Abstract
Purpose:
This study collates and maps physiotherapy pre- and post-licensure curricula and pedagogical approaches for point of care ultrasonography (POCUS).
Method:
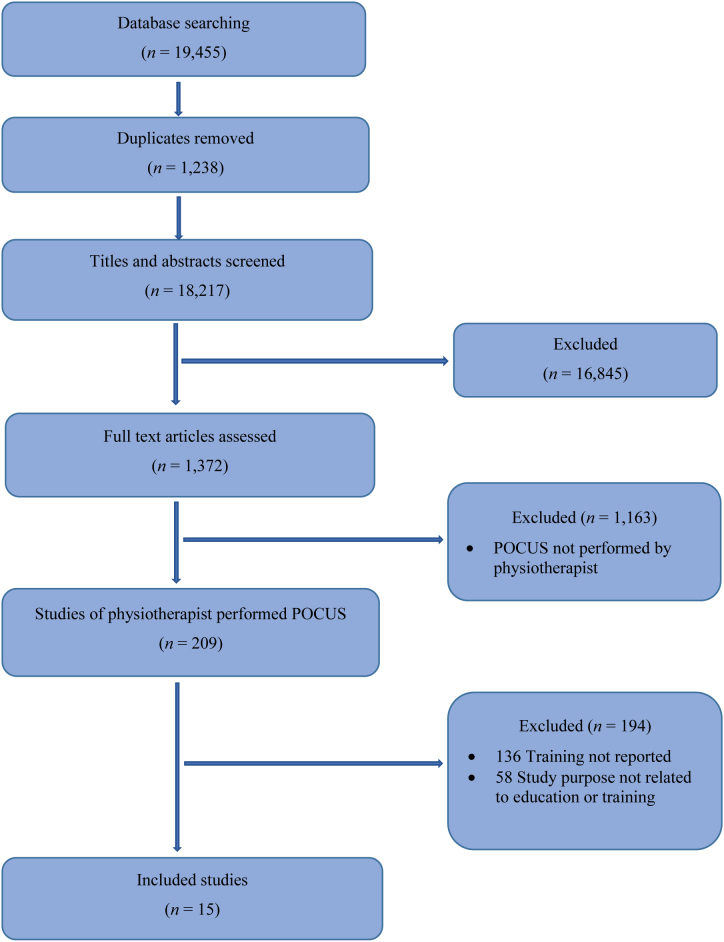
We used a standardized scoping review methodology and reporting framework. A total of 18,217 titles and abstracts, and 1,372 full text citations were screened, with 209 studies classified as physiotherapist performed POCUS.
Results:
Of the 209 studies, 15 evaluated pre- and post-licensure curricula and pedagogical approaches. Seventy-two to 98% of pre-licensure programs reported including theoretical knowledge of POCUS and 44–45% reported practical teaching or competency assessment. In post-licensure studies of POCUS, 0–61% of physiotherapists reported training for POCUS. All studies of post-licensure pedagogical approaches included an assessment of theoretical knowledge of POCUS, but only one study included a practical assessment of competency. There was considerable variability in POCUS methods and duration of pedagogical approaches. Except for one study, all pedagogical approaches reported improvement in theoretical knowledge.
Conclusion:
Progress in physiotherapy-specific, standardized, competency-based curricula and pedagogical approaches in POCUS has been limited, with minimal research available, and considerable variability both pre- and post-licensure. These findings could be used to advocate for the inclusion of POCUS in pre- and post-licensure physiotherapy curriculum, and suggest a need for clear guidelines from regulatory colleges and licensing bodies, and a common terminology for physiotherapist performed POCUS. Future directions for research include a systematic review of the psychometric properties of physiotherapist performed POCUS within and across anatomical areas, an assessment of value of different forms of training, and an evaluation of the impact of physiotherapist performed POCUS on patient outcomes.
Key Words: physical therapists, physical therapy modalities, point of care systems, teaching, ultrasonography.
Résumé
Objectif :
compiler et cartographier les programmes et les approches pédagogiques avant et après l’obtention du permis d’exercer à l’égard de l’échographie au point d’intervention (ÉPI).
Méthodologie :
analyse environnementale standardisée et cadre référentiel. Les chercheurs ont examiné un total de 18 217 titres et résumés et de 1 372 citations complètes, et 209 études ont été classées comme des ÉPI effectuées par des physiothérapeutes.
Résultats :
des 209 études, 15 évaluaient des programmes et des approches pédagogiques avant et après l’obtention du permis d’exercer. De 72 % à 98 % des programmes avant l’obtention du permis d’exercer présentaient des connaissances théoriques sur l’ÉPI, et de 44 % à 45 % traitaient de l’enseignement pratique ou de l’évaluation des compétences. Pour ce qui est des études sur l’ÉPI après l’obtention du permis d’exercer, de 0 % à 61 % des physiothérapeutes ont déclaré avoir suivi une formation sur l’ÉPI. Toutes les études sur les approches pédagogiques après l’obtention du permis d’exercer contenaient une évaluation des connaissances théoriques sur l’ÉPI, mais une seule incluait une évaluation pratique de la compétence. Les modes d’ÉPI et la durée des approches pédagogiques étaient très variables. Sauf dans une étude, toutes les approches pédagogiques entraînaient une amélioration des connaissances théoriques.
Conclusion :
les programmes et approches pédagogiques des ÉPI fondés sur les compétences, standardisés et propres à la physiothérapie ont peu évolué, on fait l’objet de très peu de recherches et sont très variables tant avant et qu’après l’obtention du permis d’exercer. Ces résultats pourraient être utilisés pour revendiquer l’inclusion des ÉPI dans les programmes de physiothérapie avant et après l’obtention du permis d’exercer et démontrent la nécessité de directives claires de la part des ordres de réglementation et des organismes d’attribution de permis, de même que d’une terminologie commune sur les ÉPI effectuées par des physiothérapeutes. Les futures orientations de la recherche comprennent une analyse systématique des propriétés psychométriques des ÉPI effectuées par un physiothérapeute dans les zones anatomiques et entre elles, une évaluation de la valeur de divers types de formation et une évaluation des effets des ÉPI effectuées par des physiothérapeutes sur les résultats cliniques des patients.
Mots-clés : échographie, enseignement, modalités de la physiothérapie, physiothérapeutes, systèmes aux points d’intervention
With advances in technology and research, new modalities and treatments are emerging in physiotherapy practice and research. For curricular and pedagogical approaches to remain aligned with these advances, pre-licensure physiotherapy programs must adapt to ensure safe and efficacious entry-level standards. Post-licensure continuing development courses must also integrate new practices into course offerings to provide educational opportunities that reflect the evolving needs of the profession. Advances in education also provide the foundation for regulatory colleges and licensing bodies to protect the public with the provision of governance frameworks and guidance on quality assurance processes.
Point of care ultrasonography (POCUS) is a relatively recent application of sonography.1 With appropriate training, physiotherapists can perform POCUS for the evaluation of a specific organ, pathology, or procedure within their area of practice.2,3 However, POCUS is operator dependent, and several authors suggest there may be a risk of misdiagnosis if it is used improperly or by untrained users.2–4 The first international meeting on physiotherapist performed diagnostic imaging, termed rehabilitative ultrasound, occurred in 2006.5 At this time, rehabilitative and diagnostic imaging by physiotherapists was in its infancy and the need to establish training standards for physiotherapists was recognized as a priority.5 Standards for training are needed to ensure competency, diagnostic accuracy, and patient safety.3 Educational curricula, professional governance, and local institutional protocols should be in place to advance the scope of the physiotherapy profession in POCUS and to ensure proper clinical implementation.3
A narrative review identified three areas of POCUS in physiotherapy practice (diagnostic, rehabilitative, interventional) and outlined a range of clinical purposes.1 A recent scoping review found 82% of studies on physiotherapist performed POCUS were published in the last 10 years, confirming POCUS as an emerging area of practice. Most studies reported on establishing psychometric properties of physiotherapist performed POCUS. Only 35% of included studies reported on the training that the physiotherapist received to perform POCUS (K. Strike et al., unpublished data, June 2021).
Despite its emergence, most pre-licensure physiotherapy programs do not provide theoretical and practical education on POCUS.1 Currently there are no internationally accepted curricula or minimum competency requirements for physiotherapist performed POCUS.1 Physiotherapists can access training programs such as the Berwin Institute of Diagnostic Medical Ultrasound and the American Registry for Diagnostic Medical Sonography.1 However, these programs do not provide physiotherapy-specific education and may not meet local regulatory requirements.1
Whittaker and colleagues proposed a competency-based education framework for POCUS as a foundation for the development and evaluation of POCUS courses for physiotherapists.1 Strike and colleagues developed a post-licensure POCUS training program for physiotherapists in hemophilia.6,7 However, information on pedagogical approaches pre- and post-licensure for physiotherapist performed POCUS remains sparse.
To better understand current methods and make recommendations for education, a greater appreciation of the literature on the curricular and pedagogical approaches for physiotherapist performed POCUS is required. Scoping reviews explore broad questions in emerging areas of practice.8 Scoping reviews methodologically map existing literature and summarize the main sources and types of evidence available on a specific topic.8 The primary objective was to collate and map physiotherapy pre- and post-licensure curricula and pedagogical approaches for POCUS.
Methods
Research questions
-
1.
What curricular and pedagogical approaches have been used in pre-licensure physiotherapy degree programs to teach POCUS?
-
2.
What curricular and pedagogical approaches have been used in post-licensure physiotherapy continuing education courses to teach POCUS?
-
3.
How were the pre- and post-licensure curricular and pedagogical approaches assessed? What were the results?
Study selection
This study protocol was developed a priori and followed the standardized scoping review methodology by Arksey & O’Malley and Levac and colleagues8,9 The Preferred Reporting Items for Systematic Reviews and Meta-analyses Extension for Scoping Reviews (PRIM-SA-ScR) was used as a framework for reporting.10 Search strategies were developed in consultation with a health research librarian. The following databases were searched from January 1, 1980—November 10, 2019: OVID Medline, CINAHL, AMED, and EMBASE. Search strategies are included in online Appendices 1–4.
Following the database search, citations were imported into EndNote X8 to remove duplicates, and exported to Covidence (2020 Veritas Health Innovation, Melbourne, Australia). For the selection of studies on physiotherapist performed POCUS, two reviewers performed a calibration exercise using a purposeful selection of 40 citations to evaluate reviewer agreement using Cohen's kappa statistic. A value of greater than 0.80 was required. This calibration exercise resulted in a Cohen's kappa of 0.886, indicating a strong level of agreement between the reviewers.11 The two reviewers independently reviewed all titles, abstracts, and full-text citations. Conflicts were resolved by discussion. If consensus could not be reached, conflicts were resolved with a third reviewer. Inclusion criteria were original research on POCUS in which the imaging was performed by a physiotherapist, or if the ultrasound operator was trained to use POCUS by a physiotherapist. Studies were excluded if they were non-English language, review articles, studies of therapeutic ultrasound, or grey literature. Studies that were classified as physiotherapist performed POCUS were then assessed by one reviewer for reporting on curriculum and pedagogical approaches.
Data extraction
The data extracted from each study included citation, study design, country, anatomical area of POCUS, sample size, and characteristics of curricula or pedagogical approaches for POCUS including methods of assessment and results.
Data synthesis and analysis
Descriptive statistics were applied to the numerical data. The descriptive numerical summary included sample size, study design, country, type and duration of pedagogical approach, and anatomical area of POCUS. Thematic analysis consisted of identifying similarities and differences in how curricula and pedagogical training approaches were assessed, and the results of these approaches.
Results
Our database search identified 19,455 citations. Following the removal of duplicates, 18,217 titles and abstracts were screened, and 1,372 full text articles were assessed, resulting in 209 studies of physiotherapist performed POCUS. Of the 209 studies, 15 evaluated POCUS curricula and pedagogical approaches. Refer to the PRISMA diagram (Figure 1).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRIMSA) flow diagram of process used to select included studies.
Characteristics of included studies
The 15 studies were published in 11 different journals with 1,930 (median = 49) participants enrolled. Most studies were descriptive surveys (n = 7; 46.7%), followed by three randomized controlled trials (20%), two non-controlled trials (13.3%), one non-randomized controlled trial, one qualitative study, and one measurement study. Eighty-six per cent (n = 13) of the studies were published from 2010–2019. Four studies were completed in Australia, three in Spain, and two in both the United Kingdom (UK) and the United States of America (USA). A single study was completed in both Singapore and New Zealand. One study was a collaboration between Australia and New Zealand and one study involved multiple countries. For details of included studies, refer to Appendix 5.
Pre-licensure physiotherapy degree programs
Curricular and pedagogical approaches
Two studies surveyed pre-licensure physiotherapy degree programs about their curricular approaches.12,13
Chipchase and colleagues used a semi-structured interview to survey 13 faculty members representing all 18 entry-level physiotherapy programs in New Zealand and Australia on current curricula for electrophysical agents including POCUS.12 POCUS for biofeedback was included in theory in 13 (72.2%) programs; however, only 8 (44%) included practical teaching. The most common reason given for this discrepancy was that POCUS was not common in clinical practice.12 Thirty-nine per cent of respondents indicated that POCUS was not an entry-level competency.12 Boissonnault and colleagues surveyed faculty from 155 physiotherapy programs in the USA.13 Of the respondents, 152 (98.1%) included imaging in their programs. The average amount of teaching time for imaging theory, clinical applications, and skills was 24.4 hours (range 2–75 hours). Sixty-eight (45%) programs assessed student competency. On a scale of 1–5 (1 = not competent, 5 = competent), respondents rated entry-level competency for the utilization of ultrasound at 1.77.13
Assessment of pedagogical approaches and results
Four studies evaluated pre-licensure pedagogical approaches for POCUS.14–17 Two studies assessed competence in palpation and ultrasound imaging of the knee and the lumbopelvic region using e-learning strategies in addition to traditional classroom teaching.15,16 One study investigated mobile learning, or m-learning, as an adjunct to traditional classroom teaching on palpation and ultrasound imaging of the shoulder.14 One study assessed if a six-hour training program was sufficient for students to reliably perform measurements of the lumbar multifi-dus using POCUS.17 As shown in Table 1, all four studies assessing pedagogical approaches demonstrated that the curriculum resulted in improvement in practical skills and theoretical knowledge. The e-learning and m-learn-ing groups scored significantly higher than the control groups on global objective standardized clinical evaluation scores.14–16 There were no differences in theoretical knowledge between groups. The two reliability studies demonstrated discordant results. Cantarero-Villanueva and colleagues demonstrated inferior interrater reliability between novice and expert examiners, while Schrank and colleagues demonstrated that interrater and intrarater reliability was high between the expert and novice raters and the three novice raters.15,17
Table 1.
Pre-Licensure Physiotherapy Degree Programs
| Pedagogical approach (n) | Citation | Anatomical area | Duration | Assessment | Results |
|---|---|---|---|---|---|
| E-learning (n = 2) | Arroyo-Morales, M.16 | Knee | 4 classroom hours 3 weeks self-study |
1. Palpation, ultrasound skills via SOCE 2. Theoretical knowledge via MCQ 3. Time to generate reliable image and to localize specific structure with palpation 4. Quality of the intervention on 5-point Likert scale |
1. E-learning group scored significantly higher on global SOCE scores 2. No intergroup difference in knowledge 3. E-learning group required less time for palpation, more time to obtain image 4. Both groups reported satisfaction with the intervention |
| Cantarero-Villanueva, I.15 | Lumbo-pelvic region | 6 classroom hours 20 self-study hours |
1. Palpation, ultrasound skills via OSCE 2. Reproducibility in measurement of multifidus cross sectional area 3. Quality of the intervention on 5-point Likert scale |
1. E-learning group scored significantly higher on OSCE 2. ICC for control and e-learning groups as compared to reference measurement was 0.61, 0.65 3. No difference between groups on quality of the intervention |
|
| Mobile learning (n = 1) | Fernandez- Lao, C.14 | Shoulder | 6 classroom hours 20 self-study hours |
1. Palpation, ultrasound skills via OSCE 2. Theoretical knowledge via MCQ 3. Time to generate reliable image and to localize specific structure with palpation 4. Quality of the intervention on 5-point Likert scale 5. M-learning group assessed satisfaction on 11-point numeric rating scale |
1. M-learning group scored significantly higher on Global OSCE scores 2. No intergroup difference in knowledge 3. No difference between groups in time to generate image and palpation 4. M-learning group reported higher ratings on items: teacher was competent, lessons were interesting, able to learn a lot, size of groups were optimal, teacher-student interaction adequate 5. M-learning satisfaction was high |
| Six-hour program (n = 1) |
Schrank, E.C.17 | Lumbar multifidus at L2-L3, L4-L5 | 6 hours: 2 hours education in ultrasound imaging, 4 hours practice time | 1. Interrater, intrarater reliability via ICC and SEM | 1. Interrater reliability for all raters at L2-L3, L4-L5 was high (ICC = 0.827 and 0.936) 2. Interrater reliability for novice raters was good at L2-L3 (ICC = 0.760), high at L4-L5 (ICC = 0.905) 3. Reliable intrarater measurements at L2-L3 and L4-L5 4. SEM showed stability of the measurements |
SOCE = structured objective clinical evaluation; MCQ = multiple choice questions; OSCE = objective structured clinical evaluation; ICC = intraclass correlation coefficient; SEM standard error of measurement.
Post-licensure physiotherapy courses
Curricular and pedagogical approaches
Six studies investigated post-licensure curricular and pedagogical approaches.18–23 Five studies were descriptive studies that surveyed physiotherapists in Australia, New Zealand, and the UK; one was a qualitative study from Australia.18–23 Four descriptive surveys investigated POCUS in physiotherapy practice, and one survey was specific to thoracic ultrasound. The qualitative study targeted POCUS for biofeedback of the pelvic floor.18–23 Three studies used random sampling and reported a range of POCUS usage in practice from 11.6% to 67% (median 24%).20,22,23 In the study of thoracic ultrasound, 31% reported using POCUS in practice.19
Methods and duration of training were highly variable. McKiernan and colleagues found 61% of respondents reported training; of these, 67% reported that the training was for “several hours.”23 Jedrzejczak and Chipchase reported that 26.7% had attended training with the majority of courses being a half day or less.22 Potter and colleagues reported that 52% of respondents received formal training ranging from 5–8 hours with 41–50% including practical sessions.21 Informal training ranged from 0–4 hours.21 Ellis and colleagues reported 43% of users of POCUS had received formal training, 48% received informal training, and 10% had not received any training but were using POCUS.20 In the survey of thoracic ultrasound, 44% of respondents had undertaken training, 8% progressed beyond the introductory course to complete a formal assessment of competency, and 3% reported using POCUS without training.19 In the focus group study of pelvic floor physiotherapists, none of the respondents reported participating in a formal course, most had participated in informal training and some reported no training at all.18
Formal training emphasized theory including ultrasound physics, safety, standardization of measurements, and practical sessions.19–21 Informal approaches included self-directed training, training provided by the supplier of the ultrasound machine, attendance at a university lecture, and clinical observation with radiologists, gynecologists, or specialist physiotherapists.18–23 Physiotherapists in all six studies identified the need for more training. Preferred methods included formal physiotherapy-specific courses, workshops, DVDs, practical hands-on sessions, e-learning, and clinical supervision.18,19,21,23
Assessment of pedagogical approaches and results
Three studies evaluated pedagogical approaches post-licensure.24–26 Two studies investigated a one-day course for physiotherapists, one focused on thoracic ultrasound, and the other focused on the lung, diaphragm, and lower limb muscles.24,25 The third study compared a one-day workshop with a self-paced DVD for POCUS of the abdominal muscles, multifidus, and pelvic floor.26 As shown in Table 2, all three studies included pre- and post-intervention knowledge assessments. One study included a practical examination of scanning competence for a limited number of participants.24
Table 2.
Post-Licensure Physiotherapy Courses
| Pedagogical approach (n) | Citation | Anatomical area | Duration | Assessment | Results |
|---|---|---|---|---|---|
| One day course (n = 2) | Ntoumenopoulos, G.24 | Thoracic | 6.5 hours: 2.5 hours didactic lectures, 4 hours practical training | 1. Pre-, post-knowledge via MCQ 2. Practical examination for 6 participants 3. Evaluation of course satisfaction 4. 4–6 week follow-up survey |
1. MCQ increased from 73.3 +/− 15.5% to 86.5 +/− 5.5% (mean, SD) 2. Median practical examination score: 15.5/16 3. All participants felt course would impact their clinical practice. 42% reported insufficient time in practical session 4. 67% performed 1–3 scans in practice. Most frequent barrier was time constraints |
| Ntoumenopoulos, G.25 | Lung, diaphragm, lower limb muscles | 6.5 hours: 2.5 hours didactic lectures, 4 hours practical training | 1. Pre-, post-knowledge via MCQ 2. Evaluation of course satisfaction |
1. Pre- and post-knowledge scores: 63% and 62% 2. 83% felt pre-reading was appropriate, 48% reported insufficient time in practical training. All sessions were rated as good or excellent |
|
| Workshop and DVI (n = 1) | D McKiernan, S.26 | Abdominal muscles, multifidus, pelvic floor | Workshop: One day DVD: 2 months |
1. Pre-, post-assessment of knowledge and perception of training using true/false, open ended and MCQ | 1. Significant increase in post-assessment scores in both groups, no difference between groups All participants reported training was good Workshop: areas of improvement: more supervision in practice sessions, more time identifying anatomy on ultrasound DVD: areas of improvement: more annotation on images in motion, more difficult examples, summary sheet of operational points |
MCQ = multiple choice questions, SD = standard deviation.
The course on thoracic ultrasound resulted in improvement in theoretical knowledge and proficiency in the practical evaluation.24 In contrast, participants in the course for ultrasound of the lung, diaphragm, and lower limb muscles did not demonstrate improvement in knowledge.25 There were statistically significant increases in post-assessment knowledge scores for both the one-day workshop and the DVD; however, there was no significant difference between the two interventions.26 Participants in both of the one-day training course studies felt that there was insufficient time in practical sessions.24,25
Discussion
This scoping review systematically mapped physiotherapy pre- and post-licensure curricula and pedagogical approaches for POCUS. While 15 studies were published between 2005–2019, progress in the development of a physiotherapy-specific, standardized, competency-based curricula remains in the early stages. The majority of studies reported assessment of theoretical knowledge; however, there was limited practical teaching and evaluation. There was considerable variability in POCUS uses, methods, and duration of pedagogical approaches.
With the exception of one, all studies reported improvement in theoretical knowledge of POCUS regardless of pedagogical approach.14–17,24–26 The study that did not report improvement in knowledge evaluated the impact of a one-day training program on POCUS of the lung, diaphragm, and lower limb muscles.25 In contrast with the other studies that focused on one anatomical area, this study taught POCUS in three anatomical areas, which may have increased the complexity of the content. Also, language barriers may have impacted the findings, as the physiotherapists were from 14 different countries and the course was provided in English.25
Effective use of POCUS is dependent on operator skill and training.3,27–29 As a key stakeholder, the Canadian Association of Radiologists (CAR) published a position statement on POCUS by non-radiologists to provide guidance on scope and training standards.27–29 The CAR cautions that inappropriate use of musculoskeletal POCUS by untrained physicians may result in patient harm via incorrect diagnoses and subsequent interventions.27–29 CAR's position states that health care professionals performing POCUS must receive training equivalent to a qualified imaging specialist within their area of practice.27 This review confirmed that there is currently no accepted standard of training for the use of POCUS by physiotherapists in any area of practice. The variation in formal and informal training and competency assessment may lead to variable skills in image acquisition, optimization, and interpretation. This review also found that physiotherapists are using POCUS in clinical practice without train-ing.18–20 The lack of training may impact the credibility of the physiotherapy profession and patient safety, highlighting concerns for regulatory colleges, licensing bodies, and medical colleagues. Scholten-Peeters and colleagues surveyed orthopedic surgeons and radiologists in the Netherlands and reported no additional value of physiotherapist performed POCUS in primary care.30 Although this is a single study, and further research is needed, perceived disadvantages of physiotherapist performed POCUS in primary care were false-positive or false-negative results, lack of experience, insufficient education, and the inability to relate the outcomes of POCUS with other forms of diagnostic imaging.30 Along with the position statement from the CAR, this study suggests that in order for the physiotherapy profession to gain credibility and support from key stakeholders, increased attention should be paid to education and competency-based training.
Variability in training may also impact the psychometric properties of POCUS. Acceptable intrarater and interrater reliability of physiotherapist performed POCUS has been documented in the assessment of the acromi-on-greater tuberosity distance, supraspinatus, transverse abdominus, lumbar multifidis, quadriceps, and the lung.31–35 However, studies have also reported suboptimal interrater reliability when compared to more experienced POCUS users, and fair inter-professional agreement with radiologists.36–38 Thoomes-de Graaf and colleagues investigated the inter-professional agreement between physiotherapists and radiologists in patients with shoulder pain, and found physiotherapists with more experience and training showed moderate agreement compared to only slight agreement in physiotherapists with less training, indicating the need for further education.37
Physiotherapists are using POCUS under different terminology and language such as rehabilitative ultrasound or real-time ultrasound.1,22 The lack of consistent definitions and terminology may also contribute to challenges in professional credibility and advancing education. This variability may be due to physiotherapists adopting different language in order to meet institutional or regulatory requirements, or to avoid perceived infringement on the scope of practice of other health care disciplines.1 To move forward, it will be important to engage key stakeholders and clinicians who are using and contributing to the research base to agree on the internationally accepted definitions, terminology, and scope of physiotherapy diagnostic ultrasound.
This scoping review identifies potential next steps. First, educators could use these findings to advocate for the inclusion of POCUS in pre- and post-licensure physiotherapy curricula. Development of physiotherapy specific pedagogical approaches should include both theoretical and practical assessments with an established procedure to ensure ongoing quality assurance. Training should be methodological and evaluative, and should include a component of experiential learning. Content of theoretical and practical teaching should be guided by local regulatory colleges, and physiotherapy scope of practice, as both vary around the world. Competency-based education is one form of pedagogy that has been reported in advanced practice physiotherapy and pelvic floor physiotherapy, and has been proposed as a possible educational framework for POCUS.1,7,39,40 Secondly, researchers could use the findings to identify research priorities moving forward. Next steps could include: a systematic review and meta-analysis on the reliability and validity of physiotherapist performed POCUS within and across diagnoses; an assessment of the value of training including the impact of different forms of education, experience, and pedagogy on the psychometric properties of POCUS; and an evaluation of the impact of physiotherapist performed POCUS on patient outcomes. Lastly, adoption of internationally accepted definitions for POCUS will promote collaboration and research agendas. Ideally, these definitions would aim to align with position statements on the use of POCUS from other stakeholders in the field.
Limitations
Database searching resulted in over 19,000 studies, and therefore non-English language, review articles, and grey literature were excluded for feasibility. All but one study reported improvement in theoretical knowledge of POCUS regardless of the methods used. However, the heterogeneity in pedagogical approaches make it difficult to provide recommendations regarding the effectiveness of one training method over another. The majority of the included studies were completed in Australia, Spain, USA, and the UK, which may affect generalizability to educational and professional systems around the world.
Conclusion
This scoping review identified 15 studies from 2005–2019 and found considerable variability in pre- and post-licensure curricular and pedagogical approaches for physiotherapist performed POCUS. Progress in the development of a physiotherapy specific, standardized, competency-based curricula has been limited, with minimal research available, and remains in the early stages.
Key Messages
What is already known on this topic
Physiotherapist performed POCUS is emerging in clinical practice, education, and research. However, there are no internationally accepted curricula or minimum competency requirements. Very little is known about the outcomes of different pedagogical approaches on theoretical knowledge and practical scanning competence.
What this study adds
Progress in the development of a physiotherapy-specific, standardized education curricula and pedagogical approaches for POCUS has been limited. This scoping review demonstrated considerable variability in pre- and post-licensure curricular and pedagogical approaches. These findings suggest that there is a need for clear guidelines from regulatory colleges and licensing bodies, physiotherapy-specific curricula and pedagogical frameworks, and a common terminology for physiotherapist performed POCUS.
Appendix 1: Search Strategy OVID Medline: 1980–November 10, 2019
1. exp Physical Therapists/
2. exp Physical Therapy Modalities/
3. exp Physical Therapy Specialty/
4. physiotherap*.mp.
5. physical therap*.mp.
6. 1 or 2 or 3 or 4 or 5
7. exp Ultrasonography/
8. dg.fs
9. ultraso*.mp.
10. sonography.mp.
11. 7 or 8 or 9 or 10
12. 6 and 11
13. point of care.mp or exp Point-of-Care Systems/
14. sports medicine.mp or exp Sports Medicine/
15. orthopedics.mp or exp Orthopedics/
16. respiratory*.mp or exp Respiratory System/
17. chest physi*.mp
18. atelectasis.mp or exp Pulmonary Atelectasis/
19. rotator cuff*.mp or exp Rotator Cuff/
20. pelvic*.mp or exp Pelvic Floor/
21. h?emophilia*.mp
22. exp Hemophilia A/
23. exp Hemophilia B/
24. neuropathy.mp
25. acupuncture.mp or exp Acupuncture/
26. rheumatology.mp or exp Rheumatology/
27. exercise therap*.mp or exp Exercise Therapy/
28. therapeutic exercise.mp
29. musculoskeletal*.mp or exp Musculoskeletal System/
30. exp Musculoskeletal Diseases/
31. exp Musculoskeletal injur
32. 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28
33. 29 and 11 and 13
34. 30 or 12
35. Limit 31 to (English language and yr = “1980-Current”)
Appendix 2: Search Strategy Cinahl: 1980–November 10, 2019
1. physical therapists/
2. exp physical therapy/
3. exp physiotherapy, evidence database/
4. physical therapy practice, evidence-based/
5. exp research, physical therapy
6. physiotherap*.mp.
7. physical therap*.mp.
8. 1 or 2 or 3 or 4 or 5 or 6 or 7
9. exp ultrasonography
10. ultraso*.mp.
11. sonography.mp.
12. 9 or 10 or 11
13. 8 and 12
14. exp “point of care testing” or “point of care”.mp
15. sports medicine.mp or exp sports medicine/
16. orthopedics.mp or exp orthopedics/
17. respiratory*.mp
18. chest physi*.mp or exp chest physical therapy
19. atelectasis.mp or exp pulmonary atelectasis/
20. rotator cuff*.mp or exp rotator cuff/
21. exp rotator cuff injuries/
22. pelvic*.mp or exp pelvic floor muscles/
23. h?emophilia*.mp or exp hemophilia/
24. exp Hemophilia B/
25. neuropathy.mp
26. acupuncture.mp or exp Acupuncture/
27. rheumatology.mp or exp Rheumatology/
28. exercise therapy.mp or exp therapeutic exercise/
29. musculoskeletal.mp or exp musculoskeletal system/
30. 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29
31. 30 and 12 and 14
32. 31 or 13
33. Limit 32 to (English language and yr = “1980-Current”)
Appendix 3: Search Strategy For Amed: 1980–November 10, 2019
1. exp physiotherapists/
2. exp physical therapy modalities/
3. exp physical therapy specialty/
4. physiotherap*.mp.
5. physical therap*.mp.
6. 1 or 2 or 3 or 4 or 5
7. exp Ultrasonography/
8. ultraso*.mp.
9. sonography.mp.
10. 7 or 8 or 9
11. 6 and 10
12. point of care.mp
13. sports medicine.mp or exp Sports Medicine/
14. orthopedics.mp or exp Orthopedics/
15. respiratory*.mp or exp respiratory muscles/
16. chest physiotherapy.mp or exp chest physiotherapy/
17. atelectasis.mp or exp atelectasis/
18. rotator cuff*.mp or exp Rotator Cuff/
19. pelvic*.mp or exp Pelvic Floor/
20. h?emophilia*.mp exp Hemophilia/
21. neuropathy.mp
22. acupuncture.mp or exp Acupuncture/
23. rheumatology.mp or exp rheumatic disease/
24. exercise therapy.mp or exp Exercise Therapy/
25. musculoskeletal.mp or exp Musculoskeletal System/
26. 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25
27. 26 and 10 and 12
28. 27 or 11
29. Limit 28 to (English language and yr = “1980-Current”)
Appendix 4: Search Strategy for EMBASE: 1980–November 10, 2019
1. exp physiotherapist/
2. exp physiotherapy/
3. exp physiotherapy practice/
4. physiotherap*.mp.
5. physical therap*.mp.
6. 1 or 2 or 3 or 4 or 5
7. exp ultrasound/
8. exp echography/
9. ultraso*.mp.
10. sonography.mp.
11. 7 or 8 or 9 or 10
12. 6 and 11
13. exp “point of care testing” or “point of care”.mp
14. sports medicine.mp or exp sports medicine/
15. orthopedics.mp or exp orthopedics/
16. respiratory*.mp
17. chest physi*.mp
18. atelectasis.mp or exp atelectasis/
19. rotator cuff*.mp or exp rotator cuff injury/
20. pelvic*.mp or exp pelvic floor muscle training/
21. h?emophilia*.mp
22. exp hemophilia A/
23. exp Hemophilia B/
24. neuropathy.mp or exp neuropathy/
25. acupuncture.mp or exp Acupuncture/
26. rheumatology.mp or exp Rheumatology/
27. exercise therapy.mp or exp kinesiotherapy/
28. musculoskeletal.mp or exp musculoskeletal system/
29. 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29
30. 29 and 11 and 13
31. 30 or 12
32. Limit 31 to (English language and yr = “1980-Current”)
Appendix 5: Details of Included Studies
| Title | Authors | Year | Journal | Study design | Sample Size | Country |
|---|---|---|---|---|---|---|
| A blended learning approach to palpation and ultrasound imaging skills through supplementation of traditional classroom teaching with an e-learning package16 | Arroyo-Morales M, Cantarero-Villanueva I, Fernandez-Lao C, Guirao-Pineyro M, Castro-Martin E, Diaz-Rodriguez L. | 2012 | Manual Therapy | Randomized controlled trial | 46 | Spain |
| Diagnostic and procedural imaging curricula in physical therapist professional degree programs13 | BoissonnaultWG, White DM, Carney S, Malin B, Smith W. | 2014 | Journal of Orthopaedic and Sports Physical Therapy | Descriptive study | Faculty from 155 PT programs | United States of America |
| Evaluation of e-learning as an adjunctive method for the acquisition of skills in bony landmark palpation and muscular ultrasound examination in the lumbopelvic region: a controlled study15 | Cantarero-Villanueva I, Fernandez-Lao C. Galiano-Castillo N, Castro-Martin E, Diaz-Rodriguez L, Arroyo-Morales M. | 2012 | Journal of Manipulative and Physiological Therapeutics | Randomized controlled trial | 50 | Spain |
| A survey of electrophysical agents’ curricula in entry-level physiotherapy programs in Australia and New Zealand12 | Chipchase LS, Williams MT, Robertson VJ. | 2005 | New Zealand Journal of Physiotherapy | Descriptive study | 13 participants representing all 18 entry level physiotherapy programs in Australia and New Zealand | Australia, New Zealand |
| Exploring the clinical use of ultrasound imaging: A survey of physiotherapists in New Zealand20 | Ellis R, De Jong R, BassettS, Helsby J, Stokes M, Cairns M. | 2018 | Musculoskeletal Science and Practice | Descriptive study | 415 | New Zealand |
| The effectiveness of a mobile application for the development of palpation and ultrasound imaging skills to supplement the traditional learning of physiotherapy students14 | Fernandez-Lao C, Cantarero-Villanueva I, Galiano-Castillo N, Caro-Moran E, Diaz-Rodriguez L, Arroyo-Morales M. | 2016 | BMC Medical Education | Randomized controlled trial | 49 | Spain |
| Diagnostic thoracic ultrasound imaging – An exploration of respiratory physiotherapists’ interest and use in clinical practice: A national survey18 | Hayward S, Smith M, Innes S. | 2019 | Ultrasound | Descriptive study | 133 | United Kingdom |
| The availability and usage frequency of real time ultrasound by physiotherapists in South Australia: an observational study22 | JedrzejczakA, Chipchase LS. | 2008 | Physiotherapy Research International | Descriptive study | 664 | Australia |
| A survey of diagnostic ultrasound within the physiotherapy profession for the design of future training tools23 | McKiernan S, Chiarelli P, Warren-Forward H. | 2011 | Radiography | Descriptive study | 99 | Australia |
| A comparison between workshop and DVD methods of training for physiotherapists in diagnostic ultrasound26 | McKiernan S, Chiarelli P, Warren-Forward H. | 2012 | Radiography | Non randomized controlled trial | 180 | Australia |
| Professional issues in the use of diagnostic ultrasound biofeedback in physiotherapy of the female pelvic floor18 | McKiernan S, Chiarelli P, Warren-Forward H. | 2013 | Radiography | Qualitative study | 16 | Australia |
| Impact of an intensive education programme of diagnostic lung and lower limb ultrasound on physiotherapist knowledge: A pilot study25 | Ntoumenopoulos G, Parry SM, Neindre AL. | 2018 | Australasian Journal of Ultrasound in Medicine | Non-controlled trial | 32 | Physiotherapists from Australia, South Africa, Singapore, Chile, Canada, Iran, New Zealand, Switzerland, Brazil, Nigeria, East Africa, West Africa, Pakistan, and United Arab Emirates |
| Evaluation of a pilot programme on diagnostic thoracic ultrasound curriculum for acute care physiotherapists24 | Ntoumenopoulos G, Ong HK, Toh HC, Saciólo RR SewaWD. | 2017 | Australasian Journal of Ultrasound in Medicine | Non-controlled trial | 12 | Singapore |
| Use of ultrasound imaging by physiotherapists: a pilot study to survey use, skills and training21 | Potter CL, Cairn MC, Stokes M. | 2012 | Manual Therapy | Descriptive study | 46 | United Kingdom |
| The reliability of rehabilitative ultrasound imaging measurements of the lumbar multifidi recorded by physical therapist students with minimal training17 | Schrank EC, Abraham K, Wilson MJ, Myers WV, King MG. | 2011 | Journal of Physical Therapy Education | Measurement study | 20 | United States of America |
References
- 1.Whittaker JL, Ellis R, Hodges PW, et al. Imaging with ultrasound in physical therapy: what is the PT's scope of practice? A competency-based educational model and training recommendations. Br J Sports Med. 2019;53(23):1447–53. 10.1136/bjsports-2018-100193. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moore CL, Copel JA. Point-of-care ultrasonography. N Engl J Med. 2011;364(8):749–57. 10.1056/nejmra0909487. Medline: [DOI] [PubMed] [Google Scholar]
- 3.Lawson W, Uy M, Strike K, et al. Point of care ultrasound in haemophilia: building a strong foundation for clinical implementation. Haemophilia. 2017;23(5):648–51. 10.1111/hae.13269. Medline: [DOI] [PubMed] [Google Scholar]
- 4.Solomon SD, Saldana F. Point-of-care ultrasound in medical education—stop listening and look. N Engl J Med. 2014;370(12):1083–5. 10.1056/nejmp1311944. Medline: [DOI] [PubMed] [Google Scholar]
- 5.Whittaker JL, Teyhen DS, Elliott JM, et al. Rehabilitative ultrasound imaging: understanding the technology and its applications. J Orthop Sports Phys Ther. 2007;37(8):434–49. 10.2519/jospt.2007.2350. Medline: [DOI] [PubMed] [Google Scholar]
- 6.Strike K, Uy M, Lawson W, et al. Point-of-care ultrasonography in haemophilia care: training and competency for muscular haematomas. Haemophilia. 2018;24(3):1–3. 10.1111/hae.13417. Medline: [DOI] [PubMed] [Google Scholar]
- 7.Strike KL, Iorio A, Jackson S, et al. Point of care ultrasonography in haemophilia care: recommendations for training and competency evaluation. Haemophilia. 2015;21(6):828–31. 10.1111/hae.12767. Medline: [DOI] [PubMed] [Google Scholar]
- 8.Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69. 10.1186/1748-5908-5-69. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. 10.1080/1364557032000119616. Medline:34647832 [DOI] [Google Scholar]
- 10.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. Epub 2018 May 5. 10.7326/m18-0850. Medline: [DOI] [PubMed] [Google Scholar]
- 11.McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012;22(3):276–82. 10.11613/bm.2012.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chipchase L, Williams M, Robertson V. A survey of electrophysical agents’ curricula in entry-level physiotherapy programs in Australia and New Zealand. NZ J Physiother. 2005;33(2):34–47. Medline: 0077293 [Google Scholar]
- 13.Boissonnault W, White D, Carney S, et al. Diagnostic and procedural imaging curricula in physical therapist professional degree programs. J Orthop Sports Phys Ther. 2014;44(8):579–8. 10.2519/jospt.2014.5379. Medline: [DOI] [PubMed] [Google Scholar]
- 14.Fernandez-Lao C, Cantarero-Villanueva I, Galiano-Castillo N, et al. The effectiveness of a mobile application for the development of palpation and ultrasound imaging skills to supplement the traditional learning of physiotherapy students. BMC Med Educ. 2016;16(1):274. 10.1186/s12909-016-0775-1. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cantarero-Villanueva I, Fernandez-Lao C, Galiano-Castillo N, et al. Evaluation of E-learning as an adjunctive method for the acquisition of skills in bony landmark palpation and muscular ultrasound examination in the lumbopelvic region: a controlled study. J Manipulative Physiol Ther. 2012;35(9):727–34. 10.1016/j.jmpt.2012.10.007. Medline: [DOI] [PubMed] [Google Scholar]
- 16.Arroyo-Morales M, Cantarero-Villanueva I, Fernandez-Lao C, et al. A blended learning approach to palpation and ultrasound imaging skills through supplementation of traditional classroom teaching with an e-learning package. Man Ther. 2012;17(5):474–8. 10.1016/j.math.2012.04.002. Medline: [DOI] [PubMed] [Google Scholar]
- 17.Schrank E, Abraham K, Wilson M, et al. The reliability of rehabilitative ultrasound imaging measurements of the lumbar multifidi recorded by physical therapist students with minimal training. J Phys Ther Educ. 2011;25(2):57–62. 10.1097/00001416-201101000-00010. [DOI] [Google Scholar]
- 18.McKiernan S, Chiarelli P, Warren-Forward H. Professional issues in the use of diagnostic ultrasound biofeedback in physiotherapy of the female pelvic floor. Radiography. 2013;19(2):117–24. 10.1016/j.radi.2013.01.006. [DOI] [Google Scholar]
- 19.Hayward S, Smith M, Innes S. Diagnostic thoracic ultrasound imaging: an exploration of respiratory physiotherapists’ interest and use in clinical practice: a national survey. Ultrasound. 2020;28(1):14–22. 10.1177/1742271X19861131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ellis R, De Jong R, Bassett S, et al. Exploring the clinical use of ultrasound imaging: a survey of physiotherapists in New Zealand. Musculoskelet Sci Pract. 2018;34:27–37. 10.1016/j.msksp.2017.12.002. Medline: [DOI] [PubMed] [Google Scholar]
- 21.Potter C, Cairns M, Stokes M. Use of ultrasound imaging by physiotherapists: a pilot study to survey use, skills and training. Man Ther. 2012;17(1):39–46. 10.1016/j.math.2011.08.005. Medline: [DOI] [PubMed] [Google Scholar]
- 22.Jedrzejczak A, Chipchase LS. The availability and usage frequency of real time ultrasound by physiotherapists in South Australia: an observational study. Physiother Res Int. 2008;13(4):231–40. 10.1002/pri.409. Medline: [DOI] [PubMed] [Google Scholar]
- 23.McKiernan S, Chiarelli P, Warren-Forward H. A survey of diagnostic ultrasound within the physiotherapy profession for the design of future training tools. Radiography. 2011;17(2):121–5. 10.1016/j.radi.2010.08.003. [DOI] [Google Scholar]
- 24.Ntoumenopoulos G, Ong HK, Toh HC, et al. Evaluation of a pilot programme on diagnostic thoracic ultrasound curriculum for acute care physiotherapists. Australas J Ultrasound Med. 2017;20(4):147–54. 10.1002/ajum.12059. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ntoumenopoulos G, Parry SM, Neindre AL. Impact of an intensive education programme of diagnostic lung and lower limb ultrasound on physiotherapist knowledge: a pilot study. Australas J Ultrasound Med. 2018;21(2):104–14. 10.1002/ajum.12089. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McKiernan S, Chiarelli P, Warren-Forward H. A comparison between workshop and DVD methods of training for physiotherapists in diagnostic ultrasound. Radiography. 2012;18(4):287–91. 10.1016/j.radi.2012.07.004. [DOI] [Google Scholar]
- 27.Chawla TP, Cresswell M, Dhillon S, et al. Canadian association of radiologists position statement on point-of-care ultrasound. Can Assoc Radiol J. 2019;70(3):219–25. 10.1016/j.carj.2019.06.001. Medline: [DOI] [PubMed] [Google Scholar]
- 28.Olszynski P, Kim D, Liu R, et al. A multidisciplinary response to the Canadian association of radiologists’ point-of-care ultrasound position statement. Can Assoc Radiol J. 2020;71(2):136–7. 10.1177/0846537119898004. Medline: [DOI] [PubMed] [Google Scholar]
- 29.Chawla T, Cresswell M, Dhillon S, et al. Reply to “a multidisciplinary response to the Canadian association of radiologists’ point-of-care ultrasound position statement”. CanAssoc Radiol J. 2020;71(2):138–9. 10.1177/0846537119899277. Medline: [DOI] [PubMed] [Google Scholar]
- 30.Scholten-Peeters GG, Franken N, Beumer A, et al. The opinion and experiences of Dutch orthopedic surgeons and radiologists about diagnostic musculoskeletal ultrasound imaging in primary care: a survey. Man Ther. 2014;19(2):109–13. 10.1016/j.math.2013.08.003. Medline: [DOI] [PubMed] [Google Scholar]
- 31.Kumar P, Attwood M. Inter rater reliability of ultrasound measurements of acromion-greater tuberosity distance between experienced and novice raters in healthy people. Musculoskelet Care. 2018;16(1):163–6. 10.1002/msc.1206. Medline: [DOI] [PubMed] [Google Scholar]
- 32.Schneebeli A, Egloff M, Giampietro A, et al. Rehabilitative ultrasound imaging of the supraspinatus muscle: intra- and interrater reliability of thickness and cross-sectional area. J Bodyw Mov Ther. 2014;18(2):266–72. 10.1016/j.jbmt.2013.09.009. Medline: [DOI] [PubMed] [Google Scholar]
- 33.Koppenhaver S, Hebert J, Fritz J, et al. Reliability of rehabilitative ultrasound imaging of the transversus abdominis and lumbar multifidus muscles. Arch Phys Med Rehabil. 2009;90(1):87–94. 10.1016/j.apmr.2008.06.022. Medline: [DOI] [PubMed] [Google Scholar]
- 34.Tillquist M, Kutsogiannis DJ, Wischmeyer PE, et al. Bedside ultrasound is a practical and reliable measurement tool for assessing quadriceps muscle layer thickness. J Parenter Enteral Nutr. 2014;38(7):886–90. 10.1177/0148607113501327. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Leech M, Bissett B, Kot M, et al. Lung ultrasound for critical care physiotherapists: a narrative review. Physiother Res Int. 2015;20(2):69–76. 10.1002/pri.1607. Medline: [DOI] [PubMed] [Google Scholar]
- 36.Hoppes CW, Sperier AD, Hopkins CF, et al. Ultrasound imaging measurement of the transversus abdominis in supine, standing, and under loading: a reliability study of novice examiners. Int J Sports Phys Ther. 2015;10(6):910–17. Medline: [PMC free article] [PubMed] [Google Scholar]
- 37.Thoomes-de Graaf M, Scholten-Peeters GG, Duijn E, et al. Interprofessional agreement of ultrasound-based diagnoses in patients with shoulder pain between physical therapists and radiologists in the Netherlands. ManTher. 2014;19(5):478–83. 10.1016/j.math.2014.04.018. Medline: [DOI] [PubMed] [Google Scholar]
- 38.Greene G, Green A. Transversus abdominis function: a reliability study using ultrasound imaging to measure changes in muscle thickness. Physiother Ireland. 2009;30(2):34–6. 10.3233/ppr-2009-30208. Medline: [DOI] [Google Scholar]
- 39.Frawley HC, Neumann P, Delany C. An argument for competency-based training in pelvic floor physiotherapy practice. Physiother Theory Pract. 2019;35(12):1117–30. 10.1080/09593985.2018.1470706. Medline: [DOI] [PubMed] [Google Scholar]
- 40.Fennelly O, Desmeules F, O'Sullivan C, et al. Advanced musculoskeletal physiotherapy practice: informing education curricula. Musculoskelet Sci Pract. 2020;48:102174. 10.1016/j.msksp.2020.102174. Medline: [DOI] [PubMed] [Google Scholar]