Abstract
Objectives
As the world population is ageing, it is vital to understand how older adults can maintain and deepen their psychological well-being as they are confronted with the unique challenges of ageing in a complex world. Theoretical work has highlighted the promising role of intentional mental training such as meditation practice for enhancing human flourishing. However, meditation-based randomised controlled trials in older adults are lacking. We aimed to investigate the effects of meditation training on psychological well-being in older adults.
Methods
This study presents a secondary analysis of the Age-Well trial (ClinicalTrials.gov: NCT02977819), which randomised 137 healthy older adults (age range: 65 to 84 years) to an 18-month meditation training, an active comparator (English language training), or a passive control. Well-being was measured at baseline, mid-intervention, and 18-month post-randomisation using the Psychological Well-being Scale (PWBS), the World Health Organisation’s Quality of Life (QoL) Assessment psychological subscale, and composite scores reflecting the meditation-based well-being dimensions of awareness, connection, insight, and a global score comprising the average of these meditation-based dimensions.
Results
The 18-month meditation training was superior to English training on changes in the global score (0.54 [95% CI: 0.26, 0.82], p = 0.0002) and the subscales of awareness, connection, insight, and superior to no-intervention only on changes in the global score (0.54 [95% CI: 0.26, 0.82], p = 0.0002) and awareness. Between-group differences in psychological QoL in favour of meditation did not remain significant after adjusting for multiple comparisons. There were no between-group differences in PWBS total score. Within the meditation group, psychological QoL, awareness, insight, and the global score increased significantly from baseline to 18-month post-randomisation.
Conclusion
The longest randomised meditation training conducted to date enhanced a global composite score reflecting the meditation-based well-being dimensions of awareness, connection, and insight in older adults. Future research is needed to delineate the cognitive, affective, and behavioural factors that predict responsiveness to meditation and thus help refine the development of tailored meditation training.
Introduction
We live in a complex society confronted with unprecedented existential risks and a growing mental health crisis unfolding across generations [1–4]. These complex challenges can disrupt established lifestyles and narratives and expose limitations in both personal and collective capacities for meaning-making [5–7]. The world population is ageing rapidly and older adults present a particularly vulnerable group during these challenging times [8–10]. The physical, social, and psychological difficulties associated with ageing are, today, compounded by the challenges of navigating a fast and uncertain world. Research conducted over the past decades suggested that older adults, despite the physical and cognitive changes associated with ageing, maintain high levels of well-being [11–13]. However, changes over recent years (widespread use of smart phones/internet, COVID-19, geopolitical tensions, increased public awareness of existential risks [e.g., climate change]) might have introduced unique and as-of-yet insufficiently understood pressures on older adults’ psychological well-being (see e.g., [4, 14]). For instance, recent research has indicated that, contrary to expectations expressed during the beginning of the COVID-19 pandemic [4], older adults did not adapt well to the novel psychosocial stressors posed by the COVID-19 pandemic, reporting significant decreases in quality of life, insufficient sleep, and significant increases in the prevalence of depressive and anxiety symptoms [10, 15, 16]. Moreover, the pandemic has led to an increase in the use of at least one psychotropic drug compared to pre-lockdown periods, further highlighting the profound impact of the pandemic on mental health [17]. Understanding how older adults can maintain and deepen their psychological well-being amidst the perils of ageing in today’s complex world presents a pertinent scientific and cultural question.
Over the past decades, research and theory on psychological well-being has aimed to offer answers by understanding the conditions that predict and constitute psychological well-being [18–20]. Psychological well-being is a multidimensional construct. The possibilities and range of human flourishing are deep and wide [21]. Naturally, the conceptions of well-being that have been introduced tended to emphasise different dimensions of human flourishing. In addition to this differentiation, recent theoretical work has increasingly conceptualised psychological well-being as a trainable skill that can be cultivated by specific practices [22]. The cultivation of inner flourishing and the alleviation of suffering have been central tenets of the Greco-Roman philosophical schools as well as Buddhist meditative traditions for millennia but only recently have researchers begun to explicitly synthesise these contemplative perspectives with contemporary scientific models of well-being [22–24].
Particularly Buddhist meditation practices and secular forms of meditation practice derived from Buddhist traditions, including types of mindfulness and loving-kindness and compassion practices, have received a substantial amount of scientific and popular attention [25–30]. Despite this interest and the notable increase in publications on meditation practices, little is known about how these forms of mental training may contribute to human flourishing. Another noteworthy lacuna is the striking lack of research on the effects of meditation training in ageing populations (see [31]). The assumption that well-being is a skill that can be trained not only during periods of seemingly heightened plasticity but across the entire lifespan warrants empirical investigation and suggests that older adults could have the potential to meaningfully enhance their well-being through specific practices [22, 24, 32, 33].
Other important questions of this nascent research field regard the impact of specific meditation practices and the delineation of those well-being dimensions that are particularly amenable to meditation training. Similarly, there is a need for research comparing the utility of meditation training-based theories of human flourishing to prominent scientific models of well-being whose development has not been informed by contemplative perspectives. No line of research or theory can address these complex questions single-handedly. To that end, we employed well-being outcomes that were based on three distinct models of human flourishing: Ryff’s theory of well-being [34], the World Health Organisation’s model of quality of life (QoL; [35]), and the mental training-based framework for well-being developed by Dahl et al. [22].
Ryff [34] proposed a theoretical framework for contemporary scientific perspectives on human flourishing that could unify the largely data-driven and atheoretical research on well-being that had been conducted in this area. Ryff aimed to identify the fundamental dimensions of positive functioning that characterise what it means to be psychologically well. This work proposed six dimensions of well-being, namely self-acceptance, positive relations with others, autonomy (independence), environmental mastery (ability to manage life’s demands), purpose in life, and personal growth (sense of developing and growing; [34]). Ryff’s theory, its accompanying questionnaire (i.e., the 42-item Psychological Well-being Scale; [36], and the vast body of empirical work it generated have significantly shaped the field of well-being research over the past decades [20, 37].
The World Health Organisation (WHO) conceptualises quality of life as an aspect of well-being that reflects “individuals’ perceptions of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns” [35]. Focused on a holistic, cross-cultural approach to health care, the WHO’s work in this area underscores the notion that health is a subjective state of physical and psychological well-being, not simply the absence of disease [35]. The widely used WHO Quality of Life (WHOQOL) assessment includes a psychological domain, which aims to reflect levels of self-esteem, positive feelings (e.g., sense of meaningfulness) and body image, negative feelings (e.g., anxiety), and concentration abilities (i.e., a lack of mind-wandering and distraction, which are associated with lower levels of well-being; see [38]).
Dahl et al.’s [22] mental training-based theory of well-being draws on neuroscientific, psychological, and contemplative perspectives on human flourishing. This model includes a skill-based conception of the well-being dimensions of awareness, connection, and insight. In this framework, awareness can be defined as a heightened, malleable, and undistracted attentiveness to one’s lived experience (including thoughts, feelings, and sensations). Connection encompasses a felt sense of kinship, empathy, gratitude, and understanding toward others that forms the foundation for meaningful interactions and relationships. Insight describes the experiential understanding of how thoughts, feelings, and worldviews contribute to the shaping of one’s perception of self and world [22, 23, 39].
In a recent randomised controlled trial of an 8-week mindfulness-based intervention in older adults at heightened risk of dementia [40], we used outcome measures derived from Ryff’s [34], the WHO’s [35], and three dimensions of Dahl et al.’s [22] models of well-being (i.e., awareness, connection, insight) and found only limited effects. The mindfulness-based intervention was superior to its active comparator (health self-management programme) only on changes in connection at post-intervention, but, in both groups, none of the well-being measures indicated an increase. We concluded that longer intervention studies with waitlist control groups are required to assess if the limited effects could be due to the interventions’ brevity (i.e., 8 weeks) or small base rate changes in well-being in older adults [40]. In contrast to the previous 8-week trial, the present study includes a longer meditation training period (i.e., 18 months), two specific training modules (mindfulness, loving-kindness and compassion), a no-intervention control group, and a different population (i.e., healthy older adults).
We aimed to compare the effects of an 18-month meditation training for older adults on measures of psychological well-being reflective of the three approaches introduced above to a structurally matched English training and a no-intervention condition. These comparisons present a secondary analysis of the Age-Well randomised controlled trial, in which the primary outcomes (mean change in volume and perfusion of the anterior cingulate cortex and insula from pre- to post-intervention) were not significantly modified by the 18-month intervention [41]. Whereas the primary outcome paper only provided data from two time points (i.e., baseline and post-intervention) and compared the meditation group only to the English training group, the present study also presents data from mid-intervention at 9 months, thus offering (i) a more fine-grained analysis of the trajectories of these outcomes in relation to the mindfulness module and loving-kindness and compassion module, (ii) a comparison between the meditation training and no-intervention, and (iii) and a description of the specificity of the newly developed meditation-based composite score (i.e., assessing its trajectory compared those of two established measures of well-being).
In line with prior theory [22, 24], we hypothesised a priori that meditation training would cultivate awareness, connection, and insight, and thus, more broadly, also the forms of well-being captured by the PWBS and the WHO’s psychological QoL subscale. We expected these changes in well-being during the meditation training to be superior to English training and no-intervention. We also predicted that during the two-module meditation training, the initial 9-month mindfulness module would primarily train the meditation-based well-being dimensions of awareness and insight, whereas the subsequent 9-month loving kindness and compassion module would primarily cultivate connection. These hypotheses are based on a model of meditation and ageing developed by the European Medit-Ageing Project [24]. In this model, mindfulness practices are hypothesised to enhance psychological well-being by training attentional control, emotion regulation, and meta-cognitive capacities, thereby weakening maladaptive mental schemes and enabling more emotionally balanced states. Compassion practices in this model are hypothesised to enhance well-being by training perspective taking and cognitive reappraisal, fostering caring expressions, perceptions of kinship, and prosocial behaviour. These practices, whether directed towards the self or others, are expected to reduce social stress reactivity through an empathy-based resilience. In this framework, mindfulness and compassion practices have distinct and overlapping mechanisms for improving well-being. Both train meta-awareness and attention control, yet mindfulness practices primarily downregulate maladaptive mental patterns by increasing the malleability, flexibility, and availability of different views and interpretations. Compassion and loving-kindness practices, in contrast, primarily manifest their salutary impact via the upregulation of positive emotions, caring attitudes, and benevolent intentions for self and others. The combination of these practices within a single meditation-based intervention is hypothesised to optimise and synergise the effects of meditation training on older adults [24]. Furthermore, we aimed to assess the potential moderating effects of total amount of practice, responsiveness, expectancy, baseline, sex, cognition, and baseline well-being scores.
Methods
This study used longitudinal data from the Age-Well randomised controlled trial of the European Union’s Horizon 2020-funded Medit-Ageing European project (public name: Silver Santé Study). The published trial protocol includes detailed information on intervention design, recruitment procedure, eligibility criteria, and assessments [42]. The present study presents a secondary analysis of the Age-Well trial.
Study design
Age-Well was a monocentric, randomised, controlled superiority clinical trial targeting mental health and well-being in older adults. The three parallel arms comprise a two-module (i.e. mindfulness, and loving-kindness and compassion) 18-month meditation training, a structurally matched 18-month foreign language (English) training, and a passive no-intervention control condition. Participants in the no-intervention group were asked to not engage in meditation or foreign language training during the 18-month period. Randomisation to one of the three groups was performed at a ratio of 1:1:1. Participants were assessed at three visits: pre-intervention at baseline (V1), mid-intervention at 9 months (V2), and post-intervention at 18 months (V3). The primary outcomes of the Age-Well trial, mean change in volume and perfusion of the anterior cingulate cortex and insula from pre- to post-intervention, are reported elsewhere [41].
The intervention was delivered in Caen (France). Written informed consent was obtained from all participants after the procedures had been explained to them and prior to participation. Age-Well received ethics approval from the Comité de Protection des Personnes CPP Nord-Ouest III in Caen (trial registration number: EudraCT: 2016-002441-36; IDRCB: 2016-A01767-44; ClinicalTrials.gov Identifier: NCT02977819). The Age-Well trial has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Participants
A total of 137 participants were randomised. Two participants were excluded from the trial after randomisation: one participant presented with amyotrophic lateral sclerosis and one participant had previously experienced a head trauma with loss of consciousness for more than one hour. Another participant died before the end of the trial. The present study thus included data from 134 cognitively unimpaired, older adults (age range: 65 to 78 years [meditation]; 65 to 84 years [English training]; 65 to 75 years [no-intervention]), who had no major neurological or psychiatric disorder, no present or past regular or intensive practice of meditation, were native French speakers, were retired for at least one year, and had completed at least seven years of formal education (Table 1).
Table 1. Demographic characteristics.
| Meditation (n = 45) | English training (n = 45) | No intervention (n = 44) | |
|---|---|---|---|
| Age, years | 69.5 (3.7) | 70.3 (4.5) | 67.6 (2.5) |
| Female, n (%) | 31 (68.9%) | 25 (55.6%) | 26 (59.1%) |
| Education, years | 13.1 (3.1) | 12.2 (3.0) | 14.3 (2.8) |
Note. All variables are mean (standard deviation) unless otherwise specified.
Interventions
Meditation training
The 18-month meditation training consisted of weekly group sessions (2 hours), daily home practice (≥20 minutes), and one retreat day that involved 5 hours of practice. Informed by existing meditation-based interventions (for details see [42], the meditation training included two 9-month modules that were specifically designed for Age-Well with a focus on developing mindfulness, kindness, and compassion to support healthy ageing and to skilfully meet the physical and psychological challenges associated with ageing. The first 9-month module of the intervention emphasised the training of mindfulness practices, whereas the subsequent 9-month module emphasised the cultivation of loving-kindness and compassion practices.
English language training
The English language training followed the same format and structure as the meditation training, and was matched in administration, duration, and dosage of group meetings and home practice. English training (for French native speakers) consisted of exercises aimed at improving participants’ vocabulary and grammatical skills and their application to reading, writing, and speaking. Whereas the meditation training was expected to exert effects on both cognitive control and emotion regulation, the English training was hypothesised to affect cognitive control only.
Measures of well-being
The 42-item Psychological Well-being Scale (PWBS; [36]) was used to capture psychological well-being. The PWBS is based on a conceptual model of well-being that includes six dimensions: self-acceptance, positive relations with others, autonomy (independence), environmental mastery (ability to manage life’s demands), purpose in life, and personal growth (sense of developing and growing; [34]). A 7-item subscale with a 7-point Likert scale anchored at 1 (strongly agree) and 7 (strongly disagree) is used to measure each dimension. After reverse scoring 21 items, subscale scores were computed by averaging their respective item scores. The total PWBS score was computed by averaging all items. For all scales, higher scores are indicative of higher levels of psychological well-being. Internal consistency of the PWBS subscales has been low to moderate (Cronbach’s alpha ranging from 0.33 to 0.56; [36]).
The World Health Organization WHOQOL-BREF Quality of Life Assessment [35] psychological subscale was used to capture psychological quality of life. The WHOQOL-BREF psychological subscale measures levels of positive feelings (e.g., sense of meaningfulness) and body image, self-esteem, the ability to concentrate, and the lack of negative feelings (e.g., anxiety). The 6-item psychological subscale uses a 5-point Likert scale ranging from 0 (not at all) to 5 (completely). After reverse scoring one item, subscale scores were computed by summing the six item scores. Higher subscale scores reflect higher levels of psychological quality of life. The WHOQOL-BREF psychological subscale has displayed good levels of internal consistency (Cronbach’s alpha = 0.81; [35]).
To capture the meditation-based well-being dimensions of awareness, connection, and insight introduced by Dahl et al. [22, 23], we used three previously developed composite scores of meditation-based psychological capacities. Detailed information on the theory-guided development and psychometric properties of these composites have been published [43]. In addition, a global composite score captured the dimensions of awareness, connection, and insight to an equal extent. These composite scores have already been reported as secondary outcomes within the primary outcome paper of the Age-well study [41]. The estimates and p-values presented here slightly differ from the primary outcome paper because the models here used data from all three time points (V1, V2, V3), whereas the primary outcome paper used data from only two time points (V1, V3). Here, we report additional data (i) comparing the trajectories of these composite scores between the mindfulness module and loving-kindness and compassion module (i.e., presenting data from mid-intervention at 9 months), (ii) comparing the meditation training to no-intervention, and (iii) assessing potential moderating effects on the composite scores (see below for a presentation of the potential moderator variables). These additional analyses are exploratory and, therefore, not controlled for multiple comparisons. The three composite scores comprise scales or subscales from six self-report measures (see Table 2), which are described in S1 Table in S1 File.
Table 2. Descriptive statistics for well-being outcomes by group and visit based on all available data.
| Outcome | Meditation | English training | No intervention | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Mid | Post | Pre | Mid | Post | Pre | Mid | Post | ||||||||||
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | |
| PWBS | ||||||||||||||||||
| Total | 45 | 5.4 (0.6) | 45 | 5.3 (0.7) | 45 | 5.3 (0.7) | 45 | 5.3 (0.7) | 45 | 5.4 (0.7) | 45 | 5.4 (0.7) | 44 | 5.6 (0.6) | 44 | 5.5 (0.6) | 44 | 5.6 (0.6) |
| Autonomy | 45 | 5.2 (0.8) | 45 | 5.1 (0.7) | 45 | 5.2 (0.7) | 45 | 5.2 (1.0) | 45 | 5.3 (1) | 45 | 5.2 (0.9) | 44 | 5.3 (0.9) | 44 | 5.4 (0.8) | 44 | 5.5 (0.8) |
| Environmental mastery | 45 | 5.6 (1.0) | 45 | 5.5 (1) | 45 | 5.5 (1.0) | 45 | 5.7 (1.0) | 45 | 5.7 (0.9) | 45 | 5.7 (1.0) | 44 | 5.9 (0.7) | 44 | 5.7 (0.7) | 44 | 5.9 (0.7) |
| Personal growth | 45 | 5.5 (0.8) | 45 | 5.5 (0.9) | 44 | 5.4 (0.9) | 45 | 5.4 (1.0) | 45 | 5.4 (1) | 45 | 5.1 (0.8) | 44 | 5.7 (0.9) | 44 | 5.7 (0.8) | 44 | 5.5 (0.8) |
| Positive relations | 45 | 5.7 (0.9) | 45 | 5.5 (1) | 45 | 5.7 (0.9) | 45 | 5.6 (1.0) | 45 | 5.5 (1.1) | 45 | 5.6 (1.0) | 44 | 5.6 (0.9) | 44 | 5.6 (0.9) | 44 | 5.7 (0.9) |
| Purpose in life | 45 | 5.5 (0.7) | 45 | 5.2 (0.9) | 45 | 5.3 (0.8) | 45 | 5.3 (0.8) | 45 | 5.3 (0.8) | 45 | 5.2 (0.8) | 44 | 5.5 (0.8) | 44 | 5.4 (0.8) | 44 | 5.6 (0.8) |
| Self-acceptance | 45 | 5.0 (1.0) | 45 | 5 (1) | 45 | 5.0 (1.0) | 45 | 4.9 (1.0) | 45 | 5 (1) | 45 | 5.2 (1.0) | 44 | 5.4 (0.9) | 44 | 5.2 (0.9) | 44 | 5.4 (0.7) |
| Psychological QoL | 45 | 22.8 (3.1) | - | - | 45 | 23.6 (3.4) | 45 | 24.0 (3.4) | - | - | 45 | 23.6 (3.3) | - | 24.1 (3.1) | - | - | 44 | 23.8 (3.0) |
| Awareness | ||||||||||||||||||
| MAIA noticing | 45 | 3.1 (1.2) | 45 | 3.4 (1.1) | 45 | 3.5 (0.9) | 45 | 3.3 (1.1) | 45 | 3.6 (1.1) | 45 | 3.5 (1.0) | 44 | 3.6 (1.1) | 44 | 3.4 (1) | 44 | 3.4 (1.1) |
| MAIA attention regulation | 45 | 2.7 (1.0) | 45 | 3.1 (0.8) | 45 | 3.4 (0.8) | 45 | 2.8 (0.9) | 45 | 2.9 (0.8) | 45 | 3.0 (0.7) | 44 | 3.0 (0.9) | 44 | 2.9 (0.9) | 44 | 2.9 (0.9) |
| MAIA emotional awareness | 45 | 3.5 (1.0) | 45 | 3.5 (1) | 45 | 3.8 (0.9) | 45 | 3.5 (1.0) | 45 | 3.5 (0.9) | 45 | 3.6 (0.9) | 44 | 3.4 (1.1) | 44 | 3.6 (1) | 44 | 3.3 (1.0) |
| MAIA self-regulation | 45 | 3.1 (0.9) | 45 | 3.4 (0.9) | 45 | 3.7 (0.8) | 45 | 3.2 (1.0) | 45 | 3.2 (1) | 45 | 3.4 (0.8) | 44 | 3.0 (1.1) | 44 | 3.3 (1) | 44 | 3.0 (1.0) |
| MAIA body listening | 44 | 2.3 (1.2) | 45 | 2.8 (1.2) | 45 | 3.2 (1.0) | 45 | 2.7 (1.2) | 45 | 2.7 (1.2) | 45 | 2.7 (1.1) | 44 | 2.5 (1.2) | 44 | 2.7 (1.2) | 44 | 2.5 (1.2) |
| FFMQ observing | 45 | 9.4 (2.9) | 45 | 9.5 (2.8) | 45 | 9.4 (2.6) | 45 | 8.8 (2.9) | 45 | 8.5 (2.7) | 45 | 9.0 (3.0) | 44 | 10.3 (2.9) | 44 | 9.9 (3.3) | 44 | 9.9 (2.9) |
| FFMQ act with awareness | 45 | 11.6 (2.1) | 45 | 11 (2.4) | 45 | 11.6 (2.2) | 45 | 11.8 (2.2) | 45 | 11.7 (2.4) | 45 | 11.2 (2.3) | 44 | 11.8 (2.3) | 44 | 12 (2.1) | 44 | 11.8 (2.2) |
| Connection | ||||||||||||||||||
| Compassionate Love Scale | 45 | 92.8 (22.1) | 45 | 95.6 (19.8) | 45 | 98.2 (18.8) | 45 | 88.6 (21.7) | 45 | 85.5 (22.6) | 45 | 85.2 (22.7) | 44 | 90.3 (20.0) | 44 | 90.7 (20.4) | 44 | 89.1 (20) |
| IRI empathic concern | 45 | 19.4 (4.8) | 45 | 19.4 (4.6) | 45 | 19.4 (4.4) | 45 | 20.2 (4.0) | 45 | 19.6 (3.9) | 45 | 19.1 (4.6) | 44 | 19.9 (4.0) | 44 | 19 (4) | 44 | 18.7 (3.7) |
| IRI perspective taking | 45 | 17.8 (3.6) | 45 | 17.5 (3.3) | 45 | 17.9 (3.9) | 45 | 16.8 (3.8) | 45 | 16.5 (3.4) | 45 | 16.5 (2.9) | 44 | 17.8 (3.0) | 44 | 17.1 (4.3) | 44 | 17.5 (2.8) |
| Prosocialness Scale | 45 | 61.8 (7.6) | 45 | 57.3 (9.3) | 45 | 60.6 (9.4) | 45 | 60.1 (7.3) | 45 | 54.7 (10.4) | 45 | 58.2 (10.7) | 44 | 59.1 (9.7) | 44 | 55.7 (10.3) | 44 | 58.3 (7.7) |
| Insight | ||||||||||||||||||
| Drexel Defusion Scale | 45 | 34.4 (5.7) | 45 | 33.5 (6.3) | 45 | 34.6 (6.4) | 45 | 33.8 (5.8) | 45 | 34.1 (6.9) | 45 | 34.0 (7.1) | 44 | 35.1 (5.4) | 44 | 35.4 (7) | 44 | 35.5 (5.7) |
| FFMQ non-judging | 45 | 11.1 (2.7) | 45 | 11.3 (2.6) | 45 | 11.2 (2.5) | 45 | 11.7 (1.9) | 45 | 11.4 (2.1) | 45 | 11.6 (2.4) | 44 | 12.1 (2.3) | 44 | 12.1 (2.2) | 44 | 12.2 (1.8) |
| FFMQ non-reactivity | 45 | 9.2 (2.4) | 45 | 9.8 (2.4) | 45 | 10.5 (2.5) | 45 | 9.7 (2.0) | 45 | 9.7 (2) | 45 | 9.3 (2.1) | 44 | 10.3 (2.3) | 44 | 9.9 (2.6) | 44 | 10.0 (2.3) |
| IRI personal distress1 | 45 | 18.4 (5.0) | 45 | 18.3 (4.6) | 45 | 18.9 (5.1) | 45 | 17.0 (5.0) | 45 | 17.2 (5.2) | 45 | 17.4 (5.4) | 44 | 18.0 (5.8) | 44 | 18.5 (5.2) | 44 | 18.7 (4.6) |
Note. PWBS = Psychological Well-being Scale; QoL = Quality of Life; SD = standard deviation; CMBAS = Caring Mindfulness-based Approach for Seniors; HSMP = Health Self-Management Program; PWBS = Psychological Well-being Scale; QoL = quality of life; MAIA = Multidimensional Assessment of Interoceptive Awareness; FFMQ = Five Facet Mindfulness Questionnaire.
1Here, higher scores indicate lower levels of distress.
To derive the three composites of meditation-based dimensions of well-being, we first reverse-scored scale scores if lower total scores reflected better functioning so that higher composite scores would indicate higher well-being at all time points. Second, we computed the difference between each scale score at each time point and the baseline pooled mean. Third, we divided these differences by the baseline pooled standard deviation. Fourth, the z-scores of the scales that were assigned to each composite were averaged, yielding three composite scores with a baseline mean of 0 and a standard deviation smaller than one. A global score was computed by averaging the three composite scores. Fifth, to simplify the interpretation of longitudinal data, we re-standardised the composite scores so that within- and between-group changes in the composite scores present changes in standard deviation units.
Statistical analyses
Sample size
Sample size calculations were based on an expected effect size of 0.75 with 80% power and a Bonferroni-corrected two-sided type I error of 1.25% for the two primary outcomes (i.e., the mean change in volume and perfusion of the anterior cingulate cortex from pre- to post-intervention between the meditation and passive control group), resulting in a minimum total number of 126 participants (42 per group), which has been exceeded (n = 137; detailed in [42]).
Comparative analyses
To evaluate between-group and within-group differences in mean changes in outcomes, we used one mixed effects linear regression model for each outcome including data from all time points, an interaction term between visit and group, and controlling for baseline scores of the outcome. Positive (negative) estimates of mean between-group differences in changes indicate greater (lower) changes in well-being in the meditation group. Missing data were not replaced and assumed to be missing-at-random. Participant data were not excluded based on very high or low scale scores. Analyses of the well-being outcomes not previously published (i.e., PWBS total scores, psychological QoL) were adjusted for multiple comparison (Bonferroni correction for multiple testing). Exploratory analyses of PWBS subscales and meditation module-specific effects on composite scores (i.e., from V1 to V2 and V2 to V3) were not adjusted for multiple comparison.
To allow for an effect size comparison with previously published meditation-based interventions, we also reported the unstandardised mean change in FFMQ total scores from V1 to V2 and V1 to V3. The FFMQ is a gold standard indicator of the efficacy of meditation-based interventions.
To assess the potential moderating effect on well-being within meditation and English, we used linear regression models with change in well-being scores from V1 to V3 as the outcome and the potential moderator variables as the predictors. Moderator variables included total amount of practice (i.e., combined time spent in class and formal home practice), responsiveness (i.e., combining self-perceived and teacher-rated response to the intervention), expectancy (“How much do you think will the intervention have positively impacted your well-being after 18 months?”), baseline neuroticism (measured by the neuroticism subscale of the 44-item Big Five Inventory [44], sex, cognition (measured by the Preclinical Alzheimer’s Cognitive Composite 5 [45], and baseline scores of the well-being outcome. Additional details of variables included in the moderation analysis can be found in S2 Table in S1 File. R version 4.0.2 and Stata/MP version 16.0 was used for statistical analysis.
Results
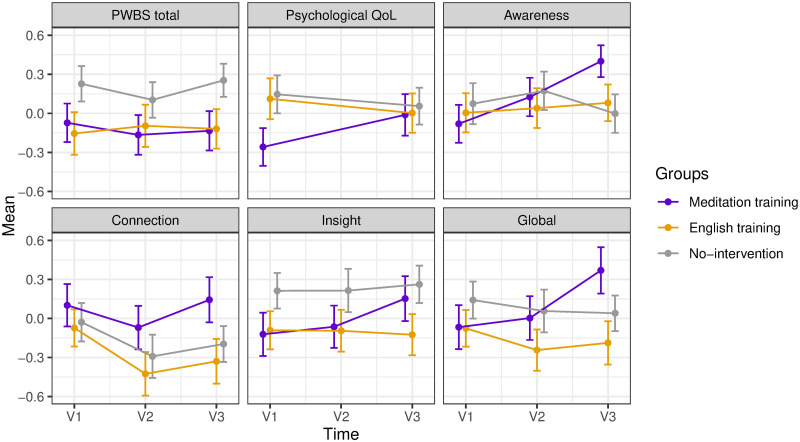
Demographic characteristics are displayed in Table 1. Descriptive statistics of well-being outcomes are reported in Table 2 and visualised in Fig 1 (based on all available data). Results from mixed effects regression models evaluating differential change in well-being outcomes are displayed in Table 3 (based on all participants who provided data at V1, V2, and V3).
Fig 1. 18-month longitudinal changes in Psychological Well-being Scale (PWBS) total scores, and WHOQOL-BREF psychological quality of life (QoL), and meditation-based well-being composite scores (awareness, connection, insight, global) by group.
In the meditation group, pre- to mid-intervention (V1 to V2) corresponds to the 9-month mindfulness module, and mid- to post-intervention (V2 to V3) corresponds to the loving kindness and compassion module. The figure displays observed standardised means and SEs (error bars = 1 SE) based on all available data.
Table 3. Results from mixed effects models assessing differential change in well-being outcomes.
| Outcome | Time | Standardised estimated change | No-intervention | Difference in change Meditation vs. English training | Difference in change Meditation vs. No-intervention | |||
|---|---|---|---|---|---|---|---|---|
| Meditation | English training | Mean (95% CI) | p | Mean (95% CI) | p | |||
| PWBS total1 | V1 to V3 | -0.06 (-0.29, 0.17) | 0.04 (-0.20, 0.27) | 0.05 (-0.19, 0.28) | -0.10 (-0.37, 0.18) | 0.482 | -0.11 (-0.38, 0.17) | 0.441 |
| Psychological QoL1 | V1 to V3 | 0.25 (0.01, 0.48) | -0.11 (-0.35, 0.13) | -0.10 (-0.33, 0.14) | 0.36 (0.02, 0.69) | 0.037 | 0.34 (0.01, 0.68) | 0.045 |
| Awareness | V1 to V3 | 0.48 (0.25, 0.72) | 0.08 (-0.16, 0.31) | -0.09 (-0.33, 0.15) | 0.41 (0.13, 0.69) | 0.0045 | 0.58 (0.29, 0.86) | 0.0001 |
| Connection | V1 to V3 | 0.04 (-0.18, 0.26) | -0.26 (-0.48, -0.04) | -0.18 (-0.40, 0.05) | 0.30 (0.04, 0.56) | 0.024 | 0.22 (-0.04, 0.48) | 0.101 |
| Insight | V1 to V3 | 0.27 (0.05, 0.50) | -0.03 (-0.26, 0.20) | 0.05 (-0.18, 0.29) | 0.31 (0.04, 0.58) | 0.026 | 0.22 (-0.05, 0.49) | 0.113 |
| Global2 | V1 to V3 | 0.43 (0.19, 0.67) | -0.11 (-0.35, 0.12) | -0.11 (-0.35, 0.13) | 0.54 (0.26, 0.82) | 0.0002 | 0.54 (0.26, 0.82) | 0.0002 |
Note. Only participants who provided data at all three time points were included in the analyses. All analyses were adjusted for baseline scores of the outcome. CI = confidence interval; PWBS = Psychological Well-being Scale; QoL = quality of life.
1These analyses were used a significance threshold of 0.025 adjusted using the Bonferroni correction for multiple testing.
2The global composite score reflects the mean score of awareness, connection, and insight.
PWBS
The differences in the mean PWBS total score changes over 18 months between meditation and English training (Cohen’s d: -0.10 [95% CI: -0.37, 0.18]) or no-intervention (-0.11 [95% CI: -0.38, 0.17]) were not statistically significant (p = 0.48 and p = 0.44, respectively). PWBS total scores did not change during meditation, English training, and no-intervention (Table 3).
Exploratory analyses suggested that across PWBS dimension, PWBS self-acceptance increased over 18 months within English training (0.24 [95% CI: 0.02, 0.47], p = 0.033). No other PWBS dimension changed during meditation, English training, and no-intervention (S3 Table in S1 File).
Psychological QoL
Differences in the mean psychological QoL changes over 18 months in favour of meditation compared to English training (Cohen’s d: 0.36 [95% CI: 0.03, 0.69], p = 0.037) and no-intervention (0.34 [95% CI: 0.01, 0.68], p = 0.045) were found. However, these differences were not statistically significant after adjusting for multiple comparisons (Bonferroni-corrected significance threshold of p < 0.025). We suggest that the effect sizes of these between-group differences are nonetheless meaningful. Post-hoc analyses indicated that meditation increased psychological QoL (0.25 [95% CI: 0.01, 0.48], p = 0.041), whereas English training (-0.11 [95% CI: -0.35, 0.13], p = 0.362) and no-intervention did not (-0.10 [95% CI: -0.33, 0.14], p = 0.423).
Meditation-based well-being dimensions
Meditation was superior on changes in awareness to English training (Cohen’s d: 0.41 [95% CI: 0.13, 0.69], p = 0.0045) and no-intervention (0.58 [95% CI: 0.29, 0.86], p = 0.0001). For connection, differences were observed in the mean changes in favour of meditation compared to English training (0.30 [95% CI: 0.04, 0.56], p = 0.024) but not compared to no-intervention (0.22 [95% CI: -0.04, 0.48], p = 0.101). Similarly, for insight, differences were found in the mean changes in favour of meditation compared to English training (0.31 [95% CI: 0.04, 0.58], p = 0.026) but not compared to no-intervention (0.22 [95% CI: -0.05, 0.49], p = 0.113). Meditation was superior on changes in global meditation composite scores to both English training (0.54 [95% CI: 0.26, 0.82], p = 0.0002) and no-intervention (0.54 [95% CI: 0.26, 0.82], p = 0.0002; Table 3).
A frequently used indicator of the efficacy of meditation-based interventions is the mean change in FFMQ total scores. In Age-Well, meditation did not increase FFMQ total scores from V1 to V2 (unstandardised estimate: -0.09 [95% CI: -1.76, 1.94], p = 0.993) or V1 to V3 (1.58 [95% CI: -0.27, 3.43], p = 0.112).
In the meditation group, exploratory analyses assessing the differential effects of the two meditation training modules indicated that the initial 9-month mindfulness module did not significantly increase awareness, connection, insight, or global scores (Table 4, Fig 1), whereas the subsequent 9-month loving kindness and compassion module significantly improved awareness (Cohen’s d: 0.25 [95% CI: 0.01, 0.49], p = 0.034) and global scores (0.38 [95% CI: 0.14, 0.62], p = 0.001). Meditation training was superior to no-intervention only on changes in awareness and global scores during the subsequent 9-month loving kindness and compassion module (i.e., V2 to V3; Table 4).
Table 4. Results from exploratory mixed effects models assessing differential change in meditation-based well-being composite scores in the meditation group by training module compared to no-intervention.
| Outcome | Time / module1 | Meditation | No-intervention | Difference in change Meditation vs. No-intervention | |
|---|---|---|---|---|---|
| Mean (95% CI) | Mean (95% CI) | p | |||
| Awareness | V1 to V2 | 0.23 (-0.01, 0.47) | 0.08 (-0.15, 0.32) | 0.15 (-0.13, 0.43) | 0.303 |
| V2 to V3 | 0.25 (0.01, 0.49) | -0.18 (-0.41, 0.06) | 0.43 (0.15, 0.71) | 0.003 | |
| Connection | V1 to V2 | -0.17 (-0.39, 0.05) | -0.27 (-0.49, -0.05) | 0.10 (-0.16, 0.36) | 0.455 |
| V2 to V3 | 0.21 (-0.01, 0.43) | 0.09 (-0.13, 0.32) | 0.12 (-0.14, 0.38) | 0.370 | |
| Insight | V1 to V2 | 0.06 (-0.17, 0.29) | 0.01 (-0.22, 0.24) | 0.05 (-0.22, 0.32) | 0.713 |
| V2 to V3 | 0.22 (-0.01, 0.45) | 0.05 (-0.18, 0.28) | 0.17 (-0.10, 0.44) | 0.224 | |
| Global2 | V1 to V2 | 0.05 (-0.19, 0.29) | -0.09 (-0.33, 0.14) | 0.14 (-0.13, 0.43) | 0.305 |
| V2 to V3 | 0.38 (0.14, 0.62) | -0.02 (-0.26, 0.22) | 0.40 (0.12, 0.68) | 0.006 | |
Note. All analyses were adjusted for baseline scores of the outcome. CI = confidence interval. Estimates in bold were associated p < 0.05.
1V1 to V2 corresponds to the 9-month mindfulness module. V2 to V3 corresponds to the 9-month loving kindness and compassion module.
2The global composite score reflects the mean score of awareness, connection, and insight.
Moderator analyses
Exploratory moderator analyses were conducted within meditation and English training groups to evaluate the relationship between baseline characteristics and intervention response over 18 months.
In the meditation group, higher baseline scores of PWBS total, psychological QoL, awareness, insight, and global scores were associated with weaker improvements over 18 months. In the English training group, sex and higher baseline scores of PWBS total, psychological QoL, and awareness were associated with weaker improvements in PWBS total, psychological QoL, and awareness over 18 months. Total amount of practice, responsiveness, and expectancy, neuroticism, and cognition did not consistently moderate the intervention response in either group. Results from the moderator analyses are displayed in S4 Table in S1 File.
Discussion
The longest randomised meditation training conducted to date enhanced a global composite score reflecting the meditation-based well-being dimensions of awareness, connection, and insight in older adults. We utilised three theory-based conceptions of well-being [22, 34, 35] to test the effects of the longest randomised meditation training to date on psychological well-being in healthy older adults. The 18-month meditation training was superior to English training on changes in awareness, connection, insight, and global scores (comprising awareness, connection, and insight) and superior to no-intervention only on changes in awareness and global scores. Compared to English training and no-intervention, the differences in the mean changes in psychological QoL over 18 months also favoured the meditation training but these between-group differences in change did not remain significant when adjusting for multiple comparisons. There was no evidence for between-group differences in PWBS total score. Post-hoc analyses indicated that within the meditation group, psychological QoL, awareness, insight, and global scores increased significantly over 18 months, whereas none of the well-being outcomes improved within the English training or no-intervention group. Importantly, however, the within-group effect of meditation training on psychological QoL could also have been due to a regression to the mean as raw psychological QoL scores in the meditation group were substantially lower at baseline (and remained lower post-intervention) than those in the English training and no-intervention groups.
Our predictions regarding the differential effects of the 9-month mindfulness module and the subsequent 9-month loving kindness and compassion module meditation-based well-being dimensions (awareness, connection, insight, global) could only be partially confirmed. Exploratory analyses without correction for multiple comparison indicated that the mindfulness module did not significantly increase any of the meditation-based well-being dimensions, although awareness was impacted to a degree that could be deemed meaningful (Cohen’s d = 0.23). One potential explanation is that the 9-month mindfulness module was not long or intense enough to significantly improve meditation-based well-being dimensions in older adults who have never meditated regularly before. The loving-kindness and compassion module, which we expected to exert its most notable effect on connection, significantly increased awareness and global scores while also showing a substantial but non-significant impact on connection and insight (all Cohen’s ds > 0.20). Taken together, in terms of effect sizes, awareness showed a steady increase across both modules, whereas connection, insight, and global scores increased only during the loving-kindness and compassion module. Importantly, our study design does not allow us to conclude that training in loving-kindness and compassion practices is more beneficial for increasing psychological well-being in older adults than mindfulness training, because the prior mindfulness training could have facilitated the impact of the loving-kindness and compassion module. Future dismantling trials with varying trainings are needed to understand potential practice order and interaction effects.
Nonetheless, our results suggest that the duration of meditation training may not be linearly related to improvement in well-being (i.e., a linear dose-response relationship). More frequent sampling of outcome measures of interest during longitudinal studies will help elucidate different trajectories of change for different types of outcomes and meditation practices. Another potential explanation relates to challenging meditation-related experiences that can commonly occur in novice meditators [46–48], but see also [49, 50] and which might have contributed to the unexpected trajectories of connection (i.e., substantial decline) and insight (i.e., no change) during the first nine months of meditation training. Unfortunately, we cannot evaluate to what extent meditation-related difficulties contributed to these counterintuitive results. Although we captured general adverse events in both trials, we did not include a fine-grained, standardised assessment of difficulties that were particularly related to the practice of meditation.
Exploratory moderator analyses indicated that, in line with previous research [40] and theory (e.g., [51]), participants who reported higher levels of psychological well-being at baseline showed a smaller improvement in well-being during the 18-month meditation training (except for connection). Older adults who are psychologically well at baseline seem to benefit less from meditation training than older adults with lower self-rated well-being. This finding, however, might not be specific to meditation training but rather reflective of a general baseline dependence of training outcomes evident in a wide variety of interventions [52]. Future work is needed to also assess the degree to which this pattern reflects potential ceiling effects associated with the measures we employed. The current gold standard measures of well-being were not conceived (and thus might not sufficiently capture) the forms, qualities, and depth of well-being that can potentially be cultivated by long-term meditation training (e.g., meditative absorptions [Pali: jhanas]; see [53–56]).
Notably, higher responsiveness did not consistently predict higher improvements on well-being outcomes during the 18-month meditation training. In other words, those participants whose overall response to the meditation training was perceived by both themselves and their meditation teachers as beneficial did not report greater increases in well-being dimensions than those for whom the impact of the intervention was perceived as less favourable. Furthermore, the total amount formal meditation practice (in class and at home), neuroticism, expectancy, sex, and cognition also did not moderate the effects of the meditation training on well-being measures. In addition, it is worth highlighting that the meditation group consisted of more female participants (68.9%) than the English (55.6%) and no-intervention groups (59.1%). This larger ratio of female participants in the meditation-based group is consistent with our previous 8-week multinational trial (i.e., 64.4%; [40]). Although the literature on differential sex-related responsiveness to meditation training is under-investigated and equivocal [57], some studies indicate that female practitioners show a greater response to meditation training [58]. Although the sex imbalance of the present study could have potentially influenced the effects of the intervention on psychological well-being, our moderator analysis did not support this conclusion. Identifying more cognitive, affective, and behavioural factors that can predict positive responses to meditation training remains an important domain for future research as this line of investigation has the potential to substantially impact the development, refinement, and effectiveness of tailored meditation training.
Two more surprising findings are noteworthy. First, connection actually decreased during the first 9 months of English training and no-intervention. A similar pattern was found in the aforementioned SCD-Well trial [40] in which compassion for others, which was used as a proxy measure for connection, significantly declined within the active comparator group (health self-management programme) over a 6-month period (i.e., from pre-intervention to follow-up). Second, in the present study, 18 months of meditation training had no impact on FFMQ total scores, which, despite its limitations (see [39]), is the current ‘gold standard’ measure of mindfulness and commonly used as a marker of MBIs’ efficacy. In the light of the substantial effects of the 18-month meditation training on other meditation-based dimensions of well-being, this surprising lack of an effect on FFMQ scores further corroborates doubts surrounding the widely used questionnaire’s validity (see [29, 39]).
The Age-Well trial has important strengths. The 18-month meditation training substantially surpasses the shorter-term meditation training periods of previous trials, which have not exceeded several months [26] and represent the largest meditation-based intervention in older adults conducted to date. The meditation intervention followed a manualised training paradigm that was tailored to the needs of older adults and included two training modules to assess the differential effects of specific practices. Acknowledging the strengths and limitations of previous work, we included a theory-based active comparator alongside a no-intervention control, and utilised three distinct theoretical models of well-being to capture diverse dimensions of human flourishing.
The Age-Well trial also has several limitations. Our sample comprised mostly well-educated, healthy participants that were recruited from a single geographic location, whose cultural, economic, and social characteristics may not be representative of other regions, limiting the generalisability of our results to populations of older adults with more demographically diverse compositions. Furthermore, we used previously published composite scores of meditation-based psychological capacities to reflect the well-being dimensions of Dahl et al.’s training-based framework for human flourishing [22]. These self-report scales were designed to capture trait-level individual differences and may be less sensitive to measuring process-level aspects of meditation-based well-being dimensions. Furthermore, the study’s reliance on self-reported data may have introduced a degree of bias, as participants’ responses could have been influenced by their perceptions, memory, or understanding of the questions. Lastly, the present study did not present follow-up data that could assess the trajectory of psychological well-being beyond the intervention period.
Taken together, our findings suggest that meditation training meaningfully impacted select dimensions of psychological well-being (most notably awareness and insight) in healthy older adults, and that these changes were not captured by established standard measures of well-being. Meditation-based interventions could present a promising non-pharmacological approach for the cultivation and enhancement of human flourishing amidst the challenges of ageing in today’s complex world.
Future directions
We would like to propose several considerations for future work in this area. Beyond the assessment of specific forms of meditation practice and their mechanisms, we recommend assessing meditators’ intentions for practice and other contextual factors [59, 60]. The range of intentions for practice is likely wider than the therapeutic, medical, or even soteriological goals hitherto acknowledged by the science of meditation. Intentions, and a meditator’s relationship to their intentions, might be crucially important for sustaining longer-term meditative training, for deepening meditative skills, and for realising the most desired benefits (e.g., specific states and traits, transformations of perception). In support of this idea, recent evidence showed that combining ethical teachings on virtuous human qualities with mindfulness training led to higher levels of prosocial behaviour than mindfulness training that did not involve such discussions [61]. In general, it will be pertinent for the field to identify and characterise additional factors—including teacher-student relations, the worldviews embedding meditation practices [62, 63], and prior psychedelic experience [64–66]—that could predict and potentially augment the effects of meditation training.
Moreover, another layer of complexity is added to meditation research if we consider that a certain meditation instruction could induce different experiences for different practitioners, or for that matter, the same practitioner at different times. Despite advances in quantifying the effects of meditation practice in psychological and physiological terms, the science of meditation lacks insight into what it is like to meditate. Therefore, whenever possible, we suggest complementing the triangulation aimed at understanding the correlates of meditative states and the effects of meditation training on well-being with first-person phenomenological methods [39, 67–69]. Relatedly, scientific theories of meditation that are informed by nuanced meditation training paradigms (e.g., see [48, 55]) and the lived experience and perceptual skills of long-term meditators will be essential for the maturation of meditation research. It remains to be discussed whether, and to what extent, intensive meditation training for meditation researchers can support this maturation.
Conclusion
Taken together, this study suggests that longer-term meditation training can enhance important dimensions of psychological well-being in healthy older adults and could thus present a promising non-pharmacological approach for the cultivation of human flourishing. While this finding presents an important contribution to our understanding of the potential of meditation training for enhancing well-being in older adults, there is much more to explore. As we continue this line of research, it will be essential to adopt an interdisciplinary approach that integrates insights from gerontology, psychology, biology (e.g., biomarkers including telomere length), neuroscience, and contemplative studies, and that carefully considers the complexities and nuances of the ageing process. By doing so, future research can further contribute to the development of interventions that support older adults in navigating the challenges of ageing and flourishing in later life.
Supporting information
(PDF)
Acknowledgments
The Medit-Ageing Research Group includes: Claire André, Florence Allais, Julien Asselineau, Eider Arenaza-Urquijo, Sebastian Baez, Martine Batchelor, Axel Beaugonin, Maelle Botton, Pierre Champetier, Anne Chocat, Nina Coll, Sophie Dautricourt, Pascal Delamillieure, Vincent De La Sayette, Marion Delarue, Harriet Demnitz-King, Yacila I. Deza-Araujo, Titi Dolma, Stéphanie Egret, Francesca Felisatti, Eglantine Ferrand-Devouges, Eric Frison, Francis Gheysen, Agathe Joret Philippe, Elizabeth Kuhn, Brigitte Landeau, Gwendoline Ledu, Valérie Lefranc, Maria Leon, Florence Mezenge, Inès Moulinet, Theresa Mueller, Valentin Ourry, Cassandre Palix, Léo Paly, Géraldine Poisnel, Anne Quillard, Géraldine Rauchs, Florence Requier, Eric Salmon, Lena Sannemann, Christine Schwimmer, Edelweiss Touron, Denis Vivien, Patrik Vuilleumier, Cédrick Wallet, and Tim Whitfield. The authors would like to thank all the contributors listed in the Medit-Ageing Research Group as well as Rhonda Smith, Charlotte Reid, the sponsor (Pôle de Recherche Clinique at Inserm), Inserm Transfert (Delphine Smagghe), and the participants in the Medit-Ageing project.
Data Availability
The data underlying this report are made available on request following approval by the executive committee and a formal data sharing agreement (https://silversantestudy.eu/2020/09/25/data-sharing). The Material can be mobilized, under the conditions and modalities defined in the Medit-Ageing Charter by any research team belonging to an Academic institution, for carrying out a scientific research project relating to the scientific theme of mental health and well-being in older people. The Material may also be mobilized by non-academic third parties, under conditions, in particular financial, which will be established by separate agreement between Inserm and by the said third party. Data sharing policies described in the Medit-Ageing charter are in compliance with our ethics approval and guidelines from our funding body. Data contain potentially identifying or sensitive patient information. To request data, please contact the data access committee via the official project website (https://silversantestudy.eu/2020/09/25/data-sharing).
Funding Statement
The Age-Well Randomised Controlled Trials is part of the Medit-Ageing project funded through the European Union in Horizon 2020 program related to the call PHC22 “Promoting mental well-being in the ageing population” and under grant agreement No667696. FC was supported by Fonds National de la Recherche Scientifique (FRS-FNRS, Belgium). The funders had no role in the study design, data acquisition, data analysis, data interpretation or manuscript writing.
References
- 1.Ehrlich PR, Ehrlich AH. Can a collapse of global civilization be avoided? Proc R Soc B Biol Sci. 2013. Mar 7;280(1754):20122845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Storm JAJ. Metamodernism: The Future of Theory. University of Chicago Press; 2021. 375 p. [Google Scholar]
- 3.Wu T, Jia X, Shi H, Niu J, Yin X, Xie J, et al. Prevalence of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis. J Affect Disord. 2021. Feb 15;281:91–8. doi: 10.1016/j.jad.2020.11.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vahia IV, Jeste DV, Reynolds CF III. Older Adults and the Mental Health Effects of COVID-19. JAMA. 2020. Dec 8;324(22):2253–4. doi: 10.1001/jama.2020.21753 [DOI] [PubMed] [Google Scholar]
- 5.Park CL. Making sense of the meaning literature: An integrative review of meaning making and its effects on adjustment to stressful life events. Psychol Bull. 2010;136(2):257–301. doi: 10.1037/a0018301 [DOI] [PubMed] [Google Scholar]
- 6.Stein Z. Education in a Time Between Worlds: Essays on the Future of Schools, Technology & Society. Bright Alliance.; 2019. 337 p. [Google Scholar]
- 7.Koltko-Rivera ME. The Psychology of Worldviews. Rev Gen Psychol. 2004. Mar 1;8(1):3–58. [Google Scholar]
- 8.Chang AY, Skirbekk VF, Tyrovolas S, Kassebaum NJ, Dieleman JL. Measuring population ageing: an analysis of the Global Burden of Disease Study 2017. Lancet Public Health. 2019. Mar 1;4(3):e159–67. doi: 10.1016/S2468-2667(19)30019-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Desa UN. World Population Prospects 2022. N Y U N Dep Econ Soc Aff Popul Div Httpesa Un Orgunpdwpp. 2022;
- 10.Zaninotto P, Iob E, Demakakos P, Steptoe A. Immediate and Longer-Term Changes in the Mental Health and Well-being of Older Adults in England During the COVID-19 Pandemic. JAMA Psychiatry. 2022. Feb 1;79(2):151–9. doi: 10.1001/jamapsychiatry.2021.3749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee EE, Depp C, Palmer BW, Glorioso D, Daly R, Liu J, et al. High prevalence and adverse health effects of loneliness in community-dwelling adults across the lifespan: role of wisdom as a protective factor. Int Psychogeriatr. 2019. Oct;31(10):1447–62. doi: 10.1017/S1041610218002120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ryff CD. In the eye of the beholder: Views of psychological well-being among middle-aged and older adults. Psychol Aging. 1989;4:195–210. doi: 10.1037//0882-7974.4.2.195 [DOI] [PubMed] [Google Scholar]
- 13.Springer KW, Pudrovska T, Hauser RM. Does psychological well-being change with age? Longitudinal tests of age variations and further exploration of the multidimensionality of Ryff’s model of psychological well-being. Soc Sci Res. 2011. Jan 1;40(1):392–8. doi: 10.1016/j.ssresearch.2010.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ayalon L, Roy S, Aloni O, Keating N. A Scoping Review of Research on Older People and Intergenerational Relations in the Context of Climate Change. The Gerontologist. 2022. Feb 21;gnac028. [DOI] [PubMed] [Google Scholar]
- 15.Tull MT, Edmonds KA, Scamaldo KM, Richmond JR, Rose JP, Gratz KL. Psychological Outcomes Associated with Stay-at-Home Orders and the Perceived Impact of COVID-19 on Daily Life. Psychiatry Res. 2020. Jul;289:113098. doi: 10.1016/j.psychres.2020.113098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bäuerle A, Teufel M, Musche V, Weismüller B, Kohler H, Hetkamp M, et al. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: a cross-sectional study in Germany. J Public Health. 2020. Nov 23;42(4):672–8. doi: 10.1093/pubmed/fdaa106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav Immun. 2020. Oct 1;89:531–42. doi: 10.1016/j.bbi.2020.05.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Diener E, Suh EM, Lucas RE, Smith HL. Subjective well-being: Three decades of progress. Psychol Bull. 1999;125:276–302. [Google Scholar]
- 19.Huppert FA. Psychological Well-being: Evidence Regarding its Causes and Consequences†. Appl Psychol Health Well-Being. 2009;1(2):137–64. [Google Scholar]
- 20.Ryff CD. Psychological Well-Being Revisited: Advances in the Science and Practice of Eudaimonia. Psychother Psychosom. 2014;83(1):10–28. doi: 10.1159/000353263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.VanderWeele TJ. On the promotion of human flourishing. Proc Natl Acad Sci. 2017. Aug;114(31):8148–56. doi: 10.1073/pnas.1702996114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dahl CJ, Wilson-Mendenhall CD, Davidson RJ. The plasticity of well-being: A training-based framework for the cultivation of human flourishing. Proc Natl Acad Sci. 2020. Dec 22;117(51):32197–206. doi: 10.1073/pnas.2014859117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dahl CJ, Lutz A, Davidson RJ. Reconstructing and deconstructing the self: cognitive mechanisms in meditation practice. Trends Cogn Sci. 2015. Sep 1;19(9):515–23. doi: 10.1016/j.tics.2015.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lutz A, Chételat G, Collette F, Klimecki OM, Marchant NL, Gonneaud J. The protective effect of mindfulness and compassion meditation practices on ageing: Hypotheses, models and experimental implementation. Ageing Res Rev. 2021. Dec 1;72:101495. doi: 10.1016/j.arr.2021.101495 [DOI] [PubMed] [Google Scholar]
- 25.Fox KCR, Dixon ML, Nijeboer S, Girn M, Floman JL, Lifshitz M, et al. Functional neuroanatomy of meditation: A review and meta-analysis of 78 functional neuroimaging investigations. Neurosci Biobehav Rev. 2016. Jun;65:208–28. doi: 10.1016/j.neubiorev.2016.03.021 [DOI] [PubMed] [Google Scholar]
- 26.Goyal M, Singh S, Sibinga EMS, Gould NF, Rowland-Seymour A, Sharma R, et al. Meditation Programs for Psychological Stress and Well-being: A Systematic Review and Meta-analysis. JAMA Intern Med. 2014. Mar 1;174(3):357–68. doi: 10.1001/jamainternmed.2013.13018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khoury B, Knäuper B, Schlosser M, Carrière K, Chiesa A. Effectiveness of traditional meditation retreats: A systematic review and meta-analysis. J Psychosom Res. 2017. Jan 1;92:16–25. doi: 10.1016/j.jpsychores.2016.11.006 [DOI] [PubMed] [Google Scholar]
- 28.Sedlmeier P, Eberth J, Schwarz M, Zimmermann D, Haarig F, Jaeger S, et al. The psychological effects of meditation: a meta-analysis. Psychol Bull. 2012. Nov;138(6):1139–71. doi: 10.1037/a0028168 [DOI] [PubMed] [Google Scholar]
- 29.Van Dam NT, van Vugt MK, Vago DR, Schmalzl L, Saron CD, Olendzki A, et al. Mind the Hype: A Critical Evaluation and Prescriptive Agenda for Research on Mindfulness and Meditation. Perspect Psychol Sci. 2018. Jan 1;13(1):36–61. doi: 10.1177/1745691617709589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schlosser M, Pfaff NG, Schweinberger SR, Marchant NL, Klimecki OM. The psychometric properties of the compassionate love scale and the validation of the English and German 7-item compassion for others scale (COS-7). Curr Psychol. 2021;42(1):579–91. [Google Scholar]
- 31.Goldberg SB, Riordan KM, Sun S, Davidson RJ. The Empirical Status of Mindfulness-Based Interventions: A Systematic Review of 44 Meta-Analyses of Randomized Controlled Trials. Perspect Psychol Sci. 2022. Jan 1;17(1):108–30. doi: 10.1177/1745691620968771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chételat G, Lutz A, Arenaza-Urquijo E, Collette F, Klimecki O, Marchant N. Why could meditation practice help promote mental health and well-being in aging? Alzheimers Res Ther. 2018. Jun 22;10(1):57. doi: 10.1186/s13195-018-0388-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Klimecki O, Marchant NL, Lutz A, Poisnel G, Chételat G, Collette F. The impact of meditation on healthy ageing—the current state of knowledge and a roadmap to future directions. Curr Opin Psychol. 2019. Aug 1;28:223–8. doi: 10.1016/j.copsyc.2019.01.006 [DOI] [PubMed] [Google Scholar]
- 34.Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J Pers Soc Psychol. 1989;57(6):1069–81. [Google Scholar]
- 35.The Whoqol Group. Development of the World Health Organization WHOQOL-BREF Quality of Life Assessment. Psychol Med. 1998. May;28(3):551–8. [DOI] [PubMed] [Google Scholar]
- 36.Ryff CD, Lee C, Keyes M. The structure of psychological well-being revisited. In: Journal of Personality & Social Psychology. 1995. p. 719–27. doi: 10.1037//0022-3514.69.4.719 [DOI] [PubMed] [Google Scholar]
- 37.Diener E, Oishi S, Tay L. Advances in subjective well-being research. Nat Hum Behav. 2018. Apr;2(4):253–60. doi: 10.1038/s41562-018-0307-6 [DOI] [PubMed] [Google Scholar]
- 38.Killingsworth MA, Gilbert DT. A wandering mind is an unhappy mind. Science. 2010. Nov 12;330(6006):932. doi: 10.1126/science.1192439 [DOI] [PubMed] [Google Scholar]
- 39.Lutz A, Jha AP, Dunne JD, Saron CD. Investigating the phenomenological matrix of mindfulness-related practices from a neurocognitive perspective. Am Psychol. 2015;70(7):632–58. doi: 10.1037/a0039585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schlosser M, Demnitz-King H, Barnhofer T, Collette F, Gonneaud J, Chételat G, et al. Effects of a mindfulness-based intervention and a health self-management programme on psychological well-being in older adults with subjective cognitive decline: Secondary analyses from the SCD-Well randomised clinical trial. medRxiv [Internet]. 2022. Jan 1; Available from: http://medrxiv.org/content/early/2022/09/09/2022.09.08.22279715.abstract [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chételat G, Lutz A, Klimecki O, Frison E, Asselineau J, Schlosser M, et al. Effect of an 18-Month Meditation Training on Regional Brain Volume and Perfusion in Older Adults: The Age-Well Randomized Clinical Trial. JAMA Neurol. 2022. Nov 1;79(11):1165–74. doi: 10.1001/jamaneurol.2022.3185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Poisnel G, Arenaza-Urquijo E, Collette F, Klimecki OM, Marchant NL, Wirth M, et al. The Age-Well randomized controlled trial of the Medit-Ageing European project: Effect of meditation or foreign language training on brain and mental health in older adults. Alzheimers Dement Transl Res Clin Interv. 2018. Jan 1;4:714–23. doi: 10.1016/j.trci.2018.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schlosser M, Barnhofer T, Requier F, Deza-Araujo YI, Abdoun O, Marchant NL, et al. Measuring Psychological Mechanisms in Meditation Practice: Using a Phenomenologically Grounded Classification System to Develop Theory-Based Composite Scores. Mindfulness. 2022. Mar 1;13(3):600–14. [Google Scholar]
- 44.John OP, Srivastava S. The Big Five Trait taxonomy: History, measurement, and theoretical perspectives. In: Handbook of personality: Theory and research, 2nd ed. New York, NY, US: Guilford Press; 1999. p. 102–38. [Google Scholar]
- 45.Papp KV, Rentz DM, Orlovsky I, Sperling RA, Mormino EC. Optimizing the preclinical Alzheimer’s cognitive composite with semantic processing: The PACC5. Alzheimers Dement Transl Res Clin Interv. 2017. Nov 10;3(4):668–77. doi: 10.1016/j.trci.2017.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lindahl JR, Fisher NE, Cooper DJ, Rosen RK, Britton WB. The varieties of contemplative experience: A mixed-methods study of meditation-related challenges in Western Buddhists. PLOS ONE. 2017. May 24;12(5):e0176239. doi: 10.1371/journal.pone.0176239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schlosser M, Sparby T, Vörös S, Jones R, Marchant NL. Unpleasant meditation-related experiences in regular meditators: Prevalence, predictors, and conceptual considerations. PloS One. 2019;14(5):e0216643. doi: 10.1371/journal.pone.0216643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sparby T. What Stands in the Way Becomes the Way: Dual and Non-Dual Approaches to Meditation Hindrances in Buddhist Traditions and Contemplative Science. Religions. 2022. Sep;13(9):840. [Google Scholar]
- 49.Anālayo B. Meditation Maps, Attainment Claims, and the Adversities of Mindfulness. Mindfulness. 2020. Sep 1;11(9):2102–12. [Google Scholar]
- 50.Anālayo B. The Dangers of Mindfulness: Another Myth? Mindfulness. 2021. Dec 1;12(12):2890–5. [Google Scholar]
- 51.Rosenkranz MA, Dunne JD, Davidson RJ. The next generation of mindfulness-based intervention research: what have we learned and where are we headed? Curr Opin Psychol. 2019. Aug;28:179–83. doi: 10.1016/j.copsyc.2018.12.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.de Vet HCW, Foumani M, Scholten MA, Jacobs WCH, Stiggelbout AM, Knol DL, et al. Minimally important change values of a measurement instrument depend more on baseline values than on the type of intervention. J Clin Epidemiol. 2015. May 1;68(5):518–24. doi: 10.1016/j.jclinepi.2014.07.008 [DOI] [PubMed] [Google Scholar]
- 53.Anālayo B. A Brief History of Buddhist Absorption. Mindfulness. 2020. Mar 1;11(3):571–86. [Google Scholar]
- 54.Arbel K. Early Buddhist Meditation: The Four Jhanas as the Actualization of Insight. London: Routledge; 2017. 234 p. [Google Scholar]
- 55.Burbea R. Seeing that frees: meditations on emptiness and dependent arising. Hermes Amara Publications; 2014. [Google Scholar]
- 56.Hagerty MR, Isaacs J, Brasington L, Shupe L, Fetz EE, Cramer SC. Case Study of Ecstatic Meditation: fMRI and EEG Evidence of Self-Stimulating a Reward System. Neural Plast. 2013;2013:1–12. doi: 10.1155/2013/653572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Katz D, Toner B. A Systematic Review of Gender Differences in the Effectiveness of Mindfulness-Based Treatments for Substance Use Disorders. Mindfulness. 2013. Dec 1;4(4):318–31. [Google Scholar]
- 58.Rojiani R, Santoyo JF, Rahrig H, Roth HD, Britton WB. Women Benefit More Than Men in Response to College-based Meditation Training. Front Psychol. 2017;8. doi: 10.3389/fpsyg.2017.00551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Condon P. Meditation in context: factors that facilitate prosocial behavior. Curr Opin Psychol. 2019. Aug 1;28:15–9. doi: 10.1016/j.copsyc.2018.09.011 [DOI] [PubMed] [Google Scholar]
- 60.Condon P, Makransky J. Recovering the Relational Starting Point of Compassion Training: A Foundation for Sustainable and Inclusive Care. Perspect Psychol Sci. 2020. Nov 1;15(6):1346–62. doi: 10.1177/1745691620922200 [DOI] [PubMed] [Google Scholar]
- 61.Chen S, Jordan CH. Incorporating Ethics Into Brief Mindfulness Practice: Effects on Well-Being and Prosocial Behavior. Mindfulness. 2020. Jan 1;11(1):18–29. [Google Scholar]
- 62.Lutz A, Dunne JD, Davidson RJ. Meditation and the neuroscience of consciousness: An introduction. In: The Cambridge handbook of consciousness. New York, NY, US: Cambridge University Press; 2007. p. 499–551. [Google Scholar]
- 63.Vörös S. All Is Burning: Buddhist Mindfulness as Radical Reflection. Religions. 2021. Dec;12(12):1092. [Google Scholar]
- 64.Griffiths RR, Johnson MW, Richards WA, Richards BD, Jesse R, MacLean KA, et al. Psilocybin-occasioned mystical-type experience in combination with meditation and other spiritual practices produces enduring positive changes in psychological functioning and in trait measures of prosocial attitudes and behaviors. J Psychopharmacol (Oxf). 2018. Jan 1;32(1):49–69. doi: 10.1177/0269881117731279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Simonsson C, Chambers R, Hendricks PS, Goldberg SB, Osika W, Schlosser M, et al. Classic Psychedelic Use and Current Meditation Practice. Mindfulness. 2023. Apr 1;14(4):763–8. doi: 10.1007/s12671-023-02103-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Smigielski L, Kometer M, Scheidegger M, Krähenmann R, Huber T, Vollenweider FX. Characterization and prediction of acute and sustained response to psychedelic psilocybin in a mindfulness group retreat. Sci Rep. 2019. Oct 24;9(1):14914. doi: 10.1038/s41598-019-50612-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Petitmengin C, van Beek M, Bitbol M, Nissou JM, Roepstorff A. Studying the experience of meditation through Micro-phenomenology. Curr Opin Psychol. 2019. Aug 1;28:54–9. doi: 10.1016/j.copsyc.2018.10.009 [DOI] [PubMed] [Google Scholar]
- 68.Poletti S, Abdoun O, Zorn J, Lutz A. Pain regulation during mindfulness meditation: Phenomenological fingerprints in novices and experts practitioners. Eur J Pain. 2021;25(7):1583–602. doi: 10.1002/ejp.1774 [DOI] [PubMed] [Google Scholar]
- 69.Varela FJ, Shear J. First-person methodologies: What, why, how. J Conscious Stud. 1999;6(2–3):1–14. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
Data Availability Statement
The data underlying this report are made available on request following approval by the executive committee and a formal data sharing agreement (https://silversantestudy.eu/2020/09/25/data-sharing). The Material can be mobilized, under the conditions and modalities defined in the Medit-Ageing Charter by any research team belonging to an Academic institution, for carrying out a scientific research project relating to the scientific theme of mental health and well-being in older people. The Material may also be mobilized by non-academic third parties, under conditions, in particular financial, which will be established by separate agreement between Inserm and by the said third party. Data sharing policies described in the Medit-Ageing charter are in compliance with our ethics approval and guidelines from our funding body. Data contain potentially identifying or sensitive patient information. To request data, please contact the data access committee via the official project website (https://silversantestudy.eu/2020/09/25/data-sharing).