Abstract
Objectives
Patients with systemic rheumatic diseases (SRDs) are at risk of admission to the intensive care unit (ICU). Data concerning these critically ill patients are limited to few retrospective studies.
Methods
This is a single-centre retrospective study of patients with SRDs admitted to an ICU at the Vienna General Hospital between 2012 and 2020. Single-predictor and multiple logistic regression analysis was performed to identify potential outcome determinants.
Results
A total of 144 patients accounting for 192 ICU admissions were included. Connective tissue diseases (CTDs), vasculitides and rheumatoid arthritis were the most common SRDs requiring ICU admission. Leading causes for ICU admission were respiratory failure and shock, as reflected by a high number of patients requiring mechanical ventilation (60.4%) and vasopressor therapy (72.9%). Overall, 29.2% of admissions were due to SRD-related critical illness. In 70.8% patients, co-existent SRD not responsible for the acute critical illness was documented. When comparing these subgroups, CTDs and vasculitides had a higher frequency in the patients with SRD-related critical illness. In a significantly higher proportion of patients in the SRD-related subgroup, diagnosis of SRD was made at the ICU. ICU and 6-month mortality in the overall population was 20.3% and 38.5%, respectively. Age, glucocorticoid therapy prior to hospital admission and disease severity were associated with poor outcome.
Conclusions
In this study, respiratory failure was the leading cause of ICU admission as reflected by high rates of required mechanical ventilation. Despite considerable severity of critical illness, survival rates were comparable to a general ICU population.
Keywords: autoimmune diseases, cardiovascular diseases, epidemiology, immune system diseases, inflammation
WHAT IS ALREADY KNOWN ON THIS TOPIC.
Data concerning these critically ill patients are limited to few retrospective studies mainly focusing on epidemiologic and demographic descriptions. In addition, these studies do not distinguish between the worsening of pre-existing rheumatic diseases as the predominant reason for intensive care unit (ICU) admission versus rheumatic conditions being merely comorbidities.
WHAT THIS STUDY ADDS
This study is the first to describe a systemic rheumatic disease (SRD) patient cohort in Central Europe. We performed a comprehensive analysis of critically ill patients with SRDs regarding the predominant reason for ICU admission (SRD-related or co-existent SRD).
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Our study advances the characterisation and understanding of patients with SRDs requiring intensive care treatment. The classification of the reasons for ICU admission in ‘SRD-related’ and ‘co-existent SRD’ has major clinical implications as these two constellations need specific therapeutic approaches.
Introduction
Enhanced pathophysiological understanding and the introduction of novel immunosuppressive and immunomodulatory drugs have significantly improved the prognosis of patients suffering from systemic rheumatic diseases (SRDs) over the last two decades.1 Despite these substantial improvements, patients with SRDs remain susceptible to life-threatening conditions that may necessitate admission to an intensive care unit (ICU). ICU admission of patients with SRDs is primarily required for acute exacerbation or flare of the underlying rheumatic disease and infections.2–4 Respiratory failure has been reported to be the leading cause for requiring critical care in patients with SRDs.2–8 The two major reasons for respiratory insufficiency are infections (especially pneumonia) and the exacerbation of the SRD itself, primarily manifesting as pulmonary oedema, diffuse alveolar haemorrhage and interstitial lung disease.2 3 7 8 Shock (septic, cardiogenic and hypovolemic) has also been recognised as a significant factor necessitating ICU admission in a substantial proportion of patients with SRDs.2 3 Other acute problems observed in this population include acute kidney injury, cardiac involvement (eg, congestive heart failure, arrhythmia) and neurologic dysfunction (eg, seizure, stroke).2–4 8
Data on critically ill patients with SRDs is limited and mainly focuses on demographic and epidemiologic findings. Furthermore, existing studies frequently describe patient cohorts with heterogeneous disease frequencies and reasons for ICU admission. Lack of discrimination between worsening of pre-existing rheumatic diseases and comorbid rheumatic conditions makes valid comparisons difficult. Consequently, current literature reports ICU mortality rates among patients with SRDs ranging from 11% to 79% across various studies.2–11 Age, severity of the acute medical condition, mechanical ventilation, the requirement for vasopressor drugs or renal replacement therapy (RRT) and ICU admission due to infectious complications have been identified as factors associated with higher mortality rates.2–4 8 10 12 However, data regarding different treatment modalities for SRDs (eg, use of immunosuppressive/immunomodulatory drugs) prior to or during ICU stay and differences in outcome are scarce. In only one retrospective study, high doses of glucocorticoids (GCs) and immunosuppressive drugs before ICU admission were associated with a worse outcome in critically ill patients with SRDs.13
Within the scope of this study, we delineated clinical features, outcome parameters and potential mortality predictors of an SRD patient cohort from a large tertiary centre in Central Europe.
Methods
Patients and study design
Since 2012, electronic patient charts have been used at all ICUs at the Medical University of Vienna enabling a complete documentation of crucial patient characteristics including diagnosis, physical examination, vital signs, laboratory tests as well as therapy and medication. Patients were included retrospectively between 1 st January 2012 and 31 st December 2020 at 11 ICU wards (medical, anesthesiological and surgical). For our study, potentially eligible patients were identified by screening electronic patient charts for SRDs using the 10th revision of the International Classification of Diseases (ICD-10). These patients were then assessed for study eligibility. Patients under the age of 18, patients with no SRD due to false coding, patients with an ICU length of stay<1 day and patients after scheduled surgery or trauma were excluded.
Diagnosis of the underlying rheumatologic disease was established according to internationally accepted and validated criteria, such as the classification criteria by the EULAR and the American College of Rheumatology.14–22
SRDs were categorised into the following groups:
Connective tissue disease (CTD) including systemic lupus erythematosus, Sjögren’s syndrome, idiopathic inflammatory myopathies, systemic sclerosis, mixed CTD and overlap syndromes.
Vasculitides including granulomatosis with polyangiitis, microscopic polyangiitis, eosinophilic granulomatosis with polyangiitis, polyarteritis nodosa, Goodpasture syndrome and large vessel vasculitides.
Rheumatoid arthritis (RA).
Seronegative spondyloarthropathies (SpA) including axial spondyloarthritis, psoriatic arthritis and arthritis associated with inflammatory bowel disease.
Others including adult-onset Still’s disease, primary antiphospholipid syndrome, deficiency of adenosine deaminase 2, Sweet’s syndrome, familial Mediterranean fever, sarcoidosis and Behçet’s disease.
This study followed the recommendations of the Strengthening the Reporting of Observational Studies in Epidemiology initiative for reporting observational studies in epidemiology.
Data collection
During the study period, 144 patients accounted for 192 ICU admissions. Following established literature, each admission was treated as an independent observation for statistical analyses.2 The 192 ICU admissions were categorised into two groups: ICU admission due to exacerbation of an underlying SRD (SRD-related cohort) and the development of critical illness with a concomitant SRD (co-existent SRD cohort). SRD exacerbation was defined as disease manifestation induced by the SRD itself, as determined by clinical, immunologic and histologic findings, as well as data regarding initiation, modification or escalation of immunosuppressive/immunomodulatory or antibiotic therapy. In the case of SRD exacerbation due to infection, these cases were assigned to the co-existent SRD cohort and not the SRD-related cohort. If the categorisation could not be definitively determined from robust evidence extracted from the patient’s medical records, the cause of admission was discussed with two independent reviewers until a consensus was achieved.
In addition, we included a control group comprising 1808 ICU patients without SRD. These patients were drawn from medical ICUs during the same study period (ie, 2012–2020). This group represents a general ICU population with solely medical background. Postoperative/postinterventional and trauma patients were excluded.
Reasons for ICU admission were defined as shock (ie, hyperinflammatory, haemorrhagic, septic, cardiogenic, hypovolemic and anaphylactic),23 cardiogenic events (ie, myocardial infarction, cardiac arrest, hypertensive crisis, arrhythmia, pulmonary embolism), respiratory failure (ie, interstitial lung disease, diffuse alveolar haemorrhage, pneumonitis, pneumonia, pulmonary oedema, chronic obstructive pulmonary disease exacerbation, pulmonary arterial hypertension),24–26 neurologic impairment (ie, epilepsy, coma, meningitis, stroke, cerebral haemorrhage), acute surgery (ie, cardiac surgery, bowel surgery, endovascular intervention) and other causes (ie, acute kidney injury, acute liver injury/failure, acute-on-chronic liver failure, pancreatitis)27 28 according to previously established criteria. As infectious diseases were only present in the co-existent SRD cohort, infections causing ICU admission were primarily included in one of the aforementioned subgroups: sepsis/septic shock in the ‘shock group’, pneumonia in the ‘respiratory failure’ group and meningitis in the ‘neurologic impairment’ group.
SRD-related organ involvement on ICU admission was recorded based on available (current or earlier) clinical, laboratory, immunological and histopathological findings. Two independent rheumatologists reviewed all patients’ charts and SRD-related organ involvement was defined according to previously published criteria.14–20
The severity of critical illness was calculated within the first 24 hours of ICU admission using the following scores: Simplified Acute Physiology Score II (SAPSII), Sequential Organ Failure Assessment (SOFA) Score and Acute Physiology and Chronic Health Evaluation II (APACHEII) Score.29–31 To assess the patients’ prior health status, Charlson Comorbidity Index (CCI) was evaluated.32 Throughout the ICU stay, data on laboratory results, life-sustaining therapies (mechanical ventilation, vasopressor support, organ replacement therapy) and immunosuppressive/immunomodulatory treatment approaches [ie, high-dose/pulse corticosteroids, conventional immunosuppressive agents (ie, methotrexate, mycophenolate mofetil, azathioprine, tacrolimus, everolimus, ciclosporin, leflunomide, hydroxychloroquine sulfasalazine), immunoglobulins, cytotoxic agents (ie, cyclophosphamide, bleomycin, vinblastine, dacarbazine, doxorubicin, cytarabine), biologicals (tyrosine kinase inhibitors and antibodies)] were documented. To account for the development and approval of new antirheumatic therapies between 2012 and 2020, the frequency of each immunosuppressive/immunomodulatory drug class and the outcome in two distinct periods, 2012–2016 and 2017–2020, were analysed.
Subsequently to ICU admission, ICU and hospital length of stay, ICU and hospital mortality as well as ICU readmission were recorded. We assessed the long-term outcome within 28 days of the ICU admission, 3 and 6 months after the ICU admission.
Statistical analysis
Quantitative parameters are presented as median (IQR), and qualitative parameters are presented as numbers (%). In the case of normal distribution, metric variables were compared between the groups using t-test. To identify differences in baseline characteristics, Pearson’s χ2 test for categorical variables and the Mann-Whitney U test for non-parametric variables were used. ICU mortality was analysed as a major outcome variable.
To identify the factors contributing to the 28-day survival probability, logistic regression was applied. In the first step, the influence of selected variables, independent of other variables, was investigated. To this end, variables of interest were entered into single-predictor models. In the second step, multivariate models were formulated. Variable selection was informed by the existing literature.33 ORs were derived for all predictors by computing their exponential values. In addition, 95% Wald CIs were calculated for each predictor. Pseudo-R2 was calculated for each model using Nagelkerke’s method.34 For variables that exhibited skewed distribution shapes, logarithmic transformation with a base of 2 was carried out. To handle negative data, we took the absolute value of data points<0, computed the logarithm and subsequently assigned the resulting number its original sign. To facilitate parameter interpretation within logistic regression, interval-scaled variables that did not exhibit skewed distribution shapes were standardised by subtracting the variable’s mean from each value and dividing it by its SD. Throughout all analyses, we did not apply type-II error adjustment, such as the Bonferroni adjustment, due to its detrimental effects on statistical power.35 Logistic regression and predictor transformation were carried out using R V.4.1.0; figures were created using ggplot2.36
Results
Overall ICU admissions
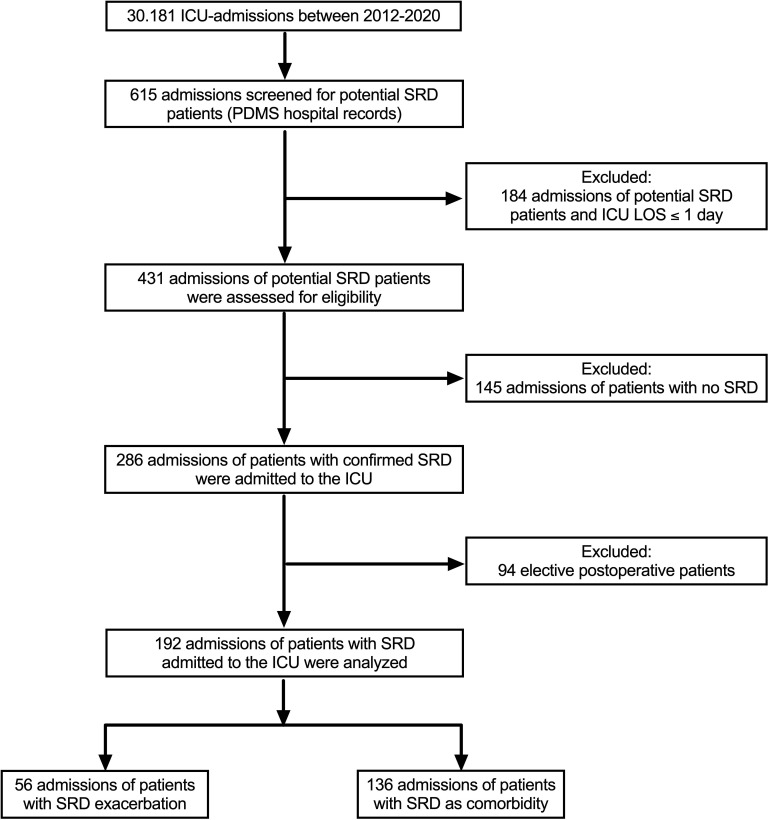
In total, 144 adult patients with SRDs admitted to the ICU directly from the emergency room, inpatient wards or other hospitals were included and analysed in our study (figure 1). These patients accounted for 192 admissions. The number of ICU admissions and outcomes per year are shown in online supplemental figure 1. The basic characteristics are depicted in table 1. The most common SRDs requiring ICU admission were CTDs, vasculitides and RA. The respiratory system, kidneys, gastrointestinal tract/liver and blood/coagulation were the most frequent SRD-related organ involvements observed at ICU admission. In 42.7% of all cases, two or more organ systems were affected by the SRD. The vast majority of ICU admissions at our tertiary centre originated from a normal ward not specialised for rheumatic diseases, followed by other ICUs/the emergency room and the normal ward of the department of rheumatology. A considerable proportion of patients (10.9%) received the diagnosis of their SRD in the ICU, meaning they had neither received such a diagnosis nor respective treatment previously. Thus, on ICU admission, 24% of patients had not received any form of disease-modifying antirheumatic drug and 13% were GC naive. The leading cause of ICU admission was respiratory failure, followed by shock, cardiogenic events and neurological impairment. Data on ICU-specific therapies and major outcome parameters are depicted in tables 2 and 3.
Figure 1.
Flowchart of the study population. ICU, intensive care unit; LOS, length of stay; PDMS, patient data management system; SRD, systemic rheumatic disease.
Table 1.
Basic characteristics
| Variable | All admissions (n=192) | SRD related (n=56) | Co-existent SRD (n=136) | P value |
| Age (years), median (IQR) | 61 (45–71) | 45 (30–64) | 65 (51–73) | <0.001 |
| Female sex (%) | 120 (62.5) | 38 (67.9) | 82 (60.3) | 0.325 |
| SOFA, median (IQR) | 9 (6–11) | 9 (7–12) | 9 (6–11) | 0.354 |
| SAPSII, median (IQR) | 45 (35–55) | 41 (27–49) | 46 (38–57) | 0.006 |
| APACHEII, median (IQR) | 21 (16–26.3) | 18 (14–25) | 23 (17–27) | 0.005 |
| CCI, median (IQR) | 4 (3–6) | 3 (1–5) | 5 (4–6) | <0.001 |
| SRD diagnosed in ICU, No. (%) | 21 (10.9) | 16 (28.6) | 5 (3.7) | <0.001 |
| SRD type | ||||
| CTD, No. (%) | 59 (30.7) | 24 (42.9) | 35 (25.7) | 0.025 |
| Vasculitis, No. (%) | 55 (28.6) | 24 (42.9) | 31 (22.8) | 0.008 |
| RA, No. (%) | 35 (18.2) | 1 (1.8) | 34 (25.0) | <0.001 |
| SpA, No. (%) | 12 (6.3) | 0 (0) | 12 (8.8) | 0.019 |
| Other, No. (%) | 31 (16.1) | 7 (12.5) | 24 (17.6) | 0.518 |
| SRD-related organ involvement | ||||
| Respiratory system, No. (%) | 88 (45.8) | 42 (75.0) | 46 (33.8) | <0.001 |
| Nervous system, No. (%) | 17 (8.9) | 12 (21.4) | 5 (3.7) | <0.001 |
| Heart and circulation, No. (%) | 14 (7.3) | 8 (14.3) | 6 (4.4) | 0.029 |
| GI and liver, No. (%) | 34 (17.7) | 13 (23.2) | 21 (15.4) | 0.302 |
| Blood and coagulation, No. (%) | 29 (15.1) | 13 (23.2) | 16 (11.8) | 0.074 |
| Kidney | 67 (34.9) | 35 (62.5) | 32 (23.5) | <0.001 |
| ≥2 organ involvements, No. (%) | 82 (42.7) | 44 (78.6) | 38 (27.9) | <0.001 |
| Reason for ICU admission | ||||
| Shock, No. (%) | 46 (24.0) | 9 (16.1) | 37 (27.2) | 0.136 |
| Cardiogenic event, No. (%) | 22 (11.5) | 1 (1.8) | 21 (15.4) | 0.005 |
| Respiratory failure, No. (%) | 91 (47.4)* | 32 (57.1) | 59 (43.4)* | 0.111 |
| Neurologic failure, No. (%) | 20 (10.4) | 5 (8.9) | 15 (11.0) | 0.798 |
| Urgent surgery, No. (%) | 7 (3.6) | 5 (8.9) | 2 (1.5) | 0.023 |
| Other, No. (%) | 5 (2.6) | 4 (7.1) | 2 (1.5) | 0.061 |
| Origin of patients | ||||
| Rheumatology ward | 39 (20.3) | 17 (30.4) | 22 (16.2) | 0.031 |
| Normal ward | 87 (45.3) | 15 (26.8) | 72 (52.9) | 0.001 |
| ICU/emergency room | 66 (34.4) | 24 (42.9) | 42 (30.9) | 0.133 |
| IS naive at hospital admission, No. (%) | 62 (32.3) | 31 (55.4) | 31 (22.8) | <0.001 |
| GC naive at hospital admission, No. (%) | 45 (23.4) | 24 (42.9) | 21 (15.4) | <0.001 |
| IS naive at ICU admission, No. (%) | 46 (24.0) | 25 (44.6) | 21 (15.4) | <0.001 |
| GC naive at ICU admission, No. (%) | 25 (13.0) | 10 (17.9) | 15 (11.0) | 0.073 |
*Two Patients had respiratory failure due to COVID-19.
APACHEII, Acute Physiology and Chronic Health Evaluation II Score; CCI, Charlson Comorbidity Index; CTD, connective tissue disease; GC, glucocorticoid; GI, gastrointestinal tract; ICU, intensive care unit; IQR, interquartile range; IS, immunosuppressive/immunomodulatory therapy; No., number of patients; No., number of patients; RA, rheumatoid arthritis; SAPSII, Simplified Acute Physiology Score II; SOFA, Sequential Organ Failure Assessment Score; SpA, seronegative spondyloarthropathies; SRD, systemic rheumatic disease.
Table 2.
ICU-specific therapy
| Variable | All admissions (n=192) | SRD related (n=56) | Co-existent SRD (n=136) | P value |
| MIV, No. (%) | 116 (60.4) | 42 (75.0) | 74 (54.4) | 0.008 |
| Length of MIV (days), median (IQR) | 10 (4–22) | 11.5 (4.8–21.3) | 10 (4–24.5) | 0.906 |
| First-line MIV, No. (%) | 68 (35.4) | 24 (42.9) | 44 (32.4) | 0.167 |
| NIV followed by MIV, No. (%) | 48 (25.0) | 18 (32.1) | 30 (22.0) | 0.142 |
| NIV only, No. (%) | 46 (24.0) | 7 (12.5) | 39 (28.7) | 0.017 |
| Vasopressive drugs, No. (%) | 140 (72.9) | 42 (75.0) | 98 (72.1) | 0.677 |
| Length of vasopressor therapy (days), median (IQR) | 4 (2–10) | 3.5 (1–11) | 4 (2–9.3) | 0.686 |
| Inotropic drugs, No. (%) | 44 (22.9) | 12 (21.4) | 32 (23.5) | 0.753 |
| RRT, No. (%) | 81 (42.2) | 26 (46.4) | 55 (40.4) | 0.445 |
| ECMO, No. (%) | 16 (8.4) | 9 (16.1) | 7 (5.2) | 0.019 |
| VA-ECMO, No. (%) | 8 (4.2)* | 3 (5.4)† | 5 (3.7)‡ | |
| VV-ECMO, No. (%) | 11 (5.8)* | 7 (12.5)† | 4 (2.9)‡ | |
| Cumulative GC dose (mg) days 1–3, mean (SD) | 389.1 (771.2) | 988.2 (1191.2) | 142.5 (230.5) | <0.001 |
| Cumulative GC dose (mg) days 1–7, mean (SD) | 598.0 (1035.4) | 1460.0 (1537.7) | 242.9 (343.5) | <0.001 |
| Cumulative GC dose (mg) days 1–28, mean (SD) | 1047.9 (1480.5) | 2267.2 (1808.1) | 545.9 (948.0) | <0.001 |
| Immune therapy during ICU, No. (%) | 68 (35.4) | 32 (57.1) | 36 (26.5) | <0.001 |
| Biological, No. (%) | 17 (8.9) | 13 (23.2) | 4 (2.9) | <0.001 |
| Immunosuppression, No. (%) | 31 (16.1) | 7 (12.5) | 24 (17.6) | 0.518 |
| Cytotoxic agents, No. (%) | 23 (12.0) | 19 (33.9) | 4 (2.9) | <0.001 |
| Immunoglobulins, No. (%) | 23 (12.0) | 12 (21.4) | 11 (8.1) | 0.014 |
| >1 therapy, No. (%) | 33 (17.2) | 15 (26.8) | 18 (13.2) | 0.034 |
*Three patients had both VA-ECMO and VV-ECMO during their ICU stay.
†One patient had both VA-ECMO and VV-ECMO during his ICU stay.
‡Two patients had both VA-ECMO and VV-ECMO during their ICU stay.
ECMO, extracorporeal membrane oxygenation; GC, glucocorticoid; ICU, intensive care unit; IQR, interquartile range; MIV, mechanical invasive ventilation; NIV, non-invasive ventilation; No., number of patients; No., number of patients; RRT, renal replacement therapy; SD, standard deviation; SRD, systemic rheumatic disease; VA, venoarterial; VV, venovenous.
Table 3.
Outcome parameters
| Variable | All admissions (n=192) | SRD related (n=56) |
Co-existent SRD (n=136) | P value |
| ICU LOS tertiary centre (days), median (IQR) | 10 (4–18.9) | 11.5 (6.0–19.8) | 8.5 (3–18) | 0.094 |
| ICU LOS overall (days), median (IQR) | 10 (4–19) | 12 (12.0–21.5) | 9 (3.3–18) | 0.092 |
| Hospital LOS (days), median (IQR) | 52 (27.8–91.2) | 57 (26–84) | 48 (28–104) | 0.607 |
| 28-day survival, No. (%) | 138 (71.9) | 38 (67.9) | 100 (73.5) | 0.481 |
| ICU survival, No. (%) | 153 (79.7) | 41 (73.2) | 112 (82.4) | 0.170 |
| 3-month survival, No. (%) | 124 (64.6) | 33 (58.9) | 91 (66.9) | 0.322 |
| 6-month survival, No. (%) | 118 (61.5) | 33 (58.9) | 85 (61.5) | 0.745 |
| ICU readmission rate, No. (%) | 34 (17.7) | 11 (19.6) | 23 (16.9) | 0.680 |
| ECMO survival rate, No. (%)* | 8 (50.0) | 3 (33.3) | 5 (71.4) | 0.315 |
*ICU survival.
ECMO, extracorporal membrane oxygenation; ICU, intensive care unit; LOS, length of stay; No., number of patients; SRD, systemic rheumatic disease.
rmdopen-2023-003287supp001.pdf (220.6KB, pdf)
SRD related versus co-existent SRD
As the two constellations, exacerbation of the inflammatory disease as the primary reason for ICU admission (SRD related) or just a comorbidity not responsible for the acute critical illness (co-existent SRD), may have major implications for the treatment of critically ill patients with SRDs, we evaluated potential differences between these subgroups (tables 1–3).
Patients in the SRD-related cohort were younger (45 vs 65 years, p<0.001), had lower disease severity scores (SAPSII 41 vs 46, p=0.006; APACHEII 18 vs 23, p=0.005) and fewer comorbid diseases, as indicated by CCI (3 vs 5, p<0.001). The most common SRD diagnoses in this cohort were CTDs (42.9%) and vasculitides (42.9%). In comparison, in the subgroup of patients with co-existent SRD, RA (25.0%), CTDs (25.7%) and vasculitides (22.8%) were equally distributed. Cases of SpA were not found in the SRD-related cohort.
Reasons for ICU admission did not differ substantially between the two subgroups. Both subgroups mainly required critical care due to respiratory failure (57.1% vs 43.4%, p=0.111), shock (16.1% vs 27.2%, p=0.136) and neurologic failure (8.9% vs 11.0%, p=0.798). Cardiogenic events could be found more often in patients with co-existent SRD (1.8 vs 15.4, p=0.005). A detailed description of the reasons for ICU admission can be found in online supplemental table 1. In the SRD-related group, respiratory deterioration was mainly caused by interstitial lung disease, diffuse alveolar haemorrhage and pneumonitis, whereas in patients with co-existent SRD pneumonia was the leading cause. Infectious diseases, including sepsis pneumonia and meningitis, were the leading cause for ICU admission (48.5%) in the co-existent SRD subgroup. In 2020, COVID-19-associated respiratory failure was documented in two patients, with none in the SRD-related group.
The differences in SRD-related organ involvement are highlighted in table 1. In patients with SRD-related ICU admission, two or more organ systems were significantly more often affected, compared with patients in the co-existent SRD group. Immunosuppressive or GC therapy prior to hospitalisation and prior to ICU admission was instituted in a significantly higher proportion of patients in the co-existent SRD subgroup (table 1). In 28.6% of the SRD-related subpopulation, the diagnosis of SRD was made at the ICU.
At the ICU, a higher proportion of patients in the SRD-related cohort needed mechanical invasive ventilation (MIV) compared with the co-existent SRD subgroup (75.0% vs 54.4%, p=0.008). The percentage of patients requiring first-line MIV or non-invasive ventilation (NIV) followed by MIV did not show significant differences between both subgroups (table 2). However, sole NIV represented a sufficient ventilation strategy for more patients in the co-existent SRD subgroup (28.7% vs 12.5%, p=0.017). In contrast, extracorporeal membrane oxygenation (ECMO) therapy was significantly more frequent in patients with SRD-related critical illness (16.1% vs 5.2%, p=0.019). We did not observe significant differences in the length of MIV, frequency of vasopressor therapy, inotropic drugs or RRT (table 2). In addition, the main outcome parameters did not differ significantly between both subgroups (table 3).
Patients in the SRD-related subgroup received higher cumulative doses of GCs during their respective ICU stay (table 2). Furthermore, a higher proportion of these patients required SRD-specific immune therapy (ie, biologicals, immunosuppressive drugs, cytotoxic agents and immunoglobulins) during their respective ICU stay (57.1% vs 26.5%, p<0.001). We did not identify distinctive differences regarding the evolution of antirheumatic treatment, especially biologic drugs (ie, tyrosine kinase inhibitors and antibodies), over the course of the study period (online supplemental table 2).
To provide a more comprehensive clinical context for our data, we also included a control group of 1808 ICU patients without SRD and with solely medical background into our manuscript. These results can be found in online supplemental table 3. Patients in the control group were older and exhibited a higher disease severity according to SOFA Score. Cardiogenic events, especially cardiac arrest, were the leading causes of ICU admission in this population. The frequency of respiratory failure as the reason for ICU admission was significantly lower in the general ICU population (21.7% vs 47.4%, p<0.001).
Factors contributing to 28-day survival
When evaluating single predictors for 28-day mortality, we observed a significant increase in 28-day mortality with higher age, disease duration and increasing SOFA Score, particularly in the cardiac and hepatic subdomains (table 4). Interestingly, these risk factors exhibited some differences between patients who were admitted to the ICU for disease flare and those with rheumatic comorbidity. Whereas higher GC intake on hospitalisation and longer in-hospital stay before ICU admission were associated with higher mortality rates in the SRD-related cohort, these factors do not appear to contribute significantly to increased mortality in the co-existent SRD cohort (table 4). The disease entity itself (especially the presence of vasculitides) also had an influence on short-term survival in the overall study population and the co-existent SRD subgroup. Consultation of a specialist in rheumatology was found to be associated with lower mortality rates in patients with co-existent SRD. However, this effect was not observed in the SRD-related group as standard rheumatic consultation was present in all patients.
Table 4.
Single-predictor logistic regression models
| SRD related | Co-existent SRD | All patients | |
| Age (standardised) | 0.57 (0.31; 1.01) | 0.56* (0.35; 0.86) | 0.64* (0.45; 0.90) |
| N R2 |
57 0.09 |
135 0.08 |
192 0.05 |
| CCI | 0.87 (0.66; 1.12) | 0.87 (0.72; 1.05) | 0.91 (0.79; 1.04) |
| N R2 |
57 0.03 |
135 0.02 |
192 0.01 |
| Disease duration (log) | 0.91* (0.82; 0.99) | 0.84* (0.69; 0.96) | 0.93* (0.87; 0.99) |
| N R2 |
56 0.11 |
126 0.09 |
182 0.04 |
| Consultation by a rheumatologist | 1.00 (0.13; 5.67) | 3.37* (1.29; 10.58) | 1.50 (0.80; 2.86) |
| N R2 |
57 0.00 |
135 0.07 |
192 0.01 |
| SOFA | 0.84* (0.71; 0.98) | 0.87* (0.78; 0.97) | 0.86** (0.78; 0.94) |
| N R2 |
57 0.11 |
135 0.06 |
192 0.08 |
| SOFA respiratory system | 0.77 (0.49; 1.13) | 0.86 (0.65; 1.11) | 0.82 (0.65; 1.01) |
| N R2 |
57 0.04 |
134 0.01 |
191 0.03 |
| SOFA CNS | 0.71 (0.45; 1.07) | 0.93 (0.73; 1.20) | 0.89 (0.73; 1.09) |
| N R2 |
57 0.06 |
135 0.00 |
192 0.01 |
| SOFA cardiovascular | 0.86 (0.61; 1.18) | 0.74* (0.54; 0.97) | 0.80* (0.64; 0.98) |
| N R2 |
57 0.02 |
135 0.05 |
192 0.03 |
| SOFA hepatic | 0.65 (0.36; 1.14) | 0.62* (0.41; 0.92) | 0.62** (0.45; 0.86) |
| N R2 |
57 0.05 |
135 0.06 |
192 0.06 |
| SOFA coagulation | 0.95 (0.62; 1.47) | 0.92 (0.61; 1.42) | 0.90 (0.68; 1.20) |
| N R2 |
57 0.00 |
135 0.00 |
192 0.00 |
| SOFA renal | 0.93 (0.69; 1.26) | 0.99 (0.79; 1.25) | 0.97 (0.81; 1.17) |
| N R2 |
57 0.01 |
135 0.00 |
192 0.00 |
| GC hospitalisation (log) | 0.63** (0.45; 0.85) | 1.00 (0.82; 1.24) | 0.87 (0.74; 1.02) |
| N R2 |
57 0.21 |
135 0.00 |
192 0.02 |
| GC ICU (log) | 0.85 (0.67; 1.05) | 1.09 (0.93; 1.29) | 0.98 (0.87; 1.10) |
| N R2 |
57 0.05 |
135 0.01 |
192 0.00 |
| LOS (log) | 0.68* (0.47; 0.95) | 0.99 (0.83; 1.18) | 0.91 (0.78; 1.05) |
| N R2 |
56 0.13 |
135 0.00 |
191 0.01 |
| Rheumatic disease | |||
| RA versus CTD | 2.19 (0.79; 6.08) | 1.64 (0.70; 3.87) | |
| RA versus SpA | 1.58 (0.40; 6.26) | 1.68 (0.43; 6.64) | |
| RA versus vasculitis | 11.45** (2.35; 55.84) | 4.95** (1.82; 13.48) | |
| RA versus other | 3.00 (0.91; 9.91) | 3.51* (1.15; 10.67) | |
| N R2 |
135 0.14 |
192 0.09 |
ORs are provided for each predictor, followed by 95% CIs. Nagelkerke pseudo-R2 and included sample size (N) are provided for each model.
*p<0.05; **p<0.01.
CCI, Charlson Comorbidity Index; CNS, central nervous system; CTD, connective tissue disease; GC hospitalisation, glucocorticoid therapy prior admission to hospital; GC ICU, GC therapy prior admission to ICU; ICU, intensive care unit; LOS, length of stay; RA, rheumatoid arthritis; SOFA, Sequential Organ Failure Assessment Score; SpA, seronegative spondyloarthropathies.
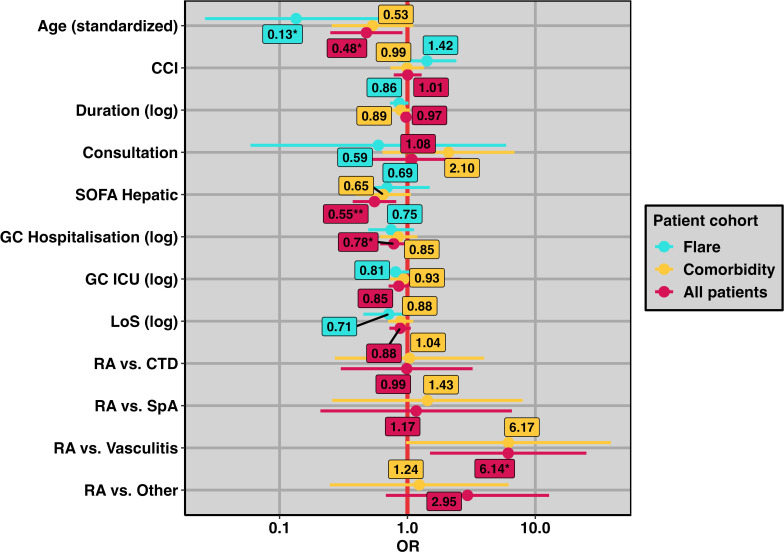
By entering all these variables into multivariate logistic regression models, we observed a robust impact of age, GC prescription prior to hospital admission, the hepatic subdomain of SOFA Score and the presence of specific disease entities (especially vasculitides) on 28-day mortality in the overall study population (table 5). Due to the limited number of patients included in the SRD-related subgroup, we were unable to perform a reasonable statistical analysis regarding outcome and disease entities in this cohort. Consequently, these data were not included in both the univariate and multivariate logistic regression models. The multivariate logistic regression models are visually displayed in a forest plot in figure 2.
Table 5.
Multivariate logistic regression models
| SRD related | Co-existent SRD | All patients | |
| Age (standardised) | 0.13* (0.02; 0.56) | 0.53 (0.26; 1.11) | 0.48* (0.25; 0.91) |
| CCI | 1.42 (0.86; 2.55) | 0.99 (0.73; 1.34) | 1.01 (0.78; 1.29) |
| Disease duration (log) | 0.86 (0.71; 1.00) | 0.89 (0.75; 1.05) | 0.97 (0.89; 1.07) |
| Consultation | 0.59 (0.05; 5.64) | 2.10 (0.64; 6.87) | 1.08 (0.45; 2.61) |
| SOFA hepatic | 0.69 (0.30; 1.46) | 0.65 (0.39; 1.06) | 0.55** (0.37; 0.82) |
| GC hospitalisation (log) | 0.75 (0.48; 1.12) | 0.85 (0.61; 1.19) | 0.78* (0.61; 1.00) |
| GC ICU (log) | 0.81 (0.54; 1.11) | 0.93 (0.73; 1.20) | 0.85 (0.71; 1.03) |
| LOS (log) | 0.71 (0.43; 1.10) | 0.88 (0.70; 1.11) | 0.88 (0.72; 1.06) |
| Rheumatic disease | |||
| RA versus CTD | 1.04 (0.27; 3.98) | 0.99 (0.30; 3.23) | |
| RA versus SpA | 1.43 (0.26; 7.97) | 1.17 (0.21; 6.56) | |
| RA versus vasculitis | 6.17 (0.98; 39.10) | 6.14* (1.50; 25.10) | |
| RA versus other | 1.24 (0.25; 6.19) | 2.95 (0.68; 12.82) | |
| N | 56 | 126 | 182 |
| R2 | 0.50 | 0.28 | 0.28 |
ORs are provided for each predictor, followed by 95% CIs. Nagelkerke pseudo-R2 and included sample size (N) are provided for each model. *p<0.05; **p<0.01. Log indicates that logarithmic transformation was applied.
CCI, Charlson Comorbidity Index; Consultation, consultation by a rheumatologist; CTD, connective tissue disease; GC hospitalisation, glucocorticoid therapy prior admission to hospital; ICU, intensive care unit; GC ICU, glucocorticoid therapy prior admission to ICU; LOS, length of stay; RA, rheumatoid arthritis; SOFA, Sequential Organ Failure Assessment Score; SpA, seronegative spondyloarthropathies.
Figure 2.
Forest plot of multivariate logistic regression models. ORs are displayed as filled circles, and corresponding 95% CIs are displayed as bars (see also table 5). Each patient cohort is indicated by a different colour. The x-axis was log-transformed using a base of 10. The red vertical line indicates an OR of 1; *p<0.05; **p<0.01. CCI, charlson comorbidity index; consultation, consultation by a rheumatologist; CTD, connective tissue disease; GC ICU, glucocorticoid therapy prior admission to ICU; ICU, intensive care unit; LOS, length of stay; RA, rheumatoid arthritis; SOFA, sequential organ failure assessment score; SpA, seronegative spondyloarthropathies.
Discussion
Critically ill patients with SRDs still represent a neglected ICU population regarding prognostic parameters and therapeutic modalities. To date, available data on critically ill patients with SRDs is limited and often inconsistent. Most studies describe patient cohorts with varying disease frequencies and, notably, fail to distinguish the reasons for ICU admission (SRD related vs co-existent SRD), making valid comparisons difficult. Within the scope of this study, we delineated clinical features, outcome parameters and potential mortality predictors in a cohort of 144 patients with SRDs accounting for 192 ICU admissions over 9 years at a large tertiary centre in Central Europe. Furthermore, we evaluated potential differences between patients admitted to the ICU due to SRD-related critical illness and patients with co-existent SRD. Finally, our multiple logistic regression model revealed that age, GC therapy prior hospital admission, the hepatic subdomain of the SOFA Score and the presence of vasculitides were associated with short-term mortality.
Within our study cohort, CTDs and vasculitides, especially systemic lupus erythematosus and anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitides, were the most common diagnoses requiring critical care, each accounting for approximately one-third of the ICU admissions. These results align with the most recent studies mainly originating from France, where CTDs and vasculitides accounted for 38.7%–56.5% and 8.7%–26.2% of ICU admissions in their respective patient cohorts.2–4 10 Due to a better understanding of the pathophysiology and a couple of new promising treatment options in the last decade, the prevalence of RA, which was the most common SRD at the ICU as reported by older studies published in the late nineties and early 2000s, has declined significantly.12 In our study, RA accounted for 18.2% of all cases, consistent with the latest studies, in which RA is described to be present in 8.7%–41.3% of patients requiring intensive care treatment.2–4 10
Among our patients, ICU mortality was 20.3%. This rate is comparable to the ones from recently published data over the past decade, in which mortality rates range between 14.3% and 23.8%.2–4 10 These findings might be explained by significant advancements in the diagnosis and treatment of critically ill patients and patients with SRDs over the past two decades since mortality rates among patients with SRD have now approached those observed in a general ICU population of approximately 19%.2–4 10 Compared with our general ICU population, patients with SRDs had significantly better ICU survival. However, these results need to be interpreted with caution, as the control group was not matched with our SRD patient cohort. Patients in the control group were older and had a higher disease severity according to SOFA Score. The considerable heterogeneity of reported ICU mortality rates ranging from 11% to 79% across different publications most likely originates from studies analysing patient cohorts with heterogeneous disease frequencies, different reasons for ICU admission and small sample sizes.
ICU admission in patients with SRD can be attributed to two conditions. First, ICU admission may be required due to a flare-up of the inflammatory disease itself, or second, the SRD just represents a comorbidity unrelated to the acute critical illness. As these two constellations may have major implications for the treatment of critically ill patients with SRD, we are the first to evaluate potential differences between these subgroups. SRD-related critical illness was the leading cause of ICU admission in nearly one-third of all cases, corroborating recent studies from France.2 3 In this subgroup, respiratory failure was the predominant organ dysfunction leading to ICU admission, occurring in 57.1% of all patients. In patients with co-existent SRD, respiratory failure was also the most common cause of admission (43.4%) but with a significantly lower frequency. Interestingly, CTD and vasculitides showed a higher prevalence in the SRD-related group. In patients with co-existent SRD, CTD, vasculitides and RA were found to be equally distributed. In summary, these findings underscore that pulmonary involvement is a source of significant morbidity and mortality in the majority of patients with SRD admitted to the ICU, especially in those presenting with SRD-related critical illness.2 3
The year 2020 marked the start of the COVID-19 pandemic caused by the novel SARS-CoV2 virus, which has led to a worldwide health and economic crisis. Although most patients with COVID-19 presented with mild flu-like symptoms, a substantial number of patients required hospitalisation and even ICU admission due to pneumonia and consequently acute respiratory distress syndrome (ARDS).37 To date, it is still debated if patients with rheumatic diseases have a higher risk of infection with SARS-CoV2 or worse outcomes compared with a general population.38 In 2020 and the first two waves of the COVID-19 pandemic, our centre witnessed 89 ICU admissions due to SARS-CoV2-induced ARDS. Of these patients, only two had a documented rheumatic disease (1×RA; 1×SpA) and both were admitted to the ICU due to COVID-19 ARDS. Because of these small numbers, we were not able to analyse the influence of COVID-19 on the outcome in our SRD patient population. The low rate of hospital and ICU admissions for SARS-CoV2 in patients with SRDs during the first two waves may be explained by the consequent shielding of this vulnerable patient population. In addition, social distancing to limit the spreading of the disease was ensured by reduced outpatient department capacity and mainly telehealth was conducted.39 These measurements changed throughout the pandemic with loosened regulations. It is therefore reasonable to assume that SARS-CoV2-related ICU admissions of patients with SRDs show an increase in subsequent years of the pandemic.
We found a significantly higher percentage of newly diagnosed SRDs in the SRD-related subgroup compared with patients with co-existent SRD (28.6% vs 3.7%, p<0.001). Previous studies reported considerable low rates of newly diagnosed SRDs at the ICU (between 2.5% and 15.0%), corresponding to our overall patient population.4 10 Our findings indicate that a high percentage of patients with SRD flare already require intensive care for initial presentation or at a very early stage of the SRD, highlighting the disease severity of this patient population.
The susceptibility to infections in patients with co-existent SRD, either due to complications of the SRD itself, the therapy-associated immunosuppression or a combination of both, aligns with our findings that pneumonia was the leading cause of respiratory failure. In addition, septic shock represented the most common form of shock in this cohort. Although distinguishing between infection and SRD-related inflammation at ICU admission is of utmost importance in clinical practice, especially since the therapeutic approaches differ substantially (anti-infective vs immunosuppressive therapy), the practical benefit of it remains uncertain. The retrospective design of this study and the simplified classification into either SRD-related inflammation or infection within this study do not sufficiently highlight the difficulty of making a correct distinction. Furthermore, the treatment strategy may be even further complicated by the concurrent existence of both conditions. As a result, physicians are often confronted by the challenge of choosing a polypragmatic treatment approach, simultaneously administering anti-infective and immunosuppressive therapy (especially GCs) until the correct diagnosis is established.
In our patient population, age, GC therapy prior to hospital admission and SOFA Score within the first 24 hours of admission were independently associated with 28-day mortality, which corresponds to the latest studies.2–4 10 13 Age has been linked to increased frailty and a higher frequency of chronic diseases, putting elderly patients at higher risk of death when requiring intensive care.40 This statement may hold true for our patient subgroup with co-existent SRD. However, with a median age of 45 years, patients with SRD-related critical illness were comparatively young. Thus, a more advanced disease status with more severe organ involvement and early development of various complications may have contributed to age as a predictive factor for short-term mortality rather than an advanced age per se. We also found that the presence of more severe diseases like CTDs and vasculitides was independently associated with short-term survival. These findings reflect the clinical situation as therapeutic options are limited in these disease entities and patients often acquire more complications during their respective course of disease compared with patients with RA and SpA.1 12
In our single-predictor regression analyses, we found that the consultation of a specialist in rheumatology was associated with improved 28-day survival in patients with co-existent SRD. Although this correlation did not reach statistical significance in multiple regression analysis, we are convinced that consultation of a rheumatologist during intensive care treatment has a positive impact on the prognosis of this specific patient population, given the complex nature, the various organ involvements and the potential range of adverse effects associated with their treatment. In contrast, in the majority of our patients with SRD-related critical illness, routine interdisciplinary consultation between rheumatologists, infectiologists and intensivists was conducted, which might explain why this correlation was not found in this patient cohort.
Limitations
The present study has several limitations. First, the retrospective design of this study may have had a negative impact on the data collection and therefore may have induced bias in interpreting its results. Second, the differentiation between solely SRD-related inflammation/critical illness and co-existent SRD as the cause of admission occasionally lacked robust evidence and may have resulted in misclassifications. Nonetheless, in such cases, two independent clinicians (intensivist and rheumatologist) rigorously reviewed the patient’s medical records, and assignment to one of these categories underwent extensive deliberation until a consensus was achieved. Third, autoimmune diseases can be both promoted and/or exacerbated by infections.41–43 However, due to the retrospective design of our study, we were able to thoroughly review all available data in the patients’ medical records in order to rule out any suspicion of infection at the time of clinical deterioration. Fourth, this study was conducted in ICU wards of a tertiary hospital with one of the biggest rheumatology reference centres in Europe, which may potentially restrict the generalisability of the results. Patients’ care may have been influenced by local policies, such as rapid admission to the ICU and routine management by both internists and intensive care physicians. Nevertheless, patients with SRDs, especially CTDs, vasculitides and complicated RA/SpA, are usually treated in specialised centres with access to state-of-the-art rheumatological and intensive care treatment. Some ICU therapies (eg, ECMO) are limited to mostly university-affiliated institutions like our centre. However, in cases of unmanageable complications, these patients are mainly transferred to tertiary hospitals. Therefore, it is reasonable to assert that our results mostly reflect situations, which are also found in other settings. Fifth, we present a relatively small patient population of 144 patients with SRD accounting for 192 ICU admissions. Due to the fact that we exclusively included patients with documented SRD diagnosis according to ICD-10 coding, there might be a certain number of patients with SRDs missing and not analysed in this study. However, SRDs generally have a low incidence and we here report the largest cohort of critically ill patients with SRD in Central Europe. Sixth, due to the aforementioned small sample size of the study population, the statistical power, especially concerning the SRD-related cohort, was somewhat limited.
Conclusion
CTDs and vasculitides were the most common rheumatic entities requiring ICU treatment. Respiratory failure followed by shock was the leading cause of ICU admission. This fact is reflected by high rates of required MIV and vasopressor therapy. Our study is the first to describe specific differences in patients with SRD-related critical illness or critically ill patients with co-existent SRD. This distinction may have major clinical implications as adequate therapy is heavily influenced by it. Despite a considerable severity of critical illness, survival rates are comparable to a general ICU population. The lack of consistent data highlights the need for further research concerning prognostic parameters and more specific guidelines in treating these critically ill patients.
Acknowledgments
The authors wish to thank Mr Bernd Becker for his tremendous help with exporting data from the AKIM EDV system.
Footnotes
Contributors: MS-G, KPM, PS and MB: concept of the study; MS-G, CH, SJ, MZ, GH, KPM, GS, TS and CZ: data collection/cleaning; MS-G, JF and MB: statistical analysis; MZ and MB: study co-ordination; MS-G, DA, KPM, PS and MB: data review; MS-G, KPM, PS and MB: drafting of the manuscript; and all authors: revision for important intellectual content as well as approval of the final manuscript. MB is responsible for the overall content as guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The study was approved by the ethics committee of the Medical University of Vienna (1976/2018) and was performed in accordance with the Declaration of Helsinki.
References
- 1.Goldblatt F, O’Neill SG. Clinical aspects of autoimmune rheumatic diseases. Lancet 2013;382:797–808. 10.1016/S0140-6736(13)61499-3 [DOI] [PubMed] [Google Scholar]
- 2.Dumas G, Géri G, Montlahuc C, et al. Outcomes in critically ill patients with systemic rheumatic disease: a multicenter study. Chest 2015;148:927–35. 10.1378/chest.14-3098 [DOI] [PubMed] [Google Scholar]
- 3.Larcher R, Pineton de Chambrun M, Garnier F, et al. One-year outcome of critically ill patients with systemic rheumatic disease: a multicenter cohort study. Chest 2020;158:1017–26. 10.1016/j.chest.2020.03.050 [DOI] [PubMed] [Google Scholar]
- 4.Faguer S, Ciroldi M, Mariotte E, et al. Prognostic contributions of the underlying inflammatory disease and acute organ dysfunction in critically ill patients with systemic rheumatic diseases. Eur J Intern Med 2013;24:e40–4. 10.1016/j.ejim.2012.11.018 [DOI] [PubMed] [Google Scholar]
- 5.Quintero OL, Rojas-Villarraga A, Mantilla RD, et al. Autoimmune diseases in the intensive care unit. An update. Autoimmun Rev 2013;12:380–95. 10.1016/j.autrev.2012.06.002 [DOI] [PubMed] [Google Scholar]
- 6.Lee J, Yim J-J, Yang S-C, et al. Outcome of patients with connective tissue disease requiring intensive care for respiratory failure. Rheumatol Int 2012;32:3353–8. 10.1007/s00296-011-2158-6 [DOI] [PubMed] [Google Scholar]
- 7.Delvino P, Monti S, Balduzzi S, et al. The role of extra-corporeal membrane oxygenation (ECMO) in the treatment of diffuse alveolar haemorrhage secondary to ANCA-associated vasculitis: report of two cases and review of the literature. Rheumatol Int 2019;39:367–75. 10.1007/s00296-018-4116-z [DOI] [PubMed] [Google Scholar]
- 8.Kouchit Y, Morand L, Martis N. Mortality and its risk factors in critically ill patients with connective tissue diseases: a meta-analysis. Eur J Intern Med 2022;98:83–92. 10.1016/j.ejim.2022.02.006 [DOI] [PubMed] [Google Scholar]
- 9.Mustafa M, Gladston Chelliah E, Hughes M. Patients with systemic rheumatic diseases admitted to the intensive care unit: what the Rheumatologist needs to know. Rheumatol Int 2018;38:1163–8. 10.1007/s00296-018-4008-2 [DOI] [PubMed] [Google Scholar]
- 10.Chabert P, Danjou W, Mezidi M, et al. Short- and long-term prognosis of acute critically ill patients with systemic rheumatic diseases: a retrospective multicentre study. Medicine (Baltimore) 2021;100:e26164. 10.1097/MD.0000000000026164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moreels M, Mélot C, Leeman M. Prognosis of patients with systemic rheumatic diseases admitted to the intensive care unit. Intensive Care Med 2005;31:591–3. 10.1007/s00134-005-2563-y [DOI] [PubMed] [Google Scholar]
- 12.Janssen NM, Karnad DR, Guntupalli KK. Rheumatologic diseases in the intensive care unit: epidemiology, clinical approach, management, and outcome. Crit Care Clin 2002;18:729–48. 10.1016/s0749-0704(02)00025-8 [DOI] [PubMed] [Google Scholar]
- 13.Thong BY, Tai DY, Goh SK, et al. An audit of patients with rheumatic disease requiring medical intensive care. Ann Acad Med Singap 2001;30:254–9. [PubMed] [Google Scholar]
- 14.Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 1997;40:1725. 10.1002/art.1780400928 [DOI] [PubMed] [Google Scholar]
- 15.van den Hoogen F, Khanna D, Fransen J, et al. Classification criteria for systemic sclerosis an American College of Rheumatology/European League Against Rheumatism Collaborative Initiative. Arthritis Rheum 2013;65:2737–47. 10.1002/art.38098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lundberg IE, Tjärnlund A, Bottai M, et al. European A/American College of Rheumatology classification criteria for adult and juvenile idiopathic inflammatory myopathies and their major subgroups. Ann Rheum Dis 2017;76:1955–64. 10.1136/annrheumdis-2017-211468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shiboski CH, Shiboski SC, Seror R, et al. American College of Rheumatology/European League Against Rheumatism classification criteria for primary Sjogren’s syndrome a consensus and data-driven methodology involving three international patient cohorts. Ann Rheum Dis 2017;76:9–16. 10.1136/annrheumdis-2016-210571 [DOI] [PubMed] [Google Scholar]
- 18.Aletaha D, Neogi T, Silman AJ, et al. 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism Collaborative Initiative. Ann Rheum Dis 2010;69:1580–8. 10.1136/ard.2010.138461 [DOI] [PubMed] [Google Scholar]
- 19.The International criteria for Behçet's disease (ICBD): a collaborative study of 27 countries on the sensitivity and specificity of the new criteria. J Eur Acad Dermatol Venereol 2014;28:338–47. 10.1111/jdv.12107 [DOI] [PubMed] [Google Scholar]
- 20.Jennette JC, Falk RJ, Bacon PA, et al. 2012 revised International chapel hill consensus conference nomenclature of vasculitides. Arthritis Rheum 2013;65:1–11. 10.1002/art.37715 [DOI] [PubMed] [Google Scholar]
- 21.Sieper J, Rudwaleit M, Baraliakos X, et al. The assessment of spondyloarthritis International society (ASAS) handbook: a guide to assess spondyloarthritis. Ann Rheum Dis 2009;68 Suppl 2:ii1–44. 10.1136/ard.2008.104018 [DOI] [PubMed] [Google Scholar]
- 22.Fautrel B, Zing E, Golmard J-L, et al. Proposal for a new set of classification criteria for adult-onset still disease. Medicine 2002;81:194–200. 10.1097/00005792-200205000-00003 [DOI] [PubMed] [Google Scholar]
- 23.Singer M, Deutschman CS, Seymour CW, et al. The third International consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 2016;315:801. 10.1001/jama.2016.0287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grasselli G, Calfee CS, Camporota L, et al. ESICM guidelines on acute respiratory distress syndrome: definition, phenotyping and respiratory support strategies. Intensive Care Med 2023;49:727–59. 10.1007/s00134-023-07050-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Afessa B, Tefferi A, Litzow MR, et al. Diffuse alveolar hemorrhage in hematopoietic stem cell transplant recipients. Am J Respir Crit Care Med 2002;166:1364–8. 10.1164/rccm.200208-792OC [DOI] [PubMed] [Google Scholar]
- 26.Bradley B, Branley HM, Egan JJ, et al. Interstitial lung disease guideline: the British Thoracic Society in collaboration with the Thoracic Society of Australia and New Zealand and the Irish Thoracic Society. Thorax 2008;63 Suppl 5:v1–58. 10.1136/thx.2008.101691 [DOI] [PubMed] [Google Scholar]
- 27.Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract 2012;120:c179–84. 10.1159/000339789 [DOI] [PubMed] [Google Scholar]
- 28.Wendon, J, et al. , European Association for the Study of the Liver. Electronic address: easloffice@easloffice.eu, Clinical practice guidelines panel . EASL clinical practical guidelines on the management of acute (fulminant) liver failure. J Hepatol 2017;66:1047–81. 10.1016/j.jhep.2016.12.003 [DOI] [PubMed] [Google Scholar]
- 29.Le Gall JR, Lemeshow S, Saulnier F. A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA 1993;270:2957–63. 10.1001/jama.270.24.2957 [DOI] [PubMed] [Google Scholar]
- 30.Vincent J-L, de Mendonca A, Cantraine F, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Critical Care Medicine 1998;26:1793–800. 10.1097/00003246-199811000-00016 [DOI] [PubMed] [Google Scholar]
- 31.Knaus WA, Wagner DP, Draper EA, et al. The APACHE III prognostic system. risk prediction of hospital mortality for critically ill hospitalized adults. Chest 1991;100:1619–36. 10.1378/chest.100.6.1619 [DOI] [PubMed] [Google Scholar]
- 32.Charlson M, Szatrowski TP, Peterson J, et al. Validation of a combined comorbidity index. J Clin Epidemiol 1994;47:1245–51. 10.1016/0895-4356(94)90129-5 [DOI] [PubMed] [Google Scholar]
- 33.Harrell JFE. Regression modeling strategies: with applications to linear models, logistic and ordinal regression, and survival analysis. 2015. [Google Scholar]
- 34.Nagelkerke NJD. A note on a general definition of the coefficient of determination. Biometrika 1991;78:691–2. 10.1093/biomet/78.3.691 [DOI] [Google Scholar]
- 35.Perneger TV. What’s wrong with Bonferroni adjustments. BMJ 1998;316:1236–8. 10.1136/bmj.316.7139.1236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wickham H. Ggplot2: Elegant graphics for data analysis. Cham: Springer-Verlag, 2016. 10.1007/978-3-319-24277-4 [DOI] [Google Scholar]
- 37.Wiersinga WJ, Rhodes A, Cheng AC, et al. Pathophysiology, transmission, diagnosis, and treatment of Coronavirus disease 2019 (COVID-19): a review. JAMA 2020;324:782–93. 10.1001/jama.2020.12839 [DOI] [PubMed] [Google Scholar]
- 38.Grainger R, Kim AHJ, Conway R, et al. COVID-19 in people with rheumatic diseases: risks, outcomes, treatment considerations. Nat Rev Rheumatol 2022;18:191–204. 10.1038/s41584-022-00755-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kavadichanda C, Shah S, Daber A, et al. Tele-rheumatology for overcoming socioeconomic barriers to healthcare in resource constrained settings: lessons from COVID-19 pandemic. Rheumatology (Oxford) 2021;60:3369–79. 10.1093/rheumatology/keaa791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Guidet B, Leblanc G, Simon T, et al. Effect of systematic intensive care unit triage on long-term mortality among critically ill elderly patients in France a randomized clinical trial. JAMA 2017;318:1450–9. 10.1001/jama.2017.13889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Avcin T, Canova M, Guilpain P, et al. Infections, connective tissue diseases and vasculitis. Clin Exp Rheumatol 2008;26:S18–26. [PubMed] [Google Scholar]
- 42.Cooke A, Ferraccioli GF, Herrmann M, et al. Induction and protection of autoimmune rheumatic diseases. The role of infections. Clin Exp Rheumatol 2008;26:S1–7. [PubMed] [Google Scholar]
- 43.Zampieri S, Ghirardello A, Iaccarino L, et al. Polymyositis-dermatomyositis and infections. Autoimmunity 2006;39:191–6. 10.1080/08916930600622348 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
rmdopen-2023-003287supp001.pdf (220.6KB, pdf)
Data Availability Statement
Data are available upon reasonable request.