Abstract
Racial inequities in blood pressure levels have been extensively documented. Experiences of racial discrimination could explain some of this disparity, although findings from previous studies have been inconsistent. To address limitations of prior literature, including measurement error, we implemented instrumental variable analysis to assess the relationship between racial discrimination in institutional settings and blood pressure. Using data from 3,876 Black and White adults with an average age of 32 years from examination 4 (1992–1993) of the Coronary Artery Risk Development in Young Adults Study, our primary analysis examined the relationship between self-reported experiences of racial discrimination in institutional settings and blood pressure using reflectance meter measurement of skin color as an instrument. Findings suggested that an increase in experiences of racial discrimination was associated with higher systolic and diastolic blood pressure (β = 2.23 mm Hg (95% confidence interval: 1.85, 2.61) and β = 1.31 (95% confidence interval: 1.00, 1.62), respectively). Our instrumental variable estimates suggest that experiences of racial discrimination within institutional settings contribute to racial inequities in elevated blood pressure and cardiovascular disease outcomes in a relatively young cohort of adults and may yield clinically relevant differences in cardiovascular health over the life course.
Keywords: blood pressure, colorism, instrumental variable analysis, racial discrimination
Abbreviations
- CARDIA
Coronary Artery Risk Development in Young Adults
- CI
confidence interval
- IV
instrumental variable
- LATE
local average treatment effect
- OLS
ordinary least squares
- SES
socioeconomic status
Substantial inequities in elevated blood pressure have been documented among marginalized racial groups in the United States. Approximately 57% of non-Hispanic Black adults have elevated resting blood pressure or are on antihypertensive medication, compared with 44% of non-Hispanic White adults (1). Several factors, including experiences of racial discrimination, have been examined as potential contributors to racial inequities in elevated blood pressure and hypertension status (2–4). However, the association between racial discrimination and elevated blood pressure or hypertension remains inconclusive (2). A recent meta-analysis found no relationship between combined measures of perceived racial discrimination and resting blood pressure; however, racial discrimination was associated with hypertension (4). Findings also suggested that experiences of racial discrimination occurring in institutional settings (e.g., housing) had strong positive associations with resting blood pressure.
Differences in the results of previous studies may reflect bias due to residual or unmeasured confounding, as well as measurement error. For example, suppressed reactions to racial discrimination could be associated with underreporting of experiences of discrimination and could be associated with elevated blood pressure (5) and, if unaccounted for in the analysis, bias the estimate obtained. Measurement error may also result in bias, especially in traditional ordinary least-squares (OLS) regression. In OLS models, both classical, nondifferential measurement error in the exposure (i.e., where errors in the measurement of discrimination are independent of blood pressure) and differential measurement error in the exposure (e.g., greater error in the measurement of discrimination among persons with high or low blood pressure) may bias estimates to varying degrees and directions (6).
Additionally, heterogeneity in the associations between racial discrimination and blood pressure outcomes suggests differences in experiences and impact of discrimination (7, 8). Evidence suggests that the association between racial discrimination and hypertension is more robust for men than for women (4). Differences in the reporting of racial discrimination by socioeconomic status (SES) have also been explored, though less is known (3). Some studies have shown positive associations between years of education and reported racism (9). In contrast, others have found nuanced experiences depending on the setting (10). Variations in the associations of stressors associated with SES on relationships between racial discrimination and elevated blood pressure have been documented (5, 8, 11). However, findings as to which populations are most impacted are not consistent. Researchers have called for further examination to understand the relationships between SES and self-reported racial discrimination pertaining to health outcomes (3).
We employed instrumental variable (IV) analysis to minimize the impacts of classical, nondifferential measurement error in the exposure and unmeasured confounding in assessing the relationship between racial discrimination in institutional settings and blood pressure. Our study attempted to instrument self-reported experiences of racial discrimination using reflectance measures of skin color. These self-reports may be subject to unmeasured confounding by individual-level factors such as reactions to stress, which may affect both reports of inequitable treatment and blood pressure. Experiences of discrimination may also be subject to nondifferential measurement error, which IV analyses attempt to correct, mainly if assessed continuously (12, 13). Previous authors have discussed how other forms of measurement error (e.g., differential) and exposure operationalization (e.g., dichotomization) may result in biased estimates from IV models (12, 14). Most importantly, IV analysis enables us to estimate the local average treatment effect (LATE)—a causal estimate of the effect of racial discrimination on blood pressure among those impacted by skin color, rather than an estimate that applies to the general population of individuals in a sample that includes persons who experience both advantage and disadvantage, capturing the relational nature of racism as a system (15). Under a specific set of assumptions (detailed in the Methods section), IV analysis allows for the estimation of unbiased effects of the exposure on the outcome even when there is measurement error in the exposure or unmeasured exposure-outcome confounding (16).
Reflectance meter measurement of skin color is proposed as an instrument because it captures one aspect through which racism, specifically discrimination, functions. Individuals often ascribe race and assign value using social and societal contexts and phenotypic characteristics (e.g., skin color, hair, physical features) before knowing how an individual self-identifies (17, 18). While skin color may inform racial/ethnic group classification, it operates distinctly from race/ethnicity and speaks to related issues of colorism (19). Colorism is often defined as privilege conferred upon persons with lighter complexions, creating a hierarchy wherein those with lighter skin color often have increased social and economic advantage (19–21). Such color hierarchy contributes to individuals with darker skin color often enduring greater material deprivation and social and economic impacts in comparison with lighter-skinned individuals across and within racial categorizations (19).
We hypothesized that increased experiences of racial discrimination are associated with elevated blood pressure and a greater probability of hypertension. We also investigated whether there is evidence of effect modification by sex, income, and educational attainment.
METHODS
Data
We used publicly available data from the Coronary Artery Risk Development in Young Adults (CARDIA) Study. CARDIA is a prospective cohort study of 5,115 Black and White adults who were aged 18–30 years at baseline data collection (1985–1986). CARDIA’s cohort recruitment strategy and study design have been summarized in further detail elsewhere (22). The CARDIA Study was established to examine risk factors for cardiovascular disease, with participants recruited from 4 centers across the United States (Birmingham, Alabama; Oakland, California; Chicago, Illinois; and Minneapolis, Minnesota) (22). Sampling was stratified to obtain an equal representation of individuals in each race (Black, White), age (18–30 years), sex (male, female), and education (≤12 years of education, >12 years of education) group, with 51% of eligible contacted persons enrolling in the baseline survey.
Our primary analysis used data from CARDIA examination 4 (year 7 (1992–1993); n = 4,085), given that this was the year skin color was measured in cohort participants. This study was considered exempt from review by the Harvard T.H. Chan School of Public Health Institutional Review Board.
Measures
Exposure.
The exposure of interest was the experience of racial discrimination in institutional settings, measured using a scale developed by Krieger (5, 23). Participants responded to questions on whether they had “ever experienced discrimination, been prevented from doing something, or been hassled or made to feel inferior in any of the following 7 situations” because of their race or color: at school; getting a job; at work; getting housing; getting medical care; from the police or in the courts; on the street or in a public setting. Responses were assessed as counts of experiences ranging from 0 to 7.
Primary and secondary outcomes.
Our primary outcome was blood pressure in examination 4. Systolic and diastolic blood pressure were captured with a random-zero sphygmomanometer by trained technicians. Per CARDIA protocol, 3 measures were taken at 1-minute intervals, with the average of the last 2 measures reported (24). Secondary outcomes included hypertension classification and changes in blood pressure over time. Participants were categorized as having a diagnosis of hypertension (yes/no) following the American College of Cardiology/American Heart Association guidelines, which define hypertension as systolic blood pressure ≥130 mm Hg or diastolic blood pressure ≥80 mm Hg (25) or self-reported use of medication for hypertension. Additionally, we assessed change in blood pressure (in continuous mm Hg) from examination 4 to examination 5 (year 10 (1995–1996); n = 3,466).
IV estimation.
We employed an IV analysis using a 2-stage least-squares linear model to estimate the LATE of racial discrimination on blood pressure.
The key assumptions of IV analysis include 1) relevance (i.e., the instrument (reflectance meter measure of skin color) is associated with the exposure (racial discrimination)); 2) the exclusion restriction (i.e., the instrument is only associated with the outcome through the exposure); and 3) marginal exchangeability, or that the instrument and the outcome have no shared causes after accounting for measured confounders (26, 27). A fourth assumption—homogeneity or monotonicity—is required to interpret the point estimate identified (26). There are several versions of the homogeneity assumption (27). Under each version, the estimate obtained from IV analysis is equal to the average treatment effect. Monotonicity is a more relaxed version of this assumption, requiring that the instrument only affects the exposure (discrimination) unidirectionally for everyone (26). However, if monotonicity is assumed, the estimated parameter identified is the average treatment effect among the compliers (or the LATE). We used the more relaxed assumption of monotonicity.
Our IV was objectively measured skin color. Assessments were taken on the inner upper arm, using blue, amber, and green filters (24). Values ranged from 0 to 100, referring to the percentage of reflected light. Low values indicate low reflectance, which is indicative of darker skin (24). We used measurements from the blue filter, as it yields the strongest instrument (i.e., highest F statistic), although the 3 filters are highly correlated (11, 28). We assessed instrument relevance using an F test on the relationship between skin color and racial discrimination, using an F statistic greater than 10 as the cutoff (29). We also performed the Wu-Hausman test, which compares the OLS estimate with the IV estimate (30). The null hypothesis is that both the OLS and IV estimates are consistent, and given that the OLS is more efficient, the OLS estimate should be used (31).
Covariates.
In OLS regressions, we included variables identified in previous literature as confounders between self-reported racial discrimination and measures of health, such as blood pressure: age (years; assessed continuously), sex (male, female), and marital status (married, never married, widowed/divorced/separated/other) (3, 32, 33).
Statistical analysis and models
Analyses were conducted to examine the association between racial discrimination and blood pressure using our instrument, skin color reflectance. The hypothesized relationships are depicted in Figure 1, a directed acyclic graph adapted from those presented by Howe et al. (34). It shows the relationship and measures in the context of historical and contemporary structural and institutional racism and how classical measurement error relates to self-reported racial discrimination experiences.
Figure 1.
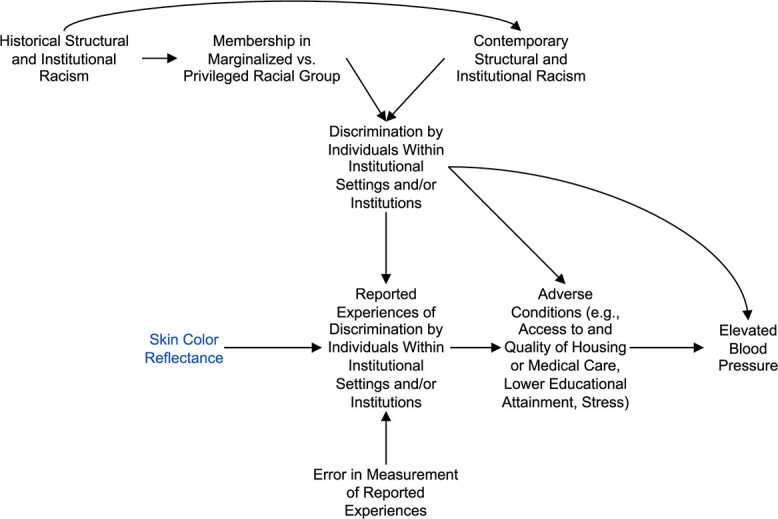
Directed acyclic graph adapted from Howe et al. (34) showing the implemented instrumental variable analysis in relation to historical and contemporary forms of structural and institutional racism and their byproducts (e.g., adverse conditions). We illustrate classical measurement error with “error in measurement of reported experiences” going into the experiences reported by individuals.
While the following models are written in the first- and reduced-stage formats, the 2-stage least-squares approach was used to estimate the LATE of racial discrimination on blood pressure, allowing for the estimation of corrected standard errors (35, 36). IV analysis consists of the “first stage” and “reduced form” models. The first stage was fitted as
 |
where SC = skin color and  = residual error. This model regresses the predicted number of self-reported experiences of racial discrimination on skin color. The associated F statistic in this stage provides support to the relevance assumption.
= residual error. This model regresses the predicted number of self-reported experiences of racial discrimination on skin color. The associated F statistic in this stage provides support to the relevance assumption.
Blood pressure (in continuous mm Hg) was then regressed on the predicted values of self-reported experiences of racial discrimination in the reduced-form model, fitted as
 |
where BP = blood pressure measures,  = the predicted values of self-reported experiences of discrimination from the first stage, and
= the predicted values of self-reported experiences of discrimination from the first stage, and  = residual error.
= residual error.  yields the IV estimator of the effect of an increase in racial discrimination on blood pressure.
yields the IV estimator of the effect of an increase in racial discrimination on blood pressure.
We also performed an OLS regression analysis to estimate the association between discrimination and blood pressure, adjusting for the covariates listed in the section above. The fully adjusted model was fitted as
 |
The analytical sample was restricted to participants with data on experiences of racial discrimination, skin color, and blood pressure measures, resulting in 3,876 eligible participants. Imputation of missing covariates was conducted using the built-in multivariate imputation by chained equations technique available in the “mice” package in R (R Foundation for Statistical Computing, Vienna, Austria) (37). A total of 144 observations were missing some combination of covariate variables (3.72% of the analytical sample), with the greatest proportion missing data on income (1.37% missing) and educational attainment (1.41% missing), though these were the only two variables to exceed missingness of 1%. Imputations were conducted over 5 iterations, using proportional odds models for ordinal categorical variables (i.e., income, educational attainment) and polytomous logistic regression for nominal categorical variables (i.e., marital status). Missing data for binary categorical variables were imputed using logistic regression (i.e., use of high–blood pressure medication (yes/no), alcohol drinking over the past year (yes/no)), while missing data for numerical variables were imputed using predictive mean modeling (i.e., waist circumference). Imputed data were used for all analyses.
Secondarily, we examined effect modification of blood pressure outcomes by sex, education, and income by modeling an interaction term in OLS models and stratifying by each variable in the IV analyses. IV models were used to examine secondary outcomes (i.e., the linear probability of meeting the criteria for hypertension during examination 4 and the LATE between discrimination on change in blood pressure from examination 4 (year 7) to examination 5 (year 10)).
All statistical analyses were conducted using R statistical software (38). The 2-stage least-squares approach was implemented using the “AER” package in R (35, 36).
RESULTS
Primary analyses
Sample characteristics are summarized in Table 1. During CARDIA examination 4, the average age of the sample was 32 years, ranging from 25 years to 37 years. Approximately 48% of the sample identified as Black, and 55% were women. Overall, the mean value of discrimination scores was 1.6 (range, 0–7), though approximately 46% of the sample reported no experiences of discrimination, and 80% of respondents reported 3 or fewer experiences. Average reports of racial discrimination were higher among Black participants (2.81) than among White participants (0.50). Average diastolic and systolic blood pressures were 69 mm Hg and 109 mm Hg, respectively. Differences between Black and White respondents’ systolic and diastolic blood pressures were present (P < 0.001).
Table 1.
Characteristics of a Sample of Participants From CARDIA Study Examination 4 (1992–1993), Overall and by Race/Ethnicity
| Race/Ethnicity | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic | Overall (n = 3,876) | Black (n = 1,865) | White (n = 2,011) | ||||||
| Mean (SD) | No. | % | Mean (SD) | No. | % | Mean (SD) | No. | % | |
| Age, years | 32.0 (3.6) | 31.5 (3.7) | 32.5 (3.3) | ||||||
| Diastolic BP | 69.4 (10.2) | 71.0 (10.9) | 67.9 (9.3) | ||||||
| Systolic BP | 108.8 (12.4) | 111.3 (13.2) | 106.4 (11.1) | ||||||
| Waist circumference, cm | 84.0 (14.1) | 85.8 (14.7) | 82.2 (13.3) | ||||||
| Discrimination scorea | 1.6 (2.0) | 2.8 (2.2) | 0.5 (0.9) | ||||||
| Skin reflectanceb | 20.6 (11.0) | 10.6 (4.5) | 30.4 (5.2) | ||||||
| Sex | |||||||||
| Female | 2,114 | 54.5 | 1,071 | 57.4 | 1,043 | 51.9 | |||
| Male | 1,762 | 45.5 | 794 | 42.6 | 968 | 48.1 | |||
| Duration of education, years | |||||||||
| ≤12 | 1,990 | 51.3 | 1,228 | 65.8 | 762 | 37.9 | |||
| >12 | 1,886 | 48.7 | 637 | 34.2 | 1,249 | 62.1 | |||
| Annual income, dollars | |||||||||
| ≤24,999 | 1,300 | 33.5 | 851 | 45.6 | 449 | 22.3 | |||
| 25,000–49,999 | 1,417 | 36.6 | 678 | 36.4 | 739 | 36.7 | |||
| ≥50,000 | 1,159 | 29.9 | 336 | 18.0 | 823 | 40.9 | |||
| Marital status | |||||||||
| Married | 1,698 | 43.8 | 650 | 34.9 | 1,048 | 52.1 | |||
| Never married | 1,600 | 41.3 | 838 | 44.9 | 762 | 37.9 | |||
| Widowed/separated/divorced/other | 578 | 14.9 | 377 | 20.2 | 201 | 10.0 | |||
| Hypertension | |||||||||
| No | 3,234 | 83.4 | 1,453 | 77.9 | 1,781 | 88.6 | |||
| Yes | 642 | 16.6 | 412 | 22.1 | 230 | 11.4 | |||
| Use of medication for BP | |||||||||
| No | 3,803 | 98.1 | 1,813 | 97.2 | 1,990 | 99.0 | |||
| Yes | 73 | 1.9 | 52 | 2.8 | 21 | 1.0 | |||
| Ever use of tobacco | |||||||||
| No | 1,596 | 41.2 | 858 | 46.0 | 738 | 36.7 | |||
| Yes | 2,280 | 58.8 | 1,007 | 54.0 | 1,273 | 63.3 | |||
| Alcohol intake in past year | |||||||||
| No | 693 | 17.9 | 455 | 24.4 | 238 | 11.8 | |||
| Yes | 3,183 | 82.1 | 1,410 | 75.6 | 1,773 | 88.2 | |||
Abbreviations: BP, blood pressure; CARDIA, Coronary Artery Risk Development in Young Adults; SD, standard deviation.
a Reported experiences of racial discrimination in institutional settings, measured using a scale developed by Krieger (5, 23). Participants responded to questions on whether they had “ever experienced discrimination, been prevented from doing something, or been hassled or made to feel inferior in any of the following 7 situations” because of their race or color: at school; getting a job; at work; getting housing; getting medical care; from the police or in the courts; on the street or in a public setting. Responses were assessed as counts of experiences ranging from 0 to 7.
b Skin color was objectively measured on the inner upper arm. Values ranged from 0 to 100, referring to the percentage of reflected light. Low values indicate low reflectance, which is indicative of darker skin (24).
Results from the Wu-Hausman tests rejected the null hypothesis of the OLS and IV models’ being consistent, indicating a benefit in the use of IV analysis (H = 45.46 (P < 0.001) and H = 96.29 (P < 0.001) for diastolic and systolic pressure, respectively) (39). Table 2 presents the results from the instrumental and OLS models that examined the relationship between racial discrimination and blood pressure. Using the F statistic and results from the test of weak instruments to evaluate the relevance assumption, we found that the reflectance meter measure of skin color had a strong association with racial discrimination scores (F = 1,472.95, P < 0.001; R2 = 0.28), where lighter skin color (greater reflectance) is associated with fewer reports of racial discrimination. However, this was not observed when results were stratified by race (F = 1.03 (P = 0.31) and F = 0.183 (P = 0.67) for Black and White respondents, respectively). IV estimates suggested that each 1.0-unit increase in reports of racial discrimination was associated with a 1.31-mm Hg (95% confidence interval (CI): 1.00, 1.62) increase in diastolic blood pressure. Similarly, the IV estimate showed that increases in racial discrimination were associated with a 2.23-mm Hg (95% CI: 1.85, 2.61) increase in systolic blood pressure. Table 2 also presents the unadjusted and adjusted OLS estimates for the effect of racial discrimination on blood pressure, respectively. Fully adjusted models suggested an increase in both diastolic and systolic blood pressure for each 1.0-unit increase in reported racial discrimination (β = 0.40 (95% CI: 0.25, 0.56) and β = 0.57 (95% CI: 0.38, 0.75), respectively). Expanded results showing the associations for included covariates are presented in Web Table 1 (available at https://doi.org/10.1093/aje/kwad150).
Table 2.
Results From Instrumental Variable and Ordinary Least-Squares Models Examining the Relationship Between Racial Discrimination and Blood Pressure Among CARDIA Study Examination 4 (1992–1993) Participants
| Model | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IV Analysis | OLS Regression for Discrimination and BP | ||||||||||||||
|
First Stagea |
Constant | IV | Constant |
Unadjusted
OLS |
Constant |
Adjusted
OLS b |
|||||||||
| Measure | β | 95% CI | F Statistic |
Intercept for
IV Model |
95% CI | β | 95% CI |
Intercept for
Unadjusted OLS Model |
95% CI | β | 95% CI |
Intercept for
Adjusted OLS Model |
95% CI | β | 95% CI |
| Total BP | −0.10c | −0.10, −0.09 | 1,472.95c | ||||||||||||
| Diastolic BP | 67.27c | 66.68, 67.87 | 1.31c | 1.00, 1.62 | 68.70c | 68.29, 69.12 | 0.42c | 0.26, 0.58 | 54.34c | 51.35, 57.33 | 0.40c | 0.25, 0.56 | |||
| Systolic BP | 105.16c | 104.43, 105.89 | 2.23c | 1.85, 2.61 | 107.67c | 107.17, 108.17 | 0.67c | 0.48, 0.87 | 97.41c | 93.87, 100.96 | 0.57c | 0.38, 0.75 | |||
Abbreviations: BP, blood pressure; CARDIA, Coronary Artery Risk Development in Young Adults; CI, confidence interval; IV, instrumental variable; OLS, ordinary least squares.
a Unadjusted OLS regression assessing whether the instrument (skin color reflectance) was associated with the exposure (racial discrimination).
b Adjusted for marital status, sex, and age at examination 4.
c P < 0.001.
Secondary analyses
Detailed interpretations of the findings are reported in the Web Appendix. Interactions between discrimination and sex were observed for diastolic blood pressure (P = 0.006; Web Table 2) but not for systolic blood pressure (P = 0.535), while interactions between discrimination and income (Web Table 3) were present for both systolic (P < 0.001) and diastolic (P < 0.001) blood pressure. Stratified results were not reported for interactions between discrimination and education, as associations were not observed for either systolic or diastolic blood pressure (P = 0.768 and P = 0.050, respectively).
Analyses of the probability of having hypertension and the change in blood pressure from examination 4 to examination 5 are presented in Web Tables 4 and 5, respectively. The IV estimate suggested that increases in experiences of racial discrimination were associated with an increase in the probability of having hypertension and increases in diastolic and systolic blood pressure over the 2 examination periods. Additional details regarding these secondary findings are presented in the Web Appendix.
DISCUSSION
Our estimates showed increases in blood pressure outcomes due to self-reported racial discrimination among a relatively young cohort of adults. Over time, these increases in blood pressure may yield clinically relevant differences in cardiovascular health over the life course, particularly estimates of the LATE. Our findings are consistent with studies that have observed associations between racial discrimination and blood pressure or hypertension outcomes (2, 3, 40), specifically among those that have used measures of racial discrimination within institutional settings (4). Prior work has found evidence of nonlinear relationships between racial discrimination and blood pressure, particularly in relation to systolic blood pressure (41, 42), where persons reporting no racial discrimination and higher levels of discrimination had increased systolic blood pressure. Inspection of plots of the residuals and fitted values from OLS models did not reveal that this linearity assumption had been violated in our analyses. As such, our use of 2-stage least-squares regression yielded consistent estimates of the LATE among individuals whose report of racial discrimination was impacted by changes in reflectance meter measurement of skin color (i.e., compliers), and this is the population we extend our findings to.
Findings of effect modification by sex and household income require further exploration. Previous work has suggested differences in the reporting of racial discrimination among Black men and women, though not consistently (8, 33). Research has documented differences in the reporting of discrimination solely by domain, though not frequency (9, 33). One found that Black men were more likely to experience racial discrimination in encounters with police, whereas Black women encountered racial discrimination frequently in the educational domain (9). It may also be that the domains in which Black women are at risk may be unmeasured or underexplored (e.g., autonomy, sexuality) (9). These differences reflect gender-based, not sex-based, differences in the experience of racial discrimination.
Regarding SES, studies have found adverse impacts of discrimination on health outcomes among individuals in high- and low-SES groups, depending on the measure used (8). Some research has found that reports of racial discrimination in institutional settings increased with higher education (43, 44) and income (45) among Black adults. It may be that higher-SES Black adults may have more exposure to overt and covert discrimination in housing (e.g., residential steering) and occupational settings (e.g., inequitable pay for similar levels of training and education), for example (46, 47). Several studies have highlighted diminishing returns in health typically associated with increases in socioeconomic position (e.g., greater income, better health outcomes) among Black people relative to Whites (48–50). For example, one found greater Black-White inequities in self-rated health among individuals at higher levels of education (50). Studies have also documented adverse outcomes due to discrimination among low-SES individuals (8). Further research is needed to understand the mechanisms through which harmful social exposures (i.e., gendered racism, SES-based racism) become embodied and the mechanisms in which sex, gender, and SES modify the adverse impacts of racial discrimination on health.
The principal strength of our study is that it used IV analysis to account for measurement error in the exposure, specifically classical measurement error. Prior investigators have found or discussed how estimates from IV analyses are unbiased despite classical measurement error in continuous exposure variables, unlike traditional OLS models (12, 14). Another strength was the use of reflectance-measured skin color as an instrument and the inclusion of populations who experienced undue advantage and undue disadvantage (15). Beyond its relevance to experiences of racial discrimination, our instrument provides some insight into how colorism operates for darker-skinned individuals in addition to discrimination. Illustrated in the first stage, we found that lighter-skinned individuals (higher reflectance) reported fewer experiences of discrimination. This is evident in prior research that used self-reported measures of skin color, such as work that found darker-skinned Black adults were 11 times as likely as lighter-skinned Black adults to report frequent experiences of racial discrimination (51) and work which found that White people reported fewer experiences across skin tone relative to Black and Latinx people (52). While some White people report experiences of racial discrimination due to their race (e.g., “reverse discrimination”) as a result of being denied entry into colleges or jobs, such complaints may reflect an aspect of threatened White privilege (53, 54). Though discrimination is also reported by White people, research has found that discrimination has different implications for Black people. For example, work by Coleman et al. (55) found that Black individuals who reported discrimination at work also showed evidence of experiencing wage discrimination, though this was not observed among White persons who reported discrimination at work. Our analysis included both Black and White individuals to encompass the relational nature of racism as a system. In this context, we captured both the undue disadvantage Black people experience due to racial discrimination and the simultaneous undue advantage encountered by White people (15, 53, 56). Our findings also align with literature that highlights colorism as a global phenomenon across racial group categorizations (15, 19, 53, 56).
Our findings should also be interpreted in the context of their limitations. We used older data from the CARDIA Study due to the availability of skin color measures and the limited methodology available for conducting longitudinal IV analyses. Investigators in recent assessments of self-reported skin color and discrimination (20), as well as discrimination and blood pressure, have observed similar associations (18, 57). Additionally, our study was underpowered to examine race-stratified analyses in the present analysis. Replication of these findings in a larger sample would be useful in understanding racial differences in the impact of additional experiences of racial discrimination in institutional settings on blood pressure. With IV analyses, 2 of the 3 assumptions cannot be confirmed, though we made efforts to evaluate the strength of our instrument using an assessment for weak instruments and the Wu-Hausman test. Additionally, our IV estimates were larger than the OLS estimates. This may have occurred because our IV reduced measurement error in the assessment of discrimination. It is also possible that the discrepancy is due to the IV’s estimating the LATE (e.g., the IV estimate is the effect of exposure only for the population affected by the instrument), whereas OLS estimates the average treatment effect across the entire population.
The validity of our instrument hinges on meeting the exclusion restriction assumption—that there is no pathway by which skin color (as measured by reflectance) influences blood pressure other than through experiences of discrimination within institutions that may be interpersonal or institutional. We cannot reject the plausibility of this assumption’s being violated. It has been proposed that skin color may indirectly affect blood pressure through variations in vitamin D levels. While differences in vitamin D levels have been documented by skin color (58, 59), neither evidence from a meta-analysis of randomized clinical trials and cohort studies (60) nor a meta-analysis of Mendelian-randomized IV studies (61) found evidence of improved blood pressure outcomes through vitamin D supplementation. Speculation about potential genetic markers associated with skin color and blood pressure has been raised. Evidence to date does not suggest that a unique gene exists that indicates a unique pathophysiology of hypertension or elevated blood pressure among Black people (62). Relatedly, work by Kizer (63) highlighted considerable variation in skin tone among siblings within the same family. It has also been proposed that skin color may be related to geographic or cultural differences in practices (e.g., diet or other health behaviors) that are linked to blood pressure. Testing these alternative explanations will require study samples with broader geographic representation than CARDIA and evaluating whether correlations exist between geography and skin color and between specific geographic/cultural factors and blood pressure. However, 2 major national studies of skin color among African Americans in the United States (the National Study of Black Americans and the National Study of American Life) showed no strong evidence of patterning in skin color variation by geography (64, 65).
Our finding that skin color does not predict self-reported discrimination within racial groups meant that we could not perform race-stratified IV analysis. In turn, conducting IV analysis on the whole sample leaves open the possibility that our instrument is correlated with other processes besides self-reported interpersonal discrimination—by which structural racism harms Black individuals. That is, our instrument could not circumvent confounding of the association between self-reported discrimination and blood pressure, although it was still useful for measurement error correction (see Figure 1). It is plausible that other levels of racism, such as structural racism, may have unique pathways through which they affect blood pressure that are not the result of self-reported discrimination at interpersonal or institutional levels or through adverse conditions as conceptualized in our adapted directed acyclic graph. Databases with measures of structural racism, self-reported racial discrimination, skin reflectance, and blood pressure outcomes will be useful in assessing these relationships. Specifically, researchers in future studies should consider how to best operationalize the complex, interinstitutional mechanisms through which structural racism operates, as suggested by several scholars (66–68), to account for potential biasing impacts of structural racism on the present analysis. Future research may also identify other instruments that are not affected by possible confounding of structural racism yet remain relevant to experiences of discrimination within institutional settings. If possible, future studies may also identify outcomes that are not affected by racial discrimination but are subject to being affected by violations of the exclusion restriction (26). To support our instrument, we conducted an overidentification test and assessed skin reflectance as a categorical variable using the Sargan test (373 degrees of freedom; J statistic = 416.634; P = 0.059). The null hypothesis of this test is that the instruments are exogenous (i.e., uncorrelated with the error terms). Results from this analysis failed to reject the null, suggesting that our instrument is exogenous.
Last, our stratified IV results on racial discrimination, education, and household income may present biased estimates. Household income and education are downstream, or consequences, of exposure to racial discrimination. By conditioning on these variables, we violated the third assumption of marginal exchangeability as a result of unmeasured confounders biasing this pathway (69). Therefore, though the OLS estimates indicate a stepwise increase in blood pressure by household income due to racial discrimination, that pattern of associations is obscured in the IV analysis. In our IV, this approach likely yielded biased estimates, given that there are adverse relationships between racial discrimination and measures of SES and, generally, positive relationships between SES measures and blood pressure. However, implementing causal mediation with IV (70) or other mediation approaches (71) and assessing exposure-mediator effect modification would help clarify the direction and magnitude of bias.
While our results must be interpreted with consideration of the assumptions of IV analysis, we demonstrate that IV may be helpful or applicable in discrimination research. Our results lend weight to the reliability of self-reported experiences of discrimination in assessing the harmful effects of racial discrimination on well-being. This work contributes to a body of literature demonstrating the adverse impacts of experiences of racial discrimination within institutional settings on health. It suggests that continued societal interventions are needed—particularly to mitigate inequitable treatment and potentially reduce inequities in blood pressure and hypertension outcomes. The inability to access or maneuver freely within institutions without experiencing discrimination remains a barrier to achieving racial health equity. Mutual aid and movement-building have been consistent practices for navigating the inability to access resources related to social, economic, and general well-being (72–74). However, these must be met with policy and context/community-specific interventions and institutional changes that center on racial equity.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Department of Social and Behavioral Sciences, Harvard T.H. Chan School of Public Health, Harvard University, Cambridge, Massachusetts, United States (Jourdyn A. Lawrence, Ichiro Kawachi, Mary T. Bassett, David R. Williams); Population Health Sciences Program, Harvard Kenneth C. Griffin Graduate School of Arts and Sciences, Harvard University, Cambridge, Massachusetts, United States (Jourdyn A. Lawrence); François-Xavier Bagnoud Center for Health and Human Rights, Harvard T.H. Chan School of Public Health, Harvard University, Cambridge, Massachusetts, United States (Jourdyn A. Lawrence, Mary T. Bassett); Department of Health Policy and Management, School of Public Health, University of Maryland, College Park, College Park, Maryland, United States (Kellee White); and Department of African and African American Studies, Harvard Kenneth C. Griffin Graduate School of Arts and Sciences, Harvard University, Cambridge, Massachusetts, United States (David R. Williams). Dr. Jourdyn A. Lawrence is now affiliated with the Department of Epidemiology and Biostatistics at the Dornsife School of Public Health, Drexel University (Philadelphia, Pennsylvania).
CARDIA Study data are available through the National Heart, Lung, and Blood Institute (NHLBI) BioLINCC database (https://biolincc.nhlbi.nih.gov/home/).
We acknowledge and thank Dr. Joy Shi for her invaluable insights regarding IV analysis and Drs. Jackie Jahn and Joy Shi for their additional feedback on revised versions of the manuscript.
This article was prepared using CARDIA research materials obtained from the NHLBI Biologic Specimen and Data Repository Information Coordinating Center (BioLINCC) and does not necessarily reflect the opinions or views of the CARDIA investigators or the NHLBI.
Conflict of interest: none declared.
REFERENCES
- 1. National Center for Health Statistics . Hypertension Prevalence Among Adults Aged 18 and Over: United States, 2017–2018. (NCHS Data Brief no. 364). Hyattsville, MD: National Center for Health Statistics; 2020. [Google Scholar]
- 2. Lewis TT, Williams DR, Tamene M, et al. Self-reported experiences of discrimination and cardiovascular disease. Curr Cardiovasc Risk Rep. 2014;8(1):365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Brondolo E, Rieppi R, Kelly KP, et al. Perceived racism and blood pressure: a review of the literature and conceptual and methodological critique. Ann Behav Med. 2003;25(1):55–65. [DOI] [PubMed] [Google Scholar]
- 4. Dolezsar CM, McGrath JJ, Herzig AJ, et al. Perceived racial discrimination and hypertension: a comprehensive systematic review. Health Psychol. 2014;33(1):20–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Krieger N, Sidney S. Racial discrimination and blood pressure: the CARDIA study of young black and white adults. Am J Public Health. 1996;86(10):1370–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Van Smeden M, Lash TL, Groenwold RH. Reflection on modern methods: five myths about measurement error in epidemiological research. Int J Epidemiol. 2020;49(1):338–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lewis TT, Van Dyke ME. Discrimination and the health of African Americans: the potential importance of intersectionalities. Curr Dir Psychol Sci. 2018;27(3):176–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Paradies Y. A systematic review of empirical research on self-reported racism and health. Int J Epidemiol. 2006;35(4):888–901. [DOI] [PubMed] [Google Scholar]
- 9. Kwate NOA, Goodman MS. Racism at the intersections: gender and socioeconomic differences in the experience of racism among African Americans. Am J Orthopsychiatry. 2015;85(5):397–408. [DOI] [PubMed] [Google Scholar]
- 10. Brondolo E, Beatty DL, Cubbin C, et al. Sociodemographic variations in self-reported racism in a community sample of blacks and Latino(a)s. J Appl Soc Psychol. 2009;39(2):407–429. [Google Scholar]
- 11. Borrell LN, Kiefe CI, Williams DR, et al. Self-reported health, perceived racial discrimination, and skin color in African Americans in the CARDIA Study. Soc Sci Med. 2006;63(6):1415–1427. [DOI] [PubMed] [Google Scholar]
- 12. Pierce BL, VanderWeele TJ. The effect of non-differential measurement error on bias, precision and power in Mendelian randomization studies. Int J Epidemiol. 2012;41(5):1383–1393. [DOI] [PubMed] [Google Scholar]
- 13. Burgess S, Small DS, Thompson SG. A review of instrumental variable estimators for Mendelian randomization. Stat Methods Med Res. 2017;26(5):2333–2355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Glymour MM, Tchetgen Tchetgen EJ, Robins JM. Credible Mendelian randomization studies: approaches for evaluating the instrumental variable assumptions. Am J Epidemiol. 2012;175(4):332–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jones CP. Confronting institutionalized racism. Phylon. 2002;50(1/2):7–22. [Google Scholar]
- 16. Ertefaie A, Small DS, Flory JH, et al. A tutorial on the use of instrumental variables in pharmacoepidemiology. Pharmacoepidemiol Drug Saf. 2017;26(4):357–367. [DOI] [PubMed] [Google Scholar]
- 17. White K, Lawrence JA, Tchangalova N, et al. Socially-assigned race and health: a scoping review with global implications for population health equity. Int J Equity Health. 2020;19(1):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Monk EP Jr. The cost of color: skin color, discrimination, and health among African-Americans. Am J Sociol. 2015;121(2):396–444. [DOI] [PubMed] [Google Scholar]
- 19. Dixon AR, Telles EE. Skin color and colorism: global research, concepts, and measurement. Annu Rev Sociol. 2017;43:405–424. [Google Scholar]
- 20. Perreira KM, Wassink J, Harris KM. Beyond race/ethnicity: skin color, gender, and the health of young adults in the United States. Popul Res Policy Rev. 2019;38(2):271–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bonilla-Silva E, Dietrich DR. The Latin Americanization of racial stratification in the US. In: Hall RE, ed. Racism in the 21st Century: An Empirical Analysis of Skin Color. New York, NY: Springer Publishing Company; 2008:151–170. [Google Scholar]
- 22. Friedman GD, Cutter GR, Donahue RP, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41(11):1105–1116. [DOI] [PubMed] [Google Scholar]
- 23. Krieger N. Racial and gender discrimination: risk factors for high blood pressure? Soc Sci Med. 1990;30(12):1273–1281. [DOI] [PubMed] [Google Scholar]
- 24. CARDIA Steering Committee . CARDIA Protocol, Year 7 Exam (1992–1993). Birmingham, AL: CARDIA Coordinating Center; 1992. [Google Scholar]
- 25. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: executive summary. J Am Coll Cardiol. 2018;71(19):2199–2269.29146533 [Google Scholar]
- 26. Labrecque J, Swanson SA. Understanding the assumptions underlying instrumental variable analyses: a brief review of falsification strategies and related tools. Curr Epidemiol Rep. 2018;5(3):214–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hernán M, Robins J. Instrumental variable estimation. In: Causal Inference: What If. Boca Raton, FL: Chapman & Hall/CRC Press; 2020:203–220. [Google Scholar]
- 28. Krieger N, Sidney S, Coakley E. Racial discrimination and skin color in the CARDIA Study: implications for public health research. Am J Public Health. 1998;88(9):1308–1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zhang Z, Uddin MJ, Cheng J, et al. Instrumental variable analysis in the presence of unmeasured confounding. Ann Transl Med. 2018;6(10):182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Nakamura A, Nakamura M. On the relationships among several specification error tests presented by Durbin, Wu and Hausman. Econometrica. 1981;49(6):1583–1588. [Google Scholar]
- 31. Hausman J. Specification tests in econometrics. Econometrica. 1978;46(6):1251–1271. [Google Scholar]
- 32. Williams DR, Lawrence JA, Davis BA, et al. Understanding how discrimination can affect health. Health Serv Res. 2019;54(suppl 2):1374–1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Brownlow BN, Sosoo EE, Long RN, et al. Sex differences in the impact of racial discrimination on mental health among black Americans. Curr Psychiatry Rep. 2019;21(11):112. [DOI] [PubMed] [Google Scholar]
- 34. Howe CJ, Bailey ZD, Raifman JR, et al. Recommendations for using causal diagrams to study racial health disparities. Am J Epidemiol. 2022;191(12):1981–1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kleiber C, Zeileis A, Zeileis MA. Package ‘AER’: Applied Econometrics with R. Vienna, Austria: R Foundation for Statistical Computing; 2008. https://cran.r-project.org/web/packages/AER/AER.pdf. Updated June 13, 2022. Accessed March 10, 2019. [Google Scholar]
- 36. Kleiber C, Zeileis A. Applied Econometrics With R. New York, NY: Springer Science+Business Media; 2008. [Google Scholar]
- 37. Buuren S, Groothuis-Oudshoorn K, Robitzsch A, et al. Package ‘mice’: Multiple Imputation by Chained Equations. Vienna, Austria: R Foundation for Statistical Computing; 2015. https://cran.r-project.org/web/packages/mice/mice.pdf. Updated May 24, 2023. Accessed September 4, 2020. [Google Scholar]
- 38. R Core Team . R: A Language and Environment for Statistical Computing. (Version 4.2.2). Vienna, Austria: R Foundation for Statistical Computing; 2013. [Google Scholar]
- 39. Colonescu C. Random regressors. In: Principles of Econometrics With R. (Self-published book). Vienna, Austria: R Foundation for Statistical Computing; 2016:161–168. https://bookdown.org/ccolonescu/RPoE4/RPoE.pdf. Accessed October 20, 2020. [Google Scholar]
- 40. Cuffee YL, Hargraves JL, Allison J. Exploring the association between reported discrimination and hypertension among African Americans: a systematic review. Ethn Dis. 2012;22(4):422–432. [PubMed] [Google Scholar]
- 41. Ryan AM, Gee GC, Laflamme DF. The association between self-reported discrimination, physical health and blood pressure: findings from African Americans, black immigrants, and Latino immigrants in New Hampshire. J Health Care Poor Underserved. 2006;17(2):116–132. [DOI] [PubMed] [Google Scholar]
- 42. Rodriguez CJ, Gwathmey TM, Jin Z, et al. Perceived discrimination and nocturnal blood pressure dipping among Hispanics: the influence of social support and race. Psychosom Med. 2016;78(7):841–850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hudson DL, Neighbors HW, Geronimus AT, et al. Racial discrimination, John Henryism, and depression among African Americans. J Black Psychol. 2016;42(3):221–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Hudson DL, Bullard KM, Neighbors HW, et al. Are benefits conferred with greater socioeconomic position undermined by racial discrimination among African American men? J Mens Health. 2012;9(2):127–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Halanych JH, Safford MM, Shikany JM, et al. The association between income, education, and experiences of discrimination in older African American and European American patients. Ethn Dis. 2011;21(2):223–229. [PMC free article] [PubMed] [Google Scholar]
- 46. Cole ER, Omari SR. Race, class and the dilemmas of upward mobility for African Americans. J Soc Issues. 2003;59(4):785–802. [Google Scholar]
- 47. Iceland J, Wilkes R. Does socioeconomic status matter? Race, class, and residential segregation. Soc Probl. 2006;53(2):248–273. [Google Scholar]
- 48. Assari S. Blacks’ diminished return of education attainment on subjective health; mediating effect of income. Brain Sci. 2018;8(9):176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Holmes CJ, Zajacova A. Education as “the great equalizer”: health benefits for black and white adults. Soc Sci Q. 2014;95(4):1064–1085. [Google Scholar]
- 50. Farmer MM, Ferraro KF. Are racial disparities in health conditional on socioeconomic status? Soc Sci Med. 2005;60(1):191–204. [DOI] [PubMed] [Google Scholar]
- 51. Klonoff EA, Landrine H. Is skin color a marker for racial discrimination? Explaining the skin color-hypertension relationship. J Behav Med. 2000;23(4):329–338. [DOI] [PubMed] [Google Scholar]
- 52. Gonlin V. Colorful reflections: skin tone, reflected race, and perceived discrimination among blacks, Latinxs, and whites. Race Soc Probl. 2020;12(3):246–264. [Google Scholar]
- 53. Malat J, Mayorga-Gallo S, Williams DR. The effects of whiteness on the health of whites in the USA. Soc Sci Med. 2018;199:148–156. [DOI] [PubMed] [Google Scholar]
- 54. Mayrl D, Saperstein A. When white people report racial discrimination: the role of region, religion, and politics. Soc Sci Res. 2013;42(3):742–754. [DOI] [PubMed] [Google Scholar]
- 55. Coleman MG, Darity WA Jr, Sharpe RV. Are reports of discrimination valid? Considering the moral hazard effect. Am J Econ Sociol. 2008;67(2):149–175. [Google Scholar]
- 56. Williams DR. Race and health: basic questions, emerging directions. Ann Epidemiol. 1997;7(5):322–333. [DOI] [PubMed] [Google Scholar]
- 57. Sweet E, McDade TW, Kiefe CI, et al. Relationships between skin color, income, and blood pressure among African Americans in the CARDIA Study. Am J Public Health. 2007;97(12):2253–2259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Xiang F, Lucas R, Gruijl F, et al. A systematic review of the influence of skin pigmentation on changes in the concentrations of vitamin D and 25-hydroxyvitamin D in plasma/serum following experimental UV irradiation. Photochem Photobiol Sci. 2015;14(12):2138–2146. [DOI] [PubMed] [Google Scholar]
- 59. Jablonski NG. The evolution of human skin and skin color. Ann Rev Anthropol. 2004;33:585–623. [Google Scholar]
- 60. Zhang D, Cheng C, Wang Y, et al. Effect of vitamin D on blood pressure and hypertension in the general population: an update meta-analysis of cohort studies and randomized controlled trials. Prev Chronic Dis. 2020;17:E03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Meng X, Li X, Timofeeva MN, et al. Phenome-wide Mendelian-randomization study of genetically determined vitamin D on multiple health outcomes using the UK Biobank Study. Int J Epidemiol. 2019;48(5):1425–1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Daniel HI, Rotimi CN. Genetic epidemiology of hypertension: an update on the African diaspora. Ethn Dis. 2003;13(2 suppl 2):S2–S53. [PubMed] [Google Scholar]
- 63. Kizer JM. Arrested by skin color: evidence from siblings and a nationally representative sample. Socius. 2017;3:2378023117737922. [Google Scholar]
- 64. Keith VM, Herring C. Skin tone and stratification in the black community. Am J Sociol. 1991;97(3):760–778. [Google Scholar]
- 65. Monk EP Jr. The unceasing significance of colorism: skin tone stratification in the United States. Daedalus. 2021;150(2):76–90. [Google Scholar]
- 66. Adkins-Jackson PB, Chantarat T, Bailey ZD, et al. Measuring structural racism: a guide for epidemiologists and other health researchers. Am J Epidemiol. 2022;191(4):539–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Jahn JL. Invited commentary: comparing approaches to measuring structural racism. Am J Epidemiol. 2022;191(4):548–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Hardeman RR, Homan PA, Chantarat T, et al. Improving the measurement of structural racism to achieve antiracist health policy: study examines measurement of structural racism to achieve antiracist health policy. Health Aff. 2022;41(2):179–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Swanson SA. A practical guide to selection bias in instrumental variable analyses. Epidemiology. 2019;30(3):345–349. [DOI] [PubMed] [Google Scholar]
- 70. Dippel C, Ferrara A, Heblich S. Causal mediation analysis in instrumental-variables regressions. Stata J. 2020;20(3):613–626. [Google Scholar]
- 71. Richiardi L, Bellocco R, Zugna D. Mediation analysis in epidemiology: methods, interpretation and bias. Int J Epidemiol. 2013;42(5):1511–1519. [DOI] [PubMed] [Google Scholar]
- 72. Bassett MT. Beyond berets: the Black Panthers as health activists. Am Public Health Assoc. 2016;106(10):1741–1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Nelson A. Body and Soul: the Black Panther Party and the Fight Against Medical Discrimination. Minneapolis, MN: University of Minnesota Press; 2011. [Google Scholar]
- 74. Cross RI, Butler B, Roberson M. An overview of the past, present, and future of black women in health policy. In: Evans SY, Davis SK, Hinkson LR, et al., eds. Black Women and Public Health: Strategies to Name, Locate, and Change Systems of Power. Albany, NY: State University of New York Press; 2022. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


