Abstract
Background: Regularly informing families of the condition of their relative can be difficult. Text messaging via mobile telephones may achieve such communication effectively.
Objective: To test the hypotheses that we could efficiently deliver real-time short message service (SMS) updates to families and that these SMS updates would be accepted and welcomed.
Design: Prospective observational study.
Participants: Cohort of 91 cardiac surgery patients and 156 family participants.
Intervention: At five distinct landmark events, we sent pre-written SMS updates to designated mobile numbers. We used the sendQuick (TalariaX) mobile messaging platform via the internet in our hospital. To alleviate privacy concerns, all patients were referred to as “your loved one”. The message confirmed the passing of each landmark and directed the families towards the next one. After the patient’s discharge, families were followed up with a telephone call and a five-point Likert scale questionnaire.
Results: We successfully sent all five SMS messages for 72 patients to 114 participants (73%). Among 114 participants, all agreed the SMS service was reassuring and that the SMS messages were easy to follow and kept participants informed. Almost all felt the SMS service did not increase anxiety and all disagreed with the SMS service being intrusive. All surveyed participants stated that they would recommend the service to other families.
Conclusion: We successfully instituted real-time SMS updates. All surveyed participants agreed that these messages were reassuring, informative and easy to follow and that they would recommend the SMS service to other families.
The admission of a critically ill patient to an intensive care unit (ICU) has been reported as an exceptionally distressing event for both the patient and their family.1,2 This anxiety is often displayed in an intense need for information and emotional support.3 Families want truthful and consistent information that is delivered frequently in an understandable way throughout the ICU admission.1 It is often impossible for family members to be continuously at the bedside or be readily available to speak to doctors during or after their ward rounds. Moreover, in our experience and in their own words, families are reluctant to call and “harass” the nurses. Recommended interventions that address family needs include handouts or brochures and the use of structured communication programs for family members of patients in the ICU.2
Mobile telephone text messaging, or short message service (SMS), has been widely used as a communication tool in health care for appointment attendance,4 adherence to medication,5, 6 and communicating results of medical investigations.7 In 2004, a Singaporean newspaper reported that ICU doctors at the National University Hospital used SMS to update families after their morning ward round.8 In 2016, Globus and colleagues9 reported on a trial from their neonatal ICU. A single automated SMS was sent to the patient’s parents daily at 9.00 am with information that included crib position, the neonate’s weight and whether medical procedures had been performed. SMS messaging, however, has never yet been utilised as a real-time continuous communication method between an ICU and patients’ families. We reasoned that sending timely SMS messages to the families of selected critically ill patients at specific landmark events during that patient’s stay may be reassuring and be viewed positively by family members. The aim of this study was to test two key hypotheses: first, that we could efficiently deliver real-time SMS updates to families during their family member’s stay in ICU, and second, that these SMS updates would be accepted and welcomed by these families.
Methods
This study was approved by the Human Research Ethics Committee of our institution (ethics approval reference: QA2017168).
We selected a cohort of post-operative elective cardiac surgical patients as our trial group because this choice allowed us to, firstly, select five distinct landmark events and, secondly, to meet the patient and family in the preadmission clinic and obtain consent from the patient to send and the family (participant) to receive SMS updates.
We pre-wrote an SMS message pertaining to each landmark and we asked for mobile numbers to which we could send the messages. Patients and families were given an information sheet with explicit details as to the format and timing of the SMS messages. These messages were delivered in addition to our normal process of updating the families in person every day, as visiting time is unrestricted in our unit. Our protocol was to send the SMS regardless of family updates at the bedside. Staff would not know whether the family member at the bedside was a trial participant or not.
Moreover, we would only send an SMS if the patient proceeded through their post-operative stay without significant adverse events. If anything untoward occurred, we planned to cease SMS messaging and continue communication with the family in person with verbal updates.
Technology and messaging
Our cardiac surgical patients are nursed 1:1. Each bedspace has an internet-enabled computer. We used the sendQuick (TalariaX; www.talariax.com) mobile messaging platform, available on every computer via the internet in our hospital. To alleviate concerns regarding patient privacy and the sending of patient identifiable data, all patients were referred to as “your loved one” without any further information as to gender, age or operation performed. The five pre-written messages were stored within the sendQuick platform to be sent at the following clinical landmarks:
-
•
ICU admission;
-
•
extubation;
-
•
morning ward round;
-
•
decision to discharge; and
-
•
discharge from the ICU.
The ICU admission and extubation usually occur on the day of surgery. Sometimes the extubation occurs overnight or in the morning of the first post-operative day. Our morning ward round is at 7.30 am on the day after surgery. The decision to discharge and the discharge from ICU usually follows that first post-operative day. Under these circumstances, the five SMS messages were sent within a 24-hour period. Via a general login, the nursing and ward clerk staff selected the pertinent SMS to send for each landmark event from a drop-down menu. The staff entered the telephone numbers on each occasion. If in those patients with two or three associated participants a mobile number was mistakenly left out, that participant did not receive the SMS, even though it was sent to the other family members.
Each SMS message had a short introduction: “Hello from the ICU”. The message then confirmed the passing of each landmark and directed the families towards the next one. Each message concluded with the offer to call us if there were any concerns and the offer to opt out should the family SMS recipient or participant not wish to receive further texts (Online Appendix).
After the patient’s discharge, families were followed up with a telephone call and a five-point Likert scale questionnaire. Families were also given the opportunity to provide open feedback on their experience of the SMS. The questions posed were to ascertain how the participants perceived the SMS service:
-
•
I felt reassured by the SMS service.
-
•
The SMS were easy to follow.
-
•
The SMS kept me informed.
-
•
The SMS service made me feel anxious.
-
•
The SMS were intrusive.
-
•
I would recommend the SMS service to other families.
For each statement, the Likert scale ranged from strongly agree to strongly disagree. We noted whether the participant was happy to provide free feedback — positive, negative or other — and documented all feedback given.
Results
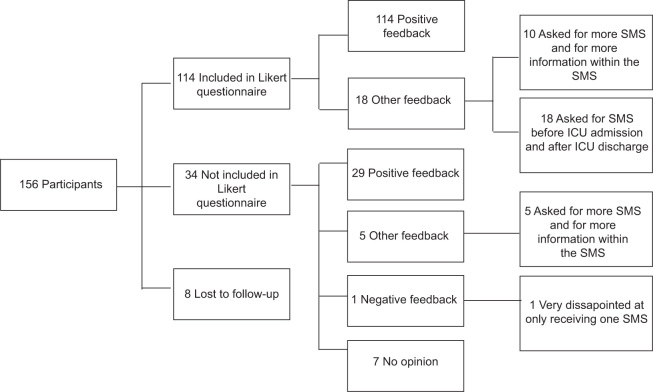
Over a 6-month period, we recruited 91 patients and 156 family participants. No participant asked to opt out of the SMS service. We did not have to cease SMS messaging for any significant untoward event. We asked for up to two participants to be designated for each patient. One patient asked for SMS messages to be sent to three family members (Figure 1). We successfully sent all five SMS messages for 72 patients to 114 participants (73%). We did not send all five SMS messages to 34 participants (22%) and eight participants (5%) were lost to follow-up (Figure 2).
Figure 1.
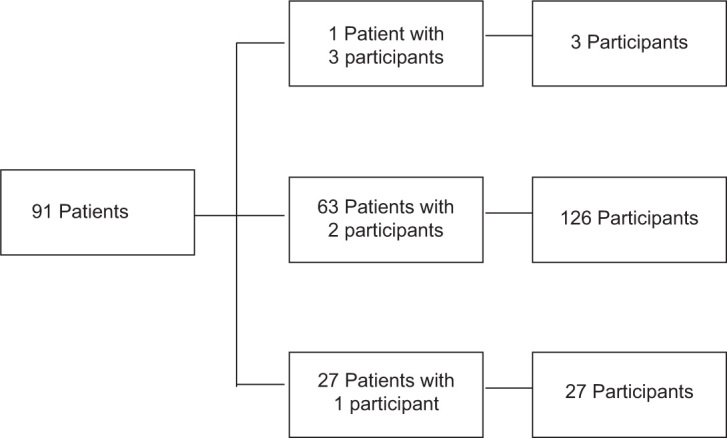
Patients and participants
Figure 2.
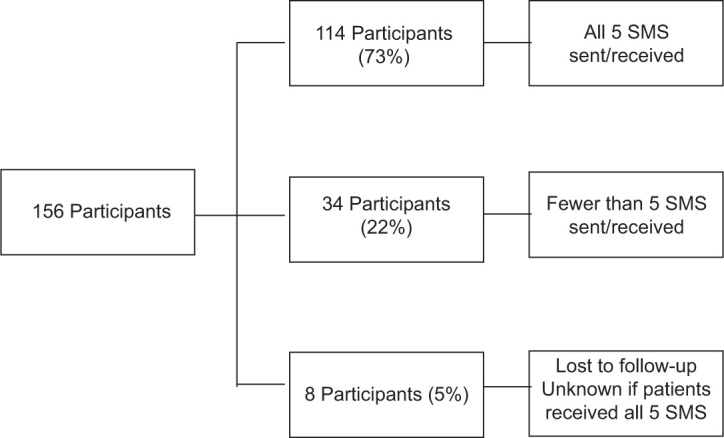
Short message service (SMS) sent/received per participant
The average number of not sent SMS was two (range, 1–5). The most common reasons for such missing SMS transmission was staff being unaware of the trial, the trial paperwork was missing from the workstation, or staff members were too busy to send the messages. Input error was the next major cause of missing SMS. In one instance, we were accidently entering a landline telephone number. This participant did not receive those SMS. A sendQuick system error is always a possibility but appears unlikely. Input errors occurred in 12 out of 34 instances. In another three out of 34 instances, the SMS were not sent, in breach of protocol, as the patient’s relatives were or had been present (Table 1). Most patients had more than one participant; some patients fit into more than one category.
Table 1.
Reason for failure to deliver the short message service (SMS)
| Number of participants | Reason for missing SMS | Examples of reasons |
|---|---|---|
| 21/34 | SMS not sent |
|
| 12/34 | Input error |
|
| 3/34 | Staff decision not to send SMS |
|
Participant follow-up
We aimed to follow up all participants after the patient’s discharge from the ICU. All participants were asked for open feedback about how they perceived the SMS messages. In doing this, we identified the 12/34 patients in the input error group who did not receive the five SMS messages although we believed we had successfully sent them. Therefore, we followed up 148 participants (95%) — eight participants (5%) were uncontactable and lost to follow-up. Only participants who received all five SMS were included in the Likert questionnaire but all participants, even those who received fewer than five SMS messages (only a partial dose) were asked for their open feedback.
Findings of the questionnaire
The Likert questionnaire included 114 participants. All of the surveyed participants agreed the SMS service was reassuring and that the SMS messages were easy to follow and kept the participant informed. Almost 100% felt the service did not increase anxiety and 100% disagreed with the sentiment the SMS service was intrusive. All of the included participants stated that they would recommend the service to other families (Table 2).
Table 2.
Results of Likert scale questionnaire in 144 participants
| Trial results: Likert scale questionnaire |
|||||
|---|---|---|---|---|---|
| Strongly agree | Agree | Neither agree nor disagree | Disagree | Strongly disagree | |
| I felt reassured by the SMS service | 67 (59%) | 47 (41%) | 0 | 0 | 0 |
| The SMS were easy to follow | 68 (60%) | 46 (40%) | 0 | 0 | 0 |
| The SMS kept me informed | 69 (61%) | 43 (39%) | 0 | 0 | 0 |
| The SMS service made me feel anxious | 0 | 0 | 1 (1%) | 82 (72%) | 31 (27%) |
| The SMS were intrusive | 0 | 0 | 0 | 83 (73%) | 31 (27%) |
| I would recommend the SMS service to other families | 112 (98%) | 2 (2%) | 0 | 0 | 0 |
SMS = short message service.
Open feedback
We contacted 148 participants (95%). We were explicit in our request for positive, negative or other feedback. All of 114 participants who received all five SMS provided positive feedback. Eighteen of them provided other feedback: requests for more frequent SMS and for more information within these SMS (Figure 3).
Figure 3.
Participants’ open feedback
Thirty-four participants did not receive all five SMS. In this group, 29 participants provided positive feedback. Five participants provided other feedback, such as requests for more SMS and for more information within these SMS. One participant was very disappointed they had only received one SMS while the other family member received all five SMS (we mistakenly tried to send the SMS to a landline), and seven offered no opinion. Participants who received three or more SMS felt positive about the experience. The eight participants reporting disappointment or offering no opinion received three SMS messages or fewer (average, 1–2).
Discussion
In a prospective observational study, we tested an SMS platform to store and send an ongoing thread of five SMS messages as continuing updates on a patient’s post-operative recovery to the majority of consenting families. In keeping with our hypotheses, we found that we could efficiently deliver real-time SMS updates to families during their family member’s stay in the ICU and that these SMS updates were accepted and welcomed by these families. In particular, we received overwhelmingly positive responses to the structured follow-up questionnaire and in the open feedback option.
Relationship to previous studies
A 2016 systematic review highlighted a significant gap of studies that investigate the effectiveness of interventions to meet the family needs of critically ill patients admitted to an adult ICU. It recommended future research studies should focus on the use of technology to meet family information needs with a view to determining whether these interventions would decrease family anxiety and improve hope and uncertainty while the patient is in the ICU.2 Our study expands on this very effectively by providing data on the use of SMS messaging to communicate with patients’ families with the simple notion of reducing anxiety by providing contemporaneous information and engagement from the ICU.
Implications of study findings
Our study implies that an SMS system can be set up to deliver structured messages at key landmark events to family members of cardiac surgery patients. Moreover, it implies that most family members valued receiving the SMS. Finally, it implies that such consumer-focused approach to the care of a specific cohort of patients provides great value at minimum cost.
Strengths and limitations
Our study has several strengths. We had ethics approval for this trial, all patients and participants provided consent, and we had a high adherence to protocol. The results are clear that the participants perceived the SMS service very favourably, with open feedback indicating that family members were impressed with and thankful for the messages. The positive feedback frequently reported that participants felt valued and important and they appreciated the effort of the ICU staff to proactively reach out to families and keep them informed. Many felt relieved of the stress of having to call in to speak to the bedside nurses. A number of participants with larger families simply forwarded the message on as a group text. Another common theme in the open feedback was from the patients’ distant and working families. Participants from distant towns (250–500 km away) and across the Bass Straight in Tasmania who were not able visit the unit were very thankful for the updates. One participant received our SMS messages while away in Denmark. Family members who were unable to take time off from work were another group that uniformly gave positive feedback. Interestingly, most participants who had only received a partial dose of the SMS protocol (fewer than five messages) did not report a higher level of anxiety at not having received the SMS as expected. In general, participants who had received three or more SMS were just as positive in their open feedback as the participants who had received all five SMS.
Our intervention has some limitations. Some participants wished for more frequent SMS and for more information in the SMS, such as little reassuring messages: “had a good night”, “sitting in a chair”, “going for a walk”. One participant asked if we could include photographs of the patient in the SMS. Other participants complained that they did not receive messages before the patient’s admission to the ICU or after their discharge. The participants would have liked a message to inform them of the beginning of surgery or if any delay had occurred during surgery. Others felt disappointed at the cessation of the SMS service once the patient had left the ICU. They would have liked further updates: “you could write a daily update from the ward to keep the next of kin fully updated”. These limitations could not be avoided. In this trial, the SMS messages were limited to the patients’ stay in the ICU. Furthermore, current recommendations advise on limiting the risk of sensitive information being available and as such we pre-wrote SMS messages to minimise this risk. The potential for structured communication via SMS messaging is endless. Future developments and trials may allow for more personalised messages and photographs being sent to patients’ families. Other trials may combine the recommended leaflets and brochures on ICU care and SMS messaging to better inform and reassure families of critically ill patients.
This was not a randomised controlled trial, but rather a pilot feasibility and social efficacy study. Thus, we could not test what the family members’ opinions of a non-SMS approach were. However, the responses received and the requests for more SMS messages support the view that this service may represent a significant improvement from the point of view of consumers.
Conclusion
We successfully instituted real-time SMS updates on a patient’s journey through the ICU to their family in a cohort of cardiac surgery patients. The family’s responses were overwhelmingly positive. All family members surveyed after receiving these messages agreed that the SMS were reassuring, informative and easy to follow. They all reported that they would recommend the SMS service to other families. In the open feedback section, the families noted that they felt valued and important and they appreciated our unit reaching out to them. Family members who were unable to be at their relative’s bedside were most grateful for the service.
Competing interests
None declared.
References
- 1.Kynoch K., Cabilan C.J., McArdle A. Experiences and needs of families with a relative admitted to an adult intensive care unit: a qualitative systematic review protocol. JBI Database System Rev Implement Rep. 2016;14:83–90. doi: 10.11124/JBISRIR-2016-003193. [DOI] [PubMed] [Google Scholar]
- 2.Kynoch K., Chang A., Coyer F., McArdle A. The effectiveness of interventions to meet family needs of critically ill patients in an adult intensive care unit: a systematic review update. JBI Database System Rev Implement Rep. 2016;14:181–234. doi: 10.11124/JBISRIR-2016-2477. [DOI] [PubMed] [Google Scholar]
- 3.Keenan A., Joseph L. The needs of family members of severe traumatic brain injured patients during critical and acute care: a qualitative study. Can J Neurosci Nurs. 2010;32:25–35. [PubMed] [Google Scholar]
- 4.Gurol-Urganci I., de Jongh T., Vodopivec-Jamsek V., et al. Mobile phone messaging reminders for attendance at healthcare appointments. Cochrane Database Syst Rev. 2013;(12):CD0077458. doi: 10.1002/14651858.CD007458.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Strandbygaard U., Thomsen S.F., Backer V. A daily SMS reminder increases adherence to asthma treatment: a three-month follow-up study. Respir Med. 2010;104:166–171. doi: 10.1016/j.rmed.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 6.Hou M.Y., Hurwitz S., Kavanagh E., et al. Using daily text-message reminders to improve adherence with oral contraceptives: a randomized controlled trial. Obstet Gynecol. 2010;116:633–640. doi: 10.1097/AOG.0b013e3181eb6b0f. [DOI] [PubMed] [Google Scholar]
- 7.Gurol-Urganci I., de Jongh T., Vodopivec-Jamsek V., et al. Mobile phone messaging for communicating results of medical investigations. Cochrane Database Syst Rev. 2012;(6):CD0077456. doi: 10.1002/14651858.CD007456.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hospitals send SMS updates on patients to relativesThe Star. 2004 https://www.thestar.com.my/news/regional/2004/06/15/hospitals-send-sms-updates-on-patients-to-relatives/ 14 June. (viewed June 2020) [Google Scholar]
- 9.Globus O., Leibovitch L., Maayan-Metzger A., et al. The use of short messages (SMS) to provide medical updating to parents in the NICU. J Perinatol. 2016;36:739–743. doi: 10.1038/jp.2016.83. [DOI] [PubMed] [Google Scholar]