Abstract
Background
Proximal humerus fractures account for 2% of all pediatric fractures. A nonoperative approach is the treatment of choice for most of these fractures; however, debates continue regarding the treatment of displaced fractures, especially in adolescents. In this study, we aimed to examine demographic data and treatment strategies for proximal humerus fractures in the pediatric population by conducting a meta-analysis. Additionally, we investigated the preferred surgical technique for operative treatment.
Methods
A systematic online search of databases, including Embase, Medline, PubMed, and Cochrane Library, was conducted to identify studies that matched our search criteria. Data collection was completed on May 1, 2022. Age, sex, degree of angulation, Neer-Horwitz classification, Salter-Harris classification, treatment method (operative vs. nonoperative), and instrument used for internal fixation were classified and documented. Effect size analysis was performed using odds ratios (ORs) or weighted mean differences (WMDs) with 95% confidence intervals (CIs), based on data types.
Results
Eight studies met our inclusion criteria. Overall, 33% of the patients (n = 195) underwent operative treatment, whereas 67% of them (n = 392) received nonoperative treatment. Among the demographic risk factors, severely displaced fracture type (OR, 10.00; 95% CI, 1.56–64.22; p = 0.020) and older age (WMD, 3.26; 95% CI, 2.29–4.23; p < 0.001) were significantly associated with operative treatment. There was no significant difference in the preference for percutaneous pinning or intramedullary nailing, the most frequently employed surgical techniques (OR, 5.09; 95% CI, 0.65–39.58; p = 0.120).
Conclusions
The operative treatment rate in pediatric proximal humerus fractures was 33%, which increased to 60% in severely displaced fractures (Neer-Horwitz grade III/IV). Severely displaced fractures and older age significantly contributed to the establishment of a treatment strategy for operative treatment. The choice of surgical technique may seem to be based on the anatomical location of the fracture rather than the surgeon’s preference.
Keywords: Humeral fracture, Operative treatment, Nonoperative treatment, Pediatrics
Proximal humerus fractures account for approximately 2% of all pediatric fractures;1) they may be caused by a fall on an outstretched hand (FOOSH) injury or direct trauma to the proximal arm. Since Neer declared in his classic paper in 1965 that open treatment of a proximal humerus fracture in a child is unjustified, even in severely displaced fractures,2) nonoperative treatment has been considered the main option to treat proximal humerus fractures in growing children and adolescents. This may be related to the unique biology around the proximal humerus, as the periosteum of an immature skeleton is metabolically active.3,4,5) Additionally, the growth plate of the proximal humerus has significant growth potential, as it governs 80% of the bone growth. Advocates of nonoperative treatment of fractures in the proximal humerus believed that these biological conditions accelerated the remodeling process at the fracture site after nonoperative treatment, regardless of the fracture displacement, angulation, rotation, or translation.6) Conversely, operative treatment has been traditionally recommended only to treat open fractures and fractures associated with nerve or arterial injuries.7,8)
However, controversy has recently arisen regarding the treatment of severely displaced proximal humerus fractures, especially in older children and adolescents. This was primarily because severe outcomes, including pain or discomfort, functional deficit, or subjective dissatisfaction, have been reported in older children with this type of fracture who underwent nonoperative treatment.2,4,6) This is possibly because these older patients have a lower remodeling capacity compared to younger children.7,8) Additionally, a recent trend that favors the early recovery of daily activity has accelerated the operative treatment of these fractures.
Both unnecessary operative treatment and improper long-term immobilization via nonoperative treatment may harm the patient. This study aimed to examine the demographic data and proximal humerus fracture treatment strategies in the pediatric population by conducting a meta-analysis. Additionally, we further investigated the preferred surgical technique for operative treatment. Our hypothesis was that operative treatment had been determined based on the degree of fracture displacement or the patient’s age, and percutaneous pinning was the most preferred surgical technique for operative treatment.
METHODS
Data Sources and Searches
A comprehensive search on pediatric proximal humerus fractures was performed using the Embase, Medline, PubMed, and Cochrane Library databases up to May 1, 2022. The following terms were used in this search: “proximal humerus fractures” and “children” or “pediatric.” This meta-analysis was conducted based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.9)
Two authors (HRS and MHS) screened each study independently in accordance with the inclusion and exclusion criteria (detailed in the following section) and reviewed reference lists of the selected studies, reviews, or comments to identify relevant studies. Only articles published in English were included.
Inclusion and Exclusion Criteria
The inclusion criteria of this meta-analysis were as follows: (1) study design (randomized or nonrandomized controlled studies with level IV evidence or above); (2) study population (patients diagnosed with proximal humerus fractures and patients under the age of 18 years); (3) comparison (demographic data, outcomes, and complications in the nonoperative and operative groups); (4) sufficient data; and (5) language (English, full-text).
The exclusion criteria were as follows: (1) study design (case reports, letters, reviews, conference abstracts, editorials, and studies not including factors of interest); (2) study population (patients with underlying diseases, such as skeletal dysplasia, neuromuscular disease, metabolic disorders, and bone tumors); and (3) insufficient data.
Data Extraction
Two authors (HRS and MHS) extracted the following data from the eligible studies: (1) study design; (2) demographic characteristics data; (3) sample size; (4) follow-up period; (5) fracture pattern; (6) treatment method; (7) outcome; and (8) complications. The fracture pattern was analyzed using the Neer-Horwitz classification, based on the amount of displacement, and the Salter-Harris classification in the cases of physeal involvement.2,10) Neer-Horwitz grade III and IV fractures, which have displacement equal to or greater than one-third of the shaft width, were classified as having severe displacements. These data were collected and analyzed, and the optimal treatment strategies for pediatric proximal humerus fractures were investigated.
Quality Assessment
The Cochrane co-bias tool was used to assess the bias risk of the searched studies. HRS and MHS estimated the bias of the studies in the following categories: (1) selective, (2) performance, (3) attrition, (4) detection, and (5) reporting biases. If an appropriate reference to the study was included, it was assessed as "the risk of bias was low." If it lacked proper mentions, it was assessed as having a “high risk of bias.” Without proper mention, the assessment was "indefinite risk of bias." HRS and MHS conducted their own assessments and exchanged opinions, and differences were resolved through discussions with other authors during the data extraction period.
Statistical Analysis
This meta-analysis used the Review Manager software (version 5.3; Cochrane Collaboration, Oxford, UK). Funnel plots were constructed using meta-essentials. Binary effect size analysis was performed using the odds ratio (OR) and its 95% confidence interval (CI). Continuous effect size analysis was performed using the weighted mean difference (WMD) and its 95% CI. Heterogeneity was tested using a chi-square test on Q statistics and the Higgins I2 test. If there was significant heterogeneity between the included studies, the pooled effect size was calculated using a random-effects model (p < 0.1 or I2 > 50%); otherwise, a fixed-effects model was applied. Publication bias was assessed via funnel plots.
RESULTS
Study Selection and Characteristics
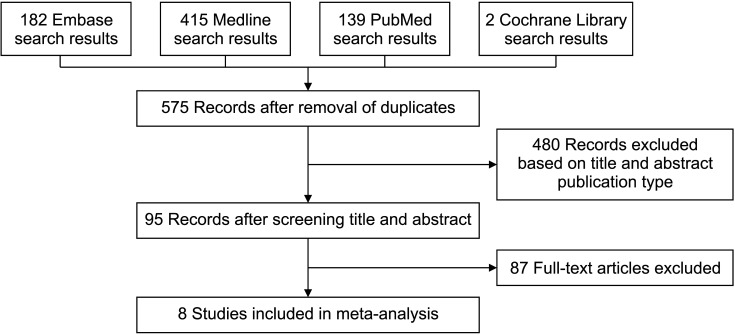
A total of 738 studies were found in the Embase (182), Medline (415), PubMed (139), and Cochrane Library (2) databases. After excluding duplicated trials, 575 studies remained as potential candidates for inclusion in our analysis. Further, 480 studies were deleted after checking the titles and abstracts. Eighty-seven studies were excluded due to insufficient data. Ultimately, 8 studies were included in our meta-analysis. Fig. 1 illustrates the selection process, and the characteristics of the study are summarized in Table 1.
Fig. 1. Flowchart of study selection process.
Table 1. Characteristics of the Studies Included in the Meta-analysis.
| Study | Year | Country | No. of patients | Operative treatment | Nonoperative treatment | Age (yr) | Follow-up period (yr) | Sex (boy : girl) | Study type | |
|---|---|---|---|---|---|---|---|---|---|---|
| Neer and Horwitz2) | 1965 | USA | IV | 89 | 22 | 67 | Range: 1−17 | 2−11 | 67 : 22 | Retrospective |
| Dobbs et al.7) | 2003 | USA | IV | 28 | 25 | 3 | Range: 5−16 | 4 (2−14) | 24 : 4 | Retrospective |
| Hohl10) | 1976 | USA | IV | 15 | 1 | 14 | Mean (range): 12 (9−15) | NA | 8 : 7 | Retrospective |
| Baxter and Wiley11) | 1986 | USA | IV | 57 | 7 | 50 | Range: 8.9−15.1 | 2.7 (2−8) | 31 : 26 | Retrospective |
| Bahrs et al.17) | 2009 | Germany | IV | 43 | 33 | 10 | Mean (range): operative, 14 (6−18); nonoperative, 12.4 (6−16) | 3.3 (1−10) | 29 : 14 | Retrospective |
| Shore et al.18) | 2015 | USA | IV | 84 | 84 | 0 | Mean (range): 13.8 (8−17) | 6 mo | 61 : 23 | Retrospective |
| Gladstein et al.19) | 2017 | USA | IV | 239 | 14 | 225 | Mean (range): 10.2 (1−17) | 5 | 142 : 97 | Retrospective |
| Chaus et al.20) | 2015 | USA | IV | 32 | 9 | 23 | Operative, 14.1; nonoperative, 10.9 | NA | 14 : 18 | Retrospective |
NA: not available.
Quality Assessment of the Studies
Six studies scored 8 points on the Newcastle-Ottawa quality assessment scale, and 2 studies scored 7 points (Table 2). Therefore, the quality of the studies was relatively high.
Table 2. Quality Assessment of the Studies Included in the Meta-Analysis According to the Newcastle-Ottawa Quality Assessment Scale.
Incidence of Operative Treatment in Pediatric Proximal Humerus Fractures
According to the selected 8 studies, 587 patients experienced pediatric proximal humerus fractures. These fractures were predominantly reported in boys (64%, n = 376), while girls accounted for only 36% (n = 211). Overall, 33% of the patients (n = 195) underwent operative treatment, whereas 67% of the patients (n = 392) received nonoperative treatment. However, surgeons frequently chose operative (n = 174) rather than nonoperative treatment (n = 117) for severely displaced proximal humerus fractures (Neer-Horwitz grade III/IV).
Operative Treatment Risk Factors in Pediatric Proximal Humerus Fractures
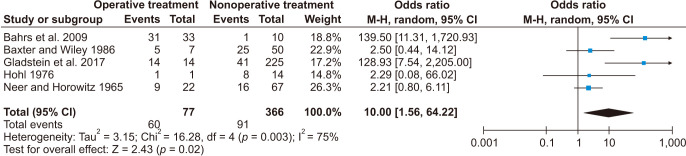
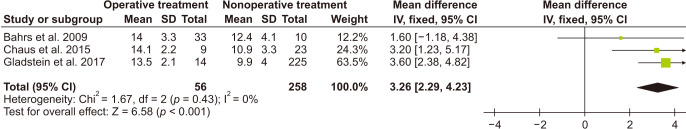
Among the demographic risk factors, severely displaced fractures (Neer-Horwitz grade III/IV; OR, 10.00; 95% CI, 1.56–64.2; p = 0.020) (Fig. 2) and older age (WMD, 3.26; 95% CI, 2.29–4.23; p < 0.001) (Fig. 3) were significantly associated with operative treatment in pediatric proximal humerus fractures (Table 3). However, there was no significant difference in the preference for percutaneous pinning or intramedullary nailing, the most frequently used surgical techniques (OR, 5.09; 95% CI, 0.65–39.58; p = 0.120).
Fig. 2. Forest plot showing the relationship between treatment strategy and fracture displacement. M-H: Mantel-Haenszel, CI: confidence interval, df: degrees of freedom.
Fig. 3. Forest plot showing the relationship between treatment strategy and age. SD: standard deviation, CI: confidence interval, df: degrees of freedom.
Table 3. Summary of Related Risks for Operative Treatment in Pediatric Proximal Humerus Fractures.
| Related factor | No. of studies | Test of difference | Test of heterogeneity | Model | ||
|---|---|---|---|---|---|---|
| OR/WMD (95% CI) | p-value | I2 (%) | p-value | |||
| Neer-Horwitz III and IV | 5 | OR, 10.00 (1.56−64.22) | 0.020* | 75 | 0.003 | R |
| Age | 3 | WMD, 3.26 (2.29−4.23) | < 0.001* | 0 | 0.430 | F |
| Surgical technique (percutaneous pinning/intramedullary nailing) | 2 | OR, 5.09 (0.65−39.58) | 0.120 | 86 | 0.007 | R |
OR: odds ratio, WMD: weighted mean difference, CI: confidence interval.
*Statistically significant.
Publication Bias
All funnel plots were symmetric, indicating the absence of a significant publication bias among the studies. The Egger’s test results for each factor were p = 0.282 (treatment strategy in severely displaced fractures) and p = 0.225 (treatment strategy depending on age). These results show that there is no clear evidence of publication bias in the dataset.
DISCUSSION
Controversy still exists with regard to the establishment of a treatment strategy (operative versus nonoperative) for pediatric proximal humeral fractures, particularly in severely displaced fractures and fractures in older children and adolescents. This meta-analysis aimed to identify the optimal strategy to treat pediatric proximal humeral fractures.
Classic studies dating from 1965 to 1990 uniformly recommended nonoperative treatment for most pediatric proximal humerus fractures, even severely displaced fractures, regardless of patient age,2,3,11,12,13,14,15,16) and operative treatment was only recommended in the case of open fractures and fractures associated with nerve or arterial injuries.7,8) In contrast, recent studies since the 1990s favor operative treatment more actively as age and displacement have become relative indications for operative treatment.4,5,7,17,18,19,20,21,22,23,24,25) As the paradigm of the treatment strategy for pediatric proximal humerus fractures presents a marked shift, the frequency of operative treatment has increased, reaching 46.4% in the United States in 2012.26)
Our study indicates that severe displacement of fractures (i.e. Neer-Horwitz grade III/IV) led to operative treatment. The rate of operative treatment for severely displaced fractures was 60%, whereas that for entire pediatric proximal humerus fractures was 33%. This concurs with previous reports that operative treatment was performed depending on fracture displacement.2,10,11,17,19) The rationale for operative treatment of severely displaced fractures is as follows: repeated attempts to achieve an acceptable reduction in these fractures can result in iatrogenic physeal injury or damage to the blood supply.12,22) This may be caused by periarticular soft-tissue entrapment, mostly due to the long head of the biceps tendon and the periosteum.8,17) Bahrs et al.17) suggested that failed closed reduction should be treated with open reduction to achieve anatomical reduction. In addition, these severely displaced fractures need supplementary internal fixation to minimize the risk of loss of reduction, even if satisfactory closed reduction has already been achieved.7,11,23) Hannonen et al.23) demonstrated that 10 out of 286 patients who underwent primary nonoperative treatment required delayed surgical intervention due to loss of primary reduction. Eventually, unresolved translation displacement may lead to a decrease in the strength and motion range of the shoulder joint as well as humeral length discrepancy,2,4,23) particularly in older patients.
This study also identified that older age is another factor determining operative treatment,17,19,20) as it is associated with a decrease in the remodeling capacity in older children and adolescents.2,8,24) The cut-off age varied from 12 to 15 years.2,7,21,27) Neer and Horwitz2) reported that patients older than 12 years required close, careful observation to achieve satisfactory outcomes. Burgos-Flores et al.21) demonstrated that patients older than 13 years with severely displaced fractures were likely to experience shoulder motion limitation and dysmetria. Beringer et al.27) emphasized the benefit of achieving anatomical reduction in children older than 15 years. Nonoperative treatment in these patients carries the risk of resulting in undesirable outcomes.20) Therefore, many authors judge these age groups as distinct patient populations and recommend strict operative treatment.2,4,7,17,21,22,25)
These results support the operative indications in the previous reports, which were established based on the degree of fracture displacement and age (Table 4). All of the studies have in common that surgical treatment is determined as the fracture becomes severely displaced or the patient ages. We have particularly concurred that Neer-Horwitz grade IV fractures or fractures with greater than 40° of angulation in patients older than 12 years of age are indications for operative treatment.18,19)
Table 4. Summary of Operative Indications of Pediatric Proximal Humerus Fractures in Previous Reports.
| Study | Year | Operative indication |
|---|---|---|
| Beaty5) | 1992 | Acceptable position |
| (1) age < 5 yr, 70° angulation and total displacement | ||
| (2) age 5–12 yr, 40°–70° angulation | ||
| (3) age > 12 yr, 40° angulation and 50% apposition | ||
| Burgos-Flores et al.21) | 1993 | Age > 13 yr, marked displacement or angulation |
| Schwendenwein et al.4) | 2001 | (1) age < 12 yr, angulation greater than 60° |
| (2) age ≥ 12 yr, angulation greater than 30° | ||
| Dobbs et al.7) | 2003 | Among Neer-Horwitz grade III and IV fractures, |
| (1) age ≤ 7 yr, angulation greater than 70° | ||
| (2) age 8 to 11 yr, angulation greater than 60° | ||
| (3) age ≥ 12 yr, angulation greater than 45° | ||
| Bahrs et al.17) | 2009 | (1) age < 10 yr, angular deformity > 60° or totally displaced |
| (2) age ≥ 10 yr, angular deformity > 30° or > 10° of valgus deformity or totally displaced | ||
| Shore et al.18) | 2015 | Age > 12 yr, Neer-Horwitz grade IV or angulation greater than 40° |
| Gladstein et al.19) | 2016 | Age > 12 yr, Neer-Horwitz grade IV or angulation greater than 40° |
| Binder et al.22) | 2016 | Age > 11 yr, angulation greater than 20° |
We could not verify which surgical technique was the most preferred technique for operative treatment in this meta-analysis. Proximal humerus fractures with physeal involvement tended to favor percutaneous pinning, as the healing process of physeal fractures is faster than that of metaphyseal or diaphyseal fractures.18) This can allow the leaving pins to be exposed for early removal. If the pins need to be retained longer than usual, it is recommended that they be buried beneath the skin. This is because if pins remain exposed for a prolonged time, pin-tract infection can occur. On the other hand, intramedullary nailing was mainly considered in diaphyseal fractures. This technique enables early rehabilitation without additional weeks-long immobilization.28) However, approximately 90% of patients who undergo intramedullary nailing require secondary removal surgery.18) Many previous reports reported that both surgical techniques showed safe and excellent clinical outcomes without major complications.7,18,28,29,30) Therefore, the choice between them might seem to be based entirely on the surgeon’s judgment according to the anatomical location of the fracture.
This meta-analysis has some limitations. First, only 8 retrospective studies were selected for the meta-analysis. This may affect the reliability of the study results. Second, the patients, operative indications, and preferred surgical techniques may vary in each center. Finally, an approach to reporting outcomes was expressed in an inconsistent manner among the included studies; therefore, it could not be analyzed in our meta-analysis. Despite these limitations, we believe this study will broaden and deepen the understanding of pediatric proximal humeral fractures and provide a potential treatment strategy. However, the definite establishment of treatment guidelines may require further analysis using more rigorous scientific methods.
In conclusion, our results indicate that severely displaced fractures and older age significantly contributed to establishing a treatment strategy for operative treatment. The choice of surgical technique may seem to be based on the anatomical location of the fracture rather than the surgeon’s preference.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Landin LA. Epidemiology of children's fractures. J Pediatr Orthop B. 1997;6(2):79–83. doi: 10.1097/01202412-199704000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Neer CS, 2nd, Horwitz BS. Fractures of the proximal humeral epiphysial plate. Clin Orthop Relat Res. 1965;41:24–31. [PubMed] [Google Scholar]
- 3.Dameron TB, Jr, Reibel DB. Fractures involving the proximal humeral epiphyseal plate. J Bone Joint Surg Am. 1969;51(2):289–297. [PubMed] [Google Scholar]
- 4.Schwendenwein E, Hajdu S, Gaebler C, Stengg K, Vecsei V. Displaced fractures of the proximal humerus in children require open/closed reduction and internal fixation. Eur J Pediatr Surg. 2004;14(1):51–55. doi: 10.1055/s-2004-815781. [DOI] [PubMed] [Google Scholar]
- 5.Beaty JH. Fractures of the proximal humerus and shaft in children. Instr Course Lect. 1992;41:369–372. [PubMed] [Google Scholar]
- 6.Shrader MW. Proximal humerus and humeral shaft fractures in children. Hand Clin. 2007;23(4):431–435. doi: 10.1016/j.hcl.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 7.Dobbs MB, Luhmann SL, Gordon JE, Strecker WB, Schoenecker PL. Severely displaced proximal humeral epiphyseal fractures. J Pediatr Orthop. 2003;23(2):208–215. [PubMed] [Google Scholar]
- 8.Di Gennaro GL, Spina M, Lampasi M, Libri R, Donzelli O. Fractures of the proximal humerus in children. Chir Organi Mov. 2008;92(2):89–95. doi: 10.1007/s12306-008-0050-7. [DOI] [PubMed] [Google Scholar]
- 9.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339(7716):b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hohl JC. Fractures of the humerus in children. Orthop Clin North Am. 1976;7(3):557–571. [PubMed] [Google Scholar]
- 11.Baxter MP, Wiley JJ. Fractures of the proximal humeral epiphysis: their influence on humeral growth. J Bone Joint Surg Br. 1986;68(4):570–573. doi: 10.1302/0301-620X.68B4.3733832. [DOI] [PubMed] [Google Scholar]
- 12.Aitken AP. Fractures of the proximal humeral epiphysis. Surg Clin North Am. 1963;43:1573–1580. doi: 10.1016/s0039-6109(16)37146-8. [DOI] [PubMed] [Google Scholar]
- 13.Smith FM. Fracture-separation of the proximal humeral epiphysis; a study of cases seen at the Presbyterian Hospital from 1929-1953. Am J Surg. 1956;91(4):627–635. doi: 10.1016/0002-9610(56)90296-3. [DOI] [PubMed] [Google Scholar]
- 14.McBride ED, Sisler J. Fractures of the proximal humeral epiphysis and the juxta-epiphysial humeral shaft. Clin Orthop Relat Res. 1965;38:143–153. [PubMed] [Google Scholar]
- 15.Kohler R, Trillaud JM. Fracture and fracture separation of the proximal humerus in children: report of 136 cases. J Pediatr Orthop. 1983;3(3):326–332. doi: 10.1097/01241398-198307000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Larsen CF, Kiaer T, Lindequist S. Fractures of the proximal humerus in children: nine-year follow-up of 64 unoperated on cases. Acta Orthop Scand. 1990;61(3):255–257. doi: 10.3109/17453679008993512. [DOI] [PubMed] [Google Scholar]
- 17.Bahrs C, Zipplies S, Ochs BG, et al. Proximal humeral fractures in children and adolescents. J Pediatr Orthop. 2009;29(3):238–242. doi: 10.1097/BPO.0b013e31819bd9a7. [DOI] [PubMed] [Google Scholar]
- 18.Shore BJ, Hedequist DJ, Miller PE, Waters PM, Bae DS. Surgical management for displaced pediatric proximal humeral fractures: a cost analysis. J Child Orthop. 2015;9(1):55–64. doi: 10.1007/s11832-015-0643-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gladstein AZ, Schade AT, Howard AW, Camp MW. Reducing resource utilization during non-operative treatment of pediatric proximal humerus fractures. Orthop Traumatol Surg Res. 2017;103(1):115–118. doi: 10.1016/j.otsr.2016.09.022. [DOI] [PubMed] [Google Scholar]
- 20.Chaus GW, Carry PM, Pishkenari AK, Hadley-Miller N. Operative versus nonoperative treatment of displaced proximal humeral physeal fractures: a matched cohort. J Pediatr Orthop. 2015;35(3):234–239. doi: 10.1097/BPO.0000000000000265. [DOI] [PubMed] [Google Scholar]
- 21.Burgos-Flores J, Gonzalez-Herranz P, Lopez-Mondejar JA, Ocete-Guzman JG, Amaya-Alarcon S. Fractures of the proximal humeral epiphysis. Int Orthop. 1993;17(1):16–19. doi: 10.1007/BF00195216. [DOI] [PubMed] [Google Scholar]
- 22.Binder H, Tiefenboeck TM, Payr S, Schurz M, Aldrian S, Sarahrudi K. Treatment of proximal humerus fractures in children and young adolescents. Wien Klin Wochenschr. 2016;128(3-4):120–124. doi: 10.1007/s00508-015-0879-3. [DOI] [PubMed] [Google Scholar]
- 23.Hannonen J, Hyvonen H, Korhonen L, Serlo W, Sinikumpu JJ. The incidence and treatment trends of pediatric proximal humerus fractures. BMC Musculoskelet Disord. 2019;20(1):571. doi: 10.1186/s12891-019-2948-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wei SW, Shi ZY, Zhao YM, et al. Comparison of conservative treatment outcomes for proximal humeral epiphyseal fractures in patients of different ages. Orthopade. 2019;48(2):119–124. doi: 10.1007/s00132-018-03677-3. [DOI] [PubMed] [Google Scholar]
- 25.Pahlavan S, Baldwin KD, Pandya NK, Namdari S, Hosalkar H. Proximal humerus fractures in the pediatric population: a systematic review. J Child Orthop. 2011;5(3):187–194. doi: 10.1007/s11832-011-0328-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cruz AI, Jr, Kleiner JE, Gil JA, Goodman AD, Daniels AH, Eberson CP. Inpatient surgical treatment of paediatric proximal humerus fractures between 2000 and 2012. J Child Orthop. 2018;12(2):111–116. doi: 10.1302/1863-2548.12.170220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Beringer DC, Weiner DS, Noble JS, Bell RH. Severely displaced proximal humeral epiphyseal fractures: a follow-up study. J Pediatr Orthop. 1998;18(1):31–37. [PubMed] [Google Scholar]
- 28.Fernandez FF, Eberhardt O, Langendorfer M, Wirth T. Treatment of severely displaced proximal humeral fractures in children with retrograde elastic stable intramedullary nailing. Injury. 2008;39(12):1453–1459. doi: 10.1016/j.injury.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 29.Pandya NK, Behrends D, Hosalkar HS. Open reduction of proximal humerus fractures in the adolescent population. J Child Orthop. 2012;6(2):111–118. doi: 10.1007/s11832-012-0398-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pogorelic Z, Kadic S, Milunovic KP, Pintaric I, Jukic M, Furlan D. Flexible intramedullary nailing for treatment of proximal humeral and humeral shaft fractures in children: a retrospective series of 118 cases. Orthop Traumatol Surg Res. 2017;103(5):765–770. doi: 10.1016/j.otsr.2017.02.007. [DOI] [PubMed] [Google Scholar]