Abstract
Introduction
The onset of COVID-19 has caused an international upheaval of traditional in-person approaches to care delivery. Rapid system-level transitions to virtual care provision restrict the ability of healthcare professionals to evaluate care quality from the patient's perspective. This poses challenges to ensuring that patient-centered care is upheld within virtual environments. To address this, the study’s objective was to review how virtual care has impacted patient experiences and outcomes during COVID-19, through the use of patient-reported experience and outcome measures (PREMs and PROMs), respectively.
Methods
A systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines to evaluate patient responsiveness to virtual care during COVID-19. Using an exhaustive search strategy, relevant peer-reviewed articles published between January 2020 and 2022 were pulled from MEDLINE, CINAHL, EMBASE, and PsychInfo databases. Study quality was independently assessed by two reviewers using the Mixed Methods Appraisal Tool. A patient partner was consulted throughout the study to provide feedback and co-conduct the review.
Results
After removing duplicates, 6048 articles underwent title and abstract review, from which 644 studies were included in the full-text review stage. Following this, 102 articles were included in the study. Studies were published in 20 different countries, were predominantly cross-sectional, and reported on the delivery of virtual care in specialized adult outpatient settings. This review identified 29 validated PREMs and 43 PROMs. Several advantages to virtual care were identified, with patients citing greater convenience, (such as saving travel time and cost, less waiting experienced to see care providers) and increased protection from viral spread. Some studies also reported challenges patients and caregivers faced with virtual care, including feeling rushed during the virtual care appointment, lack of physical contact or examination presenting barriers, difficulty with communicating symptoms, and technology issues.
Conclusion
This review provides supportive evidence of virtual care experiences during the COVID-19 pandemic from patient and caregiver perspectives. This research provides a comprehensive overview of what patient-reported measures can be used to record virtual care quality amid and following the pandemic. Further research into healthcare professionals’ perspectives would offer a supportive lens toward a strong person-centered healthcare system.
Supplementary Information
The online version contains supplementary material available at 10.1186/s41687-023-00659-8.
Keywords: Virtual care delivery, Patient-centered care, COVID-19, Patient experience, Patient-reported outcomes, Healthcare service utilization
Introduction
The SARS2-Coronavirus 2019 (COVID) crisis has severely impacted public health and disrupted the provision of healthcare, including organizing, mobilizing, and deploying extra resources to effectively address emerging needs [1]. For instance, healthcare service delivery has been impacted in numerous ways [2], changing many essential elements vital to providing person-centered care (PCC) [3, 4], and implementing widespread use of virtual care.
Virtual care is defined as any interaction between patients and/or members of their circle of care, occurring remotely, using any forms of communication or information technologies (e.g., phone calls, videoconferences, and secure messages), to facilitate or maximize the quality and effectiveness of patient care [2, 5, 6]. Virtual care can play a vital role in emergencies by supporting healthcare needs remotely [7], streamlining the necessity of healthcare services, conserving medical resources [8], directing the medical supply on the basis of priority [9], and providing telecommunication for visitor-patient interaction[10, 11].
The COVID pandemic resulted in changes to the patient care environment, impacting the delivery of PCC [2–4]. PCC promotes adherence to treatment, improved care, better health outcomes, enhanced relationships between providers and patients, improved perceptions of doctor performance, and patient trust [3]. PCC is advocated by both patients and providers as it supports a higher quality of care [3].
Worldwide, over fifty-eight percent of the countries that experienced service disruption during the pandemic adopted virtual care delivery to continue to meet healthcare needs [12]. Hence, it is crucial to understand the impact of virtual care delivery on patient experiences and outcomes. Additionally, to deliver good patient-centred care, we need to understand what barriers or challenges present and how virtual care can be optimized. Thus, we conducted this systematic review to identify evidence on how virtual care delivery has impacted patient experiences and outcomes, both measured using validated Patient-Reported Experience Measures (PREMs) and Patient-Reported Outcome Measures (PROMs) respectively, during the first 2 years of the COVID pandemic across a spectrum of diseases and healthcare settings.
PROMs are used to assess a patient’s health status at a particular point in time, which can be completed either during an illness or while treating a health condition, or pre-and post-event to measure the impact of an intervention [13]. Capturing patient experiences is an important part of an overall effort to measure health system performance and is integral to delivering patient-centred care. Routinely applying PROMs and PREMs can enhance communication between patients and care providers, inform decisions for value-based healthcare, and improve patient care experiences and outcomes. To achieving health system goals, PROMs and PREMs are increasingly recognized for providing valuable and essential information [13]. With the onset of the COVID-19 pandemic, as the healthcare systems evolve, it becomes increasingly significant to measure healthcare delivery, PREMs, PROMs, and clinical outcomes towards a strong person-centred healthcare system.
Materials and methods
Based on the exploratory nature of this review and our objective to describe and map the literature guided by our aim outlined above, a systematic review approach was selected. The strength of the systematic review methodology is that it provides a rigorous and transparent approach of mapping the literature to ensure reliable and meaningful results for end-users [14]. Study selection and screening process was performed using the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) methodological frameworks [15]. The PROSPERO registration number is CRD42022306179. Additionally, we engaged a patient research partner with experience accessing virtual care during the COVID-19 pandemic. Our patient research partner was engaged in the conduct of this review (reviewing the study protocol, search strategy, assisting in title and abstract screening, data abstraction, reviewing this manuscript and is a co-author).
Search strategy and information sources
The preliminary search strategy was developed in collaboration with a research librarian at our University, who also has research expertise in systematic reviews. The search strategy and keywords are presented in Additional file 1. The search strategy combined structure language, keywords, and relevant synonyms. The search terms for each concept were connected through Boolean Operators ‘AND’, while search terms within each concept were combined using ‘OR’. The comprehensive search terms were tailored to each data sources, including MEDLINE, CINAHL, EMBASE, and APA PsycInfo, published from January 2020 until January 2022. To minimize publication bias and missing any relevant literature, we performed an additional search from reference lists of the included studies and grey literature sources, including google scholar and conference proceedings.
Inclusion and exclusion criteria
Inclusion criteria: (1) Population: patient, caregiver, and family member; (2) Intervention: delivery of virtual care during COVID-19; (3) Outcome: virtual care experiences, and outcomes reported by patient/caregiver/family, as well as health utilization outcomes; (4) Study Design: any studies (qualitative, quantitative, and mixed methods); (5) Peer-reviewed studies published only in English language; and (6) Only studies that used validated measures (PROMs and PREMs), as reported by the authors of the included studies.
Exclusion criteria: (1) Provider's experience; (2) Use of unvalidated patient-reported measures; (3) Clinical trials (RCT), research protocols, discussion summaries, abstracts and conference posters, systematic reviews, editorials, and letters; (4) Studies that were not in the English language.
Selection of sources of evidence
References for all included studies were uploaded and managed through Covidence. Titles and abstracts were screened for eligibility by two independent reviewers. Our team of reviewers initially screened 50 references together to ensure consistency between reviewers. For the full-text articles inclusion screening, the first five articles were reviewed by all the reviewers to ensure consistency. After that, each full-text article was reviewed by two independent reviewers. Differences between reviewers were resolved through detailed discussion and consensus or consulting a third reviewer. Differences between reviewers were resolved through detailed discussion and consensus or consulting a third reviewer.
Data charting process and data items
Two independent reviewers abstracted all relevant data following the full-text screening process for eligibility. A standardized data abstraction form was created to process all data. This form was first piloted by trained reviewers for at least two studies and revised until the authors were satisfied that all relevant data was captured accurately and comprehensively. The following information was extracted from each study for collective evaluation: author, year of publication, country, objectives, study design, patient population, virtual care delivery methods, patient reported experiences, patient reported outcomes, and health utilization outcomes. One reviewer abstracted the data, and the second reviewer checked/verified the abstracted data. Any disagreement in the abstracted data was resolved through discussion and consensus between the two reviewers, or a third reviewer was consulted, if need be. The data items abstracted from each study are presented in Tables 1, 2, and 3.
Table 1.
Descriptive characteristics of all included articles
| Study characteristics | Frequency of articles (n = 102), N(%) |
|---|---|
| Study design | |
| Cross sectional study | 34 (33.3) |
| Cohort study | 31 (30.4) |
| Qualitative research | 13 (12.7) |
| Mixed methods | 12 (11.8) |
| Case series | 3 (2.9) |
| Other | 9 (8.86) |
| Healthcare setting | |
| Specialized outpatient | 80 (78.4) |
| Acute hospital care | 8 (7.8) |
| Primary care | 5 (4.9) |
| Rehabilitation centre | 4 (3.9) |
| Mental health program | 1 (0.98) |
| Primary and specialized outpatient care | 1 (0.98) |
| Rural care | 1 (0.98) |
| Primary and postnatal care | 1 (0.98) |
| Primary and pharmaceutical care | 1 (0.98) |
| Age of study population | |
| Adult | 73 (71.6) |
| Adult; pediatric | 15 (14.7) |
| Pediatric | 11 (10.8) |
| Not Specified | 3 (2.9) |
| Mode of virtual care | |
| Video call | 34 (33.3) |
| Telephone | 22 (21.6) |
| Remote monitoring | 2 (2.0) |
| Combination (telephone and video) | 35 (34.3) |
| Other | 9 (8.2) |
Table 2.
PREMs listed in the included articles [17, 20, 21, 24, 25, 27–32, 38, 40, 44–46, 49–51, 54, 60–64, 66–79]
| Author | Study design | Name of PREM | Domains of patient experiences | Who completed? | Summary of findings |
|---|---|---|---|---|---|
| Sarre 2021 [40] | Cross-sectional | Care Quality Commission's Maternity Services Survey 2019 | (i) The start of care in your pregnancy, (ii) antenatal check-ups, (iii) during your pregnancy, (iv) labour and birth, (v) staff caring for you, (vi) care in hospital after the birth, (vii) feeding your baby, and (viii) care at home after the birth | Adult patient | Most patients felt listened to during their virtual care appointments, although 49% did provide at least one challenge they had trying to access virtual care |
|
Assenza et al. 2020 [61] Wyler et al. 2021 [62] |
Cross sectional Mixed methods |
Client Satisfaction Questionnaire (CSQ) | N/A |
Adult patient or proxy [61] Adult patient [62] |
Relatively high satisfaction was reported for both virtual care programs |
| Zimmerman et al. 2022 [63] | Cohort | Clinically Useful Patient Satisfaction Scale (CUPSS) | (i) Clinician's attitude and behavior, (ii) office environment and staff, and (iii) overall satisfaction | Adult patient | Satisfaction with treatment was similar across in-person and virtual care |
|
Pooni et al. 2021 [64] Schumm et al. 2021 [65] |
Cross sectional | Communication Assessment Tool (CAT) | (i) Physician-oriented experience, (ii) staff-oriented experience |
Pediatric patient [64] Adult patient [65] |
Pooni et al. reported that satisfaction scores were highest for domains related to the patient-physician relationship (treated with respect, showing care and concern) In Schumm et al.’s article, top-box scores were lower for telemedicine patients versus in-person for ‘the doctor spent the right amount of time with me’, doctor encouraged me to ask questions” and “the doctor checked to be sure I understood everything” |
|
Santoro et al. [50] Meno et al. [54] Schumm et al. [65] Sharma et al. [66] Shaverdian et al. [67] |
Cross sectional | Consumer Assessment of Healthcare Providers and Systems—Clinician and Group Survey (CG-CAHPS | (i) Access to care, (ii) doctor communication, and (iii) courteous/helpful staff |
Proxy [50], |
In Santoro et al., caregivers found some features of virtual visit to be better (convenient time, childcare or eldercare arrangements, travel, coordination, and wait time). In the other studies as well, virtual care was believed to be comparable if not better than in-person care. However, personal connection with their provider was higher for in-person visits |
| Kludacz-Alessandri et al. [20] | Cross-sectional | General Practice Assessment Survey (GPAS) | (i) Access, (ii) technical care, (iii) communication, (iv) interpersonal care, (v) trust, (vi) knowledge of patient, (vii) nursing care, (viii) receptionists, (ix) continuity of care, (x) referral, (xi) coordination of care, (xii) patient recommendation of GP, and (xiii) overall satisfaction | Adult patient | ~ 55% of patients sampled stated that the quality of in-person and virtual care were comparable. Benefits of virtual care related to cost and time, while issues centered on difficulty accessing electronic medical records |
| Darr et al. [25] | Cohort | General Medical Council (GMC) Patient Questionnaire | N/A | Pediatric patient or proxy | Almost all patients responded agree or strongly agree in the domains of the patient-physician relationship, privacy, and trust for virtual consultations |
| Darr et al. [25] | Cohort | Telemedicine Satisfaction and Usefulness Questionnaire (TSUQ) | (i) Usefulness and (2) satisfaction | Pediatric patient or proxy | Patient satisfaction with virtual care was high in the domains of the patient-physician relationship, privacy, and trust |
| Horgan et al. [31] | Cohort | Generic Medical Interview Satisfaction Scale (G-MISS) | (i) Relief, (ii) communication, and (iii) compliance | Adult patient | Satisfaction for virtual care was high, with ~ 80% stating they would have a telephone consultation again |
| Dratch et al. [23] | Cohort | Genetic Counseling Satisfaction Scale (GCSS) [23] | N/A | Adult patient | Most patients (73%) felt virtual care improved access to services and voiced a preference for a combination of in-person and virtual care in the future |
| Wee et al. [68] | Cross-sectional | Groups Health Association of America Patient Satisfaction Survey | N/A | Adult patient | No significant difference in patient satisfaction was measured between, in-person, direct access, or virtual care |
| Piro et al. [69] | Cohort | Home Monitoring Acceptance and Satisfaction Questionnaire (HoMASQ) | (i) Relationship with their healthcare provider, (ii) ease of use of home monitoring technology, (iii) related psychological aspects, (iv) implications on general health, and (v) overall satisfaction | Adult patient | No significant difference between in-person and virtual (home) care satisfaction were provided; however, self-reported anxiety during virtual care was lower than in-person |
| Quinn et al. [21] | Cross sectional | Telephone Clinic Care survey | N/A | Adult patient | 86% of women described their virtual consultation as “good” or “very good” with 25% preferring virtual over in-person care |
| Bartoletta et al. [30] | Cohort | Press Ganey Medical Practice Telemedicine Survey | (i) Accessibility to virtual clinical encounter, (ii) care provider, (iii) telemedicine technology, and (iv) overall assessment of telemedicine visit | Adult patient | Most patients responded that arranging and connecting to a telemedicine visit, talking with the provider over a video connection, and having the provider understand the clinical problem were “very good” |
|
Bartoletta et al. [30] Porche et al. [71] Richards et al. [70] |
Cohort Cross sectional |
Press Ganey Outpatient Medical Practice Survey (PGOMPS) 2023-11-17 7:33:00 PM | (i) Access, (ii) moving through your visit, (iii) nurse/assistant, (iv) care provider, (v) personal issues, (vi) overall assessment, and (vii) telemedicine technology (added March 2020) | Adult patient | Satisfaction across all patient groups receiving virtual care was high, with improvement suggestions targeting technological challenges. [30, 70] No significant difference in satisfaction was measured between virtual and in-person care. [71] |
| Alshareef et al. [51] | Cross sectional | Questionnaire for Assessing Patient Satisfaction with Video Teleconsultation | (i) Equipment/technical issues, (ii) communication and rapport, (iii) clinical assessment, and (iv) program evaluation | Adult patient | Thirty-seven respondents (90.2%) agreed that telemedicine is cost and time efficient compared to conventional in-office visits. Of the 41 respondents, 35 (85.4%) patients thought it was easy to gain access to specialist care by telemedicine |
| Pooni et al. [64] | Cross sectional | RAND Visit-Specific Satisfaction Instrument (VSQ-9) | N/A | Pediatric patient | Patient satisfaction was related most closely with the caregiver’s inter-personal and technical skills. The lowest rated scores addressed patient wait times and challenges accessing the office by phone |
| Zimmerman et al. 2020[44] | Cross sectional | Service User Technology Acceptability Questionnaire (SUTAQ) | (i) Enhanced care, (ii) increased accessibility, (iii) privacy and discomfort, (iv) care personnel concern, (v) kit as substitution and (vi) satisfaction | Adult patient | Most patients stated that virtual care saved them time, increased care accessibility, improved their health, and facilitated improved monitoring of their symptoms |
| Wyler et al. [62] | Mixed Methods | Session Evaluation Questionnaire (SEQ) | (i) Session evaluation and (ii) post-session mood | Adult patient | Patient satisfaction with in-person and virtual care were not significantly different, however, patients and therapists did state the virtual care produced more superficial dialogue |
| Birkhoff et al. [27] | Mixed Methods | System Usability Scale (SUS) | N/A | Adult patient | 50% of patients felt that in-person and virtual nursing visits provided comparable care. Patients that did not prefer virtual care mentioned difficulties navigating technology or taking their own vitals |
|
Mojdehbakhsh et al. [17] Darr et al. [25] Edge et al. [28] Efthymiadis et al. [46] Chen et al. [72] |
Cohort Cross-sectional |
Telehealth Satisfaction Scale (TeSS) | N/A | Adult patient [17, 28, 46], pediatric patient or proxy (25), adult or pediatric patient or proxy [72] | Satisfaction across all patient groups receiving virtual care was high, however, Edge et al. reported lower scores regarding the psychological and emotional support the patients’ received through virtual care |
|
Peahl et al. [19] Dratch et al. [24] Darr et al. [25] Adamou et al. [33] Triantafillou et al. [35] Waqar-Cowles et al. [39] Fung et al.[45] Galaviz et al. [74] Park et al. [52] Finn et al. [73] Al-Sharif et al. [58] |
cohort Cross sectional Mixed methods |
Telehealth Usability Questionnaire (TUQ) | (i) Usefulness, (ii) ease of use, (iii) effectiveness (interface and interaction quality), (iv) reliability, and (v) satisfaction |
adult patient [19, 24, 33, 35, 73] adult or pediatric patient [52, 58] adult patient or proxy [39] pediatric patient or proxy [25] |
When experiential domains are assessed individually, satisfaction is reported to be relatively high, however, when virtual is directly compared to in-person care, satisfaction scores showed a significant drop in score. Triantafillou et al. [35], reported lower satisfaction levels addressing the patient-physician relationship |
| Waqar-Cowles et al. [39] | Cross sectional | Telemedicine practice in neurosurgery during COVID-19 era: an anonymized patient survey | N/A | Adult patient | ~ 97% of patients felt that their virtual care was beneficial in the context of COVID-19, with 33% of patients stating a preference for virtual over in-person care. The most common suggestion for the program was to implement video-based consults |
|
Nair et al. [32] Rush et al. [78] Wright et al. [75] Pareyson et al. [77] Pinar et al. [76] Banks et al. [49] |
Cross sectional Cohort Mixed-methods |
Telemedicine Satisfaction Questionnaire (TSQ) | (i) Quality of care provided, (ii) similarity to face-to-face encounter, and (iii) perception of the interaction |
Adult patient [32, 49, 75, 76, 78] adult patient or proxy [77] |
Satisfaction across all patient groups was relatively high, however, preference for virtual care was particularly associated with difficulty accessing in-person services and current disease stability |
| Ruelos et al. [23] | Cross sectional | Telehealth Satisfaction Questionnaire | Communication; convenience; privacy; other: ability to save time, trust of the telehealth system, the system is easy to learn, lack of physical contact, ability to meet patient's needs | Adult | Most patients favored telehealth because of its ease of use, convenience, and ability to save time |
| Murthy et al. [79] | Cross sectional | Your Virtual Appointment: Your Experience | N/A | Adult patient | Preference for in-person (14%) relative to virtual care (19%) was mixed, with technological difficulties and clinical limitations referenced for virtual care hesitancy |
| Watson et al. [38] | Mixed methods | Your Voice Matters (YVM) | (i) Appoint arrival, (ii) appoint duration, and (iii) leaving the appointment | Adult patient | Measured levels of satisfaction were significantly lower among patient receiving treatment relative to those undergoing follow-up |
| Raheja et al. [29] | Cross sectional | Patient satisfaction with telemedicine services survey | Communication; information | Adult patient | The majority of patients (either agreed/strongly agreed that the time allotted for their queries during teleconsults was sufficient |
| Imlach et al. [26] | Mixed Methods | Primary Care Patient Experience Survey | Respect; communication; convenience; Other: spend enough time, need to be seen in-person, relationships, technological barriers, views on values, patient preferences | Adult patient | Many respondents mentioned the convenience of telehealth consultations, in terms of saving time and money, and reducing stress, travel, employment disruption and exposure to infection (with COVID-19 and other pathogens) |
Table 3.
| Author | Study design | Disease/condition specific group | Name of PROM | Summary of findings |
|---|---|---|---|---|
| Riegler et al. [98] | Cohort | Mental Health | Center for Epidemiological Studies Depression Scale (CES-D) | Veterans reported significant reduction in symptoms of depressions after the telepsychotherapy parenting skills intervention |
| Eyberg Child Behavior Inventory | Frequency of clinically significant scores pre- and post-treatment were significantly different | |||
| Levinson et al. [103] | Cohort | Beck Depression Inventory II | Changes in BDI scores were not significantly different between in-person and virtual groups | |
| The Frost Multidimensional Perfectionism Scale (FMPS) | Changes in FMPS scores were not significantly different between in-person and virtual groups (pre to post treatment) | |||
| Bulkes et al. [108] | Cohort | Quick Inventory of Depression Symptomology-Self Report (QIDS-SR) | Admission and discharge QIDS-SR scores for the in-person and virtual care groups were not significantly different | |
| Zimmermann et al. [63] | Cross sectional | Remission from Depression Questionnaire (RDQ) | Significant improvements in RDQ scores between time points were recorded for virtual relative in in-person care | |
| Raykos et al. [92] | Case series | PROMIS-Anxiety and Depression scales, Short Form 8a | Statistically significant improvements in PROMIS scores were reported as therapy progressed | |
| Eating Disorders-15 Questionnaire (ED-15) | Statistically significant improvements in ED-15 scores were reported as therapy progressed | |||
|
Raykos et al. [92] Levinson et al. [103] Steiger et al. [104] |
Case series Cohort |
Eating Disorder Examination Question Version 4.0 (EDE-Q-IV) | Levinson and Steiger et al. reported that changes in EDE-Q-IV scores were not significantly different between in-person and virtual groups. Raykos et al., found statistically significant improvements in EDE-Q-IV scoring as therapy progressed | |
| Rezich et al. [109] | Cross sectional | Hospital Anxiety and Depression Scale (HADS) | Patient responsiveness to telehealth was unconnected to their respective HADS score | |
|
Piro et al. [69] Craig et al. [90] Steiger et al. [104] Graziano et al. [99] |
Cohort Experimental |
Generalized Anxiety Disorder (GAD-7) | Craig et al. [90], reported no significant difference in GAD-7 scores between satisfied and unsatisfied patients. Graziano et al. [99], showed significant reductions in depression at the two time points. Lastly, Steiger et al. [104], calculated negligible interactions between the mode of care delivery and GAD scoring | |
| van Agteren et al. [100] | Experimental | Mental Health Continuum Short Form (MHC-SF) | Participants reported mental well-being improvements before and after exposure to virtual care | |
| Ahmad et al. [91] | Cohort | Gastrointestinal | Baylor Continence Score (BCS) | BCS scores significantly improved following the virtual Bowel Movement Program |
| Cleveland Clinic Constipation Score (CCCS) | CCCS scores did not significantly improve following the virtual Bowel Movement Program | |||
| Vancouver Symptom Score for Dysfunctional Elimination Syndrome (VSS) | Significant improvements in VSS scores were reported at the 1-month and 3-month follow-up time points | |||
| Sabbagh et al.[102] | Cohort | Musculoskeletal | American Shoulder and Elbow Surgeons (ASES) Standardized Shoulder Assessment Form | No significant difference in outcomes were reported between the virtual and in-person care groups |
| Ganderton et al. [94] | Longitudinal (pre-post intervention) | Melbourne Instability Shoulder Scale (MISS) | Significant and clinically relevant improvements in MISS scores were reported at follow-up | |
| Short form Orebro Musculoskeletal Pain Questionnaire (ÖMSPQ) | Significant improvements in patient scores were reported at all follow-up meetings | |||
| Shoulder Instability Index (WOSI) | Excluding the physical subsection of the PROM, patients reported significant improvements in their WOSI scores | |||
| Tampa Scale for Kinesiophobia | The scale reported clinically significant reductions in pain-related fear at the 6-week and 12-week time points | |||
| Alsobayel et al. [95] | Cross sectional | Musculoskeletal Health Questionnaire (MSK-HQ) | Significant improvements in the MSK-HQ were recorded between baseline and follow-up | |
| Pain Self-Efficacy Questionnaire | Significant improvements in the Pain Self-Efficacy Questionnaire were recorded between baseline and follow-up | |||
| Wu et al. [106] | Cohort | Functional Assessment of Chronic Illness Therapy (FACIT)—Fatigue Scale | A significant increase in FACIT scores were reported after treatment | |
| Craig et al. [90] | Cohort | Neck Disability Index (NDI) | No significant difference in NDI scores were reported between satisfied and unsatisfied patients | |
| Oswestry Disability Index | No significant difference in Disability Index scores were reported between satisfied and unsatisfied patients | |||
| Corona et al. [107] | Cohort | Early Childhood Development | MacArthur-Bates Communicative Development Inventory (MCDI) | No statistically significant findings were reported between the in-person and virtual treatment groups |
| Lai et al. [96] | Experimental | Neurological | Quality of Life in Alzheimer's Disease (QoL-AD) | Significant improvements in QoL-AD scoring were reported for video calling relatively in audio-only meetings |
| Revised Memory and Behavior Problem Checklist (RMBPC) | No significant improvements in RMBPC scoring were reported for video calling relatively in audio-only meetings | |||
| Daswani et al. [97] | Case series | Respiratory | St George's Respiratory Questionnaire (SGRQ) | An average SGRQ improvement of 71% was reported by patients |
| Generic PROMs | ||||
| Raykos et al. [92] | Case series | N/A | Clinical Impairment Assessment (CIA) | Large decreases in patient-reported impairment was recorded |
| Thesenvitz et al. [105] | Cohort | EuroQol Five Dimension—Five Level (EQ-5D-5L) | Reported no statistically significant difference in scores between baseline and follow-up | |
|
Sabbagh et al. [102] Wu et al. [106] |
Cohort | EuroQol Five Dimension—Three Level (EQ-5D-3L) | Wu et al., reported no significant difference in patient scores before and after treatment. Sabbagh et al., found no significant difference in scoring between in-person and virtual treatment groups | |
| Lotan et al. [93] | Case series | Goal Attainment Scale (GAS) | Improvements in patient outcomes were reported in those receiving virtual care | |
|
Craig et al.[90] Steiger et al. [104] Graziano et al. [99] |
Cohort Experimental |
Patient Health Questionnaire (PHQ-9) | Craig et al., reported no significant difference in PHQ-9 scores between satisfied and unsatisfied patients. Graziano et al., showed significant reductions in depression at the two time points. Lastly, Steiger et al., calculated negligible interactions between the mode of care delivery and PHQ-9 scoring | |
| Alsobayel et al. [95] | Cross sectional | Patient-Specific Functional Scale | Significant improvements in the Patient-Specific Functional Scale were recorded between baseline and follow-up | |
| Ahmad et al. [91] | Cohort | Pediatric Quality of Life Inventory (PedsQL) | No statistically or clinically significant improvements in PedsQL scores were reported | |
| Bulkes et al. [108] | Cohort | Quality of Life Enjoyment and Satisfaction Questionnaire—Short Form (Q-LES-Q) | Admission and discharge Q-LES-Q scores for the in-person and virtual care groups were not significantly different | |
| van Agteren et al. [100] | Experimental | Satisfaction with Life Scale (SWLS) | Participants reported in increase in mental well-being before and after exposure to virtual care | |
|
Bernocchi et al. [101] Sabbagh et al. [102] |
Cohort | Short form (SF-12) Quality of Life Questionnaire | Sabbagh et al., found no significant difference in scoring between in-person and virtual treatment groups. Bernocchi et al., reported a significant improvement in the mental component but not the physical component of the survey | |
| Lai et al. [96] | Experimental | Short Form 36 Version 2 (SF-36v2) Quality of Life Questionnaire | Significant improvements in SF-36v2 scoring were reported for video calling relatively in audio-only meetings | |
| Zarit Burden Interview Scale (ZBI) | Significant improvements in ZBI scoring were reported for video calling relatively in audio-only meetings | |||
| Riegler et al. [98] | Cohort | Strengths and Difficulties Questionnaire (SDQ) | Statistically significant improvements in the SDQ were reported pre- and post-treatment | |
| Craig et al. [90] | Cohort | Visual Analog Scale (VAS) | No significant difference in VAS scores were reported between satisfied and unsatisfied patients |
Included surveys: [38]
Quality assessment
The Mixed Methods Appraisal Tool (MMAT) Version 2018 was used to assess the quality of all included studies [16]. Using the Mixed-Methods Assessment Tool (MMAT), the included articles demonstrated a relatively high degree of transparency in the presentation of their methods and results. Study quality did not dictate article exclusion from the review and, as such, these articles were still included in data extraction and analysis. Please note as well that using the MMAT questions to generate an overall score or rating of the articles is discouraged by the creators of the tool. For a more thorough overview of included study quality, please refer to the Additional file 2.
Data analysis
A careful assessment of data and analysis from all included studies was performed to establish and validate any conclusions regarding virtual care experiences during COVID-19. Bibliographic data, the population, and the setting for included studies are summarized using descriptive statistics in Table 1. The patient reported experiences, outcomes, and utilizations are synthesized in Tables 2 and 3. We summarized the results of the qualitative data by patient experience domains, guided by the qualitative software analysis, NVivo.
Results
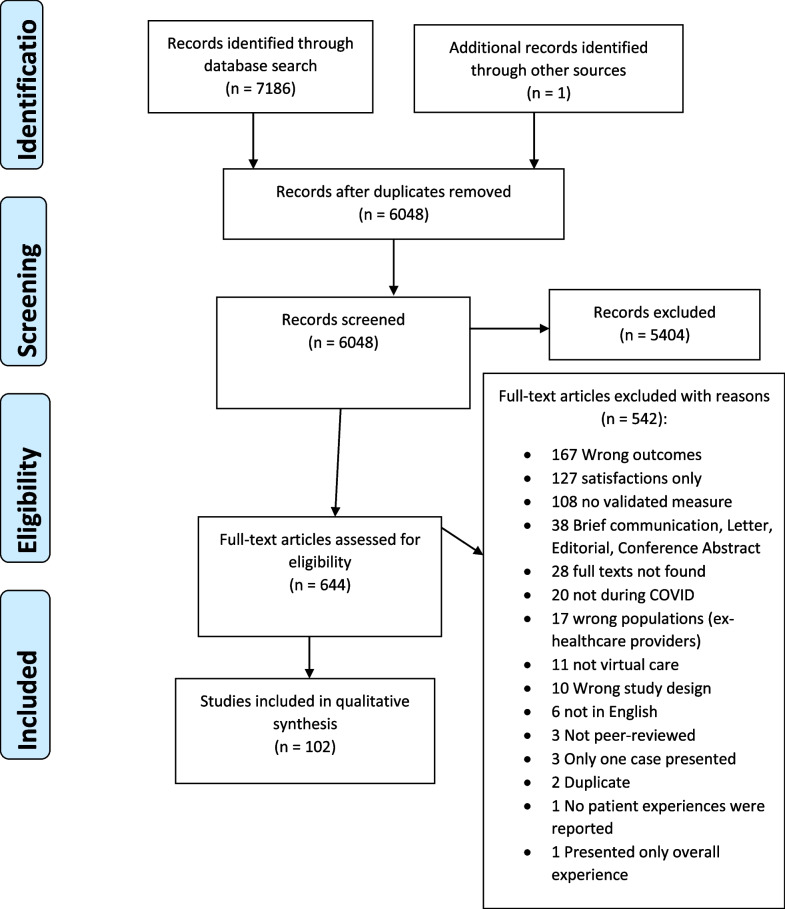
After excluding duplicates, our search captured 6048 records for the title and abstract review. After title and abstract screening, a total of 644 peer-reviewed articles were assessed for full text review. Then, after full text review, we included 102 articles in this review (Fig. 1). Reasons for exclusion included articles reporting wrong outcomes, assessing satisfaction, not validated PROMs/PREMs, full-text unavailable, and wrong timing—not during COVID-19.
Fig. 1.
PRISMA for flow chart of the literature review and article identification process
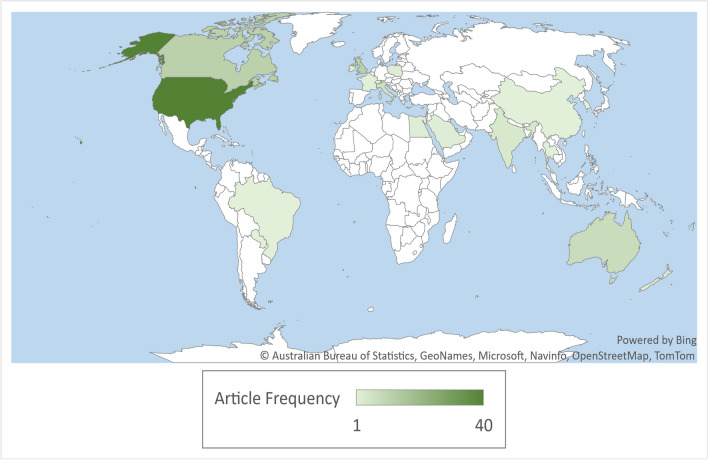
Table 1 depicts the descriptive summary of included articles. Most articles (39.2%) were published in the USA, followed by Canada (12.7%), United Kingdom (11.8%), Australia (7.8%), Italy (5.9%), and India (3.9%) (Fig. 2). Studies were of cross-sectional design (33.3%), cohort (30.4%), qualitative (12.7%), mixed methods research (11.8%), case series (2.9%), non-randomized experimental (2%), and other study designs (6.86%). In regard to the quality of the included studies, most articles addressed all (n = 41) or four out of five (n = 42) of the quality criteria listed in the assessment tool. While 19 articles fell below this quality threshold.
Fig. 2.
World map displaying the geographic origin of the articles included in the systematic review
Most studies reported virtual care delivered in the specialized outpatient setting (78.4%) during COVID-19. Some studies reported virtual care delivery in acute hospital care settings (7.8%), primary care (4.9%), and in rehabilitation centers (3.9%). Studies reported delivery of virtual care via telephone and video (34.3%), video only (33.3%), telephone only (21.6%), remote monitoring (2%), and other (8.2%). Most studies explored virtual care delivery for adults (71.6%), some reporting both adult and pediatric populations (14.7%), and few articles that reported delivery of virtual care for pediatric populations (10.8%). Most virtual care delivery was in the year 2020 (90.2%).
Identification of Patient-Reported Experiences Measures (PREMs)
Table 2 highlights the 29 validated Patient-Reported Experience Measures (PREMs) identified in the review from 47 articles that evaluated the patient experience of receiving virtual care during COVID-19. Some articles used more than one PREM. Most of these measures were completed by adult patients. Common measures included The Telehealth Usability Questionnaire (reported by 11 studies), Telemedicine Satisfaction Questionnaire (reported by 6 studies), Telehealth Satisfaction Scale (TeSS) (reported by 5 studies), and Consumer Assessment of Healthcare Providers and Systems—Clinician and Group Survey (CG-CAHPS) (reported by 5 studies). Common domains associated with these measures included access to care, communication, and domains specific to the clinician's attitude and behavior.
Benefits of virtual care delivery
Findings from patient experience measures (PREMs) highlight positive responses on virtual care from patients in various domains. Some examples include feeling comfortable in receiving care virtually (e.g. due to privacy) (n = 8, 17%) [17–25], feeling safe against COVID-19 (n = 5, 11%) [18, 21, 26–29], communication with healthcare providers (n = 31, 66%) [17, [17, 20–24, 30–43], the convenience of virtual care and saving time (n = 24, 51%) (e.g. minimizing barriers such as transportation, traffic, cost of gas and parking, and associated anxiety) [20–23, 26, 28–33, 35, 37–39, 43–55], access to care (n = 9, 19%) [19, 22, 24, 28, 35, 38, 43–45, 51, 56, 57], patient engagement in care (n = 4, 9%) [36, 37, 44], comfort in the technology/telehealth system (n = 17, 36%) [27, 28, 35, 51], and not experiencing wait time delays in seeing their healthcare providers (n = 8, 17%) [22, 28, 46, 50, 54].
In the studies that included qualitative findings, we get an in-depth understanding of the experiences of patients and caregivers with virtual care delivery during COVID-19. For instance, in the study by Al-Sharif et al.[58], they found convenience and safety to be two major advantages to virtual care delivery, especially with the high risk of getting infected with COVID-19. Juarez-Reyes et al.[59] found patient participants expressed gratitude for continued mental health support, and being able to still be a part of virtual group sessions.
Barriers with virtual care
Some studies that used PREMs and also qualitative interviews reported challenges patients and caregivers faced with virtual care, such as feeling rushed during the virtual appointment (2% of PREMs articles) [26, 38, 48], lack of physical contact with the healthcare provider for physical examinations (15% of PREMs articles) [21, 23, 26, 35, 58, 87, 88], technical challenges (2% of PREMs articles) [26, 29, 35, 37, 43, 48, 56, 77], a preference for in-person care delivery (8.5% of PREMs articles) (e.g. due to the lack of personal connection with healthcare provider online) [21, 23, 28, 38, 41, 54, 88, 89], and difficulty with communicating symptoms or asking all of their questions (6% of PREMs articles) [29, 87, 90]. For instance, the study by Gibbs et al. [48] found that adult clients undergoing assessment for autism were concerned about communication difficulties in the online environment, especially with using and reading body language and feeling self-conscious about seeing themselves on screen. Adult clients and parents/caregivers were also concerned with clinicians possibly missing certain subtle behaviors not apparent on screen [47]. The study by Stirling Cameron et al. [42] found telehealth appointments to be challenging for Syrian refugee women who used interpreters for their appointments. The women expressed disappointment with back-and-forth telephone calls, and not being able to effectively communicate with their primary care providers [42].
Identification of Patient-Reported Outcome Measures (PROMs)
We identified 43 validated Patient-Reported Outcome Measures (PROMs) that assessed patient health status during the COVID-19 pandemic (Table 3). The Generalized Anxiety Disorder (GAD-7) (used in 4 studies), Eating Disorder Examination Question Version 4.0 (EDE-Q-IV) (used in 3 studies), and Patient Health Questionnaire (PHQ-9) (used in 3 studies) were the only measures reported in more than one study. All other studies utilized various PROMs. Specific PROMs were grouped by disease/condition such as PROMs for Mental Health (n = 12, 28%), Gastrointestinal (n = 2, 7%), Musculoskeletal (n = 10, 23%), Early Childhood Development (n = 1, 2%), Neurological (n = 2, 5%), and Respiratory (n = 1, 2%). Additionally, fourteen generic PROMs were identified such as the Short Form (SF-12) Quality of Life Questionnaire, Patient Health Questionnaire (PHQ-9), and the Pediatric Quality of Life Inventory (PedsQL). These studies administered PROMs following virtual care delivery. Some studies found that patients had improvements in quality of life and reduction in symptoms [91–98], such as improvements in mental health and wellbeing [63, 92, 96, 99–101]. However, some studies also reported no significant differences in PROMs scores before and after virtual care or between different treatment groups (in-person care vs virtual care) [90, 91, 96, 102–108]. A summary of the findings from the studies is included in Table 3.
Impact of virtual care delivery on healthcare use
Eleven studies evaluated the impact of virtual care delivery on healthcare use [105, 108, 110–118]. Nascimento et al. [110] evaluated the impact of telemedicine on visits to emergency departments and hospital admissions during the pandemic in Brazil. They found rates of ED visits and hospital admissions were respectively, 17.3% and 2.3% for patients who attended at least one teleconsultation. Kesavadev et al. [111] reported successful prevention of hospitalization for nearly all patients in a virtual in-patient program. In the study by Thesenvitz et al.[105], patients reported less use of services such as Alberta’s Health Link advice line, emergency department visits, and visits with family physicians.
Discussion
During the COVID-19 pandemic, infection control efforts have necessitated the reduction of in-person clinical visits and routine procedures leading to provider- and system-level changes in the delivery of PCC. This change might have altered patient experiences with their care, and measuring patient experiences becomes increasingly significant toward a strong person-centered healthcare system. In this review, we provide an overview of the PREMs and PROMs that have been utilized to assess patient experiences with virtual care and patient-reported outcomes during the COVID-19 pandemic. Following initial screening and full-text review, 102 articles were included in this study. These studies demonstrated large heterogeneity in study design, population of interest, and virtual care modality. Most articles targeted the delivery of virtual care in specialized outpatient settings (78.4%), including fields such as oncology, dementia, neurology, urology, dermatology, and psychiatry. Studies also primarily assessed adult responses to virtual care delivery (71.6%), with far fewer studies exclusively assessing the perspectives of pediatric patients (10.8%). We also found that a relatively even number of studies assessed patient experiences with virtual care delivery via videoconferencing (33.3%), telephone calls (21.6%), or a combination of both (34.3%). While prior systematic reviews have examined PREM and PROM utilization in various in-person care settings, this study is distinct in its focus on studies that used patient-reported measures to gauge patient experiences to virtual care during the pandemic.
The sheer number of articles (N = 102) included in this review highlight the breadth of information available on patient-reported measures that were used during the virtual care provision, as well as the adaptability of international health systems. This also provides evidence of the importance healthcare professionals ascribe to amplifying the patient voice. Despite this, review findings also show increased investment in specific patient populations, leading to the potential absence of other patient groups.
One specific group that was underrepresented in this review was pediatric patients, as we found a limited number of studies conducted in this population (10.8% of studies were pediatric focused). The lack of research into the experiences and outcomes of pediatric patients receiving virtual care signifies a gap in knowledge that could provide incredibly useful insight into pediatric care provision. Santoro et al., [50] discuss the foreseeable benefits of virtual care for pediatric patients, highlighting the involvement of one or more caregivers in the transportation and supervision of pediatric patients during in-person visits in 2021. From the pediatric studies in this review, patient caregivers discussed the convenience and cost-benefits of virtual care [18, 50, 107].
A second underrepresented patient population in this review are primary (i.e., general) care recipients. Even though primary care serves as the first interaction many patients have with the healthcare system, patient experience in primary care was only assessed in 4.9% of the articles pulled. Not capturing patient perspectives on virtual primary care delivery could significantly impact other healthcare areas by restricting the ability of general practitioners to communicate, treat, and refer patients to specialists effectively.
Another concern with virtual care provision, irrespective of the patient population being researched, is acknowledging the patients who were unable to access virtual care. Virtual care has been shown to exacerbate health inequities, creating what has been termed the “digital divide” whereby health information technology and virtual care disproportionately exclude already marginalized populations from accessing care [53, 119]. This is of particular concern during the COVID-19 pandemic, as rapid transitions from in-person to virtual care have primarily been implemented using a health systems perspective with limited consideration for diverse patient partnerships [120, 121]. The potential bottlenecking of the types of patients included in this review should therefore be needed, with greater efforts placed on broadening and adapting virtual care efforts to better suit the care needs of all patients in future research.
The patient-reported measures identified in the review often addressed care accessibility, patient-care team communication, and clinician attitudes and behavior with patients during virtual care. Several advantages to virtual care were identified, with patients citing greater convenience and increased protection from viral spread. Other literature supports these findings, explaining the potential of virtual care to alleviate barriers to care in rural and geographically isolated communities [122, 123]. Buyting et al. [124], discusses the benefits of virtual care in rural settings when a priori work is done to ensure all interventions are appropriate to the population of interest. Greater ease of access to care was also evaluated by Darr et al. [25], who identified a correlation between virtual care provision and a reduction in non-attendance rates. This also highlights the potential economic benefits of virtual care, as non-attendance rates are closely linked to increased healthcare utilization [25, 125]. In addition to virtual care's advantages, patients also mentioned various challenges. Barriers to virtual care included difficulty navigating online platforms, a need for greater technical support or educational materials, and the lack of physical interactions with healthcare providers. Edge et al. [28], reported that some patients felt they received worsened psychological support through virtual care and experienced greater difficulty understanding the clinical information shared by their healthcare provider. In response to this, 1 in 5 patients were hesitant to use virtual care in the future [28].
Virtual care is associated with various benefits and challenges, offering increased access to care during times of public isolation but also restricting care to populations experiencing social marginalization or with limited technological infrastructure [126]. The polarity of responses to virtual care raises the question of whether this mode of care will continue beyond the pandemic or if care will largely return to in-person once safe to do so. While a large proportion of patients included in the review mainly expressed positive reactions to virtual care, with some stating a preference for virtual care over in-person visits, consideration should also be applied to those not heard in these studies. Therefore, if this were to continue long-term, greater attention needs to be directed toward making technology a facilitator instead of a barrier to care access. Perhaps the most promising approach to virtual care in the future is implementing specialty-specific triage practices to provide patients with the most appropriate care. Other researchers have proposed this, promoting the benefits of triaging for better allocation of resources, assessment of disease acuity, and accommodation to various social factors [127, 128].
Irrespective of the degree to which virtual care is used in the future, this research provides a comprehensive overview of what patient-reported measures can be used by healthcare professionals to evaluate virtual care quality. As virtual care represents a burgeoning approach to care provision, utilizing these measures (PROMs/PREMs) can be crucial to ensuring that the services provided are grounded in patient-centeredness [129]. This study has implications on all conceivable aspects of virtual clinical practice, by equipping healthcare professionals with the means to respond to the needs of their specific patient population.
Strengths and limitations
One key strength of this study was the patient-oriented approach. We engaged a patient research partner in our team who was involved in reviewing the study protocol, title and abstract screening, data abstraction, reviewing the results and is a co-author in this manuscript. Additionally, we enlisted the support of a research librarian to ensure our search strategy was comprehensive.
Despite the methodological rigor applied in this review, this study was not immune to limitations. One potential issue with this study is that, while the review included studies published between January 2020 and January 2022, the vast majority (90.2%) of included articles detailed work conducted in 2020. Limited information on patient experiences further into the pandemic restricted our ability to assess the effects of patient and family burnout from continued virtual care use. Another possible limitation of this study relates to our focus on patient and family responses to virtual care, exclusively. While this does exclude the perspectives of healthcare providers and administrators, our emphasis on the patient voice was also a deliberate choice to display the experiences of virtual care recipients. Another limitation in this study was our inability to perform a meta-analysis due to the inclusion of studies that differed across statistical and methodological characteristics. Lastly, though not a limitation of this review, a recurrent issue experienced in studies examining the use of PREMs, is the common, yet misguided practice, of using “experience” and “satisfaction” as interchangeable terms. These terms, while seemingly similar, do have distinct qualities with “satisfaction” associated with greater subjectivity and potentially reflecting patient expectations more so than “experience” which describes objective aspects of patient care [130, 131].
Conclusions
In future studies, it would be efficacious to explore more recent patient experiences with virtual care as well as the experiences of other key stakeholders. Improved patient receptivity to care at the onset of the pandemic has been previously documented, however, patient experiences further into the pandemic is lacking. Due to widespread burnout within the healthcare system, assessing more recently completed patient-reported measures may paint a different picture of the benefits of virtual care [132]. Additionally, further research into healthcare professionals' perspectives (I.e., healthcare providers and administrators) would offer an alternative lens on the practicality and feasibility of long-term virtual care.
Supplementary Information
Additional file 2. Quality Assessment of Included Studies.
Acknowledgements
We would like to acknowledge the support of Sydney Palmer in title, abstract review, and data extraction.
Author contributions
MJS conceptualized and lead this work, assisted with the development of the search strategy. BB developed the search strategy with the help of SA and PF and MJS critically reviewed and approved the search strategy. BB searched the database. BB, SA, PF, SR, VK, and MJS extracted the data and did quality assessment of the papers. BB, SA, and SR drafted the manuscript. MJS, PF, and VK edited and revised the manuscript. All the authors were involved in revising, editing, and finalizing the published version of the manuscript. MJS is accountable for all aspects of the work and ensures that questions related to the accuracy and integrity of work is appropriately investigated and resolved.
Funding
This work was supported by the Alberta SPOR SUPPORT (Support for People and Patient-Oriented Research and Trials) Unit (AbSPORU) Patient Engagement (PE) Team. The senior author (MJS) is the provincial Lead of the AbSPORU Patient Engagement Team.
Availability of data and materials
Data available upon request to the authors.
Declarations:
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.(2020) WHO Director-General’s opening remarks at the media briefing on COVID-19 [news released]. In: World Health Organization. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- 2.Zafar A (2020) Many Canadians used virtual medical care during COVID-19, poll suggests. In: Canadian Broadcasting Corporation. https://www.cbc.ca/news/health/virtual-care-cma-survey-1.5603713
- 3.Alberta Health Services Proclamation on Person-Centered Care Core Values
- 4.Santana MJ, Manalili K, Jolley RJ, Zelinsky S, Quan H, Lu M. How to practice person-centred care: a conceptual framework. Health Expect. 2018;21:429–440. doi: 10.1111/hex.12640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Virtual Healthcare in Canada. In: Elicare Medical. https://www.elicare.ca/virtual-healthcare
- 6.Justin Trudeau, Prime Minister of Canada (2020) Prime Minister announces virtual care and mental health tools for Canadians. In: Prime Minister of Canada. https://pm.gc.ca/en/news/news-releases/2020/05/03/prime-minister-announces-virtual-care-and-mental-health-tools. Accessed 1 Jul 2021
- 7.Smith AC, Thomas E, Snoswell CL, Haydon H, Mehrotra A, Clemensen J, Caffery LJ. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19) J Telemed Telecare. 2020;26:309–313. doi: 10.1177/1357633X20916567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Calton B, Abedini N, Fratkin M. Telemedicine in the time of coronavirus. J Pain Symptom Manag. 2020;60:e12–e14. doi: 10.1016/j.jpainsymman.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vidal-Alaball J, Acosta-Roja R, Pastor Hernández N, Sanchez Luque U, Morrison D, Narejos Pérez S, Perez-Llano J, Salvador Vèrges A, López Seguí F. Telemedicine in the face of the COVID-19 pandemic. Aten Primaria. 2020;52:418–422. doi: 10.1016/j.aprim.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wong B (2020) Medical workers wear pics of themselves smiling to comfort COVID-19 patients. In: Huffington Post. https://www.huffpost.com/entry/medical-workers-pics-smiling-covid-19-patients_l_5e8f725bc5b6b371812da523
- 11.Abelson R (2020) Doctors and patients turn to telemedicine in the coronavirus outbreak. The New York Times
- 12.(2020) COVID-19 significantly impacts health services for noncommunicable diseases. In: World Health Organization. https://www.who.int/news/item/01-06-2020-covid-19-significantly-impacts-health-services-for-noncommunicable-diseases. Accessed 24 Oct 2022
- 13.CIHI (2015) PROMs background document. Canadian Institute for Health Information. https://www.cihi.ca/sites/default/files/proms_background_may21_en-web_0.pdf. Accessed 17 Sept 2023
- 14.Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, Welch V. Cochrane handbook for systematic reviews of interventions. 2. Chichester: Wiley; 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, Gagnon M-P, Griffiths F, Nicolau B, O’Cathain A, Rousseau M-C, Vedel I (2018) Mixed methods appraisal tool (MMAT) version 2018 user guide [DOI] [PubMed]
- 17.Mojdehbakhsh RP, Rose S, Peterson M, Rice L, Spencer R. A quality improvement pathway to rapidly increase telemedicine services in a gynecologic oncology clinic during the COVID-19 pandemic with patient satisfaction scores and environmental impact. Gynecol Oncol Rep. 2021;36:100708. doi: 10.1016/j.gore.2021.100708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reid S, Bhatt M, Zemek R, Tse S. Virtual care in the pediatric emergency department: a new way of doing business? CJEM. 2021;23:80–84. doi: 10.1007/s43678-020-00048-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Peahl AF, Powell A, Berlin H, Smith RD, Krans E, Waljee J, Dalton VK, Heisler M, Moniz MH. Patient and provider perspectives of a new prenatal care model introduced in response to the coronavirus disease 2019 pandemic. Am J Obstet Gynecol. 2021;224:384.e1–384.e11. doi: 10.1016/j.ajog.2020.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kludacz-Alessandri M, Hawrysz L, Korneta P, Gierszewska G, Pomaranik W, Walczak R. The impact of medical teleconsultations on general practitioner-patient communication during COVID-19: a case study from Poland. PLoS ONE. 2021;16:e0254960. doi: 10.1371/journal.pone.0254960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Quinn LM, Olajide O, Green M, Sayed H, Ansar H. Patient and professional experiences with virtual antenatal clinics during the COVID-19 pandemic in a UK tertiary obstetric hospital: questionnaire study. J Med Internet Res. 2021;23:e25549. doi: 10.2196/25549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boydell N, Reynolds-Wright JJ, Cameron ST, Harden J. Women’s experiences of a telemedicine abortion service (up to 12 weeks) implemented during the coronavirus (COVID-19) pandemic: a qualitative evaluation. BJOG. 2021;128:1752–1761. doi: 10.1111/1471-0528.16813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ruelos VCB, Puzzitiello RN, Menendez ME, Moverman MA, Pagani NR, Rogerson A, Ryan SP, Salzler MJ. Patient perceptions of telehealth orthopedic services in the era of COVID-19 and beyond. Orthopedics. 2021;44:e668–e674. doi: 10.3928/01477447-20210817-07. [DOI] [PubMed] [Google Scholar]
- 24.Dratch L, Paul RA, Baldwin A, Brzozowski M, Gonzalez-Alegre P, Tropea TF, Raper A, Bardakjian T. Transitioning to telegenetics in the COVID-19 era: patient satisfaction with remote genetic counseling in adult neurology. J Genet Couns. 2021;30:974–983. doi: 10.1002/jgc4.1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Darr A, Senior A, Argyriou K, Limbrick J, Nie H, Kantczak A, Stephenson K, Parmar A, Grainger J. The impact of the coronavirus (COVID-19) pandemic on elective paediatric otolaryngology outpatient services—an analysis of virtual outpatient clinics in a tertiary referral centre using the modified paediatric otolaryngology telemedicine satisfaction survey (POTSS) Int J Pediatr Otorhinolaryngol. 2020;138:110383. doi: 10.1016/j.ijporl.2020.110383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Imlach F, McKinlay E, Middleton L, Kennedy J, Pledger M, Russell L, Churchward M, Cumming J, McBride-Henry K. Telehealth consultations in general practice during a pandemic lockdown: survey and interviews on patient experiences and preferences. BMC Fam Pract. 2020;21:269. doi: 10.1186/s12875-020-01336-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Birkhoff SD, McCulloh Nair J, Bald K, Frankum T, Sanchez SR, Salvatore AL. Facilitators and challenges in the adoption of a virtual nurse visit in the home health setting. Home Health Care Serv Q. 2021;40:105–120. doi: 10.1080/01621424.2021.1906374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Edge R, Meyers J, Tiernan G, Li Z, Schiavuzzi A, Chan P, Vassallo A, Morrow A, Mazariego C, Wakefield CE, Canfell K, Taylor N. Cancer care disruption and reorganisation during the COVID-19 pandemic in Australia: a patient, carer and healthcare worker perspective. PLoS ONE. 2021;16:e0257420. doi: 10.1371/journal.pone.0257420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Raheja A, Manjunath N, Garg K, Tandon V, Gupta V, Mishra S, Ather S, Suri A, Chandra PS, Singh M, Shariff A, Kale SS. Turning a new chapter in neurosurgery outpatient services: telemedicine a “savior” in this pandemic. Neurol India. 2021;69:344–351. doi: 10.4103/0028-3886.314523. [DOI] [PubMed] [Google Scholar]
- 30.Bartoletta JJ, Hinchcliff KM, Rhee PC. Comparison of patient perception and satisfaction of face-to-face versus telemedicine encounters in hand surgery. Hand (NY) 2021 doi: 10.1177/15589447211044786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Horgan TJ, Alsabbagh AY, McGoldrick DM, Bhatia SK, Messahel A. Oral and maxillofacial surgery patient satisfaction with telephone consultations during the COVID-19 pandemic. Br J Oral Maxillofac Surg. 2021;59:335–340. doi: 10.1016/j.bjoms.2020.08.099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nair PP, Aghoram R, Thomas B, Bharadwaj B, Chinnakali P. Video teleconsultation services for persons with epilepsy during COVID-19 pandemic: an exploratory study from public tertiary care hospital in Southern India on feasibility, satisfaction, and effectiveness. Epilepsy Behav. 2021;117:107863. doi: 10.1016/j.yebeh.2021.107863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Adamou M, Jones SL, Fullen T, Galab N, Abbott K, Yasmeen S. Remote assessment in adults with Autism or ADHD: a service user satisfaction survey. PLoS ONE. 2021;16:e0249237. doi: 10.1371/journal.pone.0249237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kennedy NR, Steinberg A, Arnold RM, Doshi AA, White DB, DeLair W, Nigra K, Elmer J. Perspectives on telephone and video communication in the intensive care unit during COVID-19. Ann Am Thorac Soc. 2021;18:838–847. doi: 10.1513/AnnalsATS.202006-729OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Triantafillou V, Layfield E, Prasad A, Deng J, Shanti RM, Newman JG, Rajasekaran K. Patient perceptions of head and neck ambulatory telemedicine visits: a qualitative study. Otolaryngol Head Neck Surg. 2021;164:923–931. doi: 10.1177/0194599820943523. [DOI] [PubMed] [Google Scholar]
- 36.McLachlan A, Aldridge C, Morgan M, Lund M, Gabriel R, Malez V. An NP-led pilot telehealth programme to facilitate guideline-directed medical therapy for heart failure with reduced ejection fraction during the COVID-19 pandemic. N Z Med J. 2021;134:77–88. [PubMed] [Google Scholar]
- 37.Jiang CY, Strohbehn GW, Dedinsky RM, Raupp SM, Pannecouk BM, Yentz SE, Ramnath N. Teleoncology for veterans: high patient satisfaction coupled with positive financial and environmental impacts. JCO Oncol Pract. 2021;17:e1362–e1374. doi: 10.1200/OP.21.00317. [DOI] [PubMed] [Google Scholar]
- 38.Watson L, Qi S, Delure A, Link C, Photitai E, Chmielewski L, Hildebrand A, Ruether D, Rawson K. Virtual cancer care during the COVID-19 pandemic in Alberta: evidence from a mixed methods evaluation and key learnings. JCO Oncol Pract. 2021;17:e1354–e1361. doi: 10.1200/OP.21.00144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Waqar-Cowles LN, Chuo J, Weiss PF, Gmuca S, LaNoue M, Burnham JM. Evaluation of pediatric rheumatology telehealth satisfaction during the COVID-19 pandemic. Pediatr Rheumatol. 2021;19:170. doi: 10.1186/s12969-021-00649-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sarre G, Hyer S, Chauhan-Whittingham P, Johnson A. Patients’ experience of antenatal diabetic care during the current COVID-19 pandemic: an exploratory study. Pract Diabetes. 2021;38:23–30. doi: 10.1002/pdi.2367. [DOI] [Google Scholar]
- 41.Adams L, Lester S, Hoon E, van der Haak H, Proudman C, Hall C, Whittle S, Proudman S, Hill CL. Patient satisfaction and acceptability with telehealth at specialist medical outpatient clinics during the COVID-19 pandemic in Australia. Intern Med J. 2021;51:1028–1037. doi: 10.1111/imj.15205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stirling Cameron E, Ramos H, Aston M, Kuri M, Jackson L. “COVID affected us all:” the birth and postnatal health experiences of resettled Syrian refugee women during COVID-19 in Canada. Reprod Health. 2021;18:256. doi: 10.1186/s12978-021-01309-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Brown-Johnson CG, Spargo T, Kling SMR, Saliba-Gustafsson EA, Lestoquoy AS, Garvert DW, Vilendrer S, Winget M, Asch SM, Maggio P, Nazerali RS. Patient and surgeon experiences with video visits in plastic surgery-toward a data-informed scheduling triage tool. Surgery. 2021;170:587–595. doi: 10.1016/j.surg.2021.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zimmerman BS, Seidman D, Berger N, Cascetta KP, Nezolosky M, Trlica K, Ryncarz A, Keeton C, Moshier E, Tiersten A. Patient perception of telehealth services for breast and gynecologic oncology care during the COVID-19 pandemic: a single center survey-based study. J Breast Cancer. 2020;23:542–552. doi: 10.4048/jbc.2020.23.e56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fung A, Irvine M, Ayub A, Ziabakhsh S, Amed S, Hursh BE. Evaluation of telephone and virtual visits for routine pediatric diabetes care during the COVID-19 pandemic. J Clin Transl Endocrinol. 2020;22:100238. doi: 10.1016/j.jcte.2020.100238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Efthymiadis A, Hart EJ, Guy AM, Harry R, Mahesan T, Chedid WA, Uribe-Lewis S, Perry MJ. Are telephone consultations the future of the NHS? The outcomes and experiences of an NHS urological service in moving to telemedicine. Future Healthc J. 2021;8:e15–e20. doi: 10.7861/fhj.2020-0076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gibbs V, Cai RY, Aldridge F, Wong M. Autism assessment via telehealth during the Covid 19 pandemic: experiences and perspectives of autistic adults, parents/carers and clinicians. Res Autism Spectr Disord. 2021;88:101859. doi: 10.1016/j.rasd.2021.101859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Christiansen MG, Pappot H, Pedersen C, Jarden M, Mirza MR, Piil K. Patient perspectives and experiences of the rapid implementation of digital consultations during COVID-19—a qualitative study among women with gynecological cancer. Support Care Cancer. 2022;30:2545–2554. doi: 10.1007/s00520-021-06651-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Banks J, Corrigan D, Grogan R, El-Naggar H, White M, Doran E, Synnott C, Fitzsimons M, Delanty N, Doherty CP. LoVE in a time of CoVID: clinician and patient experience using telemedicine for chronic epilepsy management. Epilepsy Behav. 2021;115:107675. doi: 10.1016/j.yebeh.2020.107675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Santoro SL, Donelan K, Haugen K, Oreskovic NM, Torres A, Skotko BG. Transition to virtual clinic: experience in a multidisciplinary clinic for down syndrome. Am J Med Genet C Semin Med Genet. 2021;187:70–82. doi: 10.1002/ajmg.c.31876. [DOI] [PubMed] [Google Scholar]
- 51.Alshareef M, Alsaleh S, Albaharna H, Alghulikah A, Aloulah M, Alroqi A, Alromaih S, Alanazy FH, Al-Dousary S. Utilization of telemedicine in rhinologic practice during COVID-19 pandemic. Am J Otolaryngol. 2021;42:102929. doi: 10.1016/j.amjoto.2021.102929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Park H-Y, Kwon Y-M, Jun H-R, Jung S-E, Kwon S-Y. Satisfaction survey of patients and medical staff for telephone-based telemedicine during hospital closing due to COVID-19 transmission. Telemed e-Health. 2021;27:724–732. doi: 10.1089/tmj.2020.0369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.López L, Green AR, Tan-McGrory A, King R, Betancourt JR. Bridging the digital divide in health care: the role of health information technology in addressing racial and ethnic disparities. Joint Comm J Qual Patient Saf. 2011;37:437–445. doi: 10.1016/s1553-7250(11)37055-9. [DOI] [PubMed] [Google Scholar]
- 54.Meno M, Abe J, Fukui J, Braun-Inglis C, Pagano I, Acoba J. Telehealth amid the COVID-19 pandemic: perception among Asian, Native Hawaiian and Pacific Islander cancer patients. Future Oncol. 2021;17:3077–3085. doi: 10.2217/fon-2021-0136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kerestes C, Delafield R, Elia J, Chong E, Kaneshiro B, Soon R. “It was close enough, but it wasn’t close enough”: a qualitative exploration of the impact of direct-to-patient telemedicine abortion on access to abortion care. Contraception. 2021;104:67–72. doi: 10.1016/j.contraception.2021.04.028. [DOI] [PubMed] [Google Scholar]
- 56.Gupta VS, Popp EC, Garcia EI, Qashqai S, Ankrom C, Wu T-C, Harting MT. Telemedicine as a component of forward triage in a pandemic. Healthc (Amst) 2021;9:100567. doi: 10.1016/j.hjdsi.2021.100567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Javanparast S, Roeger L, Kwok Y, Reed RL. The experience of Australian general practice patients at high risk of poor health outcomes with telehealth during the COVID-19 pandemic: a qualitative study. BMC Fam Pract. 2021;22:69. doi: 10.1186/s12875-021-01408-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Al-Sharif GA, Almulla AA, AlMerashi E, Alqutami R, Almoosa M, Hegazi MZ, Otaki F, Ho SB. Telehealth to the rescue during COVID-19: a convergent mixed methods study investigating patients’ perception. Front Public Health. 2021;9:730647. doi: 10.3389/fpubh.2021.730647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Juarez-Reyes M, Mui HZ, Kling SMR, Brown-Johnson C. Accessing behavioral health care during COVID: rapid transition from in-person to teleconferencing medical group visits. Ther Adv Chronic Dis. 2021;12:2040622321990269. doi: 10.1177/2040622321990269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Massaroni V, Delle Donne V, Ciccarelli N, Ciccullo A, Borghetti A, Faliero D, Visconti E, Tamburrini E, Di Giambenedetto S. Use of telehealth for HIV care in Italy: Are doctors and patients on the same page? A cross-sectional study. Int J Med Inform. 2021;156:104616. doi: 10.1016/j.ijmedinf.2021.104616. [DOI] [PubMed] [Google Scholar]
- 61.Assenza C, Catania H, Antenore C, Gobbetti T, Gentili P, Paolucci S, Morelli D. Continuity of care during COVID-19 lockdown: a survey on stakeholders’ experience with telerehabilitation. Front Neurol. 2020;11:617276. doi: 10.3389/fneur.2020.617276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wyler H, Liebrenz M, Ajdacic-Gross V, Seifritz E, Young S, Burger P, Buadze A. Treatment provision for adults with ADHD during the COVID-19 pandemic: an exploratory study on patient and therapist experience with on-site sessions using face masks vs. telepsychiatric sessions. BMC Psychiatry. 2021;21:237. doi: 10.1186/s12888-021-03236-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zimmerman M, Ward M, D’Avanzato C, Tirpak JW. Telehealth treatment of patients with borderline personality disorder in a partial hospital setting during the COVID-19 pandemic: comparative safety, patient satisfaction, and effectiveness of in-person treatment. J Pers Disord. 2022;36:277–295. doi: 10.1521/pedi_2021_35_539. [DOI] [PubMed] [Google Scholar]
- 64.Pooni R, Pageler NM, Sandborg C, Lee T. Pediatric subspecialty telemedicine use from the patient and provider perspective. Pediatr Res. 2022;91:241–246. doi: 10.1038/s41390-021-01443-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Schumm MA, Pyo HQ, Ohev-Shalom R, Tseng C-H, Livhits MJ, Zanocco KA, Hiyama DT, Yeh MW. Patient experience with electronic health record-integrated postoperative telemedicine visits in an academic endocrine surgery program. Surgery. 2021;169:1139–1144. doi: 10.1016/j.surg.2020.11.019. [DOI] [PubMed] [Google Scholar]
- 66.Sharma A, Winkelman RD, Schlenk RP, Rasmussen PA, Angelov L, Benzil DL. The utility of remote video technology in continuing neurosurgical care in the COVID-19 era: reflections from the past year. World Neurosurg. 2021;156:43–52. doi: 10.1016/j.wneu.2021.08.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Shaverdian N, Gillespie EF, Cha E, Kim SY, Benvengo S, Chino F, Kang JJ, Li Y, Atkinson TM, Lee N, Washington CM, Cahlon O, Gomez DR. Impact of telemedicine on patient satisfaction and perceptions of care quality in radiation oncology. J Natl Compr Cancer Netw. 2021;19:1174–1180. doi: 10.6004/jnccn.2020.7687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wee D, Li X, Suchman K, Trindade AJ. Patient centered outcomes regarding telemedicine prior to endoscopy during the coronavirus disease 2019 pandemic. Tech Innov Gastrointest Endosc. 2021;23:285–287. doi: 10.1016/j.tige.2021.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Piro A, Magnocavallo M, Della Rocca DG, Neccia M, Manzi G, Mariani MV, Straito M, Bernardini A, Severino P, Iannucci G, Giunta G, Chimenti C, Natale A, Fedele F, Lavalle C. Management of cardiac implantable electronic device follow-up in COVID-19 pandemic: lessons learned during Italian lockdown. J Cardiovasc Electrophysiol. 2020;31:2814–2823. doi: 10.1111/jce.14755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Richards AE, Curley K, Christel L, Zhang N, Kouloumberis P, Kalani MA, Lyons MK, Neal MT. Patient satisfaction with telehealth in neurosurgery outpatient clinic during COVID-19 pandemic. Interdiscip Neurosurg. 2021;23:101017. doi: 10.1016/j.inat.2020.101017. [DOI] [Google Scholar]
- 71.Porche K, Vaziri S, Mehkri Y, Christie C, Laurent D, Wang Y, Rahman M. Patient satisfaction scores with telemedicine in the neurosurgical population. Clin Neurol Neurosurg. 2021;205:106605. doi: 10.1016/j.clineuro.2021.106605. [DOI] [PubMed] [Google Scholar]
- 72.Chen DA, Tran AQ, Dinkin MJ, Lelli GJ. Ophthalmic virtual visit utilization and patient satisfaction during the COVID-19 pandemic. Telemed J E Health. 2022;28:798–805. doi: 10.1089/tmj.2021.0392. [DOI] [PubMed] [Google Scholar]
- 73.Finn MTM, Brown HR, Friedman ER, Kelly AG, Hansen K. Preference for telehealth sustained over three months at an outpatient center for integrative medicine. Glob Adv Health Med. 2021;10:2164956121997361. doi: 10.1177/2164956121997361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Galaviz KI, Shah NS, Gutierrez M, Collins LF, Lahiri CD, Moran CA, Szabo B, Sumitani J, Rhodes J, Marconi VC, Nguyen ML, Cantos VD, Armstrong WS, Colasanti JA. Patient experiences with telemedicine for HIV care during the first COVID-19 wave in Atlanta, Georgia. AIDS Res Hum Retroviruses. 2022;38:415–420. doi: 10.1089/aid.2021.0109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wright E, Shaltout O, Zokvic MA, Shirreff L. Delivery of menopause care during a pandemic: an evaluation of patient satisfaction with telephone visits. Menopause. 2021;29:184–188. doi: 10.1097/GME.0000000000001906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Pinar U, Anract J, Perrot O, Tabourin T, Chartier-Kastler E, Parra J, Vaessen C, de La Taille A, Roupret M. Preliminary assessment of patient and physician satisfaction with the use of teleconsultation in urology during the COVID-19 pandemic. World J Urol. 2021;39:1991–1996. doi: 10.1007/s00345-020-03432-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Pareyson D, Pantaleoni C, Eleopra R, De Filippis G, Moroni I, Freri E, Zibordi F, Bulgheroni S, Pagliano E, Sarti D, Silvani A, Grazzi L, Tiraboschi P, Didato G, Anghileri E, Bersano A, Valentini L, Piacentini S, Muscio C, Leonardi M, Mariotti C, Eoli M, Nuzzo S, Tagliavini F, Confalonieri P, De Giorgi F, Force B-T. Neuro-telehealth for fragile patients in a tertiary referral neurological institute during the COVID-19 pandemic in Milan, Lombardy. Neurol Sci. 2021;42:2637–2644. doi: 10.1007/s10072-021-05252-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Rush KL, Seaton C, Li E, Oelke ND, Pesut B. Rural use of health service and telemedicine during COVID-19: the role of access and eHealth literacy. Health Inform J. 2021;27:14604582211020064. doi: 10.1177/14604582211020064. [DOI] [PubMed] [Google Scholar]
- 79.Murthy V, Herbert C, Bains D, Escudier M, Carey B, Ormond M. Patient experience of virtual consultations in oral medicine during the COVID-19 pandemic. Oral Dis. 2022;28(Suppl 2):2400–2405. doi: 10.1111/odi.14006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Makoul G, Krupat E, Chang C-H. Measuring patient views of physician communication skills: development and testing of the Communication Assessment Tool. Patient Educ Couns. 2007;67:333–342. doi: 10.1016/j.pec.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 81.Constanzo F, Aracena-Sherck P, Hidalgo JP, Muñoz M, Vergara G, Alvarado C. Validation of a patient satisfaction survey of the teleneurology program in Chile. BMC Res Notes. 2019;12:359. doi: 10.1186/s13104-019-4358-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Dyer N, Sorra JS, Smith SA, Cleary PD, Hays RD. Psychometric properties of the Consumer Assessment of Healthcare Providers and Systems (CAHPS®) clinician and group adult visit survey. Med Care. 2012;50:S28. doi: 10.1097/MLR.0b013e31826cbc0d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.(2022) General Medical Council. https://www.gmc-uk.org/. Accessed 20 Dec 2022
- 84.Maurice-Szamburski A, Michel P, Loundou A, Auquier P, For the G-MISS Study Investigators Validation of the generic medical interview satisfaction scale: the G-MISS questionnaire. Health Qual Life Outcomes. 2017;15:36. doi: 10.1186/s12955-017-0608-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Harewood GC, Yacavone RF, Locke GR, Wiersema MJ. Prospective comparison of endoscopy patient satisfaction surveys: e-mail versus standard mail versus telephone. Am J Gastroenterol. 2001;96:3312–3317. doi: 10.1111/j.1572-0241.2001.05331.x. [DOI] [PubMed] [Google Scholar]
- 86.Bridge E, Singh S, Murdoch A, Mozuraitis M, Nicholls B, Moody L. Examining patient and visit characteristics associated with the cancer patient experience. JCO. 2019;37:204–204. doi: 10.1200/JCO.2019.37.27_suppl.204. [DOI] [Google Scholar]
- 87.Sasangohar F, Dhala A, Zheng F, Ahmadi N, Kash B, Masud F. Use of telecritical care for family visitation to ICU during the COVID-19 pandemic: an interview study and sentiment analysis. BMJ Qual Saf. 2021;30:715–721. doi: 10.1136/bmjqs-2020-011604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Parkinson A, Drew J, Hall Dykgraaf S, Fanning V, Chisholm K, Elisha M, Lueck C, Phillips C, Desborough J. “They’re getting a taste of our world”: a qualitative study of people with multiple sclerosis’ experiences of accessing health care during the COVID-19 pandemic in the Australian Capital Territory. Health Expect. 2021;24:1607–1617. doi: 10.1111/hex.13284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lowe J, Liang H, Riggs C, Henson J, Elder T. Community partnership to affect substance abuse among native American adolescents. Am J Drug Alcohol Abuse. 2012;38:450–455. doi: 10.3109/00952990.2012.694534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Craig M, Chopra A, Lasry O, Dea N, Charest-Morin R, Street J, Paquette S, Dvorak M, Kwon BK, Fisher C, Ailon T. Telehealth for outpatient spine consultation: What do the patients think? Interdiscip Neurosurg. 2022;28:101462. doi: 10.1016/j.inat.2021.101462. [DOI] [Google Scholar]
- 91.Knaus ME, Ahmad H, Metzger GA, Beyene TJ, Thomas JL, Weaver LJ, Gasior AC, Wood RJ, Halaweish I. Outcomes of a telemedicine bowel management program during COVID-19. J Pediatr Surg. 2022;57:80–85. doi: 10.1016/j.jpedsurg.2021.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Raykos BC, Erceg-Hurn DM, Hill J, Campbell BNC, McEvoy PM. Positive outcomes from integrating telehealth into routine clinical practice for eating disorders during COVID-19. Int J Eat Disord. 2021;54:1689–1695. doi: 10.1002/eat.23574. [DOI] [PubMed] [Google Scholar]
- 93.Lotan M, Downs J, Elefant C. A pilot study delivering physiotherapy support for rett syndrome using a telehealth framework suitable for COVID-19 lockdown. Dev Neurorehabil. 2021;24:429–434. doi: 10.1080/17518423.2021.1914762. [DOI] [PubMed] [Google Scholar]
- 94.Ganderton CL, Tirosh O, Munro D, Meyer D, Lenssen R, Balster S, Watson L, Warby S. Rehabilitation for atraumatic shoulder instability in circus arts performers: delivery via telehealth. J Shoulder Elbow Surg. 2022;31:e246–e257. doi: 10.1016/j.jse.2021.10.033. [DOI] [PubMed] [Google Scholar]
- 95.Alsobayel H, Alodaibi F, Albarrati A, Alsalamah N, Alhawas F, Alhowimel A. Does telerehabilitation help in reducing disability among people with musculoskeletal conditions? A preliminary study. Int J Environ Res Public Health. 2021;19:72. doi: 10.3390/ijerph19010072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lai FH-Y, Yan EW-H, Yu KK-Y, Tsui W-S, Chan DT-H, Yee BK. The protective impact of telemedicine on persons with dementia and their caregivers during the COVID-19 pandemic. Am J Geriatr Psychiatry. 2020;28:1175–1184. doi: 10.1016/j.jagp.2020.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Daswani K, Bhatia K. Physiotherapy in telerehabilitation mode improves health related quality of life and functional muscle strength in COVID 19 survivors: a case series. Indian J Physiother Occup Ther. 2021;15:36–46. doi: 10.37506/ijpot.v15i1.13345. [DOI] [Google Scholar]
- 98.James Riegler L, Raj SP, Moscato EL, Narad ME, Kincaid A, Wade SL. Pilot trial of a telepsychotherapy parenting skills intervention for veteran families: implications for managing parenting stress during COVID-19. J Psychother Integr. 2020;30:290–303. doi: 10.1037/int0000220. [DOI] [Google Scholar]
- 99.Graziano S, Boldrini F, Righelli D, Milo F, Lucidi V, Quittner A, Tabarini P. Psychological interventions during COVID pandemic: telehealth for individuals with cystic fibrosis and caregivers. Pediatr Pulmonol. 2021;56:1976–1984. doi: 10.1002/ppul.25413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.van Agteren J, Ali K, Fassnacht DB, Iasiello M, Furber G, Howard A, Woodyatt L, Musker M, Kyrios M. Testing the differential impact of an internet-based mental health intervention on outcomes of well-being and psychological distress during COVID-19: uncontrolled intervention study. JMIR Ment Health. 2021;8:e28044. doi: 10.2196/28044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Bernocchi P, Bonometti F, Serlini M, Assoni G, Zanardini M, Pasotti E, Guerrini S, Scalvini S. Telehealth and telecare: a real-life integrated experience in the covid-19 pandemic. Telemed J E Health. 2022;28:720–727. doi: 10.1089/tmj.2021.0181. [DOI] [PubMed] [Google Scholar]
- 102.Sabbagh R, Shah N, Jenkins S, Macdonald J, Foote A, Matar R, Steffensmeier A, Grawe B. The COVID-19 pandemic and follow-up for shoulder surgery: the impact of a shift toward telemedicine on validated patient-reported outcomes. J Telemed Telecare. 2021 doi: 10.1177/1357633X21990997. [DOI] [PubMed] [Google Scholar]
- 103.Levinson CA, Spoor SP, Keshishian AC, Pruitt A. Pilot outcomes from a multidisciplinary telehealth versus in-person intensive outpatient program for eating disorders during versus before the Covid-19 pandemic. Int J Eat Disord. 2021;54:1672–1679. doi: 10.1002/eat.23579. [DOI] [PubMed] [Google Scholar]
- 104.Steiger H, Booij L, Crescenzi O, Oliverio S, Singer I, Thaler L, St-Hilaire A, Israel M. In-person versus virtual therapy in outpatient eating-disorder treatment: a COVID-19 inspired study. Int J Eat Disord. 2022;55:145–150. doi: 10.1002/eat.23655. [DOI] [PubMed] [Google Scholar]
- 105.Thesenvitz J, Corley S, Solberg L, Carvalho C. Home health monitoring during the COVID pandemic: results from a feasibility study in Alberta primary care. Healthc Manag Forum. 2022;35:29–34. doi: 10.1177/08404704211041969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Wu F, Rotimi O, Laza-Cagigas R, Rampal T. The feasibility and effects of a telehealth-delivered home-based prehabilitation program for cancer patients during the pandemic. Curr Oncol. 2021;28:2248–2259. doi: 10.3390/curroncol28030207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Corona LL, Stainbrook JA, Simcoe K, Wagner L, Fowler B, Weitlauf AS, Juárez AP, Warren Z. Utilization of telemedicine to support caregivers of young children with ASD and their part C service providers: a comparison of intervention outcomes across three models of service delivery. J Neurodev Disord. 2021;13:38. doi: 10.1186/s11689-021-09387-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Bulkes NZ, Davis K, Kay B, Riemann BC. Comparing efficacy of telehealth to in-person mental health care in intensive-treatment-seeking adults. J Psychiatr Res. 2022;145:347–352. doi: 10.1016/j.jpsychires.2021.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Rezich BMZ, Malone JA, Reiser G, Zimmerman HH, Blase TL, Fishler KP. Telehealth genetic services during the COVID-19 pandemic: implementation and patient experiences across multiple specialties in Nebraska. J Genet Couns. 2021;30:1233–1243. doi: 10.1002/jgc4.1507. [DOI] [PubMed] [Google Scholar]
- 110.Nascimento BR, Brant LC, Castro ACT, Froes LEV, Ribeiro ALP, Cruz LV, Araújo CB, Souza CF, Froes ET, Souza SD. Impact of a large-scale telemedicine network on emergency visits and hospital admissions during the coronavirus disease 2019 pandemic in Brazil: data from the UNIMED-BH system. J Telemed Telecare. 2020 doi: 10.1177/1357633X20969529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Kesavadev J, Basanth A, Krishnan G, Vitale R, Parameswaran H, Shijin S, Sreelakshmi R, Raj S, Ashik A, Shankar A, Badarudeen S, Raveendran AV, Rajalakshmy I, Sanal G, Manoj A, Jose R, Unes Y, Jothydev S. A new interventional home care model for COVID management: virtual Covid IP. Diabetes Metab Syndr. 2021;15:102228. doi: 10.1016/j.dsx.2021.102228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Mahmoud MA, Daboos M, Gouda S, Othman A, Abdelmaboud M, Hussein ME, Akl M. Telemedicine (virtual clinic) effectively delivers the required healthcare service for pediatric ambulatory surgical patients during the current era of COVID-19 pandemic: a mixed descriptive study. J Pediatr Surg. 2022;57:630–636. doi: 10.1016/j.jpedsurg.2021.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Reforma LG, Duffy C, Collier AY, Wylie BJ, Shainker SA, Golen TH, Herlihy M, Lydeard A, Zera CA. A multidisciplinary telemedicine model for management of coronavirus disease 2019 (COVID-19) in obstetrical patients. Am J Obstet Gynecol MFM. 2020;2:100180. doi: 10.1016/j.ajogmf.2020.100180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Puwanant S, Sinphurmsukskul S, Krailak L, Nakaviroj P, Boonbumrong N, Siwamogsatham S, Chettakulanurak K, Ariyachaipanich A, Boonyaratavej S. The impact of the coronavirus disease and Tele-Heart Failure Clinic on cardiovascular mortality and heart failure hospitalization in ambulatory patients with heart failure. PLoS ONE. 2021;16:e0249043. doi: 10.1371/journal.pone.0249043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Agarwal P, Mukerji G, Laur C, Chandra S, Pimlott N, Heisey R, Stovel R, Goulbourne E, Bhatia RS, Bhattacharyya O, Martin D. Adoption, feasibility and safety of a family medicine-led remote monitoring program for patients with COVID-19: a descriptive study. CMAJ Open. 2021;9:E324–E330. doi: 10.9778/cmajo.20200174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Joshi C, Jacobson M, Silveira L, Shea S, Yang M, Eschbach K. Risk of admission to the emergency room/inpatient service after a neurology telemedicine visit during COVID-19 pandemic. Pediatr Neurol. 2021;122:15–19. doi: 10.1016/j.pediatrneurol.2021.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Paskudzka D, Kołodzińska A, Cacko A, Stolarz P, Łyżwiński Ł, Opolski G, Grabowski M. Telephone follow-up of patients with cardiovascular implantable electronic devices during the coronavirus disease 2019 pandemic: early results. Kardiol Pol. 2020;78:725–731. doi: 10.33963/KP.15392. [DOI] [PubMed] [Google Scholar]
- 118.Swift J, Harris Z, Woodward A, O’Kelly N, Barker C, Ghosh S. An evaluation of a virtual COVID-19 ward to accelerate the supported discharge of patients from an acute hospital setting. Br J Healthc Manag. 2022;28:7–15. doi: 10.12968/bjhc.2021.0073. [DOI] [Google Scholar]
- 119.Mistry SK, Shaw M, Raffan F, Johnson G, Perren K, Shoko S, Harris-Roxas B, Haigh F. Inequity in access and delivery of virtual care interventions: a scoping review. Int J Environ Res Public Health. 2022;19:9411. doi: 10.3390/ijerph19159411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Darrat I, Tam S, Boulis M, Williams AM. Socioeconomic disparities in patient use of telehealth during the coronavirus disease 2019 surge. JAMA Otolaryngol Head Neck Surg. 2021;147:287–295. doi: 10.1001/jamaoto.2020.5161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Clare CA. Telehealth and the digital divide as a social determinant of health during the COVID-19 pandemic. Netw Model Anal Health Inform Bioinform. 2021;10:26. doi: 10.1007/s13721-021-00300-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Sevean P, Dampier S, Spadoni M, Strickland S, Pilatzke S. Patients and families experiences with video telehealth in rural/remote communities in Northern Canada. J Clin Nurs. 2009;18:2573–2579. doi: 10.1111/j.1365-2702.2008.02427.x. [DOI] [PubMed] [Google Scholar]
- 123.O’Kane G. Telehealth—improving access for rural, regional and remote communities. Aust J Rural Health. 2020;28:419–420. doi: 10.1111/ajr.12663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Buyting R, Melville S, Chatur H, White CW, Légaré J-F, Lutchmedial S, Brunt KR. Virtual care with digital technologies for rural Canadians living with cardiovascular disease. CJC Open. 2022;4:133–147. doi: 10.1016/j.cjco.2021.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Bech M. The economics of non-attendance and the expected effect of charging a fine on non-attendees. Health Policy. 2005;74:181–191. doi: 10.1016/j.healthpol.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 126.Kichloo A, Albosta M, Dettloff K, Wani F, El-Amir Z, Singh J, Aljadah M, Chakinala RC, Kanugula AK, Solanki S, Chugh S. Telemedicine, the current COVID-19 pandemic and the future: a narrative review and perspectives moving forward in the USA. Fam Med Community Health. 2020;8:e000530. doi: 10.1136/fmch-2020-000530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Kobeissi MM, Ruppert SD. Remote patient triage: shifting toward safer telehealth practice. J Am Assoc Nurse Pract. 2021;34:444–451. doi: 10.1097/JXX.0000000000000655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Bashshur RL, Doarn CR, Frenk JM, Kvedar JC, Shannon GW, Woolliscroft JO. Beyond the COVID pandemic, telemedicine, and health care. Telemed J E Health. 2020;26:1310–1313. doi: 10.1089/tmj.2020.0328. [DOI] [PubMed] [Google Scholar]
- 129.Lloyd H, Wheat H, Horrell J, Sugavanam T, Fosh B, Valderas JM, Close J. Patient-reported measures for person-centered coordinated care: a comparative domain map and web-based compendium for supporting policy development and implementation. J Med Internet Res. 2018;20:e54. doi: 10.2196/jmir.7789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Anufriyeva V, Pavlova M, Stepurko T, Groot W. The validity and reliability of self-reported satisfaction with healthcare as a measure of quality: a systematic literature review. Int J Qual Health Care. 2021;33:mzaa152. doi: 10.1093/intqhc/mzaa152. [DOI] [PubMed] [Google Scholar]
- 131.Bull C. Patient satisfaction and patient experience are not interchangeable concepts. Int J Qual Health Care. 2021;33:mzab023. doi: 10.1093/intqhc/mzab023. [DOI] [PubMed] [Google Scholar]
- 132.Kemp KA, Fairie P, Steele BJ, Santana MJ. Adult experiences with hospitalization in Alberta, Canada during the COVID-19 pandemic: a comparative cross-sectional study. J Patient Exp. 2022;9:23743735221077520. doi: 10.1177/23743735221077518. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 2. Quality Assessment of Included Studies.
Data Availability Statement
Data available upon request to the authors.