Abstract
Background
A successful clinical outcome for total hip arthroplasty (THA) depends on accurate sizing and positioning of the implants. Using three-dimensional (3-D) pre-operative planning with a computerized tomography (CT) scan has many potential advantages over conventional 2-D planning using radiographs, including potentially more accurate assessments of the size and anteversion of the acetabulum, as well as lateral femoral offset. The purpose of this study was to compare the accuracy of 3-D to 2-D templating with respect to acetabular and femoral size, as well as lateral femoral offset.
Methods
Pre-operative templating data was collected prospectively from a consecutive series of 290 primary THAs (acetabulum on all, femoral component on 255 of the cases using one specific stem). All cases were initially templated on a digital imaging picture archiving and communication (PACS) system with calibrated images to estimate the acetabular size, femoral size, and lateral femoral offset. The 3-D templating was then performed with software based on a CT scan, and the results were compared to what was surgically implanted.
Results
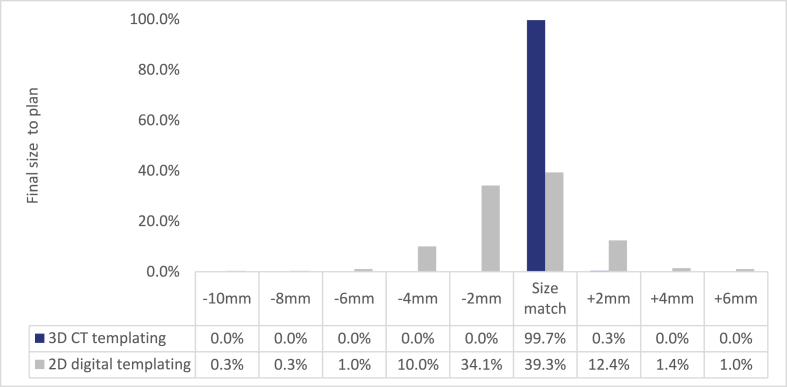
The 3-D templating for the acetabulum was accurate 99.7% of the time based on the final implanted component. The 2-D templating for the acetabulum was accurate 39% of the time, with 46% of cases templating smaller and 15% templating larger. The 3-D templating of the femoral component was accurate 63% of the time, and within one size of final implant in 96% of cases. The 2-D templating of the femoral component was accurate 53% of the time and within one size of final implant in 94% of cases. The 2-D templated femoral offset was accurate 87% of the time and was changed in 13% of cases after 3-D templating.
Conclusion
The CT-based 3-D preoperative planning was superior to 2-D planning for THA with respect to acetabular size, femoral size, and lateral femoral offset. Precise acetabular component sizing conserves bone and allows for a more predictable press fit, while facilitating efficient inventory management. Lateral femoral offset is often difficult to measure on 2-D images, and 3-D templating consistently allows for accurate offset restoration, which is important for normal hip function and stability.
1. Introduction
A successful clinical outcome for total hip arthroplasty (THA) depends on accurate sizing and positioning of the implants to restore the native hip biomechanics and function, as well as to avoid complications. Inaccurate sizing of the implants can result in fracture or compromised bone fixation. Malposition of the implants can lead to various complications such as excessive wear, dislocation, and leg-length discrepancy. Pre-operative templating is an important component of the THA procedure, as it can estimate the approximate size and type of implants required to fit an individual patient's anatomy and identify any potential complications with implant placement. It is also an important exercise to plan for the restoration of leg-length and offset, and it can serve as a rehearsal that leads to a more efficient surgical procedure.1, 2, 3
Traditionally, pre-operative templating for THA has been performed on 2-dimensional (2-D) plain or digital x-ray images. Historically, acetate templates with a built-in 20% magnification were used to overlay plain X-ray images and estimate the needed implants. In the last 3 decades, digital radiography has become standard, and these templating platforms based on image calibration have provided surgeons with a more comprehensive system to perform and archive the pre-operative templating procedure.4, 5, 6, 7
The three-dimensional (3-D) pre-operative planning using computerized tomography (CT) scans have many potential advantages over conventional 2-D planning using radiographs, including improved accuracy in the assessment of the size of the implants, transverse imaging of the native anteversion of the acetabulum, as well as the location and size of peri-acetabular osteophytes. Using 3-D templating software, surgeons can also accurately measure native femoral anteversion, head height, and lateral offset to more easily enable an attempt to restore the normal biomechanics of the hip joint, and to simulate a range of motion that is impingement-free.8, 9, 10, 11, 12 Improved accuracy of planned implant sizes can also result in enhanced procedural efficiencies, by reducing the number of implants delivered to the operating room, and reducing facility inventory needs. This may be especially beneficial in the ambulatory surgical center (ASC) setting, where implant storage space is often more limited compared to within a hospital. Previous literature has been limited by small patient numbers, data outside of the United States, and heterogeneity in indications for surgery.8, 9, 10, 11, 12 Therefore, the purpose of this study was to compare the accuracy of 3-D to 2-D templating with respect to acetabular and femoral size, as well as lateral femoral offset, from a series of consecutively performed total hip arthroplasties.
2. Materials and methods
Pre-operative templating data was collected prospectively from a consecutive series of 290 primary THAs between January 1, 2017, and December 31, 2019. Institutional review board approval to perform this study was deemed not necessary as all patient and radiographic data was de-identified.
All cases were initially templated by the attending surgeon (JC) on a digital picture archiving and communication system (PACS), with calibrated images to estimate the size of the acetabular and femoral components utilizing methods established and verified previously.13,14 Templating was done using supine antero-posterior (AP) pelvis X-rays. The X-rays were performed using a standardized technique with a 40-inch camera-to-film distance, centered over the pubic symphysis. A 25-mm (mm) metal calibration ball was attached to the proximal thigh at approximately the level of the femur from the table, and was used to calibrate the digital image. The templated acetabular component size was determined by matching the periphery of the bony femoral head and adding 4 mm, which normally equates to the appropriate fit of the acetabulum. All acetabular components were Trident IIR (Stryker, Mahwah New Jersey).
There were 255 of the 290 cases performed with the Accolade II femoral component (Stryker), and the femoral component analyses in this study were restricted to these cases. This was because there were 35 cases that utilized a different stem based on patient characteristics and surgeon discretion and were excluded from the study. The femoral size was determined by matching the best fit within the femoral metaphysis and canal at the planned implant seating level for each patient. The implant seating level was determined by the planned lengthening of the leg (in mm), matching the planned femoral head height to the planned acetabular center of rotation. Lateral femoral offset (standard 132-degree or high offset 127-degree) required to reproduce native hip joint mechanics was determined for each patient based on this templating process. Also, the planned femoral neck resection level was measured from the superior saddle of the lesser trochanter, and replicated by direct measurements, intra-operatively,
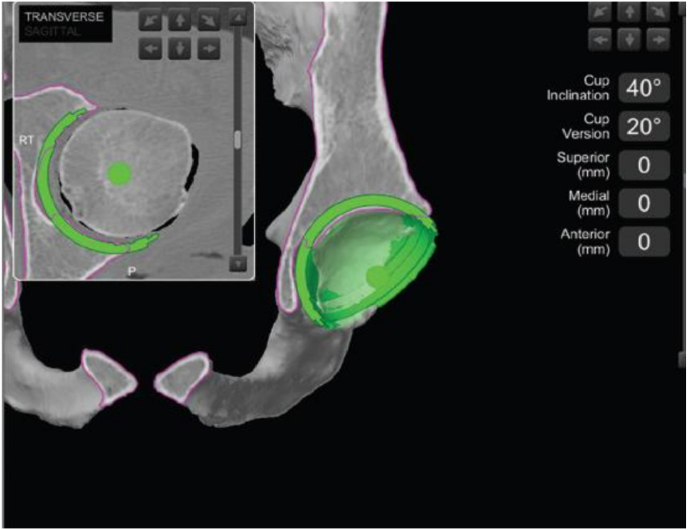
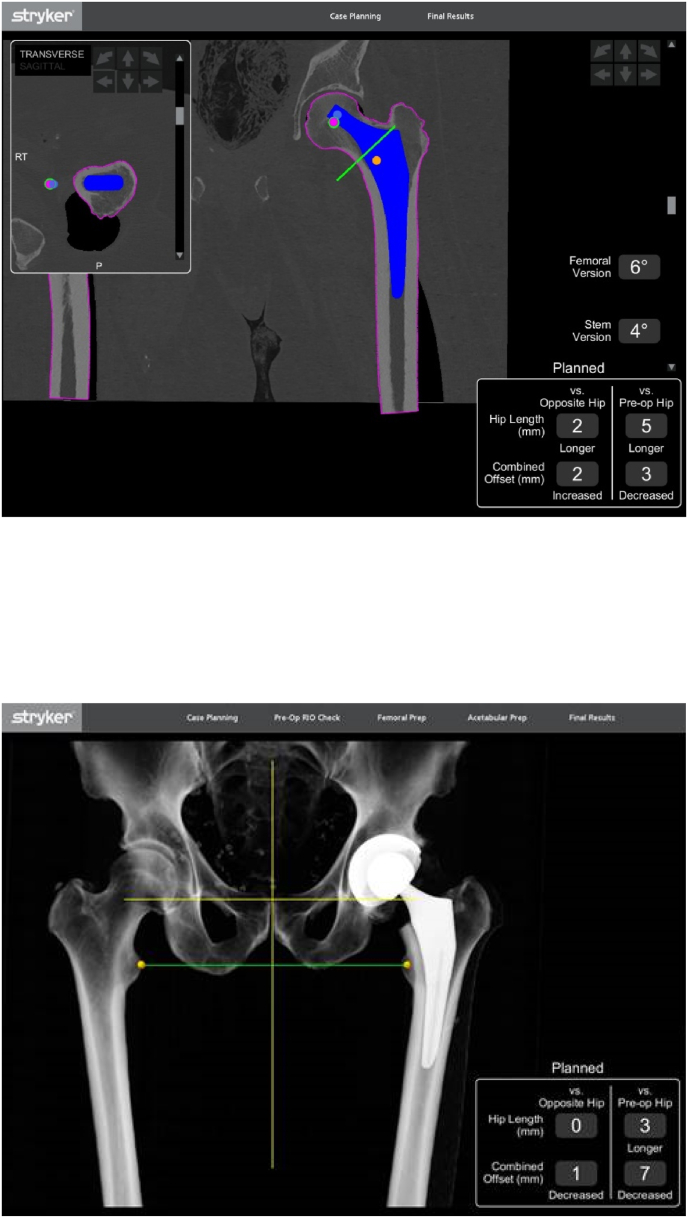
The 3-D templating was then performed with software based on a CT scan, obtained using a standardized protocol designed to be used with the Mako 4.0 THA platform (Stryker, Mahwah, New Jersey). The 3-D acetabular template was matched to the image of the bony contour of the patient's acetabulum in the coronal, transverse, and sagittal planes, with a goal of removing 1–3 mm of bone from all sectors of the acetabular cavity. A mobile 3-D image model of the planned acetabular component location and orientation was also reviewed from multiple viewing angles. These images showed the size and location of peri-acetabular osteophytes, as well as the planned seating level of the acetabulum relative to the medial wall (Fig. 1, Fig. 2). The 3-D femoral template was matched to the CT image of the proximal femur in the coronal, transverse, and sagittal planes, and the size was estimated by using the best fit relative to the femoral endosteal anatomy (Fig. 3). The results of the 2-D digital templating and the 3-D CT-based templating were recorded with respect to the planned acetabular size, femoral component size, and lateral offset, and were compared to what was actually surgically implanted. Secure press fit fixation of the acetabular component was achieved without screws 99.3% of the time. Additional fixation with 1 screw was used in 2 cases due to bony deficiency (see Fig. 4).
Fig. 1.
Mako Total Hip Application showing acetabular shell planning.
Fig. 2.
Mako Total Hip Application showing acetabular shell planning.
Fig. 3.
Mako Total Hip Application showing femoral stem planning in transverse view and X-ray view.
Chart 1.
Final acetabular shell sizing with CT-based 3-D templating was accurate to plan in 99.7% of cases, whereas 2-D digital templating was accurate in 39% of cases. A total of 46% of the cases (n = 133) templated smaller and 15% (n = 43) templated larger on the 3-D plan compared to the 2-D plan.
2.1. Data analyses
For categorical factors like demographics, associated conditions, and complications, we employed Chi-square evaluations in our two-variable analyses. When analyzing continuous factors, for instance, age, we made use of the Student's t-tests. We conducted all of our evaluations using R Studio, sourced from the University of Auckland's Statistics Department in New Zealand, setting the significance threshold at P < 0.05.
3. Results
3.1. Acetabular component
The CT-based 3-D templating for the acetabular component was accurate to the exact size 99.7% of the time (289 of 290) based on the final implanted component, significantly outperforming the 2-D digital templating, which was accurate in only 39% (114 of 290) of cases (P < 0.001). While the acetabular size was increased by 2 mm in one instance due to surgeon discretion, 46% of cases (n = 133) were templated smaller on the 3-D plan compared to the 2-D plan (P < 0.001). The most frequent size deviation was 2 mm smaller, observed in 34% (n = 99) of cases (P < 0.001). Other deviations included 10% (n = 29) templated 4 mm smaller, and smaller deviations of 6, 8, and 10 mm in 1.0% (n = 3), 0.3% (n = 1), and 0.3% (n = 1) of cases, respectively. In contrast, the 2-D plan templated 12.4% (n = 36) of cases 2 mm larger, 1.4% (n = 4) 4 mm larger, and 1.0% (n = 3) 6 mm larger (P values < 0.001, 0.043, and 0.088 respectively) (Table 1).
Table 1.
3-D vs 2-D.
| 1 | 3-D Templating | 2-D Templating | P-value | ||
|---|---|---|---|---|---|
| **Acetabular Component Accuracy** | |||||
| Accurate to exact size | 289/290 | 99.7% | 114/290 | 39.3% | <0.001 |
| Total templated smaller | 133/290 | 45.8% | 0/290 | 0.0% | <0.001 |
| Total templated larger | 0/290 | 0.0% | 43/290 | 14.8% | <0.001 |
| Most common size deviation | |||||
| 2 mm smaller | 99/290 | 34.1% | 0/290 | 0.0% | <0.001 |
| 4 mm smaller | 29/290 | 10.0% | 0/290 | 0.0% | <0.001 |
| 6 mm smaller | 3/290 | 1.0% | 0/290 | 0.0% | 0.088 |
| 8 mm smaller | 1/290 | 0.3% | 0/290 | 0.0% | 1.000 |
| 10 mm smaller | 1/290 | 0.3% | 0/290 | 0.0% | 1.000 |
| 2 mm larger | 0/290 | 0.0% | 36/290 | 12.4% | <0.001 |
| 4 mm larger | 0/290 | 0.0% | 4/290 | 1.4% | 0.043 |
| 6 mm larger | 0/290 | 0.0% | 3/290 | 1.0% | 0.088 |
| **Femoral Component Accuracy** | |||||
| Accurate to exact size | 161/255 | 63.1% | 135/255 | 52.9% | 0.015 |
| Within one size of final implant | 246/255 | 96.5% | 241/255 | 94.5% | 0.562 |
| Stem 1 size smaller | 48/255 | 18.8% | 69/255 | 27.1% | 0.022 |
| Stem 1 size larger | 37/255 | 14.5% | 37/255 | 14.5% | 1.000 |
| Stem 2 sizes smaller | 8/255 | 3.1% | 8/255 | 3.1% | 1.000 |
| Stem 3 sizes smaller | 1/255 | 0.4% | 1/255 | 0.4% | 1.000 |
| Stem 5 sizes smaller | 0/255 | 0.0% | 1/255 | 0.4% | 0.281 |
| Stem 2 sizes larger | 0/255 | 0.0% | 3/255 | 1.2% | 0.062 |
| Stem 3 sizes larger | 0/255 | 0.0% | 1/255 | 0.4% | 0.281 |
| **Lateral Femoral Offset Accuracy** | |||||
| Matched the plan | 290/290 | 100.0% | 222/255 | 87.0% | <0.001 |
| Changed after 3D templating | 0/290 | 0.0% | 33/255 | 13.0% | <0.001 |
| Switched from 132-degree to 127-degree offset | 0/290 | 0.0% | 31/255 | 12.0% | <0.001 |
| Changed from 127-degree to 132-degree offset stem | 0/290 | 0.0% | 2/255 | 1.0% | 0.088 |
3.2. Femoral component
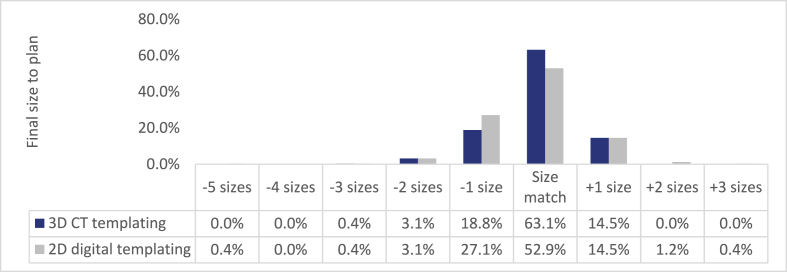
The 3-D templating of the femoral component was accurate to the exact size in 63% (161 of 255) of cases, a significant improvement over the 53% (135 of 255) accuracy of 2-D templating (P = 0.015). The 3-D templating was within one size of the final implant 96% of the time (246 of 255), comparable to the 95% (241 of 255) accuracy of 2-D templating (P = 0.562). Deviations included 19% (n = 48) of stems templated 1 size smaller and 14% (n = 37) 1 size larger in 3-D, versus 27% (n = 69) 1 size smaller and 14% (n = 37) 1 size larger in 2-D (P = 0.022 for 1 size smaller). Other deviations were consistent between the two methods (Fig. 5).
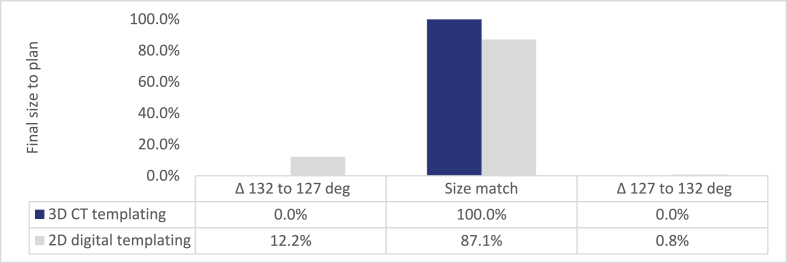
Chart 2.
Final femoral stem size with CT-based 3-D templating was accurate to plan in 63% of cases, whereas 2-D digital templating was accurate in 53% of cases.
3.3. Lateral femoral offset
Lateral femoral offset consistently matched the 3-D plan, with a 100% match rate. In contrast, the 2-D templating offset was accurate 87% of the time (222 out of 255), with changes observed in 13% of cases post 3-D templating (P < 0.001). Specifically, 12% (n = 31) of stems were adjusted from a 132-degree standard offset to a 127-degree high offset, while 1% (n = 2) transitioned from a 127-degree to a 132-degree offset stem (p < 0.001). Notably, 34% of cases initially templated for a standard offset stem in 2-D (n = 32) were switched to a high offset stem after 3-D templating to restore native hip mechanics (Fig. 6).
Chart 3.
Final femoral stem offset with CT-based 3-D templating was accurate to plan in 100% of cases, whereas 2-D digital templating was accurate in 87% of cases.
4. Discussion
Pre-operative planning is an essential part of the success of total hip arthroplasty, including templating of the pre-operative radiographic images to predict the size and shape of the implants required for every patient. Pre-operative templating is also an important exercise for the surgeon, to anticipate any anatomical challenges, plan for accurate restoration of leg length and offset, and therefore improve the efficiency of the surgical procedure itself. Numerous studies have identified the value of a stepwise pre-operative templating process. Most of these are based on 2-D digital radiographs using digital templating software, which have been shown to be reliable and reproducible.1, 2, 3, 4, 5, 6, 7
In recent years, 3-D templating processes have become available for pre-operative THA planning.8, 9, 10, 11, 12 These programs can be based on biplanar radiographs that are converted to a 3-D image such as the EOS system (ATEC Spine, Carlsbad, California).15, 16, 17 Brenneis et al. have reported improved implant size accuracy and reproducibility using this technology compared to standard 2-D digital templating.15The 3-D templating may also be based on CT scans, that are either incorporated into a free-standing templating software program, a surgical navigation program, or a robotic surgical platform. Hassani et al. have reported accurate implant sizing and reproducible implant position using CT-based planning software.9 Similarly, Wako et al. showed excellent reliability and component alignment in THAs planned with a CT-based templating software.10
The present study utilized CT-based 3-D-planning software that is embedded in the robotic surgical platform. This system has the advantage of being able to model the planned placement of the implants, and therefore optimize both the size and the planned component orientation relative to the native anatomy in each individual patient. This allows the surgeon to visualize the location of peri-acetabular osteophytes in 3 dimensions relative to the planned acetabular component placement, and to plan the anteversion of the component to optimize joint stability and to avoid anterior soft-tissue impingement. The acetabular size and location can be optimized to preserve bone in both the anterior and posterior walls, which resulted in 99.3% of the acetabular components having a stable press fit without screws in this series.
There was less of a difference in the accuracy of final femoral component size prediction between the 2-D and 3-D templating plans (53 vs 63%, respectively). Additionally, the final implanted femoral component was within 1 size of the templated size 94 and 96% of the time for the 2- and 3-D plans respectively.
It is important to note that the 3-D templating was more accurate than the 2-D plans with respect to estimating femoral offset. The 3-D software projects a true AP view of the proximal femur, allowing for optimal assessment of lateral femoral offset. It is thought that external rotation of the femur projected onto an AP pelvis digital x-ray leads to underestimation of the lateral offset. It is for this reason that 34% of the 2-D plans in this study that were templated for a standard offset 132-degree stem were switched to a high offset 127-degree stem after being templated in 3-D.
Our study demonstrated that CT-based 3-D pre-operative planning is more accurate than 2D planning with respect to acetabular and femoral component size and lateral femoral offset compared to 2-D planning. Coupled with a robotic navigation system, this has been shown to have clinical benefits including a markedly reduced rated of dislocation in posterior approach THA compared to manual techniques.16 This benefit may be due in part to the system's ability to incorporate spino-pelvic mobility into a virtual impingement model pre-operatively18,19 Other studies have demonstrated benefits of CT-based 3-D pre-operative planning in hips with developmental hip dysplasia,20,21 as well as hips with segmental acetabular defects requiring metal augments.22 Accurate pre-operative implant size prediction can also create efficiencies in the operating room by avoiding delivery of multiple unnecessary implants and reducing inventory storage demands.
This study has several strengths, including being a consecutive series of total hip arthroplasty procedures with prospectively collected 2- and 3-D templating data. All of the 2-D images were obtained using a standardized imaging technique, and all of the 3-D images were collected using a standardized CT protocol. The same acetabular component was used in all 290 cases, and the same femoral component was used in all 255 cases analyzed. All of the final implant data was also collected prospectively. A potential limitation of the study is that all of the 2-D and 3-D planning was done by a single experienced surgeon, and while it was consistent, the results could be different among surgeons using different templating techniques. The results may not be generalizable to other institutions. Differences in body mass index and gender anatomy may affect the accuracy of pre-operative planning. Additionally, reliability may differ depending on the type of implant. It is difficult to verify the reproducibility of patients with implant loosening and fragile bone quality by osteolysis. Future studies should aim to include lager patient numbers, homogenous indications for surgery, and improve the level of evidence, including randomized, controlled trials. The consideration of body mass index, gender, and impact of Dorr classification on stem size should be a focus of future studies as well. The strength of the study is the large patient numbers, homogenous indications for surgery, and data within the United States.
5. Conclusion
The CT-based 3-D preoperative planning was superior to 2-D planning for THA with respect to acetabular size, femoral size, and lateral femoral offset. The novelty of the study is strength in patient numbers, data within the United States, and homogenous indications for surgery. Precise acetabular component sizing conserves bone and results in a predictable press fit while facilitating efficient inventory management. Lateral femoral offset is often difficult to measure on 2-D images, and 3-D templating consistently allows for more accurate offset restoration, which is important for post-operative hip function and stability. This study illustrates some advantages of CT-based 3-D pre-operative planning for THA.
Ethical approval
IRB exemption due to retrospective nature and public database.
Funding
None.
Authors’ contribution
JD- Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Roles/Writing - original draft; and Writing - review & editing.
DH- Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Roles/Writing - original draft; and Writing - review & editing.
MM- Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Roles/Writing - original draft; and Writing - review & editing.
JC- Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Roles/Writing - original draft; and Writing - review & editing.
Data availability
Available in a respository upon request.
Declaration of competing interest
JD- None.
DH-None.
Acknowledgements
None.
References
- 1.Della Valle A.G., Padgett D.E., Salvati E.A. Preoperative planning for primary total hip arthroplasty. J Am Acad Orthop Surg. 2005;13:455–462. doi: 10.5435/00124635-200511000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Bono J.V. Digital templating in total hip arthroplasty. J Bone Joint Surg Am. 2004;86(suppl 2):118–122. doi: 10.2106/00004623-200412002-00016. [DOI] [PubMed] [Google Scholar]
- 3.Della Valle A.G., Slullitel G., Piccaluga F., et al. The precision and usefulness of preoperative planning for cemented and hybrid primary total hip arthroplasty. J Arthroplasty. 2005;20(1):51–58. doi: 10.1016/j.arth.2004.04.016. [DOI] [PubMed] [Google Scholar]
- 4.Iorio R., Siegel J., Specht L., et al. A comparison of acetate vs digital templating for preoperative planning of total hip arthroplasty: is digital templating accurate and safe? J Arthroplasty. 2009;24(2):175–179. doi: 10.1016/j.arth.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 5.Schichman I., Shaked O., Morgan S., et al. Digital templating in total hip arthroplasty using contralateral healthy hip results in decreased accuracy. Acta Orthop Belg. 2021;87(3):427–433. [PubMed] [Google Scholar]
- 6.Schaarani S.R., McHugh G., Collins D.A. Accuracy of digital preoperative templating in 100 consecutive uncemented total hip arthroplasties: a single surgeon series. J Arthroplasty. 2013;28(2):331–337. doi: 10.1016/j.arth.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 7.Montiel V., Troncoso S., Valente-Azcarate A., et al. Total hip arthroplasty digital templating: size predicting ability and interobserver variability. Indian J Orthop. 2020;54:840–847. doi: 10.1007/s43465-020-00217-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vigdorchik J.M., Sharma A.K., Jerabek S.A., et al. Templating for total hip arthroplasty in the modern age. J Am Acad Orthop Surg. 2021;29(5):e208–e216. doi: 10.5435/JAAOS-D-20-00693. [DOI] [PubMed] [Google Scholar]
- 9.Hassani H., Cherix S., Ek E., et al. Comparisons of preoperative three-dimensional planning and surgical reconstruction in primary cementless total hip arthroplasty. J Arthroplasty. 2014;29:1273–1277. doi: 10.1016/j.arth.2013.12.033. [DOI] [PubMed] [Google Scholar]
- 10.Wako Y., Nakamura J., Miura M., et al. Interobserver and intraobserver reliability of three-dimensional preoperative planning software in total hip arthroplasty. J Arthroplasty. 2018;33:601–607. doi: 10.1016/j.arth.2017.08.031. [DOI] [PubMed] [Google Scholar]
- 11.Bishi H., Smith J.B., Asopa V. Comparison of the accuracy of 2D and 3D templating methods for planning primary total hip replacement: a systematic review and metsa-analysis. EFORT Open Reviews: Hip. 2022;7(1):70–83. doi: 10.1530/EOR-21-0060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guenoun B., El Hajj F., Biau D., et al. Reliability of a new method for evaluating femoral stem positioning after total hip arthroplasty based on stereoradiographic 3D reconstruction. J Arthroplasty. 2015;30:141–144. doi: 10.1016/j.arth.2014.07.033. [DOI] [PubMed] [Google Scholar]
- 13.Kim M.S., Jeong M.C., Ji N.G., Lee J.S., Kim J.I., Suh K.T. Preoperative templating in PACS for total hip replacement. Journal of the Korean Orthopaedic Association. 2011;46(6):472–477. [Google Scholar]
- 14.Pongkunakorn A., Aksornthung C., Sritumpinit N. Accuracy of a new digital templating method for total hip arthroplasty using picture archiving and communication system (PACS) and iPhone technology: comparison with acetate templating on digital radiography. J Arthroplasty. 2021;36(6):2204–2210. doi: 10.1016/j.arth.2021.01.019. [DOI] [PubMed] [Google Scholar]
- 15.Brenneis M., Braun S., van Drongelen S., et al. Accuracy of preoperative templating in total hip arthroplasty with special focus on stem morphology: a randomized comparison between common digital and three-dimensional planning using biplanar radiographs. J Arthroplasty. 2021;36:1149–1155. doi: 10.1016/j.arth.2020.10.016. [DOI] [PubMed] [Google Scholar]
- 16.Escott B.G., Ravi B., Weathermon A.C., et al. EOS low dose radiography: a reliable and accurate upright assessment of lower-limb lengths. J Bone Joint Surg Am. 2013;95(e183):1–7. doi: 10.2106/JBJS.L.00989. [DOI] [PubMed] [Google Scholar]
- 17.Huang J., Zhu Y., Ma W., et al. A novel method for accurate preoperative templating for total hip arthroplasty using a biplanar digital radiographic (EOS) system. J Bone Joint Surg Am. 2020:1–7. doi: 10.2106/JBJS.OA.20.00078. e20.00078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bendich I., Vigdorchik J.M., Sharma A.K., et al. Robotic assistance for posterior approach total hip arthroplasty is associated with lower risk of revision for dislocation when compared to manual techniques. J Arthroplasty. 2022;37:1124–1129. doi: 10.1016/j.arth.2022.01.085. [DOI] [PubMed] [Google Scholar]
- 19.Anderson CG, Jang SJ, Brilliant ZR, et al. Complication rate after primary total hip arthroplasty using the posterior approach and enabling technology: a consecutive series of 2,888 hips. J Arthroplasty 2023 Pre-Proof. [DOI] [PubMed]
- 20.Hayashi S., Hashimoto S., Kuroda Y., et al. Robotic-arm assisted THA can achieve precise cup positioning in developmental dysplasia of the hip: a case control study. Bone Joint Res. 2021;10(10):629–638. doi: 10.1302/2046-3758.1010.BJR-2021-0095.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hepinstall M., Mota F., Naylor B., et al. Robotic-assisted total hip arthroplasty in patients who have developmental hip dysplasia. Surg Technol Int. 2021;39:338–347. [PubMed] [Google Scholar]
- 22.Chen F., Stoll T. Segmental acetabular defects managed by augments in conjunction with CT during robotic total hip arthroplasty. JBJS Case Connector. 2022;12 doi: 10.2106/JBJS.CC.22.00185. e22. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Available in a respository upon request.