Abstract
Objectives:
To examine the association of leisure-time sitting with radiographic incidence and progression of knee osteoarthritis (OA) over 2 years, and to determine whether worktime sitting modifies this association.
Methods:
We included adults with or at high risk for knee OA who enroled in the Osteoarthritis Initiative (OAI). Participants reported leisure-time sitting (≤4 vs. >4 h/day) and worktime sitting (frequent vs. infrequent) at enrolment, and had bilateral knee radiographs at enrolment and 2 years later. Our outcome, radiographic knee OA incidence/progression (yes/no), was defined as any increase in Kellgren-Lawrence grade over 2 years. We examined the association of leisure-time sitting (≤4 vs. >4 h/day) with risk of radiographic knee OA incidence/progression using binary linear regression, adjusting for potential confounders. We stratified by worktime sitting (frequent vs. infrequent) and repeated our analysis.
Results:
We included 4254 adults (mean age 61 years; 58% women; mean body mass index 29 kg/m2) who contributed a total of 8127 knees. Adults with >4 h/day of leisure-time sitting had 25% higher risk (adjusted risk ratio [RR] 1.25, 95% confidence interval [95% CI] 1.08–1.50) for radiographic knee OA incidence/progression compared with adults with ≤4 h/day of leisure-time sitting (referent group). Importantly, this association was intensified (RR 1.60, 95% CI 1.19–2.33) among adults with frequent worktime sitting, but was attenuated (RR 1.11, 95% CI 0.89–1.39) among adults with infrequent worktime sitting.
Conclusions:
Higher leisure-time sitting (>4 h/day) may be associated with greater risk for radiographic knee OA incidence/progression over 2 years. Furthermore, this association was intensified among adults who also reported frequent worktime sitting.
Keywords: arthritis
1 |. INTRODUCTION
Knee osteoarthritis (OA) is a serious debilitating disease that is characterised by progressive damage to the knee cartilage (Hawker, 2019). Often, such damage is attributed to excessive loading of the knee (Felson et al., 2000) or ‘overloading’. However, few studies have examined why many adults still experience knee OA incidence and progression when they spend much of their time sitting (Dunlop et al., 2011; Elena Losina et al., 2020; Thoma et al., 2018). It is likely that habitual, excessive sitting deprives knee cartilage of the mechanical load it needs to function normally (Sun, 2010), thereby creating an environment of ‘underloading’. A growing body of evidence indicates that ‘underloading’ makes knee cartilage vulnerable to thin and damage (Bader et al., 2011), though surprisingly, the effect of sitting on risk of knee OA incidence and progression has rarely been examined.
Excessive sitting, particularly during leisure-time (non-working time), is associated with numerous chronic diseases and early mortality (Katzmarzyk et al., 2009; Patel et al., 2010, 2018), making it a critical public health issue. During leisure-time, adults tend to engage in long uninterrupted bouts of sitting (Young et al., 2016), although these habits may be modified through intervention (Palmer et al., 2019). Adults can also engage in sitting during worktime, which consumes a large portion of their day. However, worktime sitting has been less consistently associated with adverse health outcomes (van Uffelen et al., 2010), and effective interventions to reduce worktime sitting remain unclear (Shrestha et al., 2018). Thus, we focused our primary research question on the consequences of leisure-time sitting and then expanded to a secondary question that also considered worktime sitting and its contribution to overall sitting time and potential ‘underloading’.
To summarise, the primary objective of this study was to examine the association of leisure-time sitting with risk of radiographic incidence and progression of knee OA over 2 years. We hypothesised that adults with higher leisure-time sitting (hours/day) were at increased risk of radiographic incidence/progression of knee OA compared with adults with lower leisure-time sitting. Our secondary objective was to determine whether worktime sitting modifies the association between leisure-time sitting and radiographic incidence/progression of knee OA. We hypothesised that among adults with higher worktime sitting, higher leisure-time sitting (compared with lower-leisure time sitting) would further amplify their risk of knee OA incidence/progression, given that their total sitting time was greatest. Conversely, we hypothesised that among adults with lower worktime sitting (who instead engaged in other activities, such as standing and walking), higher leisure-time sitting would not increase their risk of knee OA incidence/progression.
2 |. METHODS
2.1 |. The Osteoarthritis Initiative
We performed a secondary analysis of data from the Osteoarthritis Initiative (OAI). The OAI is a longitudinal, NIH/NIA-funded cohort study of men and women, aged 45–79 years at enrolment, who either had knee OA or were at high risk for developing knee OA at their baseline study visit (Fawaz-Estrup, 2004). The OAI enroled a total of 4796 adults between 2004 and 2006; specific inclusion and exclusion criteria for the OAI have been published elsewhere (Felson & Nevitt, 2004; Lester, 2008). All participants completed follow-up visits for up to 8 years (2004–2014). Clinical data and radiographic images were collected at study sites in Columbus, Ohio; Baltimore, Maryland; Pittsburgh, Pennsylvania; and Pawtucket, Rhode Island. Institutional review boards at all study sites approved the data collection, and all participants provided informed consent. OAI data are publicly available at https://nda.nih.gov/oai/.
2.2 |. Patient and public involvement
Other than the OAI participants described above, no patients or members of the public were involved in the current research study.
2.3 |. Additional study inclusion/exclusion criteria
Specifically, we used data from 4492 OAI participants (of the 4796 enroled) who had bilateral knee radiographs obtained at the baseline visit and at least one follow-up visit. At each visit, radiographs were semi-quantitatively scored for OA severity (on a scale of 0–4) using the Kellgren-Lawrence (KL) Grading Scale (Kellgren & Lawrence, 1957). First, we excluded participants if both knees met any of the following criteria at baseline: (1) poor image quality, which precluded the assessment of baseline KL grade, (2) presence of a prosthesis (e.g., knee replacement), or (3) end stage knee OA (i.e., maximum KL grade of 4). Next, we excluded participants if both knees did not have KL grade assessed at the 2-year follow-up visit, as it precluded assessment of radiographic incidence/progression in ≥1 knee over 2 years.
Lastly, for our primary analysis, we excluded participants who did not answer the question related to their leisure-time sitting (hours/day) at baseline. For our stratified analysis, we additionally excluded participants who either did not report their worktime activities at baseline or who did not work at baseline.
2.4 |. Exposure: Leisure-time sitting at baseline
At the baseline visit, OAI participants were given the Physical Activity Scale for the Elderly (PASE), an activity questionnaire designed for large cohort studies of older adults (Washburn et al., 1999). Participants reported their time spent in 12 different activity domains over the previous 7-day, including leisure-time, household, and occupational activities. The PASE demonstrates high validity and reliability in community-dwelling older adults, including those with knee pain and OA (Martin et al., 1999; Svege et al., 2012).
Participants answered PASE Item 1 to indicate how often they engaged in sitting activities (e.g., reading, watching TV, or doing handcrafts) over the previous 7 days on a 4-point scale (Never, Seldom [1–2 days], Sometimes [3–4 days], Often [5–7 days]). Then, participants may have answered PASE Item 1b to indicate how many hours/day they engaged in sitting activities on a 4-point scale (<1 h/day, ≥1 and <2 h/day, 2–4 h/day, and >4 h/day). Of note, participants who reported in PASE Item 1 that they ‘Never’ engaged in sitting activities were not prompted to answer Item 1b, so their response to Item 1b was categorised as ‘<1 h/day’ of sitting. Participants who were prompted to answer Item 1b but did not, that is, a missing response, were excluded from our analyses. We dichotomised our exposure variable, leisure-time sitting, as ‘≤4 h/day’ and ‘>4 h/day’ (Figure 1). Those above this cut-point (i.e., >4 h/day) represented the highest tertile of leisure-time sitting for the sample. Previous studies have selected cut-points ranging from 4 to 8 h/day that similarly divide the sample into tertiles or quartiles to categorise sitting (Dunstan et al., 2010; Patel et al., 2010).
FIGURE 1.
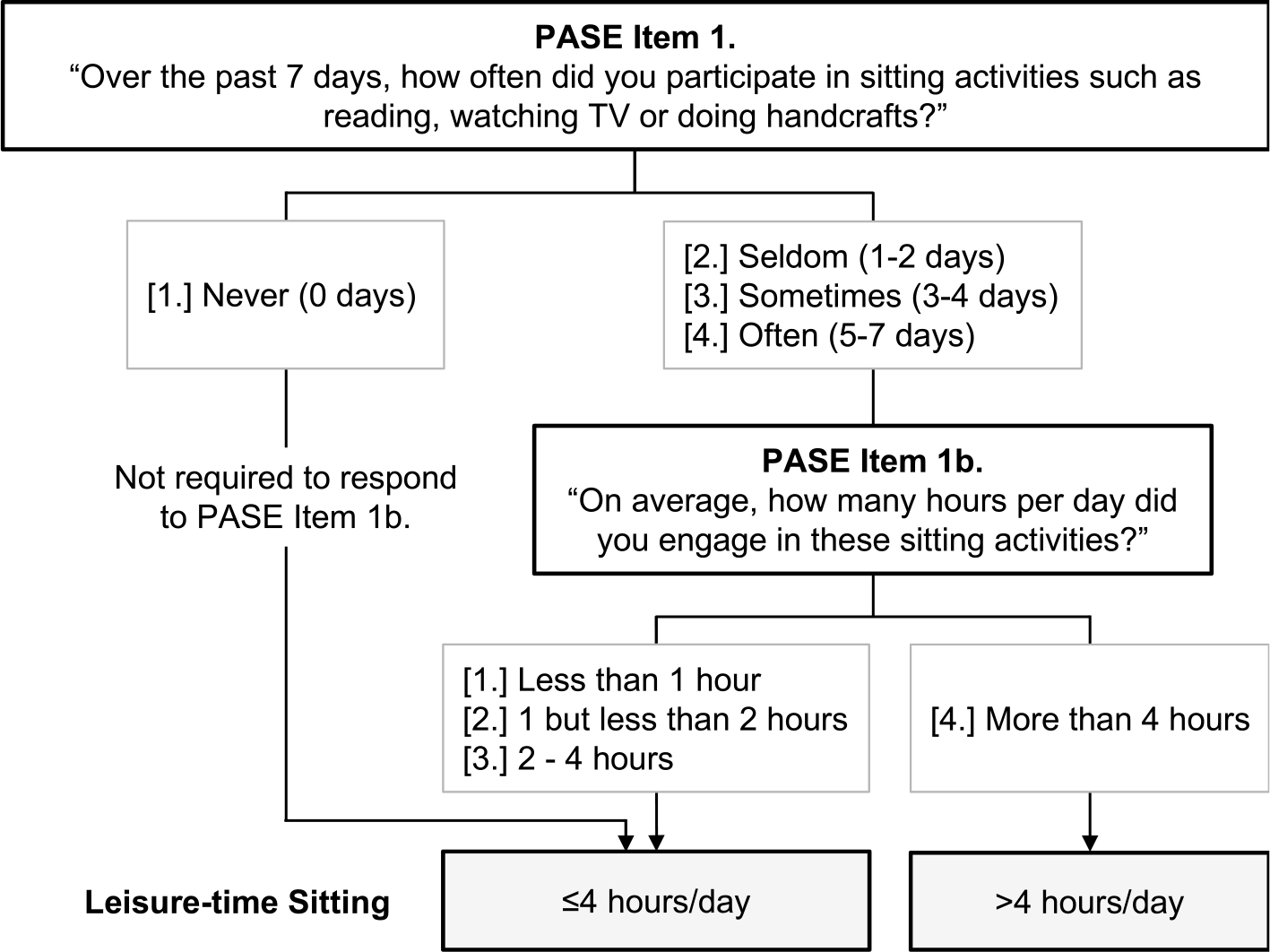
Leisure-time sitting items from the PASE were used to dichotomise participants for the primary analysis. Participants who did not respond to PASE Item 1b were excluded. PASE, Physical Activity Scale for the Elderly.
2.5 |. Effect measure modifier: Worktime sitting at baseline
Participants answered PASE Item 10 to report if they engaged in paid or volunteer work (‘Yes’ or ‘No’). Those who answered ‘Yes’ were prompted to provide additional information about their worktime activities in Item 10b. Participants reported their worktime activities on a 4-point scale: 1. Mainly sitting, 2. Sitting with some standing or walking, 3. Walking with some handling of materials generally weighing less than 50 pounds, 4. Walking and heavy manual work often require handling of materials weighing over 50 pounds. We dichotomised our effect measure modifier variable, worktime sitting, as frequent or infrequent (Figure 2). Participants who responded ‘No’ to PASE Item 10, indicating that they did not work, were excluded from the stratified analysis.
FIGURE 2.

Work items from the PASE questionnaire were used to dichotomise participants for the stratified analysis. Participants who did not respond to PASE Item 10 and/or PASE Item 10b were excluded. PASE, Physical Activity Scale for the Elderly.
2.6 |. Outcome: Radiographic incidence/progression of knee OA from baseline to 2 years
OAI participants had standing, bilateral, posterior-anterior (PA) fixed-flexion radiographs at baseline and at the 2-year follow-up visit. Two expert readers (one rheumatologist and one musculoskeletal radiologist) provided a KL grade for each radiograph. Readers were blinded to each other’s readings, participants’ clinical data, and the chronological order of follow-up radiographs. As participants had bilateral knee radiographs taken at study enrolment, each participant could either contribute one knee (if the other knee was excluded, for reasons listed above) or two knees to our analysis. Thus, we performed knee-specific analyses.
Our outcome, radiographic incidence/progression of knee OA, was dichotomous (Yes/No). The presence of radiographic incidence/progression (Yes) was defined as a full-grade increase in KL grade from baseline to the 2-year follow-up visit. To clarify, our outcome included both radiographic incidence of knee OA (i.e., KL 0–1 at baseline, and KL 2–3 after 2 years) as well as radiographic progression of knee OA (i.e., KL 2–3 at baseline, and an increase in KL grade, or presence of a knee replacement, after 2 years). However, we broadly refer to our outcome as radiographic incidence/progression of knee OA based on KL grade. A cross-sectional reliability study of KL grades in the OAI yielded kappa coefficients ranging from 0.70 to 0.78 (https://nda.nih.gov/oai/).
2.7 |. Potential confounders
We adjusted our analyses for the following potential confounders, given that they may be associated with both sitting time and radiographic knee OA incidence/progression: baseline age (years) (Losina et al., 2013; Matthews et al., 2008), BMI (Du et al., 2019; Jiang et al., 2012); sex (Srikanth et al., 2005; Yang et al., 2019); self-reported leisure-time walking (hours/day), measured via the PASE and dichotomised by the median response (<1 h/day vs. ≥1 h/day) (Dogra & Stathokostas, 2012; Felson et al., 2007; Yang et al., 2019), and baseline KL grade (0–3) (Benichou et al., 2010; Thoma et al., 2018).
2.8 |. Statistical analysis
For our primary analysis, we included all participants who met the study inclusion criteria described above. We examined the relation of leisure-time sitting to knee-specific radiographic incidence/progression of knee OA in the entire study sample using binary linear regression and robust variance estimation to determine risk ratios (RR) and 95% confidence intervals (95% CIs). We also used generalised estimating equations (GEE) to account for the potential correlation of knees belonging to the same participant. We compared those who reported >4 h/day of leisure-time sitting with those who reported ≤4 h/day of leisure-time sitting (referent group), adjusting for the potential confounders listed above.
For our stratified analysis, we excluded participants who did not report their worktime activities (i.e., a missing response to PASE Item 10) or who were ‘Not working’. We stratified the sample by the effect measure modifier, worktime sitting (frequent vs. infrequent). In each stratum, we examined the relation of leisure-time sitting (≤4 h/day vs. >4 h/day) to radiographic incidence/progression of knee OA using a separate binary linear regression model with GEE. That is, we first examined this relationship among those who reported frequent worktime sitting and then examined it among those who reported infrequent worktime sitting. Each model was adjusted for potential confounders, and participants who reported ≤4 h/day of leisure-time sitting served as the referent group. To address the potential for selection bias in our stratified analysis, we described the characteristics of adults who were included as well as excluded from this analysis (Table 1). All analyses were performed using SAS Analytics Software 9.4.
TABLE 1.
Characteristics of participants included in each analysis as well as those excluded from the stratified analysis.
| Characteristic | Primary analysis | Stratified analysis |
Excluded | |
|---|---|---|---|---|
| All n = 4254 | Frequent worktime sitting n = 863 |
Infrequent worktime sitting n = 2142 |
Not working n = 1238 | |
| Age (years) | 61.1 ± 9.1 | 59.1 ± 8.8 | 59.3 ± 8.9 | 65.5 ± 8.3 |
| BMI (kg/m2) | 28.6 ± 4.8 | 28.6 ± 4.9 | 28.4 ± 4.8 | 28.6 ± 4.8 |
| Sex (female) | 2459 (58%) | 452 (53%) | 1257 (59%) | 741 (60%) |
| Leisure-time walking (>1 h/day) | 1869 (44%) | 353 (41%) | 964 (45%) | 546 (44%) |
| Leisure-time sitting | ||||
| ≤4 h/day | 2853 (67%) | 506 (59%) | 1525 (71%) | 812 (66%) |
| ≥4 h/day | 1401 (33%) | 357 (41%) | 617 (29%) | 426 (34%) |
Note: Numbers (n=) represent participants, not knees contributed by those participants. Values are reported as either mean ± SD or n (%).
3 |. RESULTS
3.1 |. Leisure-time sitting and radiographic incidence/progression of knee OA
Our primary analysis included 4254 OAI participants, who contributed 8127 knees (Figure 3). This sample consisted of adults (58% women) aged 61.1 ± 9.1 years (reported as mean standard deviation [SD]) with a BMI of 28.5 ± 4.8 kg/m2 (mean ± SD). About one-third (33%) of the sample reported >4 h/day of leisure-time sitting (Table 1). Forty percent (3241/8127) of the included knees had a baseline KL grade of 0 (Table 2), and by the 2-year follow-up visit, 9.8% (799/8127) of the knees had radiographic incidence/progression (Table 3).
FIGURE 3.

Flow diagram depicting participants (in bold) and knees (in parentheses) excluded from each analysis.
TABLE 2.
Characteristics of knees included in each analysis as well as those excluded from the stratified analysis.
| Characteristic | Primary analysis | Stratified analysis |
Excluded | |
|---|---|---|---|---|
| All n = 8127 | Frequent worktime sitting n = 1655 |
Infrequent worktime sitting n = 4122 |
Not working n = 2330 | |
| KL grade at baseline | ||||
| KL 0 | 3241 (40%) | 736 (44%) | 1675 (41%) | 824 (36%) |
| KL 1 | 1512 (19%) | 294 (18%) | 770 (19%) | 445 (19%) |
| KL 2 | 2222 (27%) | 446 (27%) | 1131 (27%) | 639 (27%) |
| KL 3 | 1152 (14%) | 179 (11%) | 546 (13%) | 422 (18%) |
Note: Numbers (n = ) represent knees contributed by participants. Values are reported as n (%).
Abbreviation: KL, Kellgren-Lawrence.
TABLE 3.
RR and 95% CI for radiographic incidence/progression of OA in knees included in each analysis.
| Worsening ROA (%) |
Unadjusted RR (95% CI) |
Adjusted RR (95% CI) |
|
|---|---|---|---|
| Primary analysis (n = 8127 knees) | |||
| ≤4 h/day sitting n = 5464 knees | 9.1% | 1.0 (REF) | 1.0 (REF) |
| >4 h/day sitting n = 2663 knees | 11.3% | 1.24 (1.07–1.44) | 1.25 (1.08–1.50) |
| Stratified analysis (n = 5777 knees) Frequent worktime sitting (n = 1655 knees) |
|||
| ≤4 h/day sitting n = 972 knees | 7.1% | 1.0 (REF) | 1.0 (REF) |
| >4 h/day sitting n = 683 knees | 11.0% | 1.55 (1.10–2.18) | 1.60 (1.19–2.33) |
| Infrequent worktime sitting (n = 4122 knees) | |||
| ≤4 h/day sitting n = 2939 knees | 9.7% | 1.0 (REF) | 1.0 (REF) |
| >4 h/day sitting n = 1183 knees | 11.4% | 1.17 (0.95–1.45) | 1.11 (0.89–1.39) |
Note: Risk ratios in bold indicate p < 0.05. Adjusted RR were adjusted for age, BMI, sex, self-reported leisure-time walking, and baseline KL grade.
Abbreviations: 95% CI, 95% confidence intervals; OA, osteoarthritis; ROA, radiographic osteoarthritis; RR, risk ratios.
Among adults with >4 h/day of leisure-time sitting, 11.3% of knees (301/2663) had radiographic knee OA incidence/progression, compared with 9.1% (497/5464) of knees in adults with ≤4 h/day of leisure-time sitting (referent group). Therefore, participants with >4 h/day of leisure-time sitting had 1.25 times the risk of radiographic incidence/progression over 2 years compared with those with ≤4 h/day of leisure-time sitting (adjusted RR 1.25, 95% CI 1.08–1.50; Table 3).
3.2 |. Stratified analysis by worktime sitting
Our stratified analysis included 3005 OAI participants who contributed 5777 knees (Figure 3), as we excluded 1238 participants who were ‘Not working’. There were minimal differences in participant characteristics between the two strata (Table 1). Participants who were excluded from this analysis (i.e., ‘Not working’) were older (65.5 ± 8.4 years) than participants who were included (59.3 ± 8.9 years; Table 1), but otherwise their characteristics were similar.
Among participants who reported frequent worktime sitting, those with >4 h/day of leisure-time sitting had 1.6 times the risk of radiographic incidence/progression of knee OA over 2 years compared with ≤4 h/day of leisure-time sitting (adjusted RR 1.60 [1.19–2.33]; Table 3). Conversely, among participants who reported infrequent worktime sitting, leisure-time sitting was not associated with radiographic incidence/progression of knee OA over 2 years (adjusted RR 1.11 [0.89–1.39]; Table 3).
4 |. DISCUSSION
4.1 |. Principal findings
Adults who reported >4 h/day of leisure-time sitting had 25% higher risk for radiographic incidence/progression of knee OA over 2 years, as compared with adults who reported ≤4 h/day of leisure-time sitting. The risk associated with >4 h/day leisure-time sitting was further amplified to 60% higher among adults who also reported frequent worktime sitting. Based on these findings, higher sitting time may have a modest negative impact on the structural integrity of the knees. We propose that adults who regularly favour sitting (over standing/walking) may subject their knees to ‘underloading’ (Kutzner et al., 2010), which in turn leads to knee cartilage atrophy (Bader et al., 2011; Nomura et al., 2017; Wallace et al., 2019) and likely knee OA incidence/progression.
We recognise that while these adults favour sitting, they can still engage in other activities (such as standing and walking) when they are not sitting. We adjusted our analyses for self-reported leisure-time walking, given that walking is the most common type of activity in this population (Hulteen et al., 2017), although we recognise that leisure-time walking is not a proxy for overall PA. Our findings indicated that regardless of engagement in leisure-time walking (<1 h/day vs. >1 h/day), higher leisure-time sitting was associated with a 25% increase in one’s risk of radiographic knee OA incidence/progression.
The findings of our stratified analysis revealed that among adults who reported infrequent worktime sitting (i.e., who also engaged in standing and/or walking during worktime), >4 h/day of leisure-time sitting did not increase their risk of radiographic knee OA incidence/progression. It seems that their engagement in physical activity during worktime negated their risk associated with higher leisure-time sitting, whereas engagement in >1 h/day of leisure-time walking (per our primary analysis) did not negate said risk.
4.2 |. Strengths and weaknesses of the current study, in relation to other studies
The most notable strength of this study is its innovation; our study is one of few to consider that high levels of sitting, and potential ‘underloading’ may increase one’s risk of incidence/progression of knee OA. In contrast, nearly all previous studies presumed that adults with high sitting have the lowest risk of OA incidence/progression, so these adults were selected as the referent group (Ezzat & Li, 2014; Wang et al., 2020). Thus, the potential risk associated with ‘underloading’ has rarely been examined and has gone unrecognised.
A recent study by Chang et al. examined 8-year trajectories of leisure-time sitting with incident knee OA over that same period in a subset of OAI participants (n = 1194) (Chang et al., 2020). They found a non-significant dose-response relationship whereby adults with ‘low sitting’ and ‘moderate sitting’ had lower odds of incident knee OA (unadjusted odds ratios of 0.86 [0.49–1.51] and 0.97 [0.54–1.75], respectively) than adults with ‘high sitting’ (referent group). While their referent group (‘high sitting’) was opposite to ours (≤4 h/day, or ‘low sitting’), our findings are generally aligned; in both studies, adults with higher leisure-time sitting had the highest odds for incident knee OA and higher risk for short-term knee OA incidence/progression. However, it should be noted that this study by Chang et al. used a cross-sectional design (i.e., the exposure and outcome were evaluated over the same 8-year period), did not adjust for leisure-time physical activity, and did not consider the potential contribution of worktime sitting.
In contrast, our study used a longitudinal design; the exposure (self-reported sitting) was assessed at baseline, and preceded the outcome (radiographic incidence/progression from baseline to 2 years later). We also included nearly all OAI participants (4254 of 4796 total participants) with varying severity of knee OA at baseline (KL grades 0–3), and we adjusted our analyses for time spent in self-reported leisure-time walking. Finally, our study considered multiple contexts of sitting (leisure-time and worktime), thus providing a more comprehensive estimate of overall sitting time.
Other previous studies used measures of sedentary time, which includes both sitting and standing, as their exposures. A strength of the current study is that our exposure captures only sitting, while surrogate measures (e.g., sedentary time, TV-viewing time) do not (Stamatakis et al., 2019). However, these studies still concluded that higher sedentary time was associated with knee pain (Lee et al., 2019), poor function (Lee et al., 2015), and disability (Dunlop et al., 2015) in adults with knee OA. Our study provides evidence that another major outcome in knee OA, radiographic incidence/progression, may be related to sitting. That is, higher levels of sitting (as the primary component of sedentary time) may be detrimental to adults in nearly every facet of this disease: symptoms, function, disability, and structure.
We want to acknowledge some limitations of this study. First, our measures of leisure- and work - time sitting were self-reported via the PASE questionnaire. Self-report measures can be subject to recall bias (Healy et al., 2011) and sex-specific differences (Dyrstad et al., 2014), which are often overcome through activity monitoring. Unfortunately, most activity monitors do not accurately measure sitting time, so cohort studies (like the OAI) use self-report measures (Garcia et al., 2019; Piirtola et al., 2014) for their convenience and acceptable validity (Gupta et al., 2016).
Second, the validity and test-retest reliability of individual PASE items has not been established; however, sitting items in other self-report measures (similar to the PASE) have demonstrated construct validity compared to accelerometry (Pedersen et al., 2016; Rosenberg et al., 2008). Third, we restricted our length of follow-up to 2 years, despite the availability of additional OAI follow-up data. This was done because we were specifically interested in the near-term effects of leisure- and work-time sitting, and anticipated that leisure- and work - time sitting may change over time. Fourth, our findings are generalisable only to adults with characteristics similar to our study sample. However, we expanded the generalisability of our findings by including adults without knee OA (KL 0–1) and adults with mild-to-moderate knee OA (KL 2–3) in our study sample.
4.3 |. Unanswered questions and future research
The current study sheds light on an important question regarding the potential risk of high sitting among adults with knee OA, but future studies should more comprehensively examine how engaging in physical activity might attenuate this risk. In addition, future prospective studies should use an activity monitor that accurately identifies and measures sitting time (Byrom et al., 2016) so that they might overcome the limitations of self-reported sitting items.
4.4 |. Meaning of the study: Possible implications for clinicians and policymakers
Today, many clinicians (and consequently, their patients) think of sitting as a relatively benign activity for adults with knee OA, particularly in terms of structural incidence/progression. However, our study findings indicate that this may not be the case. Thus, we advocate that clinicians should recommend ‘sitting less’ to patients with or at risk knee OA, and more broadly, to all patients who engage in high leisure-time sitting, which is consistent with current public health guidelines (Piercy et al., 2018).
Clinicians can begin by asking patients how much time they spend sitting during leisure-time and worktime. Then, they can identify adults who engage in substantial leisure-time and worktime sitting, as they have the greatest need for education regarding the importance of ‘sitting less’. To this end, clinicians can draw on our study findings along with the larger body of evidence that recognises sitting as a potent risk factor for chronic disease. Perhaps more importantly, clinicians can benefit from the novelty of our study findings. We demonstrated that sitting may be a salient risk factor for knee OA incidence and progression, which can have significant implications for the prevention and management of this disease.
ACKNOWLEDGEMENTS
We want to acknowledge and thank all OAI participants for their contributions to this research. The OAI is a public-private partnership comprised of five contracts funded by the National Institutes of Health (NIH) and National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS). Private funding partners include Merck Research Laboratories, Novartis Pharmaceuticals Corporation, GlaxoSmithKline, and Pfizer, Inc. The authors received funding from NIH T32-HD007490 (Voinier), Foundation for Physical Therapy Research Promotion of Doctoral Studies I Scholarship (Voinier), NIH K24-AR070892 (Neogi), and NIH/NIAMS R21-AR07079 (White). These findings were published as a conference abstract from the 2019 American College of Rheumatology Annual Meeting in an online supplement of Arthritis and Rheumatology. They were also published in the doctoral dissertation of Dana Voinier, which is entitled “The effects of physical activity on structural worsening of knee osteoarthritis.”
Footnotes
CONFLICT OF INTEREST STATEMENT
All authors have completed the ICMJE uniform disclosure form at http://www.icmje.org/disclosure-of-interest/ and declare Dana Voinier, Tuhina Neogi, Louise M. Thoma, and Daniel K. White received research grants from the National Institutes of Health (NIH) for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
ETHICS STATEMENT
The study was approved by the Institutional Review Board at the University of Delaware. Informed consent and Institutional Review Board approval were obtained from each clinic site from the OAI. In particular, all study participants provided written informed consent before enrolment in the OAI.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available in the NDA at https://nda.nih.gov/oai/. These data were derived from the following resources available in the public domain: OAI Data, https://nda.nih.gov/oai/.
REFERENCES
- Bader DL, Salter DM, & Chowdhury TT (2011). Biomechanical influence of cartilage homeostasis in health and disease. Arthritis, 2011, 979032–979116. 10.1155/2011/979032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benichou OD, Hunter DJ, Nelson DR, Guermazi A, Eckstein F, Kwoh K, Myers SL, Wirth W, & Duryea J (2010). One-year change in radiographic joint space width in patients with unilateral joint space narrowing: Data from the osteoarthritis initiative. Arthritis Care and Research, 62(7), 924–931. 10.1002/acr.20149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrom B, Stratton G, Mc Carthy M, & Muehlhausen W (2016). Objective measurement of sedentary behaviour using accelerometers. International Journal of Obesity, 40(11), 1809–1812. 10.1038/ijo.2016.136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang AH, Lee JJ, Chmiel JS, Almagor O, Song J, & Sharma L (2020). Association of long-term strenuous physical activity and extensive sitting with incident radiographic knee osteoarthritis. JAMA Network Open, 3(5), e204049. 10.1001/jamanetworkopen.2020.4049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dogra S, & Stathokostas L (2012). Sedentary behavior and physical activity are independent predictors of successful aging in middle-aged and older adults. Journal of Aging Research, 2012, 190654–190658. 10.1155/2012/190654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du Y, Liu B, Sun Y, Snetselaar LG, Wallace RB, & Bao W (2019). Trends in adherence to the physical activity guidelines for Americans for aerobic activity and time spent on sedentary behavior among US adults, 2007 to 2016. JAMA Network Open, 2(7), e197597. 10.1001/jamanetworkopen.2019.7597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunlop DD, Song J, Arnston EK, Semanik PA, Lee J, Chang RW, & Hootman JM (2015). Sedentary time in US older adults associated with disability in activities of daily living independent of physical activity. Journal of Physical Activity and Health, 12(1), 93–101. 10.1123/jpah.2013-0311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunlop DD, Song J, Semanik PA, Chang RW, Sharma L, Bathon JM, Eaton CB, Hochberg MC, Jackson RD, Kwoh CK, Mysiw WJ, Nevitt MC, & Hootman JM (2011). Objective physical activity measurement in the osteoarthritis initiative: Are guidelines being met? Arthritis and Rheumatism, 63(11), 3372–3382. 10.1002/art.30562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunstan DW, Barr ELM, Healy GN, Salmon J, Shaw JE, Balkau B, Magliano D, Cameron A, Zimmet P, & Owen N (2010). Television viewing time and mortality: The Australian diabetes, obesity and lifestyle study (AusDiab). Circulation, 121(3), 384–391. 10.1161/circulationaha.109.894824 [DOI] [PubMed] [Google Scholar]
- Dyrstad SM, Hansen BH, Holme IM, & Anderssen SA (2014). Comparison of self-reported versus accelerometer-measured physical activity. Medicine and Science in Sports and Exercise, 46(1), 99–106. 10.1249/mss.0b013e3182a0595f [DOI] [PubMed] [Google Scholar]
- Ezzat AM, & Li LC (2014). Occupational physical loading tasks and knee osteoarthritis: A review of the evidence. Physiotherapie Canada, 66(1), 91–107. 10.3138/ptc.2012-2045BC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fawaz-Estrup F (2004). The osteoarthritis initiative: An overview. Medicine and Health Rhode Island, 87(6), 169–171. [PubMed] [Google Scholar]
- Felson DT, Lawrence RC, Dieppe PA, Hirsch R, Helmick CG, Jordan JM, & Fries JF (2000). Osteoarthritis: New insights. Part 1: The disease and its risk factors. Annals of Internal Medicine, 133(8), 635–646. 10.7326/0003-4819-133-8-200010170-00016 [DOI] [PubMed] [Google Scholar]
- Felson DT, & Nevitt MC (2004). Epidemiologic studies for osteoarthritis: New versus conventional study design approaches. Rheumatic Diseases Clinics of North America, 30(4), 783–797. vii. 10.1016/j.rdc.2004.07.005 [DOI] [PubMed] [Google Scholar]
- Felson DT, Niu J, Clancy M, Sack B, Aliabadi P, & Zhang Y (2007). Effect of recreational physical activities on the development of knee osteoarthritis in older adults of different weights: The Framingham study. Arthritis and Rheumatism, 57(1), 6–12. 10.1002/art.22464 [DOI] [PubMed] [Google Scholar]
- Garcia JM, Duran AT, Schwartz JE, Booth JN 3rd, Hooker SP, Willey JZ, Cheung YK, Park C, Williams SK, Sims M, Shimbo D, & Diaz KM (2019). Types of sedentary behavior and risk of cardiovascular events and mortality in blacks: The Jackson heart study. Journal of the American Heart Association, 8(13), e010406. 10.1161/jaha.118.010406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta N, Heiden M, Aadahl M, Korshøj M, Jørgensen MB, & Holtermann A (2016). What is the effect on obesity indicators from replacing prolonged sedentary time with brief sedentary bouts, standing and different types of physical activity during working days? A cross-sectional accelerometer-based study among blue-collar workers. PLoS One, 11(5), e0154935. 10.1371/journal.pone.0154935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawker GA (2019). Osteoarthritis is a serious disease. Clinical and Experimental Rheumatology, 37(Suppl 120), 3–6. [PubMed] [Google Scholar]
- Healy GN, Clark BK, Winkler EAH, Gardiner PA, Brown WJ, & Matthews CE (2011). Measurement of adults’ sedentary time in population-based studies. American Journal of Preventive Medicine, 41(2), 216–227. 10.1016/j.amepre.2011.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hulteen RM, Smith JJ, Morgan PJ, Barnett LM, Hallal PC, Colyvas K, & Lubans DR (2017). Global participation in sport and leisure-time physical activities: A systematic review and meta-analysis. Preventive Medicine, 95, 14–25. 10.1016/j.ypmed.2016.11.027 [DOI] [PubMed] [Google Scholar]
- Jiang L, Tian W, Wang Y, Rong J, Bao C, Liu Y, Zhao Y, & Wang C (2012). Body mass index and susceptibility to knee osteoarthritis: A systematic review and meta-analysis. Joint, Bone, Spine, 79(3), 291–297. 10.1016/j.jbspin.2011.05.015 [DOI] [PubMed] [Google Scholar]
- Katzmarzyk PT, Church TS, Craig CL, & Bouchard C (2009). Sitting time and mortality from all causes, cardiovascular disease, and cancer. Medicine and Science in Sports and Exercise, 41(5), 998–1005. 10.1249/mss.0b013e3181930355 [DOI] [PubMed] [Google Scholar]
- Kellgren JH, & Lawrence JS (1957). Radiological assessment of osteoarthrosis. Annals of the Rheumatic Diseases, 16(4), 494–502. 10.1136/ard.16.4.494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kutzner I, Heinlein B, Graichen F, Bender A, Rohlmann A, Halder A, Beier A, & Bergmann G (2010). Loading of the knee joint during activities of daily living measured in vivo in five subjects. Journal of Biomechanics, 43(11), 2164–2173. 10.1016/j.jbiomech.2010.03.046 [DOI] [PubMed] [Google Scholar]
- Lee J, Chang RW, Ehrlich-Jones L, Kwoh CK, Nevitt M, Semanik PA, Sharma L, Sohn MW, Song J, & Dunlop DD (2015). Sedentary behavior and physical function: Objective evidence from the osteoarthritis initiative. Arthritis Care & Research, 67(3), 366–373. 10.1002/acr.22432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S-H, Son C, Yeo S, & Ha I-H (2019). Cross-sectional analysis of self-reported sedentary behaviors and chronic knee pain among South Korean adults over 50 years of age in KNHANES 2013–2015. BMC Public Health, 19(1), 1375. 10.1186/s12889-019-7653-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lester G (2008). Clinical research in OA–The NIH osteoarthritis initiative. Journal of Musculoskeletal and Neuronal Interactions, 8(4), 313–314. [PubMed] [Google Scholar]
- Losina E, Silva GS, Smith KC, Collins JE, Hunter DJ, Shrestha S, Messier SP, Yelin EH, Suter LG, Paltiel AD, & Katz JN (2020). Quality-adjusted life-years lost due to physical inactivity in a US population with osteoarthritis. Arthritis Care and Research, 72(10), 1349–1357. 10.1002/acr.24035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Losina E, Weinstein AM, Reichmann WM, Burbine SA, Solomon DH, Daigle ME, Rome BN, Chen SP, Hunter DJ, Suter LG, Jordan JM, & Katz JN (2013). Lifetime risk and age at diagnosis of symptomatic knee osteoarthritis in the US. Arthritis Care and Research, 65(5), 703–711. 10.1002/acr.21898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin KA, Rejeski WJ, Miller ME, James MK, Ettinger WH Jr., & Messier SP (1999). Validation of the PASE in older adults with knee pain and physical disability. Medicine and Science in Sports and Exercise, 31(5), 627–633. 10.1097/00005768-199905000-00001 [DOI] [PubMed] [Google Scholar]
- Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, & Troiano RP (2008). Amount of time spent in sedentary behaviors in the United States, 2003–2004. American Journal of Epidemiology, 167(7), 875–881. 10.1093/aje/kwm390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nomura M, Sakitani N, Iwasawa H, Kohara Y, Takano S, Wakimoto Y, Kuroki H, & Moriyama H (2017). Thinning of articular cartilage after joint unloading or immobilization. An experimental investigation of the pathogenesis in mice. Osteoarthritis and Cartilage/OARS, Osteoarthritis Research Society, 25(5), 727–736. 10.1016/j.joca.2016.11.013 [DOI] [PubMed] [Google Scholar]
- Palmer VJ, Gray CM, Fitzsimons CF, Mutrie N, Wyke S, Deary IJ, Der G, Chastin SF, & Skelton DA; Seniors USP Team. (2019). What do older people do when sitting and why? Implications for decreasing sedentary behavior. The Gerontologist, 59(4), 686–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel AV, Bernstein L, Deka A, Feigelson HS, Campbell PT, Gapstur SM, Colditz GA, & Thun MJ (2010). Leisure time spent sitting in relation to total mortality in a prospective cohort of US adults. American Journal of Epidemiology, 172(4), 419–429. 10.1093/aje/kwq155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel AV, Maliniak ML, Rees-Punia E, Matthews CE, & Gapstur SM (2018). Prolonged leisure time spent sitting in relation to cause-specific mortality in a large US cohort. American Journal of Epidemiology, 187(10), 2151–2158. 10.1093/aje/kwy125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen SJ, Kitic CM, Bird M-L, Mainsbridge CP, & Cooley PD (2016). Is self-reporting workplace activity worthwhile? Validity and reliability of occupational sitting and physical activity questionnaire in desk-based workers. BMC Public Health, 16(1), 836. 10.1186/s12889-016-3537-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, George SM, & Olson RD (2018). The physical activity guidelines for Americans. JAMA, 320(19), 2020–2028. 10.1001/jama.2018.14854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piirtola M, Kaprio J, & Ropponen A (2014). A study of sedentary behaviour in the older Finnish twin cohort: A cross sectional analysis. BioMed Research International, 2014, 209140–209149. 10.1155/2014/209140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg DE, Bull FC, Marshall AL, Sallis JF, & Bauman AE (2008). Assessment of sedentary behavior with the international physical activity questionnaire. Journal of Physical Activity and Health, 5(Suppl 1), S30–S44. 10.1123/jpah.5.s1.s30 [DOI] [PubMed] [Google Scholar]
- Shrestha N, Kukkonen-Harjula KT, Verbeek JH, Ijaz S, Hermans V, & Pedisic Z (2018). Workplace interventions for reducing sitting at work. Cochrane Database of Systematic Reviews, 12(12), CD010912. 10.1002/14651858.cd010912.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srikanth VK, Fryer JL, Zhai G, Winzenberg TM, Hosmer D, & Jones G (2005). A meta-analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthritis and Cartilage/OARS, Osteoarthritis Research Society, 13(9), 769–781. 10.1016/j.joca.2005.04.014 [DOI] [PubMed] [Google Scholar]
- Stamatakis E, Ekelund U, Ding D, Hamer M, Bauman AE, & Lee I-M (2019). Is the time right for quantitative public health guidelines on sitting? A narrative review of sedentary behaviour research paradigms and findings. British Journal of Sports Medicine, 53(6), 377–382. 10.1136/bjsports-2018-099131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun HB (2010). Mechanical loading, cartilage degradation, and arthritis. Annals of the New York Academy of Sciences, 1211(1), 37–50. 10.1111/j.1749-6632.2010.05808.x [DOI] [PubMed] [Google Scholar]
- Svege I, Kolle E, & Risberg MA (2012). Reliability and validity of the physical activity scale for the elderly (PASE) in patients with hip osteoarthritis. BMC Musculoskeletal Disorders, 13(1), 26. 10.1186/1471-2474-13-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoma LM, Dunlop D, Song J, Lee J, Tudor-Locke C, Aguiar EJ, Master H, Christiansen MB, & White DK (2018). Are older adults with symptomatic knee osteoarthritis less active than the general population? Analysis from the osteoarthritis initiative and the national health and nutrition examination survey. Arthritis Care and Research, 70(10), 1448–1454. 10.1002/acr.23511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Uffelen JGZ, Wong J, Chau JY, van der Ploeg HP, Riphagen I, Gilson ND, Burton NW, Healy GN, Thorp AA, Clark BK, Gardiner PA, Dunstan DW, Bauman A, Owen N, & Brown WJ (2010). Occupational sitting and health risks: A systematic review. American Journal of Preventive Medicine, 39(4), 379–388. 10.1016/j.amepre.2010.05.024 [DOI] [PubMed] [Google Scholar]
- Wallace IJ, Bendele AM, Riew G, Frank EH, Hung H-H, Holowka NB, Bolze A, Venable E, Yegian A, Dingwall H, Carmody R, Grodzinsky A, & Lieberman DE (2019). Physical inactivity and knee osteoarthritis in Guinea pigs. Osteoarthritis and Cartilage/OARS, Osteoarthritis Research Society, 27(11), 1721–1728. 10.1016/j.joca.2019.07.005 [DOI] [PubMed] [Google Scholar]
- Wang X, Perry TA, Arden N, Chen L, Parsons CM, Cooper C, Gates L, & Hunter DJ (2020). Occupational risk in knee osteoarthritis: A systematic review and meta-analysis of observational studies. Arthritis Care and Research, 72(9), 1213–1223. 10.1002/acr.24333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washburn RA, McAuley E, Katula J, Mihalko SL, & Boileau RA (1999). The physical activity scale for the elderly (PASE): Evidence for validity. Journal of Clinical Epidemiology, 52(7), 643–651. 10.1016/s0895-4356(99)00049-9 [DOI] [PubMed] [Google Scholar]
- Yang L, Cao C, Kantor ED, Nguyen LH, Zheng X, Park Y, Giovannucci EL, Matthews CE, Colditz GA, & Cao Y (2019). Trends in sedentary behavior among the US population, 2001–2016. JAMA, 321(16), 1587–1597. 10.1001/jama.2019.3636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young DR, Hivert M-F, Alhassan S, Camhi SM, Ferguson JF, & Katzmarzyk PT (2016). Physical activity committee of the council on lifestyle and cardiometabolic health; council on clinical cardiology; council on epidemiology and prevention; council on functional genomics and translational biology; and stroke council. sedentary behavior and cardiovascular morbidity and mortality: A science advisory from the American heart association. Circulation, 134(13), e262–e279. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available in the NDA at https://nda.nih.gov/oai/. These data were derived from the following resources available in the public domain: OAI Data, https://nda.nih.gov/oai/.


