Abstract
Substance use disorder prevention programs are most effective when matched appropriately to the baseline risk of the population. Individuals who misuse opioids often have unique risk profiles different from those who use other substances such as alcohol or cannabis. However, most substance use prevention programs are geared toward universal audiences, neglecting key inflection points along the continuum of care. The HEAL Prevention Cooperative (HPC) is a unique cohort of research projects that represents a continuum of care, from community-level universal prevention to indicated prevention among older adolescents and young adults who are currently misusing opioids or other substances. This paper describes the theoretical basis for addressing opioid misuse and opioid use disorder across the prevention continuum, using examples from research projects in the HPC.
Keywords: Opioid use disorder, Evidence-based prevention programs, Behavioral health continuum of care
Overdose deaths for adolescents and young adults, primarily driven by opioids, remain a leading cause of preventable mortality (Monico et al., 2021). Young Americans are also at a heightened risk of opioid use disorder (OUD); a national survey from 2015 through 2016 found approximately one-fifth of adolescents (12–17 years) and more than a third of young adults (18–25 years) used a prescription opioid at least once in the past year, and past year prescription opioid misuse (e.g., without a prescription, more than intended) was reported by 3.8% of adolescents and 7.8% of young adults (Hudgins et al., 2019). However, less than a quarter of the nearly 1.4 million Americans who reported a substance use disorder (SUD) related to prescription opioids in 2019 received specialized addiction treatment (National Institute on Drug Abuse (NIDA), 2021). More than ever, communities need resources, information, and support to prevent the onset or escalation of OUD among youth and young adults. This article challenges preventionists to leverage the full continuum of care to implement evidence-based programs and practices (EBPPs) to address opioid misuse and OUD among youth and young adults.
The Current Public Health Framework for OUD Prevention
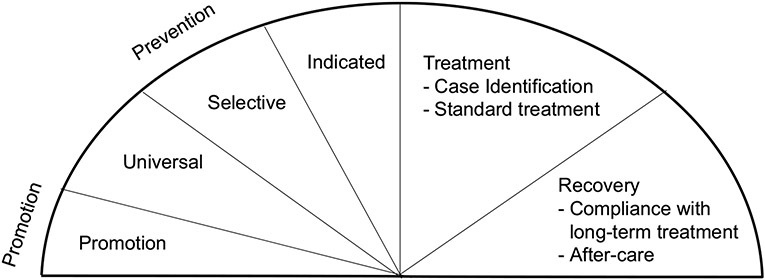
In 1994, the Institute of Medicine published the behavioral health continuum of care model (Fig. 1) as a guiding framework for classifying prevention, treatment, and recovery programming. Prevention, conceptualized as an intermediary phase between promotion and treatment, is a continuum across three levels. Universal prevention refers to interventions designed for and delivered to the general population. At the second level, selective prevention targets individuals with a known risk factor for substance use or SUD, such as a comorbid mental health disorder or familial history of substance use. Indicated prevention narrows the target to individuals on the verge of engaging in the behavior, or those who have exhibited behavior that foreshadows a SUD (e.g., experimentation with opioid misuse could lead to OUD).
Fig. 1.
The behavioral health continuum of care. Adapted from Institute of Medicine (1994). Reducing risks for mental disorders: Frontiers for preventive intervention research. The National Academies Press. https://doi.org/10.17226/2139
OUD prevention programming can also be classified through the lens of a socioecological framework (Jalali et al., 2020; McLeroy et al., 1988). Intrapersonal- or individual-level programs directly target youth and young adults. Examples of individual-level programs include awareness-raising activities such as media campaigns and school-based social-emotional learning curricula. Interpersonal-level programs target those individuals or systems that directly interact with the youth or young adults. This can include parenting and other relationship-building programs that increase connections with prosocial agents. Community-level programs focus on improving the social or structural conditions that influence the likelihood of opioid misuse. Examples include policy changes, community coalition building, and changes to the built environment.
Most substance use prevention programs are targeting the individual level and are geared toward universal audiences consisting primarily of youth who have never misused opioids in the past and have no intention of misusing opioids in the future (Substance Abuse and Mental Health Services Administration (SAMHSA), 2019). However, we argue that this model neglects key inflection points along the continuum of care where EBPPs can improve outcomes for individuals who do not fit squarely into the universal, selective, or indicated prevention categories. Specifically, prevention programs and strategies are necessary across the continuum and at multiple levels of influence to address opioid misuse before initiation and during escalation to a clinically diagnosed OUD.
Current Challenges and Opportunities in Opioid Use Disorder Prevention
Early opioid misuse prevention efforts focused on reducing access to prescription opioid medications, targeting the prescribing and dispensing of prescription opioids. These efforts focused on the three key areas: (1) education and establishment of safer opioid prescribing practices guidelines for providers (Dowell et al., 2016; Lin et al., 2017), (2) creation and expansion of prescription drug monitoring programs to track controlled substance prescriptions, and (3) legislative mandates for providers to inform patients (or parents/guardians of minors) of the risks of opioids and to review prescription drug monitoring program data for their patients before prescribing them controlled substances (Bao et al., 2018). These combined efforts showed some positive changes in prescribing behaviors (Bohnert et al., 2018; Rhodes et al., 2019; Strickler et al., 2019). Even so, the opioid overdose crisis continues—driven by diversion of prescription opioids without a prescription, use of illicit opioids, and opioid overdose among young adults (Monico et al., 2021; Nguyen et al., 2020; Roehler et al., 2021)—and must be urgently addressed. Scalable EBPPs are needed to fill the gap between universal prevention and treatment of OUD (Volkow et al., 2019). However, filling in this gap requires several considerations, including population characteristics, settings, feasibility of dissemination and implementation, and tailored approaches.
Challenges Unique to Population Characteristics
Timely and high-quality surveillance data are needed to identify communities, families, and individuals who will most benefit from prevention programming. There has been significant attention on how surveillance can be improved to address the opioid overdose crisis in the USA (Blanco et al., 2022; Hoots, 2021). However, most epidemiologic surveillance systems are based on the harms associated with opioid misuse and OUD (e.g., emergency department visits, overdose deaths). National surveys with youth and young adults that include opioid misuse and associated risk and protective factors (e.g., National Survey on Drug Use and Health, Youth Risk Behavioral Surveillance System) do not provide information at the local municipality level. The result is a paucity of data for preventionists to determine the needs of their communities.
Although education about the risks of opioid prescriptions remains critical for clinicians and caregivers (Frank et al., 2015; Worsham et al., 2021), preventionists must also harness EBPP strategies to reach the primary target population: adolescents and young adults (Bonar et al., 2020). A selective prevention approach has advantages of parsimony of resources for program delivery only to at-risk adolescents and young adults; however, this approach requires consideration of setting constraints to determine whether screening procedures to identify those at risk can be feasibly implemented. One challenge of screening at scale is that risk factors associated with opioid misuse among adolescents and young adults include both individual and social factors (Bonar et al., 2020). Key individual factors include early use and misuse of other substances (Garnier et al., 2009; McCabe et al., 2017), mental health concerns such as depressive symptoms and suicide-related factors (Edlund et al., 2015; Zullig & Divin, 2012), and childhood emotional or physical abuse (Yule et al., 2018a). Social influences of note include access to opioids (Nguyen et al., 2020) and perceived and actual misuse of opioids among peers (Sanders et al., 2014). There are also important sociodemographic and community-level factors to consider, such as region and urbanicity (Champagne-Langabeer et al., 2022; Wilkes et al., 2021), race/ethnicity (Patel et al., 2021), and social determinants of health (Acharya et al., 2022).
Challenges Unique to Settings
In addition to determining various risk factors for opioid misuse and OUD, interventionists must also ensure that recruitment and prevention programs for randomized controlled trials are culturally appropriate and can be feasibly implemented within a setting. To do so, researchers must think through the variety of needs in each setting. For example, in primary care or the emergency department (ED), prevention programming must fit within the allotted time frame of a patient visit, requiring brief interventions (Blow et al., 2006; D’Amico et al., 2018). School settings also require extensive collaboration (D’Amico et al., 2016). Some programs may take place in the classroom, using teachers and classroom time (Ellickson et al., 2003); others may occur after school (D’Amico et al., 2012), which could decrease costs (Kilmer et al., 2011) but pose other challenges (e.g., transportation).
Furthermore, any given setting may serve individuals with differing levels of need, from high to low acuity, so programming must address these different levels. For example, some youth in the school setting may never have used alcohol, whereas others may use it regularly. Similarly, youth in the juvenile justice system may be in an institutionalized or noninstitutionalized setting, have committed different types of offenses, and have varying levels of criminal justice exposure, all of which could affect intervention efficacy (Pappas & Dent, 2021). In addition, many programs also occur across multiple institutional levels (e.g., intervening at both the school and community level) and may require more extensive liaison with local community partners and provision of technical assistance (Chinman et al., 2018).
Finally, participants often face competing demands on their time, limited resources, difficulties with transportation (Dickerson et al., 2021b), or even homelessness (Tucker et al., 2017). Thus, successful interventions must be developed collaboratively with communities to confirm content is developmentally and culturally appropriate. Careful consideration of common barriers further helps to ensure the intervention is feasible to implement and is acceptable and accessible to the specific population.
Many researchers use a community-based participatory research (CBPR) approach when developing and implementing programs, collaborating closely with communities and organizations to ensure that the programming is both developmentally and culturally appropriate for the population (Dickerson et al., 2020; Minkler & Wallerstein, 2011). CBPR approaches are also crucial for continued dissemination and implementation efforts (Blue Bird Jernigan et al., 2020). Innovation occurs when the gap between research and practice is bridged to reach at-risk populations by creating programming that can continue successfully after a project ends.
Challenges Unique to Dissemination and Implementation
The length of time and degree of exposure are other important aspects of prevention programming that should conform to organizational capacity and the needs of adolescents and young adults along the behavioral health continuum. Researchers must assess whether the intervention process achieves desired and measurable outcomes when considering program duration. Adolescent and young adult audiences vary in their ability to commit time and attention to an intervention. Researchers should therefore develop creative and innovative mechanisms of delivery that overcome unique barriers to fidelity, engagement, and acceptance.
Scalable and low-cost interventions delivered with fidelity and requiring less intensive training are needed. For example, digital interventions in the form of video games are a promising mode of delivery because they (1) can reach broader audiences, especially those—like youth—who prefer digital approaches (Lenhart et al., 2008); (2) are more cost effective; (3) provide fidelity in the delivery of content; and (4) are offered in a variety of platforms, including smartphones, iPads, and computers (Lehto & Oinas-Kukkonen, 2011; Noar et al., 2009). Although longer exposure and duration has been shown to improve outcomes in traditional interventions, they may not be as relevant for video game interventions (Charlier et al., 2016). For example, one study noted that beating and completing video game levels—as opposed to the duration of the video game—increased knowledge (Montanaro et al., 2015).
It is also critical to consider contextual factors and feasibility. Schools and clinics often have numerous demands to meet and limited time in their schedules. For example, although 12 sessions totaling 10 h may be consistent with the duration of effective substance use prevention interventions (Griffin et al., 2010) and the amount of time adolescents play games, implementers must consider these time-constrained contexts (e.g., school-based health centers) due to conflicting demands, particularly as higher doses (i.e., more sessions) and longer duration are correlated with less acceptance of the intervention (Gresham, 2019). Thus, delivering an intervention with higher doses or longer duration may be challenging in some settings.
Challenges Unique to Tailoring Prevention Programs and Strategies
EBPPs for adolescents and young adults need to be tailored by integrating a developmental perspective in terms of language and content. Independence and autonomy from parent or guardian supervision increase with age, and young adults typically have more mature roles and responsibilities (Cadigan et al., 2019). Content should also be tailored to reflect access (e.g., prescriptions from healthcare providers, diversion via family and friends). Furthermore, content should be tailored to address diversity in motives for opioid misuse, whether enhancement (e.g., to experiment, to get high), medical (e.g., sleep, pain), or psychological reasons (coping with distress; Boyd et al., 2009; Havens et al., 2011; McCauley et al., 2011). EBPPs may offer alternatives to address these motives, such as enhancing pro-social activities with peers (e.g., extracurricular activities), managing pain, and coping with mental health issues. Finally, the severity of opioid misuse requires tailoring of intervention content (e.g., frequency of use, route of administration), with further referrals and resources provided as appropriate for those identified as needing indicated prevention or treatment approaches.
Overview of the HEAL Prevention Cooperative (HPC)
The Helping to End Addiction Long-TermSM (HEAL) Initiative is a dynamic trans-agency effort of the National Institutes of Health (NIH) to accelerate science-based solutions to address the national opioid crisis. The initiative funds hundreds of projects nationwide so that researchers can develop varied approaches quickly. The HPC consists of a coordinating center and 10 research projects (RPs) testing and developing EBPPs for various higher-risk segments of the US youth population. The HPC aligns prevention scientists across the country in collaborative work to understand which prevention strategies and delivery processes are most effective for specific subsets of the population who live in different geographic locations and have unique risk profiles. As part of this work, the HPC is harmonizing measures (Ridenour et al., 2022), assessing individual and collective economic impact (Dunlap, 2022), and assessing common barriers and facilitators of implementation (Patel et al., 2022). We highlight 6 of the 10 HPC RPs and how they implement EBPPs with consideration of population, setting, dissemination and implementation, and tailoring to their populations.
Community-Randomized Trial in the Cherokee Nation: Universal Prevention
The Cherokee Nation is the largest federally recognized American Indian/Alaska Native (AI/AN) tribe with nearly 370,000 registered tribal members. Within the reservation area fixed by treaty in 1866, the Cherokee Nation currently shares jurisdictional authority with the state of Oklahoma and county and municipal governments. Cherokee Nation Behavioral Health is in Tahlequah, Oklahoma, the capital of the Cherokee Nation. Its leaders have partnered with prevention scientists at Emory University Rollins School of Public Health (principal investigator (PI): Komro) to implement and rigorously evaluate a theory-based, integrated multilevel community intervention designed to prevent the onset and escalation of opioid and other drug misuse among a cohort of older adolescents (15–20 years old) living in or near the Cherokee Nation reservation within small rural communities (Komro et al., 2022). The study involves 20 high schools, with approximately half of students identifying as AI.
The study focus is universal primary prevention among multiethnic and multicultural rural communities. Rural white and AI/AN populations are two subgroups that have been hit hard by the opioid crisis and have also experienced persistent disparities related to alcohol and suicide risk (Harris, 2021; Venner et al., 2018). The AI/AN youth are at greater risk of early onset of alcohol and drug use, which puts them at higher risk for misuse of opioids into adulthood (Stanley et al., 2020). Universal and evidence-based alcohol and drug use prevention approaches are being adapted to address risk for opioid misuse onset, including screening and brief interventions with motivational interviewing delivered within schools, training for teachers and others in identifying and responding to mental health and drug use challenges, and promoting family and community preventive actions including reducing access to opioids and other drugs.
Traditions and Connections for Urban Native Americans: Universal Prevention
RAND and the University of California, Los Angeles (UCLA; PI: D’Amico, Dickerson) have partnered with the Sacred Path Indigenous Wellness Center (SPIWC), a non-profit organization that provides substance use and mental health services for the AI/AN people. For more than 2 decades, the RAND/UCLA/SPIWC research team has been funded by the NIH to develop and test culturally centered substance use treatment and prevention programs for urban AI/AN individuals (D’Amico et al., 2020; Dickerson et al., 2012, 2016, 2021a). The aims of the current study are to test a developmentally and culturally appropriate prevention intervention among urban AI/AN emerging adults (D’Amico et al., 2021).
Researchers conducted focus groups across California, meeting with providers, parents, and AI/AN emerging adults (D’Amico et al., 2021). Focus group participants noted the challenges that urban AI/AN emerging adults face, leading to the creation of two developmentally and culturally appropriate, virtual, prevention interventions. Study participants will be randomized to one of two culturally appropriate interventions, Traditions and Connections for Urban Native Americans (TACUNA), which comprises three workshops and a wellness circle, or a culturally tailored opioid education workshop.
A Digital Intervention to Prevent the Initiation of Opioid Misuse in Adolescents in School-Based Health Centers: Selective Prevention
In partnership with Schell Games and the national School-Based Health Alliance (SBHA), the play2PREVENT Lab (p2P) at the Yale Center for Health & Learning Games developed PlaySMART, a video game intervention to prevent the initiation of opioid misuse and to promote mental health among adolescents ages 16–19 (PI: Fiellin). Focus groups and interviews were conducted with youth, Freedom from Chemical Dependency (FCD; FCD 2016) prevention specialists, SBHA adult affiliates, the SBHA Youth Advisory Council, and OUD treatment providers to inform the relatable storylines, characters, and graphics of PlaySMART. Six distinct storyline themes and six distinct mini-games were designed from the focus group and interview input.
Targeting mental health strategies emerged as a salient theme for addressing opioid misuse prevention among this population. For example, most youth in the focus groups noted that they either dealt with mental health concerns on their own or knew someone who did. Several stories and mini-games thus focus on incorporating mental health strategies, including identifying adaptive coping strategies and seeking help from trusted adults, throughout the video game intervention (Michelmore & Hindley, 2012). Even though youth noted a high prevalence of challenges related to mental health among their peers or personally, a stigma associated with seeking help remains, and youth felt a significant amount of distrust toward providers. Given that adolescents are hesitant to seek help for mental health (Carlton & Deane, 2000) and that peer support may help them do so (Byrom, 2018), the storyline of one mini-game highlights the value of peers supporting peers and the therapeutic alliance to normalize the process. Through these storylines and mini-games, the goal is to empower youth to feel that they can guide their experience in seeking appropriate support for their peers and for themselves.
Optimized Interventions to Prevent OUD Among Adolescents and Young Adults in the Emergency Department (ED): Selective Prevention
In healthcare settings, efforts to reduce morbidity and mortality due to opioids have focused on either end of the continuum of care—changing provider behaviors to modify prescribing practices or treating those with OUD (e.g., medication-assisted treatment, linkage to substance use disorder treatment services such as peer recovery coaches (Magidson et al., 2021). Thus, selective-focused EBPPs for adolescents and young adults in healthcare settings who are at risk of or are currently misusing opioids are critically needed. To address this gap, the University of Michigan team (PIs: Walton, Bonar) refined, packaged, and pilot tested promising interventions from prior work (Bohnert et al., 2016; Cunningham et al., 2015; King et al., 2015; Walton et al., 2014), integrating motivational interviewing (MI; Miller & Rollnick, 2013) and cognitive behavioral therapy (Waldron & Kaminer, 2004) approaches to address opioid misuse risk factors.
The population includes ED patients, ages 16–30, who screen positive based on self-report for past 12-month prescription or illicit opioid misuse, or past 12-month prescription opioid misuse plus at least one other substance use or mental health risk factor (see Bonar et al., 2021). Among those screening positive, the study uses a 2 × 2 factorial randomized controlled trial design to test intervention combinations, including a single telehealth session with a health coach only, 30 days of portal messaging only, health coach session combined with portal messaging, and control brochure. The session uses MI concepts (e.g., supporting autonomy, acceptance, collaboration, evocation) to focus on “why change” (e.g., goals and strengths; risk perceptions of opioid medications, overdose; benefits of change) and “how to change” (e.g., individualized tools to address motives such as pain, coping, overdose, safe driving, and leisure). In the portal, health coaches send messages using MI strategies to engage participants in a dialog about opioid misuse, motives, and risk factors consistent with the Why and How model (Resnicow & McMaster, 2012). Harnessing technology to facilitate delivery of these resource-light behavioral health interventions will enhance translation of these selective prevention efforts into routine clinical care to reduce opioid misuse among adolescents and young adults, filling the gap between promotion and treatment for adolescents and young adults seen in the ED.
Preventing Opioid Use Among Justice-Involved Youth As They Transition to Adulthood: Leveraging Safe Adults—Indicated Prevention
Youth transitioning out of secure residential facilities are especially vulnerable to substance use after release because of criminal histories, associated stigma, histories of trauma, and fractured social relationships. The Texas Christian Uniersity’s Leveraging Safe Adults (LeSA) Project examines the effectiveness of Trust-based Relational Intervention (TBRI) to prevent opioid use among youth ages 15–18 as they transition from secure residential facilities to their home environment (PI: Knight). The intervention was initially conceptualized as a selective prevention intervention because it targets a group with higher-than-average risk for substance use: justice-involved youth. However, a large proportion of such youth are already misusing substances when they enter the system (Dennis et al., 2019; Mulvey et al., 2010) or have a SUD. For these reasons, components of the intervention have been adapted for use with individuals at the highest risk, making it appropriately classified as an indicated prevention intervention.
TBRI is an attachment-based, trauma-informed intervention designed to improve youth self-regulation through healthy relationships (Purvis et al., 2013). Youth and their caregivers (the individuals to whom the youth will be released) participate in group sessions where they learn and practice healthy connection (mindfulness, engagement strategies to promote empathy, and felt safety), empowerment (physiological and ecological strategies to address physical and sensory needs), and correction (proactive and responsive strategies to promote self-regulation and healthy choices). Caregivers learn how to help youth identify their needs and express themselves appropriately and to meet (and advocate for) their youth’s needs in proactive ways and model healthy relationships. Caregivers also learn strategies for helping youth navigate the inherent challenges of adolescence, which are often compounded by histories of complex developmental trauma and strained relationships.
The original TBRI caregiver intervention was developed for younger children in foster and adoptive families; the LeSA Project adapted the curriculum to address challenges that may occur due to both the population and setting. Language, terminology, examples, and activities have been modified to be more relevant for justice-involved youth and families and to avoid the potential for biological parents to feel blame or shame regarding past parenting practices. Because changing family dynamics can have significant repercussions for family roles and expectations, and because an important aim of TBRI is to help families increase youths’ feelings of safety, a companion group for youth was created. While caregivers learn TBRI principles and strategies in caregiver-only sessions, youth explore the same strategies with peers in youth-specific sessions. Families then practice new skills together as they plan for the youth’s transition back home.
Does Treating Young Persons’ Psychopathology Prevent the Onset of OUD and Other SUDs? Indicated Prevention
Behavioral health clinics are positioned to intervene and even possibly prevent the development and exacerbation of OUD and SUDs among adolescents and young adults. However, many behavioral health clinics do not systematically screen for these conditions (Zimmerman & McGlinchey, 2008). If they do screen, they may do so once at intake and not again over the course of treatment (Jensen-Doss et al., 2018). Massachusetts General Hospital and Boston Medical Center, both large, urban academic medical centers, are implementing patient-reported outcome measures (PROMs) in their electronic health record systems to screen for OUD/SUDs at five of their behavioral health clinics serving patients ages 16–30 (PIs: Wilens, Yule). Conditions commonly treated at these clinics include depressive, anxiety, somatic, attention, conduct, or traumatic stress disorders, each of which confers increased risk for OUD in adolescents (Yule et al., 2018b). The PROMs use validated instruments to conduct repeated systematic screening at intake and follow-up for initiation or escalation of opioid or substance use. Using electronic health record information, researchers will examine the development of OUD/SUDs and health service utilization (e.g., ED visits, medication prescriptions, billing diagnoses) among patients receiving care in these clinics. The main hypothesis is that systematic screening will help identify and treat budding issues with opioid or other substance misuse. The study will also examine the impact of high- and low-health-service utilization on prevention of OUDs/SUDs and will identify possible mediating and moderating variables that influence outcomes.
Conclusion
In summary, the HPC seeks to fill a gap in prevention work among diverse populations by developing and offering the field a range of EBPPs across the prevention continuum—universal, selective, and indicated approaches. Teams planning for prevention efforts focused on opioid misuse will make different decisions about where to focus on this continuum, depending on the setting and population served and considering issues of scalability and sustainability. The intervention content and delivery mechanism should be tailored to the population and setting, including careful consideration of fidelity and duration to enhance efficacy and adoption. The RPs described here illustrate these considerations as applied to prevention of opioid misuse and offer preventionists options for many of our underserved adolescents and young adults living through the opioid epidemic.
Funding
The following grants from the National Institute on Drug Abuse (NIDA) supported the authors in the development of this article: Cance/Adams/Saavedra/Ridenour, U24 DA050182; D’Amico/Palimaru, UG3/UH3 DA050235; Fiellin/Fernandes, UG3/UH3 DA050251; Walton/Bonar, UG3/UH3 DA050173; Komro, UG3/UH3 DA050234; Knight/Knight, UG3/UH3 DA050250; Youn/Rao, UG3/UH3 DA050252. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or its HEAL Initiative.
Footnotes
Conflict of Interest Dr. Fiellin holds equity with Playbl, Inc., a small commercial venture that focuses on the distribution of evidence-based video games for risk reduction and prevention in youth and young adults. This relationship is extensively managed by Dr. Fiellin and her academic institution.
References
- Acharya A, Izquierdo AM, Gonçalves SF, Bates RA, Taxman FS, Slawski MP, et al. (2022). Exploring county-level spatiotemporal patterns in opioid overdose related emergency department visits. PLoS ONE, 17(12):e0269509. 10.1371/journal.pone.0269509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bao Y, Wen K, Johnson P, Jeng PJ, Meisel ZF, & Schackman BR (2018). Assessing the impact of state policies for prescription drug monitoring programs on high-risk opioid prescriptions. Health Affairs, 37(10), 1596–1604. 10.1377/hlthaff.2018.0512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco C, Wall MM, & Olfson M (2022). Data needs and models for the opioid epidemic. Molecular Psychiatry, 27(2), 787–792. 10.1038/s41380-021-01356-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blow FC, Barry KL, Walton MA, Maio RF, Chermack ST, Bingham CR, Ignacio RV, & Strecher VJ (2006). The efficacy of two brief intervention strategies among injured, at-risk drinkers in the emergency department: impact of tailored messaging and brief advice. Journal of Studies on Alcohol, 67(4), 568–578. 10.15288/jsa.2006.67.568 [DOI] [PubMed] [Google Scholar]
- Bohnert AS, Bonar EE, Cunningham R, Greenwald MK, Thomas L, Chermack S, Blow FC, & Walton M (2016). A pilot randomized clinical trial of an intervention to reduce overdose risk behaviors among emergency department patients at risk for prescription opioid overdose. Drug and Alcohol Dependence, 163, 40–47. 10.1016/j.drugalcdep.2016.03.018 [DOI] [PubMed] [Google Scholar]
- Bohnert ASB, Guy GP Jr., & Losby JL (2018). Opioid prescribing in the United States before and after the Centers for Disease Control and Prevention’s 2016 opioid guideline. Annals of Internal Medicine, 169(6), 367–375. 10.7326/m18-1243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonar EE, Coughlin L, Roche JS, Philyaw-Kotov ML, Bixler EA, Sinelnikov S, Kolosh A, Cihak MJ, Cunningham RM, & Walton MA (2020). Prescription opioid misuse among adolescents and emerging adults in the United States: a scoping review. Preventive Medicine, 132, 105972. 10.1016/j.ypmed.2019.105972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonar EE, Kidwell KM, Bohnert ASB, Bourque CA, Carter PM, Clark SJ, Glantz MD, King CA, Losman ED, McCabe SE, Philyaw-Kotov ML, Prosser LA, Voepel-Lewis T, Zheng K, & Walton MA (2021). Optimizing scalable, technology-supported behavioral interventions to prevent opioid misuse among adolescents and young adults in the emergency department: a randomized controlled trial protocol. Contemporary Clinical Trials, 108, 106523. 10.1016/j.cct.2021.106523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd CJ, Teter CJ, West BT, Morales M, & McCabe SE (2009). Non-medical use of prescription analgesics: a three-year national longitudinal study. Journal of Addictive Diseases, 28(3), 232–242. 10.1080/10550880903028452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrom N. (2018). An evaluation of a peer support intervention for student mental health. Journal of Mental Health, 27(3), 240–246. 10.1080/09638237.2018.1437605 [DOI] [PubMed] [Google Scholar]
- Cadigan JM, Duckworth JC, Parker ME, & Lee CM (2019). Influence of developmental social role transitions on young adult substance use. Current Opinion in Psychology, 30, 87–91. 10.1016/j.copsyc.2019.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlton PA, & Deane FP (2000). Impact of attitudes and suicidal ideation on adolescents’ intentions to seek professional psychological help. Journal of Adolescence, 23(1), 35–45. 10.1006/jado.1999.0299 [DOI] [PubMed] [Google Scholar]
- Champagne-Langabeer T, Cardenas-Turanzas M, Ugalde IT, Bakos-Block C, Stotts AL, Cleveland L, Shoptaw S, & Langabeer JR (2022). The impact of pediatric opioid-related visits on U.S. emergency departments. Children (Basel), 9(4). 10.3390/children9040524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlier N, Zupancic N, Fieuws S, Denhaerynck K, Zaman B, & Moons P (2016). Serious games for improving knowledge and self-management in young people with chronic conditions: a systematic review and meta-analysis. Journal of the American Medical Informatics Association, 23(1), 230–239. 10.1093/jamia/ocv100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinman M, Ebener P, Malone PS, Cannon J, D’Amico EJ, & Acosta J (2018). Testing implementation support for evidence-based programs in community settings: a replication cluster-randomized trial of Getting To Outcomes(R). Implementation Science, 13(1), 131. 10.1186/s13012-018-0825-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham RM, Chermack ST, Ehrlich PF, Carter PM, Booth BM, Blow FC, Barry KL, & Walton MA (2015). Alcohol interventions among underage drinkers in the ED: a randomized controlled trial. Pediatrics, 136(4), e783–793. 10.1542/peds.2015-1260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Dickerson DL, Brown RA, Johnson CL, Klein DJ, & Agniel D (2020). Motivational interviewing and culture for urban Native American youth (MICUNAy): a randomized controlled trial. Journal of Substance Abuse Treatment, 111, 86–99. 10.1016/j.jsat.2019.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Dickerson DL, Rodriguez A, Brown RA, Kennedy DP, Palimaru AI, Johnson C, Smart R, Klein DJ, Parker J, McDonald K, Woodward MJ, & Gudgell N (2021). Integrating traditional practices and social network visualization to prevent substance use: study protocol for a randomized controlled trial among urban Native American emerging adults. Addiction Science & Clinical Practice, 16(1), 56. 10.1186/s13722-021-00265-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Osilla KC, & Stern SA (2016). Prevention and intervention in the school setting. In Sher KJ (Ed.), The Oxford handbook of substance use disorders (Vol. 2, pp. 675–723). Oxford University Press. [Google Scholar]
- D’Amico EJ, Parast L, Shadel WG, Meredith LS, Seelam R, & Stein BD (2018). Brief motivational interviewing intervention to reduce alcohol and marijuana use for at-risk adolescents in primary care. Journal of Consulting and Clinical Psychology, 86(9), 775–786. 10.1037/ccp0000332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Tucker JS, Miles JN, Zhou AJ, Shih RA, & Green HD Jr. (2012). Preventing alcohol use with a voluntary after-school program for middle school students: results from a cluster randomized controlled trial of CHOICE. Prevention Science, 13(4), 415–425. 10.1007/s11121-011-0269-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis M, Smith C, Belenko S, Knight D, Dembo R, Robertson A, & Wiley T (2019). Operationalizing a behavioral health services cascade of care model: lessons learned from a 33-site implementation in juvenile hustice community supervision 1. Federal Probation, 83. [PMC free article] [PubMed] [Google Scholar]
- Dickerson D, Baldwin JA, Belcourt A, Belone L, Gittelsohn J, & Keawe’aimoku Kaholokula J, Lowe J, Patten CA, & Wallerstein N (2020). Encompassing cultural contexts within scientific research methodologies in the development of health promotion interventions. Prevention Science, 21(Suppl 1), 33–42. 10.1007/s11121-018-0926-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson D, Johnson C, Castro C, Naswood E, & Leon J (2012). Community voices: integrating traditional healing services for urban American Indians/Alaska Natives in Los Angeles County. Learning Collaborative Summary Report, 1–42. [Google Scholar]
- Dickerson DL, Brown RA, Johnson CL, Schweigman K, & D’Amico EJ (2016). Integrating motivational interviewing and traditional practices to address alcohol and drug use among urban American Indian/Alaska Native youth. Journal of Substance Abuse Treatment, 65, 26–35. 10.1016/j.jsat.2015.06.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson DL, D’Amico EJ, Klein DJ, Johnson CL, Hale B, Ye F, & Dominguez BX (2021a). Drum-Assisted Recovery Therapy for Native Americans (DARTNA): results from a feasibility randomized controlled trial. Journal of Substance Abuse Treatment, 126, 108439. 10.1016/j.jsat.2021.108439 [DOI] [PubMed] [Google Scholar]
- Dickerson DL, Parker J, Johnson CL, Brown RA, & D’Amico EJ (2021b). Recruitment and retention in randomized controlled trials with urban American Indian/Alaska Native adolescents: challenges and lessons learned. Clinical Trials (london, England), 18(1), 83–91. 10.1177/1740774520971774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowell D, Haegerich TM, & Chou R (2016). CDC guideline for prescribing opioids for chronic pain–United States, 2016. JAMA, 315(15), 1624–1645. 10.1001/jama.2016.1464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunlap LJ, Kuklinski MR, Cowell A, et al. (2022). Economic Evaluation Design within the HEAL Prevention Cooperative. Prevention Science. 10.1007/s11121-022-01400-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edlund MJ, Forman-Hoffman VL, Winder CR, Heller DC, Kroutil LA, Lipari RN, & Colpe LJ (2015). Opioid abuse and depression in adolescents: results from the National Survey on Drug Use and Health. Drug and Alcohol Dependence, 152, 131–138. 10.1016/j.drugalcdep.2015.04.010 [DOI] [PubMed] [Google Scholar]
- Ellickson PL, McCaffrey DF, Ghosh-Dastidar B, & Longshore DL (2003). New inroads in preventing adolescent drug use: results from a large-scale trial of project ALERT in middle schools. American Journal of Public Health, 93(11), 1830–1836. 10.2105/ajph.93.11.1830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank D, Mateu-Gelabert P, Guarino H, Bennett A, Wendel T, Jessell L, & Teper A (2015). High risk and little knowledge: overdose experiences and knowledge among young adult nonmedical prescription opioid users. International Journal on Drug Policy, 26(1), 84–91. 10.10167/j.drugpo.2014.07.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedom from Chemical Dependency (FCD). (2016). Home page. Retrieved August 20, 2021, from https://fcd.org
- Garnier LM, Arria AM, Caldeira KM, Vincent KB, O’Grady KE, & Wish ED (2009). Nonmedical prescription analgesic use and concurrent alcohol consumption among college students. American Journal of Drug and Alcohol Abuse, 35(5), 334–338. 10.1080/00952990903075059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gresham FM (2019). Conceptualizing behavior disorders in terms of resistance to intervention. School Psychology Review, 20(1), 23–36. 10.1080/02796015.1991.12085530 [DOI] [Google Scholar]
- Griffin JA, Umstattd MR, & Usdan SL (2010). Alcohol use and high-risk sexual behavior among collegiate women: a review of research on alcohol myopia theory. Journal of American College Health, 58(6), 523–532. 10.1080/07448481003621718 [DOI] [PubMed] [Google Scholar]
- Harris BR (2021). Suicide as a hidden contributor to the opioid crisis and the role that primary care and emergency medicine play in addressing it. Preventive Medicine, 106572. 10.1016/j.ypmed.2021.106572 [DOI] [PubMed] [Google Scholar]
- Havens JR, Young AM, & Havens CE (2011). Nonmedical prescription drug use in a nationally representative sample of adolescents: evidence of greater use among rural adolescents. Archives of Pediatrics and Adolescent Medicine, 165(3), 250–255. 10.1001/archpediatrics.2010.217 [DOI] [PubMed] [Google Scholar]
- Hoots BE (2021). Opioid overdose surveillance : improving data to inform action. Public Health Reports, 136(1_suppl), 5S–8S. 10.1177/00333549211020275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudgins JD, Porter JJ, Monuteaux MC, & Bourgeois FT (2019). Prescription opioid use and misuse among adolescents and young adults in the United States: a national survey study. PLoS Medicine, 16(11), e1002922. 10.1371/journal.pmed.1002922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. (1994). Reducing risks for mental disorders: Frontiers for preventive intervention research. The National Academies Press. 10.17226/2139 [DOI] [PubMed] [Google Scholar]
- Jalali MS, Botticelli M, Hwang RC, Koh HK, & McHugh RK (2020). The opioid crisis: a contextual, social-ecological framework. Health Research Policy and Systems, 18(1), 87. 10.1186/s12961-020-00596-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen-Doss A, Smith AM, Becker-Haimes EM, Mora Ringle V, Walsh LM, Nanda M, Walsh SL, Maxwell CA, & Lyon AR (2018). Individualized progress measures are more acceptable to clinicians than sandardized masures: results of a national survey. Administration and Policy in Mental Health, 45(3), 392–403. 10.1007/s10488-017-0833-y [DOI] [PubMed] [Google Scholar]
- Jernigan BB&V, D’Amico EJ, & Keawe’aimoku Kaholokula J (2020). Prevention research with indigenous communities to expedite dissemination and implementation efforts. Prevention Science, 21(Suppl 1), 74–82. 10.1007/s11121-018-0951-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilmer B, Burgdorf JR, D’Amico EJ, Miles J, & Tucker J (2011). Multisite cost analysis of a school-based voluntary alcohol and drug prevention program. Journal of Studies on Alcohol and Drugs, 72(5), 823–832. 10.15288/jsad.2011.72.823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King CA, Eisenberg D, Zheng K, Czyz E, Kramer A, Horwitz A, & Chermack S (2015). Online suicide risk screening and intervention with college students: a pilot randomized controlled trial. Journal of Consulting and Clinical Psychology, 83(3), 630–636. 10.1037/a0038805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komro KA, D’Amico EJ, Dickerson DL, et al. (2022). Culturally responsive opioid and other drug prevention for American Indian/Alaska Native People: a comparison of reservation- and urban-based Approaches. Prevention Science. 10.1007/s11121-022-01396-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehto T, & Oinas-Kukkonen H (2011). Persuasive features in web-based alcohol and smoking interventions: a systematic review of the literature. Journal of Medical Internet Research, 13(3), e46. 10.2196/jmir.1559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenhart A, Kahne J, Middaugh E, Macgill A, Evans C, & Vitak J (2008). Teens, video games, and civics: Teens’ gaming experiences are diverse and include significant social interaction and civic engagement. Pew Internet & American Life Project. [Google Scholar]
- Lin LA, Bohnert ASB, Kerns RD, Clay MA, Ganoczy D, & Ilgen MA (2017). Impact of the opioid safety initiative on opioid-related prescribing in veterans. Pain, 158(5), 833–839. 10.1097/j.pain.0000000000000837 [DOI] [PubMed] [Google Scholar]
- Magidson JF, Regan S, Powell E, Jack HE, Herman GE, Zaro C, Kane MT, & Wakeman SE (2021). Peer recovery coaches in general medical settings: changes in utilization, treatment engagement, and opioid use. Journal of Substance Abuse Treatment, 122, 108248. [DOI] [PubMed] [Google Scholar]
- McCabe SE, Veliz P, & Patrick ME (2017). High-intensity drinking and nonmedical use of prescription drugs: results from a national survey of 12th grade students. Drug and Alcohol Dependence, 178, 372–379. 10.1016/j.drugalcdep.2017.05.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCauley JL, Amstadter AB, Macdonald A, Danielson CK, Ruggiero KJ, Resnick HS, & Kilpatrick DG (2011). Nonmedical use of prescription drugs in a national sample of college women. Addictive Behaviors, 36(7), 690–695. 10.1016/j.addbeh.2011.01.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeroy KR, Bibeau D, Steckler A, & Glanz K (1988). An ecological perspective on health promotion programs. Health Education Quarterly, 15(4), 351–377. 10.1177/109019818801500401 [DOI] [PubMed] [Google Scholar]
- Michelmore L, & Hindley P (2012). Help-seeking for suicidal thoughts and self-harm in young people: a systematic review. Suicide and Life-Threatening Behavior, 42(5), 507–524. 10.1111/j.1943-278X.2012.00108.x [DOI] [PubMed] [Google Scholar]
- Miller WR, & Rollnick S (2013). Motivational interviewing: Helping people change (3rd ed.). New York, NY: Guilford Press. [Google Scholar]
- Minkler M, & Wallerstein N (2011). Community-based participatory research for health: From process to outcomes. Hoboken, New Jersey: John Wiley & Sons. [Google Scholar]
- Monico LB, Ludwig A, Lertch E, Dionne R, Fishman M, Schwartz RP, & Mitchell SG (2021). Opioid overdose experiences in a sample of US adolescents and young adults: a thematic analysis. Addiction, 116(4), 865–873. 10.1111/add.15216 [DOI] [PubMed] [Google Scholar]
- Montanaro E, Fiellin LE, Fakhouri T, Kyriakides TC, & Duncan LR (2015). Using videogame apps to assess gains in adolescents’ substance use knowledge: new opportunities for evaluating intervention exposure and content mastery. Journal of Medical Internet Research, 17(10), e245. 10.2196/jmir.4377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulvey EP, Schubert CA, & Chassin L (2010). Substance use and delinquent behavior among serious adolescent offenders: (506942011–001). American Psychological Association. 10.1037/e506942011-001 [DOI] [Google Scholar]
- National Institute on Drug Abuse (NIDA). (2021). Medications to treat opioid use disorder research report: Overview. National Insistutes of Health. Retrieved August 20, 2021, from https://www.drugabuse.gov/publications/research-reports/medications-to-treat-opioid-addiction/overview [Google Scholar]
- Nguyen AP, Glanz JM, Narwaney KJ, & Binswanger IA (2020). Association of opioids prescribed to family members with opioid overdose among adolescents and young adults. JAMA Network Open, 3(3), e201018. 10.1001/jamanetworkopen.2020.1018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noar SM, Black HG, & Pierce LB (2009). Efficacy of computer technology-based HIV prevention interventions: a meta-analysis. AIDS, 23(1), 107–115. 10.1097/QAD.0b013e32831c5500 [DOI] [PubMed] [Google Scholar]
- Pappas LN, & Dent AL (2021). The 40-year debate: a meta-review on what works for juvenile offenders. Journal of Experimental Criminology, 1–30. 10.1007/s11292-021-09472-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel I, Walter LA, & Li L (2021). Opioid overdose crises during the COVID-19 pandemic: implication of health disparities. Harm Reduction Journal, 18(1), 89. 10.1186/s12954-021-00534-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel SV, Cance JD, Bonar EE, Carter PM, Dickerson DL, Fiellin LE, Fernandes CSF, Palimaru AI, Pendergrass Boomer TM, Saldana L, Singh RR, Tinius E, Walton MA, Youn S, Young S, McDaniel S, & Lambdin BH (2022). Accelerating solutions for the overdose crisis: an effectiveness-implementation hybrid protocol for the HEAL Prevention Cooperative. Prevention Science, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purvis KB, Cross DR, Dansereau DF, & Parris SR (2013). Trust-Based Relational Intervention (TBRI): a systemic approach to complex developmental trauma. Children and Youth Services Review, 34(4), 360–386. 10.1080/0145935X.2013.859906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnicow K, & McMaster F (2012). Motivational Interviewing: moving from why to how with autonomy support. The International Journal of Behavioral Nutrition and Physical Activity, 9, 19. 10.1186/1479-5868-9-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes E, Wilson M, Robinson A, Hayden JA, & Asbridge M (2019). The effectiveness of prescription drug monitoring programs at reducing opioid-related harms and consequences: a systematic review. BMC Health Services Research, 19(1), 784. 10.1186/s12913-019-4642-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridenour TA, Cruden G, Yang Y, et al. (2022). Methodological strategies for prospective harmonization of studies: application to 10 distinct outcomes studies of preventive interventions targeting opioid misuse. Prevention Science. 10.1007/s11121-022-01412-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roehler DR, Olsen EO, Mustaquim D, & Vivolo-Kantor AM (2021). Suspected nonfatal drug-related overdoses among youth in the US: 2016–2019. Pediatrics, 147(1). 10.1542/peds.2020-003491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanders A, Stogner J, Seibert J, & Miller BL (2014). Misperceptions of peer pill-popping: The prevalence, correlates, and effects of inaccurate assumptions about peer pharmaceutical misuse. Substance Use and Misuse, 49(7), 813–823. 10.3109/10826084.2014.880485 [DOI] [PubMed] [Google Scholar]
- Stanley LR, Swaim RC, Smith JK, & Conner BT (2020). Early onset of cannabis use and alcohol intoxication predicts prescription drug misuse in American Indian and non-American Indian adolescents living on or near reservations. American Journal of Drug and Alcohol Abuse, 46(4), 447–453. 10.1080/00952990.2020.1767639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strickler GK, Zhang K, Halpin JF, Bohnert ASB, Baldwin GT, & Kreiner PW (2019). Effects of mandatory prescription drug monitoring program (PDMP) use laws on prescriber registration and use and on risky prescribing. Drug and Alcohol Dependence, 199, 1–9. 10.1016/j.drugalcdep.2019.02.010 [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2019). A guide to SAMHSA’s strategic prevention framework. SAMHSA. Retrieved August 20, 2021, from https://www.samhsa.gov/sites/default/files/20190620-samhsa-strategic-prevention-framework-guide.pdf [Google Scholar]
- Tucker JS, D’Amico EJ, Ewing BA, Miles JN, & Pedersen ER (2017). A group-based motivational interviewing brief intervention to reduce substance use and sexual risk behavior among homeless young adults. Journal of Substance Abuse Treatment, 76, 20–27. 10.1016/j.jsat.2017.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venner KL, Donovan DM, Campbell ANC, Wendt DC, Rieckmann T, Radin SM, Momper SL, & Rosa CL (2018). Future directions for medication assisted treatment for opioid use disorder with American Indian/Alaska Natives. Addictive Behaviors, 86, 111–117. 10.1016/j.addbeh.2018.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Jones EB, Einstein EB, & Wargo EM (2019). Prevention and treatment of opioid misuse and addiction: a review. JAMA Psychiatry, 76(2), 208–216. 10.1001/jamapsychiatry.2018.3126 [DOI] [PubMed] [Google Scholar]
- Waldron HB, & Kaminer Y (2004). On the learning curve: the emerging evidence supporting cognitive-behavioral therapies for adolescent substance abuse. Addiction, 99(Suppl 2), 93–105. 10.1111/j.1360-0443.2004.00857.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton MA, Resko S, Barry KL, Chermack ST, Zucker RA, Zimmerman MA, Booth BM, & Blow FC (2014). A randomized controlled trial testing the efficacy of a brief cannabis universal prevention program among adolescents in primary care. Addiction, 109(5), 786–797. 10.1111/add.12469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkes JL, Montalban JN, Pringle BD, Monroe D, Miller A, Zapata I, Brooks AE, & Ross DW (2021). A demographic and regional comparison of opioid-related hospital visits within community type in the United States. Journal of Clinical Medicine, 10(16). 10.3390/jcm10163460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worsham CM, Woo J, Jena AB, & Barnett ML (2021). Adverse events and emergency department opioid prescriptions in adolescents. Health Affairs, 40(6), 970–978. 10.1377/hlthaff.2020.01762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yule AM, Lyons RM, & Wilens TE (2018a). Opioid use disorders in adolescents-updates in assessment and management. Curr Pediatr Rep, 6(2), 99–106. 10.1007/s40124-018-0161-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yule AM, Wilens TE, Martelon M, Rosenthal L, & Biederman J (2018b). Does exposure to parental substance use disorders increase offspring risk for a substance use disorder? A longitudinal follow-up study into young adulthood. Drug and Alcohol Dependence, 186, 154–158. 10.1016/j.drugalcdep.2018.01.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman M, & McGlinchey JB (2008). Depressed patients’ acceptability of the use of self-administered scales to measure outcome in clinical practice. Annals of Clinical Psychiatry, 20(3), 125–129. 10.1080/10401230802177680 [DOI] [PubMed] [Google Scholar]
- Zullig KJ, & Divin AL (2012). The association between nonmedical prescription drug use, depressive symptoms, and suicidality among college students. Addictive Behaviors, 37(8), 890–899. 10.1016/j.addbeh.2012.02.008 [DOI] [PubMed] [Google Scholar]