Abstract
The purpose of this study was to evaluate characteristics of reinjury following forearm fractures in adolescents. An Institutional Review Board-approved retrospective cohort study of forearm fractures (ages 10–18 years) treated by a single academic pediatric orthopaedic group from June 2009 to May 2020 was conducted. All both bone forearm (BBFA) and radius or ulna primary and secondary injuries were included. We excluded open, surgically treated, physeal, epiphyseal, and radial head/neck fractures. Demographics, injury characteristics, and radiographic data were recorded. We evaluated associations of ipsilateral same-site refracture (RE-FRACTURE) versus ipsilateral or contralateral different-site forearm fractures occurring as secondary later injuries (OTHER). Thirty-three of 719 patients sustained a secondary forearm fracture (4.6%; mean age, 11.5 years; M:F, 5.6:1). RE-FRACTURES, compared with OTHER forearm locations, were associated with a sports mechanism at time of original injury (P = 0.024) and mid-shaft position of fracture on the radius (77.6 vs. 29.8 mm from distal physis; P < 0.001) and ulna (72.0 vs. 27.2 mm from distal physis; P = 0.003). RE-FRACTURES also demonstrated increased radius to ulna distance between BBFA primary injury sites on anteroposterior (19.6 vs. 10.6 mm; P = 0.009) and lateral radiographs (19.6 vs. 10.5 mm; P = 0.020) compared with OTHER forearm locations. Residual angulation and fracture-line visibility were not significantly associated with secondary fracture. Ipsilateral same-site refractures tend to occur in adolescents within 1 year following treatment for widely spaced (>15 mm) and mid-shaft forearm fractures incurred during athletic activity. Further research may be warranted to evaluate biologic, bone health, or personality traits that may lead to secondary fractures of the pediatric forearm.
Keywords: adolescent athletes, forearm refracture, radius, reinjuries, sports, ulna
Introduction
The forearm and wrist are the most common sites of fracture in the pediatric population and among pediatric athletes [1–4]. Both bone forearm (BBFA) fractures, or diaphyseal fractures of the radius and ulna, comprise 3–15% of all pediatric fractures [2,4] and are most commonly due to falls and sporting activities [1–3].
The forearm and wrist are also the most common sites of refracture in the pediatric population [5]. Although most forearm fractures undergo rapid healing after closed treatment [6], there has been an increased reporting of forearm refracture over the past several decades [1,2]. Mid-shaft fractures are reported to refracture more often than fractures of the distal forearm [7,8], and diaphyseal BBFA fractures in particular have refracture rates of up to 15% – nearly twice that of all forearm refractures (1.4–8%) [5,9–11]. The literature suggests that forearm refractures tend to occur within 6 months after primary fracture [7–9,12–14], and previously cited characteristics associated with refracture include incomplete fracture remodeling [7–9,14], early cast removal [7], and residual angulation [7–9,15].
Children ages 10 and older are at highest risk of a secondary injury following treatment of BBFA fractures with closed reduction and casting [16,17]. While the relationship between pediatric sports involvement and reinjury has been established for common injuries such as anterior cruciate ligament tears and concussions [18–20], despite the common occurrence of forearm and wrist injuries, no prior studies have explored the association between secondary injury following forearm fractures and sports.
Identifying trends and risk factors related to secondary forearm fracture in the adolescent population can aid in modifying treatment guidelines and developing sport-based recommendations. The purpose of this study was to evaluate clinical and radiographic characteristics associated with secondary forearm fracture following prior forearm injury in the adolescent age group.
Methods
We conducted an institutional review board-approved retrospective cohort study of all forearm fractures based on current procedural terminology and international classification of disease-9/10 codes treated by a single academic pediatric orthopaedic group from June 2009 to May 2020.
We included children of ages 10–18 years with single bone (radius or ulna) or both bone primary or secondary fractures. There were no limitations regarding time to secondary injury. We excluded fractures without X-rays and those that were open, surgically treated with open reduction, or associated with the physis (Salter-Harris), epiphysis, radial head or radial neck. Thirty-three secondary fractures and 686 primary fractures (Fig. 1) remained for analysis. We compared clinical and radiographic characteristics between ipsilateral same-site secondary fractures (RE-FRACTURE) and ipsilateral or contralateral nonidentical site fractures (OTHER).
Fig. 1.
Application of inclusion and exclusion criteria. A total of 3170 forearm fractures were identified. A total of 2451 were excluded and 719 remained, resulting in a total of 33 secondary fractures for analysis.
Variables
Demographic information such as age, sex, and hand dominance was recorded. Type of primary and secondary fractures was classified as BBFA or radius only – the latter included isolated radial fractures or those with a concomitant ulnar styloid process fracture. There were no isolated ulna fractures.
Date of primary injury, laterality, and mechanism of injury for both primary and secondary fractures were recorded. Mechanism of injury was classified as contact sports, tumbling, fall, playground accident, trampoline, other, or unknown. Sport played at time of injury was documented. Injuries incurred while participating in an organized sport were defined as athletic injuries, whereas all others were designated as nonathletic. We documented length of immobilization, return to activity as determined by the clinician, and time to secondary injury. All timeframes were measured from date of primary injury.
Location of primary fracture was determined radiographically. ‘Diaphyseal’ or ‘metaphyseal’ was classified according to the Arbeitsgemeinschaft für Osteosynthesefragen (AO) Pediatric Comprehensive Classification of Long-Bone Fractures[21] on anteroposterior (AP) radiographs (Fig. 2). Position of primary fracture on radius or ulna was measured on AP and lateral radiographs as distance in millimeters from distal physis to the nearest fractured cortex (Fig. 3). Location as percentage was calculated by dividing position of primary fracture on bone by total length of radius or ulna. The latter was measured on the patient’s first postreduction AP radiograph from the center of the distal radial or ulnar physis to the articular surface of the radial head or most distal portion of ossified ulnar bone.
Fig. 2.
Determining location of primary fracture with the AO pediatric comprehensive classification of long-bone fractures. A line is drawn through the ulnar and radial physes on anteroposterior radiographs of primary injury, and a square is created utilizing this line as one of the square’s edges. Fractures located within the square are metaphyseal (a), and fractures located outside the square are diaphyseal (b).
Fig. 3.
Measuring position of primary fractures and distance between radius and ulna fractures. A line is drawn from the center of the distal physis parallel and proximal to the fracture to determine position of primary fracture on radius and ulna (a). The most distal aspect of the fracture was used to maintain consistency with oblique fracture. To measure distance between radius and ulna fractures, a line is drawn from the proximal aspect of the ulnar fracture parallel to the radius, terminating at the proximal radial fracture (b). The most proximal aspects of the fractures were used to maintain consistency with oblique fracture.
For BBFA fractures, distance between radius and ulna fractures (mm) was measured on AP and lateral radiographs (Fig. 3). Degree of angulation for primary and secondary injuries was documented on AP and lateral radiographs at time of initial injury, after reduction, and at latest follow-up. Angulation was determined by drawing one line from the center of the shaft (proximal to fracture site and distal to radial tuberosity or olecranon) to the center of the fracture site; another line was drawn from the center of the fracture site through the center of the distal radial or ulnar physis.
Fracture-line visibility was measured on AP and lateral radiographs at latest follow-up for primary injury. We utilized Baitner et al.’s [8] grading system based on callus formation, fracture-line visibility, and stage of fracture union. ‘Grade 1’ indicated a fracture with massive callus formation and barely discernable fracture line, ‘Grade 2’ indicated moderate bridging callus formation and a discernible line, and ‘Grade 3’ fractures had no bridging callus and a distinct fracture line.
Data analysis
Statistical analysis was conducted using Statistical Package for the Social Sciences (SPSS). Chi-square test, Fisher’s exact test, student’s t-test, and Mann–Whitney U test were conducted to determine statistically significant differences related to demographics, injury characteristics, and radiographic features between RE-FRACTURE (ipsilateral same-site secondary fractures) and OTHER forearm locations (ipsilateral or contralateral nonidentical site fractures). Additional analyses were conducted to compare groups based on location of primary fracture as determined by AO Pediatric guidelines (diaphysis and metaphysis). Statistical significance was set at P = 0.05.
Results
Between 2009 and 2020, there were 719 patients with forearm fractures. A total of 4.6% (33) sustained a secondary fracture. Mean age among secondary fractures was 11.48 ± 1.42 years with a male to female ratio of 5.6:1. A total of 94% of primary fractures occurred in patients between the ages of 10 and 13, and 61% of primary fractures occurred on the left arm. Average time to secondary fracture for the entire cohort was 1.4 ± 1.4 years.
Sixteen of 33 secondary fractures occurred at the same site as the original fracture (RE-FRACTURE), whereas 17 occurred at a different site (OTHER). A total of 87.5% of RE-FRACTURES occurred within 1 year. The average time to secondary fracture in same-site RE-FRACTURES was 8 ± 7 months; OTHER forearm locations’ secondary fracture time was 2.1 ± 1.5 years. The timeframe difference between RE-FRACTURE and OTHER forearm locations was statistically significant (P = 0.002) (Fig. 4).
Fig. 4.
Time to secondary fracture: RE-FRACTURE versus OTHER. Ipsilateral same-site secondary fractures have an earlier time to secondary fracture than ipsilateral and contralateral different-site secondary fractures. This finding was statistically significant (P = 0.002).
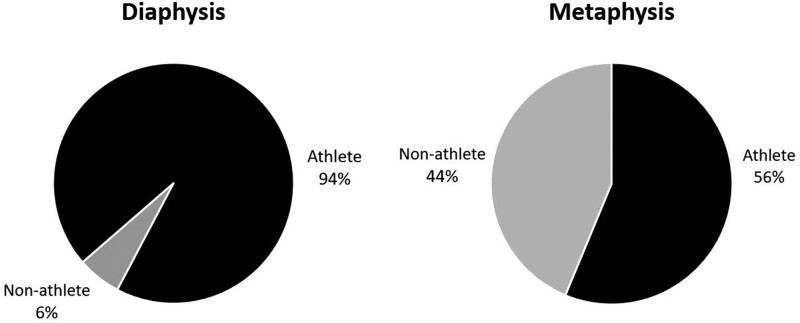
Sports were the most common mechanism of injury of both primary and secondary fractures, followed by falls (Table 1). A total of 71.4% of RE-FRACTURES were significantly associated with a sport played at time of primary fracture compared with OTHER forearm locations (P = 0.024). Soccer (35.7% vs. 5.3%) and tumbling (21.4% vs. 5.3%) were associated with primary fracture among RE-FRACTURES compared with OTHER forearm locations; basketball (15.8% vs. 0%) was associated with primary fracture among OTHER forearm locations when compared with RE-FRACTURES. Additionally, 94% of primary diaphyseal fractures that sustained refracture occurred in athletes when compared with metaphyseal fractures (P = 0.017) (Fig. 5).
Table 1.
Mechanism of injury: primary versus secondary fracture
| Injury | Sportsa | Fall | Other | Unknown |
|---|---|---|---|---|
| Primary fracture | 17 | 10 | 3 | 3 |
| Secondary fracture | 19 | 11 | 3 | 0 |
Includes contact sports and tumbling.
Fig. 5.
Athlete versus nonathlete status based on fracture location. Nearly all diaphyseal fractures that refractured occurred in athletes. This finding was statistically significant (P = 0.017).
Radiographic position of primary fracture was also statistically significant for a mid-shaft location among RE-FRACTURES on AP and lateral radiographs on both the radius and ulna (77.6 vs. 29.8 mm from distal physis; P < 0.001) (Table 2). Primary diaphyseal fractures, therefore, sustain secondary injury earlier and at the same site, whereas more distal fractures correlate with secondary injury later and at a different site.
Table 2.
Radiographic markers of location of primary fracture
| Fractured bone, radiograph | RE-FRACTURE | OTHER | P-value |
|---|---|---|---|
| Position of primary fracture (mm) | |||
| Radius, AP | 77.6 ± 40.7 (15–128) | 29.8 ± 19.4 (8–80) | < 0.001* |
| Ulna, AP | 72.0 ± 36.9 (11–126) | 27.2 ± 23.4 (6–88) | 0.003* |
| Radius, lateral | 77.1 ± 42.5 (15–126) | 31.9 ± 20.6 (11–80) | 0.001* |
| Ulna, lateral | 74.5 ± 38.2 (10–116) | 29.0 ± 22.5 (9–86) | 0.004* |
| Location as percentage | |||
| Radius, AP | 56.1 ± 18.9 (33.7–85.3) | 82.7 ± 11.0 (59.3–95.4) | 0.001* |
| Ulna, AP | 68.3 ± 15.0 (47.7–94.6) | 86.5 ± 12.0 (60.1–96.2) | 0.012* |
AP, anteroposterior.
*Significant P-value < 0.05.
Further radiographic analysis demonstrated that RE-FRACTURES at the same site were significantly associated with a greater distance between primary radial and ulnar fracture sites compared with OTHER forearm locations (P = 0.009, 0.020) (Table 3). Nine of 16 RE-FRACTURES were BBFA, and eight of these nine demonstrated a fracture site difference greater than 15 mm on AP or lateral radiographs. Residual angulation of primary fracture measured at three different time points (time of injury, postreduction, and latest follow up) had no significant relationship with RE-FRACTURE or OTHER forearm locations.
Table 3.
Distance between radial and ulnar fractures of primary injury
| Radiograph | RE-FRACTURE | OTHER | P-value |
|---|---|---|---|
| Distance between fractures (mm) | |||
| AP | 19.6 ± 5.0 (13–28) | 10.6 ± 8.1 (2–28) | 0.009* |
| Lateral | 19.6 ± 7.4 (7–30) | 10.5 ± 8.0 (2–23) | 0.020* |
| Diaphysis | Metaphysis | P-value | |
|---|---|---|---|
| Distance between fractures (mm) | |||
| AP | 19.7 ± 5.8 (10–28) | 8.6 ± 6.3 (2–21) | 0.001* |
| Lateral | 18.6 ± 8.1 (5–30) | 9.7 ± 7.5 (2–23) | 0.020* |
AP, anteroposterior.
*Significant P-value < 0.05.
Across the entire cohort, primary fractures were immobilized for an average of 1.5 months (47.8 ± 15 days; range, 0–13). Approximately 1.3 cast changes took place, and return to activity occurred after a mean of 2.7 months after primary injury (81.5 ± 21.7 days; range, 39–146). No statistically significant differences existed for these variables between RE-FRACTURE and OTHER forearm locations. Metaphyseal fractures were immobilized for an average of 10 days less than diaphyseal fractures (P = 0.044), and metaphyseal fractures returned to activity 22 days earlier than diaphyseal fractures (P = 0.003). Analysis of radiographic healing based on fracture-line visibility and callus formation demonstrated that fracture line was barely (grade 1) or moderately (grade 2) visible on most patients’ final radiographs. This finding was not statistically significant.
Discussion
Recurrent fractures of the forearm presented in 4.6% of children between the ages of 10 and 18 at a single tertiary children’s hospital. Our secondary fracture percentage falls within the range defined by prior studies (1.4–8%) [5,9–11] despite our exclusion of children younger than 10 years of age. This supports prior literature, suggesting that children ages 10 and older are at highest risk of secondary injury following conservative treatment of BBFA fractures [16,17].
Most pediatric forearm refractures occur within 6 months after primary injury [7–9,12–14]; however, average time to secondary forearm fracture in our cohort was 1.4 years. It is possible that adolescents have increased susceptibility to refracture for an extended period following primary injury compared with their younger counterparts. A combination of increased physical activity, greater calcium demand, and maximal skeletal growth during puberty can lead to a transient deficit in cortical bone mass [22] that may predispose adolescents to reinjury.
Baitner et al. [8] and Bould and Bannister [7] demonstrated that children with diaphyseal fractures are at greater risk of refracture. Our analysis reinforces this finding and further elucidates that adolescents with diaphyseal fractures are more likely to refracture at the same site of primary injury. RE-FRACTURE was significantly associated with a mid-shaft location compared with OTHER forearm locations across three different methods of determining location – AO Pediatric guidelines, radiographic measurement of fracture position on bone, and location as percentage. It is possible that a combination of greater muscular deforming forces surrounding the diaphysis and an increased requirement for callus lead to slower rates of healing [7,8] in the mid-shaft that predisposes to secondary fracture. Knowing that the mid-shaft has greater refracture susceptibility allows providers to utilize location of primary fracture to risk stratify adolescents at increased risk of reinjury.
We identified sports-related risk factors for secondary forearm fractures as well. While previous studies document falls as a leading cause of injury [7,14], sports were the most common mechanism of injury in our cohort. Greater fracture incidence due to sports in adolescents is logical, as this population is less likely to sustain forearm fracture from falls or playground accidents than younger children. In fact, adolescents with secondary fractures at the same site (RE-FRACTURE) were significantly associated with playing sports at time of primary injury. Further analysis revealed that 94% of adolescents with diaphyseal fractures that went on to refracture were athletes. Involvement in sports likely increases the risk of direct forearm impact and high-energy falls, leading to greater risk for recurrent forearm fractures. An athlete with a diaphyseal forearm fracture is, therefore, at greater risk of secondary injury and may benefit from prolonged immobilization and longer duration of rest prior to return to sport.
Radiographic distance between primary radius and ulna fracture sites also demonstrated significant relationships with secondary fracture. RE-FRACTURES and diaphyseal fractures, versus OTHER fracture locations and metaphyseal fractures, were significantly associated with a greater distance on AP and lateral radiographs. This suggests that diaphyseal BBFA fractures that occur greater than 15 mm apart are more likely to refracture at the same site. It is possible that in the initial inflammatory phase of bone healing in BBFA fractures, cytokine release and progenitor cell recruitment at one fracture site may stimulate or assist in the healing of the other fracture site when it is within 15 mm. This is a novel finding that has not been reported by previous pediatric forearm refracture studies. Providers can utilize this radiographic marker to identify those who are at greater risk of forearm refracture and provide closer follow-up after treatment to ensure appropriate healing.
Pediatric forearm refracture literature recommends 6–8 weeks of cast duration [7–9] and return to activity at 3 months when the fracture line tends to disappear [9], suggesting that these time periods allow for adequate bone healing. Our cohort sustained secondary fracture despite being immobilized for an average of 7 weeks and returning to activity after a mean of 3 months. Recommendations derived from studies based on younger pediatric populations may need to be adjusted for adolescents and athletes who are inherently returning to more vigorous activities than younger children.
Finally, the data from this study did not support the hypothesis that incomplete healing is a risk factor for refracture in adolescents. Several studies have demonstrated a trend towards greater risk of refracture with less healing [8,9,14] and suggest that fracture-line visibility can help guide decision-making regarding return to play [23,24]. We also recognize that rates of bone healing may vary depending on levels of bone maturity and growth plate fusion, especially in our cohort ranging from ages 10 to 18. However, 94% of the primary fractures in our cohort occurred in those between the ages of 10 and 13, all of whom are at similar stages of bone development and physeal closure. Although it is important to ensure appropriate fracture consolidation on radiographs, we believe factors such as location of primary fracture on bone and distance between BBFA fracture sites may be more important when determining return to play.
Limitations
We acknowledge the limitations of our study. The main limitation of this retrospective cohort study is the lack of an age-matched comparison group, which prevents us from providing a statistical relative risk for refracture based on clinical and radiographic characteristics. Another limitation of the retrospective review is that we do not have a minimum follow-up on all primary fractures. Therefore, we cannot present a refracture rate for the general adolescent population. Due to the retrospective nature of this study, we could not assess the relationship between vitamin D or calcium deficiencies and reinjury. Additionally, our study involved only a single pediatric academic center. Cultural preferences, geographic factors, and seasonal variation in sports participation may affect our interpretation of sport-related factors associated with secondary fracture of the forearm in adolescent athletes, and the interpretation of our results applies only to this study population. Despite these limitations, we can determine percentage of refracture and identify trends associated with secondary fracture in our study population. These results are useful to guiding the development of future prospective studies that can investigate causative factors of secondary forearm fracture.
Conclusion
Adolescents with primary mid-shaft forearm fractures incurred during athletic activity tend to sustain secondary injuries at the same site within the first year following treatment. We recommend greater caution in adolescent athletes with widely spaced (>15 mm) diaphyseal BBFA fractures. These groups may benefit from prolonged immobilization and longer duration of rest prior to returning to sport. Further research may be warranted to evaluate biologic, bone health, or personality traits that lead to secondary fractures of the pediatric forearm.
Acknowledgements
Conflicts of interest
There are no conflicts of interest.
References
- 1.Landin LA. Fracture patterns in children. Analysis of 8,682 fractures with special reference to incidence, etiology and secular changes in a Swedish urban population 1950-1979. Acta Orthop Scand Suppl 1983; 202:1–109. [PubMed] [Google Scholar]
- 2.Hedström EM, Svensson O, Bergström U, Michno P. Epidemiology of fractures in children and adolescents. Acta Orthop 2010; 81:148–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pannu GS, Herman M. Distal radius-ulna fractures in children. Orthop Clin North Am 2015; 46:235–248. [DOI] [PubMed] [Google Scholar]
- 4.Cheng JC, Ng BK, Ying SY, Lam PK. A 10-year study of the changes in the pattern and treatment of 6,493 fractures. J Pediatr Orthop 1999; 19:344–350. [PubMed] [Google Scholar]
- 5.Landin LA. Epidemiology of children’s fractures. J Pediatr Orthop B 1997; 6:79–83. [DOI] [PubMed] [Google Scholar]
- 6.Zionts LE, Zalavras CG, Gerhardt MB. Closed treatment of displaced diaphyseal both-bone forearm fractures in older children and adolescents. J Pediatr Orthop 2005; 25:507–512. [DOI] [PubMed] [Google Scholar]
- 7.Bould M, Bannister GC. Refractures of the radius and ulna in children. Injury 1999; 30:583–586. [DOI] [PubMed] [Google Scholar]
- 8.Baitner AC, Perry A, Lalonde FD, Bastrom TP, Pawelek J, Newton PO. The healing forearm fracture: a matched comparison of forearm refractures. J Pediatr Orthop 2007; 27:743–747. [DOI] [PubMed] [Google Scholar]
- 9.Tisosky AJ, Werger MM, McPartland TG, Bowe JA. The factors influencing the refracture of pediatric forearms. J Pediatr Orthop 2015; 35:677–681. [DOI] [PubMed] [Google Scholar]
- 10.Litton LO, Adler F. Refracture of the forearm in children: a frequent complication. J Trauma 1963; 3:41–51. [DOI] [PubMed] [Google Scholar]
- 11.Martus JE, Preston RK, Schoenecker JG, Lovejoy SA, Green NE, Mencio GA. Complications and outcomes of diaphyseal forearm fracture intramedullary nailing: a comparison of pediatric and adolescent age groups. J Pediatr Orthop 2013; 33:598–607. [DOI] [PubMed] [Google Scholar]
- 12.Blount WP, Schaefer AA, Johnson JH. Fractures of the forearm in children. J Am Med Assoc 1942; 120:111–116. [Google Scholar]
- 13.Eismann EA, Parikh SN, Jain VV. Rereduction for redisplacement of both-bone forearm shaft fractures in children. J Pediatr Orthop 2016; 36:405–409. [DOI] [PubMed] [Google Scholar]
- 14.Schwarz AF, Höcker K, Schwarz N, Jelen M, Styhler W, Mayr J, et al. [Recurrent fracture of the pediatric forearm]. Unfallchirurg 1996; 99:175–182. [PubMed] [Google Scholar]
- 15.Filipe G, Dupont JY, Carlioz H. [Recurrent fractures of both bones of the forearm in children]. Chir Pediatr 1979; 20:421–426. [PubMed] [Google Scholar]
- 16.Bowman EN, Mehlman CT, Lindsell CJ, Tamai J. Nonoperative treatment of both-bone forearm shaft fractures in children: predictors of early radiographic failure. J Pediatr Orthop 2011; 31:23–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kay S, Smith C, Oppenheim WL. Both-bone midshaft forearm fractures in children. J Pediatr Orthop 1986; 6:306–310. [DOI] [PubMed] [Google Scholar]
- 18.Kay J, Memon M, Marx RG, Peterson D, Simunovic N, Ayeni OR. Over 90 % of children and adolescents return to sport after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 2018; 26:1019–1036. [DOI] [PubMed] [Google Scholar]
- 19.Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med 2016; 44:1861–1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.O’Brien MJ, Howell DR, Pepin MJ, Meehan WP, 3rd. Sport-related concussions: symptom recurrence after return to exercise. Orthop J Sports Med 2017; 5:2325967117732516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Slongo T, Audigé L. AO pediatric comprehensive classification of long-bone fractures (PCCF). AO Foundation; 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khosla S, Melton LJ, 3rd, Dekutoski MB, Achenbach SJ, Oberg AL, Riggs BL. Incidence of childhood distal forearm fractures over 30 years: a population-based study. JAMA 2003; 290:1479–1485. [DOI] [PubMed] [Google Scholar]
- 23.Beleckas C, Calfee R. Distal radius fractures in the athlete. Curr Rev Musculoskelet Med 2017; 10:62–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Canty G, Nilan L. Return to play. Pediatr Rev 2015; 36:438–447. [DOI] [PubMed] [Google Scholar]