Abstract
The aim of the study is to reach objective results about the ergonomic risks of nurses’ working postures not only by using questionnaires but also by using Rapid Entire Body Assessment (REBA) and Rapid Upper Limb Assessment (RULA) methods, which are risk assessment methods used in engineering fields. This study is a cross-sectional study. First of all, 383 nurses were evaluated with a survey. 91.4% of the nurses were women and 6.5% were men. Average age (female: 38.20; male: 31.5), average weight (female: 65.60 kg; male: 81.50 kg), average height (female: 162.7 cm; male: 176.80 cm) and average body mass index (female: 24.80; male: 26) were calculated. In the hospital, which we grouped into in the hospital, which we divided into eight workstations, the REBA and RULA scores of the three nurses working at each workstation were calculated and the average REBA and RULA scores of the workstations were determined. The percentage of those who experienced musculoskeletal pain in the last 1 year at each workstation and the mean REBA–RULA scores were as follows; ward (92%; 6.92–5.69), operating room (98%; 10–7), emergency department (100%; 6.08–5.33), outpatient clinic (75%; 5.5–5.16), intensive care (94%; 6.21–5.57), administrative affairs (94%; 5–5), laboratory (95%; 5.80–5.2) and interventional procedure (92%; 6.4–5.4). In these stations, the highest scores were seen in the operating room. In the questionnaire, 92.46% of the nurses reported having complaints in at least one part of the musculoskeletal system in the last year. The hospital weighted mean score was REBA 6.86 and RULA 5.71. When REBA and RULA measurements were evaluated, it was determined that the risk in the departments where the nurses worked was generally at the medium risk level. REBA and RULA scores indicate that ergonomic changes and adjustments should be made. For this determination, the risks of working postures should be determined with quantitative methods.
Keywords: Ergonomics, musculoskeletal system, REBA, RULA, nurse
Introduction
Studies conducted in recent years have shown that there has been an increase in work-related musculoskeletal diseases (WRMD), which are accepted as occupational diseases in many industrializing countries.
In a study involving 6500 people in Finland, 35.1% of people had chronic pain. 1 In an article published in 2016, it was stated that 50% of the work-related ailments constituted WRMD, and today it ranks third in terms of applying to a health institution due to these ailments. 2
The incidence of WRMD, announced by the U.S. Bureau of Labor Statistics in 2020, was 25.4 per ten thousand. 3 At least one WRMD was detected in 19.7% of those who applied to the occupational diseases outpatient clinic of a university hospital in Turkey between 2015 and 2018. 4 According to the World Health Organization, an average of 1.71 billion people in the world have musculoskeletal disorders and they think that this number will increase. 5 According to the data of the European Agency for Occupational Health and Safety, the loss of incapacity life years (DALY) due to the WRMD in 2019 constituted 15% of the total. 6 Health sector working conditions are more stressful and problematic when compared to different business lines. It has been shown that the quality of working life of nurses who are health workers is also related to musculoskeletal diseases.7,8
At the point of work-related musculoskeletal system diseases, more research is being carried out in the field of health, as in all business sectors, to reduce the frequency of musculoskeletal system diseases in the world and in Turkey, to detect the changes that have occurred over the years and to make improvements. 9
Ergonomic risk analysis methods are technically divided into three categories. These are the recording method, systematic observational methods and direct measurement methods. 10 Rapid Entire Body Assessment (REBA) and Rapid Upper Limb Assessment (RULA) are systematic observational methods. Measurement evaluation with video recordings falls under advanced observation methods. Finally, there are risk analyses that are called direct measurement methods, that is, measurements made with optical instruments attached to the human body. 11
With these new and advanced methods other than questionnaire scales, pictures are taken according to the posture of the people in their work, and parameters such as extremity movements, joint angles and the loads they are exposed to are determined by the standard scores and more realistic body risk analyses are revealed. 12
REBA is preferred because it is suitable for workplace use, fast, has practical results, is economical, and does not require a device that can disturb the employee and prevent the execution of the work. This method is a simple observation-based method designed by McAtamney and Hignett in 1999 and is designed to be sensitive to the types of unpredictable working postures that exist in other service sectors, especially in the healthcare sector.13–15
One hundred and forty-four posture combinations were coded independently by ergonomists and physiotherapists, and then load, grip, and activity scores were combined to produce the REBA outcome score, which determines risk and action levels. 15
In 1993, McAtamney developed RULA to analyze the working postures of the trunk and legs, that is, neck, upper arms, lower arms and wrists. It is a method that evaluates the risks of different ergonomic impacts in terms of WRMD. It is a simple and fast observational method used in workplaces.16,17
RULA is one of the two commonly used analysis methods together with REBA to study economic reasons and ease of use. 18 RULA assessment is performed on the upper and lower parts of the body. It is mostly used to measure body risks for sedentary and laid jobs. 19 The ideal working posture in terms of its effects on the employee is a working posture that pays attention to the rules according to the posture used. 20 Work posture is an aspect of worker safety. 21 Reports and research conducted in domestic and foreign industrial sites draw attention to musculoskeletal disorders. It is known that the disorder not only causes economic problems but also affects production efficiency. Thanks to such studies, work effort will be reduced and worker safety and productivity will be increased. 22
The purpose of this study conducted on nurses is to include REBA and RULA, which are risk assessment methods based on systematic observation and mostly used in engineering fields, in addition to the survey application. Thus, original, more reliable and generalizable results and evaluations will be achieved in the research.
Methods
The study was carried out with nurses working at Istanbul Medical Faculty Hospital. Ethics committee approval was obtained from the Istanbul University Istanbul Faculty of Medicine Ethics Committee with the date of October 17, 2017 and decision number 1140.
The research materials and methods consist of three parts. The first of these will be explained about the nurse participant form. Demographic information and complaints about the musculoskeletal system were questioned in the questionnaire form. In our study, Erdinç et al. applied the Turkish validity and reliability of Cornell’s “Turkish version of the Cornell Musculoskeletal Discomfort Questionnaire: Cross-cultural adaptation” applied to nurses had values of 0.89. 23
The research population consisted of 862 nurses working at Istanbul Medical Faculty between December 2017 and March 2018. In the literature review, it is understood that approximately 40–60% of healthcare professionals have musculoskeletal disorders.24–26
Accordingly, the sample size was found to be 334 individuals with 50% incidence 95% confidence interval (type I error 0.05, power 0.80) and 6% deviation. 27
where N is the number of individuals in the universe; n is the number of individuals to be sampled; p is the incidence of the event under investigation; q is 1−p; Zα, Zβ are fixed values taken for alpha error and strength of test; d is the acceptable sampling error.
The forms were applied to 402 nurses instead of 334, taking the probability of the nurses working in the hospital to fill in the questionnaires incompletely or not answering them as 20%. When the questionnaire forms were examined, it was determined that there were 19 nurses who did not answer the basic questions, and these were not included in the evaluation. The study was carried out with the participation of 383 nurses.
Before the interview, the researcher introduced herself, stated her purpose and what she wanted to study with them, and informed the nurses about the content of the research. In addition to verbal information, the researcher obtained written consent by filling out the form by creating a section in the questionnaires stating that the necessary information about the research, approval of the Ethics Committee and institutional permissions were created. Working as a nurse at the Istanbul Faculty of Medicine at the time of the study and obtaining voluntary consent were deemed sufficient as inclusion criteria. The exclusion criteria were that the nurse was on leave during the research period or did not give consent to the research and did not answer questions about the musculoskeletal system. The second and third method used in the research, apart from the survey method, was REBA and RULA score calculations.
In REBA, one of these methods, the whole body is evaluated and scoring is done according to the angular values and posture of the relevant part of the body during the posture to be analyzed. The scoring process of the risk caused by the posture or movement analyzed in the REBA method is calculated by following various steps.
With this method, a score ranging from 1 to 15 is determined according to the loads that may occur in the neck, trunk, legs, arms and wrists during work. As this score value progresses from 1 to 15, it is determined that the necessity and urgency of taking precautions increases. 15
It also indicates that the risk level increases. At the last stage, the control measure level of the range corresponding to the REBA score is determined as shown in Table 1. 15
Table 1.
REBA risk rating.
| Degree | REBA score | Risk level | Prevention |
|---|---|---|---|
| 0 | 1 | Negligible | Not necessary |
| 1 | 2–3 | Low | It may be necessary |
| 2 | 4–7 | Middle | Necessary |
| 3 | 8–10 | High | Necessary soon |
| 4 | 11–15 | Very high | Needed immediately |
Hignett and McAtamney. 15
RULA analyzes the working postures of the wrist, lower arm, upper arm, neck, trunk and legs. In the method, the human body is divided into two different groups, A and B. Group A includes the lower arm, upper arm and wrist parts and group B includes the neck, torso and leg parts. The postures of body parts are scored according to their angular range of motion. 17
With the RULA method, musculoskeletal system problems that may occur in the individual can be detected by taking into account the power needed for the work to be done. The effects that may occur on the individual due to working conditions are evaluated with a scoring system. RULA analysis examines the individual's movements, working posture and the risk factor of the load on the musculoskeletal system. The final score obtained after completion of the analysis may vary between 1 and 7. As seen in Table 2, final scores are evaluated by dividing into four different action levels. 17
Table 2.
RULA score action levels.
| Score | Result |
|---|---|
| 1–2 | It is an acceptable result if it is not repeated for a long time. |
| 3–4 | The work done should be analyzed better, some changes can be made. |
| 5–6 | It is necessary to review the work done as soon as possible and make changes in the short term. |
| 7 | There is an urgent need to review and change the work done. |
McAtamney and Nigel Corlett. 17
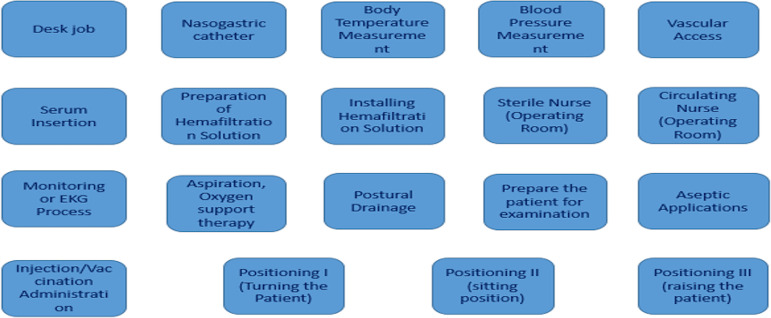
In this study, REBA and RULA scores were calculated at eight designated workstations in order to measure the body risks resulting from nurses’ working postures. These workstations are the departments where “Services, Operating Room, Emergency Service, Polyclinic, Intensive Care, Desk Works, Laboratory and Interventional Procedures” are performed. The 19 jobs most frequently performed by nurses were identified and shown in Figure 1.
Figure 1.
Work done at workstations.
In addition, since the research was conducted in a hospital with very intensive patient services, no pictures could be taken from all nurses. REBA and RULA score calculations were made by taking pictures from a total of 24 nurses, 3 from each workstation.
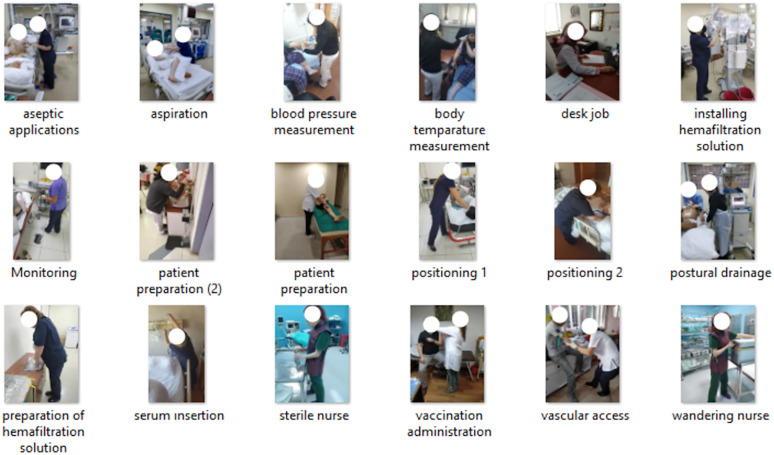
In Figure 2, the working postures of the nurses while performing various tasks at the workstations are photographed.
Figure 2.
Sample pictures where various works were done at various stations in our research.
In the statistical analysis phase, first, descriptive statistics (mean, standard deviation, median, minimum, maximum values and percentage ratio values) were calculated. For each pain region, the risk of pain according to the workstations was examined by logistic regression analysis and the odds ratio (OR) values for the back region, which were significant, were given with 95% confidence intervals. Statistical significance was accepted as two-way and p < 0.05. Statistical Package for Social Sciences 21.00 program was used for statistical evaluation.
Results
Of the 383 nurses participating in the study, 350 (91.4%) were female, 25 (6.5%) were male, and 8 (2.1%) nurses did not specify their gender. Similarly, descriptive statistics for weight, height and body mass index (BMI) variables were calculated over the respondents. Table 3 shows that the mean age of female nurses was 38.20 ± 9.09 years, and the average age of male nurses was 31.50 ± 8.80 years. Again, it was determined that the mean weight of the female nurses who said their weight measurements was 65.60 ± 11.39 kg, and the average weight of the male nurses who answered was 81.50 ± 12.40 kg. The average height of the female nurses who responded to the height measurements was 162.70 ± 5.92 cm and the average height of the male nurses was 176.80 ± 5.90 cm. In light of these data, the mean BMI was calculated to be 24.80 ± 4.29 in female nurses and 26 ± 3.7 in male nurses.
Table 3.
Age, weight, height and BMI distribution by gender.
| Variable | Gender | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Women (n:350) | Male (n:25) | |||||||||||
| n | Average | Sd. | Median | Max. | Min. | n | Average | Sd. | Median | Max. | Min. | |
| Age (n:356) | 331 | 38.20 | 9.09 | 38.00 | 64.0 | 22.00 | 25 | 31.50 | 8.80 | 28.0 | 64.00 | 23.00 |
| Weight (n:364) | 339 | 65.60 | 11.39 | 65.00 | 1100 | 43.00 | 25 | 81.50 | 12.40 | 80.0 | 103.00 | 61.00 |
| Height (n:369) | 344 | 162.70 | 5.92 | 163.00 | 1800 | 148.00 | 25 | 176.80 | 5.90 | 178.00 | 190.00 | 165.00 |
| BMİ (n:364) | 339 | 24.80 | 4.29 | 24.00 | 42.4 | 17.40 | 25 | 26.00 | 3.7 | 25.60 | 34.80 | 19.90 |
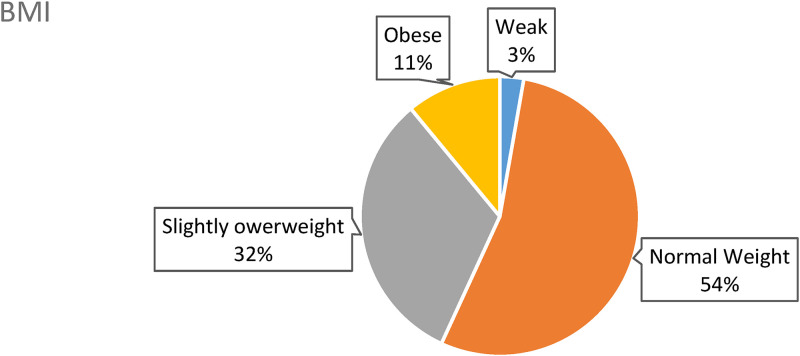
The BMI data of male and female nurses who shared their height and weight information are shown graphically in Figure 3. Three percent of the nurses were evaluated as underweight and 11% were evaluated as obese.
Figure 3.
BMI graph.
Table 4 shows the distribution of musculoskeletal complaints of nurses according to the workstations they work at. As seen in the table, neck pain was experienced in the emergency services with a maximum rate of 87.50%. Shoulder complaints were felt at the highest rate of 81.82% in interventional treatment procedures. Elbow complaints were mostly experienced in laboratories with a rate of 31.58%. Wrist complaints were observed with a rate of 63.64% at the workstation where interventional treatment was performed the most. It is seen in the table that back complaints are experienced at a high rate in almost all workstations, but the highest rate (100%) is experienced in interventional treatment procedures. Low back complaints were experienced at the highest rate of 94.44% in polyclinic nurses. Hip-thigh complaints were highest at the workstation where the interventional procedure was performed at a rate of 54.55%. Knee complaints were mostly experienced in emergency services with a rate of 62.50%. Foot complaints were detected in the polyclinic nurses at the highest rate of 72.22%.
Table 4.
Distribution of pain regions of 355 nurses with complaints by workstations.
| Workstations | Service (n:166) | Operating room (n:44) | Emergency room (n:16) | Policlinic (n:18) | Intensive care (n:66) | Desk jobs (n:15) | Lab (n:19) | İnvasive treatment (n:11) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Extremities | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % |
| Neck | 126 | 75.90 | 34 | 77.27 | 14 | 87.50 | 14 | 77.78 | 45 | 68.18 | 8 | 53.33 | 12 | 63.16 | 8 | 72.73 |
| Shoulder | 111 | 66.87 | 29 | 65.91 | 11 | 68.75 | 12 | 66.67 | 42 | 63.64 | 7 | 46.67 | 12 | 63.16 | 9 | 81.82 |
| Elbow | 30 | 18.07 | 6 | 13.64 | 1 | 6.25 | 4 | 22.22 | 11 | 16.67 | 1 | 6.67 | 6 | 31.58 | 2 | 18.18 |
| Wrist | 76 | 45.78 | 17 | 38.64 | 9 | 56.25 | 10 | 55.56 | 25 | 37.88 | 2 | 13.33 | 10 | 52.63 | 7 | 63.64 |
| Dorsal | 131 | 78.92 | 39 | 88.64 | 15 | 93.75 | 13 | 72.22 | 54 | 81.82 | 14 | 93.33 | 17 | 89.47 | 11 | 100.00 |
| Waist | 132 | 79.52 | 33 | 75.00 | 14 | 87.50 | 17 | 94.44 | 60 | 90.91 | 9 | 60.00 | 15 | 78.95 | 10 | 90.91 |
| Hip/thigh | 73 | 43.98 | 19 | 43.18 | 8 | 50.00 | 8 | 44.44 | 28 | 42.42 | 4 | 26.67 | 5 | 26.32 | 6 | 54.55 |
| Knee | 85 | 51.20 | 19 | 43.18 | 10 | 62.50 | 8 | 44.44 | 30 | 45.45 | 7 | 46.67 | 6 | 31.58 | 5 | 45.45 |
| Foot | 64 | 38.55 | 21 | 47.73 | 9 | 56.25 | 13 | 72.22 | 32 | 48.48 | 1 | 6.67 | 6 | 31.58 | 6 | 54.55 |
As seen in Table 5, when the back region was taken as the dependent variable and the workstations were taken as the independent variable and desk job was chosen as the reference, according to the logistic regression analysis, the nurses in the service had a 1.90 times higher risk of back pain compared to the nurses working at a desk. In addition, nurses working in the outpatient clinics had a 4.31 times higher risk of back pain than nurses working at a desk.
Table 5.
Logistic regression.
| Workstation | OR (95% CI) | p | |
|---|---|---|---|
| Service | 1.90 | (1106–3.29) | 0020 |
| Policlinic | 4.31 | (1.87–9.90) | <0001 |
In Table 6, the REBA scores of the jobs being done at eight workstations and the REBA scores of the workstations average scores are shown. The highest score in the work done is in the operating room nurses.
Table 6.
REBA score values of jobs done at workstations.
| Workstations | Service | Operating room | Emergency room | Policlinic | Intensive care | Desk jobs | Lab | İnvasive treatment |
|---|---|---|---|---|---|---|---|---|
| The work done | REBA | REBA | REBA | REBA | REBA | REBA | REBA | REBA |
| Desk job | 5 | 5 | 5 | 5 | 5 | 5 | 5 | |
| Nasogastric catheter | 5 | 5 | ||||||
| Body temperature measurement | 4 | 4 | 4 | 4 | ||||
| Blood pressure measurement | 5 | 5 | 5 | 5 | 5 | |||
| Vascular access | 5 | 5 | 5 | 5 | 5 | |||
| Serum insertion | 6 | 6 | 6 | 6 | ||||
| Preparation of hemaf. solution | 7 | |||||||
| Installing hemaf. solution | 7 | |||||||
| Sterile nurse | 10 | |||||||
| Circulating nurse | 10 | |||||||
| Monitoring or EKG process | 5 | 5 | 5 | 5 | 5 | |||
| Aspiration, Oxygen therapy | 8 | 8 | 8 | |||||
| Postural drainage | 5 | 5 | 5 | |||||
| Prepare the patient | 9 | |||||||
| Aseptic applications | 9 | 9 | 9 | 9 | 9 | |||
| Injection/Vaccination | 5 | 5 | 5 | 5 | 5 | |||
| Positioning I | 11 | 11 | 11 | |||||
| Positioning II | 11 | |||||||
| Positioning III | 11 | |||||||
| REBA AVERAGE | 6,92 | 10,00 | 6.08 | 5.50 | 6.21 | 5.00 | 5.80 | 6.00 |
Table 7 shows the RULA scores of the jobs being done at eight workstations and the RULA average scores of the workstations.
Table 7.
RULA score values of jobs done at workstations.
| Workstations | Service | Operating room | Emergency room | Policlinic | Intensive care | Desk jobs | Lab | İnvazive tredmant |
|---|---|---|---|---|---|---|---|---|
| The work done | RULA | RULA | RULA | RULA | RULA | RULA | RULA | RULA |
| Desk job | 5 | 5 | 5 | 5 | 5 | 5 | 5 | |
| Nasogastric catheter | 4 | 4 | ||||||
| Body temperature measurement | 3 | 3 | 3 | 3 | ||||
| Blood pressure measurement | 6 | 6 | 6 | 6 | 6 | |||
| Vascular access | 4 | 4 | 4 | 4 | 4 | |||
| Serum insertion | 5 | 5 | 5 | 5 | ||||
| Preparation of hemafiltration solution | 7 | |||||||
| Installing hemafiltration solution | 7 | |||||||
| Sterile nurse (Operating room) | 7 | |||||||
| Circulating nurse (Operating room) | 7 | |||||||
| Monitoring or EKG process | 6 | 6 | 6 | 6 | 6 | |||
| Aspiration, Oxygen support therapy | 6 | 6 | 6 | |||||
| Postural drainage | 7 | 7 | 7 | |||||
| Prepare the patient for examination | 7 | |||||||
| Aseptic applications | 7 | 7 | 7 | 7 | 7 | |||
| Injection/Vaccination administration | 4 | 4 | 4 | 4 | 4 | |||
| Positioning I (Turning the patient) | 7 | 7 | 7 | |||||
| Positioning II (sitting position) | 7 | |||||||
| Positioning III (raising the patient) | 7 | |||||||
| REBA AVERAGE | 5.69 | 7.00 | 5.33 | 5.16 | 5.57 | 5.00 | 5.20 | 5.40 |
Table 8 shows the REBA scores and musculoskeletal pain rates of the works performed at eight workstations.
Table 8.
Musculoskeletal complaints and REBA values in departments studied in the last 12 months.
| Workstation | Nurse working at workstation (n) | In the last 12 months in musculoskeletal systems those who complain | Hospital workstations REBA average scores** | Reference REBA score | REBA degree | REBA precaution | |
|---|---|---|---|---|---|---|---|
| n | %* | ||||||
| Service | 180 | 166 | 92.22 | 6.92 | 4–7 | Middle | interventional treatment |
| Operating room | 45 | 44 | 97.77 | 10.00 | 8–10 | High | Needed in a short time |
| Emergency | 16 | 16 | 100 | 6.08 | 4–7 | Middle | Necessary |
| Policlinic | 24 | 18 | 75 | 5.50 | 4–7 | Middle | Necessary |
| Intensive care | 70 | 66 | 94.28 | 6.21 | 4–7 | Middle | Necessary |
| Desk job | 16 | 15 | 93.75 | 5.00 | 4–7 | Middle | Necessary |
| Lab | 20 | 19 | 95 | 5.80 | 4–7 | Middle | Necessary |
| İnterventional treatment | 12 | 11 | 91.66 | 6.00 | 4–7 | Middle | Necessary |
| Total | 383 | 355 | 92.46 | 6.43**/6.86*** | |||
*Row percentage.
**REBA Hospital average score.
***REBA Hospital weighted average score.
In addition, the REBA hospital average score and REBA hospital weighted average score are given.
As seen in Table 8, the risk scores of REBA scores are “high” at 10.00 in operating theaters and “moderate” (4–7) in all other stations. At the same time, the rate of musculoskeletal pain among nurses working in the operating room in the last year was 97.77%.
Table 9 shows the RULA scores and musculoskeletal pain rates of the works performed at eight workstations. In addition, the RULA hospital average score and RULA hospital weighted average score are given.
Table 9.
Musculoskeletal complaints and RULA values at workstations worked in the last 12 months.
| Workstation | Nurse working at workstation (n) | In the last 12 months in musculoskeletal systems those who complain | RULA avg. score | RULA precaution | |
|---|---|---|---|---|---|
| n | %* | ||||
| Service | 180 | 166 | 92.22 | 5.69 | The work should be reviewed and changes made quickly |
| Operating room | 45 | 44 | 97.77 | 7.00 | Change must be made urgently |
| Emergency | 16 | 16 | 100 | 5.33 | The work should be reviewed and changes made quickly |
| Policlinic | 24 | 18 | 75 | 5.16 | The work should be reviewed and changes made quickly |
| Intensive care | 70 | 66 | 94.28 | 5.57 | The work should be reviewed and changes made quickly |
| Desk job | 16 | 15 | 93.75 | 5.00 | The work must be examined and changes made quickly. |
| Lab | 20 | 19 | 95 | 5.20 | The work should be reviewed and changes made quickly |
| İnterventional treatment | 12 | 11 | 91.66 | 5.40 | The work should be reviewed and changes made quickly |
| Total | 383 | 355 | 92.46 | 5.54**/5.71*** | |
*Row percentage.
**RULA Hospital average score.
***RULA Hospital weighted average score.
As seen in Table 9, the risk scores of RULA scores were “high” 7.00 in operating theaters and one level below this in all other stations. At the same time, the rate of musculoskeletal pain among nurses working in the operating room in the last year was 97.77%.
Discussion
Questionnaire forms should not be considered sufficient on their own due to the subjectivity of individuals. In a study, it was recommended to use a specific observation method in technical comparisons in measuring postural risks, and in turn to use it as a useful guide to precisely measure these postural stresses in the industry. 28 More accurate results can be obtained by applying different measurement-based techniques. In this direction, our aim in determining the risks of working postures in nurses working in the health sector is to reach more objective results and make more realistic arrangements by including REBA and RULA measurement methods, which are ergonomic risk assessment methods used in engineering fields, in addition to survey application.
In this study, BMI averages and distributions were analyzed. When the BMI distribution was examined in detail, it was seen that 3% of the nurses were underweight (BMI <18.50) and 11% were obese. The total distribution of these two groups is 14% and it can be considered that these two groups are at risk for musculoskeletal disorders and may have problems. In an article published in 2007, it was reported that patients with a BMI of 35 and above have many health problems in addition to pain complaints. 1 Another study showed that patients with high BMI also have a high rate of pain. 29 Again, the rate of health research in Turkey was found to be 21.1% among obese subjects in 2019. 30 When we look at the responses of the nurses in this study, we see that 92.46% of them have experienced musculoskeletal disorders in the last year. In an article published in 2020, it was stated that the most common musculoskeletal system complaints in working health professionals were in the lower back, back and leg regions. 31 Another article published in 2018 stated that the most common body parts that felt pain in intensive care nurses were the lower back in 88.3% and the back in 77.5%. 32 In this study, 87.50% of the nurses working in the emergency department had lower back pain and 93.75% had back pain. In the intensive care workstation, 90.91% had lower back pain and 81.22% had back pain. Nurses on the service have a higher risk of experiencing back pain than desk workers. Additionally, nurses working in outpatient clinics were 4.31 times more likely to experience back pain than those working at a desk. It can be thought that this situation can be explained by the fact that the tasks performed at the stations, such as supporting patients’ daily life activities and self-care practices, are more intense than other tasks.
In this study, the REBA hospital weighted mean score was 6.86 and the overall mean score was 6.43. When we compare the REBA average of these values according to the reference template, it is understood that it is in the range of (4–7). Again, it is seen that the risk level of this score is “medium” and that it is necessary to make changes as a precaution. This risk score in the REBA method and the level of precautions to be taken suggest that the high rate of nurses (92.46%) who stated that they had musculoskeletal disorders in the last year supports each other.
In terms of the department/station, the three highest REBA scores were found in the operating room (10.0), ward (6.92) and intensive care unit (6.21). As a result of REBA measurement in a group of operating room nurses in Tabriz in 2016, a risk score of 7.7 was found. 33 This risk level is close to the operating room risk level (10:high) in the study.
The nurses were asked about their musculoskeletal complaints such as pain, tingling and numbness. In the last year according to the departments they worked in, and the rates of nurses who said they had complaints according to the department they worked in were compared with the REBA scores in the departments they worked in. Accordingly, 97.77% of the operating room staff reported that they had such complaints in at least one region of the musculoskeletal system in the last year. Again, the REBA analysis score of the ward department, where 92.22% of the nurses working in the ward had musculoskeletal complaints in the last year, was 6.92 and the REBA score was in the range of 4–7; that is, it is clear that action is required in accordance with the definition of the precautionary situation as having a “moderate” risk level and that both the rate of responses to the questionnaire and the scores of the REBA method support each other. The rate of nurses working in intensive care, one of the departments with the third highest REBA score, experiencing the same complaints in the same time period is 94.28%. The result (6.21) determined when evaluated with the REBA technique for intensive care is also supportive of each other. For the rest of the working departments, the rate of complaints in the last twelve months does not fall below 75%. The REBA scores are also in the range of 4–7, which is considered moderate and it is necessary to make arrangements. In a public ambulance in Malaysia, they identified seven activities performed by employees and determined the risk levels for each of them with the REBA method. In the study, three activities were identified before the ambulance and their REBA scores were 4–7 “medium” risk and 8 “high” risk. Four activities were identified inside the ambulance and their scores were 4–6 “medium” risk and 10 “high” risk. Ambulance workers concluded that three of the seven defined activities were high risk. 34 In another study, the body risks of nurses working in five different intensive care units of a state hospital were determined by the REBA method and scores in the range of 5–13 were obtained. It was reported that 63.3% of these risks were high risk. In this study, it was emphasized that 11 procedures were performed in the intensive care unit and 6 procedures had high risk values in REBA score. 12 In the study, 14 procedures were identified in the intensive care unit and 3 of them were found to have high risk scores. Again, in this study, moderate risk was determined in all but one location. In another similar study, 52.9% had moderate, 17.6% had high and 5.8% had very high risk scores in body posture evaluations of laboratory workers (specialist physicians, nurses, technicians, data processing personnel and cleaning personnel) with REBA method. 35 It can be considered that the studies have similar results because even if they are two different hospitals, it is natural that the results will be similar because the working sector is in the field of health and the work performed is similar. The effects of these similar risks on individuals may be different according to working hours, shifts and demographic characteristics.
If we consider the RULA method, it is actually the starting point of the REBA method. This method is designed to evaluate workers who are exposed to musculoskeletal stresses that cause upper limb (neck-shoulder-upper arm-lower arm-elbow-hand-wrist) complaints. 36 Although it works with similar principles to the REBA method in terms of logic, there are differences. The scoring range is between 1 and 7 and there are four impact-consequence levels.
In this study, the RULA hospital weighted average score was 5.71 and the overall average score was 5.54. When we compare these scores with the RULA average according to the reference template, it is understood that it is close to the 5–6 range. Thus, according to the impact level, it is concluded that “the work should be reviewed soon and changes should be made in the short term.” In a study examining the effects of hospital equipment on the posture of healthcare workers, researchers found that the RULA scores of physicians, surgeons and laboratory workers performing extremity examinations were 6. 37 These scores are similar to the scores in the study.
This risk score in the RULA method and the level of precautions to be taken suggest that the high rate of nurses (92.46%) who stated that they had musculoskeletal disorders in the last year support each other.
When analyzed in terms of the department/station, the three highest RULA scores were found to be 7 in the operating room, 5.69 in the ward and 5.57 in the intensive care unit. In our study, it was determined that the average RULA scores in other departments were all higher than 5. When the RULA scores of the other locations in the sections under review are assessed in the RULA reference template, the risk score is in the range 5–6, that is, impact level 3 should be applied (the work should be reviewed immediately and changes made in the short term). There is a high risk level according to the operating room score (7), and it is understood that the equivalent of this score as a measure according to the RULA reference template requires action. In this case, “It is necessary to urgently review the work and make changes.” The nurses were asked about their musculoskeletal complaints such as pain, tingling and numbness. In the last year according to the departments they worked in, and the rates of nurses who said they had complaints according to the department they worked in were compared with the RULA scores in the departments they worked in. Accordingly, 97.77% of the operating room nurses reported that they had such complaints in at least one region of the musculoskeletal system in the last year. Again, when we look at the RULA score (7) of the nurses working in the operating room (RULA score range of 7 and above), it is understood that it is at a high level and there is a need to implement the definition of “urgently, the work done should be reviewed and changes should be made,” which corresponds to this score, which includes corrective actions to reduce risks in the ward. Again, the musculoskeletal complaints of the nurses working in the ward in the last year were 92.22% the RULA analysis score of the ward was 5.69 and the RULA score was in the 5–6 score range, which means that the precautionary situation with a moderate risk level should be carried out in accordance with the definition of “the work should be reviewed soon and changes should be made in the short term” and it is clear that both the rate of responses to the questionnaire and the scores of the RULA method support each other. In 2010, a RULA risk assessment was performed on a section of nurses working in the ward at a state university and they reached a score of 7, which is one level higher than the score of 5.69 found in our ward. 28 The scores in our study and in this study show that both risks require some ergonomic changes to be made, but measures to improve the body risks of nurses, which are the subject of this review in the literature, should be done “urgently.” In other words, unlike in this study, the change needs to be realized in a shorter period of time. The rate of nurses working in intensive care, one of the departments with the third highest RULA score in our study, experiencing the same complaints in the same time period is 94.28%. When evaluated with two different techniques for intensive care, it is seen that both results support each other again.
RULA scores were also found to be in the range of 5–6 and it is seen that it is necessary to make a regulation as “the work should be reviewed soon and changes should be made in the short term.” In a risk assessment analysis conducted on the working postures of dentists in Konya in 2016, RULA scores were found to be 6, that is, a moderate risk at rates similar to our study, and it was stated that the work should be reviewed ergonomically and changes should be made. 38
In the survey application, it is understood that the rates of nurses who stated that they had musculoskeletal disorders in the last year and the results of the analysis using the RULA method confirm each other. However, the average scores of the body risk analysis using the RULA method fall within the definition of a medium-level evaluation in all departments except the operating room, and it is seen that this level will definitely cause musculoskeletal disorders and that it is necessary to make arrangements, but when making general evaluations and comments, the existence of an upper level, which falls within the definition of the fourth impact level risk in the RULA reference table in the score range of 7 and above, and which is in the precautionary level of “urgently, the work should be reviewed and changes should be made” should not be ignored.
In a study published in 2022 in which nurses’ posture risk was calculated using the RULA method, 10% of subjects were at low risk, while 44% and 46% were at high and medium risk, respectively, of developing musculoskeletal disorders. 39
In a 2023 posture risk study of surgeons, the average RULA was 6.09 (4–7). 40
This similarity of evaluation is natural because REBA is derived from the RULA method. The REBA and RULA methods, which showed similar evaluations in our study, also show high risks in some studies and do not give completely healthy results. 41
Fifty-nine percent of ergonomics experts recommend RULA and REBA analysis methods rather than other analysis methods. 42
Limitations of the study
In addition, since the research was conducted in a hospital with very intensive patient services, no pictures could be taken from all nurses. REBA and RULA score calculations were made by taking pictures from a total of 24 nurses, 3 from each workstation. In this case, we could not calculate REBA and RULA scores from every nurse we surveyed, and we could not make logistic regression comparisons. This was the most important limitation of the study.
Another disadvantage was the time-consuming nature of data collection by observation and questionnaires, and the fact that health care delivery is a time-competitive task. It is well known that nurses carry out their critical tasks in an environment where they have to be carried out rapidly and without hesitation as a whole.
Conclusions
As a result, the literature on this subject was examined and it was understood that the musculoskeletal complaints of the nurses were seen at levels that we can characterize as high, that is, above the medium values in both the survey results and the REBA and RULA score results.
It is seen that this study and the literature reviewed have similar results. The subjectivity of the data in surveys can affect the reliability of the results. Therefore, it is recommended that posture risks be measured at regular intervals not only by survey method but also by systematic observation methods in order to be cheap and objective. Although NIOSH, OWAS, etc. measurement methods are among the systematic observation methods, REBA and RULA methods have recently been preferred in the field of health due to their suitability.
In addition, after measurement determinations, ergonomic improvements and training should be organized for nurses, and working and shift hours should be updated. The necessary number of rest breaks must be arranged and a sufficient number of nurses must be employed.
The study is considered to be useful and further studies on this subject are recommended.
Acknowledgment
We would like to thank Istanbul University, Istanbul Faculty of Medicine and Istanbul University Health Sciences Institute for their permission to publish the findings. We would also like to thank the nurse team who participated in this study.
Author biographies
Özkan AYVAZ, he holds a PhD in Public Health. His research area is Occupational Health and Safety, Environmental Health.
Bedia Ayhan Özyıldırım, he is a Professor of Public Health. His research area is occupational health, employee health and occupational diseases, as well as health management.
Halim İşsever, he is a Professor of Public Health. His research area is occupational health and safety.
Gözde Öztan, he holds a PhD in molecular biology and medical genetics. His research area is medical genetics and molecular biology.
Muhammed Atak, he holds a PhD in Public Health. His research area is Occupational Health and Safety, Environmental health and other public health areas.
Sevda Özel, he holds a PhD in Biostatistics. His research area is making biostatistical calculations and inferences using various research methods in health.
Footnotes
Authors’ note: Description of the roles played by each author in the content of the article: Özkan Ayvaz is the first author of the article; Bedia Ayhan Özyıldırım was involved in study design consultant; Halim İşsever was involved in data analysis; Gözde Öztan was the study design consultant; Muhammed Atak was involved in literature and article draft; Sevda Özel was involved in data analysis.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Özkan Ayvaz https://orcid.org/0000-0002-2675-4439
Halim İşsever https://orcid.org/0000-0002-5435-706X
Gözde Öztan https://orcid.org/0000-0002-2970-1834
References
- 1.Cımbız A, Uzgören N, Aras Ö, et al. Kas İskelet Sisteminde Ağrıya ait Risk Faktörlerinin Lojistik Regresyon Analizi ile Belirlenmesi: pilot çalışma. Fizyoterapi Rehabilitasyon 2007; 18: 20–27. [Google Scholar]
- 2.Dilek B, Korkmaz F, Baş G, et al. Bir Üniversite Hastanesinde Çalışan Hekimlerde Kas İskelet Sistemi Problemleri ve Yaşam Kalitesinin Değerlendirilmesi. Dokuz Eylül Üniversitesi Tıp Fakültesi Dergisi 2016; 30: 25–30. [Google Scholar]
- 3.U.S. Bureau of Labor Statistics. Survey of occupational injuries and illnesses data 2020, https://www.bls.gov/iif/soii-data.htm.
- 4.Doğrul Z, Mazican N, Turk M. The prevalence of work-related muskuloskeletal disorders (WRMSDs) and related factors among occupational disease clinic patients. Int Arch Public Heal Community Med 2019; 3: 030. [Google Scholar]
- 5.WHO. Musculoskeletal Health, https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions (2023, accessed 11 May 2023).
- 6.2019 Avrupa. Work-related MSDs: prevalence, costs and demographics in the EU, European Risk Observatory Executive summary, European Agency for Safety and Health at Work, 2019; p. 13.
- 7.Lang J, Ochsmann E, Kraus T, et al. Psychosocial work stressors as antecedents of musculoskeletal problems: a systematic review and meta-analysis of stability-adjusted longitudinal studies. Soc Sci Med 2012; 75: 1163–1174. [DOI] [PubMed] [Google Scholar]
- 8.Aydın İ, Çelik Y, Uğuroğlu Ö. Sağlık personeli çalışma yaşam kalitesi ölçeği: geliştirilmesi, geçerliliği ve güvenilirliği. Toplum ve Sosyal Hizmet 2011; 22: 79–100. [Google Scholar]
- 9.Esen H, Fığlalı N. Çalışma duruşu analiz yöntemleri ve çalışma duruşunun kas-iskelet sistemi rahatsızlıklarına etkileri. SAÜ Fen Bilimleri Enstitüsü Dergisi 2013; 17: 41–51. [Google Scholar]
- 10.Felekoğlu B, Taşan SÖ. İş ile ilgili kas iskelet sistemi rahatsızlıklarına yönelik ergonomik risk değerlendirme: Reaktif/proaktif bütünleşik bir sistematik yaklaşım. J Fac Eng Arch Gazi Univ 2017; 32: 777–793. [Google Scholar]
- 11.Erçelik Z. Ergonomik Risk Analizinin Lastik İmalat Fabrikasında Uygulanması (tez). Kocaeli: Kocaeli Üniversitesi Fen Bilimleri Enstitüsü, 2017. [Google Scholar]
- 12.Kahya E, Gülbandılar S, Gürleyen E. Nöroloji Yoğun Bakım Ünitesinde Çalışan Hemşirelerin Maruz Kaldığı Fiziksel Zorlanmaların Analizi. Ergonomi 2018; 1: 39–48. [Google Scholar]
- 13.Mert EA. Ergonomik Risk Değerlendirme Yöntemlerinin Karşılaştırılması Ve Bir Çanta İmalat Atölyesinde Uygulanması (tez). Ankara: TC Çalışma ve Sosyal Güvenlik Bakanlığı İş Sağlığı ve Güvenliği Genel Müdürlüğü, 2014. [Google Scholar]
- 14.Stanton NA, Hedge A, Brookhuis K, et al. Handbook of human factors and ergonomics methods. Boca Raton, FL: CRC Press, 2004. [Google Scholar]
- 15.Hignett S, McAtamney L. Rapid entire body assessment (REBA). Appl Ergon 2000; 31: 201–205. [DOI] [PubMed] [Google Scholar]
- 16.Tee KS, Low E, Saim H, et al. A study on the ergonomic assessment in the workplace 2017; AIP Conference Proceedings 1883, 020034-1, 020034-11.
- 17.McAtamney L, Nigel Corlett E. RULA: a survey method for the İnvestigation of work-related upper limb disorders. Appl Ergon 1993; 24: 91–99. [DOI] [PubMed] [Google Scholar]
- 18.Khandan M, Vosoughi S, Poursadeghiyan M, et al. Research paper: ergonomic assesment of posture risk factors among Iranian workers: an alternative to conventional methods. Iran Rehab J 2017; 16: 11–16. [Google Scholar]
- 19.Hashim A, Dawal SZ, Yusoff N. Ergonomic evaluation of postural stress in school workshop. Work 2012; 41: 827–831. [DOI] [PubMed] [Google Scholar]
- 20.Muslim B, Devira S, Seno BA, et al. Hubungan Durasi Kerja dan Postur Tubuh dengan Keluhan Low Back Pain (Lbp) Penjahit di Nagari Simpang Kapuak Kabupaten Lima Puluh Kota. J Sehat Mandiri 2021; 16: 138–146. [Google Scholar]
- 21.Engka AA, Sumampouw OJ, Kaunang W. Postur Kerja dan Keluhan Muskuloskeletal pada Nelayan di Desa Borgo Satu Kecamatan Belang. KESMAS 2022; 11: 44–51. [Google Scholar]
- 22.Jeong S, Kook J. CREBAS: computer-based REBA evaluation system for wood manufacturers using MediaPipe. Appl Sci 2023; 13: 938. [Google Scholar]
- 23.Erdinç O, Hot K, Ozkaya M. Turkish version of the Cornell Musculoskeletal Discomfort Questionnaire: cross-cultural adaptation and validation. Work 2011; 39: 251–260. [DOI] [PubMed] [Google Scholar]
- 24.Yıldız T, Onler E. Hastane Ergonomik Koşullarının Hemşirelerin Mesleki Kas İskelet Sistemi Rahatsızlıkları Üzerine Etkisi. Scientif Sci 2015; 3: 1–7. [Google Scholar]
- 25.Edlich RF, Winters KL, Hudson MA, et al. Prevention of disabling back injuries in nurses by the use of mechanical patient lift systems. J Long Term Eff Med Implants 2004; 14: 521–533. [DOI] [PubMed] [Google Scholar]
- 26.Şirzai H, Doğu B, Erdem P, et al. Hastane Çalışanlarında İşe Bağlı Kas İskelet Sistemi Hastalıkları: üst Ekstremite Problemleri. Şişli Etfal Hastanesi Tıp Bülteni 2015; 49: 135–141. [Google Scholar]
- 27.Aksakoğlu G. Sağlıkta Araştırma Teknikleri ve Analiz Yöntemleri, Dokuz Eylül Üniversitesi Yayın Komisyonu. İzmir, 2001.
- 28.Ithnin A, Kong D, Venkataraman S. Occupational risk factors for carpal tunnel syndrome among nurses in medical. Int J Public Health Res 2012; 2: 137–143. [Google Scholar]
- 29.Gül A, Üstündağ H, Kahraman B, et al. Hemşirelerde Kas İskelet Ağrılarının Değerlendirilmesi. Sağlık Bilimleri ve Meslekleri Dergisi 2015; 1: 1–10. [Google Scholar]
- 30.TÜİK. Türkiye Sağlık Araştırması 2019, https://data.tuik.gov.tr/Bulten/Index?p=Turkiye-Saglik-Arastirmasi-2019-33661.
- 31.Ülgüdür C, Dedeli Caydam Ö. Assessment of ergonomıcs and musculoskeletal system disorders ın health professıonals. Izmır Democr Unıv Health Scı J ıduhes 2020; 3: 8–37. [Google Scholar]
- 32.Çelik S, Taşdemir N, Öksüzoǧlu A, et al. Critical-care nurses’ pain experiences and the prognostic factors. Dimens Crit Care Nurs 2018; 37: 3–11. [DOI] [PubMed] [Google Scholar]
- 33.Abdollahzade F, Mohammadi F, Dianat I, et al. Working posture and its predictors in operating room nurses. Health Promot Perspect 2016; 6: 17–22, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4847110/ . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Deros BM, Daruıs DDI, Thiruchelvam S. Evaluation on ambulance design and musculoskeletal disorders risk factors among ambulance emergency medical service personnel. Iran J Public Health 2016; 45: 52–60. [Google Scholar]
- 35.Atasoy A, Keskin F, Başkesen Net al. et al. Laboratuvar Çalışanlarında İşe Bağlı Kas- İskelet Sistemi Sorunları ve Ergonomik Risklerin Değerlendirilmesi. Sağlıkta Performans ve Kalite Dergisi 2010; 2: 90–113. [Google Scholar]
- 36.Hoy J, Mubarak N, Nelson S, et al. Whole body vibration and posture as risk factors for low back pain among forklift truck drivers. J Sound Vib 2005; 284: 933–946. [Google Scholar]
- 37.Alp E, Bozkurt M, Başçiftçi İ. Hastane Malzemelerinin Sağlık Çalışanlarının Postürüne Etkileri. SAÜ Fen Bilimleri Enstitüsü Dergisi 2012; 16: 221–226. [Google Scholar]
- 38.Karabacak N, Peker A. An ergonomic study on dentists working posture invfaculty of dentistry in konya. J Selçuk Univ Nat Appl Sci 2016; 5: 1–14. [Google Scholar]
- 39.Kothari V, Mahajan P, Shinde Met al. et al. Evaluation of risk of musculoskeletal diorder using RULA and REBA ergonomic assessment among nursing professionals a cross sectional study vihaa nimit kothari, SSRN Product & Services 2022: 11.
- 40.Monagle N, Eberle L, Dyche T, et al. Ergonomic assessment of surgical residents using the rapid upper limb and rapid entire body assessments. Arch Phys Med Rehabil 2023; 104: 27.35926570 [Google Scholar]
- 41.Kong K, Yong Lee Y, Suk Lee S, et al. Comparisons of ergonomic evaluation tools (ALLA, RULA, REBA and OWAS) for farm work. Int J Occup Saf Ergon 2018; 24: 218–223. [DOI] [PubMed] [Google Scholar]
- 42.Pascual SA, Naqvi S. An İnvestigation of ergonomics analysis tools used in industry in the identification of work-ralated musculoskeletal disorders. Int J Occup Saf Ergon 2008; 14: 237–245. [DOI] [PubMed] [Google Scholar]