Abstract
Introduction
We used an educational healthcare simulation tool called room of errors (ROE) to raise pharmacy operators’ awareness of potential errors in a chemotherapy production process and assessed its impact on their knowledge and satisfaction.
Methods
Twenty-five errors (compiled from internal procedures, literature and our hospital's reported incidents) were categorised as static (n = 7, visible by the participant anytime) and dynamic (n = 18, made by a pseudooperator in front of the participant). Our simulated cytotoxic production unit (CPU) hosted the 1 h-simulation. Two pharmacists (supervisor/pseudo-operator) welcomed the trainee for a 10-min briefing. During the 20-min simulation, participants watched the pseudo-operator's gestures in a simulated chemotherapy production process. Participants called out each error observed (recorded by the supervisor). A 20-min debriefing followed. ROE's impact on knowledge was measured through participants’ answers to a before-and after 18-item questionnaire about CPU's procedures and certainty about answers on a scale (0%–100%). Participants evaluated the training using a satisfaction questionnaire (Likert scale, 1–6).
Results
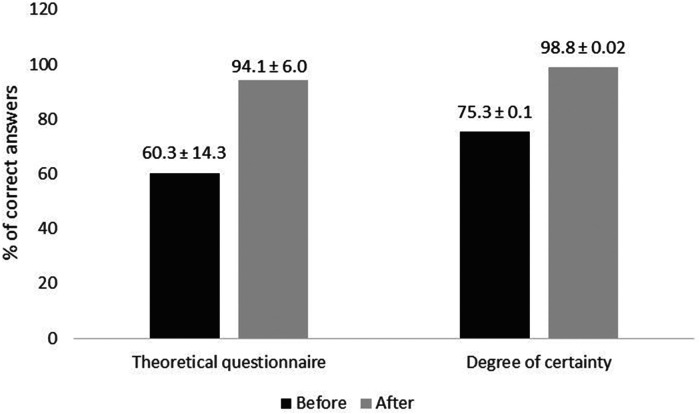
The 14 participants detected 70.4% ± 11.4% of errors. Least-detected errors were “using non-disinfected vials” (42.9%) and “touching syringe plunger” (0%). Critical errors (expired leftovers or glucose instead of sodium chloride) were detected at 57.1%. Knowledge improved from 60.3% to 94.1% (p < 0.001) and certainty from 75.3% to 98.8% (p < 0.001). Participants appreciated this non-judgmental, informative, and original training (satisfaction 95.7%). Some pointed out difficulties settling into the game quickly and visualising static and dynamic errors simultaneously.
Conclusion
This ROE simulation improved operators’ knowledge and certainty. Longer-term testing should be done to measure knowledge retention over time.
Keywords: simulation, knowledge assessment, pharmaceutical training, chemotherapy, errors
Introduction
Our hospital pharmacy produced 17,000 chemotherapy preparations in 2021. The centralisation of antibody preparation in February 2022 increased this number by 5000 but without any new equipment. Pharmaceutical technology operators are known to face frequent high-stress levels linked to short-staffing 1 and high levels of interruptions and disturbances. 2 These factors can lead to errors with significant impacts on patients. A descriptive analysis of centralised chemotherapy preparation in a French hospital reported 140 defective preparations out of 30,819 (0.45%), including major errors such as wrong dose, wrong labelling, unauthorized drugs, incompatible diluents and incompatible bags. 3 Moreover, good manufacturing practices (GMPs) require the initial and continuous training of operators to improve the quality of cytotoxic preparation. 4 Continuous training is generally done once a year. 5 In our hospital, operators undergo an initial three-month training period and are requalified annually by a pharmacy instructor. However, evaluations mainly focus on aseptic manipulation skills and not on the overall competencies required during the entire chemotherapy preparation process.
Simulation is increasingly used to complement traditional teaching approaches such as lectures or distributing theoretical materials.6–9 It has become an integral part of medical education at all levels. 10 Simulation techniques are playful pedagogical tools that can be applied in different ways, such as using error-based simulations (clean rooms containing errors and preparation sheets printed with errors) or game-based simulations (escape games, role-playing games and board games). 6
The room of errors (ROE) concept is particularly interesting because it is a realistic, playful and educational health simulation tool that can be used to raise awareness by discovering errors in a guilt-free context. In an ROE exercise, errors and risks to the patients are deliberately “hidden” in a specially prepared room. Health professionals try, whether individually or in teams, to discover the errors and understand the risks they create. This type of training is already used with health professionals such as physicians, 11 dentists 12 and nurses 13 or for inter-professional purposes between nurses and pharmacists.14,15 Considering the advantages of this type of education for improving the quality of operator training, we created a clean-room of errors reproducing a cytostatic drug production unit and dedicated to training pharmacy operators and pharmaceutical technology pharmacists.
The present study's primary objective was to raise operators’ awareness of the potential risks and errors existing in the cytotoxic drug preparation process. The second objective was to assess this original training method's impact on operators’ knowledge and their level of satisfaction with the exercise.
Methods
Study design
Two pharmacists drew up a table of 25 possible errors in the field of chemotherapy drug production using three different sources: the incidents reported in our hospital relating to the pharmaceutical production unit between April 2019 and August 2021, a non-systematic literature review about ROE exercises involving pharmaceutical technology in hospital pharmacies and a list of critical safety points in our existing procedures. These critical safety issues were discussed at a meeting of pharmacists specialising in chemotherapy production. The project was scheduled over six weeks, with one pharmacist working on this project for 80% of their time. Week 1 involved choosing the training method; week 2, choosing the errors and creating the scenario; week 3, adapting our existing simulation room, creating the knowledge questionnaire, testing the training session with an oncology pharmacist to validate the ROE's design; weeks 4–5, performing the ROE training sessions; and week 6, analysing the results. The training took place in a simulated chemotherapy preparation unit with a logistics room, a dressing room and a drug preparation room. The equipment used in the drug preparation step included a vertical laminar airflow hood.
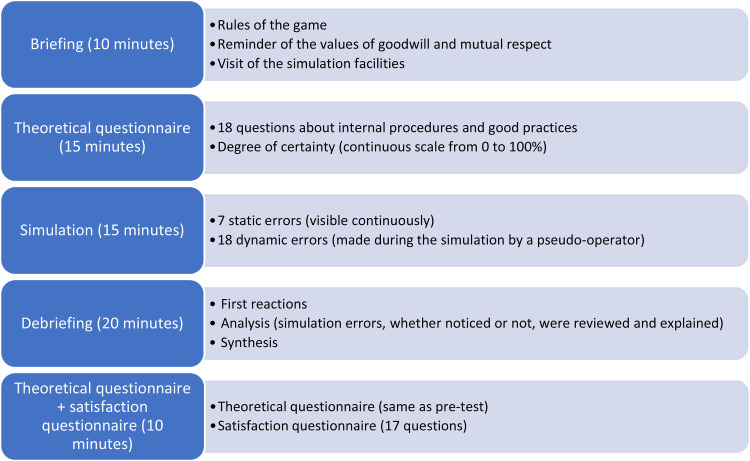
The training session's organisation followed simulation good practices recommendations (briefing, exercise and debriefing), 16 which are summarised in Figure 1. Each session involved one operator at a time being welcomed by two pharmacy instructors, one of whom acted as the supervisor, explaining the room of errors concept, the rules of the game and reminding the participant of the values of goodwill and mutual respect during the briefing (± 10 min). The other pharmacy instructor was the pseudo-operator, dedicated to playing the role of a pharmacy operator making mistakes. Next, the participant answered the knowledge questionnaire (± 15 min), which was marked by the supervisor while the pseudo-operator gave the participant a guided tour of the simulation facilities. During the simulation exercise itself (± 20 min), 25 errors were made throughout the game in two different forms: static errors that were already present in the room when the participant arrived or dynamic errors made deliberately by the pseudo-operator. Each participant was faced with the same errors. The participant was tasked with observing the room and the pseudo-operator's work and calling out all the errors they saw. The simulation covered every step of a typical chemotherapy preparation process in every zone of the clean room: choice of materials, hand-washing, hand disinfection, dressing, preparation, control and bag shipment. 5 The game supervisor also stood in the room to record all the errors called out by the participant. Debriefings (± 20 min) followed a standard process of recording participants’ reactions (answers to the questions “How do you feel?” and “Were you able to get into the game?”), analysing their observations (reviewing and explaining all of the errors in the simulation, whether noticed or not) and synthesising final outcomes (answers to the questions “In one sentence, what have you remembered from this exercise?”, “What did you learn?” and “What will you improve in your everyday practice?”). The participant then completed the same theoretical questionnaire as before and a satisfaction survey (± 10 min). In total, the training session lasted approximately 1 h and 15 min.
Figure 1.
Simulation exercise design.
Satisfaction
Satisfaction was assessed using Likert scale items rating answers from 0 to 6. Seventeen questions were divided into three categories: training evaluation (seven questions), scenario evaluation (five questions) and personal satisfaction (five questions). The participant's mean result for every category (from 0 to 6) was transformed into a percentage.
Knowledge improvement
Improvements in knowledge were assessed using the 18 items of a before-and-after questionnaire that looked at various subjects related to the errors in the simulation (Table 1). Our challenge was to respect the concept of pedagogical alignment: assessment tasks should directly address the intended learning outcomes. Regarding the questionnaire, with its 10 multiple choice questions and 8 open-ended questions, we strived to follow the rule of one question per error, as shown in the following three examples. Question no 1 (“What should we check when assembling the material?”) was related to the errors of “Wrong diluent bag, wrong vial, wrong syringe in the preparation tray.” Question no 4 (“What are the hand-washing movements required before entering the clean room?”) was related to the hand-washing errors, including “The pseudo-operator forgets the interlocked fingers hand-washing step.” Question no 16 (“Why must the tubing be clamped after purging?”) was related to the error of “The pseudo-operator does not clamp the preparation after purging.” All the completed questionnaires were marked by the same person. For multiple choice questions with just one correct answer, participants received one point for choosing correctly. For multiple choice questions with several correct answers expected, 1 point was given if all the participant's choices were correct, half a point was given if one or several correct choices were missing and zero points were given if no correct answers were chosen. For the open-ended questions, we used a list of keywords representing the expected answers. One point was given if the participant answered using one or several keywords. Questions answered without using a keyword received zero points. Participants also had to estimate their degree of certainty about each of their answers using a continuous scale from 0% to 100%. 17
Table 1.
Theoretical knowledge questionnaire.
| No | Question | Type | Answer expected |
|---|---|---|---|
| 1 | What should you check when assembling the material? | Open-ended |
|
| 2 | What is the minimum time required for hand washing before entering the clean room (according to the WHO)? | MCQ |
|
| 3 | What is the minimum time required for hand disinfection (according to the WHO)? | MCQ |
|
| 4 | Name the movements for hand-washing before entering the clean room. | Open-ended |
|
| 5 | What is the minimum hand-washing procedure before entering a clean room? | MCQ |
|
| 6 | Why should you dry your hands completely by dabbing and not rubbing? | Open-ended | To avoid spreading residual bacteria |
| 7 | Why use a neutral soap (e.g., Lactacyd) for hand-washing before entering the clean room? | Open-ended | Reaction between anionic ordinary soap and cationic (chlorhexidine disinfectant). Lactacyd is a neutral soap. |
| 8 | Why not use hydroalcoholic solution to disinfect gloves? | Open-ended | Because it contains an emollient agent that can make the gloves permeable |
| 9 | When should you remove your surgical mask (worn against COVID-19) when entering the clean room? | MCQ |
|
| 10 | What does a vertical laminar airflow hood do? | MCQ |
|
| 11 | Why must the workspace under a vertical laminar airflow be tidy? | Open-ended | Not to disturb the airflow direction |
| 12 | How should you clean a vertical laminar airflow hood or the area beneath it? | MCQ |
|
| 13 | Out to what distance does an object disturb the airflow? | MCQ |
|
| 14 | How many particles can be emitted by a single unprotected movement of the head or hands? | MCQ |
|
| 15 | What should you do if your gloves come outside the airflow? | MCQ |
|
| 16 | Why must the tubing be clamped after purging? | Open-ended | Risk of contamination when connecting the bag at the bedside |
| 17 | For which product(s) should filter tubing be used? | MCQ |
|
| 18 | What should be checked when approving a bag for release? | Open-ended |
|
Data analysis
Excel® software was used to tabulate the results of the theoretical questionnaires and participants’ error detection. Paired t-tests were used to compare the results from before and after the training session.
Results
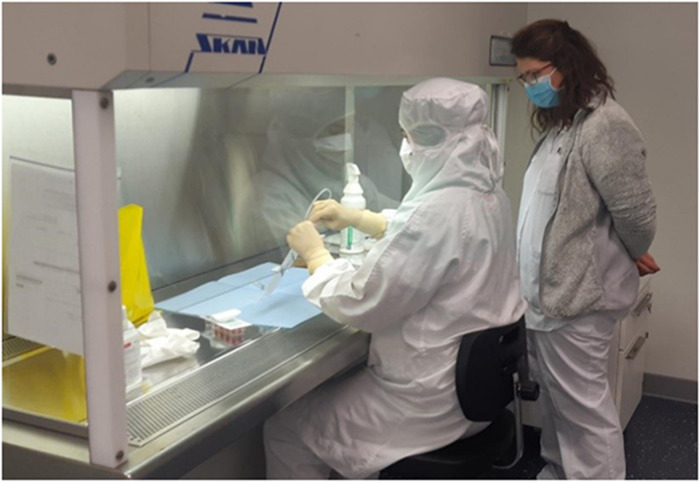
The training sessions took place between October and November 2021 (Figures 2 and 3), and 14 operators participated (4 pharmacists and 10 pharmacy technicians).
Figure 2.
Beginning of the simulation.
Figure 3.
Preparation step during the simulation.
Error detection rate
Errors were separated into the five categories of logistics, hygiene, dressing, preparation and bag approval. Operators found 70.4% ± 11.4% of the errors (Table 2). The most-reported errors were “wrong mask” and “tubing not clamped”, and the least-reported errors were “Vials not disinfected before entering the airflow” and “Touching the syringe plunger”.
Table 2.
List of errors and results by operator.
| Category | No | Error | Operator | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | Total (/14) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Error type | ||||||||||||||||||
| Logistics | 1 | Wrong bag (Glucose instead of NaCl 0.9%) | Static | x | x | x | x | x | x | x | x | 8 | ||||||
| 2 | Wrong vial (Treosulfan instead of Etoposide phosphate) | Static | x | x | x | x | x | x | x | x | x | x | x | x | x | 13 | ||
| 3 | Wrong syringe (30 mL instead of 10 mL to withdraw 8 mL) | Static | x | x | x | x | x | x | x | x | x | x | x | x | 12 | |||
| Hygiene | 4 | Hands washed using anionic soap (instead of neutral soap) | Dynamic | x | x | x | x | x | x | x | x | x | 9 | |||||
| 5 | Hand-washing error (one step of the procedure missed) | Dynamic | x | x | x | x | x | x | x | x | x | 9 | ||||||
| Dressing | 6 | Surgical mask not removed before entering the clean room | Dynamic | x | x | x | x | x | x | x | x | x | x | x | 11 | |||
| 7 | Wrong mask worn (non-sterile instead of sterile mask) | Dynamic | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 14 | |
| 8 | Sterile gloves not donned correctly | Dynamic | x | x | x | x | x | x | x | x | x | 9 | ||||||
| 9 | Gloves disinfected with the wrong product | Dynamic | x | x | x | x | x | x | x | x | x | x | x | 11 | ||||
| 10 | Watch is not removed | Dynamic | x | x | x | x | x | x | x | x | x | x | x | 11 | ||||
| Preparation | 11 | There is only one Petri dish in the airflow (instead of two) | Static | x | x | x | x | x | x | x | x | x | x | 10 | ||||
| 12 | There is clutter inside the airflow (the workspace should be tidy) | Static | x | x | x | x | x | x | x | x | 8 | |||||||
| 13 | The wrong preparation sheet is provided | Static | x | x | x | x | x | x | x | x | x | x | x | x | x | 13 | ||
| 14 | The vials are not disinfected before entering the airflow | Dynamic | x | x | x | x | x | x | 6 | |||||||||
| 15 | The sterile material is opened outside of the airflow | Dynamic | x | x | x | x | x | x | x | x | 8 | |||||||
| 16 | The gloves are not disinfected inside the airflow | Dynamic | x | x | x | x | x | x | x | x | x | 9 | ||||||
| 17 | The IV line is not clamped | Dynamic | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 14 | |
| 18 | The leftover drugs have expired | Static | x | x | x | x | x | x | x | x | 8 | |||||||
| 19 | The dark part of the needle is touched | Dynamic | / | x | x | x | x | x | x | x | 7 | |||||||
| 20 | The manipulation is done without any pads | Dynamic | x | x | x | x | x | x | x | x | x | 9 | ||||||
| 21 | The syringe plunger is touched | Dynamic | / | 0 | ||||||||||||||
| 22 | The preparation is not packed in an opaque bag | Dynamic | x | x | x | x | x | x | x | x | x | x | x | 11 | ||||
| Liberation | 23 | The presence of the tamper-proof cap is not verified | Dynamic | x | x | x | x | x | x | x | x | x | x | x | x | x | 13 | |
| 24 | The preparation is sent at the wrong temperature | Dynamic | x | x | x | x | x | x | x | x | x | x | x | 11 | ||||
| 25 | The preparation is sent to the wrong ward | Dynamic | x | x | x | x | x | x | x | x | x | x | x | 11 | ||||
| Total (/23 for operator 1 and /25 for others) | 17 | 11 | 17 | 13 | 16 | 23 | 20 | 20 | 17 | 17 | 17 | 22 | 17 | 18 | ||||
X = error detected; / = error forgotten by the pseudo-operator; No = operator.
Satisfaction
Mean satisfaction levels with the overall training session and the scenario were 96.5% and 93.5%, respectively. Personal satisfaction about the benefits of this exercise was rated 96.9%. Total average satisfaction was thus 95.7%. (Table 3). Positive comments were given on the learning environment (“good atmosphere”, “very interesting”, “informative and educational”, “lack of judgement appreciated”, “very intense”) and the training session's impact (“questioning one's habits”, “efficient reminder of the procedures”, “a good way to improve oneself”). Difficulties encountered by the participants concerned the simulated environment (“complicated to get involved in the scenario”, “environment was not totally real”) and the game's rules (“perturbing not to be doing the actions oneself”, “hard to see static errors and dynamic errors at the same time”).
Table 3.
Results of the satisfaction survey.
| Category assessment | Question | Mean results (%) |
|---|---|---|
| Training | This simulation is relevant to my daily professional practice | 94.0 |
| My prior experience and knowledge enabled me to detect errors easily | 87.5 | |
| This room of errors model is a relevant pedagogical tool for the continuous training of drug production operators | 97.0 | |
| The simulation's playful aspect adds more value to reviewing procedures than “traditional” teaching | 97.6 | |
| The simulation's total duration was appropriate/adequate | 98.8 | |
| The simulation was well organised | 100 | |
| The briefing and debriefing were well run | 96.4 | |
| Overall assessment of the training | 95.9 | |
| Scenario | Errors were varied | 96.4 |
| The choice of errors was relevant | 96.4 | |
| The level of difficulty of the errors was relevant to my professional experience | 96.4 | |
| The pseudo-operator made the dynamic errors visible enough | 84.5 | |
| The scenario reflected reality | 94.0 | |
| Overall assessment of the scenario | 93.5 | |
| Personal satisfaction | I have benefited from this room of errors training session | 96.4 |
| This experience will help me improve my daily professional practice | 92.9 | |
| I will recommend this exercise to colleagues | 100 | |
| The room of errors enabled me to update my knowledge | 95.2 | |
| There was a good general atmosphere throughout the simulation | 100 | |
| Overall personal satisfaction | 96.9 | |
| Overall satisfaction | 95.4 | |
Knowledge improvement
Participants’ mean scores for the theoretical questionnaire and their degree of certainty, both before and after training, are provided in Figure 4. There were significant increases in mean scores and degrees of certainty after the simulation exercise (p < 0.001).
Figure 4.
Mean theoretical knowledge questionnaire results and degrees of certainty with their standard deviations (n = 14, p < 0.001).
Discussion
To the best of our knowledge, this was the first study assessing the efficacy of a room of errors simulation for improving knowledge in pharmaceutical technologies.
Knowledge improvement
According to our non-systematic literature review, room of errors simulations of pharmaceutical technology are mainly used to raise operators’ awareness of major potential errors during drug preparation18,19 or to enhance their continuous training.20,21 These studies only assessed participants’ error detection rates, but there was no focus on improving operators’ knowledge. Hence, our improvements in knowledge scores, from 60.3% to 94.1%, and our improvements in participants’ degrees of certainty, from 75.3% to 98.8%, cannot be directly compared with the pharmaceutical technology literature involving other room of errors simulations.
Error detection rate
The error detection rate reported in the literature on simulation studies in the field of pharmaceutical technology went from 52.2% to 78.5%.18,22 Hence, our error detection rate of 70.43% was within the expected range. It is, however, difficult to compare simulation studies that do not contain the same number of errors, categories of errors (logistical, dressing, preparation, etc.) or types of errors (static or dynamic). Loboda et al. also used the concept of static and dynamic errors, but they separated them into two separate simulation situations of 20 min each. 23 Our study's added value was its mixing of static and dynamic errors throughout the same simulation session. Using this approach confronts participants with a situation much closer to reality, where errors can occur at any point during the process.
Satisfaction
Some negative comments in Loboda et al.'s study concerned the lack of immediate feedback after the simulation exercise because of scheduling issues. 23 Our study rigorously included a personal debriefing of each participant immediately after their simulation training, and they highly appreciated this. The overall mean satisfaction rate in Cotteret et al.'s study was 87.1%, with all the respondents being satisfied or very satisfied with the workshop, considering it relevant to their daily work practices and that it provided them with new expertise. 4 Mean overall satisfaction with our training session was a very encouraging 95.4%, although it should be noted that two item statements received mean ratings under 90%: “My prior experience and knowledge enabled me to detect errors easily” (87.5%) and “The pseudo-operator made the dynamic errors visible enough” (84.5%) (Table 3). Concerning the first statement, all the participating operators had at least five years of experience in chemotherapy preparation in our hospital. This rating may be explained by the choice of errors rarely committed by these participants (touching the needle) or not considered as errors by some of them (removing the needle from the vial without a pad). Concerning the second statement, although each participant was presented with the same static errors, dynamic errors were dependent on the pseudo-operator making them on purpose. Consequently, some unexpected errors made by the pseudo-operator were reported by the participants and some deliberate errors were not reported because they were less visible.
Design of the room of errors
Participants were warned that the simulation would use a laminar airflow hood instead of the isolator used in our production facility, and they were given a guided tour of the clean room before starting the game. However, a few participants admitted in the debriefing that they had been perturbed by the discrepancy between the role-playing situation and their daily professional reality, as in Loboda et al.'s study. These issues (lack of fidelity in the equipment used and slight variations in the pseudo-operator's gestures) were also encountered by Loboda et al. and may have induced some bias in the results. 23 This highlights the importance of using a well-rehearsed pseudo-operator and the most realistic equipment.
Evaluating a training session's effectiveness, and therefore its usefulness, is fundamental and should be done by assessing operators’ competencies before and after it. The present study's objective was to improve operators’ knowledge of the chemotherapy preparation process through their ability to detect the errors made by somebody else during this process. The challenge of pedagogical alignment was respected for most of the questions. However, question no 13, “Out to what distance does an object disturb the airflow?” was related to the error “There is clutter in the airflow”, and the answer in the standard operating procedures documentation is “3 times its diameter”. It was impossible to answer this question without having read the procedures, and this was only discussed briefly during the debriefing. We encourage future researchers to stick to the rule of one question for one error. Moreover, although using a questionnaire is the easiest and fastest way to collect data, to avoid any memory bias, we recommend that the pre-test and post-test questions be asked in different orders.
Development of the room of errors
Of five different simulation training tools used in pharmaceutical technology, Bonnet et al. considered setting up a room of errors to be the most time-consuming. 7 To put this statement into perspective, every potential error that an operator might make in a clean room has been thought of and implemented in several room of errors described in the literature since the first one in 2015. 22 In the absence of a literature review listing all these errors, it is indeed necessary to take the time to select the mistakes most pertinent to one's working environment and to ready a simulated clean room for this kind of session. We were able to design and execute this study in six weeks, which could be considered quick because one pharmacist dedicated 80% of her working week to this project.
Concerning implementation, our scenario required two trainers for one participant for more than 1 h, which is resource intensive. However, the time spent should be weighed against the efficacy of this kind of active training session. Studies directly comparing the efficacy of different forms of training in the field of pharmaceutical technologies are needed.
Limitations
The errors reproduced in our simulation were not ostensibly linked to levels of criticality, as in other studies.18,23,24 However, as every undetected error was reviewed during the debriefing, the emphasis could be put on serious errors such as a wrong diluent infusion bag or a wrong drug. Encouraging the participants to express their emotions linked to specific errors (the relief of having detected them or regret of having missed them) was an impactful way of highlighting their criticality.
Berthod et al. showed that improvements in pharmacy staff's knowledge of GMP were still significant 1 month after an escape room training session. 5 However, we did not assess medium-term knowledge retention, and it would have been interesting to compare our results with those of Berthod et al.
Finally, we made no evaluation of the training session's impact on practice (level 3 in Kirkpatrick's pyramid of learning). Unfortunately, it is not because operators have improved their knowledge that they will necessarily improve their behaviour in their daily practice. A before-and-after evaluation of some simple mistakes would have been interesting, but organising such real-life audits is time-consuming and incompatible with our study schedule.
Conclusion
The educational, playful learning approach used in our room of errors simulation was very much appreciated by our pharmacy production operators. It allowed us to improve their knowledge and their degree of certainty concerning various procedures. Further studies are needed to confirm the efficacy of this kind of training using rigorous evaluation methods that include assessments of the training's impact on operators’ daily practice. Considering the growing number of studies using this training tool in the field of hospital pharmacy chemotherapy production, it would be beneficial for future researchers to have a list of potential errors available and combined with their assessment questions in the form of a user guide. This could be based on the same model as the Patient Safety Switzerland Foundation ROE user guide which provides six scenarios that can be set up in any hospital facility. 25
Footnotes
AG and LBu designed the study. LBu collected the data and performed the analysis. AG and LBu interpreted the results. All authors reviewed and approved the final version of the manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Alexandra Garnier https://orcid.org/0000-0002-2397-0072
References
- 1.Lapane KL, Hughes CM. Baseline job satisfaction and stress among pharmacists and pharmacy technicians participating in the fleetwood phase III study. Consult Pharm 2004; 19: 1029–1037. [DOI] [PubMed] [Google Scholar]
- 2.Boyle TA, Bishop A, Morrison Bet al. Pharmacist work stress and learning from quality related events. Res Soc Adm Pharm 2016; 12: 772–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Limat S, Drouhin JP, Demesmay Ket al. et al. Incidence and risk factors of preparation errors in a centralized cytotoxic preparation unit. Pharm World Sci 2001; 23: 102–106. [DOI] [PubMed] [Google Scholar]
- 4.Cotteret C, Marry S, Loeuillet Ret al. et al. A virtual centralized cytotoxic preparation unit simulation to evaluate the pharmacy staff knowledge. J Oncol Pharm Pract 2019; 25: 1187–1194. [DOI] [PubMed] [Google Scholar]
- 5.Berthod F, Bouchoud L, Grossrieder F, , et al. Learning good manufacturing practices in an Escape room: validation of a new pedagogical tool. J Oncol Pharm Pract 2020; 26: 853–860. [DOI] [PubMed] [Google Scholar]
- 6.Garnier A, Vanherp R, Bonnabry Pet al. et al. Use of simulation for education in hospital pharmaceutical technologies: a systematic review. Eur J Hosp Pharm 2021: 1–7. 10.1136/ejhpharm-2021-003034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bonnet M, Chalopin M, Oger Cet al. et al. Formation initiale et continue des préparateurs dans une unité de préparation des anticancéreux : revue des outils disponibles. Le Pharmacien Hospitalier et Clinicien 2021; 56: 368–377. [Google Scholar]
- 8.Boet S, Granry J-C, Savoldelli G. La Simulation En Santé : De La Théorie à La Pratique (Lavoisier, 2013).
- 9.Girault C. Gestion Des Risques et Simulation En Santé : Application Au Secteur de Reconstitution Des Chimiothérapies. (Toulouse, 2017).
- 10.Barry Issenberg S, Mcgaghie WC, Petrusa ERet al. et al. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Med Teach 2005; 27: 10–28. [DOI] [PubMed] [Google Scholar]
- 11.Farnan JM, Gaffney S, Poston JTet al. et al. Patient safety room of horrors: a novel method to assess medical students and entering Residents’ ability to identify hazards of hospitalisation. BMJ Qual Saf 2016; 25: 153–158. [DOI] [PubMed] [Google Scholar]
- 12.Borsa L, Tramini P, Lupi L. The dental ‘box of Horrors’ clinical practice game: a pilot project. J Dent Educ 2022; 86: 615–621. [DOI] [PubMed] [Google Scholar]
- 13.Daupin J, Atkinson S, Bédard P, , et al. Medication errors room: a simulation to assess the medical, nursing and pharmacy Staffs’ ability to identify errors related to the medication-use system. J Eval Clin Pract 2016; 22: 907–916. [DOI] [PubMed] [Google Scholar]
- 14.Bracq M-S, Michinov E, Le Duff M, , et al. Training situational awareness for scrub nurses: error recognition in a virtual operating room. Nurse Educ Pract 2021; 53: 103056. [DOI] [PubMed] [Google Scholar]
- 15.Villeneuve V, Thyard E, Lemaire Set al. et al. Chambre des erreurs : outil de simulation pour améliorer la prise en charge des patients. Le Pharmacien Hospitalier et Clinicien 2015; 50: 319–320. [Google Scholar]
- 16.de Santé HA. Guide de Bonnes Pratiques En Matière de Simulation En Santé. 2012, https://www.has-sante.fr/upload/docs/application/pdf/2013-01/guide_bonnes_pratiques_simulation_sante_guide.pdf.
- 17.Bruttomesso D, Gagnayre R, Leclercq Det al. The use of degrees of certainty to evaluate knowledge. Patient Educ Couns 2003; 51: 29–37. [DOI] [PubMed] [Google Scholar]
- 18.Martin J, Ribes O, Sainfort Aet al. et al. PS-062 A playful approach to improve safety of the preparation process in a centralised pharmaceutical unit for chemotherapy drugs. Eur J Hosp Pharm 2017; 24: A254–A256. [Google Scholar]
- 19.Bellegarde J, Kimbidima R, Veillet Ret al. et al. Controlled Atmosphere Area of Errors: To Learn Otherwise. 2017, http://www.gerpac.eu/controlled-atmosphere-area-of-errors-to-learn-otherwise.
- 20.Moine M, Nicoulaud JC, Roux Cet al. et al. An Isolator of Errors: A Useful Training Tool for Hospital Technicians. 2016, https://www.gerpac.eu/an-isolator-of-errors-a-useful-training-tool-for-hospital-technicians.
- 21.Decarout L, Gailland T, Viard-Gaudin G.https://www.gerpac.eu/set-up-of-a-mistakes-isolator-in-the-cytotoxic-drug-reconstitution-unit-cdr Set up of a Mistakes Isolator in the Cytotoxic Drug Reconstitution Unit (CDR). 2018,
- 22.Klaczynski V, Beausir A, Fournier C. How and Why Did We Set up a Controlled Atmosphere Area of Errors ?, 2015, https://www.gerpac.eu/how-and-why-did-we-set-up-a-controlled-atmosphere-area-of-errors.
- 23.Loboda C, Vigneron J, Mulot Cet al. et al. A ‘chamber of Errors’ adaptation to assess pharmaceutical Assistants’ knowledge in chemotherapy preparation. J Oncol Pharm Pract 2019; 25: 454–459. [DOI] [PubMed] [Google Scholar]
- 24.Jaffuel M, Mangavelle J, Vernardet Set al. et al. 5PSQ-052 The error room: a fun training tool for the pharmaceutical chemotherapy unit. Eur J Hosp Pharm 2019; 26: A225 [Google Scholar]
- 25.Fondation Sécurité des patients Suisse. Apprentissage Interactif Grâce à Une Chambre Des Erreurs - Guide d’utilisation. 2019, https://www.securitedespatients.ch/fileadmin/user_upload/1_Projekte_und_Programme/Aktionswoche/2019/Chambre_des_erreurs_Guide_d_utilisation_F.pdf.