Abstract
Background
A daily habit of yogic practice or walking, along with an oral hypoglycemic agent (OHA) could be beneficial for better control of type 2 diabetes mellitus (T2DM). We conducted a systematic review and meta-analysis of randomized controlled trials (RCTs) to find out the efficiency of yoga or walking on glycemic control in T2DM.
Methodology
The present systematic review and meta-analysis were completed according to the PRISMA guidelines. The risk of bias in included studies was evaluated, by using the revised Cochrane risk-of-bias tool for randomized trials. Meta-analysis was implemented using RevMan software. Forest plots were used to illustrate the study findings and meta-analysis results.
Results
Sixteen studies were included in this systematic review, where 1820 participants were allocated to one of the following interventions: yoga, walking, and without any regular exercise (control group). Participants were between 17–75 years of age. Compared to the control group, the yoga group had a significant reduction in fasting blood glucose (FBG) by 31.98 mg/dL (95% CI = –47.93 to –16.03), postprandial blood glucose (PPBG) by 25.59 mg/dL (95% CI = –44.00 to –7.18], glycosylated hemoglobin (HbAlc) by 0.73% (95% CI = –1.24 to -0.22), fasting insulin by 7.19 μIU/mL (95% CI = –12.10 to –2.28), and homeostatic model assessment for insulin resistance (HOMA-IR) by 3.87 (95% CI = –8.40 to -0.66). Compared to the control group, the walking group had a significant reduction in FBG by 12.37 mg/dL (95% CI = –20.06 to –4.68) and HbA1c by 0.35% (95% CI = –0.70 to –0.01). Compared to the walking group, the yoga group had a significant reduction in FBG by 12.07 mg/dL (95% CI = –24.34 to – 0.20), HbA1c by 0.20% (95% CI = –0.37 to –0.04), fasting insulin by 10.06 μIU/mL (95% CI = –23.84 to 3.71) and HOMA-IR by 5.97 (95% CI = –16.92 to 4.99).
Conclusions
Yoga or walking with OHA has positive effects on glycemic control. For the management of T2DM, yoga has relatively more significant effects on glycemic control than walking.
Review registration number: PROSPERO registration number CRD42022310213
Keywords: yoga, walking, type 2 diabetes, glycemic control, insulin resistance
INTRODUCTION
Type 2 diabetes mellitus (T2DM) is a common metabolic disorder characterized by chronic hyperglycemia.1 It is affected by a combination of two primary factors: defective insulin secretion of pancreatic β-cells and the inability of insulin-sensitive tissues to respond appropriately to insulin.2 Poor glycemic control among T2DM patients is a major community health problem and is a significant risk factor for the advancement of diabetic complications. Glycemic control is the key healing objective for the prevention of organ damage and other health-related problems from diabetes. A rapid change in people’s lifestyle in terms of physical inactivity collectively increases metabolic complications and gives rise to the problems related to T2DM.3
Yoga is an ancient pre-Vedic science and a way of life. Yoga originated in ancient India over 5000 years ago. It mainly aims to develop the psychophysiological health of an individual. The practice of yoga embraces moral observances (Yama), self-disciplines (Niyama), physical postures (Asana), voluntarily controlled breathing (Pranayama), Sensory withdrawal (Pratyahara), Concentration (Dharana), Meditation (Dhyana), and self-realization (Samadhi) and certain philosophical principles.4 Regular yogic practice with proper scientific dose is beneficial for controlling numerous lifestyle diseases, including type 2 diabetes.5 Walking is a natural and primitive exercise pattern that an individual follows from childhood. It is the fundamental base of locomotion and good exercise for the whole body.6
A daily habit of yogic practice reduces mental and oxidative stress and is beneficial to attain glycemic control.5,7 A growing body of evidence reports that regular physical activity like walking or yoga has a beneficial effect on metabolic activity by helping to promote better glycemic control.7,8 Scientific research on walking suggests that walking is one of the safest cardiovascular activities that improves glycemic control and insulin sensitivity.6,8
Walking and yoga have an impact on glycemic control and insulin resistance for type 2 diabetes patients. The aim of this systematic review and meta-analysis was to pool all experimental results of randomized control trials (RCTs) to update and consolidate the evidence on the effect of yoga and walking on glycemic control in patients with T2DM.
METHODOLOGY
The present systematic review and meta-analysis was completed following PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.9
Search strategies
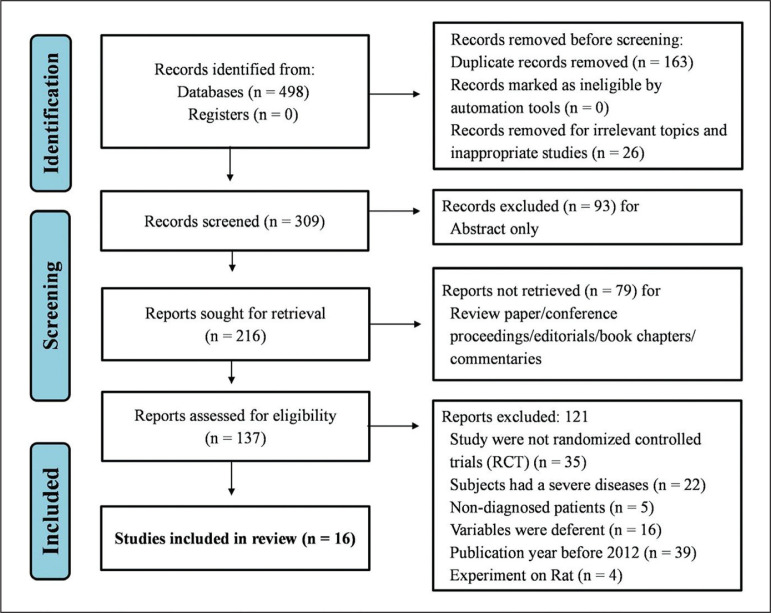
Data were collected by searching the online databases PubMed, Scopus, Web of Science, BioMed Central, ClinicalTrials.gov, and International Clinical Trials Registry Platform (ICTRP) to find out appropriate RCTs. The following keywords were used: ‘type 2 diabetes,’ ‘T2DM,’ ‘yoga,’ ‘walking,’ ‘yoga and Type 2 diabetes,’ and ‘walking and Type 2 diabetes,’ which is illustrated in Table 1. Appropriate trials were limited to human subjects and only trials published with the full text in the last 10 years (2012 to 2022) and written in English were included in this study. The related studies acquired from the above databases were assembled and duplicates were removed; some inappropriate studies were further screened and excluded by reading the title, abstract, and selected manuscripts. After the final assessment, eligible articles were included in the systematic review and meta-analysis. The total selection process is illustrated in Figure 1.
Table 1.
Articles identified according to search sequence and database used for the systematic review
| Bibliographic databases↓ | Search strategies | |||
|---|---|---|---|---|
| Yoga vs control on T2DM | Walking vs control on T2DM | Yoga vs walking on T2DM | Other exercises on T2DM | |
| PubMed = 154 | 64 | 52 | 16 | 22 |
| Scopus = 113 | 40 | 38 | 17 | 18 |
| Web of Science = 99 | 28 | 29 | 18 | 24 |
| BioMed Central = 79 | 28 | 29 | 13 | 9 |
| ClinicalTrials.gov (United States National Library of Medicine) = 27 | 12 | 8 | 4 | 3 |
| International Clinical Trials Registry Platform (ICTRP) = 26 | 6 | 8 | 0 | 12 |
Figure 1.
Flow diagram of the present study prepared as per PRISMA guidelines.
Eligibility criteria
Inclusion criteria
The existing studies followed the PICOS criteria,10 including:
(P) Participants: patients with type 2 diabetes mellitus with standard medication (OHA).
(I) Intervention: walking and yoga.
(C) Control: without any regular exercise.
(O) Outcomes: fasting blood glucose (FBG), postprandial blood glucose (PPBG) and glycosylated hemoglobin (HbAlc), fasting insulin level and homeostatic model assessment for insulin resistance (HOMA-IR).
(S) Study design: randomized controlled trials (RCT).
Exclusion criteria
Participants: adolescents with T2DM (under 17 years of age) and geriatric age groups (above 75 years of age); those with severe diseases or any severe illness; pregnancy; those who were participating in another physical exercise program at the same time.
Study design: articles that were not RCTs were not included in the study;
Review studies, duplicate studies, only abstracts, conference proceedings, editorials, book chapters, and commentaries were excluded.
Studies published before the year 2012 were excluded.
Risk of bias assessment
The risk of bias in included studies was evaluated by using the revised Cochrane risk-of-bias tool for randomized controlled trials (RoB-2)11 which is illustrated in Table 5. According to this tool, the risk of bias in the study was assessed through five Domains. 1. Risk of bias arising from the randomization procedure; 2. Risk of bias due to deviances from the intended interventions (effect of assignment to intervention and adhering to intervention); 3. Risk of bias due to missing results data; 4. Risk of bias in the measurement of the outcome; and 5. Risk of bias in the selection of the reported outcome. The risk of bias is classified as “Low risk,” “Some concerns,” and “High risk”.
Table 5.
Risk of bias assessment of the included studies
| Sl. No | Authors and year | Domain 1 (randomization process) | Domain 2 (assignment to intervention) | Domain 2 (adhering to intervention) | Domain 3 (missing outcome data) | Domain 4 (measurement of the outcome) | Domain 5 (selection of the reported result) | Overall risk of bias |
|---|---|---|---|---|---|---|---|---|
| 1 | Gowri et al., 2022 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| 2 | Kaur et al., 2021 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| 3 | Danasegaran et al., 2021 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| 4 | Viswanathan et al., 2021 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| 5 | Sharma et al., 2020 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| 6 | Kumpatla et al., 2015 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| 7 | Leischik 2021 | Low risk | Low risk | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| 8 | Rafii et al., 2018 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| 9 | Akbarina et al., 2018 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| 10 | Karstoft et al., 2013 | Low risk | Some concerns | Low risk | Low risk | Low risk | Low risk | Some concerns |
| 11 | Yuniartikaet et al., 2021 | Low risk | Low risk | Low risk | Some concerns | Low risk | Low risk | Some concerns |
| 12 | Gupta et al., 2020 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| 13 | Saberipour et al., 2020 | Low risk | Some concerns | Low risk | Low risk | Low risk | Low risk | Some concerns |
| 14 | Singh et al., 2020 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| 15 | Keerthi et al., 2017 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| 16 | McDermott et al., 2014 | Low risk | High risk | Low risk | Some concerns | High risk | High risk | High risk |
Statistical analysis
Quantitative outcomes were collected from the included studies3,6,12-25 for the statistical meta-analysis was performed by using RevMan statistical software (version 5.4.1). In order to pool the measures of treatment effect, a random effects model based on the inverse variance method was used. The effect size was calculated by taking the difference from mean and standard deviation (SD) of FBG, PPBG, HbA1c levels, fasting insulin, and HOMA-IR in the subjects before and after the intervention in both the experimental group and the control group. If the study failed to report this data, the effect size of the mean difference and SD difference was calculated by the following formula:26,27
where r=0.7. Gowri et al., reported only the Median and interquartile range (upper and lower value) in their study so in that case from Median (m), First quartile (q1), and Third quartile (q3) sample Mean () and SD was calculated by using this formula and .28
Mean difference and 95% confidence intervals were used as the summary statistic for the overall effect sizes. The I2 statistic was used to test for heterogeneity of effect size among studies included in the meta-analysis. Forest plots were used to illustrate the study findings and meta-analysis results. FBG and PPBG are stated as mg/dL. HbA1c is stated as a percentage (%). Fasting insulin is stated as μIU/mL.
RESULTS
Study characteristics
After the removal of duplicates, screening of studies, and excluding some studies, 16 RCTs were finally included in this systematic review. Nine studies were included as a comparison of the yoga intervention group with the control group. They are summarized in Table 2. Seven studies were included as a comparison of the walking intervention group with the control group. They are summarized in Table 3. Six studies were included as a comparison of the yoga intervention group with the walking group. They are summarized in Table 4. Three studies were included as a comparison of yoga and walking with the control group.6,12,13 These three studies were analyzed in three sub-groups (yoga vs control, walking vs control, and yoga vs walking). A total of 1820 participants (1054 males, 766 females) were included, and the age range of participants was 17–75 years.
Table 2.
Characteristics of included studies on yoga intervention and control group
| Sl. No. | Authors and year | Participants (Recruited, age and sex) | Intervention (Type, intensity and duration) | Comparison condition | Outcomes | Study design |
|---|---|---|---|---|---|---|
| 1 | Gowri et al., 2022 | Yoga – M/F 14/21, Age 54 ± 13 Control – M/F 23/12, Age 52.5 ± 11.2 |
Yoga 60 min/day, 2 days/week for 16 weeks |
Control group with standard medication | FBG, PPBG, HbA1c, BMI, HOMA-IR, Lipids | RCT |
| 2 | Kaur et al., 2021 | Yoga – M/F 19/72, Age 47.77 ± 9.59 Control – M/F 30/63, Age 49.24 ± 10.53 |
Yoga 60 min/day, 5 days/week for 12 weeks |
Control group with standard medication | FBG, PPBG, HbA1c, BMI, WC, Lipids | RCT |
| 3 | Danasegaran et al., 2021 | Yoga – M/F 40/0, Age 51.95 ± 6.17 Control – M/F 40/0, Age 51.48 ± 8.47 |
Yoga 40 min/day, 5 days/week for 12 weeks with medication |
Control group with standard medication | FPG, BP, Insulin, BMI, Lipids | RCT |
| 4 | Viswanathan et al., 2021 | Yoga – M/F 93/57, Age 50.8 ± 8.3 Control – M/F 103/47, Age 52.8 ± 7.0 |
Yoga 50 min/day, 5 days/week for 12 weeks |
Control group with standard medication | FPG, PPPG, HbA1c, Lipids | RCT |
| 5 | Yuniartika et al., 2021 | Yoga – M/F 7/11, Age 51.66 Control – M/F 8/10, Age 51.11 |
Yoga 60 min/day, 3 days/week for 12 weeks |
Control group with standard medication | FBG, Lipids | RCT |
| 6 | Saberipour et al., 2020 | Yoga – M/F 32/0, Age 48.25 ± 7.14 Control – M/F 33/0, Age 51.66 ± 11.06 |
Yoga 60 min/day, 3 days/week for 8 weeks |
Control group with standard medication | FBG, Lipids, BP, BMI | RCT |
| 7 | Sharma et al., 2020 | Yoga – M/F 32/20, Age 50.8 ± 8.3 Control – M/F 25/27, Age 52.8 ± 7.0 |
Yoga 40 min/day, 5 days/week for 24 weeks |
Control group with standard medication | FBG, PPBG, HbA1c, Lipids, WHR | RCT |
| 8 | Keerthi et al., 2017 | Yoga – M/F 31/29, Age 37.28 ± 6.21 Control – M/F 32/27, Age 36.72 ± 6.12 |
Yoga 38-45 min/day, 3 days/week for 12 weeks |
Control group with standard medication | FPG, Fasting Insulin, HOMA-IR, QoL, IDRS | RCT |
| 9 | Kumpatla et al., 2015 | Yoga – M/F 87/44, Age 41.0 ± 8.7 Control – M/F 71/39, Age 44.2 ± 7.4 |
Yoga 30 min/day, 7 days/week for 12 Weeks |
Control group with standard medication | FPG, PPPG, HbA1c, BP, Lipids, BMI | RCT |
FPG – Fasting Plasma Glucose; PPBG – Post-prandial Blood Glucose; HbA1c – Glycosylated hemoglobin; BMI – Body Mass Index; HOMA-IR – Homeostatic Model Assessment for Insulin Resistance; BMI – Body Mass Index; WC – Waist Circumference; PPPG – Post-prandial Plasma Glucose; FBG – Fasting Blood Glucose; RCT – Randomized Controlled Trial; WHR – Waist Hip Ratio, QoL – Quality of Life
Table 3.
Characteristics of included studies of walking intervention and control group
| Sl. No. | Authors and year | Participants (Recruited, age and sex) | Intervention (Type, intensity and duration) | Comparison condition | Outcomes | Study design |
|---|---|---|---|---|---|---|
| 1 | Leischik 2021 | Waking – M/F 17/0, Age 60.4 ± 5.9 Control – M/F 16/0, Age 59.1 ± 8.5 |
Walking 40 min/day, 3 days/week for 12 weeks |
Control group with standard medication | FPG, HbA1c, Lipids | RCT |
| 2 | Yuniartika et al., 2021 | Walking – M/F 5/13, Age 61.33 Control – M/F 8/10, Age 51.11 |
Walking 30 min/day, 3 days/week for 12 weeks |
Control group with standard medication | FBG, Lipids | RCT |
| 3 | Saberipour et al., 2020 | Walking – M/F 33/0, Age 49.83 ± 9.58 Control – M/F 33/0, Age 51.66 ± 11.06 |
Walking 60 min/day, 3 days/week for 8 weeks |
Control group with standard medication | FBG, Lipids, BP, BMI | RCT |
| 4 | Rafii et al., 2018 | Waking – M/F 15/18, Age 53.18 ± 4.99 Control – M/F 14/20, Age 51.85 ± 7.83 |
Walking 30 min/day, 3 days/week for 8 weeks |
Control group with standard medication | FBG, BMI | RCT |
| 5 | Akbarina et al., 2018 | Waking – M/F 0/12, Age 61.92 ± 3.63 Control – M/F 0/12, Age 61.92 ± 3.63 |
Walking 45-60 min/day, 3 days/week for 8 weeks |
Control group with standard medication | FBG, BMI, HbA1c, Lipids | RCT |
| 6 | Keerthi et al., 2017 | Walking – M/F 30/28, Age 37.28 ± 6.21 Control – M/F 32/27, Age 36.72 ± 6.12 |
Walking 45 min/day, 3 days/week for 12 weeks |
Control group with standard medication | FPG, Fasting Insulin, HOMA-IR, QoL, IDRS | RCT |
| 7 | Karstoft et al., 2013 | Waking – M/F 4/8, Age 60.8 ± 2.2 Control – M/F 3/5, Age 57 ± 3.0 |
Walking 60 min/day, 5 days/week for 16 weeks |
Control group with standard medication | FBG, Fasting Insulin, HbA1c, BP, Lipids. | RCT |
FPG – Fasting Plasma Glucose; FBG – Fasting Blood Glucose; BP – Blood Pressure; BMI – Body Mass Index; HbA1c – Glycosylated hemoglobin; HOMA-IR – Homeostatic Model Assessment for Insulin Resistance; IDRS – Indian Diabetes Risk Score; RCT – Randomized Controlled Trial
Table 4.
Characteristics of included studies on yoga intervention and walking intervention
| Sl. No. | Authors and year | Participants (Recruited, age and sex) | Yoga (Type, intensity and duration) | Walking (Type, intensity and duration) | Outcomes | Study design |
|---|---|---|---|---|---|---|
| 1 | Yuniartika et al., 2021 | Yoga – M/F 7/11, Age 51.66 Walking – M/F 5/13, Age 61.33 |
Yoga 60 min/day, 3 days/week for 12 weeks |
Walking 30 min/day, 3 days/week for 12 weeks |
FBG, Lipids | RCT |
| 2 | Gupta et al., 2020 | Yoga – M/F 21/19, Age 51.1 ± 8.6 Walking – M/F 24/17, Age 50.2 ± 8.6 |
Yoga 45 min/day, 5 days/week for 16 weeks |
Walking 30 min/day, 5 days/week for 16 weeks |
FPG, SBP, DBP, HbA1c, Lipids, BMI, WC | RCT |
| 3 | Saberipour et al., 2020 | Yoga – M/F 32/0, Age 48.25 ± 7.14 Walking – M/F 33/0, Age 49.83 ± 9.58 |
Yoga 60 min/day, 3 days/week for 8 weeks |
Walking 60 min/day, 3 days/week for 8 weeks |
FBG, SBP, DBP, Lipids, BMI | RCT |
| 4 | Singh et al., 2020 | Yoga – M/F 41/60, Age 50.3 ± 9.1 Walking – M/F 49/50, Age 49.4 ± 8.7 |
Yoga 38-115 min/day, 5 days/week for 12 weeks |
Walking 30 min/day, 5 days/week for 12 weeks |
HbA1c, SSAI, STAI, BDI, ESE | RCT |
| 5 | Keerthi et al., 2017 | Yoga – M/F 31/29, Age 37.28 ± 6.21 Walking – M/F 30/28, Age 37.28 ± 6.21 |
Yoga 38-45 min/day, 3 days/week for 12 weeks |
Walking 45 min/day, 3 days/week for 12 weeks |
FPG, Fasting Insulin, HOMA-IR, QoL, IDRS | RCT |
| 6 | McDermott et al., 2014 | Yoga – M/F 9/12, Age 47.0 ± 9.7 Control – M/F 7/13, Age 47.2 ± 9.1 |
Yoga 75 min/day, 3-6 days/week for 8 weeks |
Walking 30 min/day, 3-6 days/week for 8 weeks |
FBG, PPBG, HbA1c, HOMA-IR, BP, Lipids | RCT |
FBG – Fasting Blood Glucose; FPG – Fasting Plasma Glucose; SBP – Systolic Blood Pressure; DBP – Diastolic Blood Pressure; HbA1c – Glycosylated hemoglobin; BMI – Body Mass Index; WC – Waist Circumference; SSAI – Spielberger’s State Anxiety Inventory; STAI – Spielberger’s Trait Anxiety Inventory; BDI – Beck Depression Inventory; ESE – Exercise Self-Efficacy; HOMA-IR – Homeostatic Model Assessment for Insulin Resistance; BP – Blood Pressure
In this review study, included articles used yoga interventions like Trikonasana, Paschimottanasana, Ardha-Matsyendrasana, Dhanurasana, Pawanmuktasana, Vakrasana, Bhujangasana, Anulom-vilom and Bhamri Pranayama, and relaxation techniques such as meditation, prayer, and Savasana. In the majority of the included studies, yoga interventions involved 30-60 minutes per day and five days per week (5 d/w) for twelve weeks (12 w). Subjects of every included study joined the yoga practice in the morning; these practices were facilitated by a yoga expert from the day of recruitment. Included studies had selected similar kinds of OHA: metformin and glimepiride.
This review study included articles that used walking interventions for 30-60 minutes, three days per week (3 d/w) for 8-12 weeks with moderate intensity (brisk walking) on a plane ground surface.
Risk of bias analysis
According to the criteria of the revised Cochrane risk-of-bias tool for randomized controlled trials that is illustrated in Table 5, eleven studies showed ‘low risk of bias’ because these eleven studies were judged to be at low risk of bias for all domains. Four studies showed ‘some concerns’ as these studies were judged to raise some concerns in at least one domain for this effect, but not to be at high risk of bias for any domain. Two studies failed to maintain the criteria of RoB-2 for low risk of bias due to deviances from the intended interventions (intervention assignment).12,14 One study failed to maintain the criteria of low risk of bias due to deviations from the intended interventions (adhering to intervention),15 and one study failed to maintain the criteria of low risk of bias due to missing result data.6 One study showed a ‘high risk of bias’; this study was judged to be at high risk of bias in at least one domain for this outcome or the study is judged to have some concerns for multiple domains in a way that substantially lowers confidence in the result. This study was judged to be at ‘high risk of bias’ due to deviances from the intended interventions (intervention assignment), measurement of the outcome, and selection of the reported result.24
Effect of yoga on glycemic control
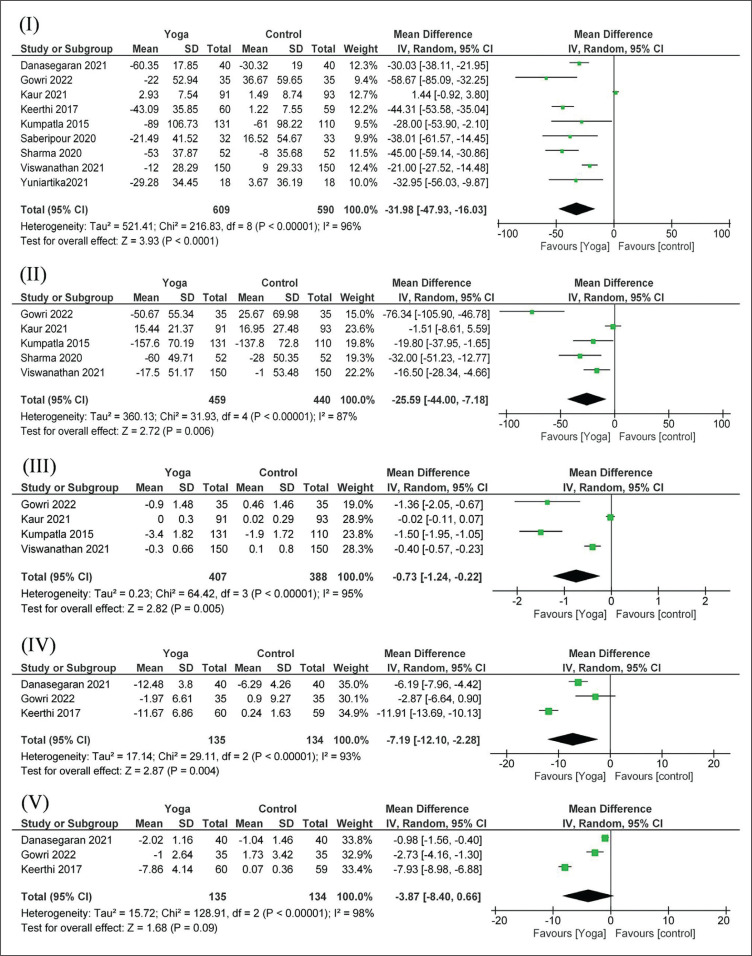
Glycemic control was determined by measuring FBG, PPBG, and HbA1c along with fasting insulin level and HOMA-IR. The effect on FBG was studied in nine studies (9 interventions, n = 1199)3,6,12,13,16,17 included in the meta-analysis. Forest plots for FBG in Figure 2(I) show that there was a significant reduction in FBG in the yoga group in comparison to the control group. The pooled mean difference for FBG between the yoga group and control groups from random effects analysis was 31.98 mg/dL (95% CI = –47.93 to–16.03), and the statistical heterogeneity of the data as indicated by I2 = 96% was statistically significant (p <0.00001). There were five studies (5 interventions, n = 899)3,16-19 in which the effect of yoga on PPBG was studied. The pooled mean difference for PPBG between the yoga group and control groups from random effects analysis was 25.59 mg/dL (95% CI = –44.00 to –7.18; I2 = 87%, p <0.00001) in Figure 2(II). HbA1c was assessed in four of the studies3,16-18 included in the meta-analysis (4 interventions, n = 795). The pooled mean difference from random effects analysis was 0.73% (95% CI = –1.24 to -0.22; I2 = 95%, p <0.00001) in Figure 2(III). There were three studies (3 interventions, n = 269)3,13,20 for fasting insulin between the yoga group and control groups. The pooled mean difference from random effects analysis was 7.19 μIU/ mL (95% CI = –12.10 to –2.28; I2 = 93%, p <0.00001) in Figure 2(IV). HOMA-IR was assessed in 3 of the studies included in the meta-analysis (3 interventions, n = 269).3,13,20 The pooled mean difference for HOMA-IR between the yoga group and control groups from random effects analysis was 3.87 (95% CI = –8.40 to -0.66) in Figure 2(V), and the statistical heterogeneity of the data as indicated by I2 = 98% was significant (p <0.00001).
Figure 2.
Forest plots presenting the effect of Yoga compared to Control group on (I) Fasting Blood Glucose, (II) Postprandial Blood Glucose, (III) Glycosylated Hemoglobin, (IV) Fasting Insulin and (V) Insulin Resistance.
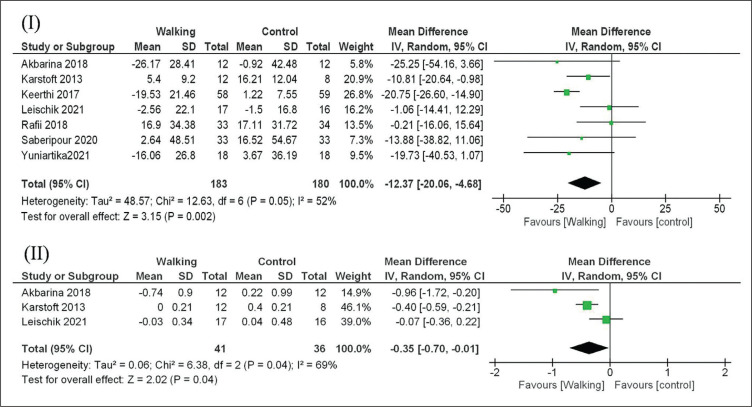
Effect of walking on glycemic control
Glycemic control was determined in the same way by measuring FBG, PPBG, and HbA1c along with fasting insulin and HOMA-IR. The effect on FBG was studied in 7 studies (7 interventions, n = 363)6,12-15,21,22 included in the meta-analysis. There was a statistically significant reduction in FBG in the walking group in comparison to the control group. Forest plots for FBG Figure 3(I) show that there was a significant reduction in FBG in the walking group. The pooled mean difference for FBG between the walking group and control groups from random effects analysis was 12.37 mg/dL (95% CI = –20.06 to –4.68), and the statistical heterogeneity of the data as indicated by I2 = 52% was statistically significant (p = 0.05). There were three studies (3 interventions, n = 77)14,15,22 in which the effect of walking on HbA1c was studied. The pooled mean difference for HbA1c from random effects analysis was 0.35% (95% CI = –0.70 to –0.01; I2 = 69%, p = 0.04) Figure 3(II). The change of HbA1c by 0.35% and FBG of 12.37 mg/dL in the walking group in comparison to the control group is statistically significant but may not be clinically significant.
Figure 3.
Forest plots presenting the effect of Walking compared to Control group on (I) Fasting Blood Glucose and (II) Glycosylated Hemoglobin.
Comparative effect of yoga and walking on glycemic control
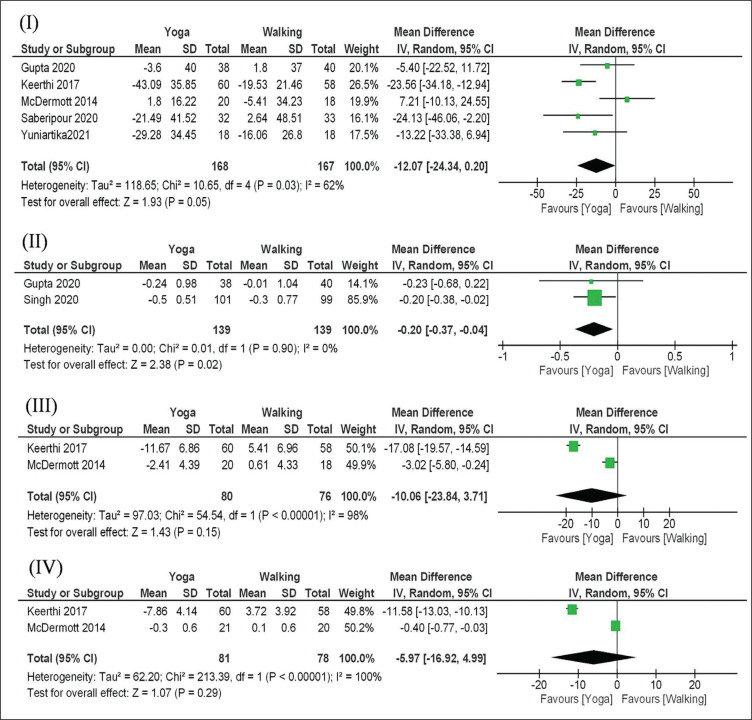
The effect on FBG was studied in five studies (5 interventions, n = 335)6,12,13,23,24 included in the meta-analysis. There was a statistically significant reduction in FBG in the yoga group in comparison to the walking group.
Forest plots for FBG in Figure 4(I) showed that there was a significant reduction in FBG in the yoga group. The pooled mean difference from random effects analysis was 12.07 mg/dL (95% CI = –24.34 to – 0.20; p = 0.03, I2 = 62%). There were two studies (2 interventions, n = 278)23,25 in which the effect of yoga and walking on HbA1c was studied. The pooled mean difference for HbA1c between the yoga group and walking group from random effects analysis was 0.20% (95% CI = –0.37 to –0.04; I2 = 0%, p <0.90) in Figure 4(II). The effect on fasting insulin was studied in two studies (n = 156)13,24 included in the meta-analysis. The pooled mean difference for fasting insulin between the yoga group and walking group from random effects analysis was 10.06 μIU/mL (95% CI = –23.84 to 3.71; I2 = 98%, p <0.00001) in Figure 4(III). There were two studies (2 interventions, n = 159)13,24 in which the effect of yoga and walking on HOMA-IR was studied. The pooled mean difference for HOMA-IR between the yoga group and walking group from random effects analysis was 5.97 (95% CI = –16.92 to 4.99; I2 = 99%, p <0.00001) in Figure 4 (IV).
Figure 4.
Forest plots presenting the effect of Yoga compared to Walking intervention on (I) Fasting Blood Glucose, (II) Glycosylated Hemoglobin, (III) Fasting Insulin and (IV) Insulin Resistance.
DISCUSSION
This meta-analysis observed either the effects of yoga or walking on glycemic control among patients with T2DM. Nine studies with 1197 adults (719 males, 478 females) comparing the yoga intervention to a control group were evaluated. Yoga interventions improved glycemic control by reducing HbA1c, FBG, PPBG, fasting insulin, and HOMA-IR compared to the control group. Seven studies with 365 adults (211 males, 154 females) comparing the walking intervention to a control group were evaluated. Walking interventions improved glycemic control by reducing HbA1c and FBG compared to the control group. Six studies with 541 adults (289 males, 252 females) comparing the yoga intervention to a walking intervention were evaluated. Yoga interventions improved glycemic control by reducing HbA1c, FBG, fasting insulin, and HOMA-IR compared to the walking intervention. Three studies were included comparing yoga and walking with control groups; these were analyzed in three sub-groups (yoga vs control, walking vs control, and yoga vs walking).6,12,13
Our results demonstrate a significant reduction in FBG (31.98 mg/dL), PPBG (25.59 mg/dL), HbA1c (0.73%), fasting insulin (7.19 μIU/mL), and HOMA-IR (3.87) in the yoga intervention compared to the control group (no exercise) in the pooled analysis. In the case of walking intervention compared to the control group (no exercise), the significant reduction of FBG was 12.37 mg/dL and HbA1c was 0.35% in the pooled analysis, but they did not evaluate the PPBG. Only Keerthi et al., evaluated fasting insulin and insulin resistance.13 Similarly our results show a significant reduction in FBG (12.07 mg/dL), HbA1c (0.20%), fasting insulin (10.06 μIU/mL) and HOMA-IR (5.97) in the yoga intervention compared to the walking group in the pooled analysis. Kour et al., showed that after yoga intervention, the mean difference of glycemic control (FBG, PPBG, and HbA1c) decreased in a smaller amount than the control group in patients with type 2 diabetes mellitus.16 McDermott showed that walking has more significant effects on FBG in comparison to yoga in type 2 diabetes mellitus patients.24
Viswanathan et al., revealed that there was a significant reduction in blood glucose levels and HbA1c in the yoga group as compared to the non-yoga group.18 Kumpatla et al., showed that the regular practice of yoga along with conventional medicines could be beneficial for better control of diabetes.17 Saberipour et al., showed that yoga and walking had a positive effect on improving the laboratory indicators in men with type 2 diabetes, but yoga had more significant effects in diabetic patients as compared to walking.12 Some studies exhibited a reduction in FBG, PPBG and HbA1c in the control group compared to the baseline and post-intervention due to the taking of oral hypoglycemic drugs (OHD),15,17-20,22 but this change was not statistically significant. Diabetes is a psychosomatic disease related to both mind and body so psychoneuroendocrine and immune mechanisms are involved in the benefits of yoga on diabetes.5
Diabetes is a growing epidemic among lifestyle-associated cardiometabolic risk syndromes. It is accompanied by insulin resistance.29 The idea of positive health was first introduced by Charaka, the father of the ancient Indian medical system called Ayurveda. He is the composer of the Ayurvedic foundational text, “Charaka Samhita.” According to Charaka, body, mind, and soul are like a tripod.30 In the Vasistha Samhita, we find two types of disease. One is mental (Adhija Vyadhi) and the other is physical (Anadhija Vyadhi).31,32 Disease can germinate in either body or mind. Psychosomatic diseases are those that manifest in the mind and creep into the body, while in somatopsychic it is reversed. Yoga is a therapy that is a mind–body medicine.33 Yoga as a part of Vedic philosophy that regards the human body as a combination of the mind, body, and soul.34
From this study, it may be recommended that Trikonasana, Paschimattanasana, Pawanmuktasana, Vakrasana, Bhujangasana, Ardha-Matseyendrasana, Dhanurasana, Sabasana, Kapalbhati, Anulom-Vilom and meditation for at least 45-60 minutes for five days per week can be beneficial for patients with diabetes. Walking five days per week and at least 45 minutes daily for people with diabetes can realize benefits to improve glycemic control. Additionally, concentration towards walking (Buddhist walking meditation) has a more favorable effect than the traditional walking program in patients with type 2 diabetes.35 Future studies should emphasize the effects of different parameters of walking exercise on glycemic control of diabetes patients, such as walking frequency, walking time, and intensity.
CONCLUSIONS
In conclusion, this systematic review and meta-analysis provides evidence that either yoga or walking has positive effects on glycemic control and insulin resistance in comparison to the control group (no regular exercise) in patients with type 2 diabetes taking oral hypoglycemic agents. The change of HbA1c and FBG in the walking group compared to the control group is statistically significant but may not be clinically significant. Comparatively, yoga has more significant effects on glycemic control and insulin resistance in comparison to walking for the management of type 2 diabetes.
Statement of Authorship
The authors certified fulfillment of ICMJE authorship criteria.
CRediT Author Statement
BD: Methodology, Software, Validation, Formal analysis, Investigation, resources, Data Curation, Writing – original draft preparation, Writing – review and editing, Visualization, Project administration; SC: Conceptualization, Methodology, Validation, Investigation, Resources, Data Curation, Writing – original draft preparation, Writing – review and editing, Visualization, Supervision, Project administration; SSD: Validation, Writing – review and editing, Supervision, Project administration; MC: Validation, Writing – review and editing, Supervision.
Author Disclosure
The authors declared no conflict of interest.
Funding Source
None.
References
- 1.Hurtado MD, Vella A. What is type 2 diabetes? Medicine. 2019;47(1): 10–5. 10.1016/j.mpmed.2018.10.010. [DOI] [Google Scholar]
- 2.Galicia-Garcia U, Benito-Vicente A, Jebari S, et al. Pathophysiology of type 2 diabetes mellitus. Int J Mol Sci. 2020;21(17):6275. PMID: . PMCID: . 10.3390/ijms21176275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gowri MM, Rajendran J, Srinivasan AR, Bhavanani AB, Meena R. Impact of an integrated yoga therapy protocol on insulin resistance and glycemic control in patients with type 2 diabetes mellitus. Rambam Maimonides Med J. 2022;13(1):e0005. PMID: . PMCID: . 10.5041/RMMJ.10462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mooventhan A, Nivethitha L. Evidence based effects of yoga practice on various health related problems of elderly people: A review. J Bodyw Mov Ther. 2017;21(4):1028–1032. PMID: . 10.1016/j.jbmt.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 5.Raveendran AV, Deshpandae A, Joshi SR. Therapeutic role of yoga in type 2 diabetes. Endocrinol Metab (Seoul). 2018;33(3):307–17. PMID: . PMCID: . 10.3803/EnM.2018.33.3.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yuniartika W, Sudaryanto A, Muhlisin A, Hudiyawati D, Pribadi DR. Effects of yoga therapy and walking therapy in reducing blood sugar levels on diabetes mellitus patients in the community. J Med Sci. 2021; 25;9(E):906–12. 10.3889/oamjms.2021.7104. [DOI] [Google Scholar]
- 7.Hegde SV, Adhikari P, Kotian S, Pinto VJ, D’Souza S, D’Souza V. Effect of 3-month yoga on oxidative stress in type 2 diabetes with or without complications: A controlled clinical trial. Diabetes Care. 2011;34(10):2208–10. PMID: . PMCID: . 10.2337/dc10-2430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koo BK, Han KA, Ahn HJ, Jung JY, Kim HC, Min KW. The effects of total energy expenditure from all levels of physical activity vs. physical activity energy expenditure from moderate-to-vigorous activity on visceral fat and insulin sensitivity in obese Type 2 diabetic women. Diabet Med. 2010;27(9):1088–92. PMID: . 10.1111/j.1464-5491.2010.03045.x. [DOI] [PubMed] [Google Scholar]
- 9.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. PMID: . PMCID: . 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S. PICO, PICOS and SPIDER: A comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res. 2014;14:579. PMID: . PMCID: . 10.1186/s12913-014-0579-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sterne JAC, Savović J, Page MJ, et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. PMID: . 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 12.Saberipour B, Gheibizadeh M, Maraghi E, Moradi L. Comparing the effect of walking and yoga on clinical and laboratory parameters in men with type II diabetes: A randomized controlled clinical trial. Jundishapur J Chro Dise Care. 2020;9(2)e99977. 10.5812/jjcdc.99977. [DOI] [Google Scholar]
- 13.Keerthi GS, Pal P, Pal GK, Sahoo JP, Sridhar MG, Balachander J. Effect of 12 weeks of yoga therapy on quality of life and ndian diabetes risk score in normotensive Indian young adult prediabetics and diabetics: randomized control trial. J Clin Diagn Res. 2017;11(9):CC10–4. PMID: . PMCID: . 10.7860/JCDR/2017/29307.10633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Karstoft K, Winding K, Knudsen SH, et al. The effects of free-living interval-walking training on glycemic control, body composition, and physical fitness in type 2 diabetic patients: A randomized, controlled trial. Diabetes Care. 2013;36(2):228–36. PMID: . PMCID: . 10.2337/dc12-0658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leischik R, Schwarz K, Bank P, et al. Exercise improves cognitive function—a randomized trial on the effects of physical activity on cognition in type 2 diabetes patients. J Per Med. 2021;11(6):530. 10.3390/jpm11060530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kaur N, Majumdar V, Nagarathna R, Malik N, Anand A, Nagendra HR. Diabetic yoga protocol improves glycemic, anthropometric and lipid levels in high risk individuals for diabetes: A randomized controlled trial from Northern India. Diabetol Metab Syndr. 2021;13(1):149. PMID: . PMCID: . 10.1186/s13098-021-00761-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kumpatla S, Michael C, Viswanathan V. Effect of Yogasanas on glycaemic, haemodynamic and lipid profile in newly diagnosed subjects with type 2 diabetes. Int J Diabetes Dev Ctries. 2015;35(2): 181–8. 10.1007/s13410-014-0255-2. [DOI] [Google Scholar]
- 18.Viswanathan V, Sivakumar S, Sai Prathiba A, Devarajan A, George L, Kumpatla S. Effect of yoga intervention on biochemical, oxidative stress markers, inflammatory markers and sleep quality among subjects with type 2 diabetes in South India: results from the SATYAM project. Diabetes Res Clin Pract. 2021;172:108644. PMID: . 10.1016/j.diabres.2020.108644. [DOI] [PubMed] [Google Scholar]
- 19.Sharma, S., Bhardwaj, S., Jangir, S., & Gupta, B. Influence of yoga on status of lipid indices in type 2 diabetes mellitus subjects. Int J Diabetes Dev Ctries, 2020; 40(3), 410–5. 10.1007/s13410-020-00813-8. [DOI] [Google Scholar]
- 20.Danasegaran M, Pal GK, Sahoo J, Pal P, Nanda N, Renugasundari M. Effects of 12 weeks practice of yoga on heart rate variability in males with type 2 diabetes receiving oral antidiabetic drugs: A randomized control trial. J Altern Complement Med. 2021;27(12):1105–15. PMID:. https://doi:10.1089/acm.2020.0489. [DOI] [PubMed] [Google Scholar]
- 21.Rafii F, Masroor D, Haghani H, Azimi H. The effects of tai chi and walking on fasting blood glucose among patients with type II diabetes mellitus. Nursing and Midwifery Studies. 2018;7(2):56. https://doi:10.4103/nms.nms_77_17. [Google Scholar]
- 22.Akbarinia A, Kargarfard M, Naderi M. Aerobic training improves platelet function in type 2 diabetic patients: Role of microRNA-130a and GPIIb. Acta Diabetol. 2018;55(9):893–9. PMID: . 10.1007/s00592-018-1167-2. [DOI] [PubMed] [Google Scholar]
- 23.Gupta U, Gupta Y, Jose D, et al. Effectiveness of yoga-based exercise program compared to usual care, in improving HbA1c in individuals with type 2 diabetes: A randomized control trial. Int J Yoga. 2020; 13(3):233–8. PMID: . PMCID: . 10.4103/ijoy.IJOY_33_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McDermott KA, Rao MR, Nagarathna R, et al. A yoga intervention for type 2 diabetes risk reduction: A pilot randomized controlled trial. BMC Complement Altern Med. 2014;14:212. PMID: . PMCID: . 10.1186/1472-6882-14-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Singh VP, Khandelwal B. Effect of yoga and exercise on glycemic control and psychosocial parameters in type 2 diabetes mellitus: A randomized controlled study. Int J Yoga. 2020;13(2):144–51. PMID: . PMCID: . 10.4103/ijoy.IJOY_45_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Clifton L, Birks J, Clifton DA. Comparing different ways of calculating sample size for two independent means: A worked example. Contemp Clin Trials Commun. 2018;13:100309. PMID: . PMCID: . 10.1016/j.conctc.2018.100309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yagiz G, Akaras E, Kubis HP, Owen JA. The effects of resistance training on architecture and volume of the upper extremity muscles: A systematic review of randomised controlled trials and meta-analyses. Applied Sciences. 2022;12(3):1593. 10.3390/app12031593. [DOI] [Google Scholar]
- 28.Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. PMID: . PMCID: . 10.1186/1471-2288-14-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chatterjee S, Bhattacharya P. Cardiometabolic syndrome and effects of yoga. The Principles and Practice of Yoga in Cardiovascular Medicine. Singapore: Springer Nature Singapore; 2022. [Google Scholar]
- 30.Mondal S. Science of exercise: Ancient Indian origin. J Assoc Physicians India. 2013;61(8):560–2. PMID: . [PubMed] [Google Scholar]
- 31.Kuvalayananda S, Vinekar SL. Yogic therapy basic principles and methods. Twari OP, Kaivalyadhama, Lonavla, India; 2019. (reprinted). [Google Scholar]
- 32.Nagarathna R, Nagendra HR. Yoga for hypertension and heart diseases. Bangalore, India: Vivekananda Yoga Research Foundation, Swami Vivekananda Yoga Prakashana; 2002. (reprinted). [Google Scholar]
- 33.Bhavanani AB. Yoga: The original mind body medicine. 2012. https://www.researchgate.net/publication/237077700. [Google Scholar]
- 34.Taittiriyopanisad SS. Ch. 2: 1–6. Chennai: Shree Ramakrishna Publication; 2008. [Google Scholar]
- 35.Gainey A, Himathongkam T, Tanaka H, Suksom D. Effects of Buddhist walking meditation on glycemic control and vascular function in patients with type 2 diabetes. Complement Ther Med. 2016;26:92–7. PMID: . 10.1016/j.ctim.2016.03.009. [DOI] [PubMed] [Google Scholar]