Key Points
Question
Do learning programs that share treatment recommendations for genomic alterations, particularly treatments with low evidence levels, contribute to standardization of quality in molecular tumor boards?
Findings
In this quality improvement study of 50 simulated cancer cases, participation in the learning program improved the concordance rate of recommendations by molecular tumor boards and centrally developed the consensus treatment recommendations.
Meaning
These findings suggest that sharing treatment recommendations for genomic alterations with low evidence levels contributes to the improvement of the quality of molecular tumor boards.
This quality improvement study examines the effectiveness of a learning program for molecular tumor boards to share best practices for providing optimal treatment recommendations in 50 identical simulated cases of advanced cancer.
Abstract
Importance
Substantial heterogeneity exists in treatment recommendations across molecular tumor boards (MTBs), especially for biomarkers with low evidence levels; therefore, the learning program is essential.
Objective
To determine whether a learning program sharing treatment recommendations for biomarkers with low evidence levels contributes to the standardization of MTBs and to investigate the efficacy of an artificial intelligence (AI)–based annotation system.
Design, Setting, and Participants
This prospective quality improvement study used 50 simulated cases to assess concordance of treatment recommendations between a central committee and participants. Forty-seven participants applied from April 7 to May 13, 2021. Fifty simulated cases were randomly divided into prelearning and postlearning evaluation groups to assess similar concordance based on previous investigations. Participants included MTBs at hub hospitals, treating physicians at core hospitals, and AI systems. Each participant made treatment recommendations for each prelearning case from registration to June 30, 2021; participated in the learning program on July 18, 2021; and made treatment recommendations for each postlearning case from August 3 to September 30, 2021. Data were analyzed from September 2 to December 10, 2021.
Exposures
The learning program shared the methodology of making appropriate treatment recommendations, especially for biomarkers with low evidence levels.
Main Outcomes and Measures
The primary end point was the proportion of MTBs that met prespecified accreditation criteria for postlearning evaluations (approximately 90% concordance with high evidence levels and approximately 40% with low evidence levels). Key secondary end points were chronological enhancements in the concordance of treatment recommendations on postlearning evaluations from prelearning evaluations. Concordance of treatment recommendations by an AI system was an exploratory end point.
Results
Of the 47 participants who applied, 42 were eligible. The accreditation rate of the MTBs was 55.6% (95% CI, 35.3%-74.5%; P < .001). Concordance in MTBs increased from 58.7% (95% CI, 52.8%-64.4%) to 67.9% (95% CI, 61.0%-74.1%) (odds ratio, 1.40 [95% CI, 1.06-1.86]; P = .02). In postlearning evaluations, the concordance of treatment recommendations by the AI system was significantly higher than that of MTBs (88.0% [95% CI, 68.7%-96.1%]; P = .03).
Conclusions and Relevance
The findings of this quality improvement study suggest that use of a learning program improved the concordance of treatment recommendations provided by MTBs to central ones. Treatment recommendations made by an AI system showed higher concordance than that for MTBs, indicating the potential clinical utility of the AI system.
Introduction
Comprehensive genome profiling (CGP) tests are increasingly being used for precision oncology in patients with advanced cancer. While previous research demonstrated that genomically matched therapies based on the CGP test results enhanced the outcomes of patients with advanced cancer,1,2 other reports showed that the clinical benefit of CGP tests was minimal.3,4,5,6,7 Thus, the clinical utility of CGP testing remains controversial.
As of October 2022, CGP testing in Japan has been covered by the Japanese Public Health Insurance System and reimbursed at 233 government-designated institutions, including 12 core hospitals, 33 hub hospitals, and 188 cooperative hospitals.8 Comprehensive genome profiling test results are required to be reviewed by molecular tumor boards (MTBs) at the 12 core and 33 hub hospitals, and the MTBs then develop specific treatment recommendations for each patient based on the CGP test results.9,10
To develop proper treatment recommendations and assess the necessity for referring patients for genetic counseling based on the results of CGP tests, multidisciplinary MTBs have been implemented globally. However, the process by which MTBs make treatment recommendations has not been well-defined. While some studies have evaluated the differences in treatment recommendations across MTBs,11,12 the sample sizes were small and the factors affecting the discrepancies were not fully investigated. Naito et al13 previously observed that treatment recommendations differed significantly among MTBs, notably in genomic alterations with low evidence levels for which appropriate treatments are still being examined. Because most treatment recommendations for biomarkers with poor evidence levels were investigational new drug (IND) trials, sharing information on IND trials with low evidence levels across MTBs may be useful in improving MTB quality.
As a result, we established a learning program for physicians at core hospitals as well as for MTBs at hub hospitals to share best practices for providing optimal treatment recommendations, concentrating on a treatment recommendation for patients with highly frequent genomic alterations with low evidence levels. We performed this nationwide prospective quality improvement study to examine the effectiveness of the learning program by using 50 identical simulated cases of advanced cancer. Furthermore, an artificial intelligence (AI)–based annotation system may help to guide clinical decision-making more properly in precision oncology14,15; therefore, we simultaneously investigated the efficiency of an AI system in this study.
Methods
Creation of Simulated Cases and Central Treatment Recommendations
The central committee, comprised of MTB representatives from all 12 key institutions, generated 50 simulated cases, as in the previous study.13 Briefly, based on the CONCORD-316 and The Cancer Genome Atlas (TCGA),17 commonly reported cancer types and genomic changes were chosen. Every case included simulated clinical information such as patient characteristics, specimen information, clinical course, and simulated test reports. The central committee assessed all simulated instances to determine whether they were appropriate and realistic13 and then reviewed relevant treatment recommendations for each simulated instance based on the simulated clinical information and test data. Central treatment recommendations were summarized, consisting of genomically matched therapies and information from clinical trials, and updated every 4 months (eTable 1 in Supplement 1). The institutional review board at the National Cancer Center was consulted for the study protocol; however, this research did not include actual patients; as a result, this study did not require institutional review board approval or informed consent. We followed the Standards for Quality Improvement Reporting Excellence (SQUIRE) reporting guideline.
Evidence Levels
As in the previous study,13 evidence levels were established according to the clinical practice guidance for next-generation sequencing in cancer diagnosis and treatment10 (eTable 2 in Supplement 1). Evidence levels A, B, and R, common biomarkers for routine clinical practice, were defined as high, whereas evidence levels C, D, and E were defined as low.
Study Design
The existence or absence of TP53 (OMIM 191170) changes, which were identified as characteristics linked with the concordance of treatment recommendations by multivariate analysis in the earlier study,13 and the amount of evidence (high vs low) were used to stratify 50 simulated cases into prelearning and postlearning evaluation groups (Figure 1A). The cancer types and genomic alterations present in each case in the prelearning and postlearning assessment groups are displayed in eTable 1 in Supplement 1. Eligible participants in this research included MTBs at hub hospitals, physicians at core hospitals, and AI system companies. Each participant created treatment recommendations for each case in the prelearning evaluation group by using the simulated clinical data and test reports from registration to June 30, 2021; thereafter, they participated in the learning program on July 18, 2021, and created treatment recommendations for each case in the postlearning evaluation group from August 3 to September 30, 2021. The central committee evaluated the concordance between central treatment recommendations and the treatment recommendations made by participants (Figure 1B). Similar to the results in the previous study by Naito et al,13 concordance was defined as follows: (1) among therapies suggested by the central treatment recommendations, at least 1 must be recommended; and (2) if evidence level of R, which indicates genomic changes resistant to a particular treatment, was included in the simulated case, all treatments identified as avoided should not be applied.
Figure 1. Study Overview.
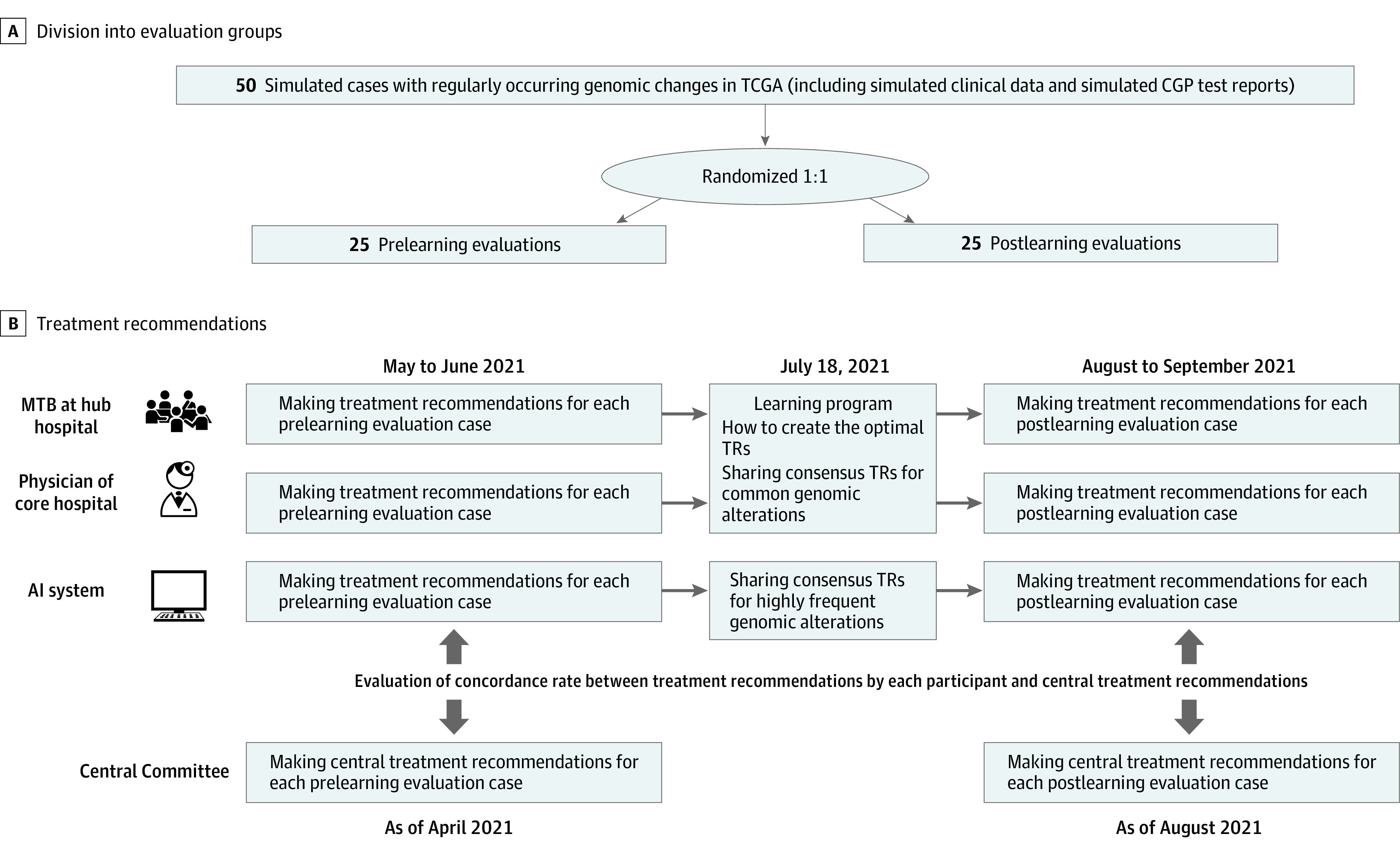
A, Fifty simulated cases were randomly divided into prelearning and postlearning evaluations (25 cases in each), stratified by levels of evidence (high vs low) and presence or absence of TP53 alteration. B, From May 1 to June 30, 2021, each participant made treatment recommendations (TRs) for each simulated case in the prelearning evaluation. Then, they participated in the learning program on July 18, 2021. Finally, TRs were made for simulated cases in postlearning evaluations from August 1 to September 30, 2021. The central committee evaluated the concordance in the prelearning evaluations between TRs by the participant and the central TRs prepared in April 2021. In postlearning evaluations, TRs by participants were evaluated for concordance with the central TRs prepared in August 2021. AI indicates artificial intelligence; CGP, comprehensive genome profiling; MTBs, molecular tumor boards; and TCGA, The Cancer Genome Atlas.
Learning Program
The online learning program demonstrated the methodology of making optimal treatment recommendations, particularly in IND trials related to biomarkers with low evidence levels, including those with alterations in TP53. We also shared central treatment recommendations for cases with common genomic alterations (eTable 3 in Supplement 1).
End Points
The primary end point was the accreditation rate of MTBs, defined as the proportion of MTBs that met prespecified accreditation criteria according to the postlearning evaluation results. As described by Naito et al,13 the accreditation criteria were defined as approximately 90% concordance in cases harboring genomic alteration with high evidence levels and approximately 40% in cases of genomic alterations with low evidence levels. The secondary end points were the proportion of physicians who met predetermined accreditation standards for postlearning evaluations and chronological improvements in concordance of treatment recommendations on postlearning compared with prelearning evaluations for each participant. The agreement of treatment recommendations with the AI system was an exploratory end point.
Statistical Analysis
Data were analyzed from September 2 to December 10, 2021. The projected sample size was 27 MTBs, calculated based on an expected accreditation rate of 50% and a threshold of 20%, with a 2-sided α = .05 and a power of 80%. For the primary analysis, we conducted an exact 2-tailed binomial test against the null hypothesis that the accreditation rate is the threshold of 20%. Furthermore, the Clopper-Pearson 95% CI was determined. The learning program was one of the components evaluated using logistic mixed-effect models for concordance (eMethods in Supplement 1). The 2 variables, prelearning and postlearning evaluations and evidence levels, were incorporated into the model as fixed-effect variables. The random intercept was used to deal with the heterogeneity of the participants in the models. The model’s predictive performance was approximated using the mean of the area under the receiver operating characteristic curve that was constructed from 2000 iterations of 5-fold cross-validation. In all analyses, 2-sided P ≤ .05 was regarded as statistically significant. Analyses were performed using R, version 4.1.0 (R Program for Statistical Computing).
Results
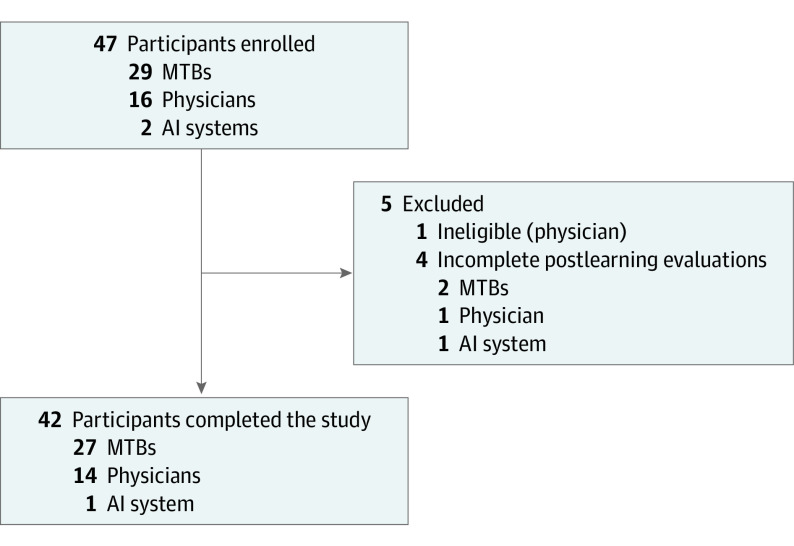
Participants
Forty-seven participants consisting of 29 MTBs, 16 physicians, and 2 AI companies applied from April 7 to May 13, 2021. Five participants were excluded: 1 physician was ineligible for this study, and 4 participants (2 MTBs, 1 physician, and 1 AI company) did not complete the treatment recommendations for the postlearning evaluation. Forty-two participants consisting of 27 MTBs, 14 physicians, and 1 AI company completed this research (Figure 2). As a result, the post hoc statistical power was 0.99 for the primary end point. The AI system developed by a domestic company uses a knowledge database consisting of published information about approved drugs, guidelines, and clinical trials to make treatment recommendations.
Figure 2. Study Flow Diagram.
AI indicates artificial intelligence; MTBs, molecular tumor boards.
Central Treatment Recommendations
The central committee developed central treatment recommendations for all 50 simulated cases in April 2021 for prelearning evaluations and updated them in August 2021 for postlearning evaluations (eTable 1 in Supplement 1). Due to the approval of new medications or a change in the status of IND trial enrollment, central treatment recommendations were revised in 11 of 50 simulated cases (22.0%).
Accreditation Rate for Postlearning Tests
The accreditation rate of MTBs was 55.6% (95% CI, 35.3%-74.5%; P < .001), which was significantly higher than the prespecified threshold. For individuals, the accreditation rate was 35.7% (95% CI, 12.8%-64.9%; P = .17).
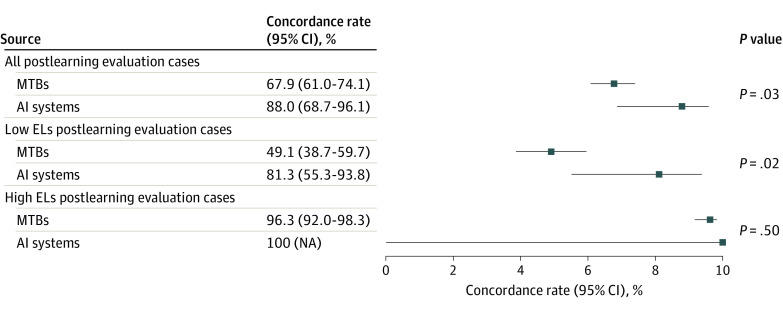
Concordance in Postlearning Tests
In postlearning evaluations, the concordance rate between central treatment recommendations and the treatment recommendations made by MTBs, was 67.9% (95% CI, 61.0%-74.1%); by physicians, 57.5% (95% CI, 51.7%-63.1%); and by an AI system, 88.0% (95% CI, 68.7%-96.1%) (Figure 3 and eTable 4 in Supplement 1). The concordance of treatment recommendations made by the AI system was significantly higher than that of treatment recommendations by MTBs (P = .03). According to evidence levels, there was no difference in concordance between the AI system and MTBs at high evidence levels (100% [95% CI, not applicable] and 96.3% [95% CI, 92.0%-98.3%], respectively; P = .50), but the difference in concordance between the AI system and MTBs was significantly larger at low evidence levels (81.3% [95% CI, 55.3%-93.8%] and 49.1% [95% CI, 38.7%-59.7%], respectively; P = .02) (Figure 3).
Figure 3. Analysis of Concordance of Treatment Recommendations by Molecular Treatment Boards (MTBs) and an Artificial Intelligence System (AI) in Postlearning Evaluations .
The concordance of treatment recommendations made by the AI system was significantly higher than that of treatment recommendations made by 27 MTBs in all postlearning evaluations, especially those cases with genomic alterations with low evidence levels (ELs). NA indicates not applicable.
Improvement of the Concordance
The concordance increased from 58.7% (95% CI, 52.8%-64.4%) in prelearning evaluations to 67.9% (95% CI, 61.0%-74.1%) in postlearning evaluations in MTBs (odds ratio [OR], 1.40 [95% CI, 1.06-1.86]; P = .02), and from 55.3% (95% CI, 42.3%-67.6%) in prelearning evaluations to 61.0% (95% CI, 47.8%-72.8%) in postlearning evaluations in physicians (OR, 1.26 [95% CI, 0.85-1.87]) (eFigure 1 in Supplement 1). For the AI participant, the concordance also increased from 80.0% (95% CI, 60.0%-91.4%) to 88.0% (95% CI, 68.7%-96.1%). In MTBs, there was a considerable improvement in the concordance of biomarkers with low evidence (OR, 1.32 [95% CI, 1.00-1.73]; P = .03), but not in physicians (OR, 1.11 [95% CI, 0.75-1.63]; P = .52) (eFigure 2 in Supplement 1).
Factors Associated With Concordance
The univariable analysis demonstrated that a high evidence level was a significant factor associated with concordance in both MTBs and individuals (eTable 5 in Supplement 1). Furthermore, multivariable analysis for factors associated with concordance revealed that participating in the learning program was an independent factor associated with the enhancement of the concordance in MTBs (Table). The mean areas under the receiver operating characteristic curve were 0.811 (95% CI, 0.761-0.858) for MTBs and 0.828 (95% CI, 0.762-0.891) for physicians.
Table. Multivariable Analysis for Factors Associated With Concordance Rate.
| Factors | OR (95% CI) | P value |
|---|---|---|
| MTBs (n = 27) | ||
| Prelearning vs postlearning evaluations | 1.40 (1.06-1.86) | .02 |
| Evidence level, low vs high | 0.05 (0.025-0.070) | <.001 |
| Physicians (n = 14) | ||
| Prelearning vs postlearning evaluations | 1.26 (0.85-1.87) | .25 |
| Evidence level, low vs high | 0.08 (0.05-0.13) | <.001 |
Abbreviations: MTBs, molecular tumor boards; OR, odds ratio.
Consistency of Treatment Recommendations
On an exploratory basis, we assessed the consistency of treatment recommendations in postlearning evaluations. Nine simulated cases with TP53 alterations had recommendations for treatment with AMG 650, while the AI system suggested AMG 650 with treatment recommendations for 8 cases (88.9%); however, they were less consistent in MTBs and physicians (2.8 [31.3%] and 3.3 [36.5%], respectively) (eTable 6 in Supplement 1).
Discussion
We created a learning program to enhance treatment recommendations made by MTBs and examined the effectiveness of the program by assessing the concordance between central treatment recommendations and the treatment recommendations made by participants in postlearning evaluations. The accreditation rate of MTBs in the postlearning evaluation was 55.6% (95% CI, 35.3%-74.5%; P < .001), which was significantly higher than the prespecified threshold. Concordance for cases with biomarkers with low evidence levels improved significantly in the postlearning evaluation among MTBs (OR, 1.32 [95% CI, 1.00-1.73]). These results indicate that the learning program increases the concordance between treatment recommendations provided by MTBs and central recommendations, particularly recommendations for cases with biomarkers having low evidence levels, including the IND trials. Sunami et al18 previously reported that approximately 60% of the cases that received genomically matched therapies based on CGP test results were identified as IND trials. Furthermore, they demonstrated a positive correlation between the number of cases enrolled in IND trials and the proportion receiving matched treatments at core hospitals.18 As a result, by helping MTBs select eligible IND studies, our learning approach may help increase the accessibility of genomically matched medicines.
In this research, our central treatment recommendations were revised every 4 months, after which 11 (22.0%) of them were changed. Since the main reason for these dynamic changes was a trial structure with the opening and closing of treatment cohorts in corresponding IND trials, a system of facilitating the sharing of the latest information regarding IND trials is urgently required.
Although it is always vital to keep up with the latest information on the availability of enrollment in IND trials to make appropriate treatment recommendations for CGP test results, manually searching for available trials is an error-prone process for MTB members. Consequently, an AI-based annotation system may aid in providing more precise treatment recommendations. In this investigation, treatment recommendations generated by the AI system had a concordance that was higher than treatment recommendations generated by MTBs. The difference in concordance between the AI system and MTBs was larger for genomic alterations with low evidence levels (81.3% [95% CI, 55.3%-93.8%] and 49.1% [95% CI, 38.7%-59.7%], respectively; P = .02). These results indicate that an AI system may more appropriately suggest an appropriate IND trial than an MTB.
Limitations
Our study has several limitations. First, this study comparatively analyzed the concordance between treatment recommendations by MTBs and central recommendations and did not determine whether the latter truly improved patient outcomes. However, Naito et al13 previously demonstrated that central treatment recommendation properly covered the candidate treatment. In terms of providing appropriate treatment options, we defined the central treatment recommendations that are the best recommendations. Second, we assessed treatment recommendations not for actual cases, but for simulated cases. To ensure that there were no differences with actual cases, confirmation by multiple medical oncologists was conducted. Furthermore, all of the simulated cases had patients whose diseases were progressing despite standard therapy or for whom there were no effective standard treatments. These statuses are consistent with the indication for CGP tests in Japan. Third, because optimal treatment recommendations will change over time, our central treatment recommendations might have been created at a chronologically different time from the treatment recommendations made by participants. To minimize the difference over time, we updated the central treatment recommendations every 4 months. Fourth, we could only assess 1 AI system. Since manually searching for the latest information regarding available IND trials and scientific evidence related to identified genomic alterations is a time-consuming and error-prone task for MTBs, AI-based support systems are being developed. Further investigation is needed to examine the optimal AI system to provide treatment recommendations.
Conclusions
In this quality improvement study, our learning program significantly improved the quality of treatment recommendations by MTBs. The AI-based treatment recommendations demonstrated higher concordance with central consensus treatment recommendations than MTBs, indicating the utility of AI-based treatment recommendations over those made by MTBs.
eFigure 1. Improvement in Concordance
eFigure 2. Improvement in Concordance of Treatment Recommendations for Cases With High ELs and Low ELs
eTable 1. List of Simulated Cases in Prelearning and Postlearning
eTable 2. Evidence Levels Based on Clinical Practice Guidance for Next-Generation Sequencing in Cancer Diagnosis and Treatment (Edition 2.1)
eTable 3. List of Central Treatment Recommedations of High Frequent Genomic Alterations
eTable 4. Concordance Rate in Postlearning
eTable 5. Univariable Analysis for Factors Associated With Concordance Rate
eTable 6. Concordance of Treatment Recommendations for AMG 650
eMethods. Details of Multivariable Mixed-Effects Model
Data Sharing Statement
References
- 1.Radovich M, Kiel PJ, Nance SM, et al. Clinical benefit of a precision medicine based approach for guiding treatment of refractory cancers. Oncotarget. 2016;7(35):56491-56500. doi: 10.18632/oncotarget.10606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Olsen S, Liao J, Hayashi H. Real-world clinical outcomes after genomic profiling of circulating tumor DNA in patients with previously treated advanced non–small cell lung cancer. Curr Oncol. 2022;29(7):4811-4826. doi: 10.3390/curroncol29070382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.André F, Bachelot T, Commo F, et al. Comparative genomic andomizedon array and DNA sequencing to direct treatment of metastatic breast cancer: a multicentre, prospective trial (SAFIR01/UNICANCER). Lancet Oncol. 2014;15(3):267-274. doi: 10.1016/S1470-2045(13)70611-9 [DOI] [PubMed] [Google Scholar]
- 4.Le Tourneau C, Delord JP, Gonçalves A, et al. ; SHIVA investigators . Molecularly targeted therapy based on tumour molecular profiling versus conventional therapy for advanced cancer (SHIVA): a multicentre, open-label, proof-of-concept, andomized, controlled phase 2 trial. Lancet Oncol. 2015;16(13):1324-1334. doi: 10.1016/S1470-2045(15)00188-6 [DOI] [PubMed] [Google Scholar]
- 5.Eckhardt SG, Lieu C. Is precision medicine an oxymoron? JAMA Oncol. 2019;5(2):142-143. doi: 10.1001/jamaoncol.2018.5099 [DOI] [PubMed] [Google Scholar]
- 6.Trédan O, Wang Q, Pissaloux D, et al. ; ProfiLER investigators . Molecular screening program to select molecular-based recommended therapies for metastatic cancer patients: analysis from the ProfiLER trial. Ann Oncol. 2019;30(5):757-765. doi: 10.1093/annonc/mdz080 [DOI] [PubMed] [Google Scholar]
- 7.Chan KKW, Tannock IF. Should basket trials be pathways to drug registration for biomarker-defined subgroups of advanced cancers? J Clin Oncol. 2021;39(22):2426-2429. doi: 10.1200/JCO.21.00552 [DOI] [PubMed] [Google Scholar]
- 8.Ebi H, Bando H. Precision oncology and the universal health coverage system in Japan. JCO Precis Oncol. 2019;3:1-12. doi: 10.1200/PO.19.00291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sunami K, Naito Y, Aimono E, et al. The initial assessment of expert panel performance in core hospitals for cancer genomic medicine in Japan. Int J Clin Oncol. 2021;26(3):443-449. doi: 10.1007/s10147-020-01844-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Naito Y, Aburatani H, Amano T, et al. ; Japanese Society of Medical Oncology; Japan Society of Clinical Oncology; Japanese Cancer Association . Clinical practice guidance for next-generation sequencing in cancer diagnosis and treatment (edition 2.1). Int J Clin Oncol. 2021;26(2):233-283. doi: 10.1007/s10147-020-01831-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rieke DT, Lamping M, Schuh M, et al. Comparison of treatment recommendations by molecular tumor boards worldwide. JCO Precis Oncol. 2018;2:1-14. doi: 10.1200/PO.18.00098 [DOI] [PubMed] [Google Scholar]
- 12.Koopman B, Groen HJM, Ligtenberg MJL, et al. Multicenter comparison of molecular tumor boards in the Netherlands: definition, composition, methods, and targeted therapy recommendations. Oncologist. 2021;26(8):e1347-e1358. doi: 10.1002/onco.13580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Naito Y, Sunami K, Kage H, et al. Concordance between recommendations from multidisciplinary molecular tumor boards and central consensus for cancer treatment in Japan. JAMA Netw Open. 2022;5(12):e2245081. doi: 10.1001/jamanetworkopen.2022.45081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Muiños F, Martínez-Jiménez F, Pich O, Gonzalez-Perez A, Lopez-Bigas N. In silico saturation mutagenesis of cancer genes. Nature. 2021;596(7872):428-432. doi: 10.1038/s41586-021-03771-1 [DOI] [PubMed] [Google Scholar]
- 15.Tamborero D, Dienstmann R, Rachid MH, et al. ; Cancer Core Europe consortium . Support systems to guide clinical decision-making in precision oncology: the Cancer Core Europe Molecular Tumor Board Portal. Nat Med. 2020;26(7):992-994. doi: 10.1038/s41591-020-0969-2 [DOI] [PubMed] [Google Scholar]
- 16.Allemani C, Matsuda T, Di Carlo V, et al. ; CONCORD Working Group . Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391(10125):1023-1075. doi: 10.1016/S0140-6736(17)33326-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Cancer Institute . The Cancer Genome Atlas Program (TCGA). Accessed February 27, 2023. https://www.cancer.gov/ccg/research/genome-sequencing/tcga
- 18.Sunami K, Naito Y, Komine K, et al. Chronological improvement in precision oncology implementation in Japan. Cancer Sci. 2022;113(11):3995-4000. doi: 10.1111/cas.15517 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Improvement in Concordance
eFigure 2. Improvement in Concordance of Treatment Recommendations for Cases With High ELs and Low ELs
eTable 1. List of Simulated Cases in Prelearning and Postlearning
eTable 2. Evidence Levels Based on Clinical Practice Guidance for Next-Generation Sequencing in Cancer Diagnosis and Treatment (Edition 2.1)
eTable 3. List of Central Treatment Recommedations of High Frequent Genomic Alterations
eTable 4. Concordance Rate in Postlearning
eTable 5. Univariable Analysis for Factors Associated With Concordance Rate
eTable 6. Concordance of Treatment Recommendations for AMG 650
eMethods. Details of Multivariable Mixed-Effects Model
Data Sharing Statement