Key Points
Question
What is the comparative effectiveness associated with transitional care interventions with different complexity levels in improving health care utilization and patient outcomes after hospital discharge?
Findings
In this systematic review and network meta-analysis including 126 trials with 97 408 participants, low- and medium-complexity interventions were associated with decreased odds of readmission at 30 days compared with usual care. All intervention complexities were associated with significant reductions in the odds of readmissions at 180 days.
Meaning
These findings suggest that low- and medium-complexity transitional care interventions may be more effective for reducing readmission for patients transitioning from hospitals to the community.
This systematic review and network meta-analysis evaluates the comparative effectiveness associated with transitional care interventions with different complexity levels at improving health care utilization and patient outcomes in the transition from hospitals to the community.
Abstract
Importance
Discharge from the hospital to the community has been associated with serious patient risks and excess service costs.
Objective
To evaluate the comparative effectiveness associated with transitional care interventions with different complexity levels at improving health care utilization and patient outcomes in the transition from the hospital to the community.
Data Sources
CENTRAL, Embase, MEDLINE, and PsycINFO were searched from inception until August 2022.
Study Selection
Randomized clinical trials evaluating transitional care interventions from hospitals to the community were identified.
Data Extraction and Synthesis
At least 2 reviewers were involved in all data screening and extraction. Random-effects network meta-analyses and meta-regressions were applied. The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines were followed.
Main Outcomes and Measures
The primary outcomes were readmission at 30, 90, and 180 days after discharge. Secondary outcomes included emergency department visits, mortality, quality of life, patient satisfaction, medication adherence, length of stay, primary care and outpatient visits, and intervention uptake.
Results
Overall, 126 trials with 97 408 participants were included, 86 (68%) of which were of low risk of bias. Low-complexity interventions were associated with the most efficacy for reducing hospital readmissions at 30 days (odds ratio [OR], 0.78; 95% CI, 0.66 to 0.92) and 180 days (OR, 0.45; 95% CI, 0.30 to 0.66) and emergency department visits (OR, 0.68; 95% CI, 0.48 to 0.96). Medium-complexity interventions were associated with the most efficacy at reducing hospital readmissions at 90 days (OR, 0.64; 95% CI, 0.45 to 0.92), reducing adverse events (OR, 0.42; 95% CI, 0.24 to 0.75), and improving medication adherence (standardized mean difference [SMD], 0.49; 95% CI, 0.30 to 0.67) but were associated with less efficacy than low-complexity interventions for reducing readmissions at 30 and 180 days. High-complexity interventions were most effective for reducing length of hospital stay (SMD, −0.20; 95% CI, −0.38 to −0.03) and increasing patient satisfaction (SMD, 0.52; 95% CI, 0.22 to 0.82) but were least effective for reducing readmissions at all time periods. None of the interventions were associated with improved uptake, quality of life (general, mental, or physical), or primary care and outpatient visits.
Conclusions and Relevance
These findings suggest that low- and medium-complexity transitional care interventions were associated with reducing health care utilization for patients transitioning from hospitals to the community. Comprehensive and consistent outcome measures are needed to capture the patient benefits of transitional care interventions.
Introduction
An increased demand for urgent hospital care has created pressure to discharge patients to the community,1 with some patients being discharged too early or without necessary support to recover in the community. especially during the COVID-19 pandemic.2,3 There is evidence that 1 in 5 patients may experience suboptimal or unsafe care around the time of discharge from a hospital, mainly because of the prompt reduction in continuity of care and coordination challenges of multiple independent professionals and agencies.1,4,5
To date, several trials have evaluated transitional care interventions to improve health care utilization and patient outcomes in the transition from hospitals to the community. Some interventions include multiple components,6 implemented mainly prior to discharge but some also after discharge,7,8 and/or involve a care coordinator or case manager.9,10 Other less-intensive interventions target 1 key challenge of the discharge process (eg, medication safety)11,12 at 1 stage of the discharge process.13,14 A number of systematic reviews suggest that various transitional care interventions are promising for improving health care utilization and possibly patient outcomes.15,16,17,18 However, most of these systematic reviews have focused on certain health care settings or populations or have included data from varying study designs that cannot be pooled together.19,20 Hence, despite the large number of trials conducted to improve discharge from hospitals to the community, there is no definitive evidence on how intensive (in terms of the number of components and number of discharge stages) transitional care interventions must be to work best, and whether different intervention complexity levels are best for improving certain outcomes.
This systematic review and network meta-analysis21 examined the comparative effectiveness and uptake associated with different intensities of transitional care interventions in improving health care utilization and patient outcomes in the transition from the hospital to the community.
Methods
This systematic review and network meta-analysis is reported following the Preferred Reporting Items for Systematic Reviews and Meta-analyses Extension Statement for Reporting of Systematic Reviews Incorporating Network Meta-analyses of Health Care Interventions (PRISMA-NMA) reporting guideline.22 The review protocol is registered on PROSPERO (record No. CRD42020166169).
Patient and Public Involvement
We regularly consulted a group of 4 patient and carer partners who were members of an established patient and public involvement group about the appropriateness of our research questions, development of the review protocol, classification of the complexity levels of transitional care interventions, and selection of the outcome measures of this study. Patient and carer partners also advised on the interpretation of our findings, and their dissemination including drafting lay summaries.
Search Methods
Searches were performed in the Cochrane Central Register of Controlled Trials, CINAHL, Embase, MEDLINE, and PsycINFO from inception until August 2022, with no language restriction. We used combinations of Medical Subject Headings terms and text words in discharge, intervention, readmission, continuity of patient care. The full search strategy for each database is available in eAppendix 1 in Supplement 1. The search strategy was adapted from a Cochrane discharge planning from hospital review19 and the reference lists of 2 relevant reviews were screened.19,20
Eligibility Criteria
Population
All patients in hospitals (acute, rehabilitation, or community) were eligible. Patients of any age, sex, or condition were eligible.
Intervention
Inclusion criteria were randomized clinical trials (RCTs) or cluster RCTs evaluating an intervention for transitional care from hospitals to the community, implemented prior to discharge (discharge planning), after discharge, or across the discharge period (before, bridging, and after). We excluded studies whereby the transitional or discharge element was a minor component of a multifaceted intervention. We also excluded studies that were solely about follow-up in the community without a discharge component.
Comparator
Any comparator was eligible for inclusion. Comparators included usual care, another intervention, minimal intervention, or no intervention.
Outcome
The primary outcomes were readmission at 30, 90, and 180 days after discharge. Secondary outcomes included emergency department (ED) visits, mortality, quality of life (QOL), patient satisfaction, medication adherence, length of stay, primary care and outpatient visits, and intervention uptake.
Data Collection and Extraction
A 3-stage screening was conducted. Title screening was conducted by 2 authors independently (N.T. and M.P.). One author screened 100% of abstracts (N.T.) and 4 authors double-screened 25% of abstracts each, independently (A. Hodkinson, C.K., and A. Hall). One author screened 100% of full texts (N.T.) and 2 authors double-screened 50% each, independently (C.K., A. Hall).
Quantitative data were extracted by 1 author (N.T.) and checked for consistency by 2 authors (A. Hodkinson and M.P.). Descriptive data were extracted by 2 authors (P.P.J. and O.G.W.) and checked for consistency by 2 authors (C.K. and A. Hall). A novel data extraction Excel spreadsheet version 1 (Microsoft) was used that was based on the Cochrane data extraction spreadsheet but refined for the needs of this study. The spreadsheet was piloted on 5 studies and adapted after discussion among 3 authors (N.T., A. Hodkinson, and M.P.).
Classification of Intervention Complexity
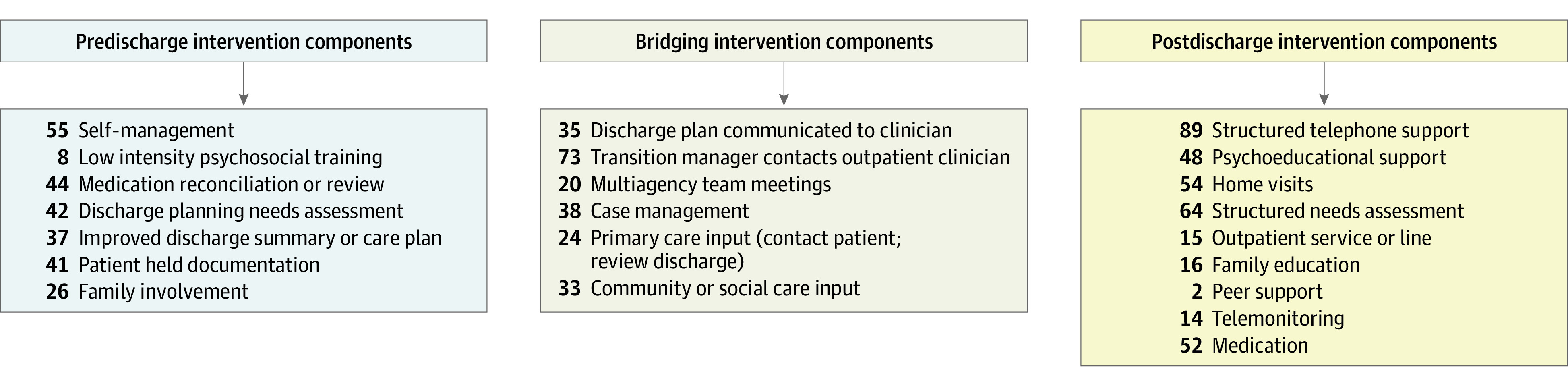
For determining the complexity of the interventions, we focused on the number of key transitional care components included, as well as the number of discharge stages (before discharge, after discharge, or bridging) at which the components were implemented. These components were themed after reviewing previous systematic reviews of transitional care interventions,23,24,25,26,27,28 consultations within our research team, and professionals and patients with lived experience of transitioning from hospitals to the community. The transitional care components per discharge phase are presented in Figure 1. Interventions that included 8 or more of these components were classified as high complexity, those with 4 to 7 components, medium complexity, and those with 1 to 3 components, low complexity.
Figure 1. Transitional Care Components Per Discharge Phase.
Assessment of Risk of Bias
We used 4 risk of bias (ROB) criteria from the Cochrane Risk of Bias Tool for RCTs: allocation concealment (range, 1-3; 3 indicates adequate; 2, less adequate; 1, unclear), intention-to-treat (range, 1-3; 3 indicates yes; 2, no; 1, unclear), attrition (range, 0-2; 2 indicates low [<5%]; 1, medium [5%-20%]; 0, high or unclear [>20%]) and selection reporting bias (range, 0-2; 2 indicates low; 1, medium; 0, unclear); we excluded blinding because it was used in service-level interventions. A total ROB score was calculated for each study, which ranged from 2 to 10. Scores greater than 6 were classified as low ROB overall and scores of 6 of less were classified as high ROB overall.
Missing Data
Study authors were contacted (3 attempts were made) where there was missing or unclear data (eg, relating to the primary outcomes). Studies for which sufficient primary data were not obtained were excluded.
Statistical Analysis
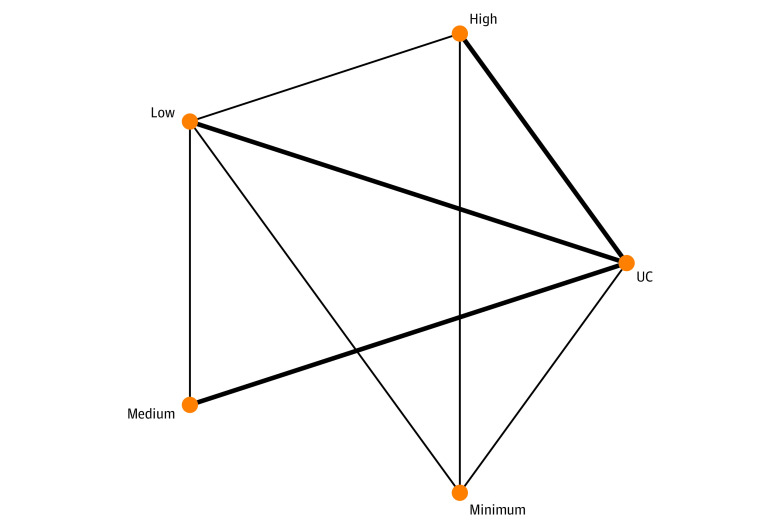
Network Meta-Analyses of Primary Outcomes
We conducted network meta-analyses on the complexity of interventions (low, medium, high), including minimal control interventions, to reduce readmission at 30, 90, and 180 days after discharge; ED visits; mortality; and intervention uptake compared with usual care (UC) at the level of significance of α = .05. We conducted pairwise meta-analyses using Dersimonian Laird random effects on the complexity of interventions to reduce adverse events, patient safety incidents, medication adherence, length of hospital stay, general QOL, and patient satisfaction at the level of significance of α = .05. We converted the dichotomous outcome data to log odds ratios (ORs) and then back to ORs. Continuous data were converted to the standardized mean difference (SMD), and pooled effect sizes were interpreted according to Cohen criteria.16 The Comprehensive Meta-Analysis version 3 (Biostat) was used to perform the transformations.
Random-effects network meta-analysis models were based on the frequentist package netmeta in R version 4.0.5 (R Project for Statistical Computing). Network graphs scaled by the number of studies and forest plots presented by each intervention complexity compared with no intervention or UC, were presented. League tables of all head-to-head comparisons of interventions were also inspected (eAppendix 2 in Supplement 1). The I2 statistic and the heterogeneity variance in the random effect’s distribution (τ2) were used to measure the extent of the influence of variability across and within studies on intervention effects. Traditionally, values of 25% indicate low heterogeneity; 50%, moderate heterogeneity; and 75%, high heterogeneity. We considered the P-score, a frequentist analogue to surface under the cumulative ranking,18 to rank the interventions’ performance. We separated direct from indirect evidence by use of node splitting to evaluate consistency.19 Cochrane Q statistic was used to calculate consistency throughout the entire network.19 We produced network funnel plots to examine the presence of bias due to small-study effect, which allowed us to visually scrutinize the criterion of symmetry. A sensitivity network meta-analysis for 30- and 90-day readmissions was conducted based on the number of discharge stages (1 to 3) and their 7 combinations (before, after, bridging, before to after, before and bridging, after and bridging, and before, after, and bridging).
Meta-Regressions
A series of univariate network meta-regressions were conducted for readmissions at 30 and 90 days, intervention uptake, and mortality, with a level of significance of α = .05. All models were fitted in OpenBUGS version 3.2.3 (MRC Biostatistics Unit, University of Cambridge) using uninformative prior distributions for the intervention effects and a minimally informative prior distribution for common heterogeneity SD. We assumed uninformative priors for all meta-regression coefficients. Model convergence was ensured by visual inspection of the 3 Markov Chain Monte Carlo chains after considering the Brooks Gelman Rubin diagnostic. Overall, 8 factors were examined, including age (<45, 45 to 59, 60 to 79, ≥80 years), sex (studies involving 54% or more females, studies involving 54% or more males, mixed or not reported), Organization for Economic Cooperation and Development (OECD) (no, yes, or not reported), World Health Organization (WHO) region (Africa, America, Southeast Asia, Europe, Eastern Mediterranean, Western Pacific, or unclear), delivery professional (nurse, pharmacist, medic, care coordinator, multidisciplinary team, 2 professionals, allied health professionals, nonclinical staff, social worker, or not reported), medication reconciliation (no, yes, or not reported), patient population (medical or mental health), ROB, and patient complexity (low vs high, based on studies that explicitly reported the population as high risk, high complexity or described multimorbidity, polypharmacy, vulnerability, and terminal illness).
Results
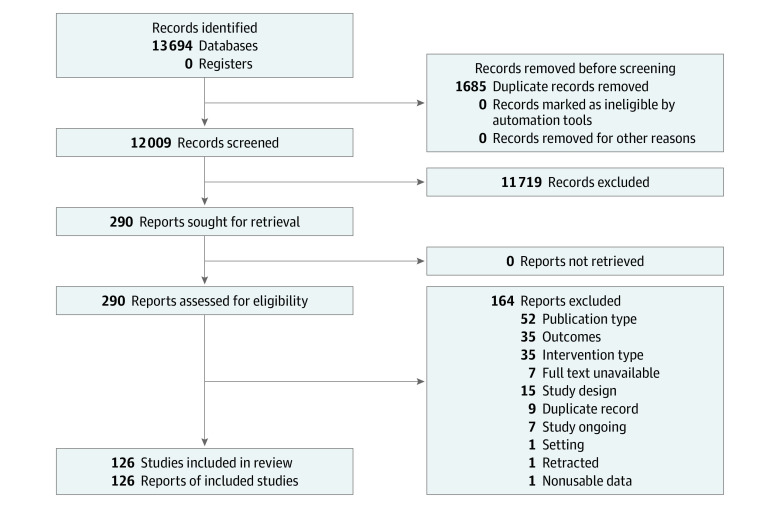
After removing duplicates, the search retrieved 10 685 references. Following title and abstract screening, 274 full texts were retrieved. A total of 126 RCTs7,8,10,11,12,13,14,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148 involving 97 408 participants met our inclusion criteria (Figure 2). The study characteristics are presented in eAppendix 3 in Supplement 1.
Figure 2. Flowchart of Study Selection.
Descriptive Characteristics of the Included Studies
Most studies were conducted in OECD countries (88 studies [70%]); 51 studies (40%) were conducted in the Americas, 35 studies (28%) in Europe, 28 studies (22%) in the Western Pacific, 8 studies (6%) in the Eastern Mediterranean, 3 studies (2%) in Africa, and 1 study (1%) in South-East Asia. Forty-two studies (33%) included mostly female participants, 42 studies (33%) included mostly male participants, and 37 studies (29%) included an equal percentage of male and female participants. The mean age of the participants ranged between 2 and 87 years (median [IQR], 66 [59-75] years). Nine studies (7%) were conducted in mental health hospitals, and the remaining 117 studies (93%) were conducted in general hospitals. There were 56 studies (44%) that did not use a condition reporting index, 21 studies (17%) that used the Charlson Comorbidity Index, 10 studies (8%) that used the New York Heart Association functional classification, and 39 studies (33%) that used another reporting index (eAppendix 3 in Supplement 1).
In assessment of study interventions, 37 studies (29%) applied low-complexity interventions, 41 studies (33%) used medium-complexity interventions, and 48 studies (38%) used high-complexity interventions. In terms of discharge stage, 49 studies (38%) applied intervention elements across all 3 stages (before discharge, after discharge, and bridging), 49 studies (39%) applied intervention elements in 2 stages, and 28 studies (22%) applied the intervention in 1 stage only. We found 45 studies (36%) that included a medication reconciliation component. In 45 studies (36%), interventions were conducted by a nurse, 34 studies (27%) had interventions conducted by another health professional, 29 studies (23%) used a multidisciplinary team, 8 studies (6%) had interventions conducted by social care professionals, and 10 studies (8%) had interventions conducted by others.
Assessment of Risk of Bias
In ROB analysis, 86 studies (68%) were of low ROB, whereas 40 studies (32%) showed high ROB. Ratings for each of the ROB domains are provided in eAppendix 4 in Supplement 1.
Network Meta-Analysis
30-Day Hospital Readmissions
Pooling data from the 73 studies7,8,11,12,13,14,29,30,31,34,35,36,37,38,39,43,45,46,47,48,49,50,51,52,53,54,56,58,59,60,63,67,68,69,70,73,76,77,79,80,81,85,86,87,88,89,90,94,95,96,97,98,102,104,106,111,112,113,114,115,116,119,121,125,127,128,129,131,133,135,141,146,147 (85 direct comparisons) involving 77 201 participants, low-complexity (OR, 0.78; 95% CI, 0.66 to 0.92) and medium-complexity (OR, 0.82; 95% CI, 0.68 to 0.97) interventions were associated with decreased odds of readmission at 30 days compared with usual care (Figure 3; eAppendix 2 in Supplement 1). High-intensity interventions were not associated with reductions in readmissions (OR, 0.96; 95% CI, 0.80 to 1.15). The P-score also showed that low-complexity interventions (P-Score, 89%) were associated with the most efficacy in reducing the 30-day readmission odds. Global heterogeneity of the network was seen to be moderate (I2 = 65%; 95% CI, 53% to 71%). There was evidence of inconsistency through node-splitting analysis in the comparison of high-complexity interventions against minimal interventions (ratio OR, 2.96; 95% CI, 1.20 to 7.29) and the comparison of minimal interventions against usual care (ratio OR, 4.29; 95% CI, 1.80 to 10.18) (eAppendix 5 in Supplement 1). There was evidence of publication bias (Egger P < .001) (eAppendix 6 in Supplement 1), and the league table of head-to-head comparisons also showed that low-complexity (OR, 0.50; 95% CI, 0.32 to 0.77), medium-complexity (OR, 0.52; 95% CI, 0.33 to 0.81), and high-complexity (OR, 0.61; 95% CI, 0.40 to 0.92) interventions were significantly associated with reducing 30-day readmissions compared with minimal interventions.
Figure 3. Network Meta-Analysis of Association of Discharge Intervention Intensities With Reducing 30-Day Readmissions.
Minimum indicates minimal intervention; UC, usual care. Line thickness indicates number of included studies.
Meta-regressions (eAppendix 7 in Supplement 1) showed that low-complexity interventions were associated with more efficacy for reducing 30-day readmissions when delivered by a health professional other than a nurse or social carer (β = −1.51; 95% CI, −2.47 to −0.56; P = .002) and in studies with high ROB (β = −0.88; 95% CI, −2.47 to −0.09; P = .04). Medium-complexity interventions were associated with more efficacy for reducing 30-day readmissions in studies based in Western Pacific (β = −0.84; 95% CI, −1.47 to −0.20; P = .01) compared with the Americas. Sensitivity analysis focused on discharge stages revealed that interventions applied at 1 discharge stage (OR, 0.68; 95% CI, 0.55 to 0.84; P-score = 0.99; I2 = 66%) and especially after discharge (OR, 0.56; 95% CI, 0.40 to 0.78; P-score = 0.90; I2 = 64%) were only associated with reducing 30-day readmissions (eAppendix 8 in Supplement 1).
90-Day Hospital Readmissions
Using data from 34 studies33,36,44,48,54,55,58,61,64,66,67,74,76,81,83,87,91,92,93,95,96,103,105,109,110,117,118,120,123,125,127,130,139,144 (34 direct comparisons) involving 16 774 participants, medium-complexity (OR, 0.64; 95% CI, 0.45 to 0.92), and high-complexity (OR, 0.72; 95% CI, 0.57 to 0.91) interventions were associated decreased odds of readmission at 90 days compared with usual care (eAppendix 2 and eAppendix 9 in Supplement 1). Low-intensity interventions were not associated with reductions in readmissions (OR, 0.65; 95% CI, 0.41 to 1.02). The P-score ranked medium-complexity interventions (P-Score, 73%) as being associated with the most efficacy in reducing 90-day readmissions. Global heterogeneity of the network was seen to be moderate (I2 = 68%; 95% CI, 50% to 78%), and since there was no indirect evidence, inconsistency assessment was not applicable (eAppendix 5 in Supplement 1). However, there was evidence for publication bias (Egger P < .001) (eAppendix 8 in Supplement 1).
Meta-regressions showed that low-complexity interventions were associated with less efficacy for reducing 90-day readmissions in non-OECD countries (β = 1.39; 95% CI, 0.35 to 2.44; P = .009) and when delivered by a professional who was not nurse, other HCP, or social carer (β = 2.30; 95% CI, 0.61 to 3.99; P = .008) or an MDT (β = 1.79; 95% CI, −0.51 to 3.06; P = .006). High-complexity interventions were less effective for reducing 90-day readmissions in studies involving mixed sexes (β = 0.89; 95% CI, 0.30 to 1.48; P = .003) compared with studies with more than 54% female participants.
Sensitivity analysis focused on discharge stage showed that interventions applied at 1 discharge stage were associated with the most efficacy for reducing 90-day readmissions (OR, 0.31; 95% CI, 0.16 to 0.59; P-score = 0.99, I2 = 65%) although interventions with any number of discharge stages were also associated with efficacy. Specifically, interventions at the postdischarge stage (OR, 0.31; 95% CI, 0.16 to 0.59; P-score = 0.95, I2 = 63%) were associated with the most efficacy in reducing 90-day readmissions.
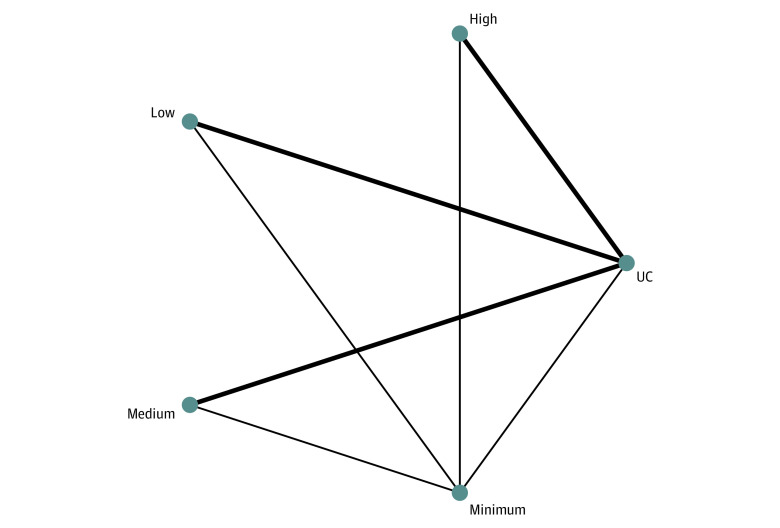
180-Day Hospital Readmissions
Pooling data from 27 studies9,36,40,44,48,55,58,62,75,77,82,85,95,96,97,99,106,107,124,130,134,136,138,140,141,143,145 (34 direct comparisons) involving 13 039 participants, low-complexity (OR, 0.45; 95% CI, 0.30 to 0.66), medium-complexity (OR, 0.57; 95% CI, 0.35 to 0.91), and high-complexity (OR, 0.78; 95% CI, 0.62 to 0.98) interventions were associated decreased odds of readmission at 180 days compared with usual care (Figure 4). The P-score showed that low-complexity interventions (P-Score = 94%) were most effective in reducing the 180-day readmission odds. Global heterogeneity of the network was seen to be moderate (I2 = 64%; 95% CI, 48% to 76%). No evidence of inconsistency in the model was found (eAppendix 5 in Supplement 1), and publication bias assessment revealed no concerns (Egger P = .06) (eAppendix 6 in Supplement 1). The only significant head-to-head finding from the league table of comparisons was that low-complexity interventions were associated with significantly better reductions in 180-day readmissions (OR, 0.57; 95% CI, 0.36 to 0.90) compared with high-complexity interventions.
Figure 4. Network Meta-Analysis of Association of Discharge Intervention Intensities With Reducing 180-Day Readmissions.
Minimum indicates minimal intervention; UC, usual care. Line thickness indicates number of included studies.
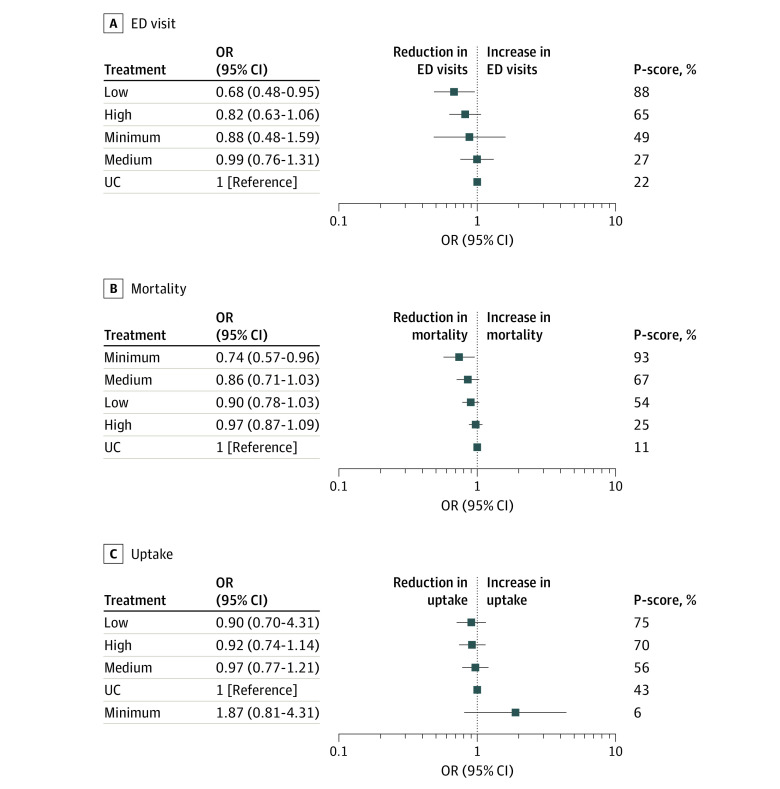
ED Visits
Across 41 studies7,9,29,30,31,34,35,37,39,47,48,49,50,52,56,57,58,60,61,67,68,73,78,80,87,88,94,102,105,106,113,115,119,121,125,130,132,137,145,146,148 (45 direct comparisons) involving 28 034 participants, only low-complexity interventions (OR, 0.68; 95% CI, 0.48 to 0.96) were associated decreased odds of ED visits compared with usual care (Figure 5). The P-score showed that low-complexity interventions (P-Score, 87%) were associated with the most efficacy in reducing the odds of the ED visits. Global heterogeneity of the network was seen to be moderate (I2 = 72%; 95% CI, 60% to 80%), and there was no evidence of inconsistency in the model (eAppendix 5 in Supplement 1). There was evidence of publication bias (Egger P = .03) (eAppendix 6 in Supplement 1).
Figure 5. Association of Intervention Intensity With Emergency Department (ED) Visits, Mortality, and Intervention Uptake.
Minimum indicates minimal intervention; OR, odds ratio; UC, usual care.
Mortality
Across 42 studies7,9,10,12,32,35,37,39,40,44,47,48,56,57,70,76,77,78,79,83,89,91,92,93,94,97,98,100,106,110,111,114,116,121,123,125,127,137,139,141,142,148 (53 direct comparisons) involving 31 988 participants, none of the 3 intervention intensities were significantly associated with reducing mortality compared with usual care (Figure 5). Global heterogeneity of the network was seen to be very low (I2 = 0%; 95% CI, 0% to 36%), and there was no evidence of inconsistency in the model (eAppendix 5 in Supplement 1). There was evidence of publication bias (Egger P = .001) (eAppendix 6 in Supplement 1). Meta-regressions did not reveal significant moderators for the association of intervention intensities with mortality.
Intervention Uptake
Pooling uptake data from 109 studies7,8,9,10,11,12,13,14,29,30,31,32,33,34,35,36,37,38,39,41,43,44,47,49,50,51,52,53,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,72,73,74,75,76,77,78,79,80,81,83,84,85,86,87,88,91,92,93,94,95,96,97,98,99,101,102,103,104,106,107,111,112,113,115,116,117,118,119,120,121,122,123,124,125,126,128,129,131,132,133,134,135,136,137,138,139,140,141,143,144,145,146,147,148 (123 direction comparisons) involving 82 623 participants, none of the intervention intensities were associated with increasing the odds of intervention uptake compared with usual care (Figure 5). Global heterogeneity of the network was seen to be moderate (I2 = 63%; 95% CI, 51% to 67%), and there was no evidence of inconsistency in the model (eAppendix 5 in Supplement 1) or publication bias (Egger P = .41) (eAppendix 6 in Supplement 1). Meta-regressions showed that medium-complexity interventions were associated with lower uptake in studies involving mixed sexes (β = −0.78; 95% CI, −1.55 to −0.02; P = .046) and when delivered in Africa (β = −3.86; 95% CI, −5.41 to −2.30; P < .001).
Pairwise Meta-Analyses
Adverse Events
Medium-complexity interventions were associated decreased odds of adverse events after discharge (5 studies11,102,104,134,138: OR, 0.42; 95% CI, 0.24 to 0.75) without heterogeneity (I2 = 0%; 95% CI, 0% to 75%). Low-complexity (3 studies52,113,116) and high-complexity (3 studies52,84,106) interventions were not significantly associated with reducing adverse events.
Patient Safety Incidents
Low-complexity interventions were associated with decreased odds of patient safety incidents (2 studies14,52: fixed-effects OR, 0.71; 95% CI, 0.53 to 0.94). High-complexity (4 studies31,50,52,56) and medium-complexity (5 studies11,67,102,104,138) interventions were not significantly associated with patient safety incidents.
Medication Adherence
High-complexity (5 studies63,74,86,91,101: SMD, 0.19; 95% CI, 0.03 to 0.36) and medium-complexity (7 studies44,93,94,103,130,134,138: SMD, 0.49; 95% CI, 0.30 to 0.67) interventions were associated with increases in medication adherence. Heterogeneity was low. Low-complexity interventions (3 studies98,119,127) were not significantly associated with medication adherence.
Length of Hospital Stay
High-complexity interventions were associated with reductions in the length of hospital stay (12 studies56,65,71,72,74,87,90,99,101,109,110,112: SMD, −0.20; 95% CI, −0.38 to −0.03). Heterogeneity was high (I2 = 75%; 95% CI, 56% to 86%). Low-complexity (6 studies8,13,38,43,89,126) and medium-complexity (5 studies30,51,55,80,121) interventions were not significantly associated with length of hospital stay.
Patient Satisfaction
High-complexity interventions were associated with increased patient satisfaction (7 studies9,74,81,91,105,133,143: SMD, 0.52; 95% CI, 0.22 to 0.82). Heterogeneity was moderate (I2 = 58%; 95% CI, 3% to 82%). Low-complexity (5 studies7,13,32,43,115) and medium-complexity (4 studies62,67,80,130) interventions were not significantly associated with patient satisfaction.
QOL
None of the intervention intensities were associated with significantly improved QOL. This included general (27 studies9,32,38,44,56,65,66,83,84,85,91,97,105,107,110,112,114,123,125,126,132,133,140,141,145,148), mental (8 studies13,32,81,95,99,131,133,135), or physical QOL (5 studies38,13,81,131,135) QOL measures among patients after discharge.
Discussion
This systematic review and network meta-analysis found that low-complexity interventions, followed by medium-complexity interventions, especially those with a postdischarge component (eg, patient follow-up visit or phone call) were associated with the most efficacy in reducing health care utilization and mortality. These interventions were associated with between 18% and 55% reductions in hospital readmissions compared with usual care. High-complexity interventions were associated with reducing some health care utilization outcomes, but their associations were less pronounced. Moreover, we obtained preliminary evidence from pairwise meta-analysis that medium-complexity interventions might be best for reducing patient and medication harms (ie, adverse events11,102,104,134,138 and medication adherence44,93,94,103,130,134,138) whereas high-complexity interventions might be best for improving patient satisfaction.9,74,81,91,105,133,143 In general, the intervention complexity did not affect the intervention uptake; the only exception was that the uptake of medium-complexity interventions might be lower in low-resource settings, such as African countries, compared with high-resource countries. Moreover, an important but unintended finding of this review was that the range of outcomes reported by interventions was very narrow. Most trials reported hospital readmissions and, at best, some additional health care utilization outcomes (eg, ED visits,7,9,29,30,31,34,35,37,39,47,48,49,50,52,56,57,58,60,61,67,68,73,78,80,87,88,94,102,105,106,113,115,119,121,125,130,132,137,145,146,148 length of hospital stay8,13,30,38,43,51,55,56,65,71,72,74,80,87,89,90,99,101,109,110,112,121,126), and adverse outcomes (mortality7,9,10,12,32,35,37,39,40,44,47,48,56,57,70,76,77,78,79,83,89,91,92,93,94,97,98,100,106,110,111,114,116,121,123,125,127,137,139,141,142,148). Few trials have measured patient-reported outcomes (eg, QOL9,32,38,44,56,65,66,83,84,85,91,97,105,107,110,112,114,123,125,126,132,133,140,141,145,148 and patient satisfaction with the transitional care7,9,13,32,43,62,67,74,80,81,91,105,115,130,133,143) and broader risks for patient harm and safety11,14,31,50,52,56,67,102,104,138; none of the studies reported staff outcomes, despite the fact that transitional care interventions were mostly service delivery interventions relying on staff engagement for their success.
The evidence from previous reviews about the effectiveness of transitional care interventions from hospitals to the community is inconclusive. Direct comparisons with our findings are not possible because to our knowledge, this is the first network meta-analysis that examined the comparative effectiveness of intervention complexities. For example, some reviews have found little or no evidence that discharge planning interventions reduce readmissions,20,26,27 whereas other reviews concluded that intensive interventions promoting integrated systems between inpatient and community care and multidisciplinary working might be most effective.149 However, most of these systematic reviews have focused on hospital subsettings, were underpowered to detect significant reductions in readmissions, or their conclusions reflected the mixed findings of RCTs and observational studies. Our findings are partly consistent with the findings of a previous narrative systematic review15 that examined interventions to improve mental health care transitions and found that less complex interventions targeting 1 specific outcome, such as homelessness, were more likely to be successful compared with more complex interventions that aimed to reduce readmissions.
Our findings convey 3 key messages for clinicians and policymakers. First, low- and medium-complexity interventions may be the most effective options to reduce health care utilization and prevent ED visits for patients transitioning from hospital to the community. Second, the targets and benefits of high-complexity interventions must be reviewed. The achieved reductions in readmission rates may not show good value for the cost of high-complexity interventions,23,150 but improvements in patient and staff experience of discharge could better justify their costs and need for scalable implementation. Third, a core outcome set needs to be developed and used as standard practice by future trials of transitional care interventions. This core outcome set should complement health care utilization outcomes with patient-reported outcomes151,152 and staff-reported outcomes, as staff experiences are important for the success (ie, delivery as planned) and sustainability of service delivery interventions. Key prerequisites to inform actionable clinical practice and guidelines are better understanding of how patient factors and intervention mechanisms impact the effectiveness of transitional care interventions for patients transitioning from hospitals to the community, more comprehensive data on cost-effectiveness, and establishing core outcome sets to capture the full range of benefits and impacts of such interventions.
Strengths and Limitations
This systematic review has numerous methodological strengths but has also important limitations. First, our classification approach is not flawless; for example, some of the components might be more important than others in improving all or some of the health care utilization or patient outcomes. Our classification system of the interventions is an integrated version of similar classification systems that previous reviews have used.23,24,25,26,27,28 We also included expert and patient and public involvement input when deciding on the intervention components of the classification system. However, we recommend that future trials adopt a more standardized approach to reporting the intervention components they have used. This practice will facilitate comparisons between different transitional care interventions and support similar meta-analyses in the future. Second, only a small proportion of the included studies had secondary outcomes including patient-reported outcomes, which precluded the use of network meta-analyses; nevertheless, these outcomes were quantified using pairwise meta-analyses. Moreover, although we did a series of network meta-regressions to identify factors associated with moderating the intervention outcomes, we were not able to examine whether clinical or social characteristics of patients (eg, frailty or multimorbidity, having carers) were confounders in our analyses due to low reporting quality of individual patient–level data.153,154 We used patient complexity as a moderator by comparing studies that explicitly described the patient group as high risk or high complexity or described multimorbidity, polypharmacy, vulnerability, or terminal illness across the whole patient population of the study. However, we recommend individual-patient data meta-analysis to reliably examine whether patient level factors, such as patient complexity or index disease, moderate the effectiveness of different interventions needed. Furthermore, realist reviews could shed further light into the mechanisms of action and implementation of transitional care interventions.155
Conclusions
The findings of this systematic review and meta-analysis mostly supported the use of low- and medium-complexity transitional care interventions for reducing health care utilization for patients transitioning from hospitals to the community. We strongly recommend the development of a core outcome set that will include patient-reported and staff-reported outcomes to better capture the full range of benefits and impacts of transitional care interventions, especially high-complexity interventions.
eAppendix 1. Search Criteria
eAppendix 2. League Table of Head-to-Head Comparisons
eAppendix 3. Characteristics of Included Studies
eAppendix 4. Risk of Bias Assessment
eAppendix 5. Inconsistency Analysis
eAppendix 6. Publication Bias and Funnel Plots
eAppendix 7. Meta-Regressions
eAppendix 8. Sensitivity Analysis
eAppendix 9. 90-Day Readmissions and Secondary Outcomes
Data Sharing Statement
References
- 1.Coleman EA, Berenson RA. Lost in transition: challenges and opportunities for improving the quality of transitional care. Ann Intern Med. 2004;141(7):533-536. doi: 10.7326/0003-4819-141-7-200410050-00009 [DOI] [PubMed] [Google Scholar]
- 2.Safely home: what happens when people leave hospital and care settings? Healthwatch England. July 15, 2015. Accessed September 26, 2018. https://www.healthwatch.co.uk/report/2015-07-21/safely-home-what-happens-when-people-leave-hospital-and-care-settings
- 3.Braithwaite J, Churruca K, Long JC, Ellis LA, Herkes J. When complexity science meets implementation science: a theoretical and empirical analysis of systems change. BMC Med. 2018;16(1):63. doi: 10.1186/s12916-018-1057-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aase K, Schibevaag L, Waring J. Crossing boundaries: quality in care transitions. In: Researching Quality in Care Transitions. Springer International Publishing; 2017:3-29. doi: 10.1007/978-3-319-62346-7_1 [DOI] [Google Scholar]
- 5.Wright N, Rowley E, Chopra A, Gregoriou K, Waring J. From admission to discharge in mental health services: a qualitative analysis of service user involvement. Health Expect. 2016;19(2):367-376. doi: 10.1111/hex.12361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Waring J, Bishop S, Marshall F, Tyler N, Vickers R. An ethnographic study comparing approaches to inter-professional knowledge sharing and learning in discharge planning and care transitions. J Health Organ Manag. 2019;33(6):677-694. doi: 10.1108/JHOM-10-2018-0302 [DOI] [PubMed] [Google Scholar]
- 7.Adamuz J, Viasus D, Simonetti A, et al. Impact of an educational program to reduce healthcare resources in community-acquired pneumonia: the EDUCAP randomized controlled trial. PLoS One. 2015;10(10):e0140202. doi: 10.1371/journal.pone.0140202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Danielsen SO, Moons P, Sandvik L, et al. Impact of telephone follow-up and 24/7 hotline on 30-day readmission rates following aortic valve replacement—a randomized controlled trial. Int J Cardiol. 2020;300:66-72. doi: 10.1016/j.ijcard.2019.07.087 [DOI] [PubMed] [Google Scholar]
- 9.Lainscak M, Kadivec S, Kosnik M, et al. Discharge coordinator intervention prevents hospitalizations in patients with COPD: a randomized controlled trial. J Am Med Dir Assoc. 2013;14(6):450.e1-450.e6. doi: 10.1016/j.jamda.2013.03.003 [DOI] [PubMed] [Google Scholar]
- 10.Meisinger C, Stollenwerk B, Kirchberger I, et al. Effects of a nurse-based case management compared to usual care among aged patients with myocardial infarction: results from the randomized controlled KORINNA study. BMC Geriatr. 2013;13(1):115. doi: 10.1186/1471-2318-13-115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bouchand F, Leplay C, Guimaraes R, et al. Impact of a medication reconciliation care bundle at hospital discharge on continuity of care: a randomised controlled trial. Int J Clin Pract. 2021;75(8):e14282. doi: 10.1111/ijcp.14282 [DOI] [PubMed] [Google Scholar]
- 12.Graabaek T, Hedegaard U, Christensen MB, Clemmensen MH, Knudsen T, Aagaard L. Effect of a medicines management model on medication-related readmissions in older patients admitted to a medical acute admission unit—a randomized controlled trial. J Eval Clin Pract. 2019;25(1):88-96. doi: 10.1111/jep.13013 [DOI] [PubMed] [Google Scholar]
- 13.Dawes HA, Docherty T, Traynor I, Gilmore DH, Jardine AG, Knill-Jones R. Specialist nurse supported discharge in gynaecology: a randomised comparison and economic evaluation. Eur J Obstet Gynecol Reprod Biol. 2007;130(2):262-270. doi: 10.1016/j.ejogrb.2006.02.002 [DOI] [PubMed] [Google Scholar]
- 14.Finn S, D’arcy E, Donovan P, Kanagarajah S, Barras M. A randomised trial of pharmacist-led discharge prescribing in an Australian geriatric evaluation and management service. Int J Clin Pharm. 2021;43(4):847-857. doi: 10.1007/s11096-020-01184-0 [DOI] [PubMed] [Google Scholar]
- 15.Tyler N, Wright N, Waring J. Interventions to improve discharge from acute adult mental health inpatient care to the community: systematic review and narrative synthesis. BMC Health Serv Res. 2019;19(1):883. doi: 10.1186/s12913-019-4658-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lambrinou E, Kalogirou F, Lamnisos D, Sourtzi P. Effectiveness of heart failure management programmes with nurse-led discharge planning in reducing re-admissions: a systematic review and meta-analysis. Int J Nurs Stud. 2012;49(5):610-624. doi: 10.1016/j.ijnurstu.2011.11.002 [DOI] [PubMed] [Google Scholar]
- 17.Steffen S, Kösters M, Becker T, Puschner B. Discharge planning in mental health care: a systematic review of the recent literature. Acta Psychiatr Scand. 2009;120(1):1-9. doi: 10.1111/j.1600-0447.2009.01373.x [DOI] [PubMed] [Google Scholar]
- 18.Ospina MB, Mrklas K, Deuchar L, et al. A systematic review of the effectiveness of discharge care bundles for patients with COPD. Thorax. 2017;72(1):31-39. doi: 10.1136/thoraxjnl-2016-208820 [DOI] [PubMed] [Google Scholar]
- 19.Gonçalves-Bradley DC, Lannin NA, Clemson LM, Cameron ID, Shepperd S. Discharge planning from hospital. Cochrane Database Syst Rev. 2016;2016(1):CD000313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Coffey A, Leahy-Warren P, Savage E, et al. Interventions to promote early discharge and avoid inappropriate hospital (re)admission: a systematic review. Int J Environ Res Public Health. 2019;16(14):2457. doi: 10.3390/ijerph16142457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li T, Puhan MA, Vedula SS, Singh S, Dickersin K; Ad Hoc Network Meta-analysis Methods Meeting Working Group . Network meta-analysis-highly attractive but more methodological research is needed. BMC Med. 2011;9:79. doi: 10.1186/1741-7015-9-79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777-784. doi: 10.7326/M14-2385 [DOI] [PubMed] [Google Scholar]
- 23.Vigod SN, Kurdyak PA, Dennis CL, et al. Transitional interventions to reduce early psychiatric readmissions in adults: systematic review. Br J Psychiatry. 2013;202(3):187-194. doi: 10.1192/bjp.bp.112.115030 [DOI] [PubMed] [Google Scholar]
- 24.Feltner C, Jones CD, Cené CW, et al. Transitional care interventions to prevent readmissions for persons with heart failure: a systematic review and meta-analysis. Ann Intern Med. 2014;160(11):774-784. doi: 10.7326/M14-0083 [DOI] [PubMed] [Google Scholar]
- 25.Rennke S, Nguyen OK, Shoeb MH, Magan Y, Wachter RM, Ranji SR. Hospital-initiated transitional care interventions as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158(5 Pt 2):433-440. doi: 10.7326/0003-4819-158-5-201303051-00011 [DOI] [PubMed] [Google Scholar]
- 26.Laugaland K, Aase K, Barach P. Interventions to improve patient safety in transitional care—a review of the evidence. Work. 2012;41(suppl 1):2915-2924. doi: 10.3233/WOR-2012-0544-2915 [DOI] [PubMed] [Google Scholar]
- 27.Rennke S, Ranji SR. Transitional care strategies from hospital to home: a review for the neurohospitalist. Neurohospitalist. 2015;5(1):35-42. doi: 10.1177/1941874414540683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liebzeit D, Rutkowski R, Arbaje AI, Fields B, Werner NE. A scoping review of interventions for older adults transitioning from hospital to home. J Am Geriatr Soc. 2021;69(10):2950-2962. doi: 10.1111/jgs.17323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Arendts G, Bullow K, Etherton-Beer C, et al. A randomized-controlled trial of a patient-centred intervention in high-risk discharged older patients. Eur J Emerg Med. 2018;25(4):237-241. doi: 10.1097/MEJ.0000000000000444 [DOI] [PubMed] [Google Scholar]
- 30.Auger KA, Simmons JM, Tubbs-Cooley HL, et al. ; H2O Trial study group . Postdischarge nurse home visits and reuse: the Hospital to Home Outcomes (H2O) trial. Pediatrics. 2018;142(1):e20173919. doi: 10.1542/peds.2017-3919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Balaban RB, Weissman JS, Samuel PA, Woolhandler S. Redefining and redesigning hospital discharge to enhance patient care: a randomized controlled study. J Gen Intern Med. 2008;23(8):1228-1233. doi: 10.1007/s11606-008-0618-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barfar E, Sharifi V, Amini H, et al. Cost-effectiveness analysis of an aftercare service vs treatment-as-usual for patients with severe mental disorders. J Ment Health Policy Econ. 2017;20(3):101-110. [PubMed] [Google Scholar]
- 33.Barker RE, Jones SE, Banya W, et al. The effects of a video intervention on posthospitalization pulmonary rehabilitation uptake. a randomized controlled trial. Am J Respir Crit Care Med. 2020;201(12):1517-1524. doi: 10.1164/rccm.201909-1878OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bell SP, Schnipper JL, Goggins K, et al. ; Pharmacist Intervention for Low Literacy in Cardiovascular Disease (PILL-CVD) Study Group . Effect of pharmacist counseling intervention on health care utilization following hospital discharge: a randomized control trial. J Gen Intern Med. 2016;31(5):470-477. doi: 10.1007/s11606-016-3596-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Biese KJ, Busby-Whitehead J, Cai J, et al. Telephone follow-up for older adults discharged to home from the emergency department: a pragmatic randomized controlled trial. J Am Geriatr Soc. 2018;66(3):452-458. doi: 10.1111/jgs.15142 [DOI] [PubMed] [Google Scholar]
- 36.Bloodworth LS, Malinowski SS, Lirette ST, Ross LA. Pharmacist linkage in care transitions: from academic medical center to community. J Am Pharm Assoc (2003). 2019;59(6):896-904. doi: 10.1016/j.japh.2019.08.011 [DOI] [PubMed] [Google Scholar]
- 37.Bloom SL, Stollings JL, Kirkpatrick O, et al. Randomized clinical trial of an ICU recovery pilot program for survivors of critical illness. Crit Care Med. 2019;47(10):1337-1345. doi: 10.1097/CCM.0000000000003909 [DOI] [PubMed] [Google Scholar]
- 38.Blum K, Gottlieb SS. The effect of a randomized trial of home telemonitoring on medical costs, 30-day readmissions, mortality, and health-related quality of life in a cohort of community-dwelling heart failure patients. J Card Fail. 2014;20(7):513-521. doi: 10.1016/j.cardfail.2014.04.016 [DOI] [PubMed] [Google Scholar]
- 39.Bonetti AF, Bagatim BQ, Mendes AM, et al. Impact of discharge medication counseling in the cardiology unit of a tertiary hospital in Brazil: a randomized controlled trial. Clinics (Sao Paulo). 2018;73:e325. doi: 10.6061/clinics/2018/e325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bonnet-Zamponi D, d’Arailh L, Konrat C, et al. ; Optimization of Medication in AGEd study group . Drug-related readmissions to medical units of older adults discharged from acute geriatric units: results of the Optimization of Medication in Aged multicenter randomized controlled trial. J Am Geriatr Soc. 2013;61(1):113-121. doi: 10.1111/jgs.12037 [DOI] [PubMed] [Google Scholar]
- 41.Bonsack C, Golay P, Gibellini Manetti S, et al. Linking primary and secondary care after psychiatric hospitalization: comparison between transitional case management setting and routine care for common mental disorders. Front Psychiatry. 2016;7:96. doi: 10.3389/fpsyt.2016.00096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bradburn M, Goodacre SW, Fitzgerald P, et al. ; RATPAC Research Team . Interhospital variation in the RATPAC trial (Randomised Assessment of Treatment Using Panel Assay of Cardiac Markers). Emerg Med J. 2012;29(3):233-238. doi: 10.1136/emj.2010.108522 [DOI] [PubMed] [Google Scholar]
- 43.Brühwiler LD, Beeler PE, Böni F, et al. A RCT evaluating a pragmatic in-hospital service to increase the quality of discharge prescriptions. Int J Qual Health Care. 2019;31(8):G74-G80. doi: 10.1093/intqhc/mzz043 [DOI] [PubMed] [Google Scholar]
- 44.Chen C, Li X, Sun L, et al. Post-discharge short message service improves short-term clinical outcome and self-care behaviour in chronic heart failure. ESC Heart Fail. 2019;6(1):164-173. doi: 10.1002/ehf2.12380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chen L, Chen Y, Chen X, Shen X, Wang Q, Sun C. Longitudinal study of effectiveness of a patient-centered self-management empowerment intervention during predischarge planning on stroke survivors. Worldviews Evid Based Nurs. 2018;15(3):197-205. doi: 10.1111/wvn.12295 [DOI] [PubMed] [Google Scholar]
- 46.Dalal AK, Schaffer A, Gershanik EF, et al. The impact of automated notification on follow-up of actionable tests pending at discharge: a cluster-randomized controlled trial. J Gen Intern Med. 2018;33(7):1043-1051. doi: 10.1007/s11606-018-4393-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dawson NL, Hull BP, Vijapura P, et al. Home telemonitoring to reduce readmission of high-risk patients: a modified intention-to-treat randomized clinical trial. J Gen Intern Med. 2021;36(11):3395-3401. doi: 10.1007/s11606-020-06589-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dhalla IA, O’Brien T, Morra D, et al. Effect of a postdischarge virtual ward on readmission or death for high-risk patients: a randomized clinical trial. JAMA. 2014;312(13):1305-1312. doi: 10.1001/jama.2014.11492 [DOI] [PubMed] [Google Scholar]
- 49.Edey R, Edwards N, Von Sychowski J, Bains A, Spence J, Martinusen D. Impact of deprescribing rounds on discharge prescriptions: an interventional trial. Int J Clin Pharm. 2019;41(1):159-166. doi: 10.1007/s11096-018-0753-2 [DOI] [PubMed] [Google Scholar]
- 50.Englander H, Michaels L, Chan B, Kansagara D. The care transitions innovation (C-TRAIN) for socioeconomically disadvantaged adults: results of a cluster randomized controlled trial. J Gen Intern Med. 2014;29(11):1460-1467. doi: 10.1007/s11606-014-2903-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Evans RL, Hendricks RD. Evaluating hospital discharge planning: a randomized clinical trial. Med Care. 1993;31(4):358-370. doi: 10.1097/00005650-199304000-00007 [DOI] [PubMed] [Google Scholar]
- 52.Farris KB, Carter BL, Xu Y, et al. Effect of a care transition intervention by pharmacists: an RCT. BMC Health Serv Res. 2014;14:406. doi: 10.1186/1472-6963-14-406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Finlayson K, Chang AM, Courtney MD, et al. Transitional care interventions reduce unplanned hospital readmissions in high-risk older adults. BMC Health Serv Res. 2018;18(1):956. doi: 10.1186/s12913-018-3771-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gardner RL, Pelland K, Youssef R, et al. Reducing hospital readmissions through a skilled nursing facility discharge intervention: a pragmatic trial. J Am Med Dir Assoc. 2020;21(4):508-512. doi: 10.1016/j.jamda.2019.10.001 [DOI] [PubMed] [Google Scholar]
- 55.Ghadiri Vasfi M, Moradi-Lakeh M, Esmaeili N, Soleimani N, Hajebi A. Efficacy of aftercare services for people with severe mental disorders in Iran: a randomized controlled trial. Psychiatr Serv. 2015;66(4):373-380. doi: 10.1176/appi.ps.201400111 [DOI] [PubMed] [Google Scholar]
- 56.Gilbert T, Occelli P, Rabilloud M, et al. ; PROUST Study Group . A nurse-led bridging program to reduce 30-day readmissions of older patients discharged from acute care units. J Am Med Dir Assoc. 2021;22(6):1292-1299.e5. doi: 10.1016/j.jamda.2020.09.015 [DOI] [PubMed] [Google Scholar]
- 57.Gillespie U, Alassaad A, Henrohn D, et al. A comprehensive pharmacist intervention to reduce morbidity in patients 80 years or older: a randomized controlled trial. Arch Intern Med. 2009;169(9):894-900. doi: 10.1001/archinternmed.2009.71 [DOI] [PubMed] [Google Scholar]
- 58.Goldman LE, Sarkar U, Kessell E, et al. Support from hospital to home for elders: a randomized trial. Ann Intern Med. 2014;161(7):472-481. doi: 10.7326/M14-0094 [DOI] [PubMed] [Google Scholar]
- 59.Gurwitz JH, Field TS, Ogarek J, et al. An electronic health record-based intervention to increase follow-up office visits and decrease rehospitalization in older adults. J Am Geriatr Soc. 2014;62(5):865-871. doi: 10.1111/jgs.12798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hanrahan NP, Solomon P, Hurford MO. A pilot randomized control trial: testing a transitional care model for acute psychiatric conditions. J Am Psychiatr Nurses Assoc. 2014;20(5):315-327. doi: 10.1177/1078390314552190 [DOI] [PubMed] [Google Scholar]
- 61.Harrison MB, Browne GB, Roberts J, Tugwell P, Gafni A, Graham ID. Quality of life of individuals with heart failure: a randomized trial of the effectiveness of two models of hospital-to-home transition. Med Care. 2002;40(4):271-282. doi: 10.1097/00005650-200204000-00003 [DOI] [PubMed] [Google Scholar]
- 62.Harvey P, Storer M, Berlowitz DJ, Jackson B, Hutchinson A, Lim WK. Feasibility and impact of a post-discharge geriatric evaluation and management service for patients from residential care: the Residential Care Intervention Program in the Elderly (RECIPE). BMC Geriatr. 2014;14:48. doi: 10.1186/1471-2318-14-48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Heaton PC, Frede S, Kordahi A, et al. Improving care transitions through medication therapy management: a community partnership to reduce readmissions in multiple health-systems. J Am Pharm Assoc (2003). 2019;59(3):319-328. doi: 10.1016/j.japh.2019.01.005 [DOI] [PubMed] [Google Scholar]
- 64.Hegelund A, Andersen IC, Andersen MN, Bodtger U. The impact of a personalised action plan delivered at discharge to patients with COPD on readmissions: a pilot study. Scand J Caring Sci. 2020;34(4):909-918. doi: 10.1111/scs.12798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hengartner MP, Passalacqua S, Heim G, Andreae A, Rössler W, von Wyl A. The Post-Discharge Network Coordination Programme: a randomized controlled trial to evaluate the efficacy of an intervention aimed at reducing rehospitalizations and improving mental health. Front Psychiatry. 2016;7:27. doi: 10.3389/fpsyt.2016.00027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sarboozi Hosein َAbadi T, Namazi Nia M, Mazlom SR. Effect of self-determination theory-based discharge program on lifestyle and readmission of patients with heart failure: a clinical trial. Evidence Based Care. 2020;10(1):25-35. doi: 10.22038/ebcj.2020.46225.2264 [DOI] [Google Scholar]
- 67.Hu R, Gu B, Tan Q, et al. The effects of a transitional care program on discharge readiness, transitional care quality, health services utilization and satisfaction among Chinese kidney transplant recipients: a randomized controlled trial. Int J Nurs Stud. 2020;110:103700. doi: 10.1016/j.ijnurstu.2020.103700 [DOI] [PubMed] [Google Scholar]
- 68.Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178-187. doi: 10.7326/0003-4819-150-3-200902030-00007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Jennings JH, Thavarajah K, Mendez MP, Eichenhorn M, Kvale P, Yessayan L. Predischarge bundle for patients with acute exacerbations of COPD to reduce readmissions and ED visits: a randomized controlled trial. Chest. 2015;147(5):1227-1234. doi: 10.1378/chest.14-1123 [DOI] [PubMed] [Google Scholar]
- 70.Karaoui LR, Ramia E, Mansour H, Haddad N, Chamoun N. Impact of pharmacist-conducted anticoagulation patient education and telephone follow-up on transitions of care: a randomized controlled trial. BMC Health Serv Res. 2021;21(1):151. doi: 10.1186/s12913-021-06156-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kennedy L, Neidlinger S, Scroggins K. Effective comprehensive discharge planning for hospitalized elderly. Gerontologist. 1987;27(5):577-580. doi: 10.1093/geront/27.5.577 [DOI] [PubMed] [Google Scholar]
- 72.Ko FW, Cheung NK, Rainer TH, Lum C, Wong I, Hui DS. Comprehensive care programme for patients with chronic obstructive pulmonary disease: a randomised controlled trial. Thorax. 2017;72(2):122-128. doi: 10.1136/thoraxjnl-2016-208396 [DOI] [PubMed] [Google Scholar]
- 73.Kripalani S, Roumie CL, Dalal AK, et al. ; PILL-CVD (Pharmacist Intervention for Low Literacy in Cardiovascular Disease) Study Group . Effect of a pharmacist intervention on clinically important medication errors after hospital discharge: a randomized trial. Ann Intern Med. 2012;157(1):1-10. doi: 10.7326/0003-4819-157-1-201207030-00003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Laramee AS, Levinsky SK, Sargent J, Ross R, Callas P. Case management in a heterogeneous congestive heart failure population: a randomized controlled trial. Arch Intern Med. 2003;163(7):809-817. doi: 10.1001/archinte.163.7.809 [DOI] [PubMed] [Google Scholar]
- 75.Latour CH, de Vos R, Huyse FJ, de Jonge P, van Gemert LA, Stalman WA. Effectiveness of post-discharge case management in general-medical outpatients: a randomized, controlled trial. Psychosomatics. 2006;47(5):421-429. doi: 10.1176/appi.psy.47.5.421 [DOI] [PubMed] [Google Scholar]
- 76.Lavesen M, Ladelund S, Frederiksen AJ, Lindhardt BØ, Overgaard D. Nurse-initiated telephone follow-up on patients with chronic obstructive pulmonary disease improves patient empowerment, but cannot prevent readmissions. Dan Med J. 2016;63(10):A5276. [PubMed] [Google Scholar]
- 77.Lea M, Mowé M, Molden E, Kvernrød K, Skovlund E, Mathiesen L. Effect of medicines management versus standard care on readmissions in multimorbid patients: a randomised controlled trial. BMJ Open. 2020;10(12):e041558. doi: 10.1136/bmjopen-2020-041558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Legrain S, Tubach F, Bonnet-Zamponi D, et al. A new multimodal geriatric discharge-planning intervention to prevent emergency visits and rehospitalizations of older adults: the optimization of medication in AGED multicenter randomized controlled trial. J Am Geriatr Soc. 2011;59(11):2017-2028. doi: 10.1111/j.1532-5415.2011.03628.x [DOI] [PubMed] [Google Scholar]
- 79.Lembeck MA, Thygesen LC, Sørensen BD, Rasmussen LL, Holm EA. Effect of single follow-up home visit on readmission in a group of frail elderly patients—a Danish randomized clinical trial. BMC Health Serv Res. 2019;19(1):751. doi: 10.1186/s12913-019-4528-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Levine DM, Ouchi K, Blanchfield B, et al. Hospital-level care at home for acutely ill adults: a pilot randomized controlled trial. J Gen Intern Med. 2018;33(5):729-736. doi: 10.1007/s11606-018-4307-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Li J, Wang H, Xie H, et al. Effects of post-discharge nurse-led telephone supportive care for patients with chronic kidney disease undergoing peritoneal dialysis in China: a randomized controlled trial. Perit Dial Int. 2014;34(3):278-288. doi: 10.3747/pdi.2012.00268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lin R, Gallagher R, Spinaze M, et al. Effect of a patient-directed discharge letter on patient understanding of their hospitalisation. Intern Med J. 2014;44(9):851-857. doi: 10.1111/imj.12482 [DOI] [PubMed] [Google Scholar]
- 83.Lindhardt T, Loevgreen SM, Bang B, Bigum C, Klausen TW. A targeted assessment and intervention at the time of discharge reduced the risk of readmissions for short-term hospitalized older patients: a randomized controlled study. Clin Rehabil. 2019;33(9):1431-1444. doi: 10.1177/0269215519845032 [DOI] [PubMed] [Google Scholar]
- 84.Liu ZC, Gao L, Zhang WH, Wang J, Liu RR, Cao BH. Effects of a 4-week Omaha System transitional care programme on rheumatoid arthritis patients’ self-efficacy, health status, and readmission in mainland China: a randomized controlled trial. Int J Nurs Pract. 2020;26(4):e12817. doi: 10.1111/ijn.12817 [DOI] [PubMed] [Google Scholar]
- 85.Lockwood KJ, Harding KE, Boyd JN, Taylor NF. Predischarge home visits after hip fracture: a randomized controlled trial. Clin Rehabil. 2019;33(4):681-692. doi: 10.1177/0269215518823256 [DOI] [PubMed] [Google Scholar]
- 86.Magny-Normilus C, Nolido NV, Borges JC, et al. Effects of an intensive discharge intervention on medication adherence, glycemic control, and readmission rates in patients with type 2 diabetes. J Patient Saf. 2021;17(2):73-80. doi: 10.1097/PTS.0000000000000601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.McWilliams A, Roberge J, Anderson WE, et al. Aiming to Improve Readmissions Through Integrated Hospital Transitions (AIRTIGHT): a pragmatic randomized controlled trial. J Gen Intern Med. 2019;34(1):58-64. doi: 10.1007/s11606-018-4617-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mehta SJ, Hume E, Troxel AB, et al. Effect of remote monitoring on discharge to home, return to activity, and rehospitalization after hip and knee arthroplasty: a randomized clinical trial. JAMA Netw Open. 2020;3(12):e2028328. doi: 10.1001/jamanetworkopen.2020.28328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Moher D, Weinberg A, Hanlon R, Runnalls K. Effects of a medical team coordinator on length of hospital stay. CMAJ. 1992;146(4):511-515. [PMC free article] [PubMed] [Google Scholar]
- 90.Naylor M, Brooten D, Jones R, Lavizzo-Mourey R, Mezey M, Pauly M. Comprehensive discharge planning for the hospitalized elderly: a randomized clinical trial. Ann Intern Med. 1994;120(12):999-1006. doi: 10.7326/0003-4819-120-12-199406150-00005 [DOI] [PubMed] [Google Scholar]
- 91.Nazareth I, Burton A, Shulman S, Smith P, Haines A, Timberal H. A pharmacy discharge plan for hospitalized elderly patients—a randomized controlled trial. Age Ageing. 2001;30(1):33-40. doi: 10.1093/ageing/30.1.33 [DOI] [PubMed] [Google Scholar]
- 92.Negarandeh R, Zolfaghari M, Bashi N, Kiarsi M. Evaluating the effect of monitoring through telephone (tele-monitoring) on self-care behaviors and readmission of patients with heart failure after discharge. Appl Clin Inform. 2019;10(2):261-268. doi: 10.1055/s-0039-1685167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Nguyen T, Nguyen TH, Nguyen PT, et al. Pharmacist-led intervention to enhance medication adherence in patients with acute coronary syndrome in Vietnam: a randomized controlled trial. Front Pharmacol. 2018;9:656. doi: 10.3389/fphar.2018.00656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Noel K, Messina C, Hou W, Schoenfeld E, Kelly G. Tele-transitions of care (TTOC): a 12-month, randomized controlled trial evaluating the use of telehealth to achieve triple aim objectives. BMC Fam Pract. 2020;21(1):27. doi: 10.1186/s12875-020-1094-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.O’Connell MJ, Sledge WH, Staeheli M, et al. Outcomes of a peer mentor intervention for persons with recurrent psychiatric hospitalization. Psychiatr Serv. 2018;69(7):760-767. doi: 10.1176/appi.ps.201600478 [DOI] [PubMed] [Google Scholar]
- 96.Odeh M, Scullin C, Hogg A, Fleming G, Scott MG, McElnay JC. A novel approach to medicines optimisation post-discharge from hospital: pharmacist-led medicines optimisation clinic. Int J Clin Pharm. 2020;42(4):1036-1049. doi: 10.1007/s11096-020-01059-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ong MK, Romano PS, Edgington S, et al. ; Better Effectiveness After Transition–Heart Failure (BEAT-HF) Research Group . Effectiveness of remote patient monitoring after discharge of hospitalized patients with heart failure: the Better Effectiveness After Transition—Heart Failure (BEAT-HF) randomized clinical trial. JAMA Intern Med. 2016;176(3):310-318. doi: 10.1001/jamainternmed.2015.7712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Oscalices MIL, Okuno MFP, Lopes MCBT, Campanharo CRV, Batista REA. Discharge guidance and telephone follow-up in the therapeutic adherence of heart failure: randomized clinical trial. Rev Lat Am Enfermagem. 2019;27:e3159. doi: 10.1590/1518-8345.2484.3159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ougrin D, Corrigall R, Stahl D, et al. Supported discharge service versus inpatient care evaluation (SITE): a randomised controlled trial comparing effectiveness of an intensive community care service versus inpatient treatment as usual for adolescents with severe psychiatric disorders: self-harm, functional impairment, and educational and clinical outcomes. Eur Child Adolesc Psychiatry. 2021;30(9):1427-1436. doi: 10.1007/s00787-020-01617-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Pardessus V, Puisieux F, Di Pompeo C, Gaudefroy C, Thevenon A, Dewailly P. Benefits of home visits for falls and autonomy in the elderly: a randomized trial study. Am J Phys Med Rehabil. 2002;81(4):247-252. doi: 10.1097/00002060-200204000-00002 [DOI] [PubMed] [Google Scholar]
- 101.Parsons M, Parsons J, Pillai A, et al. Post-acute care for older people following injury: a randomized controlled trial. J Am Med Dir Assoc. 2020;21(3):404-409.e1. doi: 10.1016/j.jamda.2019.08.015 [DOI] [PubMed] [Google Scholar]
- 102.Phatak A, Prusi R, Ward B, et al. Impact of pharmacist involvement in the transitional care of high-risk patients through medication reconciliation, medication education, and postdischarge call-backs (IPITCH Study). J Hosp Med. 2016;11(1):39-44. doi: 10.1002/jhm.2493 [DOI] [PubMed] [Google Scholar]
- 103.Piette JD, Striplin D, Aikens JE, et al. Impacts of Post-hospitalization accessible health technology and caregiver support on 90-day acute care use and self-care assistance: a randomized clinical trial. Am J Med Qual. 2021;36(3):145-155. doi: 10.1177/1062860620943673 [DOI] [PubMed] [Google Scholar]
- 104.Pourrat X, Leyrat C, Allenet B, et al. Effectiveness of a multicomponent pharmacist intervention at hospital discharge for drug-related problems: a cluster randomised cross-over trial. Br J Clin Pharmacol. 2020;86(12):2441-2454. doi: 10.1111/bcp.14349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Qian C, Zhong D, Shen Y, Du Q, Du Q. Evaluation of clinical efficacy of transitional care mode for patients with strokes. Int J Clin Exp Med. 2019;12(1):981-988. [Google Scholar]
- 106.Ravn-Nielsen LV, Duckert ML, Lund ML, et al. Effect of an in-hospital multifaceted clinical pharmacist intervention on the risk of readmission: a randomized clinical trial. JAMA Intern Med. 2018;178(3):375-382. doi: 10.1001/jamainternmed.2017.8274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Reynolds W, Lauder W, Sharkey S, Maciver S, Veitch T, Cameron D. The effects of a transitional discharge model for psychiatric patients. J Psychiatr Ment Health Nurs. 2004;11(1):82-88. doi: 10.1111/j.1365-2850.2004.00692.x [DOI] [PubMed] [Google Scholar]
- 108.Rice KL, Dewan N, Bloomfield HE, et al. Disease management program for chronic obstructive pulmonary disease: a randomized controlled trial. Am J Respir Crit Care Med. 2010;182(7):890-896. doi: 10.1164/rccm.200910-1579OC [DOI] [PubMed] [Google Scholar]
- 109.Rich MW, Vinson JM, Sperry JC, et al. Prevention of readmission in elderly patients with congestive heart failure: results of a prospective, randomized pilot study. J Gen Intern Med. 1993;8(11):585-590. doi: 10.1007/BF02599709 [DOI] [PubMed] [Google Scholar]
- 110.Rich MW, Beckham V, Wittenberg C, Leven CL, Freedland KE, Carney RM. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. N Engl J Med. 1995;333(18):1190-1195. doi: 10.1056/NEJM199511023331806 [DOI] [PubMed] [Google Scholar]
- 111.Ritchie CS, Houston TK, Richman JS, et al. The e-Coach technology-assisted care transition system: a pragmatic randomized trial. Transl Behav Med. 2016;6(3):428-437. doi: 10.1007/s13142-016-0422-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Sahota O, Pulikottil-Jacob R, Marshall F, et al. The Community In-Reach Rehabilitation and Care Transition (CIRACT) clinical and cost-effectiveness randomisation controlled trial in older people admitted to hospital as an acute medical emergency. Age Ageing. 2017;46(1):26-32. doi: 10.1093/ageing/afw149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Salameh LK, Abu Farha RK, Abu Hammour KM, Basheti IA. Impact of pharmacist’s directed medication reconciliation on reducing medication discrepancies during transition of care in hospital setting. J Pharm Health Serv Res. 2019;10(1):149-156. doi: 10.1111/jphs.12261 [DOI] [Google Scholar]
- 114.Sales VL, Ashraf MS, Lella LK, et al. Utilization of trained volunteers decreases 30-day readmissions for heart failure. J Card Fail. 2013;19(12):842-850. doi: 10.1016/j.cardfail.2013.10.008 [DOI] [PubMed] [Google Scholar]
- 115.Salmany SS, Ratrout L, Amireh A, et al. The impact of pharmacist telephone calls after discharge on satisfaction of oncology patients: a randomized controlled study. J Oncol Pharm Pract. 2018;24(5):359-364. doi: 10.1177/1078155217709616 [DOI] [PubMed] [Google Scholar]
- 116.Santana MJ, Holroyd-Leduc J, Southern DA, et al. ; e-DCT Team . A randomised controlled trial assessing the efficacy of an electronic discharge communication tool for preventing death or hospital readmission. BMJ Qual Saf. 2017;26(12):993-1003. doi: 10.1136/bmjqs-2017-006635 [DOI] [PubMed] [Google Scholar]
- 117.Shahrokhi A, Azimian J, Amouzegar A, Oveisi S. Effect of telenursing on outcomes of provided care by caregivers of patients with head trauma after discharge. J Trauma Nurs. 2018;25(1):21-25. doi: 10.1097/JTN.0000000000000338 [DOI] [PubMed] [Google Scholar]
- 118.Shaw H, Mackie CA, Sharkie I. Evaluation of effect of pharmacy discharge planning on medication problems experienced by discharged acute admission mental health patients. Int J Pharm Pract. 2000;8(2):144-153. doi: 10.1111/j.2042-7174.2000.tb00999.x [DOI] [Google Scholar]
- 119.Strano A, Briggs A, Powell N, et al. Home healthcare visits following hospital discharge: does the timing of visits affect 30-day hospital readmission rates for heart failure patients? Home Healthc Now. 2019;37(3):152-157. doi: 10.1097/NHH.0000000000000740 [DOI] [PubMed] [Google Scholar]
- 120.Sudas Na Ayutthaya N, Sakunrak I, Dhippayom T. Clinical outcomes of telemonitoring for patients on warfarin after discharge from hospital. Int J Telemed Appl. 2018;2018:7503421. doi: 10.1155/2018/7503421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Thygesen LC, Fokdal S, Gjørup T, Taylor RS, Zwisler AD; Prevention of Early Readmission Research Group . Can municipality-based post-discharge follow-up visits including a general practitioner reduce early readmission among the fragile elderly (65+ years old): a randomized controlled trial. Scand J Prim Health Care. 2015;33(2):65-73. doi: 10.3109/02813432.2015.1041831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Tomita A, Herman DB. The impact of critical time intervention in reducing psychiatric rehospitalization after hospital discharge. Psychiatr Serv. 2012;63(9):935-937. doi: 10.1176/appi.ps.201100468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Utens CM, Goossens LM, Smeenk FW, et al. Early assisted discharge with generic community nursing for chronic obstructive pulmonary disease exacerbations: results of a randomised controlled trial. BMJ Open. 2012;2(5):e001684. doi: 10.1136/bmjopen-2012-001684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.van der Heijden AAWA, de Bruijne MC, Nijpels G, Hugtenburg JG. Cost-effectiveness of a clinical medication review in vulnerable older patients at hospital discharge, a randomized controlled trial. Int J Clin Pharm. 2019;41(4):963-971. doi: 10.1007/s11096-019-00825-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Van Spall HGC, Lee SF, Xie F, et al. Effect of patient-centered transitional care services on clinical outcomes in patients hospitalized for heart failure: the PACT-HF randomized clinical trial. JAMA. 2019;321(8):753-761. doi: 10.1001/jama.2019.0710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Vesterby MS, Pedersen PU, Laursen M, et al. Telemedicine support shortens length of stay after fast-track hip replacement. Acta Orthop. 2017;88(1):41-47. doi: 10.1080/17453674.2016.1256939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Vinluan CM, Wittman D, Morisky D. Effect of pharmacist discharge counselling on medication adherence in elderly heart failure patients: a pilot study. J Pharm Health Serv Res. 2015;6(2):103-110. doi: 10.1111/jphs.12093 [DOI] [Google Scholar]
- 128.Webster J, Connolly A, Paton F, Corry J. The effectiveness of protocol drive, nurse-initiated discharge in a 23-h post surgical ward: a randomized controlled trial. Int J Nurs Stud. 2011;48(10):1173-1179. doi: 10.1016/j.ijnurstu.2011.02.022 [DOI] [PubMed] [Google Scholar]
- 129.Weiss ME, Yakusheva O, Bobay KL, et al. ; READI Site Investigators . Effect of implementing discharge readiness assessment in adult medical-surgical units on 30-day return to hospital: the READI randomized clinical trial. JAMA Netw Open. 2019;2(1):e187387. doi: 10.1001/jamanetworkopen.2018.7387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Wong FK, Mok MP, Chan T, Tsang MW. Nurse follow-up of patients with diabetes: randomized controlled trial. J Adv Nurs. 2005;50(4):391-402. doi: 10.1111/j.1365-2648.2005.03404.x [DOI] [PubMed] [Google Scholar]
- 131.Wong FK, Chow SK, Chan TM, Tam SK. Comparison of effects between home visits with telephone calls and telephone calls only for transitional discharge support: a randomised controlled trial. Age Ageing. 2014;43(1):91-97. doi: 10.1093/ageing/aft123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Wong FK, Yeung SM. Effects of a 4-week transitional care programme for discharged stroke survivors in Hong Kong: a randomised controlled trial. Health Soc Care Community. 2015;23(6):619-631. doi: 10.1111/hsc.12177 [DOI] [PubMed] [Google Scholar]
- 133.Wong FK, Ng AY, Lee PH, et al. Effects of a transitional palliative care model on patients with end-stage heart failure: a randomised controlled trial. Heart. 2016;102(14):1100-1108. doi: 10.1136/heartjnl-2015-308638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Wu Q, Zhang D, Zhao Q, et al. Effects of transitional health management on adherence and prognosis in elderly patients with acute myocardial infarction in percutaneous coronary intervention: a cluster randomized controlled trial. PLoS One. 2019;14(5):e0217535. doi: 10.1371/journal.pone.0217535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Xie X, Song Y, Yang H, Nie A, Chen H, Li JP. Effects of transitional care on self-care, readmission rates, and quality of life in adult patients with systemic lupus erythematosus: a randomized controlled trial. Arthritis Res Ther. 2018;20(1):184. doi: 10.1186/s13075-018-1670-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Xu H, Zou J, Ye X, et al. Impacts of clinical pharmacist intervention on the secondary prevention of coronary heart disease: a randomized controlled clinical study. Front Pharmacol. 2019;10:1112. doi: 10.3389/fphar.2019.01112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Yiadom MYAB, Domenico HJ, Byrne DW, et al. Impact of a follow-up telephone call program on 30-day readmissions (FUTR-30): a pragmatic randomized controlled real-world effectiveness trial. Med Care. 2020;58(9):785-792. doi: 10.1097/MLR.0000000000001353 [DOI] [PubMed] [Google Scholar]
- 138.Yin D, Guo Q, Geng X, et al. The effect of inpatient pharmaceutical care on nephrotic syndrome patients after discharge: a randomized controlled trial. Int J Clin Pharm. 2020;42(2):617-624. doi: 10.1007/s11096-020-00975-9 [DOI] [PubMed] [Google Scholar]
- 139.You J, Wang S, Li J, Luo Y. Usefulness of a nurse-led program of care for management of patients with chronic heart failure. Med Sci Monit. 2020;26:e920469. doi: 10.12659/MSM.920469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Zhang P, Xing FM, Li CZ, Wang FL, Zhang XL. Effects of a nurse-led transitional care programme on readmission, self-efficacy to implement health-promoting behaviours, functional status and life quality among Chinese patients with coronary artery disease: a randomised controlled trial. J Clin Nurs. 2018;27(5-6):969-979. doi: 10.1111/jocn.14064 [DOI] [PubMed] [Google Scholar]
- 141.Indraratna P, Biswas U, McVeigh J, et al. A Smartphone-based model of care to support patients with cardiac disease transitioning from hospital to the community (Teleclinical Care): pilot randomized controlled trial. JMIR Mhealth Uhealth. 2022;10(2):e32554. doi: 10.2196/32554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Kowalkowski MA, Rios A, McSweeney J, et al. Effect of a transitional care intervention on rehospitalization and mortality after sepsis: a 12-month follow-up of a randomized clinical trial. Am J Respir Crit Care Med. 2022;206(6):783-786. doi: 10.1164/rccm.202203-0590LE [DOI] [PubMed] [Google Scholar]
- 143.Jayaram L, Gillman A, Casanelia S, et al. A nurse-led asthma care team transitioning patients from hospital to home improves asthma control: a pilot study exploring an alternative model of care. Health Promot J Austr. 2023;34(2):429-436. doi: 10.1002/hpja.620 [DOI] [PubMed] [Google Scholar]
- 144.DeVore AD, Granger BB, Fonarow GC, et al. Effect of a hospital and postdischarge quality improvement intervention on clinical outcomes and quality of care for patients with heart failure with reduced ejection fraction: the CONNECT-HF randomized clinical trial. JAMA. 2021;326(4):314-323. doi: 10.1001/jama.2021.8844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Coskun S, Duygulu S. The effects of nurse led transitional care model on elderly patients undergoing open heart surgery: a randomized controlled trial. Eur J Cardiovasc Nurs. 2022;21(1):46-55. doi: 10.1093/eurjcn/zvab005 [DOI] [PubMed] [Google Scholar]
- 146.Habib B, Buckeridge D, Bustillo M, et al. Smart About Meds (SAM): a pilot randomized controlled trial of a mobile application to improve medication adherence following hospital discharge. JAMIA Open. 2021;4(3):ooab050. doi: 10.1093/jamiaopen/ooab050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Bawazeer G, Sales I, Alsunaidi A, et al. Student-led discharge counseling program for high-risk medications in a teaching hospital in Saudi Arabia: a pilot study. Saudi Pharm J. 2021;29(10):1129-1136. doi: 10.1016/j.jsps.2021.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Gillard S, Bremner S, Patel A, et al. ; ENRICH trial study group . Peer support for discharge from inpatient mental health care versus care as usual in England (ENRICH): a parallel, two-group, individually randomised controlled trial. Lancet Psychiatry. 2022;9(2):125-136. doi: 10.1016/S2215-0366(21)00398-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Leppin AL, Gionfriddo MR, Kessler M, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174(7):1095-1107. doi: 10.1001/jamainternmed.2014.1608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Joynt KE, Jha AK. Thirty-day readmissions–truth and consequences. N Engl J Med. 2012;366(15):1366-1369. doi: 10.1056/NEJMp1201598 [DOI] [PubMed] [Google Scholar]
- 151.Bee P, Gibbons C, Callaghan P, Fraser C, Lovell K. Evaluating and Quantifying User and Carer Involvement in Mental Health Care Planning (EQUIP): co-development of a new patient-reported outcome measure. PLoS One. 2016;11(3):e0149973. doi: 10.1371/journal.pone.0149973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Tyler N, Wright N, Grundy A, Waring J. Developing a core outcome set for interventions to improve discharge from mental health inpatient services: a survey, Delphi and consensus meeting with key stakeholder groups. BMJ Open. 2020;10(5):e034215. doi: 10.1136/bmjopen-2019-034215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Linkens AEMJH, Milosevic V, van der Kuy PHM, Damen-Hendriks VH, Mestres Gonzalvo C, Hurkens KPGM. Medication-related hospital admissions and readmissions in older patients: an overview of literature. Int J Clin Pharm. 2020;42(5):1243-1251. doi: 10.1007/s11096-020-01040-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Pereira F, Verloo H, Zhivko T, et al. Risk of 30-day hospital readmission associated with medical conditions and drug regimens of polymedicated, older inpatients discharged home: a registry-based cohort study. BMJ Open. 2021;11(7):e052755. doi: 10.1136/bmjopen-2021-052755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Alharbi K, Blakeman T, van Marwijk H, Reeves D, Tsang JY. Understanding the implementation of interventions to improve the management of frailty in primary care: a rapid realist review. BMJ Open. 2022;12(6):e054780. doi: 10.1136/bmjopen-2021-054780 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix 1. Search Criteria
eAppendix 2. League Table of Head-to-Head Comparisons
eAppendix 3. Characteristics of Included Studies
eAppendix 4. Risk of Bias Assessment
eAppendix 5. Inconsistency Analysis
eAppendix 6. Publication Bias and Funnel Plots
eAppendix 7. Meta-Regressions
eAppendix 8. Sensitivity Analysis
eAppendix 9. 90-Day Readmissions and Secondary Outcomes
Data Sharing Statement