Abstract
Surgery on spinal tumors becomes challenging when the tumor is ventral to the spinal cord. Conventionally, we approach it posteriorly through bilateral laminectomy and rotate the cord after sectioning the dentate ligament and nerve roots. However, manipulating the cord can be hazardous, and a long bilateral laminectomy can be invasive. Meanwhile, a narrow operative field and a limited lateral viewing angle in a unilateral approach constrained the surgeon. To overcome these problems, we previously reported a technique of modified unilateral approach where we incised the skin and the fascia horizontally and placed a pair of retractors longitudinally.
The current article reports our experience applying this approach in 15 patients with ventrally located spinal tumors. The approach was performed on 10 schwannomas, 2 meningiomas, and 3 others. We evaluated paraspinal muscle atrophy on postoperative magnetic resonance imaging.
The modified unilateral approach provided an excellent surgical field for removing ventrally located tumors. Gross total removal was achieved in 11 patients (92% of benign tumors). No neurological complications occurred except for one case of transient weakness. We encountered no wound-related late complications such as pain or deformity. The reduction of the cross-sectional area of the paraspinal muscles on the approach side (compared to the nonapproach side) was 0.93 (95% confidence interval: 0.72-1.06), indicating 7% atrophy (statistically nonsignificant, p = 0.48).
We believe this simple technique can be useful for removing spinal tumors located ventral to the spinal cord.
Keywords: spinal tumor, spinal meningioma, spinal schwannoma, surgical technique
Introduction
Ventrally located spinal tumors are challenging in surgery. Conventionally, we rotate the spinal cord by sectioning the dentate ligament and nerve roots.1,2) However, it poses some risk to the spinal cord1,2) and is not feasible when the function of the nerve roots is important or there is a radiculomedullary artery. It also requires a long bilateral laminectomy, while a less-invasive unilateral approach would be preferable. However, in the unilateral approach, the lateral viewing angle is limited by the skin, muscle, and retractor blade. Inserting instruments is also constrained to relatively perpendicular angles.
Previously, we published a case report describing a simple technique to solve these problems.3) The technique consisted of a horizontal skin incision, unilateral laminar exposure, horizontal fascial incision, longitudinal retraction of the paraspinal muscles, and unilateral laminotomy. This modified unilateral approach provided a wide surgical field with a good lateral viewing angle to remove a ventrally located meningioma at the C2 level. The ability to insert instruments from lateral angles greatly facilitated the safe removal of the tumor. This approach was quite effective, but its safety in a wide range of patients is inconclusive. In particular, a long-term effect on the paraspinal muscles was a concern.
This article describes our experience applying this approach in 15 patients with ventrally or ventrolaterally located tumors. In addition, we have described our findings on follow-up magnetic resonance imaging (MRI) indicating paraspinal-muscle atrophy.
Materials and Methods
Study design
This study is a retrospective observational study of a consecutive case series at a single teaching hospital. The institutional review board approved the study protocol and informed consent (No. 21R179). Consecutive patients who underwent removal of ventrally or ventrolaterally located spinal tumors from December 2015 to June 2022 were included in the study. The first author (a neurosurgeon with over 30 years of experience) operated on all the patients and followed all the patients after surgery at the outpatient clinic. The patients' outcome was evaluated using the McCormick score4) (Supplementary Table 1) at the last clinical visit. The atrophy of the paraspinal muscles was evaluated with the last follow-up MRI.
Operative technique
We call this approach the modified unilateral approach in this article. Figure 1 shows the details of this approach. We first made a 7-10-cm horizontal skin incision crossing the midline so that approximately two-thirds of the incision lay on the ipsilateral side (Fig. 1A). We then performed a subperiosteal dissection of the ipsilateral spinous processes and laminae (Fig. 1A). Next, we made a horizontal incision on the dorsal fascia that covered the ipsilateral paraspinal muscles (Fig. 1B). This fascial incision facilitated the retraction of the muscles. We then placed a pair of retractors on the paraspinal muscles and retracted them in the longitudinal direction with the blades kept in oblique angles (Fig. 1C). A small incision on the most medial portion of the muscle was usually needed to facilitate retraction (Fig. 1C). The length of the muscle incision decreased as we became more experienced. This preparation exposed the unilateral laminae with an excellent lateral viewing angle. The tumor was then approached with unilateral laminotomy (Fig. 1D). The surgeon could manipulate the ventrally located tumor with minimal spinal cord retraction. He could insert the instruments from the lateral angles while maintaining a natural, comfortable posture (Fig. 1D).
Fig. 1.
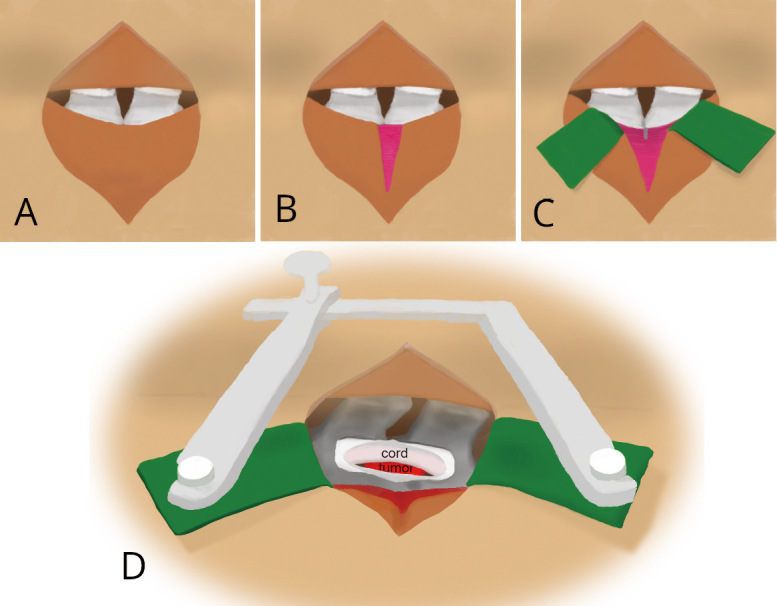
Schemas showing the operative technique. A: We made a horizontal skin incision crossing the midline to dissect the unilateral laminae. B: We then made a horizontal incision on the dorsal fascia. C: After retracting the ipsilateral paraspinal muscles longitudinally, a small incision was made on the most medial portion of the muscle (gray line). D: We held the paraspinal muscles with a pair of retractors placed longitudinally and approached the tumor from a lateral viewing angle through a minimal unilateral laminotomy.
After tumor removal, we grossly reapproximated the length of the muscle incision and sutured the fascia in a usual fashion (Supplementary Video 1).
Evaluation of paraspinal muscle atrophy
The spine MRI at the last follow-up visit was analyzed for paraspinal muscle atrophy. The mean follow-up period for imaging was 39.3 months (standard deviation (SD) = 60.8). The axial T2-weighted image at the surgical level was loaded into ImageJ software (version 1.53, National Institute of Health, USA), and the regions of interest (ROI) were manually set to the paraspinal muscles on both sides. The ROI included the multifidus muscles in the thoracic and lumbar spine and the multifidus/semispinalis cervicis muscles in the cervical spine5) (Supplementary Figure 1). The image specifications were then adjusted to only display the muscle tissue. Then, the cross-sectional area of the muscle in each ROI was measured. Using the contralateral side, untouched during surgery, as the control, the cross-sectional area ratio (approach-side to nonapproach-side area) was calculated. This ratio was transformed with the logarithmic function and analyzed with Student's t-test. The mean value and the 95% confidence interval were then transformed back to the actual value with the exponential function.
Evaluation of postoperative pain
From June 2016 to August 2017, we administered a short survey on postoperative pain. We asked patients who underwent surgery for spinal tumors (intradural schwannomas or meningiomas) to score their postoperative wound pain using the visual analog scale (VAS). We compared the scores between the two groups: those who underwent the modified unilateral approach and those who underwent the standard bilateral laminectomy. The first author chose the surgical approach (standard or paramedian). The scores were compared with Student's t-test.
Statistical analysis
R (version 4.2, The R Foundation for Statistical Computing, Vienna, Austria, https://www.R-project.org/) was used for statistical calculations on a personal computer. A p-value less than 0.05 was considered statistically significant.
Results
Case series
We performed the modified unilateral approach on 15 patients with ventral or ventrolateral spinal tumors during the study period. Table 1 shows the detailed information of the series. There were 5 men and 10 women with a mean age of 53.6 years and a SD of 22.5 years. The median follow-up period was 53 months (25th quartile = 22 months, 75th quartile = 66 months, range: 6-86). The series included 10 schwannomas, 2 meningiomas, and 3 others. There were 7 cervical, 6 thoracic, and 2 lumbar lesions. Case 1 has been previously reported as a case report.3)
Table 1.
Summary of the Series
| Case | Age | sex | Location | Pathology | Extent of Resection | follow-up (months) | McCormick |
|---|---|---|---|---|---|---|---|
| 1 | 79 | f | Cervical | meningioma | gross total | 86 | I |
| 2 | 69 | f | Cervical | schwannoma | subtotal | 74 | I |
| 3 | 2 | m | Cervical | DSRCT | subtotal | 12 | death |
| 4 | 76 | f | Cervical | schwannoma | gross total | 70 | I |
| 5 | 60 | f | Cervical | meningioma | gross total | 66 | I |
| 6 | 56 | m | Lumbar | schwannoma | gross total | 66 | I |
| 7 | 77 | f | Thoracic | meningioma | gross total | 66 | I |
| 8 | 70 | f | Thoracic | schwannoma | gross total | 61 | I |
| 9 | 37 | f | Lumbar | schwannoma | gross total | 53 | I |
| 10 | 31 | f | Thoracic | germ cell tumor | subtotal | 40 | IV |
| 11 | 60 | f | Cervical | schwannoma | subtotal | 37 | I |
| 12 | 18 | m | Thoracic | germ cell tumor | gross total | 23 | I |
| 13 | 50 | m | Thoracic | schwannoma | gross total | 21 | I |
| 14 | 72 | f | Thoracic | schwannoma | gross total | 18 | II |
| 15 | 57 | m | Thoracic | schwannoma | gross total | 6 | I |
DSRCT: desmoplastic small round-cell tumor
Representative cases
Case 13
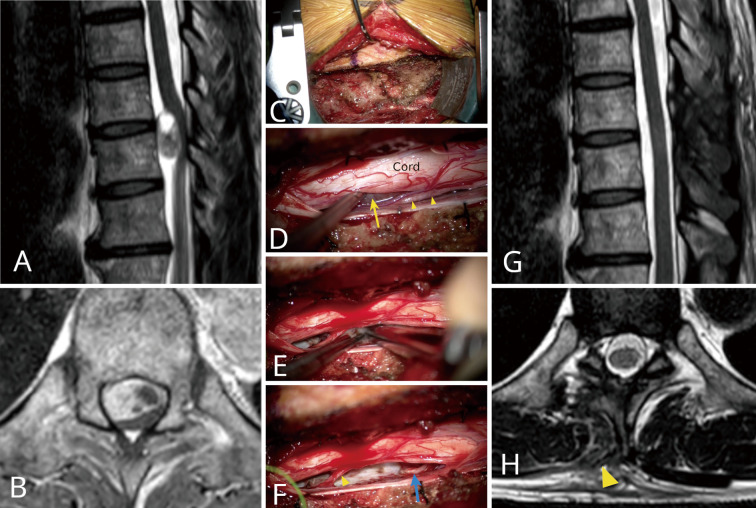
A 50-year-old man complained of severe pain radiating to his bilateral flank areas. He also had a mild gait disturbance. Neurological exams showed hypesthesia below the level of T9, hyperreflexia, and positive Babinski signs in both lower extremities. Thoracic-spine MRI revealed a mass lesion on the ventral side of the spinal cord at T9/10 (Fig. 2A). This lesion was inhomogeneously enhanced after gadolinium administration (Fig. 2B).
Fig. 2.
Case 13. A: A T2-weighted sagittal image showing a round, well-demarcated mass at the level of T10. B: A T1-weighted axial image showing the mass located on the ventral side of the spinal cord, severely compressing toward the dorsal side. C: Exposure of the right T9 and T10 laminae. D: Exposure of the tumor on the ventral side of the cord. Arrow: tumor, arrowheads: right T10 posterior root, E: Internal tumor decompression with an ultrasonic aspirator. F: After removal of the tumor. Arrowhead: right T10 posterior root. Blue arrow: Right T10 motor root (tumor origin). G: Postoperative MRI (T2-weighted sagittal image). H: Postoperative MRI (T2-weighted axial image). Note the minimal damage to the paraspinal muscles (arrowhead).
The surgical video of this case is available in Supplementary Video 1. We chose the modified unilateral approach for this ventrally located tumor (Fig. 2C). A unilateral hemilaminotomy of T9 and partial hemilaminectomy of T10 were performed with medial facetectomy up to the medial aspect of the pedicles. After the dura was opened, most of the tumor was invisible due to being covered by the spinal cord (Fig. 2D). We removed the tumor through a small space on the lateral side of the cord, repeating internal decompression and tumor extraction (Fig. 2E). The modified unilateral approach provided a wide and bright operative field with an excellent lateral viewing angle for the gross total tumor removal with minimal cord retraction (Fig. 2F). We removed only the medial portion of the facet joint, so fixation was unnecessary. The patient showed good neurological recovery. The pathology indicated a schwannoma. The severity of his postoperative wound pain was equivalent to that of other posterior approaches. He complained of no wound-related symptoms thereafter. Gross total removal was confirmed on a postoperative MRI (Fig. 2GH). The patient returned to normal activities and was doing well 21 months after surgery.
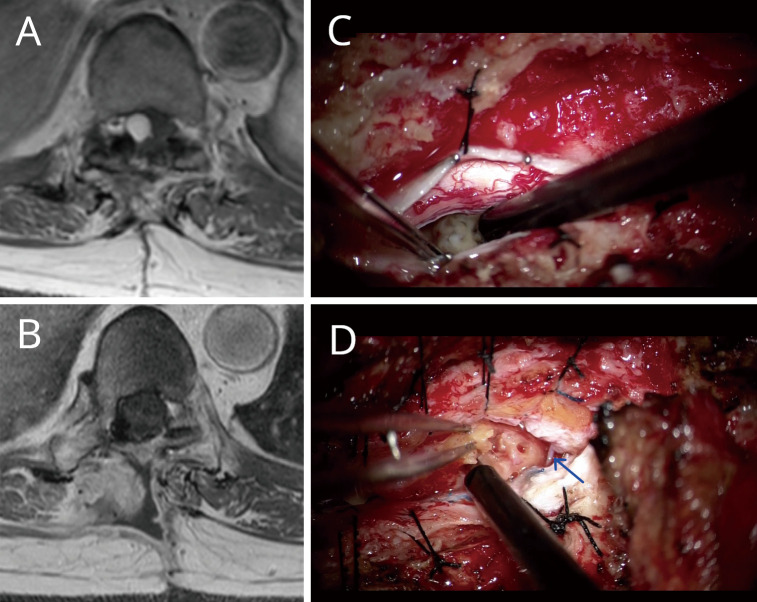
Case 14
This recurrent case of spinal schwannoma was effectively treated with the modified unilateral approach (Fig. 3ABCD). The patient had undergone the removal of a ventrally located thoracic spinal schwannoma at T10 at another hospital. The surgery ended in partial removal. Twenty years later, the tumor recurred, and we performed a reoperation with the standard posterior approach. The tumor was located on the right ventrolateral side of the spinal cord (Fig. 3A). The surgery was hampered by significant adhesion. A radiculomedullary artery also prevented sufficient rotation of the spinal cord (Fig. 3CD). Since the tumor was solid and floating, debulking with an ultrasonic aspirator inserted from a relatively perpendicular angle was difficult. This surgery also ended in partial removal, but her symptoms significantly improved.
Fig. 3.
Case 14. A: Preoperative MRI with gadolinium enhancement. B. Postoperative MRI with gadolinium enhancement. C: Image during the previous operation with the standard midline approach. The ultrasonic aspirator is inserted at a relatively perpendicular angle because of the skin and retractor blade restriction. Removing a solid, floating tumor was difficult with this insertion angle. D. Image during the second operation with the modified unilateral approach. The arrow indicates the radiculomedullary artery preventing cord rotation. The ultrasonic aspirator could be inserted from a more lateral angle to allow the safe removal of the tumor.
Three years later, her symptoms worsened, and we planned another operation. This time, we decided to use the modified unilateral approach with a horizontal skin incision crossing the previous one. This technique allowed better exposure of the ventrally located tumor without much cord retraction. The more lateral angle of instrument insertion facilitated debulking and tumor removal (Fig. 3D). Gross total removal of the tumor was accomplished (Fig. 3B), and the patient's preoperative symptom of paraparesis improved significantly. No wound-related complaints exist after 18 months of follow up.
Outcomes and complications
Eleven of twelve benign tumors (10 schwannomas and 2 meningiomas) were classified as McCormick grade I. In one patient with recurrent thoracic schwannoma (Case 14), preoperative lower-extremity paresis improved after surgery but remained. One patient (Case 10) with dissemination from a germ cell tumor had an outcome of grade IV. One patient (Case 3) died one year after surgery because of the progression of malignancy. Gross total removal was achieved in both meningiomas. In the 10 schwannomas, a gross total removal was achieved in 8 cases, and a portion of the tumor was left outside the foramen in two cases. One patient (Case 2) with cervical schwannoma originating from a motor root developed postoperative biceps weakness, which recovered within three months. No cerebrospinal fluid (CSF) leak or wound problem exists. There was no recurrence or any wound-related pain or deformity during the median follow-up period of 53 months.
Paraspinal muscle atrophy
The final postoperative MRI was available for 15 patients. The median follow-up period with MRI was 12.0 months (25th percentile = 6.3 months, 75th percentile = 25.6 months). The mean ratio (approach side to nonapproach side) of the paraspinal muscle was 0.93 (95% confidence interval: 0.74-1.12) (Fig. 4). This meant, supposing that the nonapproach side had no atrophy, that the approach-side paraspinal muscle showed 7% atrophy, although it was statistically nonsignificant on the t-test (p = 0.48).
Fig. 4.
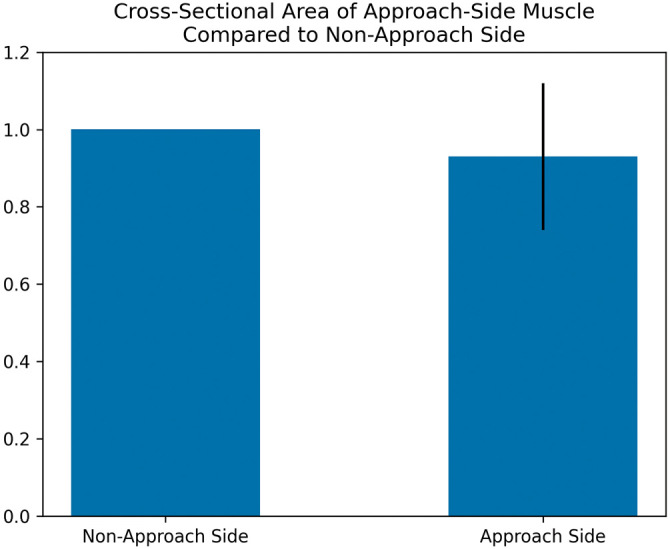
A bar graph shows the paraspinal muscles' cross-sectional areas in the postoperative MRI. The left bar represents the cross-sectional area of the nonapproach side as the control. The right bar represents the cross-sectional area on the approach side (calculated as the rate to the nonapproach side). The error bar represents the 95% confidence interval.
Postoperative pain
During the survey period, six patients underwent the modified unilateral approach (cervical 3, thoracic 1, lumbar 2), and seven patients underwent standard bilateral laminectomy (cervical 3, thoracic 2, lumbar 1). The mean VAS score was significantly lower (p = 0.04) in the patients who underwent the modified unilateral approach (mean 3.1, SD 2.0) than in those who underwent standard bilateral laminectomy (mean 5.6, SD 2.0).
Discussion
This article presented our modified unilateral approach and its effectiveness for removing ventrally located spinal tumors. The technique was a simple modification of the unilateral approach to the spinal canal. Instead of incising the skin longitudinally, we used a horizontal skin incision. Instead of applying the retractors horizontally, we applied them in the longitudinal direction. These modifications allowed a wider lateral viewing angle to manipulate the ventrally located tumors with minimal cord retraction. However, the disadvantage of this technique is the possible damage to the ipsilateral paraspinal muscles due to a small muscle incision on the medial portion of the multifidus muscles.
Our technique differed from the conventional posterior midline approach in the following ways. In the conventional approach, bilateral laminectomies were preferred instead of unilateral laminectomies, thereby causing damage to the bilateral paraspinal muscles. Additionally, it required cord rotation after incising the dentate ligament and nerve roots. A longer exposure of the spinal cord was necessary for this purpose. Sacrificing nerve roots was not always feasible, and manipulating the compressed spinal cord posed significant risks.
One can also use a conventional unilateral approach, which is less invasive than a bilateral laminectomy. However, this approach makes the operative field narrow and deep and the lateral viewing angle limited. Our technique solved these problems by making the skin incision horizontally and placing the retractors longitudinally, thereby removing the obstruction to the lateral viewing angle.
Removing the facet joint is another option for obtaining the lateral viewing angle. Ito et al.6) reported this technique in their series of ventrally located spinal tumors. However, in their experience, patients with two-level facetectomy experienced postoperative instability. Additionally, although removing the facet joint creates a lateral viewing angle at the bottom of the operative field, it will still be blocked by the paraspinal muscles and the skin. In our approach, we performed medial facetectomy up to the medial aspect of the pedicle (Supplementary Figure 2). This was sufficient for obtaining a good lateral viewing angle (Supplementary Video 1). Complete facetectomy was unnecessary to our series.
Our technique utilizes the less-invasive unilateral approach and obtains a good lateral viewing angle. The viewing angle and the angle of instrument insertion were also improved, enabling easy manipulation of the ventrally located tumors. The contralateral muscles were not violated. It also allowed shorter longitudinal exposure. It was advantageous compared to conventional bilateral laminectomy, which necessitated longer spinal cord exposure for its safe rotation.
We argue that this approach is less-invasive than it may seem. Because of its unilateral nature, the contralateral paraspinal muscles are preserved. Since no spinal cord manipulation is needed, the length of longitudinal exposure was reduced.
Even so, one may criticize that this approach causes too much damage to the ipsilateral paraspinal muscles. In response to this criticism, we present the MRI findings of postoperative paraspinal muscle atrophy, which showed a 7% (statistically insignificant) mean reduction of the cross-sectional area of the ipsilateral muscles compared to the contralateral nonapproach side. Kim et al.7) reported 4.5-17.3% postoperative reduction in the cross-sectional area of the paraspinal muscles in the unilateral approach to the lumbar spine. Watanabe et al.8) reported a 5.3% reduction in the spinous-process splitting approach to the lumbar spine. Based on these data, we can estimate that the paraspinal-muscle damage in our approach is comparable to the unilateral approach to the lumbar spine, which is generally considered less invasive. Meanwhile, Watanabe et al. showed a 23.9% reduction in the cross-sectional area when conventional bilateral laminectomy was used. Therefore, we may consider that our approach is much less invasive than conventional laminectomy in longer segments.
Recently, a few clinical series have shown that minimally invasive surgery (MIS) could provide a satisfactory outcome in patients with intradural extramedullary tumors.9,10) Although this technique may be less invasive than the conventional approach, a narrow tubular retractor makes microsurgical manipulation technically challenging.9) Additionally, MIS may not be currently indicated for ventrally located intradural tumors.9) Even with the MIS technique, damage to the paraspinal muscles is inevitable.11) Fan et al. reported a 12.2% reduction in the MRI cross-sectional area of the multifidus muscles after MIS pedicle screw fixation (PSF) of the lumbar spine.12) Hyun et al. reported a 4.8% reduction after PSF with a paramedian interfascial approach.13) Our technique may be interpreted as a variant of MIS. Although we did not use a tubular retractor, our exposure was limited to the minimal necessity for tumor removal, and the damage to the paraspinal muscle was comparable to the MIS technique. Our approach, however, had a large advantage of a wider operative field with excellent maneuverability.
There are some limitations in this study. It is a retrospective observational study at a single center without a comparative group. The outcome measurement was surgeon-oriented. The follow-up period of the patients and the postoperative MRI were relatively short. A longer-term follow-up of the patients will be necessary in the future. The cross-sectional areas of the cervical paraspinal muscles are relatively small, possibly causing a less accurate evaluation of atrophy. This technique is unsuitable for a long tumor. Additionally, one should be cautious in performing this technique on young patients because we do not have enough experience.
Conclusions
We described a simple modification to the unilateral approach for approaching the spinal canal, consisting of a horizontal incision in the skin and fascia and longitudinal placement of the retractors. A wide lateral surgical view was provided, enabling better visualization and manipulation of ventrally located spinal tumors. This approach can be a valuable addition to the spine surgeon's armamentarium.
Supplementary Material
Conflicts of Interest Disclosure
No conflicts of interest exist in any of the authors.
Supplementary Material
Region of interest (ROI) of postoperative paraspinal muscle atrophy. A. Cervical (Case 2) ROI included the multifidus and the semispinalis cervicis muscles. B. Thoracolumbar (Case 14) ROI included the multifidus muscles.
Postoperative CT of Case 13. A. 3D reconstruction from an oblique posterior view showing the range of the T9 hemilaminectomy and T10 partial hemilaminectomy.
Surgical video of Case 13.
References
- 1). Slin'ko EI, Al-Qashqish II: Intradural ventral and ventrolateral tumors of the spinal cord: surgical treatment and results. Neurosurg Focus 17: ECP2, 2004 [DOI] [PubMed] [Google Scholar]
- 2). Angevine PD, Kellner C, Haque RM, McCormick PC: Surgical management of ventral intradural spinal lesions. J Neurosurg Spine 15: 28-37, 2011 [DOI] [PubMed] [Google Scholar]
- 3). Chang HS: Posterior paramedian approach to ventrally located spinal meningioma. World Neurosurg 105: 755-759, 2017 [DOI] [PubMed] [Google Scholar]
- 4). Manzano G, Green BA, Vanni S, Levi AD: Contemporary management of adult intramedullary spinal tumors-pathology and neurological outcomes related to surgical resection. Spinal Cord 46: 540-546, 2008 [DOI] [PubMed] [Google Scholar]
- 5). Elliott JM, Cornwall J, Kennedy E, Abbott R, Crawford RJ: Towards defining muscular regions of interest from axial magnetic resonance imaging with anatomical cross-reference: part II - Cervical spine musculature. BMC Musculoskelet Disord 19: 171, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6). Ito K, Aoyama T, Miyaoka Y, Seguchi T, Horiuchi T, Hongo K: Surgery for ventral intradural thoracic spinal tumors with a posterolateral transpedicular approach. Acta Neurochir (Wien) 158: 1563-1569, 2016 [DOI] [PubMed] [Google Scholar]
- 7). Kim K, Isu T, Sugawara A, Matsumoto R, Isobe M: Comparison of the effect of 3 different approaches to the lumbar spinal canal on postoperative paraspinal muscle damage. Surg Neurol 69: 109-113, 2008 [DOI] [PubMed] [Google Scholar]
- 8). Watanabe K, Hosoya T, Shiraishi T, Matsumoto M, Chiba K, Toyama Y: Lumbar spinous process-splitting laminectomy for lumbar canal stenosis: Technical note. J Neurosurg: Spine 3: 405-408, 2005 [DOI] [PubMed] [Google Scholar]
- 9). Mannion RJ, Nowitzke AM, Efendy J, Wood MJ: Safety and efficacy of intradural extramedullary spinal tumor removal using a minimally invasive approach. Operative Neurosurg 68: ons208-ons216, 2011 [DOI] [PubMed] [Google Scholar]
- 10). Wong AP, Lall RR, Dahdaleh NS, et al. : Comparison of open and minimally invasive surgery for intradural-extramedullary spine tumors. Neurosurg Focus 39: E11, 2015 [DOI] [PubMed] [Google Scholar]
- 11). Pourtaheri S, Issa K, Lord E, et al. : Paraspinal muscle atrophy after lumbar spine surgery. Orthopedics 39: e209-e214, 2016 [DOI] [PubMed] [Google Scholar]
- 12). Fan S, Hu Z, Zhao F, Zhao X, Huang Y, Fang X: Multifidus muscle changes and clinical effects of one-level posterior lumbar interbody fusion: minimally invasive procedure versus conventional open approach. Eur Spine J 19: 316-324, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13). Hyun SJ, Kim YB, Kim YS, et al. : Postoperative changes in paraspinal muscle volume: comparison between paramedian interfascial and midline approaches for lumbar fusion. J Korean Med Sci 22: 646-651, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Region of interest (ROI) of postoperative paraspinal muscle atrophy. A. Cervical (Case 2) ROI included the multifidus and the semispinalis cervicis muscles. B. Thoracolumbar (Case 14) ROI included the multifidus muscles.
Postoperative CT of Case 13. A. 3D reconstruction from an oblique posterior view showing the range of the T9 hemilaminectomy and T10 partial hemilaminectomy.
Surgical video of Case 13.