Abstract
Background
Despite the changing roles of faculty in the health professions over the past two decades, none of the reviews has been paid enough attention to the impact of the faculty development programs on these roles. The objective of this review is to synthesize the existing evidence that addresses the questions: “What are the types and outcomes of faculty development programs based on the Harden teachers’ role framework and which of the areas described by Harden and Crosby are the authors referring to?”
Methods
This review was conducted according to the guidance for Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) framework. In 2020, a literature search was conducted in MEDLINE/PubMed, Scopus, ERIC, ScienceDirect, Google Scholar, Magiran and SID databases. The review included 119 studies (between 1990 and 2020) that met the review criteria. Data were extracted using a modified coding sheet. We used the modified Kirkpatrick model to assess the educational outcomes of faculty development programs.
Results
The majority of faculty development programs were workshops (33.61%) with various durations. Most programs focused on the domain of information provider and coach (76.47%), followed by the facilitator of learning and mentor (53.78%) and assessor and diagnostician (37.81%). Only five faculty development programs focused on the domain of role model. The majority (83.19%) of outcomes reported were at level 2B, level 1 (73.95%) and level 2A (71.42%). Gains in knowledge and skills related to teaching methods and student assessment were frequently noted. Behavior changes included enhanced teaching performance, development of new educational curricula and programs, improved feedback and evaluation processes, new leadership positions, increased academic output and career development. The impact on the organizational practice continued to be underexplored.
Conclusion
Based on the review findings, broadening the scope of faculty development programs beyond the traditional roles of the faculty members by utilizing a competency-based framework for developing a comprehensive faculty development program is recommended. Attention to individualized form of faculty development programs and incorporating more informal approaches into the design and delivery of faculty development programs is also needed.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12909-023-04863-4.
Keywords: Faculty development, Program evaluation, Faculty, Role, Competency-based education
Background
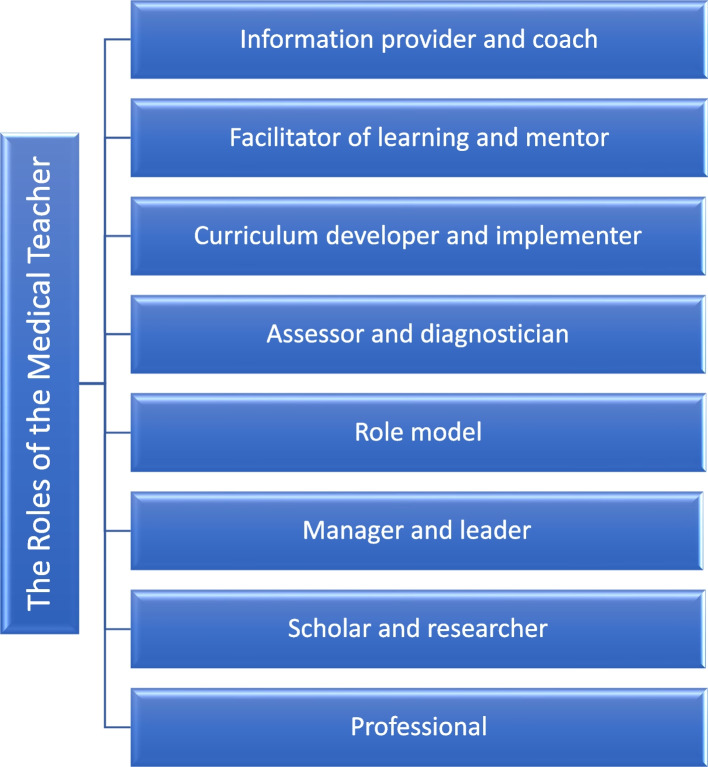
Faculty development has become an integral part of organizational development [1] and can play an important role in promoting organizational change [2]. As noted by Wilkerson and Irby [3], “Academic vitality is dependent upon faculty members’ interest and expertise; faculty development has a critical role to play in promoting academic excellence and innovation, and it is a tool for improving the educational vitality of our institutions through attention to the competencies needed by individual teachers and to the institutional policies required to promote academic excellence”. This notion is further supported by the work of Harden and Crosby [4], who described and were further expanded the eight roles of the medical teacher (information provider and coach, facilitator of learning and mentor, curriculum developer and implementer, assessor and diagnostician, role model, manager and leader, scholar and researcher and professional) in the education programme (Fig. 1). This teachers’ role framework can be considered as a guide for designing and evaluating faculty development programs, as described by Harden and Crosby [4], in that it provides evidence about which faculty’ roles covered by the programs and identifies the needs for faculty development programs [4]. Moreover, considering this competency-based framework in the design and evaluation of faculty development programs can play an important role in expanding our approaches to faculty development programs and would help to inform both content and desired outcomes [2].
Fig. 1.
The eight roles of the medical teachers
To date, few publications have reviewed the impact and outcome of faculty development programs in the health professions education. Despite the emergence of outcome-based education and its impact on faculty development programs [5] on the one hand, and the introduction of medical teachers’ role framework by Harden and Crosby [4] on the other, none of the reviews followed this teachers’ role framework. In 2006 and 2016, Steinert et al. reviewed the literature on faculty development initiatives designed to improve teaching effectiveness in medical education and concluded that despite the usefulness of faculty development programs for participants and changes in their learning and behavior, further research to explore outcomes at the individual and organizational levels is needed. These reviews were limited to faculty development designed to enhance the effectiveness of teaching in medicine. They suggested that it would now be useful to update these reviews and to carry out a similar review of faculty development focusing on other faculty roles [6, 7]. Johnston et al. [8] reviewed 70 articles on faculty development initiatives in academic dentistry and pointed to the need for more research in more areas and using additional methodologies. Bilal et al. [9] conducted a systematic review of studies, published during 2003–2016, to explore the effectiveness of faculty development programs on medical and allied health faculty’s professional development. They highlighted that there is no well-structured theoretical framework for faculty development programs that can be incorporated across institutions. More recently, Behar-Horenstein et al. [10] reviewed the literature (published between 2006 and 2018) on faculty development initiatives in the health professions and recommended that future faculty development studies include pre-test and post-test measures with control and treatment groups or implement time series studies to assess the impact of the intervention beyond the conclusion of faculty development program. We decided to conduct this review for several reasons. Firstly, we believed that this 30-year review would allow us to describe the evolution of faculty development programs in the past three decades. Secondly, we wanted to identify emerging trends and articulate a sound theoretical basis to help advance the practice. Thirdly, despite the changing roles of faculty in the health professions over the past two decades, none of the reviews has been paid enough attention to the impact of the faculty development programs on these roles. Fourthly, given the expanding number of roles of faculty in the health professions, there has been no comprehensive systematic review of faculty development programs to target all health professions teachers’ roles. Lastly, we wanted to address limitations and recommendations identified by previous reviews.
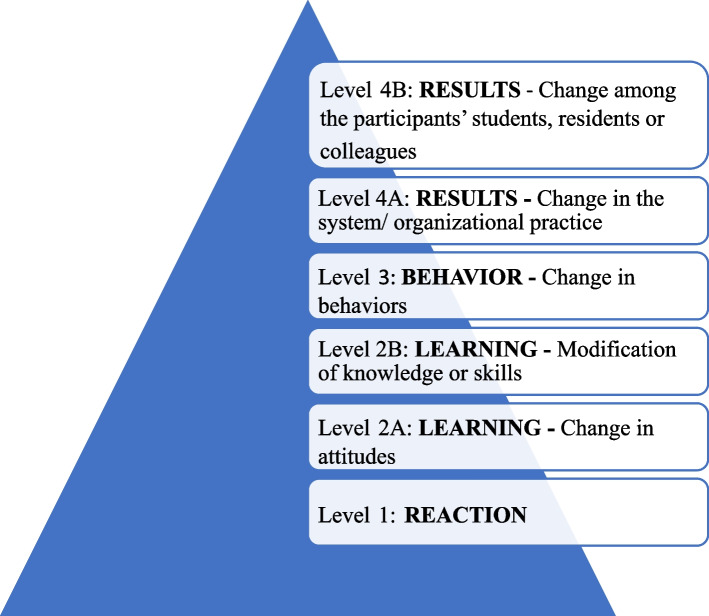
Notably, our study is the first systematic review of faculty development programs based on the Harden teachers’ role framework model. In addition, we appraised the quality of the studies using a reliable tool for appraising methodological quality of medical education research, the Medical Education Research Study Quality Instrument (MERSQI) [11]. Moreover, we used the modified Kirkpatrick model (Fig. 2) to assess the educational outcomes of faculty development programs. This model was adopted by the BEME (Best Evidence Medical Education) Collaboration and includes students, residents and colleagues (instead of patients) at level 4B [7]. It is also noteworthy that in the present study, in addition to international databases, national databases were also searched from 1990 to 2020. Given the potential importance of faculty development programs in the health professions, the objective of this review is to determine the types and outcomes of faculty development programs based on the Harden teachers’ role framework model and to identify, or explain, to which of the areas described by Harden and Crosby the authors are referring. More specifically, this review addressed the following research questions:
Fig. 2.
Kirkpatrick’s model for evaluating educational outcomes
What are the types and duration of faculty development programs designed to prepare faculty members for their various roles in health sciences education?
Which of the areas, or faculty’ roles, described by Harden and Crosby are the authors referring to?
What are the impacts of faculty development programs on the knowledge, attitudes and skills of faculty members in health sciences education, and on the institutions in which they work?
We hope that such a review of the literature and a synthesis of quantitative and qualitative studies will help to conceptualize our knowledge of the field and guide educators interested in the design, development, and evaluation of faculty development.
Methods
This systematic review was conducted according to the guidance for Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) framework suggested by Moher et al. [12] in January 2020 to explore the types and outcomes of faculty development programs designed to prepare faculty members for their various roles in health sciences education based on the Harden teachers’ role framework model. The review was a part of a doctoral dissertation performed to fulfil the requirements of a Ph.D. (Doctor of Philosophy) program in medical education at Isfahan University of Medical Sciences and Health Services. The study was approved by the Institutional Research Ethics Committee of Medical University of Isfahan.
Information sources and search strategy
In January 2020, the authors conducted an extensive review of published articles between 1990 and 2020 to identify all potentially relative studies. A literature search was conducted in MEDLINE/PubMed (Last searched on February 29, 2020), Scopus (Last searched on April 30, 2020), ERIC (Last searched on June 30, 2020), ScienceDirect (Last searched on August 30, 2020), Google Scholar (Last searched on October 30, 2020), Magiran (Last searched on November 30, 2020) and SID (Scientific Information Database, Last searched on December 30, 2020) using the following keywords: “faculty development”; “faculty empowerment”; “faculty training”; “faculty education”; “faculty promotion”; “teacher education”; “teacher training”; “teacher improvement”; “teacher promotion”; “in-service training”; “in-service teacher education”; “professional development”; “medical education”; “program evaluation”; “medical teacher”; “health sciences educator/education”; “medical faculty”; “nursing faculty”; “dental faculty”; “pharmacy faculty” and “clinical teacher”. Keywords were combined with the Boolean operators AND/OR. Although the search was not limited by country of practice, the search was conducted with limitation on publication year, language, study design and full text availability. Search results limited to full text empirical studies published in English or Persian during 1990–2020. We chose these databases because they cover faculty development programs in the health sciences education. A copy of the search strategy used within MEDLINE/PubMed is provided in Appendix 1 (see Additional file 1). In addition, we conducted an extensive review of published articles in medical education core journals. The journals searched included: Medical Teacher, Medical Education, Academic Medicine, Teaching and Learning in Medicine, The Clinical teacher, Medical Science Educator, International Journal of Medical Education, Advances in Health Sciences Education and The Journal of Faculty Development. We also searched reference lists of all review articles.
Inclusion/exclusion criteria
The following criteria guided the selection of studies for this review:
Study focus: Based on the review questions, all types of faculty development programs, of whatever duration, designed to prepare faculty members for their various roles in health sciences education were included. Studies not relating to faculty development programs in the health professions were excluded.
Study population: We included studies that involved faculty development programs for both basic science and clinical faculty members in all disciplines of health sciences. Any study involving the development of staff and students was excluded.
Study design: To be included, studies must have intervention and measurement (outcome data). Thus, only empirical studies with pre-test post-test design were included. Both quantitative and qualitative studies were included. Reviews and articles described general information about faculty development programs with no intervention or evaluation data were excluded. Additionally, empirical studies with post-test design only were excluded.
Year of publication: We selected all qualitative and quantitative studies assessing faculty development programs from 1990 to 2020 for inclusion. The selection of articles for review was completed in 2020.
Language and country of practice: Although the search was not limited by country of practice, the review was limited to studies published in English and Persian. Articles not written in the English or Persian language were excluded.
Screening and study selection
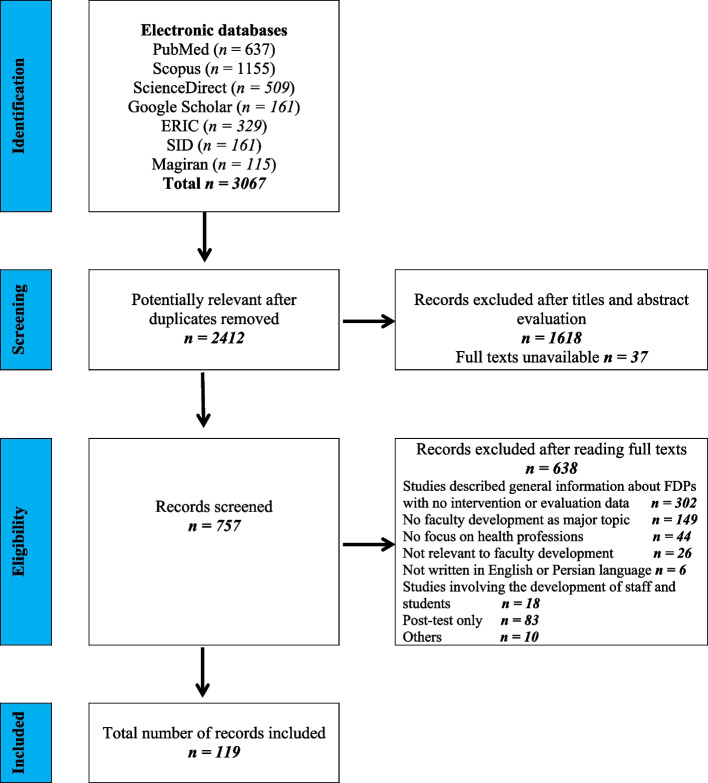
In total 3067 articles were identified through the initial search of the seven databases. The study screening was done by three authors (MK, NY and TC) in three stages: by title, then by abstract, and finally by full text review. From an initial 3067 articles, 2412 articles were potentially relevant after duplicates removed by one of three reviewers (MK). After removing duplicates, title and abstract screening was undertaken independently by two authors (MK or NY) with disagreements between them resolved by consensus. A third author (TC) was recruited to facilitate agreement when needed. This resulted in 757 articles being identified as potentially relevant and retrieved in full text for comprehensive review. Full-text screening was carried out by one of two authors (MK or NY) based on pre-determined eligibility criteria with any studies deemed ineligible cross-checked by the third author (TC). Of the 757 full papers that were screened, 638 studies were excluded as they did not meet the inclusion criteria for the review. Finally, a total of 119 studies met the inclusion criteria and were submitted to data extraction (Fig. 3).
Fig. 3.
PRISMA flow chart of the systematic review
Data extraction and summary of findings
Relevant information was extracted from each included studies using a coding sheet, which was developed from previous systematic review work (BEME Guide No. 8). The applicability of the coding sheet was assessed in the original study by the pilot study and the Faculty Development Topic Review Group members’ research experience [7]. The coding sheet, which was based on the original prototype provided by the BEME Guide No. 8, was modified to data extraction. Data were extracted included following components: authors and publication years, country and institution, type of program or intervention and duration, participants, faculty roles covered by the program, study design, outcomes, outcome level and study quality (MERSQI) score. The coding sheet is provided in Appendix 2 (see Additional file 2). Data extraction was conducted by MK checked by a second author (NY). Where necessary, the third reviewer (TC) assisted in resolving differences. To identify to which of the areas, or faculty, roles, described by Harden and Crosby the authors are referring, two authors (MK and NY) separately read the research articles. Thereafter, they assigned the faculty development programs to one or more of Harden’s eight domains. Discrepancies in judgment between the two authors were resolved through discussion. The third author (TC) was recruited to facilitate agreement when needed. Once the coding sheet was completed, the extracted data were grouped for the synthesis stage based on the review objectives. This was done manually by the first author (MK) and checked by the second author (NY).
Quality assessment
The quality of the studies was appraised using the Medical Education Research Study Quality Instrument (MERSQI). We chose this instrument because the MERSQI was developed to appraise the methodological quality of experimental, quasi-experimental, and observational studies in medical education research, typically in the process of a literature review of a field or topic in medical education [11]. The MERSQI evaluates study quality based on the following items: study design, sampling (institutions & response rate), type of data, validity evidence for evaluation instrument scores, data analysis (sophistication & appropriate) and outcome. Each item is scored on a scale of 1–3 and summed to determine a total score. The maximum score for each domain was 3, therefore the maximum MERSQI score is 18 with a potential range of 5–18.
Results
For better collation and interpretation, review findings will be organized into four sections:
Overview of articles included in review- which will be further divided into: publication years, country and institution.
Description of faculty development programs and expected outcomes- which will be further divided into: type of program or intervention, duration, participants, outcomes and outcome level.
Eight domains of faculty roles covered by the faculty development programs according to Harden- which will be further divided into: the teacher as an information provider and coach, the teacher as a facilitator of learning and mentor, the teacher as a curriculum developer and implementer, the teacher as an assessor and diagnostician, the teacher as a role model, the teacher as a manager and leader, the teacher as a scholar and researcher and the teacher as a professional.
Quality appraisal of the studies- which will be further divided into: study design, sampling (institutions & response rate), type of data, validity evidence for evaluation instrument scores, data analysis (sophistication & appropriate) and outcome.
Overview of articles included in review
Figure 3 provides an overview of the search strategy and the process of study selection. The characteristics of the 119 included studies, along with the quality assessment score, are summarised in Table S1 (see Additional file 3).
Publication years
The year of publication for the 119 selected studies ranged from 1992 to 2019. The year with the highest number of published studies was 2017 (n = 12, 10.08%).
Country and institution
Of the 119 articles reviewed, most of the studies were conducted in the USA (n = 86, 72.27%). Ninety two of the included studies (77.31%) were conducted by universities. Of these, 33 (35.86%) came from schools of medicine; Ten (10.86%) were conducted by colleges of Pharmacy; 8 (8.69%) were undertaken by schools of dentistry and two implemented in nursing schools. Table 1 shows the results of this section.
Table 1.
General characteristics of the included studies
| n , total = 119 | % | |
|---|---|---|
| Publication years | ||
| 1992-1996 | 4 | 3.4 |
| 1997-2001 | 5 | 4.2 |
| 2002-2006 | 25 | 21 |
| 2007-2011 | 13 | 10.9 |
| 2012-2016 | 46 | 38.7 |
| 2017-2020 | 26 | 21.8 |
| Country | ||
| USA | 86 | 72.27 |
| Canada | 5 | 4.20 |
| India | 4 | 3.37 |
| Iran | 3 | 2.52 |
| Germany | 2 | 1.68 |
| Nepal | 2 | 1.68 |
| Russia | 2 | 1.68 |
| Switzerland | 2 | 1.68 |
| Sweden | 2 | 1.68 |
| Bhutan | 1 | 0.84 |
| China | 1 | 0.84 |
| Chile | 1 | 0.84 |
| Japan | 1 | 0.84 |
| Mexico | 1 | 0.84 |
| Mongolia | 1 | 0.84 |
| Qatar | 1 | 0.84 |
| South Korea | 1 | 0.84 |
| Tanzania | 1 | 0.84 |
| Taiwan | 1 | 0.84 |
| UK | 1 | 0.84 |
| Institution | ||
| Universities | 92 | 77.31 |
| Hospitals | 10 | 8.40 |
| Foundations and societies | 17 | 14.29 |
-
(b)
Description of faculty development programs and expected outcomes.
Type of program or intervention
According to the included studies, the majority of faculty development programs were workshops (n = 40, 33.61%) with various durations. Nineteen (nearly 16% of faculty development programs) were described as a short course and sixteen (13.44%) as a seminar series. In six (5.04%) studies, the use of a mentorship program was described. There were three fellowship studies. Twenty nine (24.36%) were described as a longitudinal program and six fell under ‘other’, which included a journal club, OSTE (Objective Structured Teaching Exercise) and conferences.
Duration
The duration of faculty development programs varied depending on the type of intervention and ranged from 20 min to six years. The duration of workshops ranged from one hour to six weeks, with a median duration of two days. The duration of the seminar series ranged from one and a half hours to seven weeks, with a median duration of twenty-eight hours. The short courses ranged from one hour to four weeks (with a median duration of one day), and the longitudinal programs ranged from seven weeks to five years with a median duration of one year. Mentorship programs ranged in duration from nine months to 4 years, with a median duration of two years. The duration of fellowship programs ranged from one year to six years.
Participants
The 119 included studies involved a total of 7633 participants (sample sizes from 5 to 516). Studies were heterogeneous in terms of participant populations. The majority of faculty development programs (n = 64, 53.78%) involved faculty from multiple disciplines. Thirty five (29.41%) studies out of 119 occurred in medicine only. Studies in pharmacy (n = 10, 8.4%), dentistry (n = 8, 6.72%) and nursing (n = 2, 1.68%) constituted less than one fifth of the articles reviewed. In twelve (10.08%) studies, in addition to faculty members, residents also participated as participants. Twenty six (21.84%) faculty development programs were designed for both basic scientists and clinical faculty members. The majority of faculty development programs targeted clinical faculty members, with a predominance of interventions in family medicine and internal medicine.
Outcomes and outcome level
We classified the reported outcomes using the Kirkpatrick’s model of educational outcomes. The majority (n = 99, 83.19%) of outcomes reported are at level 2B (modification of knowledge or skills). Only four studies [13–16] assessed change among the participants’ students, residents or colleagues (level 4B). Table 2 shows the summary of faculty development outcomes by Kirkpatrick level.
Table 2.
Summary of faculty development outcomes by Kirkpatrick level*
| Level of outcomes | % |
|---|---|
| Reaction | 73.95 |
| Learning | 94.95 |
| 85/119 assessed changes in attitudes | |
| 99/119 assessed changes in knowledge/skills | |
| Behavior | 49.57 |
| Results | 15.96 |
| 19/119 assessed change in the system/ organizational practice | |
| 4/119 assessed change among the participants’ students, residents or colleagues |
*Numbers may not equal 100% as some studies assessed outcomes in more than one way
(c) Eight domains of faculty roles covered by the faculty development programs according to Harden.
Summary of included studies based on Harden’s eight domains is presented in Table 3. As we anticipated, the majority (n = 79, 66.38%) of faculty development programs covered more than one domain of faculty roles; however, none of the programs covered all eight domains of faculty roles. Most of the articles focused on the domain of information provider and coach (76.47%), followed by the facilitator of learning and mentor (53.78%) and assessor and diagnostician (37.81%). We have detailed the study findings based on the Harden teacher’s role framework in Appendix 3 (see Additional file 4).
Table 3.
Summary of included studies based on Harden’s eight domains
| Information provider and coach | Facilitator of learning and mentor | Curriculum developer and implementer | Assessor and diagnostician | Role model | Manager and leader | Scholar and researcher | Professional | |
|---|---|---|---|---|---|---|---|---|
| Frequency n (%) | 91 (76.47%) | 64 (53.78%) | 18 (15.12%) | 45 (37.81%) | 5 (4.2%) | 19 (15.96%) | 29 (24.36%) | 24 (20.16%) |
| Type of Intervention | ||||||||
| Workshops | 32 (35.16%) | 24 (37.50%) | 6 (33.33%) | 18 (40%) | 1 (20%) | 7 (36.84%) | 10 (34.48%) | 4 (16.66%) |
| Short course | 15 (16.48%) | 9 (14.06%) | 1 (5.55%) | 6 (13.33%) | 3 (60%) | 2 (10.52%) | 3 (10.34%) | 4 (16.66%) |
| Seminar series | 15(16.48%) | 9 (14.06%) | 3 (16.66%) | 10 (22.22%) | 0 | 3 (15.78%) | 3 (10.34%) | 3 (12.5%) |
| Mentorship | 2 (2.19%) | 3 (4.68%) | 1 (5.55%) | 0 | 0 | 0 | 3 (10.34%) | 3 (12.5%) |
| Fellowship | 2 (2.19%) | 1 (1.56%) | 1 (5.55%) | 1 (2.22%) | 0 | 1 (5.26%) | 3 (10.34%) | 1 (4.16%) |
| Longitudinal program | 20 (21.97%) | 17 (26.56%) | 6 (33.33%) | 9 (20%) | 1 (20%) | 6 (31.57%) | 6 (20.68%) | 9 (37.5%) |
| Other | 5 (5.49%) | 1 (1.56%) | 0 | 1 (2.22%) | 0 | 0 | 1 (3.44%) | 0 |
| Study design | ||||||||
| Single group | 58 (63.73%) | 37 (57.81%) | 7 (38.88%) | 26 (57.77%) | 3 (60%) | 9 (47.36%) | 16 (55.17%) | 15 (62.5%) |
| Cohort study | 19 (20.87%) | 17 (26.56%) | 7 (38.88%) | 12 (26.66%) | 1 (20%) | 7 (36.84%) | 9 (31.03%) | 6 (25%) |
| Nonrandomised controlled study | 11 (12.08%) | 9 (14.06%) | 4 (22.22%) | 6 (13.33%) | 1 (20%) | 3 (15.78%) | 4 (13.79%) | 3 (12.5%) |
| Randomized controlled study | 3 (3.29%) | 1 (1.56%) | 0 | 1 (2.22%) | 0 | 0 | 0 | 0 |
| Qualitative methodology | 1 (1.09%) | 1 (1.56%) | 0 | 0 | 0 | 0 | 0 | 1 (4.16%) |
| Mixed methodology | 11 (12.08%) | 9 (14.06%) | 2 (11.11%) | 7 (15.55%) | 2 (40%) | 1 (5.26%) | 6 (20.68%) | 5 (20.83%) |
| Type of Data | ||||||||
| Self-reported | 50 (54.94%) | 35 (54.68%) | 9 (50%) | 23 (51.11%) | 2 (40%) | 10 (52.63%) | 18 (62.06%) | 13 (54.16%) |
| Objective | 3 (3.29%) | 2 (3.12%) | 1 (5.55%) | 5 (11.11%) | 0 | 0 | 0 | 0 |
| Self-reported, Objective | 38 (41.75%) | 27 (42.18%) | 8 (44.44%) | 17 (37.77%) | 3 (60%) | 9 (47.36%) | 11 (37.93%) | 11 (45.83%) |
| Level of outcomes | ||||||||
| Level 1 | 70 (76.92%) | 53 (82.81%) | 14 (77.77%) | 35 (77.77%) | 4 (80%) | 17 (89.47%) | 23 (79.31%) | 18 (75%) |
| Level 2A | 68 (74.72%) | 56 (87.50%) | 15 (83.33%) | 35 (77.77%) | 5 (100%) | 15 (78.94%) | 21 (72.41%) | 21 (87.5%) |
| Level 2B | 76 (83.51%) | 53 (82.81%) | 15 (83.33%) | 40 (88.88%) | 4 (80%) | 18 (94.73%) | 26 (89.65%) | 20 (83.33%) |
| Level 3 | 47 (51.64%) | 31 (48.43%) | 10 (55.55%) | 28 (62.22%) | 2 (40%) | 12 (63.15%) | 17 (58.62%) | 14 (58.33%) |
| Level 4A | 17 (18.68%) | 13 (20.31%) | 7 (38.88%) | 9 (20%) | 2 (40%) | 7 (36.84%) | 9 (31.03%) | 7 (29.16%) |
| Level 4B | 4 (4.39%) | 2 (3.12%) | 1 (5.55%) | 1 (2.22%) | 0 | 0 | 1 (3.44%) | 1 (4.16%) |
The teacher as an information provider and coach
With reference to Harden’s domains, the one most covered by the faculty development programs is an information provider and coach, which can be identified in 91 studies [13–103]. Pharmacy, nursing, medical, and dental faculty as well as basic science and clinical science teachers from different departments participated in these studies. The majority of outcomes reported were at level 2B (83.51%). The majority of faculty development programs led to significant increases in faculty members’ cognitive knowledge and skills of different aspects of the teaching-learning process and coaching such as educational concepts and principles, teaching strategies, methods and techniques. Participants also reported an improvement in their teaching and coaching skills such as teaching communication skills, clinical teaching, office-based teaching, giving effective feedback and promoting reflection.
The teacher as a facilitator of learning and mentor
Sixty four of faculty development programs focused on the domain of facilitator of learning and mentor [13, 16, 18, 23–27, 29, 30, 32, 37–42, 44, 45, 47–50, 52–62, 64, 66, 67, 69–73, 77, 78, 81–83, 85–88, 90, 93, 96, 97, 99, 100, 102–108]. Studies included faculty participants in medicine, nursing, pharmacy and dentistry and as well as basic science and clinical science teachers from different departments. The majority of outcomes reported were at level 2A (87.50%). Most programs led to self-reported changes in participants’ attitudes about and perceptions of teaching, learning and mentoring.
The teacher as a curriculum developer and implementer
Eighteen of faculty development programs focused on the domain of curriculum developer and implementer [14, 25, 44, 52–54, 58, 61, 79, 81, 83, 84, 87, 93, 100, 106, 109, 110]. Participants in these studies included community-based physician faculty, critical care faculty, academic podiatric physicians and faculty in medicine, nursing, pharmacy, dentistry, psychology, nutrition, audiology, physical therapy and occupational therapy as well as faculty from seven surgical and related disciplines and five medical subspecialties. The majority of outcomes reported were at level 2A and level 2B (83.33% each). Most programs led to significant changes in participants’ confidence for a wide range of academic skills such as curriculum design.
The teacher as an assessor and diagnostician
Forty-five of faculty development programs focused on the domain of assessor and diagnostician [15, 18, 20, 23, 27, 32, 37, 39, 40, 44, 47, 49, 52–59, 61, 67, 70, 72, 75, 77–79, 81, 83, 85, 87, 90, 93, 100, 102–104, 111–117]. Faculty from the schools of medicine, nursing, pharmacy and dentistry as well as faculty members from the departments of basic, clinical and allied sciences participated in these studies. The majority of outcomes reported were at level 2B (88.88%). The majority of faculty development programs led to significant increases in faculty members’ cognitive knowledge and skills of different aspects of assessment of students’ learning such as development of MCQs, giving effective feedback and workplace-based assessment.
The teacher as a role model
Five of faculty development programs focused on the domain of role model [70, 90, 93, 105, 118]. University-based and community-based general medicine faculty and as well as a mix of medical educators from multiple schools participated in these studies. The majority of outcomes reported were at level 2A (100%). Changes in attitudes and perceptions attributable to the educational program were infrequently noted.
The teacher as a manager and leader
Nineteen of faculty development programs focused on the domain of manager and leader [18, 23–25, 40, 49, 51–53, 58, 61, 65, 87, 90, 100, 106, 119–121]. Faculty from the colleges of medicine, dentistry, nursing and pharmacy and as well as basic science teachers from different departments and clinical teachers in family medicine, general pediatrics, and general internal medicine participated in these studies. The majority of outcomes reported were at level 2B (94.73%). The majority of faculty development programs led to significant increases in faculty members’ cognitive knowledge and skills of different aspects of the educational leadership and management such as time management, change management, small-group leadership, leadership and management of work teams, educational leadership and hospital administration and management. Participants also reported an improvement in their clinical leadership skills and financial skills.
The teacher as a scholar and researcher
Twenty nine of faculty development programs focused on the domain of scholar and researcher [14, 21, 24, 25, 27, 29, 47, 51–54, 58, 61, 80, 83, 84, 87, 100, 106, 112, 122–130]. Participants in these studies included faculty from the schools of medicine, dentistry, nursing and pharmacy and as well as entry level medical teachers and junior/mid-career clinical teachers in family medicine, general pediatrics, critical care and general internal medicine. The majority of outcomes reported were at level 2B (89.65%). The majority of faculty development programs led to significant improvement in participants’ self-reported knowledge and skills of different domains of the educational research and scholarship of teaching and learning, such as research design, critical appraisal of the literature, scientific writing, writing grant applications and evidence-based medicine (EBM). Participants also reported an improvement in their technology/informatics skills (e.g., search MEDLINE, use filters while searching, read journals on-line).
The teacher as a professional
Twenty four of faculty development programs focused on the domain of professional [16, 18, 25, 27, 29, 32, 34, 52, 54, 58, 61, 73, 76, 82, 83, 90, 100, 105–107, 118, 123, 129, 131]. A mix of professions, including medicine, nursing, pharmacy, dentistry, physical therapy, occupational therapy and speech-language pathology as well as junior/mid-career clinical faculty members and community-based physician faculty participated in these studies. The majority of outcomes reported were at level 2A (87.5%). Self-reported changes in attitudes included greater enthusiasm and motivation for lifelong learning, development or strengthening of responsibility for teaching, and an increased sense of community and collegiality. Participants also reported an increased understanding of individual professional development, career development, professional responsibility and interpersonal relationships.
-
(d)
Quality appraisal of the studies
The quality of the studies was appraised using the Medical Education Research Study Quality Instrument (MERSQI). The overall methodological quality of studies was moderate. Total MERSQI scores amongst the 119 studies ranged from 7 to 16, with a mean (standard deviation) of 11.32 (0.74).
Study design
The majority of studies (n = 72, 60.5%) used a single-group with a pre- and post- test design, with the addition of a delayed post-test in some programs. Forty three (36.13%) studies out of 119 were nonrandomized study with pre-test post-test design and there were four (3.36%) randomized controlled trials. Of the 119 articles reviewed, two authors employed a qualitative methodology only, though 19 (15.96%) researchers used a mixed methodology in their work.
Sampling (institutions)
Although in most programs (n = 74, 62.18%), participants were from one institution, four studies were designed for the faculty of two institutions. In 41 studies, faculty from 3 or more institutions participated in the programs.
Sampling (response rate)
In most programs (nearly 80% of programs), the response rate was ≥ 75%. Nearly 14.5% of studies (n = 17) had a response rate ranging from 50 to 74%. Seven studies reported a response rate of less than 50%.
Type of data
More than half of the studies (51.26%) used participants’ self-report data to assess program outcomes. In 58 studies, in addition to self-reported data, objective data sources (e.g., expert opinion, student or resident ratings, student exam scores, retention rates, or success in promotion/tenure, engagement index, CV review) were also used.
Validity evidence for evaluation instrument scores
Of the 119 articles reviewed, fifty eight (nearly 49% of the studies) did not measure a psychological construct. Forty three studies (nearly 36% of the reviewed publications) reported relevant content evidence included using theory, guidelines, experts, and existing instruments to identify or refine the instrument. In 11 studies, in addition to validity evidence for content, relevant internal structure evidence included all reliability (internal consistency, interrater, interstation, and test–retest) and factor analysis were reported. Moreover, seven studies reported relevant evidence of relationships to other variables included concurrent or predictive correlation with other variables.
Data analysis (sophistication)
Although fifteen studies used descriptive analysis only, in 104 studies, in addition to descriptive analyses (e.g., frequency, mean, and median), statistical inference tests were also used.
Data analysis (appropriate)
In most studies (nearly 93.5% of the reviewed articles), data analysis was appropriate for study design and type of data.
Outcome
In previous section (section b), we reviewed all included studies to determine which level of outcomes were assessed.
Discussion
This review, which focused on faculty development programs designed to prepare faculty members for their various roles in health sciences education, included 119 articles published over a 30-year period. In this review, we searched the empirical health professions faculty development studies, both national and international, to determine the types and outcomes of faculty development programs designed to prepare faculty members for their various roles based on the Harden teacher’s role framework model and to identify, or explain, to which of the areas described by Harden and Crosby the authors are referring. In this section, first, we discussed the results of the review based on the research questions outlined in this paper. Next, we recommended several implications for future practice and research in the field. Finally, the authors presented the strengths and limitations of the review.
Responses to review questions
In response to the first question of review, what are the types and duration of faculty development programs designed to prepare faculty members for their various roles in health sciences education, reviewers observed that the majority of faculty development programs were workshops with various durations, followed by longitudinal programs, short courses and seminar series. In considering the different approaches to faculty development illustrated by Steinert [132], it appears that the majority of faculty development programs in this review were conducted through formal approaches and occurred mostly in groups. This means that it has been less focused on the informal faculty development activities and as well as formal, individualized form of faculty development programs (e.g., peer coaching, peer & student feedback, and online learning). Although our review of findings by intervention type is consistent with previous literature reviews [6, 7, 9, 10, 133], it has recently been suggested that faculty developers incorporate more informal faculty development approaches (e.g., role modeling, reflection, and learning from peers) into the design and delivery of faculty development programs [134–136]. In one study [135], researchers identified three everyday educational practices (applying evidence to educational practice; and evaluating and sharing educational practice) that provide opportunities for informal faculty development for health professions educators in the academic setting. Providing informal learning opportunities in authentic contexts, can also lead to a community of practice [137]. As O’Sullivan and Irby [138] have noted, it would be timely to consider the role of workplace learning and communities of practice in investigating the effectiveness of faculty development programs and activities.
In our review, the duration of faculty development programs varied depending on the type of intervention and ranged from 20 min to six years. Interestingly, reviewers observed a notable shift in the length and format of faculty development programs (from one-time workshops to longitudinal programs such as teaching scholars programs, seminar series, fellowships and mentorship programs). As Gruppen [139] noted, intensive longitudinal programs are not only an investment in faculty; they are an investment in institutional health. The dynamic nature of aligning the goals of an intensive longitudinal program with the institution can promote educational leadership and scholarly productivity, and build a sense of community in the workplace.
In general, given the key features of effective faculty development (the role of experiential and authentic learning, the value of feedback and reflection, the importance of peers as role models and as providers of collegial support and the value of extended programs) highlighted in the literature [5, 7], it is time to reflect on the length and format of faculty development programs.
In response to the second question of review, which of the areas, or faculty, roles, described by Harden and Crosby are the authors referring to, our findings showed that the majority of authors focused on the role of the teacher as an information provider and coach. Moreover, the domains of facilitator of learning and mentor and assessor and diagnostician are of interest for authors in the faculty development field. A much smaller number focused on the roles that faculty development programs can play in the preparation of faculty members for their roles as scholar and researcher and professional. Few articles focused on the roles of faculty members as manager and leader as well as curriculum developer and implementer. Only five faculty development programs emphasized on the role of the teacher as a role model. These findings mean that although we have seen a growth in the domains of faculty development programs, specifically in faculty development for research and scholarship, as well as leadership development, this growth has not been balanced and the majority of faculty development programs still tend to focus on enhancing the traditional role of faculty members as transmitters of information or lecturers. Clearly, focusing on the role of faculty members as role models merits further development and inquiry. Although reasons for this unbalanced growth may vary, including an emphasis on teaching effectiveness in teacher evaluation systems, focus on knowledge and skill acquisition rather than the formation – or development of – faculty members’ professional identity, overemphasis on faculty perceived or self-identified needs, institutional policies, as well as limited resources for faculty development programs, the need to expand the areas of faculty development programs remains acute. As highlighted by Steinert [2], it is time for us to broaden the scope of faculty development programs from teaching to academic development and intentionally design new programs targeting all of the roles that faculty members play. As implied at the outset, and as a number of authors have proposed [4, 140–143], utilizing a competency-based framework for faculty development (e.g. Harden teacher’s role framework) can play an important role in expanding our approaches to faculty development programs and would help to inform both content and desired outcomes [2]. Moving forward, it would be worthwhile to consider these frameworks in the design and evaluation of faculty development programs.
In response to the third question of review, we discussed the outcomes of faculty development programs based on the Harden teacher’s role framework described in Fig. 1 in Appendix 3 (see Additional file 4). Our findings showed that the majority of outcomes reported are at level 2B, level 1 and level 2A. This means that there were an overwhelming number of positive changes in participants’ attitudes, knowledge and skills in all eight domains of faculty roles following participation in faculty development programs, which suggests that faculty development programs were beneficial. The impact on the organizational practice as well as the impact on participants’ students, residents or colleagues continued to be underexplored, which may be disappointing. Outcomes of this review are consistent with Steinert, study in 2016 [6], where the major outcome was teaching performance.
Implications for future practice
Based on the review findings, we recommend the following suggestions for future practice:
-
Utilizing a competency-based framework for developing a comprehensive faculty development program
Although we have seen a growth in the domains of faculty development programs, this growth has not been balanced and the majority of faculty development programs have been designed independently of a curriculum for faculty members, often in response to perceived or self-identified needs. Moving forward, we should adopt a competency-based framework (e.g. Harden teacher’s role framework) to program development, implementation and evaluation. As mentioned previously, utilizing a competency-based framework for faculty development can be considered as a guide for designing and evaluating faculty development programs and would help to address all faculty members’ roles.
-
Broadening the scope of faculty development programs beyond the traditional roles of the faculty members
As stated earlier, there has been a steady growth in the scope of faculty development programs and our findings showed that the majority of faculty development programs covered more than one domain of faculty roles. Nevertheless, most of these programs continued to focus on enhancing the traditional role of faculty members as information providers and assessors, often in an academic setting. Given the expanding number of roles of faculty in the health professions, there is a critical need to broaden the scope of faculty development programs outside of the academic milieu to target all health professions teachers’ roles.
-
Incorporating more informal approaches into the design and delivery of faculty development programs
The majority of faculty development programs in this review were conducted through formal approaches and occurred mostly in groups. Whereas these formal, structured approaches such as workshops, short courses, seminars and other longitudinal programs are expected and reflect the growth of the field to incorporate more systematic planning and program design [6], informal approaches to faculty development that take advantage of experiential learning in authentic environments, which include learning by doing, by observing, and by reflecting on experience as well as workplace learning and learning in a community of practice, should be considered.
-
Attention to individualized form of faculty development programs
As mentioned above, the majority of faculty development programs in this review took place primarily in groups (e.g. workshops of varying duration, short courses, seminar series and other longitudinal programs). With a nod to social learning theories and the role of feedback in promoting change, faculty developers can develop faculty expertise through individual approaches to faculty development such as learning from experience, learning from peers and students, peer coaching and online learning.
-
Moving fromworkshop-based teaching to workplace learning
In this review, faculty development programs were most commonly delivered through workshops that were not situated in the workplace, requiring participants to take their ‘lessons learned’ back to their own contexts. Given the challenges of using this approach for faculty development in the health professions in an ever-changing (and complex) environment, including integrating strategies to promote transfer to the workplace, this trend should be changed. Clearly, a re-orientation of activities from the workshop to the authentic environments such as workplace can increase participation, motivation, and access [2]. Moreover, by moving to the workplace and taking advantage of working together and participating in the activities of a larger community, faculty can build new knowledge and develop new approaches to challenges encountered in teaching and practice [144].
-
Fostering intensive longitudinal programs
We observed a notable shift in the length and format of faculty development programs (from one-time workshops to longitudinal programs such as teaching scholars programs, seminar series, fellowships and mentorship programs). Longitudinal programs that extend over time, have the potential to produce outcomes not apparent in one-time interventions. It is also not surprising that brief, one-time interventions are unlikely to have a significant impact on role modeling or reflective practice [134]. Given the multiple benefits of longitudinal approaches to faculty development noted in this review, other approaches that complement longitudinal programs included certificate programs and advanced degrees are needed.
-
Promoting role modeling and reflective practice
Although role modeling and reflective practice are important elements in all faculty roles [134], only 5% of faculty development programs in this review focused on the domain of role model. Faculty development for role modeling necessitates an awareness of the power of this teaching and learning strategy, attention to personal and professional behaviors, and a focus on the environment in which professional practice unfolds. Reflective practice is closely tied to role modeling and increased reflection enhances role modeling in all faculty roles [145]. Providing opportunities for feedback and reflection, which allowed participants to reflect on their practices, values, and beliefs, can promote role modelling.
-
Moving from focusing on knowledge and skill acquisition to the formation – or development of – faculty members’ professional identity
In this review, most faculty development programs focused on knowledge and skill acquisition rather than the formation – or support of – faculty members’ professional identity. As professional identity can have a powerful impact on academic and career development, academic roles and responsibilities, and professional development opportunities [146], we should strengthen identity through faculty development activities such as building opportunities for community building and networking; promoting reflection; and capitalizing on mentorship.
-
Moving from measurement of outcomes at the individual level to the organizational level
The current literature demonstrates a continuing overreliance on measurement of outcomes at the individual level (changes in cognitive learning or performance). As faculty development can play an important role in promoting organizational change and development, we need more programs to report on changes in organizational systems, as well as changes in student (or resident) behavior.
Implications for future research
To build upon and complement existing research, we suggest the following recommendations for future faculty development studies:
-
Conducting more rigorous research designs, incorporating control or comparison groups or time series studies
As mentioned previously, the overall methodological quality of included studies was moderate and the majority of studies continued to employ a single-group with a pre- and post- test design. There is a need for more rigorous research designs and a greater use of control or comparison groups or time series studies to assess the impact of the faculty development intervention.
-
Make more deliberate use of qualitative methodologies and mixed methods approaches
Of the 119 articles reviewed, two authors employed a qualitative methodology only, though 19 researchers used a mixed methodology in their work. We need to conduct more qualitative and mixed methods studies to capture the complexity of faculty development interventions, as well as, to better understand the process of change, both as a result of the intervention and within the individual and the organization.
-
Using a more robust approach to data collection to assess program outcomes
This review demonstrates a continuing overreliance on participants’ self-report data and survey questionnaires to assess program outcomes. Moreover, nearly 49% of the studies did not measure psychometric properties. Moving forward, researchers should consider greater use of novel assessment methods for assessing behavioral and organizational changes. They also should use validated measures, or report validity evidence for evaluation instruments that are used. It would also be important to collect data over time, to better understand the long-term retention of outcomes.
-
Assessing change and the transfer of knowledge to practice over time
Although a number of studies used delayed post-tests for assessing the maintenance of change over time, there is a need for more studies to explore further the durability of change, those supports which help to sustain it, and the value of specific activities such as ‘booster’ sessions or other follow-up activities.
-
Exploring the impact of faculty development programs on the organizational development and change in a more rigorous and systematic fashion
As mentioned previously, most of the literature to date focuses on measurement of outcomes at the individual level (changes in cognitive learning or performance). To move forward, more studies is needed to observe the potential impact of faculty development programs on the organizational change. Such studies will help us to better understand the benefits of faculty development in producing organizational change.
-
Carry out process-oriented studies in addition to outcome-oriented ones
As we observed, most of the literature to date focuses on measurement of outcomes. There is a need for more qualitative studies to better understand how change occurs in faculty development, both as a result of the intervention and within the individual and the organization.
-
Grounding faculty development studies in theoretical foundation
Moving forward, we should adopt a sound theoretical basis for our research studies. We should also utilize theory in the interpretation of our results. From the perspective of external validity, it is critical that researchers base their studies on theoretical foundation.
-
Exploring the impact of faculty development programs in a single field of health sciences education
This systematic review included empirical health professions faculty development studies that assessed the impact of faculty development programs in all disciplines of health sciences. A more precise and dedicated analysis could have been the review and quantitative and qualitative synthesis of studies on only one of the disciplines of health sciences. This might be a future effort that can explicitly explore the impact of faculty development programs in a single field of health professions education.
Strengths and limitations of the review
As noted in background, a major strength of this review is that our study is the first systematic review of faculty development programs designed to prepare faculty members for their various roles in health sciences education based on the Harden teachers’ role framework model. The use of a structured Coding Sheet, which was developed from previous systematic review work [7], was an additional strength. In addition, we appraised the quality of the studies using a reliable tool for appraising methodological quality of medical education research, the Medical Education Research Study Quality Instrument (MERSQI). Moreover, we used the modified Kirkpatrick model to assess the educational outcomes of faculty development programs. It is also noteworthy that the search process was extensive and in addition to international databases, national databases were also searched from 1990 to 2020.
There are some limitations to this study. A potential limitation of this study was the exclusion of program reports, dissertations and empirical studies with post-test design only from this review. Furthermore, articles not written in the English or Persian language were excluded. This means that this review may have been influenced by publication bias that prevents a fuller picture of faculty development from an international perspective. Negative results are also rarely reported, reflecting another possible publication bias towards positive results. It should also be noted that a complex search strategy in a field such as this one, where the terminology is still inconsistent across international and professional boundaries [7], created numerous challenges during the search process. Despite the rigorous process we undertook to achieve consensus, inter-rater reliability and agreement on the Coding Sheet was a challenge throughout the review process. Finally, the nature of the articles reviewed presented a number of challenges. For example, authors frequently omitted validity evidence for evaluation instruments that are used. In addition, an inconsistent use of terminology (e.g., to describe program types or study designs) often led to conflicting interpretations of the same information.
Conclusion
In this review, we searched the empirical health professions faculty development studies published over a 30-year period, both national and international, to determine the types and outcomes of faculty development programs designed to prepare faculty members for their various roles based on the Harden teacher’s role framework model and to identify, or explain, to which of the areas described by Harden and Crosby the authors are referring. We observed a significant growth in faculty development programs world-wide. The majority of faculty development programs in this review were conducted through formal approaches and occurred mostly in groups (e.g., workshops with various durations, longitudinal programs, short courses and seminar series). Reviewers observed a notable shift in the length and format of faculty development programs (from one-time workshops to longitudinal programs such as teaching scholars programs, seminar series, fellowships and mentorship programs). Although we have seen a growth in the domains of faculty development programs, specifically in faculty development for research and scholarship, as well as leadership development, this growth has not been balanced and the majority of faculty development programs still tend to focus on enhancing the traditional role of faculty members as transmitters of information or lecturers. There were an overwhelming number of positive changes in participants’ attitudes, knowledge and skills in all eight domains of faculty roles following participation in faculty development programs, which suggests that faculty development programs were beneficial. The impact on the organizational practice as well as the impact on participants’ students, residents or colleagues continued to be underexplored, which may be disappointing. Lastly, based on the review findings, we recommended several implications for future practice and research in the field.
Supplementary Information
Additional file 1: Appendix 1. A copy of the search strategy used within MEDLINE/PubMed database.
Additional file 2: Appendix 2. The Coding Sheet.
Additional file 3: Table S1. Summary of included studies.
Additional file 4: Appendix 3. The study findings based on the Harden teacher’s role framework.
Acknowledgements
The review was a part of a doctoral dissertation performed to fulfil the requirements of a Ph.D. program in medical education at Isfahan University of Medical Sciences and Health Services. We gratefully acknowledge the Isfahan University of Medical Sciences and Health Services for financial support.
Abbreviations
- BEME
Best Evidence Medical Education
- CV
Curriculum Vitae
- EBM
Evidence-based Medicine
- ED
Emergency Department
- ERIC
Education Resources Information Center
- IPE
Interprofessional Education
- MCQs
Multiple-Choice Questions
- MERSQI
Medical Education Research Study Quality Instrument
- mini-CEX
Mini-Clinical Evaluation Exercise
- OSTE
Objective Structured Teaching Exercise
- PBL
Problem-Based Learning
- Ph.D.
Doctor of Philosophy
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- QI
Quality Improvement
- RN/MD
Registered Nurse/ Medical Doctor
- SID
Scientific Information Database
Authors’ contributions
The study screening was done by MK, NY and TC in three stages: by title, then by abstract, and finally by full text review. After removing duplicates by MK, title and abstract screening was undertaken independently by MK and NY with disagreements between them resolved by consensus. TC was recruited to facilitate agreement when needed. Full-text screening was carried out by MK or NY based on pre-determined eligibility criteria with any studies deemed ineligible cross-checked by TC. MK wrote the article. NY and TC reviewed and edited the article. All authors have read and approved the final version.
Funding
This study was funded by Isfahan University of Medical Sciences and Health Services. No funding bodies had any role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Availability of data and materials
All data generated or analysed during this review are included in this published article and its additional files.
Declarations
Ethics approval and consent to participate
The study was approved by the Institutional Research Ethics Committee of Medical University of Isfahan.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Steinert Y, Mann KV. Faculty development: principles and practices. J Vet Med Educ. 2006;33(3):317–324. doi: 10.3138/jvme.33.3.317. [DOI] [PubMed] [Google Scholar]
- 2.Steinert Y. Faculty development: from rubies to oak. Med Teach. 2020;42(4):429–435. doi: 10.1080/0142159X.2019.1688769. [DOI] [PubMed] [Google Scholar]
- 3.Wilkerson L, Irby DM. Strategies for improving teaching practices: a comprehensive approach to faculty development. Acad Med. 1998;73(4):387–396. doi: 10.1097/00001888-199804000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Harden RM, Crosby J. AMEE guide no 20: the good teacher is more than a lecturer - the twelve roles of the teacher. Med Teach. 2000;22(4):334–347. doi: 10.1080/014215900409429. [DOI] [Google Scholar]
- 5.McLean M, Cilliers F, Van Wyk J. Faculty development: yesterday, today and tomorrow. Med Teach. 2008;30(6):555–584. doi: 10.1080/01421590802109834. [DOI] [PubMed] [Google Scholar]
- 6.Steinert Y, Mann K, Anderson B, Barnett BM, Centeno A, Naismith L, Prideaux D, Spencer J, Tullo E, Viggiano T, et al. A systematic review of faculty development initiatives designed to enhance teaching effectiveness: a 10-year update: BEME Guide No. 40. Med Teach. 2016;38(8):769–786. doi: 10.1080/0142159X.2016.1181851. [DOI] [PubMed] [Google Scholar]
- 7.Steinert Y, Mann K, Centeno A, Dolmans D, Spencer J, Gelula M, Prideaux D. A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8. Med Teach. 2006;28(6):497–526. doi: 10.1080/01421590600902976. [DOI] [PubMed] [Google Scholar]
- 8.Johnston C, Ganas J, Jeong YN, Nevius A, Bassir SH, Dragan IF. Faculty development initiatives in academic dentistry: a systematic review. J Dent Educ. 2019;83(9):1107–1117. doi: 10.21815/JDE.019.096. [DOI] [PubMed] [Google Scholar]
- 9.Bilal, Guraya SY, Chen S. The impact and effectiveness of faculty development program in fostering the faculty's knowledge, skills, and professional competence: A systematic review and meta-analysis. Saudi J BiolSci. 2019;26(4):688–697. doi: 10.1016/j.sjbs.2017.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Behar-Horenstein LS, Kuang H, Tolentino LA, Zhang H. Faculty development in the health professions: a review of the literature. J Fac Dev. 2019;33(2):77–95. [Google Scholar]
- 11.Cook DA, Reed DA. Appraising the quality of medical education research methods: the Medical Education Research Study Quality Instrument and the Newcastle-Ottawa Scale-Education. Acad Med. 2015;90(8):1067–1076. doi: 10.1097/ACM.0000000000000786. [DOI] [PubMed] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shields HM, Guss D, Somers SC, Kerfoot BP, Mandell BS, Travassos WJ, Ullman SM, Maroo S, Honan JP, Raymond LW, et al. A faculty development program to train tutors to be discussion leaders rather than facilitators. Acad Med. 2007;82(5):486–492. doi: 10.1097/ACM.0b013e31803eac9f. [DOI] [PubMed] [Google Scholar]
- 14.Batsche CN, Monoson PK. A four-phase multidisciplinary faculty development model in aging. Educ Gerontol. 1993;19(6):551–567. doi: 10.1080/0360127930190607. [DOI] [Google Scholar]
- 15.Christie C, Bowen D, Paarmann C. Effectiveness of faculty training to enhance clinical evaluation of student competence in ethical reasoning and professionalism. J Dent Educ. 2007;71(8):1048–1057. doi: 10.1002/j.0022-0337.2007.71.8.tb04371.x. [DOI] [PubMed] [Google Scholar]
- 16.Blatt B, Plack MM, Simmens SJ. Preparing interprofessional faculty to be humanistic mentors for medical students: the GW-gold mentor development program. J Continuing Educ Health Professions. 2018;38(2):117–125. doi: 10.1097/CEH.0000000000000203. [DOI] [PubMed] [Google Scholar]
- 17.Sherbino J, Frank J, Lee C, Bandiera G. Evaluating ED STAT! A novel and Effective Faculty Development Program to Improve Emergency Department teaching. Acad Emerg Med. 2006;13(10):1062–1069. doi: 10.1197/j.aem.2006.05.025. [DOI] [PubMed] [Google Scholar]
- 18.Cole KA, Barker LR, Kolodner K, Williamson P, Wright SM, Kern DE. Faculty Development in Teaching skills: an intensive longitudinal model. Acad Med. 2004;79(5):469–480. doi: 10.1097/00001888-200405000-00019. [DOI] [PubMed] [Google Scholar]
- 19.Evans KH, Bereknyei S, Hikoyeda N, Tzuang M, Braddock CH. The impact of a faculty development program in health literacy and ethnogeriatrics. Acad Med. 2014;89(12):1640–1644. doi: 10.1097/ACM.0000000000000411. [DOI] [PubMed] [Google Scholar]
- 20.Quirk ME, DeWitt T, Lasser D, Huppert M, Hunniwell E. Evaluation of primary care futures: a faculty development program for community health center preceptors. Acad Med. 1998;73(6):705–707. doi: 10.1097/00001888-199806000-00019. [DOI] [PubMed] [Google Scholar]
- 21.Manwell LB, Pfeifer J, Stauffacher EA. An interdisciplinary faculty development model for the prevention and treatment of Alcohol Use Disorders. Alcoholism: Clin Experimental Res. 2006;30(8):1393–1399. doi: 10.1111/j.1530-0277.2006.00166.x. [DOI] [PubMed] [Google Scholar]
- 22.Lye P, Heidenreich C, Wang-Cheng R, Bragg D, Simpson D. Experienced clinical educators improve their clinical teaching effectiveness. Ambul Pediatr. 2003;3(2):93–97. doi: 10.1367/1539-4409(2003)003<0093:ECEITC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 23.Roberts KB, Devries JM. APA/HRSA National Faculty Development scholars Program: community-based teaching track. Ambul Pediatr. 2004;4(1 SUPPL):92–97. doi: 10.1367/1539-4409(2004)004<0092:HNFDSP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 24.Simpson DE, Bragg D, Biernat K, Treat R. Outcomes results from the evaluation of the APA/HRSA Faculty scholars Program. Ambul Pediatr. 2004;4(1 SUPPL):103–112. doi: 10.1367/1539-4409(2004)004<0103:ORFTEO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 25.Walsh DS, Lazorick S, Lawson L, Lake D, Garrison HG, Higginson J, Vos P, Baxley E. The Teachers of Quality Academy: evaluation of the effectiveness and impact of a Health Systems Science Training Program. Am J Med Qual. 2019;34(1):36–44. doi: 10.1177/1062860618778124. [DOI] [PubMed] [Google Scholar]
- 26.Skeff KM, Stratos GA, Bergen MR, Sampson K, Deutsch SL. Regional teaching improvement programs for community-based teachers. Am J Med. 1999;106(1):76–80. doi: 10.1016/S0002-9343(98)00360-X. [DOI] [PubMed] [Google Scholar]
- 27.Mitcham MD, Lancaster CJ, Stone BM. Evaluating the effectiveness of occupational therapy faculty development workshops. Am J Occup Ther. 2002;56(3):335–339. doi: 10.5014/ajot.56.3.335. [DOI] [PubMed] [Google Scholar]
- 28.Assemi M, Mutha S, Hudmon KS. Evaluation of a train-the-trainer program for cultural competence. Am J Pharm Educ. 2007;71(6):110. doi: 10.5688/aj7106110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Haines SL, Popovich NG. Engaging external senior faculty members as faculty mentors. Am J Pharm Educ. 2014;78(5):1–6. doi: 10.5688/ajpe785101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.LeBlanc JM, Pruchnicki MC, Rohdieck SV, Khurma A, Dasta JF. An instructional seminar for online case-based discussions. Am J Pharm Educ. 2007;71(3):42. doi: 10.5688/aj710342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee KC, Ma JD, Hudmon KS, Kuo GM. A train-the-trainer approach to a shared pharmacogenomics curriculum for US colleges and schools of pharmacy. Am J Pharm Educ. 2012;76(10):1–8. doi: 10.5688/ajpe7610193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Popovich NG, Peverly SL, Jackson TR. Effectiveness of a weekly faculty conversation forum about teaching. Am J Pharm Educ. 2006;70(5):1–7. doi: 10.5688/aj7005107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stein SM, Fujisaki BS, Davis SE, MacLean LG. A 1-day course to improve the teaching effectiveness of health professions faculty members. Am J Pharm Educ. 2012;76(1):1–9. [DOI] [PMC free article] [PubMed]
- 34.Shealy SC, Worrall CL, Baker JL, Grant AD, Fabel PH, Walker CM, Ziegler B, Maxwell WD. Assessment of a faculty and preceptor development intervention to foster self-awareness and self-confidence. Am J Pharm Educ. 2019;83(7):1534–1546. doi: 10.5688/ajpe6920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Paige JT, Arora S, Fernandez G, Seymour N. Debriefing 101: training faculty to promote learning in simulation-based training. Am J Surg. 2015;209(1):126–131. doi: 10.1016/j.amjsurg.2014.05.034. [DOI] [PubMed] [Google Scholar]
- 36.Wong JG, Son D, Miura W. Cross-cultural Interprofessional Faculty Development in Japan: results of an Integrated Workshop for Clinical teachers. Am J Med Sci. 2017;354(6):597–602. doi: 10.1016/j.amjms.2016.09.007. [DOI] [PubMed] [Google Scholar]
- 37.Gardner AK, Timberlake MD, Dunkin BJ. Faculty Development for the operating room: an examination of the effectiveness of an intraoperative teaching course for surgeons. Ann Surg. 2019;269(1):184–190. doi: 10.1097/SLA.0000000000002468. [DOI] [PubMed] [Google Scholar]
- 38.Davis BP, Clevenger CK, Posnock S, Robertson BD, Ander DS. Teaching the teachers: Faculty development in inter-professional education. Appl Nurs Res. 2015;28(1):31–35. doi: 10.1016/j.apnr.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 39.Skeff KM, Stratos GA, Berman J, Bergen MR. Improving clinical teaching. Evaluation of a national dissemination program. Arch Intern Med. 1992;152(6):1156–1161. doi: 10.1001/archinte.1992.00400180028004. [DOI] [PubMed] [Google Scholar]
- 40.Ebrahimi S, Kojuri J. Assessing the impact of faculty development fellowship in Shiraz University of Medical Sciences. Arch Iran Med. 2012;15(2):79–81. [PubMed] [Google Scholar]
- 41.Lye PS, Simpson DE, Wendelberger KJ, Bragg DS. Clinical teaching rounds. A case-oriented faculty development program. Arch Pediatr Adolesc Med. 1998;152(3):293–295. doi: 10.1001/archpedi.152.3.293. [DOI] [PubMed] [Google Scholar]
- 42.Junod Perron N, Nendaz M, Louis-Simonet M, Sommer J, Gut A, Cerutti B, Van Der Vleuten CP, Dolmans D. Impact of postgraduate training on communication skills teaching: a controlled study. BMC Med Educ. 2014;14(1):1–12. doi: 10.1186/1472-6920-14-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nasmith L, Franco ED. Minor surgical procedures: Faculty development workshop. Can Fam Phys. 1997;43:715–718. [PMC free article] [PubMed] [Google Scholar]
- 44.Lemoine JB, Chauvin SW, Broussard L, Oberleitner MG. Statewide interprofessional faculty development in simulation-based education for health professions. Clin Simul Nurs. 2015;11(3):153–162. doi: 10.1016/j.ecns.2014.12.002. [DOI] [Google Scholar]
- 45.Davis TS, Desselle SP. Perceptions of a faculty cohort using education scholar as a basis for faculty development in active learning strategies. Curr Pharm Teach Learn. 2013;5(5):394–401. doi: 10.1016/j.cptl.2012.06.001. [DOI] [Google Scholar]
- 46.Sturpe DA, Layson-Wolf C, Lynn McPherson M, Haines ST. An objective structured teaching examination (OSTE) for faculty development. Curr Pharm Teach Learn. 2013;5(6):616–619. doi: 10.1016/j.cptl.2013.07.015. [DOI] [Google Scholar]
- 47.Zagar M, Sampognaro L, Robertson C, Craft G. A description and opinions of a longitudinal book club for comprehensive pharmacy faculty development. Curr Pharm Teach Learn. 2019;11(9):909–914. doi: 10.1016/j.cptl.2019.05.005. [DOI] [PubMed] [Google Scholar]
- 48.Thampy H, Bond K. Sharing experiences of clinical teaching: an evaluation of contrasting workshops. Educ Prim Care. 2016;27(4):320–321. doi: 10.1080/14739879.2016.1165081. [DOI] [PubMed] [Google Scholar]
- 49.Skeff KM, Stratos GA, Bergen MR. Evaluation of a medical Faculty Development Program: a comparison of traditional Pre/Post and retrospective Pre/Post Self-Assessment ratings. Eval Health Prof. 1992;15(3):350–366. doi: 10.1177/016327879201500307. [DOI] [Google Scholar]
- 50.Delver H, Jackson W, Lee S, Palacios M. FM POD: an evidence-based blended teaching skills program for rural preceptors. Fam Med. 2014;46(5):369–377. [PubMed] [Google Scholar]
- 51.Gjerde CL, Kokotailo P, Olson CA, Hla KM. A Weekend Program Model for Faculty Development with Primary Care Physicians. Fam Med. 2004;36(SUPPL):110–114. [PubMed] [Google Scholar]
- 52.Morzinski JA, Simpson DE. Outcomes of a comprehensive faculty development program for local, full-time faculty. Fam Med. 2003;35(6):434–439. [PubMed] [Google Scholar]
- 53.Rust G, Taylor V, Herbert-Carter J, Smith QT, Earles K, Kondwani K. The morehouse faculty development program: evolving methods and 10-year outcomes. Fam Med. 2006;38(1):43–49. [PubMed] [Google Scholar]
- 54.Williams BC, Schigelone AR, Fitzgerald JT, Halter JB. Successful implementation of a faculty development program in geriatrics for non-primary care physician educators. Gerontol Geriatr Educ. 2008;28(3):5–27. doi: 10.1300/J021v28n03_02. [DOI] [PubMed] [Google Scholar]
- 55.Kuhnigk O, Schreiner J, Harendza S. Sustained change in didactic skills–does teacher training last? GMS Z Med Ausbild. 2013;30(3):Doc37. doi: 10.3205/zma000880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Garner SL, Killingsworth E, Bradshaw M, Raj L, Johnson SR, Abijah SP, Parimala S, Victor S. The impact of simulation education on self-efficacy towards teaching for nurse educators. Int Nurs Rev. 2018;65(4):586–595. doi: 10.1111/inr.12455. [DOI] [PubMed] [Google Scholar]
- 57.Salerno SM, Malley PGO, Pangaro LN, Wheeler GA, Moores LK, Jackson JL. Preceptor improve feedback in the ambulatory setting. J Gen Intern Med. 2002;17:779–787. doi: 10.1046/j.1525-1497.2002.11233.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kesselheim JC, Clayton CP, Fritz J, Smith RE, Gitlin SD, Reid E, Zuckerman KS, Kahn MJ. The American Society of Hematology (ASH) medical educators Institute: a pilot Faculty Development Project for Hematology Educators. J Cancer Educ. 2019;34(4):719–724. doi: 10.1007/s13187-018-1363-3. [DOI] [PubMed] [Google Scholar]
- 59.Mokkapati A, Mada P. Effectiveness of a teacher training workshop: an interventional study. J Clin Diagn Res. 2018;12(2):JC09–JC12. [Google Scholar]
- 60.Arnett M, Korte D, Richards PS, Saglik B, Taichman LS, Kinney JS, Gwozdek AE. Effect of Faculty Development activities on Dental Hygiene Faculty perceptions of and teaching about motivational interviewing: a pilot study. J Dent Educ. 2017;81(8):969–977. doi: 10.21815/JDE.017.048. [DOI] [PubMed] [Google Scholar]
- 61.Gates P, Ubu N, Smithey L, Rogers J, Haden NK, Rodriguez T, Albino JEN, Evans C, Zarkowski P, Weinstein G, et al. Faculty Development for Underrepresented Minority Dental Faculty and residents. J Dent Educ. 2013;77(3):276–291. doi: 10.1002/j.0022-0337.2013.77.3.tb05469.x. [DOI] [PubMed] [Google Scholar]
- 62.Johnstone-Dodge V, Bowen DM, Calley KH, Peterson TS. A Faculty Development Course to Enhance Dental Hygiene Distance Education: a pilot study. J Dent Educ. 2014;78(9):1319–1330. doi: 10.1002/j.0022-0337.2014.78.9.tb05804.x. [DOI] [PubMed] [Google Scholar]
- 63.McAndrew M, Eidtson WH, Pierre GC, Gillespie CC. Creating an objective structured teaching examination to evaluate a Dental Faculty Development Program. J Dent Educ. 2012;76(4):461–471. doi: 10.1002/j.0022-0337.2012.76.4.tb05278.x. [DOI] [PubMed] [Google Scholar]
- 64.McAndrew M, Motwaly S, Kamens TE. Long-term Follow-Up of a Dental Faculty Development Program. J Dent Educ. 2013;77(6):716–722. doi: 10.1002/j.0022-0337.2013.77.6.tb05523.x. [DOI] [PubMed] [Google Scholar]
- 65.Sabato E, DeCastro JE, Fenesy K. An innovative, Comprehensive Faculty Recruitment and Development Program at one U.S. Dental School: early results. J Dent Educ. 2017;81(6):649–657. doi: 10.21815/JDE.016.029. [DOI] [PubMed] [Google Scholar]
- 66.Tricio JA, Montt JE, Ormeño AP, Del Real AJ, Naranjo CA. Impact of Faculty Development Workshops in Student-centered teaching methodologies on Faculty Members’ teaching and their students’ perceptions. J Dent Educ. 2017;81(6):675–684. doi: 10.21815/JDE.017.014. [DOI] [PubMed] [Google Scholar]
- 67.Berbano EP, Browning R, Pangaro L, Jackson JL. The impact of the Stanford Faculty Development Program on ambulatory teaching behavior. J Gen Intern Med. 2006;21(5):430–434. doi: 10.1111/j.1525-1497.2006.00422.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bigby J, Barnes HN. Evaluation of a faculty development program in substance abuse education. J Gen Intern Med. 1993;8(6):301–305. doi: 10.1007/BF02600141. [DOI] [PubMed] [Google Scholar]
- 69.Eckstrom E, Homer L, Bowen JL. Measuring outcomes of a one-minute preceptor faculty development workshop. J Gen Intern Med. 2006;21(5):410–414. doi: 10.1111/j.1525-1497.2006.00418.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Green ML, Gross CP, Kernan WN, Wong JG, Holmboe ES. Integrating teaching skills and clinical content in a faculty development workshop. J Gen Intern Med. 2003;18(6):468–474. doi: 10.1046/j.1525-1497.2003.20933.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hatem DS, Barrett SV, Hewson M, Steele D, Purwono U, Smith R. Teaching the medical interview: methods and key learning issues in a faculty development course. J Gen Intern Med. 2007;22(12):1718–1724. doi: 10.1007/s11606-007-0408-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Salerno SM, Jackson JL, O’Malley PG. Interactive Faculty Development Seminars improve the quality of Written Feedback in Ambulatory Teaching. J Gen Intern Med. 2003;18(10):831–834. doi: 10.1046/j.1525-1497.2003.20739.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sullivan AM, Lakoma MD, Billings JA, Peters AS, Block SD, PC Faculty Creating enduring change: demonstrating the long-term impact of a faculty development program in palliative care. J Gen Intern Med. 2006;21(9):907–914. doi: 10.1007/BF02743136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Willett LR. Brief report: utilizing an audiotape for outpatient preceptor faculty development. J Gen Intern Med. 2006;21(5):503–505. doi: 10.1111/j.1525-1497.2006.00437.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Weppner WG, Fisher AK, Hagman M, Inouye L, King I, Smith CS, Wilper AP, Knight CL. Taking SGIM’s Teaching Educators across the Continuum of Health Care on the Road-A Local, Interprofessional Faculty Development Innovation. J Graduate Med Educ. 2017;9(3):378–379. doi: 10.4300/JGME-D-16-00761.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lang VJ, O’Connor AB, Blatt A, Gracey C. Collaborative development of teaching scripts: an efficient faculty development approach for a busy clinical teaching unit. J Hosp Med. 2012;7(8):644–648. doi: 10.1002/jhm.1971. [DOI] [PubMed] [Google Scholar]
- 77.Mookherjee S, Monash B, Wentworth KL, Sharpe BA. Faculty development for hospitalists: structured peer observation of teaching. J Hosp Med. 2014;9(4):244–250. doi: 10.1002/jhm.2151. [DOI] [PubMed] [Google Scholar]
- 78.Podrazik PM, Levine S, Smith S, Scott D, DuBeau CE, Baron A, Whelan C, Johnson J, Cook S, Arora V, et al. The curriculum for the hospitalized aging medical patient program: a collaborative faculty development program for hospitalists, general internists, and geriatricians. J Hosp Med. 2008;3(5):384–393. doi: 10.1002/jhm.348. [DOI] [PubMed] [Google Scholar]
- 79.Coogle CL, Hackett L, Owens MG, Ansello EF, Mathews JH. Perceived self-efficacy gains following an interprofessional faculty development programme in geriatrics education. J Interprof Care. 2016;30(4):483–492. doi: 10.1080/13561820.2016.1177003. [DOI] [PubMed] [Google Scholar]
- 80.Koffel J, Reidt S. An interprofessional train-the-trainer evidence-based practice workshop: design and evaluation. J Interprof Care. 2015;29(4):367–369. doi: 10.3109/13561820.2014.962127. [DOI] [PubMed] [Google Scholar]
- 81.Mkony CA, O’Sullivan PS, Owibingire SS, Fyfe MV, Omer S, Freeman P, Makubi A, Mloka DA, Portillo CJ, Leyna GH, et al. Teaching and educational scholarship in Tanzania: Faculty initiative to improve performance of health professions’ students. J Public Health Policy. 2012;33(SUPPL.1):S150. doi: 10.1057/jphp.2012.45. [DOI] [PubMed] [Google Scholar]
- 82.Sigalet EL, Davies JL, Scott EA, Brisseau GF, Shumway JB, Blackie BJ. Designing interprofessional simulation based faculty development in a new women and children’s hospital in the Middle East: a pilot study. J Taibah Univ Med Sci. 2016;11(6):594–600. [Google Scholar]
- 83.Pinheiro SO, Liechty DK, Busch KV, Johnson ES, Dora DL, Butler RM. Institutional impact of a part-time faculty development fellowship program for osteopathic community-based physicians. J Am Osteopath Assoc. 2002;102(11):637–642. [PubMed] [Google Scholar]
- 84.Green ML. A train-the-trainer model for integrating evidence-based medicine training into podiatric medical education. J Am Podiatr Med Assoc. 2005;95(5):497–504. doi: 10.7547/0950497. [DOI] [PubMed] [Google Scholar]
- 85.Baral N, Nepal AK, Paudel BH, Lamsal M. Effect of teachers training workshop outcomes on real classroom situations of undergraduate medical students. Kathmandu Univ Med J. 2015;13(50):162–166. doi: 10.3126/kumj.v13i2.16791. [DOI] [PubMed] [Google Scholar]
- 86.Baral N, Paudel BH, Das BKL, Aryal M, Gautam A, Lamsal M. Preparing tutors for problem-based learning: an experience from B. P. Koirala Institute of Health Sciences, Nepal. Kathmandu Univ Med J. 2010;8(29):141–145. doi: 10.3126/kumj.v8i1.3237. [DOI] [PubMed] [Google Scholar]
- 87.Yoon HB, Shin JS, Lee SH, Kim DH, Sung M, Amgalan N, Chinzorig T. Transnational collaboration for faculty development in health professions education in Mongolia. Korean J Med Educ. 2016;28(4):381–390. doi: 10.3946/kjme.2016.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Pololi LH, Frankel RM. Humanising medical education through faculty development: linking self-awareness and teaching skills. Med Educ. 2005;39(2):154–162. doi: 10.1111/j.1365-2929.2004.02065.x. [DOI] [PubMed] [Google Scholar]
- 89.Wong JG, Agisheva K. Developing teaching skills for medical educators in Russia: a cross-cultural faculty development project. Med Educ. 2007;41(3):318–324. doi: 10.1111/j.1365-2929.2006.02676.x. [DOI] [PubMed] [Google Scholar]
- 90.Roos M, Kadmon M, Kirschfink M, Koch E, Jünger J, Strittmatter-Haubold V, Steiner T. Developing medical educators - a mixed method evaluation of a teaching education program. Med Educ Online. 2014;19(1):1–8. doi: 10.3402/meo.v19.23868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Smith MA, Cherazard R, Fornari A, Adelman P, Snopkowski M, Lesser M. A unique approach to faculty development using an observed structured teaching encounter (OSTE) Med Educ Online. 2018;23(1):1–5. doi: 10.1080/10872981.2018.1527627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Schaefer EW, Wayne DB, McGaghie WC, Kozmic SE, Grais IM, Butter J. Impact of Cardiac Physical Examination Faculty Development on Medical Student performance: a Randomized Trial. Med Sci Educ. 2014;24(2):165–172. doi: 10.1007/s40670-014-0031-4. [DOI] [Google Scholar]
- 93.Chung HS, Issenberg SB, Phrampus P, Miller G, Mo Je S, Ho Lim T, Min Kim Y. The impact of an international faculty development program on simulation-based healthcare education. Med Teach. 2012;34(6):510–510. doi: 10.3109/0142159X.2012.675458. [DOI] [PubMed] [Google Scholar]
- 94.Johansson J, Skeff K, Stratos G. Clinical teaching improvement: the transportability of the Stanford Faculty Development Program. Med Teach. 2009;31(8):e377. doi: 10.1080/01421590802638055. [DOI] [PubMed] [Google Scholar]
- 95.Johansson J, Skeff KM, Stratos GA. A randomised controlled study of role play in a faculty development programme. Med Teach. 2012;34(2):e123. doi: 10.3109/0142159X.2012.644832. [DOI] [PubMed] [Google Scholar]
- 96.Rodrigue C, Seoane L, Gala RB, Piazza J, Amedee RG. Implementation of a faculty development curriculum emphasizing quality improvement and patient safety: results of a qualitative study. Ochsner J. 2013;13(3):319–321. [PMC free article] [PubMed] [Google Scholar]
- 97.Lee WW, Alkureishi ML, Isaacson JH, Mayer M, Frankel RM, London DA, Wroblewski KE, Arora VM. Impact of a brief faculty training to improve patient-centered communication while using electronic health records. Patient Educ Couns. 2018;101(12):2156–2161. doi: 10.1016/j.pec.2018.06.020. [DOI] [PubMed] [Google Scholar]
- 98.Perron NJ, Cullati S, Hudelson P, Nendaz M, Dolmans D, Van Der Vleuten C. Impact of a faculty development programme for teaching communication skills on participants’ practice. Postgrad Med J. 2014;90(1063):245–250. doi: 10.1136/postgradmedj-2012-131700. [DOI] [PubMed] [Google Scholar]
- 99.Wong JG, Holmboe ES, Jara GB, Martin J, Becker WC, Fiellin DA. Faculty development in small-group teaching skills associated with a training course on office-based treatment of opioid dependence. Substance Abuse. 2004;25(4):35–40. doi: 10.1300/J465v25n04_05. [DOI] [PubMed] [Google Scholar]
- 100.Rosenbaum ME, Lenoch S, Ferguson KJ. Outcomes of a teaching scholars program to promote leadership in faculty development. Teach Learn Med. 2005;17(3):247–252. doi: 10.1207/s15328015tlm1703_8. [DOI] [PubMed] [Google Scholar]
- 101.Wong JG, Agisheva K. Cross-cultural faculty development: initial report of an American/Russian experience. Teach Learn Med. 2004;16(4):376–380. doi: 10.1207/s15328015tlm1604_12. [DOI] [PubMed] [Google Scholar]
- 102.Wong JG, Fang Y. Improving clinical teaching in China: initial report of a Multihospital Pilot Faculty Development Effort. Teach Learn Med. 2012;24(4):355–360. doi: 10.1080/10401334.2012.719801. [DOI] [PubMed] [Google Scholar]
- 103.Phillips C, Bassell K, Fillmore L. Transforming nursing education through clinical faculty development. Teach Learn Nurs. 2019;14(1):47–53. doi: 10.1016/j.teln.2018.09.007. [DOI] [Google Scholar]
- 104.Liao KC, Pu SJ, Liu MS, Yang CW, Kuo HP. Development and implementation of a mini-clinical evaluation exercise (mini-CEX) program to assess the clinical competencies of internal medicine residents: from faculty development to curriculum evaluation. BMC Med Educ. 2013;13(1):1–1. doi: 10.1186/1472-6920-13-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Fornari A, Tortez LM, Lay M, Hirsch B, Tanzi D, Friedman I, Ricardo AP, Pekmezaris R, Branch W. A mixed-methods approach to humanistic interprofessional faculty development. J Continuing Educ Health Prof. 2018;38(1):66–72. doi: 10.1097/CEH.0000000000000184. [DOI] [PubMed] [Google Scholar]
- 106.Moore JE, Pinsky MR. Faculty development for fellows: developing and evaluating a broad-based career development course for critical care medicine trainees. J Crit Care. 2015;30(5):1152.e1151–1152.e1156. doi: 10.1016/j.jcrc.2015.05.032. [DOI] [PubMed] [Google Scholar]
- 107.Baker L, Egan-Lee E, Leslie K, Silver I, Reeves S. Exploring an IPE faculty development program using the 3-P model. J Interprof Care. 2010;24(5):597–600. doi: 10.3109/13561820.2010.481336. [DOI] [PubMed] [Google Scholar]
- 108.Efstathiou JA, Drumm MR, Paly JP, Lawton DM, O’Neill RM, Niemierko A, Leffert LR, Loeffler JS, Shih HA. Long-term impact of a faculty mentoring program in academic medicine. PLoS One. 2018;13(11):1–12. doi: 10.1371/journal.pone.0207634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Safavi A, Sadeghi A. Reconstructing academic Staff Development Program: by implementing a supervised and feedback on experience strategy in Order to Improve their teaching skills in lesson planning. Bimon Educ Strateg Med Sci. 2017;10(5):358–363. [Google Scholar]
- 110.Windish DM, Gozu A, Bass EB, Thomas PA, Sisson SD, Howard DM, Kern DE. A ten-month program in curriculum development for medical educators: 16 years of experience. J Gen Intern Med. 2007;22(5):655–661. doi: 10.1007/s11606-007-0103-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Derakhshan F, Allami A, Ahmadi S. Effect of Faculty Training Programs on Improving Quality of Residency Exams in 2013–2014. J Res Med Educ. 2015;7(1):19–26. doi: 10.18869/acadpub.rme.7.1.19. [DOI] [Google Scholar]
- 112.Sánchez-Mendiola M, Morales-Castillo D, Torruco-García U, Varela-Ruiz M. Eight years’ experience with a Medical Education Journal Club in Mexico: a quasi-experimental one-group study. BMC Med Educ. 2015;15(1):1–8. doi: 10.1186/s12909-015-0499-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Griffeth B, Wiederman M. Faculty development effects on clerkship grades. Clin Teacher. 2018;15(2):151–155. doi: 10.1111/tct.12651. [DOI] [PubMed] [Google Scholar]
- 114.Nemec EC, Welch B. The impact of a faculty development seminar on the quality of multiple-choice questions. Curr Pharm Teach Learn. 2016;8(2):160–163. doi: 10.1016/j.cptl.2015.12.008. [DOI] [Google Scholar]
- 115.Dellinges MA, Curtis DA. Will a short Training Session improve multiple-choice item-writing quality by Dental School Faculty? A pilot study. J Dent Educ. 2017;81(8):948–955. doi: 10.21815/JDE.017.047. [DOI] [PubMed] [Google Scholar]
- 116.Tenzin K, Dorji T, Tenzin T. Construction of multiple choice questions before and after an educational intervention. J Nepal Med Assoc. 2017;56(205):112–116. doi: 10.31729/jnma.2976. [DOI] [PubMed] [Google Scholar]
- 117.Schlair S, Dyche L, Milan F. Longitudinal Faculty Development Program to Promote Effective Observation and Feedback skills in Direct Clinical Observation. MedEdPORTAL. 2017;13:10648–10648. doi: 10.15766/mep_2374-8265.10648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Register S, Peterson DT, Swatzell K, White ML. Effect of interprofessional (IP) faculty development on perceptions of IP collaboration and on IP behaviors. J Interprof Care. 2019;33(6):809–811. doi: 10.1080/13561820.2019.1593115. [DOI] [PubMed] [Google Scholar]
- 119.McCurdy FA, Beck G, Maroon A, Gomes H, Lane PH. The administrative colloquium: developing management and leadership skills for faculty. Ambul Pediatr. 2004;4(1 SUPPL):124–128. doi: 10.1367/1539-4409(2004)004<0124:TACDMA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 120.Rao SK, Carballo V, Cummings BM, Millham F, Jacobson JO. Developing an Interdisciplinary, Team-based Quality Improvement Leadership Training Program for clinicians: the partners clinical process improvement Leadership Program. Am J Med Qual. 2017;32(3):271–277. doi: 10.1177/1062860616648773. [DOI] [PubMed] [Google Scholar]
- 121.Yanamadala M, Criscione-Schreiber LG, Hawley J, Heflin MT, Shah BR. Clinical quality improvement curriculum for Faculty in an Academic Medical Center. Am J Med Qual. 2016;31(2):125–132. doi: 10.1177/1062860614558086. [DOI] [PubMed] [Google Scholar]
- 122.Baldwin CD, Gusic ME, Chandran L. The impact of a National Faculty Development Program embedded within an academic Professional Organization. Acad Med. 2017;92(8):1105–1113. doi: 10.1097/ACM.0000000000001496. [DOI] [PubMed] [Google Scholar]
- 123.Fleming GM, Simmons JH, Xu M, Gesell SB, Brown RF, Cutrer WB, Gigante J, Cooper WO. A facilitated peer mentoring program for Junior Faculty to Promote Professional development and peer networking. Acad Med. 2015;90(6):819–826. doi: 10.1097/ACM.0000000000000705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Klein M, Niebuhr V, D’Alessandro D. Innovative online faculty development utilizing the power of social media. Acad Pediatr. 2013;13(6):564–569. doi: 10.1016/j.acap.2013.07.005. [DOI] [PubMed] [Google Scholar]
- 125.Grimes DA, Schulz KF, Droegemueller W, Munsick RA, Lisanti S. A faculty development course in obstetrics and gynecology. Am J Obstet Gynecol. 2000;183(4):1041–1044. doi: 10.1067/mob.2000.107381. [DOI] [PubMed] [Google Scholar]
- 126.Jackevicius CA, Le J, Nazer L, Hess K, Wang J, Law AV. A formal mentorship program for faculty development. Am J Pharm Educ. 2014;78(5):100. doi: 10.5688/ajpe785100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Reader S, Fornari A, Simon S, Townsend J. Promoting Faculty scholarship – an evaluation of a program for busy clinician-educators. Can Med Educ J. 2015;6(1):e43–e60. doi: 10.36834/cmej.36666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.John A, Joy TM, Paul N, Javed R, Sasidharan A, Menon UK. Effectiveness of a ‘Short training in teaching methodology’ for entry level medical teachers. Indian J Community Health. 2016;28(3):300–304. [Google Scholar]
- 129.Brown GE, Bharwani A, Patel KD, Lemaire JB. An orientation to wellness for new faculty of medicine members: meeting a need in faculty development. Int J Med Educ. 2016;7:255–260. doi: 10.5116/ijme.578a.2064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Srivastava TK, Waghmare LS, Rawekar A, Mishra VP. Fostering educational research among medical teachers: evaluation of a faculty development program in India. J Clin Diagn Res. 2016;10(12):JC09–JC11. doi: 10.7860/JCDR/2016/22564.9115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Taylor CT, Berry TM. A Pharmacy Faculty Academy to foster professional growth and long-term retention of junior faculty members. Am J Pharm Educ. 2008;72(2):32–32. doi: 10.5688/aj720232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Steinert Y. Faculty development: from workshops to communities of practice. Med Teach. 2010;32(5):425–428. doi: 10.3109/01421591003677897. [DOI] [PubMed] [Google Scholar]
- 133.Leslie K, Baker L, Egan-Lee E, Esdaile M, Reeves S. Advancing faculty development in medical education: a systematic review. Acad Med. 2013;88(7):1038–1045. doi: 10.1097/ACM.0b013e318294fd29. [DOI] [PubMed] [Google Scholar]
- 134.Steinert Y. Faculty development in the health professions: a focus on research and practice. Dordrecht: Springer; 2014. [Google Scholar]
- 135.King SM, Richards J, Murray AM, Ryan VJ, Seymour-Walsh A, Campbell N, Kumar K. Informal faculty development in health professions education: identifying opportunities in everyday practice. Med Teach. 2021;43(8):874–878. doi: 10.1080/0142159X.2021.1931080. [DOI] [PubMed] [Google Scholar]
- 136.Webster-Wright A. Reframing professional development through understanding authentic professional learning. Rev Educ Res. 2009;79(2):702–739. doi: 10.3102/0034654308330970. [DOI] [Google Scholar]
- 137.Wenger E. Communities of practice: learning, meaning, and identity. Cambridge: Cambridge university press; 1999. [Google Scholar]
- 138.O’Sullivan PS, Irby DM. Promoting Scholarship in Faculty Development: Relevant Research Paradigms and Methodologies. In: Steinert Y, editor. Faculty Development in the Health Professions: A Focus on Research and Practice. Dordrecht: Springer, Netherlands; 2014. pp. 375–398. [Google Scholar]
- 139.Gruppen LD. Intensive Longitudinal Faculty Development Programs. In: Faculty Development in the Health Professions: A Focus on Research and Practice edn. Edited by Steinert Y. Dordrecht: Springer Netherlands; 2014: 197–216.
- 140.Milner RJ, Gusic ME, Thorndyke LE. Perspective: toward a competency framework for faculty. Acad Med. 2011;86(10):1204–1210. doi: 10.1097/ACM.0b013e31822bd524. [DOI] [PubMed] [Google Scholar]
- 141.Srinivasan M, Li ST, Meyers FJ, Pratt DD, Collins JB, Braddock C, Skeff KM, West DC, Henderson M, Hales RE, et al. Teaching as a competency: competencies for medical educators. Acad Med. 2011;86(10):1211–1220. doi: 10.1097/ACM.0b013e31822c5b9a. [DOI] [PubMed] [Google Scholar]
- 142.Harris DL, Krause KC, Parish DC, Smith MU. Academic competencies for medical faculty. Fam Med. 2007;39(5):343–350. [PubMed] [Google Scholar]
- 143.Molenaar WM, Zanting A, van Beukelen P, de Grave W, Baane JA, Bustraan JA, Engbers R, Fick TE, Jacobs JC, Vervoorn JM. A framework of teaching competencies across the medical education continuum. Med Teach. 2009;31(5):390–396. doi: 10.1080/01421590902845881. [DOI] [PubMed] [Google Scholar]
- 144.Lave J, Wenger E. Situated learning: legitimate peripheral participation. New York (NY): Cambridge university press; 1991. [Google Scholar]
- 145.Mann KV. Faculty Development to Promote Role-Modeling and Reflective Practice. In: Steinert Y, editor. Faculty Development in the Health Professions: A Focus on Research and Practice. Dordrecht: Springer, Netherlands; 2014. pp. 245–264. [Google Scholar]
- 146.Steinert Y, O’Sullivan PS, Irby DM. Strengthening teachers’ Professional identities through Faculty Development. Acad Med. 2019;94(7):963–968. doi: 10.1097/ACM.0000000000002695. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Appendix 1. A copy of the search strategy used within MEDLINE/PubMed database.
Additional file 2: Appendix 2. The Coding Sheet.
Additional file 3: Table S1. Summary of included studies.
Additional file 4: Appendix 3. The study findings based on the Harden teacher’s role framework.
Data Availability Statement
All data generated or analysed during this review are included in this published article and its additional files.