.7% of patients reported psychological reasons for not returning to sport.5,32 The most commonly cited factor for not returning to sport in our review was fear of reinjury, also called kinesiophobia, cited by 42.8% of patients. Additionally, 13.3% of patients cited psychosocial factors such as lack of social support, and 6.4% cited lack of motivation. These rates are higher than a recent systematic review in arthroscopic Bankart repair surgery from Kim et al, 21 which found that 17.7% of patients cited fear of reinjury and 8.5% cited lack of motivation as factors impeding RTS. These previously documented psychological impediments to RTS are consistent with our results that fear of reinjury is the most commonly reported psychological factor affecting RTS in shoulder stabilization surgery.
Depression and anxiety have been found to be independent risk factors for poorer outcomes in shoulder stabilization surgery.16,32,55 Depression and anxiety were cited by 12.2% and 12.5%, respectively, of patients in our review as factors limiting RTS. The prevalence of preoperative depression in patients with shoulder instability has been reported as high as 51%, significantly higher than the prevalence nationally as well as numbers found in other sports-related surgeries such as ACL reconstruction (23%). 32 Weekes et al 55 compared outcomes in patients with and without preoperative depression who underwent shoulder stabilization surgery where both groups had significant improvement in postoperative outcomes at 12 months; yet, depressed patients had lower outcome scores. They observed no correlation between preoperative and postoperative shoulder function in their study, providing further evidence that depression has a significant impact on shoulder function outcomes after stabilization surgery.
In the current review, the mean time until RTS was 6.8 months. This is consistent with current literature that demonstrates an RTS of 5.9 months after arthroscopic Bankart, 8.2 months after open Bankart, 5.1 months after open Latarjet, 5.9 months after arthroscopic Latarjet, and 7 months after arthroscopic Bankart with remplissage.1,6,19,22,30 There is no standard definition for RTS in the peer-reviewed literature. Few studies explicitly define RTS, with many of the data being self-reported. Therefore, there may be a contribution of selection bias contributing to the lower RTS found in our review of studies that included a psychological component compared with prior reviews. Nonetheless, there are a significant number of athletes who either do not RTS or do not return to their previous level of activity after shoulder stabilization surgery whose reasons may be independent of shoulder function. The results of this study support the hypothesis that psychological factors could account for this gap.
A growing understanding of the significance of psychological factors on RTS and outcomes independent of shoulder function has led to the utilization of a variety of measurement tools in shoulder stabilization surgery. The data from this study identified the following measurement tools: SIRSI, QIDS-SR16, WOSI, and the DOSIS. These assessments have independently demonstrated significant predictive ability in quantifying the impact of psychological factors on RTS.13,23,52,55
The SIRSI is a consistent self-assessment scale that was adapted from an analogous ACL scale that can be utilized to assess an athlete's psychological readiness to RTS. 13 SIRSI scores are often significantly higher among patients who successfully RTS.3,13,17,18 While not currently popularized within surgical fields, the QIDS-SR16 has been utilized as a depression-screening tool among athletes with higher scores indicating higher risks for depression.44,50,55 The WOSI is a 21-item, self-administered questionnaire that comprises 4 domains (physical symptoms, work, lifestyle, emotions). 23 WOSI scores have been validated after shoulder surgery with patients unable to RTS reporting higher scores. 33 Further, the WOSI emotion subscale domain has been independently associated with delayed RTS.33,52 The DOSIS assessment was developed to address sport-specific psychometric properties among athletes with anterior shoulder instability. 2 Lower DOSIS scores often correlate with greater degrees of subjective shoulder instability. 52
This review highlights several preoperative and postoperative screening assessments that may be utilized after shoulder stabilization surgery. Fully understanding the patient's expectations and perceptions of surgery, anxiety and depression levels before surgery, and other psychosocial factors that may affect their recovery in the preoperative period allows for early intervention, which may improve postoperative outcomes. In addition to employing preoperative screening measures, we posit that psychological assessments should be considered in postoperative rehabilitation. These objective measures may be used to assist in determining the psychological readiness of an athlete to RTS. These objective assessments also may have a role such that rehabilitation care can be best tailored to address the specific psychological barriers an athlete may encounter. Future work can be performed to further validate the psychological tools discussed in this review and investigate optimal-use methodologies of objective psychological measures to target postoperative rehabilitation more appropriately after shoulder instability surgery.
Limitations
The presented study has several limitations. The methodological quality of the included studies varied and may have limited the overall quality of data and subsequent analysis that we were able to extract and perform. We did not limit our review and inclusion of studies to recently published articles because of the expected paucity of included studies; as such, the analyzed data included in this review spanned several decades. This wide inclusion undoubtedly resulted in a heterogeneity of clinical practices and outcomes including surgical techniques, rehabilitation protocols, and RTS criteria. Another limitation of the presented studies lies in the inherent crossover between psychological and physical function factors that allow successful RTS. Many patients may exhibit a fear of reinjury if they have persistent apprehension in the abduction external rotation position, which makes identifying a single causative factor difficult. Finally, given the currently available data in the literature, we were unable to quantify the degree of revision surgeries within our cohort of patients. Given the 31.5% incidence of Latarjet procedures among our included patients, one could posit that there was a greater degree of revision surgeries among the included cohort. One might anticipate that athletes requiring revision surgeries are faced with additional psychological challenges affecting their RTS.
Future prospective studies are needed to assess the efficacy and compare the usefulness of the presented psychological measures identified throughout this review. Subgroup analysis among varied populations and postoperative time frames may also yield insightful additions to the shoulder instability literature. While RTS is one component of successful surgery for shoulder instability, the presented study limited its scope and did not assess the role of psychology on shoulder function or other patient-reported outcome scores that are also important for successful outcomes.
Conclusion
Psychological factors play an important role in RTS after shoulder instability surgery. Fear of reinjury, anxiety, depression, and lack of confidence were all commonly cited as reasons for not returning to sport after shoulder instability surgery. Further understanding of both the preoperative and postoperative psychosocial risk factors that affect a patient's ability to RTS is of the utmost importance in maximizing outcomes after shoulder instability surgery.
Footnotes
Final revision submitted May 10, 2023; accepted June 2, 2023.
One or more of the authors has declared the following potential conflict of interest or source of funding: C.H. has received honoraria from Musculoskeletal Transplant Foundation. G.J. has received honoraria from MTF Biologics. J.B. has received consulting fees from Stryker and Linvatec, nonconsulting fees from Smith & Nephew, and hospitality payments from Stryker. G.C. has received education payments from Arthrex and Smith & Nephew. R.R. has received education payments from Smith & Nephew and hospitality payments from Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Abdul-Rassoul H, Galvin JW, Curry EJ, Simon J, Li X. Return to sport after surgical treatment for anterior shoulder instability: a systematic review. Am J Sports Med. 2019;47(6):1507-1515. doi: 10.1177/0363546518780934 [DOI] [PubMed] [Google Scholar]
- 2. Blonna D, Bellato E, Bonasia DE, et al. Design and testing of the Degree of Shoulder Involvement in Sports (DOSIS) scale. Am J Sports Med. 2015;43(10):2423-2430. doi: 10.1177/0363546515597485 [DOI] [PubMed] [Google Scholar]
- 3. Bohu Y, Abadie P, van Rooij F, Nover L, Berhouet J, Hardy A. Latarjet procedure enables 73% to return to play within 8 months depending on preoperative SIRSI and Rowe scores. Knee Surg Sports Traumatol Arthrosc. 2021;29(8):2606-2615. doi: 10.1007/s00167-021-06475-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Buckup J, Welsch F, Gramlich Y, et al. Back to sports after arthroscopic revision Bankart repair. Orthop J Sports Med. 2018;6(2):2325967118755452. doi: 10.1177/2325967118755452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Burland JP, Toonstra JL, Howard JS. Psychosocial barriers after anterior cruciate ligament reconstruction: a clinical review of factors influencing postoperative success. Sports Health. 2019;11(6):528-534. doi: 10.1177/1941738119869333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chen AZ, Greaves KM, deMeireles AJ, Fortney TA, Saltzman BM, Trofa DP. Clinical outcomes of arthroscopic bony Bankart repair for anterior instability of the shoulder: a systematic review. Am J Sports Med. 2023;51(10):2758-2765. doi: 10.1177/03635465221094832 [DOI] [PubMed] [Google Scholar]
- 7. Domos P, Gokaraju K, Walch G. Long-term outcomes after the open Latarjet procedure for the surgical management of humeral avulsion of the glenohumeral ligament lesions. Am J Sports Med. 2022;50(9):2476-2480. doi: 10.1177/03635465221102904 [DOI] [PubMed] [Google Scholar]
- 8. Douglas L, Whitaker J, Nyland J, et al. Return to play and performance perceptions of baseball players after isolated SLAP tear repair. Orthop J Sports Med. 2019;7(3):2325967119829486. doi: 10.1177/2325967119829486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Eriksen MB, Frandsen TF. The impact of patient, intervention, comparison, outcome (PICO) as a search strategy tool on literature search quality: a systematic review. J Med Libr Assoc. 2018;106(4):420-431. doi: 10.5195/jmla.2018.345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ernat JJ, Rakowski DR, Hanson JA, et al. High rate of return to sport and excellent patient-reported outcomes after an open Latarjet procedure. J Shoulder Elbow Surg. 2022;31(8):1704-1712. doi: 10.1016/j.jse.2022.01.139 [DOI] [PubMed] [Google Scholar]
- 11. Feng S, Chen M, Chen J, Li H, Chen J, Chen S. Patient outcomes and fear of returning to sports after arthroscopic Bankart repair with remplissage. Orthop J Sports Med. 2021;9(4):23259671211001775. doi: 10.1177/23259671211001775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Galvin JW, Yu H, Slevin J, et al. High incidence of anterior shoulder pain in young athletes undergoing arthroscopic posterior labral repair for posterior shoulder instability. Arthrosc Sports Med Rehabil. 2021;3(5):e1441-e1447. doi: 10.1016/j.asmr.2021.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gerometta A, Klouche S, Herman S, Lefevre N, Bohu Y. The Shoulder Instability–Return to Sport after Injury (SIRSI): a valid and reproducible scale to quantify psychological readiness to return to sport after traumatic shoulder instability. Knee Surg Sports Traumatol Arthrosc. 2018;26(1):203-211. doi: 10.1007/s00167-017-4645-0 [DOI] [PubMed] [Google Scholar]
- 14. Gottlieb U, Springer S. The relationship between fear avoidance beliefs, muscle strength, and short-term disability after surgical repair of shoulder instability. J Sport Rehabil. 2021;30(7):973-980. doi: 10.1123/jsr.2020-0035 [DOI] [PubMed] [Google Scholar]
- 15. Herman S, Bohu Y, Klouche S, Lefevre N, Gerometta A. Should we stabilizing surgically [sic] the shoulder of the athlete after the first episode of instability? Comparative study versus conservative treatment in 138 rugby players. Arthroscopy. 2017;33(10):e164-e165. doi: 10.1016/j.arthro.2017.08.213 [DOI] [Google Scholar]
- 16. Hines AC, Pill SG, Boes N, et al. Mental health status, not resilience, influences functional recovery after arthroscopic rotator cuff repairs. J Shoulder Elbow Surg. 2022;31(6)(suppl):S117-S122. doi: 10.1016/j.jse.2022.02.005 [DOI] [PubMed] [Google Scholar]
- 17. Hurley ET, Davey MS, Mojica ES, et al. Analysis of patients unable to return to play following arthroscopic Bankart repair. Surgeon. 2022;20(4):e158-e162. doi: 10.1016/j.surge.2021.06.005 [DOI] [PubMed] [Google Scholar]
- 18. Hurley ET, Davey MS, Montgomery C, et al. Analysis of athletes who did not return to play after open Latarjet. Orthop J Sports Med. 2022;10(2):23259671211071082. doi: 10.1177/23259671211071082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kasik CS, Rosen MR, Saper MG, Zondervan RL. High rate of return to sport in adolescent athletes following anterior shoulder stabilisation: a systematic review. J ISAKOS. 2019;4(1):33-40. doi: 10.1136/jisakos-2018-000224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kelley TD, Clegg S, Rodenhouse P, Hinz J, Busconi BD. Functional rehabilitation and return to play after arthroscopic surgical stabilization for anterior shoulder instability. Sports Health. 2022;14(5):733-739. doi: 10.1177/19417381211062852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kim M, Haratian A, Fathi A, et al. Can we identify why athletes fail to return to sports after arthroscopic Bankart repair: a systematic review and meta-analysis. Am J Sports Med. 2023;51(9):2480-2486. doi: 10.1177/03635465221089980 [DOI] [PubMed] [Google Scholar]
- 22. Kim SH, Ha KI, Kim SH. Bankart repair in traumatic anterior shoulder instability: open versus arthroscopic technique. Arthroscopy. 2002;18(7):755-763. doi: 10.1053/jars.2002.31701 [DOI] [PubMed] [Google Scholar]
- 23. Kirkley A, Griffin S, McLintock H, Ng L. The development and evaluation of a disease-specific quality of life measurement tool for shoulder instability. Am J Sports Med. 1998;26(6):764-772. doi: 10.1177/03635465980260060501 [DOI] [PubMed] [Google Scholar]
- 24. Kjeldsen SR, Tordrup PJ, Hvidt EP. Return to sport after a Bankart operation of the shoulder using the Mitek anchor system. Scand J Med Sci Sports. 1996;6(6):346-351. doi: 10.1111/j.1600-0838.1996.tb00105.x [DOI] [PubMed] [Google Scholar]
- 25. Kordasiewicz B, Małachowski K, Kiciński M, et al. Intraoperative graft-related complications are a risk factor for recurrence in arthroscopic Latarjet stabilisation. Knee Surg Sports Traumatol Arthrosc. 2019;27(10):3230-3239. doi: 10.1007/s00167-019-05400-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kraeutler MJ, Aberle N, II, Brown CC, Ptasinski JJ, McCarty EC. Clinical outcomes and return to sport after arthroscopic anterior, posterior, and combined shoulder stabilization. Orthop J Sports Med. 2018;6(4):2325967118763754. doi: 10.1177/2325967118763754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kraeutler MJ, Aberle N, II, Long C, McCarty EC. Return to sport following arthroscopic anterior shoulder stabilization: High outcome scores despite moderate rate of return to play. Orthop J Sports Med. 2013;1(4): 2325967113S00098. doi: 10.1177/2325967113S00098 [DOI] [Google Scholar]
- 28. Krespi R, Maman E, Factor S, et al. Combined Bankart and SLAP repair: patient-reported outcome measurements after a minimum 5-year follow-up. Arch Orthop Trauma Surg. 2023;143(5):2621-2626. doi: 10.1007/s00402-022-04599-8 [DOI] [PubMed] [Google Scholar]
- 29. Laboute E, Hoffmann R, Bealu A, Ucay O, Verhaeghe E. Recurrence and return to sport after surgery for shoulder instability: arthroscopic Bankart versus Latarjet procedure. JSES Int. 2021;5(4):609-615. doi: 10.1016/j.jseint.2021.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Memon M, Kay J, Cadet ER, Shahsavar S, Simunovic N, Ayeni OR. Return to sport following arthroscopic Bankart repair: a systematic review. J Shoulder Elbow Surg. 2018;27(7):1342-1347. doi: 10.1016/j.jse.2018.02.044 [DOI] [PubMed] [Google Scholar]
- 31. Kraeutler MJ, Aberle N, II, Long C, McCarty EC. Return to sport following arthroscopic anterior shoulder stabilization: high outcome scores despite moderate rate of return to play. Orthop J Sports Med. 2013;1(4)(suppl):2325967113S00098. [Google Scholar]
- 32. Nwachukwu BU, Adjei J, Rauck RC, et al. How much do psychological factors affect lack of return to play after anterior cruciate ligament reconstruction? A systematic review. Orthop J Sports Med. 2019;7(5):2325967119845313. doi: 10.1177/2325967119845313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Olds M, Webster KE. Factor structure of the Shoulder Instability Return to Sport after Injury scale: performance confidence, reinjury fear and risk, emotions, rehabilitation and surgery. Am J Sports Med. 2021;49(10):2737-2742. doi: 10.1177/03635465211024924 [DOI] [PubMed] [Google Scholar]
- 34. Owens BD, Agel J, Mountcastle SB, Cameron KL, Nelson BJ. Incidence of glenohumeral instability in collegiate athletics. Am J Sports Med. 2009;37(9):1750-1754. doi: 10.1177/0363546509334591 [DOI] [PubMed] [Google Scholar]
- 35. Pavlik A, Tátrai M, Papp E. Return to sport after arthroscopic treatment of posterior shoulder instability. Orthop J Sports Med. 2020;8(12):2325967120969151. doi: 10.1177/2325967120969151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Petrera M, Dwyer T, Tsuji MR, Theodoropoulos JS. Outcomes of arthroscopic Bankart repair in collision versus noncollision athletes. Orthopedics. 2013;36(5):e621-e626. doi: 10.3928/01477447-20130426-25 [DOI] [PubMed] [Google Scholar]
- 37. Plath JE, Feucht MJ, Saier T, et al. Sporting activity after arthroscopic Bankart repair for chronic glenohumeral instability. Arthroscopy. 2015;31(10):1996-2003. doi: 10.1016/j.arthro.2015.04.087 [DOI] [PubMed] [Google Scholar]
- 38. Polio W, Brolin TJ. Remplissage for anterior shoulder instability: history, indications, and outcomes. Orthop Clin North Am. 2022;53(3):327-338. doi: 10.1016/j.ocl.2022.02.005 [DOI] [PubMed] [Google Scholar]
- 39. Provencher CMT, Midtgaard KS. Editorial commentary: evidence to support surgical intervention for first-time shoulder instability: stabilize them early! Arthroscopy. 2020;36(9):2533-2536. doi: 10.1016/j.arthro.2020.07.034 [DOI] [PubMed] [Google Scholar]
- 40. Rao S, Jeyamohan H, D’Amore T, et al. Return to play in adolescent baseball players after SLAP repair (131). Orthop J Sports Med. 2021;9(10 suppl5): 2325967121S00274. doi: 10.1177/2325967121S00274. [DOI] [Google Scholar]
- 41. Rossi LA, Pasqualini I, Tanoira I, Ranalletta M. Factors that influence the return to sport after arthroscopic Bankart repair for glenohumeral instability. Open Access J Sports Med. 2022;13:35-40. doi: 10.2147/oajsm.S340699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Rossi LA, Tanoira I, Brandariz R, Pasqualini I, Ranalletta M. Reasons why athletes do not return to sports after arthroscopic Bankart repair: a comparative study of 208 athletes with minimum 2-year follow-up. Orthop J Sports Med. 2021;9(7):23259671211013394. doi: 10.1177/23259671211013394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Rossi LA, Tanoira I, Gorodischer T, Pasqualini I, Ranalletta M. High variability in functional outcomes and recurrences between contact sports after arthroscopic Bankart repair: a comparative study of 351 patients with a minimum 3-year follow-up. Arthrosc Sports Med Rehabil. 2020;2(5):e575-e581. doi: 10.1016/j.asmr.2020.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Rush AJ, Trivedi MH, Carmody TJ, et al. Self-reported depressive symptom measures: sensitivity to detecting change in a randomized, controlled trial of chronically depressed, nonpsychotic outpatients. Neuropsychopharmacology. 2005;30(2):405-416. doi: 10.1038/sj.npp.1300614 [DOI] [PubMed] [Google Scholar]
- 45. Rao S, Jeyamohan H, D’Amore T, et al. Return to play in adolescent baseball players after SLAP repair (131). Orthop J Sports Med. 2021;9(10)(suppl 5):2325967121S00274. [Google Scholar]
- 46. Salmon JM, Bell SN. Arthroscopic stabilization of the shoulder for acute primary dislocations using a transglenoid suture technique. Arthroscopy. 1998;14(2):143-147. doi: 10.1016/s0749-8063(98)70032-5 [DOI] [PubMed] [Google Scholar]
- 47. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712-716. doi: 10.1046/j.1445-2197.2003.02748.x [DOI] [PubMed] [Google Scholar]
- 48. Tjong VK, Devitt BM, Murnaghan ML, Ogilvie-Harris DJ, Theodoropoulos JS. A qualitative investigation of return to sport after arthroscopic Bankart repair: beyond stability. Am J Sports Med. 2015;43(8):2005-2011. doi: 10.1177/0363546515590222 [DOI] [PubMed] [Google Scholar]
- 49. Trikha R, Schroeder GG, Greig DE, Kremen TJ., Jr. Characterizing health events and return to sport in collegiate swimmers. Orthop J Sports Med. 2022;10(4):23259671221083588. doi: 10.1177/23259671221083588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Trivedi MH, Rush AJ, Ibrahim HM, et al. The Inventory of Depressive Symptomatology, Clinician Rating (IDS-C) and Self-Report (IDS-SR), and the Quick Inventory of Depressive Symptomatology, Clinician Rating (QIDS-C) and Self-Report (QIDS-SR) in public sector patients with mood disorders: a psychometric evaluation. Psychol Med. 2004;34(1):73-82. doi: 10.1017/s0033291703001107 [DOI] [PubMed] [Google Scholar]
- 51. van Ierssel J, Pennock KF, Sampson M, Zemek R, Caron JG. Which psychosocial factors are associated with return to sport following concussion? A systematic review. J Sport Health Sci. 2022;11(4):438-449. doi: 10.1016/j.jshs.2022.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Vascellari A, Ramponi C, Venturin D, Ben G, Blonna D, Coletti N. The Degree of Shoulder Involvement in Sports (DOSIS) scale is a valid and responsive instrumentation for shoulder assessment in patients after surgery for anterior instability. Knee Surg Sports Traumatol Arthrosc. 2018;26(1):195-202. doi: 10.1007/s00167-017-4642-3 [DOI] [PubMed] [Google Scholar]
- 53. Vascellari A, Ramponi C, Venturin D, Ben G, Coletti N. The relationship between kinesiophobia and return to sport after shoulder surgery for recurrent anterior instability. Joints. 2019;7(4):148-154. doi: 10.1055/s-0041-1730975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Watson S, Allen B, Grant JA. A clinical review of return-to-play considerations after anterior shoulder dislocation. Sports Health. 2016;8(4):336-341. doi: 10.1177/1941738116651956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Weekes DG, Campbell RE, Shi WJ, et al. Prevalence of clinical depression among patients after shoulder stabilization: a prospective study. J Bone Joint Surg Am. 2019;101(18):1628-1635. doi: 10.2106/jbjs.18.01460 [DOI] [PubMed] [Google Scholar]
- 56. Wilbur RR, Shirley MB, Nauert RF, et al. Anterior shoulder instability in throwers and overhead athletes: long-term outcomes in a geographic cohort. Am J Sports Med. 2022;50(1):182-188. doi: 10.1177/03635465211059195 [DOI] [PubMed] [Google Scholar]