Abstract
Background
Assessing an older adult’s fitness-to-drive is an important part of clinical decision making. However, most existing risk prediction tools only have a dichotomous design, which does not account for subtle differences in risk status for patients with complex medical conditions or changes over time. Our objective was to develop an older driver risk stratification tool (RST) to screen for medical fitness-to-drive in older adults.
Methods
Participants were active drivers aged 70 and older from 7 sites across 4 Canadian provinces. They underwent in-person assessments every 4 months with an annual comprehensive assessment. Participant vehicles were instrumented to provide vehicle and passive Global Positioning System (GPS) data. The primary outcome measure was police-reported, expert-validated, at-fault collision adjusted per annual kilometers driven. Predictor variables included physical, cognitive, and health assessment measures.
Results
A total of 928 older drivers were recruited for this study beginning in 2009. The average age at enrollment was 76.2 (standard deviation [SD] = 4.8) with 62.1% male participants. The mean duration for participation was 4.9 (SD = 1.6) years. The derived Candrive RST included 4 predictors. Out of 4 483 person-years of driving, 74.8% fell within the lowest risk category. Only 2.9% of person-years were in the highest risk category where the relative risk for at-fault collisions was 5.26 (95% confidence interval = 2.81–9.84) compared to the lowest risk group.
Conclusions
For older drivers whose medical conditions create uncertainty regarding their fitness-to-drive, the Candrive RST may assist primary health care providers when initiating a conversation about driving and to guide further evaluation.
Keywords: Driving issues, Geriatric assessment, Primary care
While the vast majority of older drivers are safe drivers (1,2), concerns regarding medical fitness-to-drive arise when the effects of health conditions associated with aging lead to functional limitations that may affect driving ability. For older adults, driving remains important for community mobility, social participation, and independence (1); however, functional impairments associated with health conditions can impair the ability to drive. While the relative risk of collision increases among those with certain medical conditions (2–4), a diagnosis or age alone (5) is not sufficient to make a clinical determination of one’s fitness-to-drive. Other factors, such as the severity of the disease and its functional impact (eg, mild vs severe stroke) as well as comorbidities and medications should also be considered (6). Hence, correctly determining someone’s fitness-to-drive can be very challenging.
In a study of patients with Alzheimer’s disease, Ranchet et al. found that physicians overestimated the ability to drive in 35% of cases and underestimated the ability in 22% of cases (7). When an older driver is wrongly labeled as unsafe, a premature revocation of licensure and corresponding losses in mobility has dire outcomes ranging from depression to increased risk of death (8). Despite the importance of this topic for health in later life, there is not a validated office-based tool that can be used to predict collision risk (9). Furthermore, simply testing all older drivers using on-road approaches has not proven effective in reducing collisions, and is neither practical nor feasible for every driver for whom there may be a medical concern (10,11). Therefore, efforts to develop screening approaches are needed (1,12).
A major limitation of many proposed screening tools for driving is their dichotomous design, which is not always helpful when determining the level of risk. In complex daily activities, such as driving, a risk stratification tool (RST) may be more useful to categorize the level of behind-the-wheel risk, which can facilitate informed discussions about driving and possibly follow patients over time. This approach has been used successfully for complex health issues, such as risk of hospital readmission among patients with congestive heart failure (13). An ongoing challenge when developing objective tools is to establish a link between the quantification of risk and the outcome in question, which in the present case is at-fault motor vehicle collisions (MVCs) (14). However, rates of at-fault MVCs must be adjusted for actual driving exposure (15,16) given that such rates vary by level of exposure (16,17). The primary aim of the Candrive older driver study was to develop a practical RST that can be easily used as a screening tool by health care providers in their office (18). Such a tool could provide objective information to guide clinicians when fitness-to-drive in older adulthood has been questioned for medical reasons.
Method
Study Design
The Candrive study was a prospective, multicenter study using convenience samples from 7 Canadian sites, and 2 parallel study sites in Australia and New Zealand (Ozcandrive results not included in this analysis) (18). Participant recruitment spanned the period from June 2009 to November 2010; participants were followed until December 2016. Participants were recruited through older adult community organizations, media interview exposure, and advertisements. All sites received approval from their respective research ethics board. All participants provided consent to participate and further provided consent for their provincial or state licensing authority to release their personal driving records to study investigators.
Study Population
Participants were included if they met the following criteria: at least age 70 years, up-to-date driver’s license, access to a vehicle, and driving at least 4 times per week (to have sufficient exposure given the chosen primary outcome measure), estimated life expectancy greater than 5 years, intention to continue to drive for the next 5 years, and a vehicle model year of 1996 or newer. The last criterion was necessary for compatibility with the in-car recording device (ICRD) that required an onboard diagnostic (OBD-II) port, which was mandated in all Canadian vehicles starting in 1996 (19). A unique feature of this longitudinal prospective study was that participants were anticipated to contribute multiple person-years of data, which were updated annually. Each year contributed to 1 person-year of data and ultimately a participant could contribute up to a maximum of 7 person-years of data, depending on how long they remained in the study.
Study Protocol
The Candrive protocol has been previously published (18). Participants from 4 Canadian provinces (Quebec, Ontario, Manitoba, and British Columbia) underwent a comprehensive in-person evaluation annually that included: medical history, driving history, physical examination, cognition screening, and completion of questionnaires related to driving attitudes and perceptions. All participants had their primary vehicle instrumented with a Persentech ICRD that had passive GPS capabilities. Driving data were captured at a rate of 1 Hz and stored on a secure digital (SD) card. In between annual evaluations, participants were followed every 4 months for the first 5 years of the study and then every 6 months to confirm driving status, review their driving record (eg, collisions), changes in health status or medications, and exchange SD cards. For participants who shared their primary vehicle (eg, with a spouse), a radio frequency identification key fob was provided on the vehicle key that automatically detected the driver in the study.
Ministries of Transportation from 3 Canadian provinces provided participant driving records, including police collision reports on an annual basis. Police reports were independently reviewed by 2 collision reconstruction experts who determined the at-fault status for each collision. For 1 jurisdiction (Winnipeg, Manitoba), collision reports were initially police collision reports, but then changed to insurance claims-based data from a public insurance provider (Manitoba Public Insurance [MPI]), as provincial legislation changed the threshold for police involvement in MVCs (20). For the Manitoba collision data, at-fault status was provided by MPI.
Primary Outcome Measure
The objective primary outcome measure was police-reported, blinded, expert-validated, at-fault collisions adjusted per annual kilometers driven (14). The annual distance driven, an objective measure, was derived from the ICRD. If data were missing, the distance was calculated based on extrapolations from the participants’ ICRD with considerations for driving of alternate vehicles or device failure, which amounted to an 8.1% increase in kilometers driven.
Sample Size
Our assumption was that multiple factors from each of the contributing global and contextual domains, including physical, cognitive, emotional, sensory, health, and driving experience and behavior, can affect driving, and thus potentially contribute to the final RST. Given the range of predictive factors across multiple domains while being cognizant of the need for a practical RST, the investigators set the anticipated number of variables to be entered into the final model at approximately 10–12. Using the process to develop clinical prediction rules (21,22), a minimum of 5 and a maximum of 10 outcomes were required for each predictor variable that was entered into the final model (23,24). With up to 12 variables entered into the final model, a minimum of 96 at-fault collisions were required (to conduct stable and valid multivariable analyses). Based on collision rates from Ontario data (25), we determined that the recruitment of 1 000 drivers would be required to provide 25 at-fault collisions per year.
Statistical Analysis
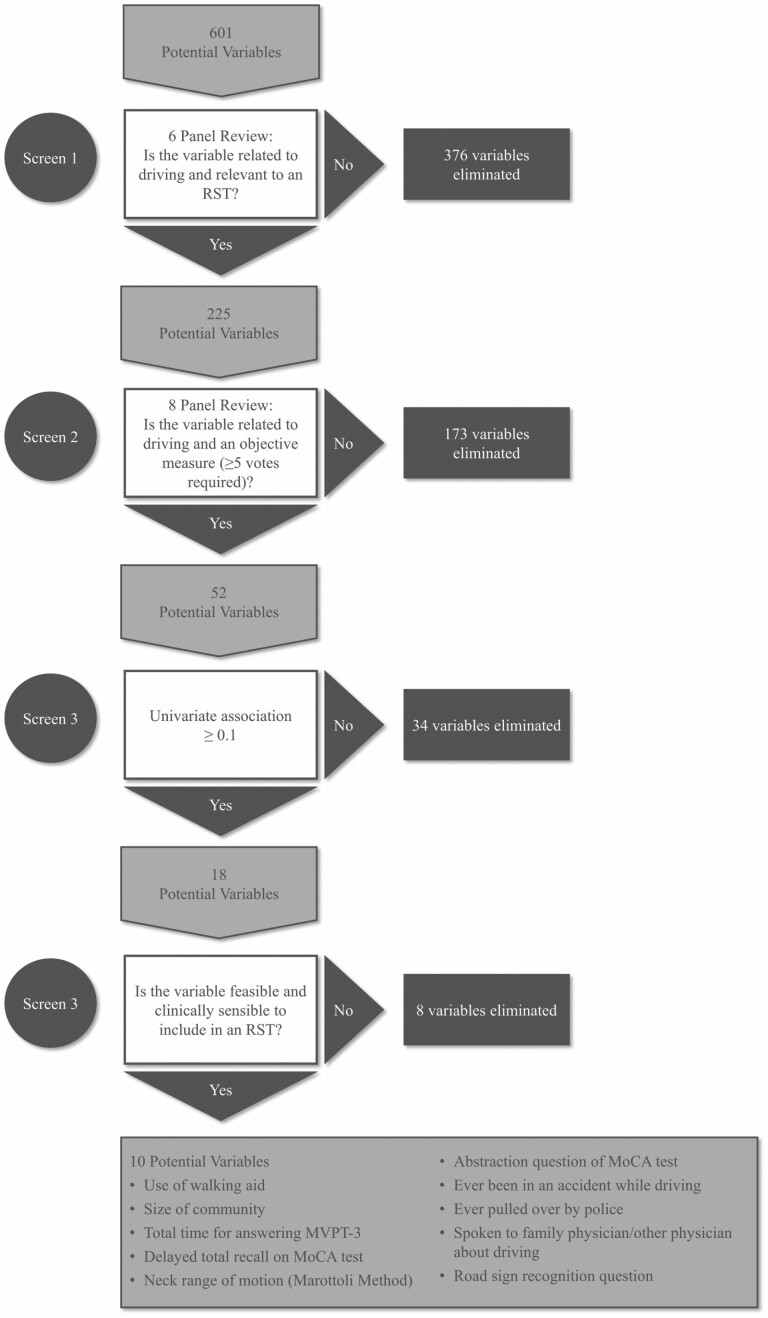
Descriptive statistics were used to characterize the Candrive cohort. The Candrive data set contains 1 480 individual variables (independent of vehicle data) of which many were used for other projects conducted simultaneously with the RST derivation study. Out of 601 potential variables directly related to driving, the investigators identified 52 potential predictor variables that were formally reviewed and determined by the investigators as being objective, could feasibly be collected in an office assessment, and contribute to an RST aimed at estimating the risk of an at-fault collision. We planned to include only objective predictor variables for the RST to reduce the risk of the derived tool’s potential for response bias. For example, subjective measures of confidence or attitudes, which may be predictive of collision risk, would be more susceptible to response bias from patients. Using generalized estimating equations (GEE) to account for participants contributing multiple person-years to the data, univariate analyses were conducted on these 52 variables. Ultimately, 10 of these variables based on the results of the univariate analysis were selected for potential inclusion in the RST (Figure 1).
Figure 1.
Flow diagram for variable selection for Candrive risk stratification tool from the Candrive prospective older driver study. MOCA = Montreal Cognitive Assessment; MVPT-3 = motor-free visual perception test-3; RST = risk stratification tool.
Poisson regression modeling, in combination with GEE, was used to develop the models and Nomograms provided the relative contributions or weights of each variable to the level of estimated risk of an at-fault collision. Statistical analyses were completed using SAS (version 9.3, SAS Institute, Cary, NC).
Results
Demographics
In total, 928 older drivers were recruited across 7 Canadian sites. At the start of the study, participants were 76.2 (standard deviation [SD] = 4.8) years old on average and 62.1% were male participants (Table 1).
Table 1.
Candrive Cohort Demographics
| Parameters | Mean (SD) or No. (%) |
|---|---|
| Age | 76.2 (4.8) |
| Gender | |
| Female | 351 (37.8) |
| Male | 577 (62.1) |
| Marital status | |
| Married | 544 (58.6) |
| Widowed | 231 (24.9) |
| Separated/divorced | 87 (9.4) |
| Common-law | 36 (3.9) |
| Never married | 30 (3.2) |
| Place of residence | |
| Rural | 95 (10.2) |
| Urban | 833 (89.8) |
| Highest level of education completed | |
| Postgraduate | 200 (21.6) |
| Undergraduate degree | 219 (23.6) |
| College diploma | 101 (10.9) |
| Trade/technical certificate | 71 (7.7) |
| High school | 241 (26.0) |
| Grade school | 96 (10.3) |
| Employment status | |
| Full-time | 19 (2.1) |
| Part-time | 106 (11.4) |
| Not employed | 803 (86.5) |
Note: SD = standard deviation.
Attrition
As anticipated for this prospective cohort study, there was attrition because of health, psychosocial factors, and driving cessation. The average number of years contributed was 4.9 (SD = 1.6) out of a maximum of 7 years. By the fifth year of the study, there were 583 participants remaining, with an average age of 79.8 years (SD = 4.5). The total number of participants declined for years 5, 6, and 7 because of 2 sites closing when the study was extended from 5 to 7 years and due to initial rolling recruitment over 1 year where those entering later resulted in less contribution of person-years to the study (Table 2; Supplementary Table 1).
Table 2.
Outcome Measures for Candrive Participants Years 1–7 (abbreviated)
| Parameters | Year 1 (n = 928) | Year 2 (n = 884) | Year 3 (n = 831) | Year 4 (n = 753) | Year 5 (n = 583) | Year 6 (n = 387) | Year 7 (n = 149) |
|---|---|---|---|---|---|---|---|
| Montreal Cognitive Assessment | |||||||
| Total; mean (SD) | 25.9 (2.5) | 26.1 (2.6) | 25.8 (2.6) | 26.0 (2.6) | 26.1 (4.0) | 26.1 (2.6) | 26.5 (2.5) |
| Abstraction (scale 0–2); no. (%) | |||||||
| 0 | 81 (8.8) | 58 (6.6) | 66 (8.0) | 43 (5.7) | 34 (5.9) | 14 (3.6) | 9 (6.0) |
| 1 | 202 (21.8) | 196 (22.3) | 158 (19.0) | 144 (19.2) | 90 (15.6) | 50 (13.0) | 15 (10.1) |
| 2 | 642 (69.4) | 627 (71.2) | 606 (73.0) | 565 (75.1) | 454 (78.6) | 322 (83.4) | 125 (83.9) |
| Missing values | 3 | 3 | 1 | 1 | 5 | 1 | — |
| Delayed recall (scale 0–5); no. (%) | |||||||
| 0 | 64 (6.9) | 65 (7.4) | 76 (9.2) | 73 (9.7) | 64 (11.1) | 40 (10.4) | 19 (12.8) |
| 1 | 74 (8.0) | 61 (6.9) | 85 (10.2) | 70 (9.3) | 44 (7.6) | 40 (10.4) | 10 (6.7) |
| 2 | 163 (17.6) | 138 (15.7) | 148 (17.8) | 129 (17.2) | 96 (16.6) | 71 (18.4) | 17 (11.4) |
| 3 | 230 (24.8) | 206 (23.4) | 182 (21.9) | 174 (23.1) | 136 (23.5) | 78 (20.2) | 31 (20.8) |
| 4 | 246 (26.6) | 226 (25.7) | 197 (23.7) | 151 (20.1) | 138 (23.9) | 87 (22.5) | 41 (27.5) |
| 5 | 149 (16.1) | 185 (21.0) | 142 (17.1) | 155 (20.6) | 100 (17.3) | 70 (18.1) | 31 (20.8) |
| Missing values | 2 | 3 | 1 | 1 | 5 | 1 | — |
| Road sign recognition; no. (%) | |||||||
| Incorrect | 76 (8.2) | 67 (7.6) | 69 (8.3) | 58 (7.8) | 46 (8.1) | 23 (6.0) | 14 (9.5) |
| Correct | 847 (91.8) | 810 (92.4) | 762 (91.7) | 688 (92.2) | 524 (91.9) | 361 (94.0) | 134 (90.5) |
| Missing values | 5 | 7 | 0 | 7 | 13 | 3 | 1 |
| Walking aid; no. (%) | |||||||
| No | 848 (91.4) | 789 (89.3) | 730 (87.9) | 652 (86.6) | 507 (87.0) | 328 (84.8) | 135 (90.6) |
| Yes | 80 (8.6) | 95 (10.8) | 101 (12.2) | 101 (13.4) | 76 (13.0) | 59 (15.3) | 14 (9.4) |
| Missing values | — | — | — | — | — | — | — |
Note: SD = standard deviation.
Collisions
There were 231 (5.2%) police-reported collisions (except Manitoba due to different police reporting patterns) over a total of 4 483 person-years, equating to 5.2% collisions per person-year contributed. Of these, 112 (48%) were at-fault collisions (a participant could contribute greater than 1 at-fault collision). Out of the 112 at-fault collisions, there were 2 associated deaths and 36 associated injuries requiring transportation to the hospital.
Driving Exposure
Older drivers in the Candrive study drove on an average of 11 017.6 (SD = 6 959.9) km per year in the first year of the study, with declines in driving distance and frequency occurring as the study progressed. There was considerable variability in the number of kilometers driven per year across the cohort (Supplementary Table 2).
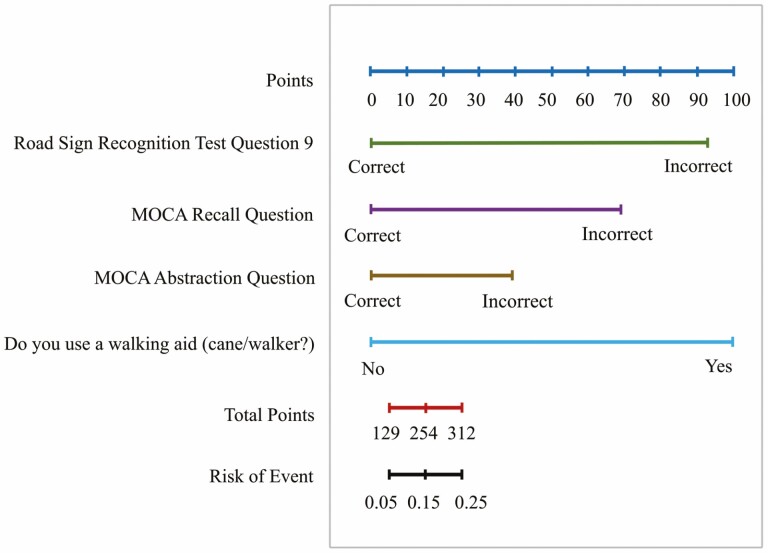
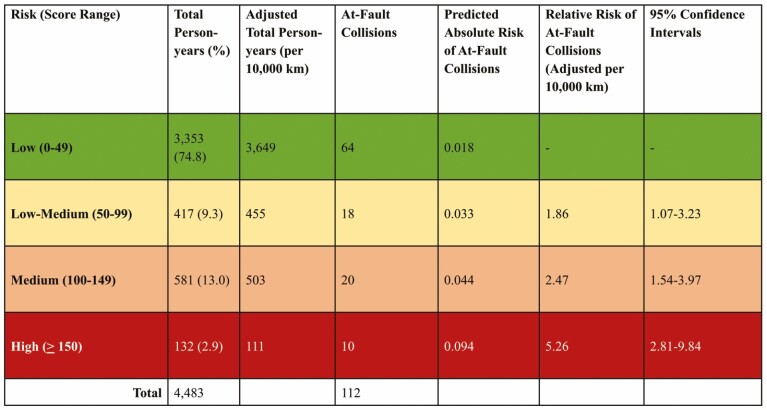
Candrive Older Driver Risk Stratification Tool
Using Poisson regression modeling, 4 independent variables were identified as contributing to the most parsimonious model for the Candrive RST. These 4 weighted variables included a road sign recognition question, the Montreal Cognitive Assessment test (MoCA) 5-word delayed recall question, the MoCA abstraction question, and the participant’s identified need for an assistive walking device. The nomogram in Figure 2 shows the relative contribution of each variable to risk outcome. The sum of these weighted scores determined the risk category for the drivers spanning 4 categories from low to high risk (Figure 3). Based on the weighted variables, drivers in the lowest category scored 0 on all variables and may still have been included if they failed only the abstraction task. The low–medium (RR = 1.86, 95% confidence interval [CI] = 1.07–3.23) and medium (RR = 2.47, 95% CI = 1.54–3.97) risk group represented drivers failing one of the variables or a single variable and the abstraction task. The high-risk category would include those drivers failing at least 2 out of recall, road sign recognition tasks or need for walking aid, and would have 5.26 times the risk of drivers in the low-risk category (95% CI = 2.81–9.84). The highest risk category represented just 2.9% of driver person-years, whereas the majority (74.8%) of driver person-years were in the lowest risk category.
Figure 2.
Nomogram using objective variables (at-fault collisions). MOCA = Montreal Cognitive Assessment.
Figure 3.
Risk stratification tool categories demonstrating relative risk of at-fault collision adjusted for kilometers driven on older drivers.
Discussion
There are 4 predictors to this RST with different weights contributing to an overall risk categorization score. Two of these predictors were derived from the MoCA. While the MoCA test alone has not been shown to adequately predict driving safety (26), our study results indicate that 2 of the questions, in combination with other items, contribute to predicting driver collision risk. The first predictor from the MoCA (27) is the short-term recall task where the older driver is asked to recall 5 words after a delay, and only if none of the 5 words are recalled is the risk score increased. Failing to recall a single word may suggest very significant memory impairment and likely is a marker of global cognitive decline. The abstraction question from the MoCA provides 2 pairs of words and asks for the similar category that the word pair belongs to, which is a test of executive function (28–30). This is the second predictor of the RST, and if either answer for the 2-word pairs is incorrect, the risk score is increased. The road sign recognition task is the third predictor and comprises a 3-item multiple choice question about the meaning of a sign (hidden bus stop sign) that is not a commonly encountered road sign. The unfamiliarity of this sign for drivers presents an opportunity for evaluating deductive reasoning due to the need to process and interpret visual information. Both abstraction and deductive reasoning are elements of executive functioning skills that have been shown to affect driving ability in older adults (31). The final predictor of the RST is the participant’s identified need for a mobility assistance device, such as a cane or walker. This item is reflective of physical mobility challenges, and a potential marker of frailty and physical limitations. Physical limitations have been shown to be associated with an increased risk of other negative driving outcomes (32,33) including reduced mileage and driving cessation.
For this study, person-years were used, as participants contributed multiple years of driving to the study. A noteworthy result of the study is that the majority of person-years of driving (74.8%) fell within the lowest risk category, whereas 9.3% fell in the low–medium category, and 13.0% and 2.9%, respectively, fell within the medium-risk and high-risk categories (Figure 3). At-fault collision risk was also calculated per 10 000 km driven to adjust for exposure. While this study initially recruited participants driving at least 4 times per week, it was anticipated that driving exposure and distance would decline over the course of the study for a significant number of drivers. Langford in 3 separate studies (34–36) has demonstrated the increased risk of low mileage drivers, which needs to be accounted for when assessing risk within this age group.
The advantages of this RST are that (i) it takes approximately 5 minutes to administer, and (ii) it can be completed within any clinic setting without a computer or other special equipment. One potential limitation is that the 4 items making up the RST were derived from a comprehensive battery of assessments where their validity has not been established as a stand-alone tool, therefore requiring further study to confirm its utility in this derived format. Finally, one of the major challenges of the proposed RST is to prevent its misuse. The investigators strongly suggest that this RST not be used for all older drivers presenting to a primary care practitioner, but only when there is genuine uncertainty by the primary care provider regarding fitness-to-drive in the context of medical conditions.
The Candrive RST has been derived prospectively on a cohort of older drivers using a meaningful outcome (ie, at-fault collision adjusted for kilometers driven) and provides an objective risk estimate. While the majority of person-years in the study were in the low-risk category consistent with the collision risk associated with this age group, there was a small percentage of older driver person-years identified as having a greater than 5 times higher risk for at-fault collision.
The Candrive RST is a unique tool in that compared to other tools, it has been developed prospectively on a community sample of older drivers which would be comparable to a primary care setting. Driving prediction tools have typically been developed based on older drivers referred for further driving assessment typically through behind-the-wheel testing (37–39). Furthermore, most tools to date have been based on the primary outcome of the on-road testing result versus the outcome of at-fault collision; while direct observation of driving ability clearly demonstrates function, this step would be seen as a potential next stage for the Candrive RST which would identify higher risk drivers for possible behind-the-wheel testing.
As with any new tool, the implementation and validation of the RST are important considerations. Specifically, since this RST was derived from multiple variables, it is evident that administration in the clinical setting will be different from the study setting, particularly for the 5-item recall test. Intervening tasks and distractors are different, which could affect performance results. While we do provide recommendations based on each risk level (Supplementary Table 3), the RST is not definitive and should complement sound clinical judgment, in that there may be situations where drivers falling in the lower risk categories may not be completely safe to drive and drivers in the highest risk category may, in fact, be potentially safe (40). While the concept of person-years may be difficult to explain to a patient, we believe that explaining the risk as comparison to drivers their own age would be easily comprehended. For example, in the lowest risk category, these drivers would appear to be at similar risk to most drivers of their age. Drivers in the highest risk category would likely need to be informed that they are at significantly higher risk for at-fault collisions and may need to have a further assessment of their fitness-to-drive through objective on-road testing. For the moderate risk categories, this could potentially open discussion with regards to driving and potential opportunities to improve skills or accommodate for limitations and even prepare for the potential future possibility of driving cessation. On the other hand, this clinical tool will also need to be interpreted in the context of the individual assessment recognizing that there may be explanations for the higher risk score, for example where there has been long-term use of a walking aid for a preexisting disability or in temporary situations where the condition is likely to resolve, once again emphasizing that this RST should be used as a part of a broader clinical assessment process.
We anticipate that the RST will not only be of use to primary care providers but also to other health care professionals who interact with older drivers such as psychologists and occupational therapists (41), in settings where the topic of driving ability may be broached. Ideally, the RST will provide an objective starting point for a health care provider to consistently approach and screen for fitness-to-drive in older drivers. This RST should be used by the primary care provider only where there are genuine concerns about an older driver’s ability to drive because applying the RST too broadly may increase the risk of safe drivers being labeled at-risk, for example, when highly functional older patients present with medical conditions not related to driving (eg, sprained ankle from running). Issues that could raise genuine concern by the primary care provider are myriad, but would include specific medical conditions and resulting functional impairments associated with increased driving risks such as cataracts, substance use, dementia, stroke, or obstructive sleep apnea (3). Functional decline, frailty, or family concerns would be other potential indicators. The aim of the RST, thus, is to allow an objective and fair approach to screening for driving risk in older adults with medical conditions, when warranted. We concur with Dickerson et al. (9) that stand-alone measures of fitness-to-drive are not useful. Rather, the value of any evaluation is to identify drivers who are at higher risk and for whom a discussion about driving can guide current and future planning of personal transportation, including whether further in-depth assessments may be needed (Supplementary Table 3). For those drivers in the low-risk category, the driver could be informed that their risk is similar to that of other drivers their own age and this could lead to a conversation about safe driving practices and approaches to maintaining driving skills. For those in the intermediate categories, patients may need to be advised that they are at increased risk, and based on clinical judgment with all elements of the health and social factors available, the primary care provider may be in a position to offer guidance on whether further assessments may be necessary. For the highest risk group where the risk of an at-fault collision exceeds 5 times that of the low-risk drivers, considerations for management would likely include the need for further evaluation or recommendation of driving discontinuation, once again taking into account all elements of the patient history.
Two key questions remain: (i) Is the RST generalizable to a broader older driver population, and (ii) Are the risk categories for at-fault collisions clinically useful? Regarding the generalizability of the results, the Candrive research group has previously compared the Candrive cohort to older Canadian drivers as identified through the Canadian Community Health Survey from Statistics Canada where the 2 groups were found to be similar overall (40). However, a limitation of the Candrive RST is that it was not developed within the clinic or office-based setting. Nevertheless, over the 7 years of the study, many participants developed health issues, and thus possibly a driving safety concern that may have led to driving cessation. The development of aging-related medical conditions may have provided an approximation of the patient population seen by primary care providers for whom the Candrive RST would be appropriate. Furthermore, the collision rate of 5.2% per person-year from our study, for which more than 60% of the drivers were from the province of Ontario, exceeds that of the Ontario population aged 75 and older, which has an annual collision rate of 2.43% (25). However, these data are not adjusted for driving exposure where the Canadian Community Health Survey has shown that greater than 25% of drivers over age 65 with active licenses in the highest functional category, whom had not driven in the previous month, contributed to lower collision rates per licensed driver (42(p. 2)).
Conclusion
This RST may aid primary care providers and other health care professionals with initiating a conversation about driving and guide the further evaluation of fitness-to-drive in older adults with medical conditions that may affect driving performance. Further validation of the RST, including an assessment of its implementation in an office setting, and using data from the Ozcandrive sites, is in progress.
Supplementary Material
Contributor Information
Shawn Marshall, Department of Medicine, The Ottawa Hospital, University of Ottawa, Ottawa, Ontario, Canada; Department of Physical Medicine and Rehabilitation, Bruyère Research Institute, Ottawa, Ontario, Canada.
Michel Bédard, Centre for Research on Safe Driving, Lakehead University, Thunder Bay, Ontario, Canada.
Brenda Vrkljan, School of Rehabilitation Science, McMaster University, Hamilton, Ontario, Canada.
Holly Tuokko, Department of Psychology, University of Victoria, Victoria, British Columbia, Canada.
Michelle M Porter, Faculty of Kinesiology and Recreation Management, University of Manitoba, Winnipeg, Manitoba, Canada.
Gary Naglie, Department of Medicine and Rotman Research Institute, Baycrest Health Sciences, Toronto, Ontario, Canada; Department of Medicine and Institute of Health Policy, Management and Evaluation, University of Toronto, Toronto, Ontario, Canada.
Mark J Rapoport, Department of Psychiatry, Sunnybrook Health Sciences Centre, University of Toronto, Toronto, Ontario, Canada.
Barbara Mazer, School of Physical & Occupational Therapy, McGill University, Montreal, Québec, Canada; Centre for Interdisciplinary Research in Rehabilitation of Greater Montreal, Montreal, Québec, Canada.
Isabelle Gélinas, School of Physical & Occupational Therapy, McGill University, Montreal, Québec, Canada; Centre for Interdisciplinary Research in Rehabilitation of Greater Montreal, Montreal, Québec, Canada.
Sylvain Gagnon, School of Psychology, University of Ottawa, Ottawa, Ontario, Canada.
Judith L Charlton, Monash University Accident Research Centre, Monash University, Clayton, Victoria, Australia.
Sjaan Koppel, Monash University Accident Research Centre, Monash University, Clayton, Victoria, Australia.
Lynn MacLeay, Department of Medicine, The Ottawa Hospital, University of Ottawa, Ottawa, Ontario, Canada.
Anita Myers, School of Public Health & Health Systems, University of Waterloo, Waterloo, Ontario, Canada.
Ranjeeta Mallick, Department of Medicine, The Ottawa Hospital, University of Ottawa, Ottawa, Ontario, Canada.
Tim Ramsay, Department of Medicine, The Ottawa Hospital, University of Ottawa, Ottawa, Ontario, Canada.
Ian Stiell, Department of Medicine, The Ottawa Hospital, University of Ottawa, Ottawa, Ontario, Canada; Department of Emergency Medicine, University of Ottawa, Ottawa, Ontario, Canada.
George Wells, Department of Medicine, The Ottawa Hospital, University of Ottawa, Ottawa, Ontario, Canada.
Malcolm Man-Son-Hing, Department of Medicine, The Ottawa Hospital, University of Ottawa, Ottawa, Ontario, Canada; Island Health, Campbell River, British Columbia, Canada.
Funding
This study was funded by a Team Grant from the Canadian Institutes of Health Research (CIHR) entitled “The CIHR Team in Driving in Older Persons (Candrive II) Research Program” (Grant 90429). Additional support was provided by the Ottawa Hospital Research Institute and the Toronto Rehabilitation Institute, the University Health Network, and the University of Manitoba. The Australian coauthors were supported by an Australian Research Council Linkage grant (LP 100100078; Managing Older Driver Safe Mobility: An International Collaboration) awarded to the Monash University in partnership with La Trobe University, VicRoads, Victorian Government Department of Justice and Victoria Police, the Transport Accident Commission, New Zealand Transport Agency Community Road Safety Fund, the Ottawa Hospital Research Institute, and Eastern Health. The funders had no role in considering the study design or in the collection, analysis, interpretation of data, writing of the report, or decision to submit the article for publication.
Conflict of Interest
M.B. was supported by a Canada Research Chair in Aging and Health during the development phase of this study. G.N. was supported by the George, Margaret and Gary Hunt Family Chair in Geriatric Medicine, University of Toronto, received a grant from the Canadian Consortium on Neurodegeneration in Aging and served as Chair for the Canadian Institutes of Health Research Institute on Aging Advisory Board. M.J.R. was supported by the Sunnybrook Psychiatry Partnership, received grants or contracts from the Canadian Institute of Health Research, Canadian Consortium of Neurodegeneration and Aging, and Centre for Brain Health Innovation, participated on a Data Safety Monitoring Board for a study on multiple sclerosis and exercise, and served as Program Director for Geriatric Psychiatry at the University of Toronto. M.M.P. received grants or contracts from the Social Sciences and Humanities Research Council, Natural Science and Engineering Research Council, Aging Gracefully across Environments using Technology to Support Wellness, Engagement and Long Life Networks of Centres of Excellence Inc., Canadian Institutes of Health Research, New Horizons for Seniors Program, Winnipeg Foundation, Riverview Health Centre Foundation, Mitacs, University Research Grants Program and served as Chair of the Board for Transportation Options Network for Seniors in Manitoba. S.K. served as a Board Member of the Association of the Advancement of Automotive Medicine. The other authors declare no conflict.
Author Contributions
S.M. has full access to the data and is the guarantor of the study. S.M. attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. The Candrive Investigators thank the Candrive cohort study participants for their dedication. Without their commitment, this publication would not have been possible. The Ozcandrive Investigators thank the Ozcandrive cohort study participants for their dedication. Without their commitment, this publication would not have been possible. The Candrive Investigators thank the additional support staff for their dedication and contribution to the success of the study; Dorothyann Curran, Kelly Weegar, and Chantal Rockwell (Ottawa). The Candrive Investigators thank the Research Associates for their dedication and contribution to the success of the study (in order of participant recruitment); Jennifer Biggs and Anita Jessup (Ottawa Coordinating Centre), Phyllis McGee (Victoria), Linda Johnson and Joanne Parsons (Winnipeg), Novlette Fraser and Sue Woodard (Toronto), Sheila Garrett (Hamilton), Felice Mendelsohn, Minh-Thy Dinh Truong, Suzie Schwartz, and Rivi Levkovich (Montreal); Laura Morrison and Hillary Maxwell (Thunder Bay). The Candrive Investigators wish to thank the following individuals for their work associated with the in-vehicle driving data: Glenys Smith, Andrew Cull, Satoru Nakagawa, Sandra Webber, and Maureen Babb (Winnipeg), and Akram Alakel (Ottawa). The Australian Investigators acknowledge the expert advice and significant contribution throughout the project to the Australian-based project investigators: Jim Langford, Marilyn di Stefano, Peteris Darzins, Morris Odell, and Wendy Macdonald. The Ozcandrive Investigators thank Lorraine Atkinson, Ozcandrive Program Manager, for her role in managing and operationalizing the study for the Australian site and Dr. Jared Thomas for oversight of the project at the Wellington site. The Ozcandrive Investigators wish to thank the Research Associates for their dedication and contribution to the success of the study: Louise Beasley and Elizabeth Jacobs (Melbourne), Grace Rive, Kate Mora, and Abigail Harding (Wellington).
References
- 1. Mathias JL, Lucas LK. Cognitive predictors of unsafe driving in older drivers: a meta-analysis. Int Psychogeriatr. 2009;21(4):637–653. doi: 10.1017/S1041610209009119 [DOI] [PubMed] [Google Scholar]
- 2. Marshall SC. The role of reduced fitness to drive due to medical impairments in explaining crashes involving older drivers. Traffic Inj Prev. 2008;9(4):291–298. doi: 10.1080/15389580801895244 [DOI] [PubMed] [Google Scholar]
- 3. Charlton J, Koppel S, Odell M. Influence of chronic illness on crash involvement of motor vehicle drivers.2010;( 300). https://www.monash.edu/__data/assets/pdf_file/0008/216386/Influence-of-chronic-illness-on-crash-involvement-of-motor-vehicle-drivers-2nd-edition.pdf.
- 4. Vaa T. Impairments, diseases, age and their relative risks of accident involvement: results from meta-analysis. The Institute of Transport Economics; 2020;( 690). https://www.toi.no/getfile.php?mmfileid=5780. Accessed August 24, 2021. [Google Scholar]
- 5. Hogan DB, Scialfa CT, Caird JK. Consensus statements on the assessment of older drivers. Can Geriatr J. 2014;17(2):76–81. doi: 10.5770/cgj.17.111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Marshall SC, Man-Son-Hing M. Multiple chronic medical conditions and associated driving risk: a systematic review. Traffic Inj Prev. 2011;12(2):142–148. doi: 10.1080/15389588.2010.551225 [DOI] [PubMed] [Google Scholar]
- 7. Ranchet M, Tant M, Akinwuntan AE, Morgan JC, Devos H. Fitness-to-drive disagreements in individuals with dementia. Gerontologist. 2017;57(5):833–837. doi: 10.1093/geront/gnw119 [DOI] [PubMed] [Google Scholar]
- 8. Chihuri S, Mielenz TJ, DiMaggio CJ, et al. Driving cessation and health outcomes in older adults. J Am Geriatr Soc. 2016;64(2):332–341. doi: 10.1111/jgs.13931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dickerson AE, Molnar L, Bedard M, Eby DW, Classen S, Polgar J. Transportation and aging: an updated research agenda for advancing safe mobility. J Appl Gerontol. 2019;38(12):1643–1660. doi: 10.1177/0733464817739154 [DOI] [PubMed] [Google Scholar]
- 10. Langford J, Fitzharris M, Koppel S, Newstead S. Effectiveness of mandatory license testing for older drivers in reducing crash risk among urban older Australian drivers. Traffic Inj Prev. 2004;5(4):326–335. doi: 10.1080/15389580490509464 [DOI] [PubMed] [Google Scholar]
- 11. Langford J, Bohensky M, Koppel S, Newstead S. Do age-based mandatory assessments reduce older drivers’ risk to other road users? Accid Anal Prev. 2008;40(6):1913–1918. doi: 10.1016/j.aap.2008.08.010 [DOI] [PubMed] [Google Scholar]
- 12. Molnar LJ, Charlton JL, Eby DW. Self-regulation of driving by older adults: comparison of self-report and objective driving data. Transportation 4090. Transp Res Part F Traffic Psychol Behav. 2013;20:29–38. doi: 10.1016/j.trf.2013.05.001 [DOI] [Google Scholar]
- 13. Stiell IG, Clement CM, Brison RJ, et al. A risk scoring system to identify emergency department patients with heart failure at high risk for serious adverse events. Acad Emerg Med. 2013;20(1):17–26. doi: 10.1111/acem.12056 [DOI] [PubMed] [Google Scholar]
- 14. Regev S, Rolison JJ, Moutari S. Crash risk by driver age, gender, and time of day using a new exposure methodology. J Saf Res. 2018;66:131–140. doi: 10.1016/j.jsr.2018.07.002 [DOI] [PubMed] [Google Scholar]
- 15. Emerson JL, Johnson AM, Dawson JD, Uc EY, Anderson SW, Rizzo M. Predictors of driving outcomes in advancing age. Psychol Aging. 2012;27(3):550–559. doi: 10.1037/a0026359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Elvik R. A framework for a critical assessment of the quality of epidemiological studies of driver health and accident risk. Accid Anal Prev. 2011;43(6):2047–2052. doi: 10.1016/j.aap.2011.05.024 [DOI] [PubMed] [Google Scholar]
- 17. Langford J, Koppel S. Epidemiology of older driver crashes—identifying older driver risk factors and exposure patterns. Transportation 4090. Transp Res Part F Traffic Psychol Behav. 2006;9(5):309–321. doi: 10.1016/j.trf.2006.03.005 [DOI] [Google Scholar]
- 18. Marshall SC, Man-Son-Hing M, Charlton J, Molnar LJ, Koppel S, Eby DW. The Candrive/Ozcandrive prospective older driver study: methodology and early study findings. Accid Anal Prev. 2013;61:233–235. doi: 10.1016/j.aap.2013.07.007 [DOI] [PubMed] [Google Scholar]
- 19. California Air Resources Board. Onboard diagnostic II (OBD II) systems fact sheet.https://ww2.arb.ca.gov/resources/fact-sheets/board-diagnostic-ii-obd-ii-systems-fact-sheet. Accessed August 25, 2021.
- 20. Porter MM. An examination of the concordance between self-reported collisions, driver records, and insurance claims in older drivers. J Saf Res. 2018;67:211–215. doi: 10.1016/j.jsr.2018.07.007 [DOI] [PubMed] [Google Scholar]
- 21. Stiell IG, Greenberg GH, Wells GA, et al. Prospective validation of a decision rule for the use of radiography in acute knee injuries. JAMA. 1996;275(8):611–615. doi: 10.1001/jama.1996.03530320035031 [DOI] [PubMed] [Google Scholar]
- 22. Stiell IG, Wells GA. Methodologic standards for the development of clinical decision rules in emergency medicine. Ann Emerg Med. 1999;33(4):437–447. doi: 10.1016/s0196-0644(99)70309-4 [DOI] [PubMed] [Google Scholar]
- 23. Vittinghoff E, McCulloch CE. Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epidemiol. 2007;165(6):710–718. doi: 10.1093/aje/kwk052 [DOI] [PubMed] [Google Scholar]
- 24. Peduzzi P, Concato J, Feinstein AR, Holford TR. Importance of events per independent variable in proportional hazards regression analysis. II. Accuracy and precision of regression estimates. J Clin Epidemiol. 1995;48(12):1503–1510. doi: 10.1016/0895-4356(95)00048-8 [DOI] [PubMed] [Google Scholar]
- 25. Road Safety Policy Office—Vehicles. Ontario Ministry of Transportation. Ontario road safety— annual report 2009.http://www.bv.transports.gouv.qc.ca/per/1022891/17_2009.pdf. Accessed August 24, 2021.
- 26. Hollis AM, Duncanson H, Kapust LR, Xi PM, O’Connor MG. Validity of the Mini-Mental State Examination and the Montreal Cognitive Assessment in the prediction of driving test outcome. J Am Geriatr Soc. 2015;63(5):988–992. doi: 10.1111/jgs.13384 [DOI] [PubMed] [Google Scholar]
- 27. Nasreddine ZS, Phillips NA, Bedirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–699. doi: 10.1111/j.1532-5415.2005.53221.x [DOI] [PubMed] [Google Scholar]
- 28. Loue S, Sajatovic M, eds. Abstract thinking. In: Encyclopedia of Aging and Public Health. Springer Reference. New York: Springer; 2008. [Google Scholar]
- 29. Davies G, Piovesana A. Adult verbal abstract reasoning assessment instruments and their clinimetric properties. Clin Neuropsychol. 2015;29(7):1010–1033. doi: 10.1080/13854046.2015.1119889 [DOI] [PubMed] [Google Scholar]
- 30. Montreal Cognitive Assessment (MoCA). PyschDB.https://www.psychdb.com/cognitive-testing/moca#resources. Accessed March 17, 2022.
- 31. Daigneault G, Joly P, Frigon JY. Executive functions in the evaluation of accident risk of older drivers. J Clin Exp Neuropsychol. 2002;24(2):221–238. doi: 10.1076/jcen.24.2.221.993 [DOI] [PubMed] [Google Scholar]
- 32. Crowe CL, Kannoth S, Andrews H. Associations of frailty status with low-mileage driving and driving cessation in a cohort of older drivers. Geriatr Basel. 2020;5(1):19–29. doi: 10.3390/geriatrics5010019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Albert G, Lotan T, Weiss P, Shiftan Y. The challenge of safe driving among elderly drivers. Heal Technol Lett. 2018;5(1):45–48. doi: 10.1049/htl.2017.0002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Langford J, Methorst R, Hakamies-Blomqvist L. Older drivers do not have a high crash risk—a replication of low mileage bias. Accid Anal Prev. 2006;38(3):574–578. doi: 10.1016/j.aap.2005.12.002 [DOI] [PubMed] [Google Scholar]
- 35. Langford J, Charlton JL, Koppel S, et al. Findings from the Candrive/Ozcandrive study: low mileage older drivers, crash risk and reduced fitness to drive. Accid Anal Prev. 2013;61:304–310. doi: 10.1016/j.aap.2013.02.006 [DOI] [PubMed] [Google Scholar]
- 36. Langford J, Koppel S, McCarthy D, Srinivasan S. In defence of the ‘low-mileage bias.’ Accid Anal Prev. 2008;40(6):1996–1999. doi: 10.1016/j.aap.2008.08.027 [DOI] [PubMed] [Google Scholar]
- 37. Anstey KJ, Eramudugolla R, Huque MH, et al. Validation of brief screening tools to identify impaired driving among older adults in Australia. JAMA Netw Open. 2020;3(6):e208263. doi: 10.1001/jamanetworkopen.2020.8263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Betz ME, Haukoos JS, Schwartz R, et al. Prospective validation of a screening tool to identify older adults in need of a driving evaluation. J Am Geriatr Soc. 2018;66(2):357–363. doi: 10.1111/jgs.15222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Dobbs BM, Schopflocher D. The introduction of a new screening tool for the identification of cognitively impaired medically at-risk drivers: the SIMARD a modification of the DemTect. J Prim Care Community Health. 2010;1(2):119–127. doi: 10.1177/2150131910369156 [DOI] [PubMed] [Google Scholar]
- 40. Gagnon S, Marshall S, Kadulina Y. CIHR Candrive cohort comparison with Canadian household population holding valid driver’s licenses. Can J Aging. 2016;1:99–109. doi: 10.1017/S0714980816000052 [DOI] [PubMed] [Google Scholar]
- 41. College of Occupational Therapists of Ontario. Discretionary reporting of fitness to drive.https://www.coto.org/docs/default-source/default-document-library/guide-to-discretionary-reporting-of-drivers-2018.pdf?sfvrsn=f8d3244e_22. Accessed October 5, 2022.
- 42. Table 2: proportion of people aged 65 and over with a driver’s licence, who drove a vehicle in the previous month and for whom driving was the main form of transportation, by level of functional capacity. 2009. https://www150.statcan.gc.ca/n1/pub/11-008-x/2012001/t/11619/tbl02-eng.htm. Accessed March 16, 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.