Abstract
Background
Ebstein’s anomaly occurs when there is an apical displacement of the tricuspid valve with septal and posterior valve leaflets tethering. This condition often occurs in association with other congenital, structural, or conduction system diseases, including intracardiac shunts, valvular lesions, arrhythmias, accessory conduction pathways, and first-degree atrioventricular (AV) block. We present for the first time a case of a patient with Ebstein’s anomaly who presented with second-degree Mobitz II AV block and was successfully treated with conduction system pacing (CSP) due to her young age and the likelihood of a long-term high percentage of pacing.
Case summary
We present a case of a 42-year-old lady with a background of complex congenital heart disease, including severe pulmonary stenosis, Ebstein anomaly, and atrial septal defect (ASD). She required complex surgical intervention, including tricuspid valve (TV) repair and subsequently replacement, ASD closure, and pulmonary balloon valvuloplasty. She presented to our hospital with symptomatic second-degree Mobitz II AV block (dizziness, shortness of breath, and exercise intolerance) and right bundle branch block (RBBB) on her baseline ECG. Her echocardiogram showed dilated right ventricle (RV) and left ventricle (LV) with low normal LV systolic function. Due to her young age and the likelihood of a long-term high percentage of RV pacing, we opted for CSP after a detailed discussion and patient consent. The distal HIS position is the preferred pacing strategy at our centre. We could not cross the TV with the standard Medtronic C315 HIS catheter, so we had to use the deflectable C304 HIS catheter. Mapping and pacing of the distal HIS bundle were achieved by Medtronic Selectsecure 3830, 69 cm lead. HIS bundle pacing led to the correction of both second-degree Mobitz II AV block and pre-existing RBBB. The implantation was uneventful, and the patient was discharged home the next day without any acute complications.
Discussion
Distal HIS pacing is feasible in patients with surgically treated complex Ebstein anomaly and heart block. This approach can normalize the QRS complex with a high probability of preserving or improving LV function.
Keywords: Conduction system pacing, His pacing, Ebstein’s anomaly, 2nd-degree Mobitz II AV block, Right bundle branch block, Case report
Learning points.
Crossing the tricuspid valve could be problematic, so that a deflectable C315 HIS catheter can facilitate the process.
Distal HIS pacing is achievable and safe in patients with surgically treated complex Ebstein’s anomaly and heart block.
This approach can normalize the QRS complex with a high probability of preserving or improving LV function.
Introduction
Conduction system pacing (CSP) gained popularity in the last decade as a more physiological alternative to right ventricular pacing for treating bradycardia or as an alternative to biventricular pacing for cardiac resynchronization therapy (CRT). It is divided into His bundle pacing (HBP) and left bundle branch area pacing. The current European Society of Cardiology guidelines for pacing and CRT present HBP as a class IIb indication (level of evidence C) and a left ventricular ejection fraction > 40% who require frequent (more than 20%) ventricular pacing or as part of a ‘pace and ablate’ strategy for rapidly conducted supra-ventricular arrhythmias. It also has a class IIa indication (level of evidence B) in CRT candidates in case of failed coronary sinus lead implantation.1 In patients with narrow QRS complexes, His bundle pacing allows similar ventricular activation pattern with preservation of QRS duration and morphology.2
To the best of our knowledge, we report the first case of HBP in a patient with corrected Ebstein’s anomaly, second-degree Mobitz II AV block, and RBBB.
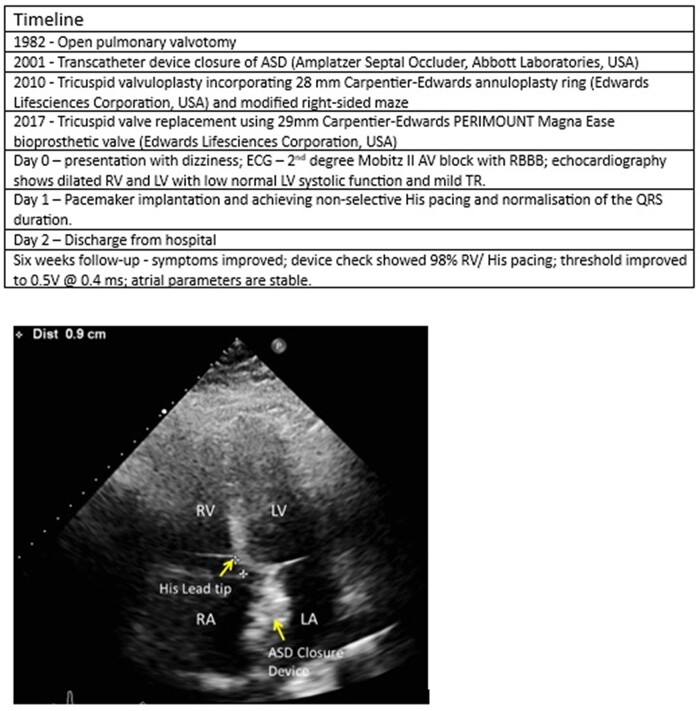
Summary figure
Case summary
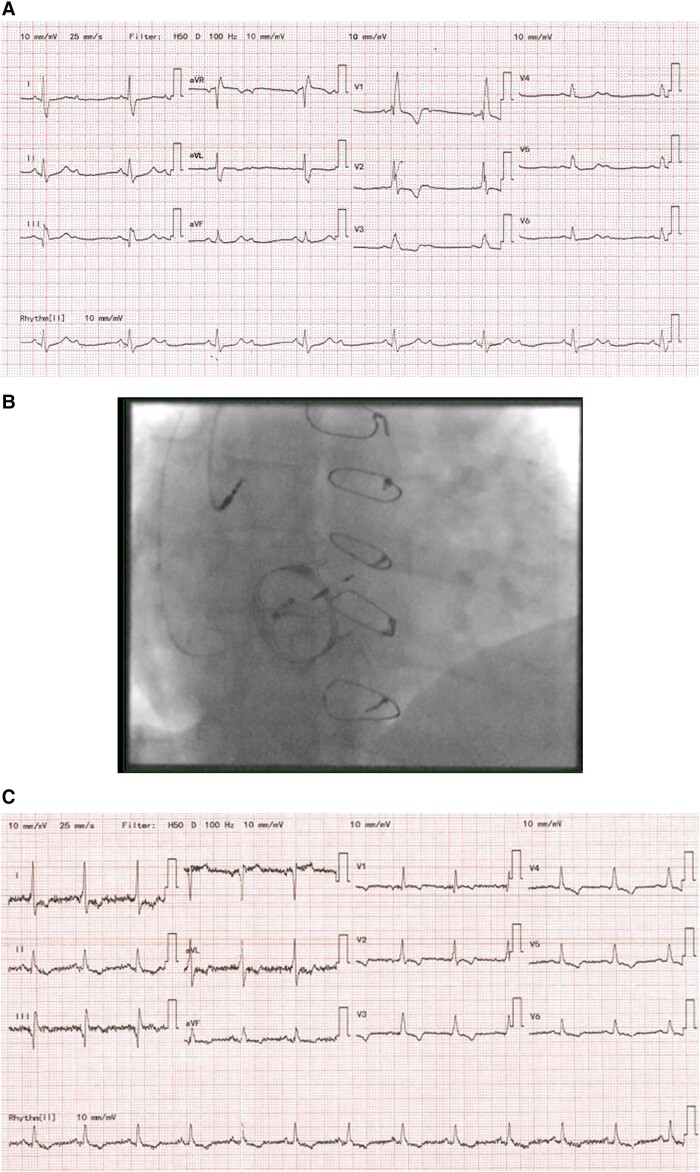
We present a case of a 42-year-old lady with a background of complex congenital heart disease, including severe pulmonary stenosis, Ebstein anomaly, and atrial septal defect (ASD). She required open pulmonary valvotomy in 1982, transcatheter device closure of ASD (Amplatzer Septal Occluder, Abbott Laboratories, USA), tricuspid valvuloplasty incorporating 28 mm Carpentier-Edwards annuloplasty ring (Edwards Lifesciences Corporation, USA), and modified right-sided maze and tricuspid valve replacement using 29 mm Carpentier-Edwards PERIMOUNT Magna Ease bioprosthetic valve (Edwards Lifesciences Corporation, USA). Her medical history also includes heterozygous factor V Leiden deficiency, benign intracranial hypertension and previous vitreous haemorrhage with bilateral papilloedema. She presented to our hospital with newly developed dizziness and previously reported shortness of breath and exercise intolerance. Her resting ECG showed a right bundle branch block, QRS of 152 ms, 2:1 heart block, and normal QRS axis (Figure 1A). Lung sounds were clear bilaterally in all lobes anteriorly and posteriorly. There was a variation in the intensity of the first heart sound consistent with a 2:1 atrioventricular (AV) block. Vital signs were stable, and laboratory tests did not show any abnormality.
Figure 1.
(A) 12-Lead ECG on admission. (B) Antero-posterior view on X-ray after pacemaker implantation. (C) 12-Lead ECG after His bundle pacemaker implantation.
Her echocardiogram showed dilated RV and LV, low normal LV systolic function, and mild tricuspid regurgitation. This represented a worsening in her LV function, which was normal on previous exams. Due to her young age and the likelihood of a long-term high percentage of RV pacing, we opted for CSP after a detailed discussion and consent from the patient.
Ultrasound-guided axillary venous access was obtained for both atrial and CSP lead. A Medtronic SelectSecure 3830 lead, 69 cm lead, and C315 HIS catheter were used to map and pace the HIS bundle. We encountered difficulties crossing the TV, so we used the deflectable C304 HIS catheter. The distal HIS position is the preferred pacing strategy at our centre. An anatomical approach was targeted at the basal RV septal site after crossing the prosthesis with a small HIS, far-field, and a large ventricular signal (Figure 1B).
We managed to achieve full correction of right bundle branch block (RBBB) with non-selective HIS pacing throughout. Pacing parameters were satisfactory with sensing of 8 mV, threshold of 1 mV at 0.4 ms, and local RV capture of 0.375 V at 0.4 ms with a paced QRS of 114 ms (Figure 1C). The patient was discharged home the next day without any acute complications.
She came for her device follow-up 6 weeks post-implantation. Symptoms improved, the device check showed 98% RV/HIS pacing, and threshold improved to 0.5 V at 0.4 ms. Atrial parameters are stable. There is a good biventricular function and trivial tricuspid regurgitation on echocardiography.
Discussion
Ebstein’s anomaly occurs when there is an apical displacement of the tricuspid valve with septal and posterior valve leaflets tethering. This condition often occurs in association with other congenital, structural, or conduction system diseases, including intracardiac shunts, valvular lesions, arrhythmias, accessory conduction pathways, and first-degree AV block.3 High-degree AV block is a rare presentation.4 Tricuspid valve surgeries and challenging morphological abnormalities in these patients often demand exceptional skills during pacemaker implantation.5 Sharma et al.6 demonstrated the feasibility of HBP in patients with RBBB allowing further widening the potential benefits of CSP. His bundle pacing can significantly benefit the physiological ventricular activation pattern. Nevertheless, it presents challenges such as the difficulty of lead implantation, reduced R-wave amplitudes, and high and unstable pacing thresholds. His bundle pacing in patients with Ebstein’s anomaly could be even more challenging as in some cases, His-potentials could be demonstrated only in the atrialized portion of the ventricle7 or because of a possible intra- and infra-hisian conduction delay.8
In this case, the HBP was confirmed by as follows:
HIS signal on the lead intracardiac electrogram.
Two different thresholds on threshold testing; first at 1 V with correction of the RBBB and second is local RV septal capture at a lower output, broader QRS notched, and LBBB morphology.
We achieved full correction of RBBB with non-selective HIS pacing accompanied by the disappearance of the patient’s symptoms.
The effect of transvalvular lead placement on tricuspid regurgitation in patients with tricuspid valve repair or replacement is an important factor to be considered before the decision for pacemaker implantation. Cardiovascular implantable electronic device-related tricuspid regurgitation due to lead placement is a possible complication of pacemaker implantation secondary to direct trauma or further interaction of the electrode leading to impingement of the leaflets and malcoaptation. In addition, leaflet adhesion, fibrosis, and encapsulation could contribute to tricuspid regurgitation.9 Alternatives to transvalvular lead implantation in patients with tricuspid valve replacement are described in the literature. Lead placement in the lateral and anterolateral veins also provides the benefit of resynchronization and presents good lead parameters.10–12 Paravalvular lead placement is achievable13 as well as leadless permanent pacemaker implantation.14
In conclusion, pacemaker implantation is challenging in patients with surgically treated complex Ebstein’s anomaly and heart block. We demonstrated that distal HIS pacing is feasible in these patients. This approach can normalize the QRS complex with a high probability of preserving or improving LV function.
Supplementary Material
Acknowledgements
G.A.N. is supported by a British Heart Foundation Programme Grant (RG/17/3/32,774) and the Medical Research Council Biomedical Catalyst Developmental Pathway Funding Scheme (MR/S037306/1).
Consent: The authors confirm that written informed consent for submission and publication of this case report including image and associated text has been obtained from the patient in line with COPE guidance.
Funding: British Heart Foundation Grant Number: RG/17/3/32,774.
Contributor Information
Ivelin Koev, Department of Cardiovascular Sciences, University of Leicester, University Rd, Leicester LE1 7RH, UK; Department of Cardiology, Glenfield Hospital, University Hospitals of Leicester NHS Trust, Groby Rd, Leicester LE3 9QP, UK.
G Andre Ng, Department of Cardiovascular Sciences, University of Leicester, University Rd, Leicester LE1 7RH, UK; Department of Cardiology, Glenfield Hospital, University Hospitals of Leicester NHS Trust, Groby Rd, Leicester LE3 9QP, UK; National Institute for Health Research Leicester Biomedical Research Centre, Leicester, UK.
Aidan P Bolger, Department of Cardiovascular Sciences, University of Leicester, University Rd, Leicester LE1 7RH, UK; National Institute for Health Research Leicester Biomedical Research Centre, Leicester, UK; East Midlands Congenital Heart Centre, Glenfield Hospital, University Hospitals of Leicester NHS Trust, Leicester, UK.
Mokhtar Ibrahim, Department of Cardiology, Glenfield Hospital, University Hospitals of Leicester NHS Trust, Groby Rd, Leicester LE3 9QP, UK.
Lead author biography
 Dr Ibrahim graduated from Ain Shams University in Egypt in 2005. He works as a consultant cardiologist and electrophysiologist at the University Hospitals of Leicester, UK. He established conduction system pacing in Leicester and leading this service nationally with education, training, and research.
Dr Ibrahim graduated from Ain Shams University in Egypt in 2005. He works as a consultant cardiologist and electrophysiologist at the University Hospitals of Leicester, UK. He established conduction system pacing in Leicester and leading this service nationally with education, training, and research.
Supplementary material
Supplementary material is available at European Heart Journal – Case Reports online.
Data availability
The data underlying this article are available in the article and in its online Supplementary material.
References
- 1. Glikson M, Nielsen JC, Kronborg MB, Michowitz Y, Auricchio A, Barbash IM, et al. 2021 ESC guidelines on cardiac pacing and cardiac resynchronization therapy. Eur Heart J 2021;42:3427–3520. [DOI] [PubMed] [Google Scholar]
- 2. Sharma PS, Dandamudi G, Herweg B, Wilson D, Singh R, Naperkowski A, et al. Permanent His-bundle pacing as an alternative to biventricular pacing for cardiac resynchronization therapy: a multicenter experience. Heart Rhythm 2018;15:413–420. [DOI] [PubMed] [Google Scholar]
- 3. Safi LM, Liberthson RR, Bhatt A. Current management of Ebstein’s anomaly in the adult. Curr Treat Options Cardiovasc Med 2016;18:56. [DOI] [PubMed] [Google Scholar]
- 4. Attenhofer Jost CH, Connolly HM, Dearani JA, Edwards WD, Danielson GK. Ebstein’s anomaly. Circulation 2007;115:277–285. [DOI] [PubMed] [Google Scholar]
- 5. Allen MR, Hayes DL, Warnes CA, Danielson GK. Permanent pacing in Ebstein’s anomaly. Pacing Clin Electrophysiol 1997;20:1243–1246. [DOI] [PubMed] [Google Scholar]
- 6. Sharma PS, Naperkowski A, Bauch TD, Chan JYS, Arnold AD, Whinnett ZI, et al. Permanent His bundle pacing for cardiac resynchronization therapy in patients with heart failure and right bundle branch block. Circ Arrhythm Electrophysiol 2018;11:e006613. [DOI] [PubMed] [Google Scholar]
- 7. von Bernuth G, Lang D, Hedayati M, Belz GG. The bundle of His electrogram in ebstein-s anomaly of the tricuspid valve. Z Kardiol 1975;64:1029–1035. [PubMed] [Google Scholar]
- 8. He BJ, Merriman AF, Cakulev I, Stambler BS, Srivastava D, Scheinman MM. Ebstein’s anomaly: review of arrhythmia types and morphogenesis of the anomaly. JACC Clin Electrophysiol 2021;7:1198–1206. [DOI] [PubMed] [Google Scholar]
- 9. Vij A, Kavinsky CJ. The clinical impact of device lead-associated tricuspid regurgitation: need for a multidisciplinary approach. Circulation 2022;145:239–241. [DOI] [PubMed] [Google Scholar]
- 10. Sideris S, Drakopoulou M, Oikonomopoulos G, Gatzoulis K, Stavropoulos G, Limperiadis D, et al. Left ventricular pacing through coronary sinus is feasible and safe for patients with prior tricuspid valve intervention. Pacing Clin Electrophysiol 2016;39:378–381. [DOI] [PubMed] [Google Scholar]
- 11. Grimard C, Clementy N, Fauchier L, Babuty D. Ventricular pacing through coronary sinus in patients with tricuspid prosthesis. Ann Thorac Surg 2010;89:e51–e52. [DOI] [PubMed] [Google Scholar]
- 12. Vijayakumar M, Kamath P, Pai PG. Permanent pacing in a patient with tricuspid prosthesis—widening therapeutic use of coronary sinus. Indian Heart J 2013;65:611–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Michaelis A, Wagner F, Riede FT, Schroeter T, Daehnert I, Pfannmueller B, et al. Performance of pacemaker leads in alternative lead positions after tricuspid valve replacement. Pacing Clin Electrophysiol 2020;43:1382–1389. [DOI] [PubMed] [Google Scholar]
- 14. Morani G, Bolzan B, Pepe A, Ribichini FL. Leadless pacemaker through tricuspid bioprosthetic valve: early experience. J Arrhythm 2021;37:414–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available in the article and in its online Supplementary material.