Abstract
Diabetic foot ulcer (DFU) is a serious complication of diabetes mellitus and a cause of significant morbidity, mortality and healthcare expenditure. Treatment of DFU includes multimodal approach like surgical debridement, infection control, vascular assessment, dressing etc. Multidisciplinary approach towards foot care is becoming a mainstay of therapy, and even with this comprehensive approach, there is still room for improvement in DFU outcomes. Integrative management includes the adoption of various systems of treatment with standard treatment for better outcomes. In the present case series, six cases of DFU were managed with the integration of Ayurveda and allopathic treatments. The cases were managed according to the standard diabetic foot ulcer management principles like surgical debridement, insulin therapy, along with incorporation of Ayurveda procedures like Vimlapana, Prakshalana, Bandhana etc. Standard assessment of ulcers at different time points was done using the Bates- Jensen Ulcer assessment tool. All the six DFU healed with minimal scar formation and in less time, lowering the risk of further amputation. Promising results were obtained in all six cases by adopting integrated Ayurveda and allopathic treatments, which indicates the potential benefits of alternative systems of medicine.
Keywords: Diabetic foot ulcer (DFU), Integrative management, Bates- jensen ulcer assessment tool, Vrana Ropana, Vrana Shodhana
1. Introduction
Integrated care is a concept that can be adopted in the management and organization of services related to health promotion [1]. Integration overcomes the ambiguities of each health care discipline and allows them to shoulder one another to give the best comprehensive patient care [1]. Ayurveda is proved to be effective in the management of various chronic ailments, including ulcers. Diabetic foot ulcer is a challenging condition for treatment, because of multiple factors, and infection is one of them. Evidence from published literature showed that there were 100,000 leg amputations per year due to diabetes-related problems [2]. Out of 62 million diabetics in India, 25% develop DFU and the 10-year death rate is 40% [2]. Approximately 45%–60% of all diabetic foot ulcerations are purely neuropathic, whereas 45% have both neuropathic and ischemic components [3].
Standard treatment principles for diabetic foot ulcer comprise of necrotic tissue debridement, drainage of pus, insulin therapy, antibiotics, and amputation. Diabetic foot ulcers are well managed by a multidisciplinary and comprehensive approach, which modern medical science has explored well in treating acute conditions [4]. The principles of ulcer care are very well highlighted by Acharya Sushruta, contributing major chapters in his treatise Sushruta Samhita and explaining Shastiupakramas (60 therapeutic measures) for managing different types of ulcers [5]. These principles are commonly used in the management of DFU, with the adoption of internal and external purificatory measures. Integration of two systems according to condition, i.e. acute phase of DFU, which needs aggressive therapy for control of infection and sugar levels, which can be well achieved by contemporary (allopathic) science, and once the patient is stabilized with systemic events, can be shifted to an ayurvedic line of management for better clinical outome. Keeping this specific objective in mind and to promote the integrative practice that is the need of the hour, we are reporting six cases of diabetic foot ulcers with different clinical presentations that were effectively managed with an integrated approach.
2. Patient information and clinical findings
2.1. Case 1
A 55-year-old female, non-hypertensive and known case of diabetes mellitus for 12 years, came with complaints of blackish discoloration of the first toe with a spreading ulcer over the dorsal aspect of her left foot for 1 month. The ulcer has been accompanied by pain, a burning sensation, a foul odor, pus discharge, and reddish discoloration around the digits. Initially, the patient received conservative treatment by a local physician with antibiotics and dressing, but the condition of the patient started deteriorating as she did not respond well to oral medications. Her economic status, cost affordability, and fear drove her to seek alternative medical care, and she came to our hospital. The case was treated at KLE Ayurveda Hospital, Belagavi, Karnataka, from 04/01/2018 to 10/04/2018 (OPD NO 18000191/IPD-0056) MR No. KLE 18000207. Clinical evaluation revealed that she was having a fever (101 ° F) with chills and rigor. Past history and family history were not specific to the disease. She was anemic, moderately built and nourished. Systemic examination showed that she was well oriented to time and place, respiratory rate (22/min), tachycardia with increased pulse rate (105/min). Local examination revealed gangrenous changes in the first toe of the left foot; an oval-shaped ulcer at the dorsal aspect of the foot measuring 6 × 5 cm (Fig. 1); edematous edges; a foul odor; and a yellow-colored slough with exposed tendons on the floor. On palpation, local rise of temperature, tenderness, and pitting odema along with reddish discoloration surrounding the ulcer were present (Fig. 1). Dorsalis pedis, anterior tibial and posterior tibial artery pulsations of left foot was found feeble on palpation. The Semmes-Weinstein monofilament (SWM) test was used to assess peripheral neuropathy, which revealed diminished sensation, i.e., grade 1 [6]. The ulcer was graded as grade 5 according to the Wagner classification. The WBC count was 17,300 cells/cumm (Neutrophil-74%, Lymphocyte-18%, Eosinophil-6%), FBS was 230 mg/dl, PPBS was 351 mg/dl, HbA1c was 9.2, Hb was 10.5 gm%, blood urea was 34 gm%, and serum creatinine was 1.4 gm%. The rest of the other blood parameters were within normal limits. An X-ray of the left foot revealed no osteomyelitic changes in the metatarsals.
Fig. 1.
Changes in the healing of case 1 and 2 ulcer.
2.2. Case 2
A 45-year-old male recently diagnosed with hypertension (HTN) and diabetes mellitus (DM) came with complaints of an ulcer at the plantar aspect of his right foot for 1 month, associated with fever and swelling in the right foot up to the ankle region. The case was treated at KLE Ayurveda Hospital from 13/09/2019 to 09/11/2019 (MR–KLE 19018887). The patient's occupation was courier delivery, and he used to ride his bike for 8–10 h per day. Due to the rainy season, improper foot care resulted in the formation of an ulcer on the foot, which flared up to form cellulitis. Fever with chills and rigors worsened the condition and forced to seek medical advice. Conservative treatment was done with the prescription of antibiotics, analgesics, and dressings. He came to our hospital to seek further investigation and treatment. Clinical evaluation revealed that he was having a fever (99 ° F) with pitting odema and blackish discolouration of the right foot. Past history and family history were not specific to the disease; he was thin-built and moderately nourished. Systemic examination revealed that he was well oriented with normal respiratory (18/min) and pulse rate (96/min). Local examination revealed a spherical ulcer (3 × 3 cm) at the arch of the plantar aspect of the right foot. Blackish discoloration surrounding the ulcer with punched out edges and necrosed tissue on the floor. Dorsalis pedis, anterior tibial and posterior tibial artery pulsations of the right foot were normal (Fig. 1). A neurological examination suggested that touch sensation was reduced. The ulcer was diagnosed as grade 2 according to the Wagner classification. WBC count was 7300 cells/cumm (Neutrophil-72%), Lymphocyte-16%, Eosinophil-4%), FBS-210 mg/dl, PPBS-379 mg/dl, Hb-10.3%. Blood urea was 32 gm%, serum creatinine was 0.8 gm%, and all other blood parameters were within normal limits.
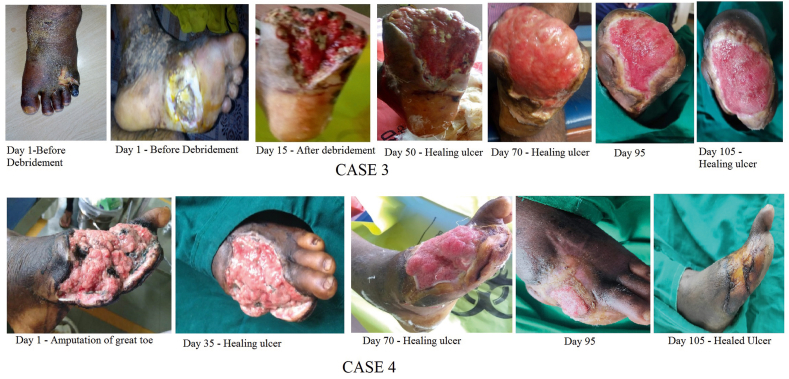
2.3. Case 3
A 54-year-old male with a known case of DM and HTN for 5 years on medication came with complaints of a foul-smelling ulcer on the dorsal and plantar aspect of his left foot for 2 months, associated with fever, chills, rigor, and swelling with blebs extending up to the ankle region. The case was treated at KLE Ayurveda Hospital from 17/08/2019 to 05/1/2020 (MR–KLE 19018339). The patient was in septicemia with uncontrolled diabetes, so he was referred for amputation at the level of the metatarsophalangeal joint of all digits with extensive debridement on both dorsal and plantar aspects at KLE centenary hospital, Yellur. The patient was treated there for 15 days with allopathic treatment, and later for ulcer management, he was referred back to our hospital. He was thin-built and moderately nourished, with no specific past history and a family history suggesting that all members of the family had DM. The cardiovascular, respiratory, and central nervous system examinations were all normal. Local examination of the left foot revealed amputated digits with “V" shaped ulcers, red granulation tissue on both sides of the foot (dorsal and ventral), and slough measuring 5 × 7 cm at the dorsal aspect and 8 × 7 cm at the plantar aspect with sloping edges (Fig. 2). Dorsalis pedis, anterior tibial and posterior tibial artery pulsations of the left foot were normal. Neurological examination suggested that touch sensation was normal. The ulcer was graded as grade 4 according to Wagner's classification. The WBC count was 11,200 cells/cumm (Neutrophil-74%, Lymphocyte-18%, Eosinophil-5%), FBS was 170 mg/dl, PPBS was 320 mg/dl, HbA1c was 9.2 and Hb was 11.6%, blood urea was 37 gm%, serum creatinine was 1.2 gm% and other blood parameters were within normal limits.
Fig. 2.
Changes in the healing of case 3 and 4 ulcer.
2.4. Case 4
A 61-year-old male with a known case of DM and HTN for 22 years came with complaints of a foul-smelling ulcer at the dorsal aspect of the left foot along with an amputed first toe and second toe at mid metatarsal level, associated with fever, chills, and rigour for 7 days. The case was treated at KLE Ayurveda Hospital from 16/07/2019 to 30/10/2019 (MR–KLE 19015804) [Table 1]. Past history suggested that he developed an ulcer over the first toe due to trauma while walking barefoot. The patient underwent debridement and toe amputation at an allopathic hospital in Ghataprabha due to suppuration in the left foot. Significant improvement in the condition was not seen in spite of the amputation, so he was advised to have a below knee amputation. He sought treatment through alternative medical systems due to his fear of losing limbs and his financial situation. He was well built and well-nourished with normal systemic examination findings. Local examination revealed that there was a foul-smelling ulcer on the dorsal and medial aspect of the left foot with abundant slough at amputed digits measuring 10 × 8 cm (Fig. 1) with edematous, irregular edges. Blackish discoloration and pitting were present surrounding the ulcer up to the ankle region (Fig. 2). Dorsalis pedis, anterior tibial, and posterior tibial artery pulsations of the left foot were found feeble. The Semmes-Weinstein monofilament (SWM) test was used to assess peripheral neuropathy, which revealed diminished sensation, i.e., grade 1. The ulcer was diagnosed as grade 4 according to the Wagner classification. The WBC count was 17,300 cells/cumm (Neutrophil-74%, Lymphocyte-18%, Eosinophil-6%), FBS was 220 mg/dl, PPBS was 310 mm/dl, HbA1c was 9.1, Hb was 10.3%, blood urea was 35 gm%, and serum creatinine was 1.5 gm%. An X-ray of the left foot revealed that no bony tissues were involved. The intervention was started with Ayurveda oral medicines and local procedures but patient developed small pus pockets at ventral aspect of the foot (near 1st and 2nd web space) so the patient was referred to KLE centenary hospital, Yellur for wound debridement. The patient was referred back to our hospital for further ulcer care after 15 days.
Table 1.
Plan of care for Diabetic foot ulcer patients.
| Case 1 | ||
|---|---|---|
| System of medicine | Plan of care | |
| Allopathy | IV Antibiotics - Injection ceftriaxone with salbactum 1.5 g intravenous twice a day for 5 days | |
| Insulin therapy - Injection Human mixtard Subcutaneous (8units morning and 10 units at night before food) | ||
| Amputation of great toe at metatarso phalangeal joint under local anaesthesia. | ||
| Ayurveda | Local Ulcer treatment procedures | Vrana Shodhana, Vrana Ropana, Vrana Bandhana, Vrana Dhupana∗ |
| Oral Medications |
|
|
| Case 2 | ||
| Allopathy | Diabetic medications – Tab Metformin 500 mg with Glimepride 1 mg twice daily with water before food | |
| Ayurveda | Local Ulcer treatment procedures | Vrana Shodhana, Vrana Ropana, Vrana Bandhana, Vrana Dhupana∗ |
| Oral Medications |
|
|
| Case 3 | ||
| Allopathy | Tab Amoxicillin with clavinic acid 675 mg two times daily with water after food. | |
| Insulin therapy - (Injection Human mixtard) Subcutaneous (20 units morning – 20 units afternoon – 12 units night) | ||
| Amputation | ||
| Ayurveda | Local Ulcer treatment procedures | Vrana Shodhana, Vrana Ropana, Vrana Bandhana, Vrana Dhupana∗ |
| Oral Medications |
|
|
| Case 4 | ||
| Allopathy | IV Antibiotics - Injection ceftriaxone with salbactum 1.5 g intravenous twice a day for 5 days | |
| Insulin therapy - (Inj Human mixtard) Subcutaneous (20 units morning and 20 units night) | ||
| Ulcer debridement | ||
| Ayurveda | Local Ulcer treatment procedures | Vrana Shodhana, Vrana Ropana, Vrana Bandhana, Vrana Dhupana∗ |
| Oral Medications |
|
|
| Case 5 | ||
| Allopathy | IV Antibiotics - Injection ceftriaxone with salbactum 1.5 g intravenous twice a day for 5 days | |
| Insulin therapy - (Inj Human mixtard) Subcutaneous (10 units morning, 10 units afternoon and 14 units night) | ||
| Ulcer debridement | ||
| Ayurveda | Oral Medications |
|
| Case 6 | ||
| Allopathy | IV Antibiotics - Injection ceftriaxone with salbactum 1.5 g intravenous twice a day for 5 days | |
| Insulin therapy - (Inj Human mixtard) Subcutaneous (10 units morning, 10 units afternoon and 14 units night) | ||
| Ulcer debridement | ||
| Ayurveda | Oral Medications |
|
| Surgical debridement/ Ulcer debridement/ Amputation | |
|---|---|
| Vrana Shodhana (ulcer cleansing) | Prakshalana with Panchavalkala Kashaya and Vimlapana with Jatyadi taila |
| Vrana Ropana (ulcer healing) | Jatyadi taila application |
| Vrana Bandhana (ulcer bandage) | Bandaging with Jatyadi Taila |
| Vrana Dhupana (ulcer fumigation) | Ulcer fumigation with Guggula, Aguru, Vacha, Sarja rasa, Sarshapa, Saindhava lavana, Nimba Patra and ghee |
2.5. Case 5
A 30-year-old female was accidently diagnosed with DM two months ago and is currently being treated on insulin therapy. The patient presented with pain, gross swelling, and gangrenous changes in the 3rd and 4th digits of the right foot associated with foul smell, pus discharge, and multiple blebs over the foot. The case was treated at KLE Ayurveda Hospital from 11/11/2020 to 15/03/2021 (MR–KLE 20015921). The clinical examination revealed tenderness over the right foot, high grade fever (102 ° F) associated with chills and tachycardia. The patient was referred to KLE centenary hospital for initial treatment as the patient was in septicemia and underwent debridement with the amputation of 3rd and 4th digits at the level of the metatarsophalangeal joint. The patient was stabilized by insulin therapy and antibiotics for 10 days. She was referred back to our hospital for ulcer management. Past history and family history were not specific. She was well built and well nourished. The cardiovascular, respiratory, and central nervous system examinations were normal. Local examination of the right foot revealed a gross ulcer (8 × 9 cm) over the dorsum of the foot with inverted V shaped, sloping edges; the floor was covered with yellow colored slough with exposed tendons along with amputated 3rd and 4th digits (Fig. 3). The Semmes-Weinstein monofilament (SWM) test was used to assess peripheral neuropathy, which revealed diminished sensation, i.e., grade 1. The ulcer was diagnosed as grade 4 according to Wagner's classification. Blood investigations during septicemia conditions showed Hb%-9.7 g/dl, WBC count – 18,900 cells/cumm (Neutrophil – 82%, Lymphocyte – 12%, Eosinophil – 05%), ESR – 170 mm at 1st hour, FBS – 176 mg/dl, PPBS – 288 mg/dl, HbA1c – 8.2, blood urea – 36 gm% and serum creatinine – 1.4 gm%. Blood tests after the second admission were within normal limits, but Hb% was 8.6 g/dl, RBS was 214 mg/dl, and HbA1c was 7.5.
Fig. 3.
Changes in the healing of case 5 and 6 ulcer.
2.6. Case 6
A 60-year old male patient with a known case of diabetes (5 years), hypertension (1.5 years), and stroke (2.5 years), presently on regular medication, came with complaints of pain, swelling over the calf, and a non-healing ulcer over the posterior aspect of the left calf region, extending to the ankle joint associated with pus discharge. The case was treated at KLE Ayurveda Hospital from 1/12/2020 to 22/02/2021 (MR – KLE 210017694). He was thin-built and moderately nourished with normal systemic examination findings. Local examination revealed that the ulcer was associated with an exposed and infected Achilles tendon. Dorsalispedis, anterior tibial and posterior tibial artery pulsation of the left foot was feeble (Fig. 3). Semmes-Weinstein monofilament (SWM) revealed a diminished sensation, i.e., grade 1. The ulcer was diagnosed as grade 4 according to the Wagner classification. The WBC count was 14,200 cells/cumm (Neutrophil-73%, Lymphocyte-17%, Eosinophil-5%), FBS was 180 mg/dl, PPBS was 280 mg/dl, HbA1c was 8.1, Hb was 11.7%, blood urea was 33 gm%, and serum creatinine was 1.4 gm%. The patient had controlled diabetes and was on oral hypoglycemic drugs with no signs of systemic involvement (septicemia). The patient was treated with Ayurvedic treatment only. The plan of care was to perform Chedana karma (excise) of the dead infected tendon with local and systemic management by Ayurvedic medicine only.
3. Diagnostic assessment
The clinical examination was based on the size, shape, margin, floor and depth of the ulcer. All DFU patients were diagnosed using the Wagner classification, which included case 1 (Grade V), case 2 (Grade II), case 3 (Grade IV), case 4 (Grade IV), case 5 (Grade IV), case 6 (Grade IV), and blood tests. After analyzing the signs and symptoms according to Ayurvedic principles, the patients were diagnosed as Dustavrana (non-healing ulcer) and treatment was planned accordingly [5].
4. Therapeutic intervention
The treatment was tailored to the severity of the ulcer (Wagner classification) as well as the dosha (Vata, Pitta, and Kapha) and Dushya (Twak, Rakta, Mamsa, Meda, Asthi) involved in the disease's manifestation. Integration of standard and Ayurvedic treatment (Table 1) was planned in order to control DM, dehydration, and septicemia in the initial phase. Later, the ulcers were managed with Ayurvedic treatment (internal and external) procedures to enhance the healing process.
5. Follow up and outcome
6. Follow up of the patients was done for one year to observe for recurrence, but all the patients recovered well with an improved quality of life. The patients were treated with integrated treatment based on the clinical symptoms and severity. In the initial phase of management, allopathic treatment has minimized the infection and, in the latter phase, adopted Ayurvedic treatment has given good results and improved the quality of patient life. The patients with Wagner classification II and without signs of septicemia were well managed on pure Ayurvedic treatment both internally and externally, which has given good results (Table 2) (Fig. 1). The ulcer on Case 2 patient healed in 60 days, whereas the other cases took approximately 3 months (Table 2) (Fig. 2, Fig. 3). Blood parameters like complete blood count, ESR, blood urea, serum creatinine and HbA1c of all the six cases were found normal in the post treatment phase, and patients were advised to continue the same standard treatment for of hyperglycemia control.
Table 2.
Assessment of various Ulcer parameters by Bates Jenson criteria.
| Assessment of Ulcer parameters in Days | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Day | Size | Depth | Edges | Under-mining | Necrotic Tissue Type |
Necrotic Tissue Amount |
Exudate type | Exudate Amount | Skin Color Surrounding Ulcer |
Peripheral Tissue Edema | Peripheral Tissue Induration | Granul-ation Tissue |
Epitheliali-zation | Total Score | |
| Case 1 | 1–15 | 3 | 3 | 3 | 2 | 3 | 4 | 5 | 4 | 3 | 4 | 3 | 5 | 4 | 46 |
| 25–-40 | 3 | 2 | 2 | 2 | 2 | 3 | 4 | 3 | 2 | 2 | 2 | 4 | 3 | 34 | |
| 55–70 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 2 | 1 | 1 | 1 | 3 | 2 | 22 | |
| 85–95 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 13 | |
| Case 2 | 1–10 | 2 | 2 | 2 | 2 | 4 | 2 | 4 | 3 | 5 | 4 | 3 | 3 | 3 | 39 |
| 20–30 | 2 | 2 | 2 | 1 | 2 | 1 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 23 | |
| 40–55 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 13 | |
| Case 3 | 1–15 | 5 | 5 | 4 | 4 | 4 | 4 | 5 | 4 | 5 | 4 | 4 | 4 | 4 | 50 |
| 30–50 | 4 | 4 | 3 | 3 | 3 | 3 | 4 | 3 | 3 | 2 | 3 | 3 | 3 | 35 | |
| 65–80 | 3 | 3 | 2 | 2 | 2 | 2 | 3 | 2 | 3 | 2 | 2 | 2 | 2 | 24 | |
| 95–110 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 3 | 1 | 1 | 1 | 1 | 15 | |
| Case 4 | 1–20 | 4 | 4 | 4 | 3 | 4 | 4 | 4 | 4 | 5 | 4 | 4 | 4 | 4 | 52 |
| 35–55 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 2 | 3 | 3 | 3 | 40 | |
| 70–80 | 2 | 2 | 2 | 2 | 2 | 2 | 3 | 2 | 2 | 2 | 2 | 2 | 2 | 29 | |
| 90–105 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 13 | |
| Case 5 | 1–15 | 5 | 5 | 5 | 4 | 5 | 5 | 5 | 5 | 5 | 4 | 4 | 4 | 4 | 56 |
| 30–50 | 4 | 4 | 4 | 3 | 4 | 4 | 4 | 4 | 5 | 4 | 4 | 4 | 4 | 48 | |
| 65–75 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 2 | 3 | 3 | 3 | 33 | |
| 90–100 | 2 | 2 | 2 | 2 | 2 | 2 | 3 | 2 | 2 | 2 | 2 | 2 | 2 | 27 | |
| 110–120 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 13 | |
| Case 6 | 1–10 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 2 | 3 | 3 | 3 | 38 |
| 25–32 | 3 | 2 | 3 | 3 | 2 | 3 | 3 | 2 | 3 | 2 | 2 | 3 | 3 | 34 | |
| 50–60 | 2 | 2 | 2 | 2 | 2 | 2 | 3 | 2 | 2 | 2 | 2 | 2 | 2 | 19 | |
| 75–82 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 13 | |
| Ulcer Status continuum | ||||||||||
| 1 | 5 | 10 13 15 | 20 | 25 | 30 | 35 | 40 | 45 | 50 | 55 60 |
| Tissue Health | Ulcer Regeneration | Ulcer degeneration | ||||||||
6. Discussion
Non-mainstream therapies that can be utilized in addition to conventional treatment are referred to as complementary and integrative medicine (CIM). It includes a wide range of therapeutic modalities, such as natural goods (like herbs), mind-body techniques (massage, acupuncture), and additional complementary health modalities [7]. The case was diagnosed as dustavrana and it was treated on the shastiupakrama principle based on analyzing dosha and dushya and incorporating modern medical principles of diabetic foot care. A multidisciplinary approach is to be adopted for comprehensive and integrated care due to the multifaceted nature of foot ulcers and the numerous comorbidities associated with the patients. Published literature has highlighted the importance of integrated approaches for diabetes foot ulcer management in terms of better outcomes and improved quality of life [5].
Ulcer bed preparation is the prime step in ulcer assessment and management, which is achieved by the ‘TIME’ acronym, i.e., tissue debridement, infection or inflammation, moisture balance, and edge effect [8]. The presence of infection is one of the main factors that leads to delay in healing or non-closure of cutaneous ulcers [9]. Guidelines for the choice of empirical antibiotics and criteria to assess the severity of DFIs were published by the Infectious Disease Society of America (IDSA) in 2012 and the International Working Group on the Diabetic Foot (IWGDF) in 2016 [10]. Antibiotics in ulcer management (Table 1) favour cellular and vascular proliferation and reduce infection, thus accelerating ulcer healing [11]. Surgical debridement is an essential step in the protocol for treating diabetic foot ulcers, which aims to remove nonviable and necrotic tissue, which prevents the formation of healthy granulation tissue (Table 2) and provides a good environment for harbouring bacteria, thus increasing the risk of sepsis [11]. Vrana Shodhana (Ulcer cleansing) with decoction of Panchavalkala (barks of five trees – Vata (Ficus bengalensis L.), Udumbara (Ficus glomerata Roxb.), Ashwatha (Ficus religiosa L.), Parish (Thespesia populenea Soland. ex corea.), Plaksha (Ficus lacor Buch-Ham.), are proved in the management of ulcer infection. The pharmacological action of Panchavalkala proves that it has anti-inflammatory, analgesic, antimicrobial, and ulcer healing properties [12]. Vranaropana (ulcer healing) is achieved by combining vimlapana with jatyadi taila. Vimlapana is a gentle massage using jatyadi taila, with the help of the thumb and pulp of the fingers, which leads to a rise in the local temperature. This in turn relieves vasoconstriction and provides the necessary nutrients (vitamin C, oxygen, insulin, etc.) to the ulcer site. It is through this mechanism that the anoxic condition of the ulcer is alleviated, and it helps in the regeneration of the epithelial cells and heals the ulcer in a shorter duration of time when compared to the other ulcer healing (Fig. 1, Fig. 2, Fig. 3) processes seen in the DFU [13].
Vrana Dhupana (ulcer fumigation) (Table 1) is a procedure in which an ulcer is subjected to fumes by heating powder of medicinal plants in a special instrument, and it is indicated for ulcers with pain, foul smell, and discharge [14]. Guggulu, Aguru, Vacha, Sarjarasa, Sarshapa, Saindhava lavana, Nimbapatra, and ghee were used in the procedures that have anti-microbial properties against Salmonella typhi, Pseudomonas aeruginosa, Klebsiella pneumoniae, Staphylococcus aureus and reduces pain, secretion, odour from the ulcer [14]. Bandaging was done with Jatyaditaila (JT), which is known for its ulcer healing activity. Previous studies reported that JT has flavonoids, essential oils, tannins, glycosides, steroids, and alkaloids. The HPTLC of JT confirmed the presence of karanjin, lupeol, and β-sitosterol. Topical application of JT on excised ulcers showed a faster reduction in ulcer area and a significant increase in protein, hydroxyproline, and hexosamine content in the granulation tissue [15]. Asanadi Gana drugs are indicated in the management of prameha and research has proved that these drugs possess anti-diabetic effects [16]. Capsule Grab constitutes of Triphala Guggulu, Gandhaka Rasayana, Vranapahari Rasa, Arogyavardhini Vati, Manjistha(Rubia cordifolia. Linn), and Guduchi (Tinospora cordifolia.Thunb). These drugs are proven to combat Prameha and Vrana [[17], [18], [19]]. The ingredients of Kaishoreguggulu are Triphala, Guduchi, Trikatu, and Guggulu, which are helpful in the management of pitta-related disorders and in the management of Vrana [20]. Aragwadha kashaya is known to possess a vrana shodhana effect, and it is indicated in Kaphavikara, Dustavrana, Kandu, and Kustha [21]. Nishamalaki churna is commonly prescribed in clinical practice for Diabetes and it contains two drugs: Curcuma longa (turmeric) and Emblica officinalis (Indian gooseberry). Previous studies on these drugs have proven their anti-hyperglycemic and immunomodulatory activities, which are beneficial in the management of DM and its complications like DFU [22].
Clinical studies on integrative medicine are essential for producing evidence-based practises which are mainly dependent on outcome assessment [23]. Currently, interest is growing in this regard where integration of conventional medicine with other systems of medicine is found useful for treatment of chronic ailments associated with lifestyle and food habits [24].
7. Informed consent
Informed consent regarding documentation and publication of the case was obtained from all the patients.
8. Conclusion
An integrated approach with allopathic and Ayurveda is essential for proper assessment and treatment of diabetic foot ulcers. Recurrent infection is a major drawback of treatment, which worsens the patient's condition and leads to amputation after prolonged conservative management. Integrated treatment adopted in all the six cases has given good outcomes. Randomised clinical trials with good sample size in this aspect are necessary for producing evidence-based practises in the future.
Author statement
All the authors provided their contributions in treating the patients. Dr Ramesh Killedar and Dr Pradeep Shindhe involved in the collection of data. Analysis, interpretation of the data was done by all the authors. Manuscript drafting was done by Dr Ramesh Killedar and review, correction of manuscript was done by Dr Pradeep Shindhe and Dr Ajay Kale. Approval from all the authors was provided for the submitted manuscript.
Financial support and sponsorship
Nil.
Declaration of competing interest
No conflicts of interest.
Acknowledgement
Dr.Suhas Kumar Shetty, Principal, KAHER's Shri B. M. Kankanawadi Ayurveda Mahavidyalaya, Shahapur, Belagavi and all the patients for providing the consent for treatment and publication.
Footnotes
Peer review under responsibility of Transdisciplinary University, Bangalore.
References
- 1.Kodner D.L., Spreeuwenberg C. Integrated care: meaning, logic, applications, and implications--a discussion paper. Int J Integrated Care. 2002;2:e12. doi: 10.5334/ijic.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Everett E., Mathioudakis N. Update on management of diabetic foot ulcers. Ann N Y Acad Sci. 2018;1411(1):153–165. doi: 10.1111/nyas.13569. PMID: 29377202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reiber G.E., Vileikyte L., Boyko E.J., del Aguila M., Smith D.G., Lavery L.A., et al. Causal pathways for incident lower-extremity ulcers in patients with diabetes from two settings. Diabetes Care. 1999;22:157–162. doi: 10.2337/diacare.22.1.157. [PubMed] [Google Scholar] [DOI] [PubMed] [Google Scholar]
- 4.Neelambika G.B., Balu V., Rashel Rego M., Kesari C. Integrative approach for diabetic foot management- a case report. J Ayurveda Integr Med. 2018;9(4):298–301. doi: 10.1016/j.jaim.2018.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alexiadou K., Doupis J. Management of diabetic foot ulcers. Diabetes Ther. 2012;3(1):4. doi: 10.1007/s13300-012-0004-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Feng Y., Schlösser F.J., Sumpio B.E. The Semmes Weinstein monofilament examination as a screening tool for diabetic peripheral neuropathy. J Vasc Surg. 2009;50:675–682. doi: 10.1016/j.jvs.2009.05.017. [DOI] [PubMed] [Google Scholar]
- 7.Leong M., Smith T.J., Rowland-Seymour A. Complementary and integrative medicine for older adults in palliative care. Clin Geriatr Med. 2015;31(2):177–191. doi: 10.1016/j.cger.2015.01.004. [PubMed] [CrossRef] [Google Scholar] [DOI] [PubMed] [Google Scholar]
- 8.Halim A.S., Khoo T.L., Saad A.Z. Ulcer bed preparation from a clinical perspective. Indian J Plast Surg. 2012;45(2):193–202. doi: 10.4103/0970-0358.101277. PMID: 23162216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Altoé L.S., Alves R.S., Sarandy M.M., Morais-Santos M., Novaes R.D., Gonçalves R.V. Does antibiotic use accelerate or retard cutaneous repair? A systematic review in animal models. PLoS One. 2019;14(10):1–22. doi: 10.1371/journal.pone.0223511. PMID: 31600279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kwon K.T., Armstrong D.G. Microbiology and antimicrobial therapy for diabetic foot infections. Infect Chemother. 2018 Mar;50(1):11–20. doi: 10.3947/ic.2018.50.1.11. PMID: 29637748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bowler P.G., Duerden B.I., Armstrong D.G. Ulcer microbiology and associated approaches to Ulcer management. Clin Microbiol Rev. 2001;14(2):244–269. doi: 10.1128/CMR.14.2.244-269.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhat K.S., Vishwesh B.N., Sahu M., Shukla V.K. A clinical study on the efficacy of Panchavalkala cream in Vrana Shodhana w.s.r to its action on microbial load and Ulcer infection. Ayu. 2014;35(2):135–140. doi: 10.4103/0974-8520.146216. PMID: 25558157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kulkarni Y.S., Emmi S.V., Dongargaon T.N., Wali A.A. Ulcer healing effect of Vimlāpanakarma with Jātyāditailam in diabetic foot. Ancient Sci Life. 2015;34(3):171–174. doi: 10.4103/0257-7941.157164. PMID: 26120233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Acharya Y.T., editor. Sushruta, Sushruta Samhita (ChikitsaSthan, 1/80,)., with dalhan nibandhasangraha commentary. 1st ed. Chaukhambha Surabharati Publication; Varanasi, Uttar Pradesh, India: 1994. p. 404. [Google Scholar]
- 15.Shailajan S., Menon S., Pednekar S., Singh A. Ulcer healing efficacy of JatyadiTaila: in vivo evaluation in rat using excision Ulcer model. J Ethnopharmacol. 2011 Oct 31;138(1):99–104. doi: 10.1016/j.jep.2011.08.050. PMID: 21907784. [DOI] [PubMed] [Google Scholar]
- 16.Gupta V., Keshari B.B., Tiwari S.K., Murthy K.H. A comparative study of Shilajatu and Asanadi Ghana Vati in the management of Madhumeha w.s.r. to type-2 diabetes mellitus. Ayu. 2016;37(2):120–124. doi: 10.4103/ayu.AYU_211_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sathish H.S., Dudhamal Tukaram, Gupta Sanjay, Bhuyan C., Baghel M.S. Overview of academic researches on vranaropan (tissue healing) properties of ayurvedic drugs. Indian Journal of Ancient Medicine and Yoga. 2014;7(1):33–47. [Google Scholar]
- 18.Mitra S., Prajapati P.K., Shukla V.J., Ravishankar B. Impact of Bhavana Samskara on physico-chemical parameters with special reference to Gandhaka Rasayana prepared by different media and methods. Ayu. 2010;31(3):382–386. doi: 10.4103/0974-8520.77155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hegde P., Hemanth D.T., Emmi S.V., Shilpa M.P., Shindhe P.S., Santosh Y.M. A case discussion on eczema. Int J Ayurveda Res. 2010;1(4):268–270. doi: 10.4103/0974-7788.76792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bharati P.L., Agrawal P., Prakash O. A case study on the management of dry gangrene by kaishore Guggulu, sanjivani vati and dashanga lepa. Ayu. 2019;40(1):48–52. doi: 10.4103/ayu.AYU_244_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ratha K.K., Barik L., Panda A.K., Hazra J. A single case study of treating hypertrophic lichen planus with Ayurvedic medicine. Ayu. 2016;37(1):56–61. doi: 10.4103/ayu.AYU_1_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Panda V., Deshmukh A., Singh S., Shah T., Hingorani L. An Ayurvedic formulation of Emblica officinalis and Curcuma longa alleviates insulin resistance in diabetic rats: involvement of curcuminoids and polyphenolics. J Ayurveda Integr Med. 2021;12(3):506–513. doi: 10.1016/j.jaim.2021.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Greeson J.M., Rosenzweig S., Halbert S.C., Cantor I.S., Keener M.T., Brainard G.C. Integrative medicine research at an academic medical center: patient characteristics and health-related quality-of-life outcomes. J Alternative Compl Med. 2008;14(6):763–767. doi: 10.1089/acm.2008.0114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Seetharaman M., Krishnan G., Schneider R.H. The future of medicine: frontiers in integrative health and medicine. Medicina. 2021;57(12):1303. doi: 10.3390/medicina57121303. Published 2021 Nov 28. [DOI] [PMC free article] [PubMed] [Google Scholar]