Abstract
We present the case of a vulval superficial myofibroblastoma with a lymphocytic and eosinophilic rim in a woman in her late 20s. The tumour presented in pregnancy as a cystic lesion with pain and increasing size. While the histopathology of superficial myofibroblastomas has been well defined in the literature, to our knowledge, there has been no documentation of the presence of an inflammatory infiltrate of lymphocytes and eosinophils surrounding and within the tumour. This may potentially act as a diagnostic or prognostic reference.
Keywords: Pathology, Obstetrics and gynaecology
Background
Superficial myofibroblastomas are rare benign mesenchymal tumours theorised to arise from subepithelial tissue of the female lower genital tract.1 Most commonly, they are seen in the vagina but also occur in the cervix and vulva. Less than 60 cases have been reported.2–12 No more than seven cases relate specifically to the vulva.2 3 8 10 11 There is a wide age range from 23 to 80 years.1 They can vary greatly in size, with reports up to 6.5 cm.1 13 Macroscopically, they are well circumscribed and solid.1 13 On microscopy, the superficial myofibroblastomas show a grenz zone and are composed of a bland spindle cell population.1 13 The spindle cells usually do not follow any distinct patterns but they may have lace-like, sieve-like or fascicular patterns with a collagenous stroma and wavy nucleus.1 13 Immunohistochemistry is usually positive for vimentin, desmin and oestrogen and progesterone receptors.1 13 While they have a benign course, local recurrence may potentially occur years later.2 By writing this case report of this relatively rare condition, we hope to be able to increase recognition of this tumour by introducing a diagnostic reference of an inflammatory infiltrate around the rim of the tumour.
Case presentation
A woman in her late 20s first noticed a pea-sized right vulval soft mass at the end of her second trimester. On examination, a soft 3 cm mass, presumed cystic, was located at 7–8 o’clock on the vulva within the right posterior labia majora near the location of Bartholin’s gland. Drainage was attempted during delivery but failed. She returned 8 weeks post partum for an examination under anaesthesia and underwent an excision.
The patient had a history of genital warts and low-grade squamous intraepithelial lesion on a previous Pap smear, but no other significant medical history or family history was elicited.
Investigations
Pathological examination showed a soft solid cream mass in the dermis with a normal overlying epidermis. On microscopy, a well-demarcated spindle cell tumour was observed beneath a grenz zone (figure 1). The tumour had a rim of lymphocytes and eosinophils and these were also seen around the blood vessels within the tumour itself (figure 2). The tumour was composed of bland spindle cells with short wavy nuclei and hyalinised or oedematous matrix (figure 3). Small blood vessels were scattered throughout. No infiltration of adjacent dermis, atypia or mitoses were seen. Immunostaining showed tumour cells strongly positive for oestrogen receptor (figure 4). Scattered small blood vessels were highlighted CD34 (figure 5). Tumour cells were negative for smooth muscle actin, STAT6, desmin, S100, CD34, ALK1 and HMB45. The deep margin was involved.
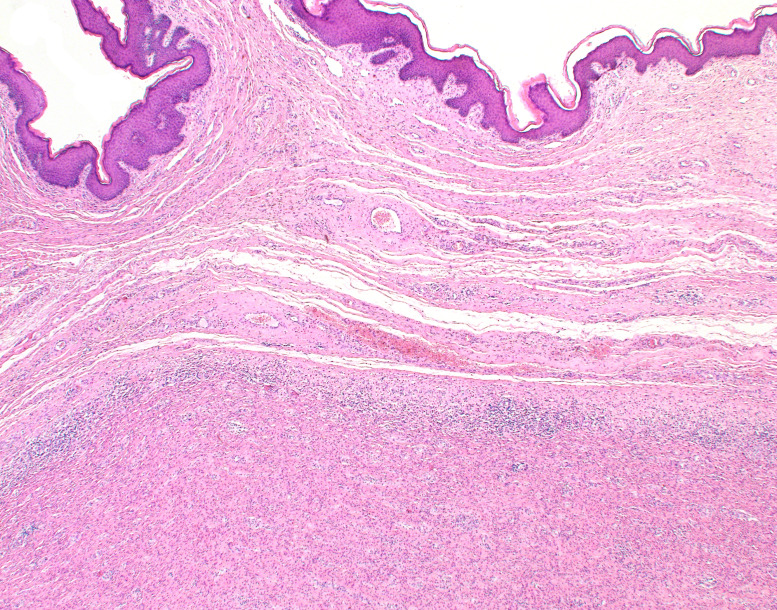
Figure 1.
Grenz zone between epidermis and dermal spindle cell tumour with rim of inflammatory cells (H&E×20).
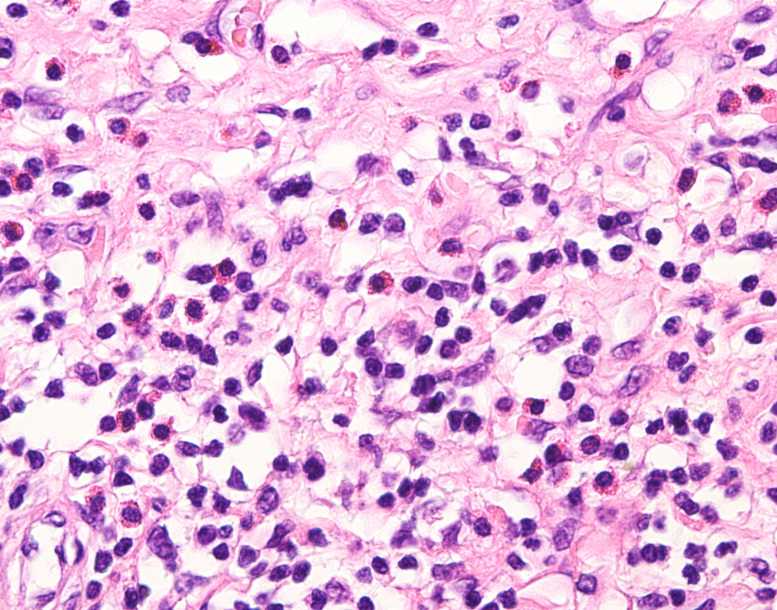
Figure 2.
Rim of lymphocytes with occasional eosinophils (H&E×400).
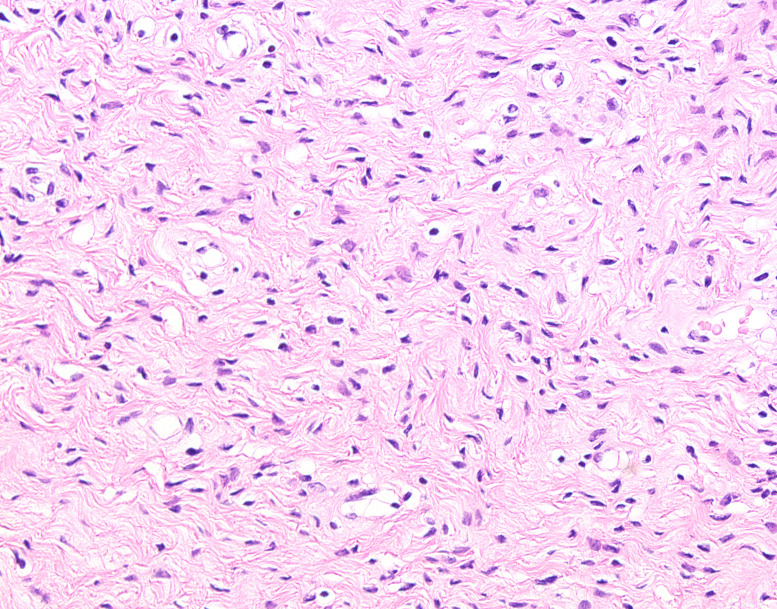
Figure 3.
Bland spindle cell proliferation (H&E×200).
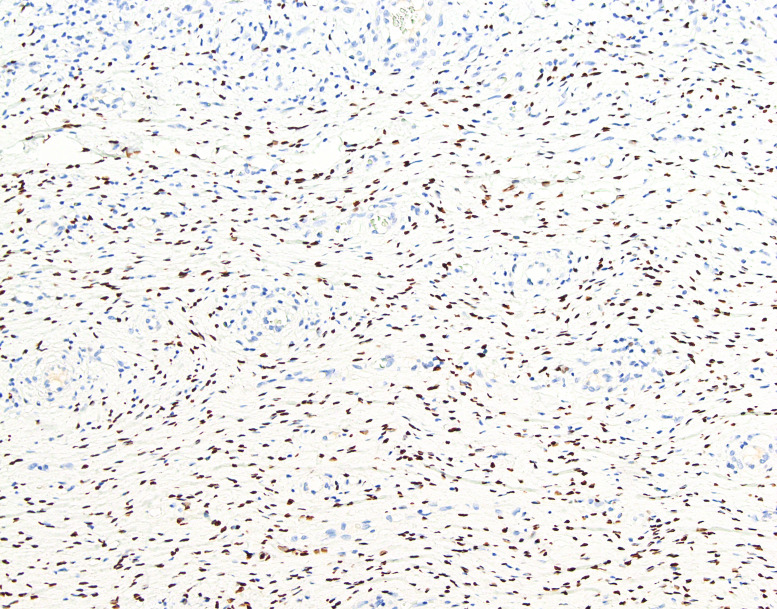
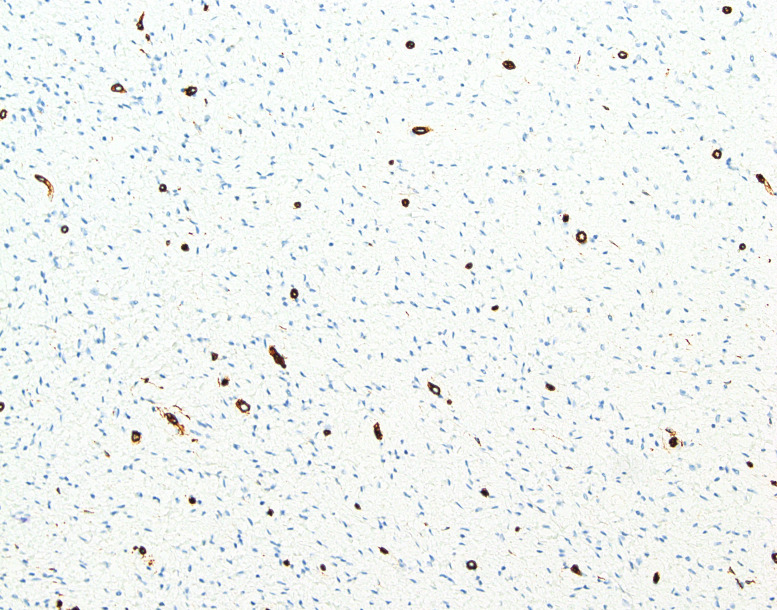
Figure 4.
Positive oestrogen receptor staining in spindle cell nuclei (IPX×100).
Figure 5.
Scattered small blood vessels stained with CD34 (IPX×100).
Differential diagnosis
Angiomyofibroblastoma and cellular angiofibroma are other genital mesenchymal tumours occurring on the vulva.1 13 Like superficial myofibroblastoma, they are circumscribed and have positive oestrogen receptors.1 13 However, these tumours differ from superficial myofibroblastoma by having numerous thick and thin-walled blood vessels compared with the evenly distributed small blood vessels in our case.
Inflammatory myofibroblastic tumour (IMT) is a mesenchymal tumour with admixed inflammatory cells, principally lymphocytes which may occur in many sites in the body.13 14 Our case was negative for ALK1, which is the key marker for IMT.13–15 Also, IMT has not been reported on the vulva outside of a neonatal case.16
Treatment
Vulval mass excised.
Outcome and follow-up
The patient recovered well from the procedure on follow-up 6 weeks after and did not have any complaints. She presented for a follow-up 6 months postexcision and reported that the surgical site has healed well.
Discussion
Superficial myofibroblastomas are rare benign tumours of the female lower genital tract, with most cases reported in the literature occurring in the vagina.1–13
Here, we report a vulval superficial myofibroblastoma with an unusual finding of an inflammatory infiltrate consisting of lymphocytes and eosinophils at the rim and also within the tumour. While mast cells and lymphoid aggregates have been reported in superficial myofibroblastoma, we can find no existing report of an infiltrate of lymphocytes with rimming the tumour. If this finding is replicated by others, it could potentially act as a recognition aid of the tumour itself.
The tumour in our case was positive for oestrogen receptor which may explain its growth in pregnancy. Our tumour was negative for smooth muscle actin, STAT6, desmin, S100, CD34, ALK1 and HMB45. The negative muscle stains are unusual in superficial myofibroblastoma. However, there has been one case reported with similarly negative desmin.2
Patient’s perspective.
Future patients may be helped by their medical teams by using this case report to more accurately diagnose this rare tumour.
Learning points.
Presence of inflammatory infiltrate around spindle cell tumours can aid recognition or act as prognostic factor and indicate a possible diagnosis of superficial myofibroblastoma.
Immunohistochemistry may not be helpful in differentiating between similar tumours, necessitating a more comprehensive set of histological features to improve diagnostic accuracy.
Footnotes
Contributors: QTT drafted and edited the article for the case report and took scientific photographs of the histological samples. TM is the treating doctor of the patient, obtained informed consent from the patient for the article and edited the article. JPS is the designated pathologist for the patient case, observed and interpreted significance of the findings and critically reviewed and edited the article.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Case reports provide a valuable learning resource for the scientific community and can indicate areas of interest for future research. They should not be used in isolation to guide treatment choices or public health policy.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
References
- 1.Ganesan R, Howitt BE. Superficial myofibroblastoma. In: WHO classification of tumours editorial board, editor. WHO classification of tumours series, 5th ed; vol 4. Lyon (France): International Agency for Research on Cancer, 2020: 490. [Google Scholar]
- 2.Ganesan R, McCluggage WG, Hirschowitz L, et al. Superficial myofibroblastoma of the lower female genital tract: report of a series including tumours with a vulval location. Histopathology 2005;46:137–43. 10.1111/j.1365-2559.2005.02063.x [DOI] [PubMed] [Google Scholar]
- 3.Magro G, Caltabiano R, Kacerovská D, et al. Vulvovaginal myofibroblastoma: expanding the morphological and immunohistochemical spectrum. A clinicopathologic study of 10 cases. Hum Pathol 2012;43:243–53. 10.1016/j.humpath.2011.04.027 [DOI] [PubMed] [Google Scholar]
- 4.Laskin WB, Fetsch JF, Tavassoli FA. Superficial cervicovaginal myofibroblastoma: fourteen cases of a distinctive mesenchymal tumor arising from the specialized subepithelial stroma of the lower female genital tract. Human Pathology 2001;32:715–25. 10.1053/hupa.2001.25588 [DOI] [PubMed] [Google Scholar]
- 5.R. Stewart CJ, Amanuel B, Brennan BA, et al. Superficial cervico-vaginal myofibroblastoma: a report of five cases. Pathology 2005;37:144–8. 10.1080/00313020500058284 [DOI] [PubMed] [Google Scholar]
- 6.Olinici CD, Crişan D, Zolog A, et al. Vaginal superficial myofibroblastoma. Case report and review of the literature. Rom J Morphol Embryol 2007;48:165–70. [PubMed] [Google Scholar]
- 7.Wang Q, Wu Y, Wang J. Superficial cervicovaginal myofibroblastoma: report of four cases and literature review. Chin Med J (Engl) 2010;123:1093–6. 10.3760/cma.j.issn.0366-6999.2010.08.022 [DOI] [PubMed] [Google Scholar]
- 8.Patrizi L, Borelli B, Di Prete M, et al. A rare case of vulvar superficial myofibroblastoma associated with ambigous and unusual differential diagnosis. Gynecol Oncol Rep 2020;34:100637. 10.1016/j.gore.2020.100637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Atinga A, El-Bahrawy M, Stewart V, et al. Superficial myofibroblastoma of the genital tract: a case report of the imaging findings. BJR Case Rep 2019;5:20180057. 10.1259/bjrcr.20180057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peng WX, Wada R, Kure S, et al. Superficial myofibroblastoma in the vulva mimicking aggressive angiomyxoma: a case report and review of the literature. Case Rep Pathol 2019;2019:1582714. 10.1155/2019/1582714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harou K, Ouchraa J, Houari S, et al. Superficial myofibroblastoma: unusual hymenal localization. Sch Int J Obstet Gynec 2020;03:27–30. 10.36348/sijog.2020.v03i02.001 [DOI] [Google Scholar]
- 12.Liu J-L, Su T-C, Shen K-H, et al. Vaginal superficial myofibroblastoma: a rare mesenchymal tumor of the lower female genital tract and a study of its association with viral infection. Med Mol Morphol 2012;45:110–4. 10.1007/s00795-011-0566-z [DOI] [PubMed] [Google Scholar]
- 13.Clement PB, Stall JN, Young RH. Atlas of gynaecologic surgical pathology 4th ed. Netherlands: Elsevier, 2000: 25-6, 293-4. [Google Scholar]
- 14.Parra-Herran C, Lee CH, Bennett JA, et al. Inflammatory myofibroblastic tumour. In: WHO classification of tumours editorial board, editor. WHO classification of tumours series, 5th ed; vol 4. Lyon (France): International Agency for Research on Cancer, 2020: 298–9. [Google Scholar]
- 15.Pickett JL, Chou A, Andrici JA, et al. Inflammatory myofibroblastic tumors of the female genital tract are under-recognized. Am J Surg Pathol 2017;41:1433–42. 10.1097/PAS.0000000000000909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lenh B-V, Duc NM, My T-TT, et al. A rare case of inflammatory myofibroblastic tumor of the vulva in a newborn. Radiol Case Rep 2021;16:1352–4. 10.1016/j.radcr.2021.03.020 [DOI] [PMC free article] [PubMed] [Google Scholar]