Abstract
Objectives: To evaluate the epidemiology of rapid response team (RRT) reviews that led to intensive care unit (ICU) admissions, and to evaluate the frequency of in-hospital cardiac arrests (IHCAs) among ICU patients with confirmed coronavirus disease 2019 (COVID-19) in Australia.
Design: Multicentre, retrospective cohort study.
Setting: 48 public and private ICUs in Australia.
Participants: All adults (aged ≥ 16 years) with confirmed COVID-19 admitted to participating ICUs between 25 January and 31 October 2020, as part of SPRINT-SARI (Short PeRiod IncideNce sTudy of Severe Acute Respiratory Infection) Australia, which were linked with ICUs contributing to the Australian and New Zealand Intensive Care Society Adult Patient Database (ANZICS APD).
Main outcome measures and results: Of the 413 critically ill patients with COVID-19 who were analysed, 48.2% (199/413) were admitted from the ward and 30.5% (126/413) were admitted to the ICU following an RRT review. Patients admitted following an RRT review had higher Acute Physiology and Chronic Health Evaluation (APACHE) scores, fewer days from symptom onset to hospitalisation (median, 5.4 [interquartile range (IQR), 3.2–7.6] v 7.1 days [IQR, 4.1–9.8]; P < 0.001) and longer hospitalisations (median, 18 [IQR, 11–33] v 13 days [IQR, 7–24]; P < 0.001) compared with those not admitted via an RRT review. Admissions following RRT review comprised 60.3% (120/199) of all ward-based admissions. Overall, IHCA occurred in 1.9% (8/413) of ICU patients with COVID-19, and most IHCAs (6/8, 75%) occurred during ICU admission. There were no differences in IHCA rates or in ICU or hospital mortality rates based on whether a patient had a prior RRT review or not.
Conclusions: This study found that RRT reviews were a common way for deteriorating ward patients with COVID-19 to be admitted to the ICU, and that IHCA was rare among ICU patients with COVID-19.
The coronavirus disease 2019 (COVID-19) pandemic has been associated with more than 433 million cases and over 5.9 million deaths worldwide, as of 6 March 2022.1 While most patients experience mild disease, critically ill patients often have significant complications, including malignant arrhythmias and severe hypoxia, leading to cardiac arrest.2 Initial studies from Wuhan, China,3 and later the United States4 reported a large number of in-hospital cardiac arrests (IHCAs) in patients with COVID-19 pneumonia, with a high associated case fatality rate.3,4 Recent cross-sectional studies5,6 and two systematic reviews revealed overall mortality rates between 89.9% and 91.7%7,8 among patients with COVID-19 experiencing IHCA.
The Australian experience of the COVID-19 pandemic in 2020 has differed vastly to that internationally,9 with a reported mortality rate considerably lower than in other parts of the world.1 However, in critically ill patients with COVID-19 in Australia, the incidence of IHCA is unknown. Moreover, the proportion of this cohort admitted to the intensive care unit (ICU) after review by a rapid response team (RRT) remains unclear. Australian hospitals have well established RRTs, which are a common mode of admission to the ICU from the ward,10 and have demonstrated reductions in IHCAs in the non-COVID-19 era.11, 12, 13
In this study, we evaluated the epidemiology of RRT reviews that led to ICU admission in patients with COVID-19. Furthermore, we evaluated the frequency of IHCA among patients admitted to the ICU, based on prior RRT review. In the context of mature rapid response systems, we hypothesise that RRT reviews would be a common way for deteriorating ward patients with COVID-19 to be admitted to the ICU, and that the rates of IHCA in these patients in ICU might be lower than that reported internationally.
Methods
Ethics approval
The Alfred Hospital Human Research Ethics Committee in Melbourne, Australia, approved this study (project No.798/20), with a waiver of informed consent. Access to the Australian and New Zealand Intensive Care Society (ANZICS) Adult Patient Database (APD) was granted by the ANZICS Centre for Outcome and Resource Evaluation (CORE) Management Committee in accordance with standard protocols.
Study design
We conducted a retrospective multicentre observational study of ICU admissions of patients with COVID-19 in Australia between 25 January 2020 and 31 October 2020. Forty-eight public and private ICUs in Australia contributed data to the ANZICS APD and SPRINT-SARI (Short PeRiod IncideNce sTudy of Severe Acute Respiratory Infection) databases.
Changes to RRTs in Australia during the COVID-19 pandemic
All sites contributing to this study had an RRT as part of mandatory requirements linked to hospital accreditation.14 Local responses to COVID-19-related deterioration were developed by hospitals using available evidence and regional and national guidance.15 ANZICS convened forums for sharing information related to RRTs based on international recommendations.16,17 To cope with the expected demand for extra beds, progressive reductions in elective surgeries were implemented in some jurisdictions during the peak phases of the pandemic. Meetings were encouraged in each hospital to improve interactions between ward and ICU clinicians to enhance earlier identification of patients with suspected or confirmed COVID-19.
Source of data
SPRINT-SARI is a multicentre, prospective, observational study of patients with COVID-19 admitted to participating ICUs in Australia. Details concerning the study design, partners, and data collection have been published elsewhere.18 Patients aged ≥ 16 years with a confirmed positive polymerase chain reaction (PCR) test for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) who were admitted to a participating ICU were included. Biological samples for PCR testing could be obtained from the nasopharynx, trachea, or lower airways via bronchoscopy. Research staff at each ICU screened all admissions for patients with COVID-19. Deidentified data were submitted by participating sites using a standardised case report form via REDCap (Vanderbilt University). The study was coordinated by the Australian and New Zealand Intensive Care Research Centre (ANZIC-RC), Monash University.
Data from SPRINT-SARI Australia was complemented by data from the ANZICS APD via data linkage, with probabilistic methods using eight de-identified variables including hospital, age (in years), sex, vital status at discharge, and hospital and ICU admission and discharge dates. Matching was carried out over 17 stages. After initially matching identically on all eight variables, matching criteria for dates and ages were gradually loosened to allow a discrepancy of ± 2 days (for dates) or years (for ages). If a pair of records was matched in stage 1 with tight criteria, it would also be matched when the criteria were loosened. However, as linking was sequential, any patient who was matched in stage 1 was then excluded from matching in stage 2.
The ANZICS APD contains routine quality assurance and benchmarking data collected by ANZICS CORE. This database prospectively collects de-identified patient data, including admission diagnosis, chronic health status, and physiological and biochemical variables within the first 24 hours of admission. This allows calculation of Acute Physiology and Chronic Health Evaluation (APACHE) II and III illness severity scores, Australian and New Zealand Risk of Death (ANZROD), and ICU and hospital outcomes. This database also records whether the ICU admission was associated with an RRT review. However, clinical and physiological data at the time of RRT review are not routinely recorded in the ANZICS APD.
Data extraction
Data extracted from the SPRINT-SARI Australia database included duration of symptoms before hospitalisation, treatment and organ support administered, and complications (including IHCA) occurring during the hospital stay. Demographic information, APACHE scores, source of ICU admission, and date and time of hospital and ICU admission and discharge were extracted from the ANZICS APD. In addition, ICU and hospital mortality, length of ICU and hospital stays, and discharge destinations were recorded. The presence of a prior RRT review was determined from review of the ANZICS APD data. Patients were excluded where no data were available concerning RRT activation before ICU admission.
Study outcomes
The study aim was to evaluate the baseline characteristics and outcomes of patients admitted to the ICU with COVID-19 based on a prior RRT review. The primary outcome was the proportion of COVID-19 ICU admissions that occurred following an RRT call. The secondary outcomes included clinically relevant outcomes (ICU and hospital length of stay, and ICU and hospital mortality), and differences in interventions provided and complications observed based on a prior RRT review. Finally, we also explored the occurrence of an IHCA at any time before hospital discharge in patients with COVID-19 requiring ICU admission.
Sensitivity analysis
Given that a large proportion of admissions to the ICU comes from the emergency department (ED), where RRT reviews are uncommon in Australia, we performed a sensitivity analysis investigating patients admitted from the ward only.
Statistical analysis
Based on a projected ratio of 2:1, with a minimum of 100 RRT cases, this study will have > 80% power (two-sided P value of 0.05) to detect a difference in proportion of 17%. Between dichotomised categories, continuous normally distributed variables were compared using Wilcoxon ranksum tests and reported as median (interquartile range [IQR]). Categorical data were compared using Fisher exact tests and reported as n (%). Time until ICU admission, from hospitalisation, was shown in cumulative distribution plots. A two-sided P < 0.05 was considered statistically significant and all analyses were conducted in R v.4.0.3.
Results
Participants
There were 423 COVID-19 admissions to the ICU, which could be identified from linking the SPRINT-SARI Australia database and the ANZICS APD, across 48 ICUs from a total of 2492 COVID-19 admissions to hospital in Victoria during the study period.19 As most COVID-19 cases and hospitalisations occurred in Victoria during the second wave,19 these numbers closely approximate Australian hospitalisations of patients with COVID-19. After excluding ten patients with missing data, 413 COVID-19 patients were included in the final analysis. The baseline characteristics, comorbid conditions and vital signs for ICU admissions are presented in Table 1. The median age was 61 years (IQR, 50-70 years) and 64.2% (265/413) were male. Common comorbid conditions included diabetes mellitus (29.2%, 117/402), obesity (28%, 110/393) and chronic cardiac failure (14.7%, 58/395). The ICU admission source was predominantly from the ward (48.2%, 199/413) and the ED (42.1%, 174/413). Patients with COVID-19 admitted to the ICU had a significant disturbance in respiratory physiology, as evidenced by tachypnoea (median respiratory rate, 30 min-1), high fraction of inspired oxygen (FiO2) requirement (median, 0.5), and low arterial partial pressure of oxygen (PaO2) to FiO2 ratio (median, 134 mmHg).
Table 1.
Baseline characteristics of patients admitted to the intensive care unit (ICU) with coronavirus disease 2019 (COVID-19)
| Characteristic | Overall | RRT call | No RRT call | P |
|---|---|---|---|---|
| Total number of patients | 413 | 126 | 287 | |
| Age, years, median (IQR) | 61 (50-70) | 62 (54-71) | 60 (48-70) | 0.07 |
| < 60 | 196 (47.5) | 53 (42.1) | 143 (49.8) | |
| 60-69 | 103 (24.9) | 35 (27.8) | 68 (23.7) | |
| 70-79 | 94 (22.8) | 32 (25.4) | 62 (21.6) | 0.51 |
| > 80 | 20 (4.8) | 6 (4.8) | 14 (4.9) | |
| Sex, male | 265 (64.2%) | 88 (69.8%) | 177 (61.7%) | 0.12 |
| APACHE II score, median (IRQ) | 15 (10-19) | 15 (11-20) | 14 (9-19) | 0.042 |
| ANZROD, %, mean (SD) | 10.4% (14.7%) | 12.7% (16.2%) | 9.4% (13.9%) | 0.030 |
| Hours between hospital and ICU admission, median (IQR) | 8.8 (2.1-52.3) | 60.5 (33.6-105.6) | 4.0 (0.9-17.0) | < 0.001 |
| Days between symptoms and hospital admission, median (IRQ) | 6.5 (3.9-9.2) | 5.4 (3.2-7.6) | 7.1 (4.1-9.8) | < 0.001 |
| Days between symptoms and ICU admission, median (IQR) | 8.2 (5.4-10.9) | 8.4 (5.6-10.8) | 7.7 (5.3-11.0) | 0.32 |
| Treatment limitation orders | 28 (6.8%) | 5 (4.0%) | 23 (8.0%) | 0.20 |
| Body mass index, kg/m2, median (IQR) | 29.8 (25.7-35.2) | 29.9 (25.7-33.8) | 29.7 (25.7-35.7) | 0.57 |
| Clinical frailty score, mean (SD) | 2.7 (1.2) | 2.9 (1.2) | 2.6(1.3) | 0.07 |
| Cardiac arrest in the previous 24 h | 2/401 (0.5%) | 1/122 (0.8%) | 1/279 (0.4%) | 0.52 |
| ICU source of admission | < 0.001 | |||
| Operating room | 3 (0.7%) | 0 (0.0%) | 3 (1.0%) | |
| Emergency department | 174 (42.1%) | 5 (4.0%) | 169 (58.9%) | |
| Ward | 199 (48.2%) | 120 (95.2%) | 79 (27.5%) | |
| Other hospital | 26 (6.3%) | 0 (0.0%) | 26 (9.1%) | |
| Home | 11 (2.7%) | 0 (0.0%) | 11 (3.8%) | |
| Coexisting disorders | ||||
| Diabetes mellitus | 117/401 (29.2%) | 38/121 (31.4%) | 79/280 (28.2%) | 0.55 |
| Obesity | 110/393 (28.0%) | 25/120 (20.8%) | 85/273 (31.1%) | 0.039 |
| Use of ACEI or ARB | 81/391 (20.7%) | 28/121 (23.1%) | 53/270 (19.6%) | 0.42 |
| Chronic cardiac failure | 58/395 (14.7%) | 16/121 (13.2%) | 42/274 (15.3%) | 0.65 |
| Smoker | 50/386 (13.0%) | 21/117 (17.9%) | 29/269 (10.8%) | 0.07 |
| Chronic pulmonary disease* | 33/393 (8.4%) | 9/119 (7.6%) | 24/274 (8.8%) | 0.84 |
| Asthma | 56/394 (14.2%) | 19/120 (15.8%) | 37/274 (13.5%) | 0.53 |
| Immunosuppression | 31/393 (7.9%) | 11/120 (9.2%) | 20/273 (7.3%) | 0.55 |
| Vital signs within first 24 h of ICU admission† median (IQR) | ||||
| Heart rate, beats/min | 100 (86-111) | 100 (89-110) | 100 (86-112) | 0.88 |
| Respiratory rate, breaths/min | 30 (24-37) | 28 (23-34) | 30 (24-38) | 0.004 |
| Mean arterial pressure, mmHg | 80 (70-94) | 82 (72-94) | 80 (69-94) | 0.48 |
| Temperature, °C | 38.3 (37.4-38.9) | 38.5 (37.7-39.1) | 38.1 (37.3-38.8) | 0.004 |
| SpO2, % | 92 (88-95) | 92 (88-94) | 92 (88-95) | 0.54 |
| Laboratory test in the first 24 hours, median (IQR) | ||||
| PaO2/FiO2, mmHg | 134 (98-205) | 134 (102-187) | 134 (97-209) | 0.69 |
| FiO2 | 0.50 (0.30-0.60) | 0.50 (0.40-0.60) | 0.45 (0.30-0.60) | 0.23 |
| pH | 7.43 (7.37-7.47) | 7.43 (7.37-7.47) | 7.42 (7.37-7.46) | 0.22 |
ACEI = angiotensin-converting enzyme inhibitor; APACHE = Acute Physiology and Chronic Health Evaluation; ARB = angiotensin II receptor blocker; FiO2 = fraction of inspired oxygen; IQR = interquartile range; PaO2 = arterial partial pressure of oxygen; RRT = rapid response team; SD = standard deviation; SpO2 = oxygen saturation measured by pulse oximetry. Percentages may not total 100 because of rounding. Where the denominator does not match the total number of patients at the head of the table, this is due to missing data.
Not considering asthma.
Vital signs are the worst available data within 24 hours of hospital admission (highest heart rate, respiratory rate and temperature, and lowest mean arterial pressure)
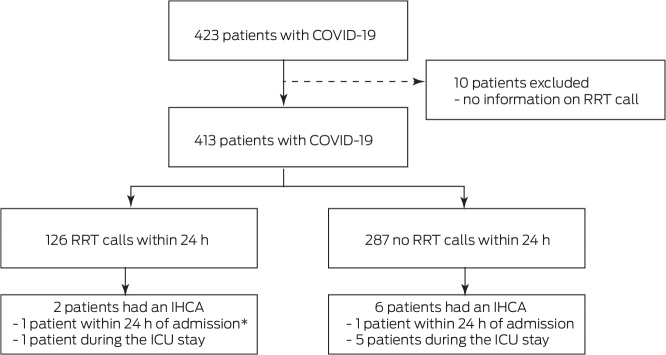
Primary outcome
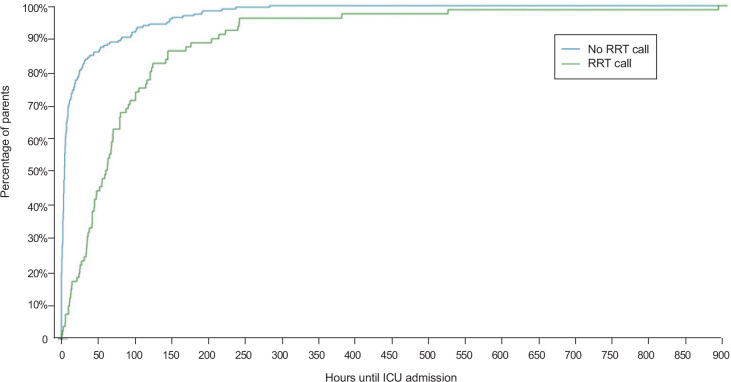
Overall, 30.5% (126/413) of patients were admitted to the ICU following an RRT review (Figure 1), comprising 60.3% (120/199) of all ward-based admissions. There were some notable differences in the baseline characteristics among patients admitted to the ICU after an RRT review compared with those who were not (Table 1). RRT review patients had higher APACHE and ANZROD scores and a shorter time from symptom onset to hospitalisation (median, 5.4 [IQR, 3.2-7.6] v 7.1 days [IQR, 4.1-9.8]; P < 0.001). In addition, RRT review patients also had a longer time between hospitalisation and ICU admission (median, 60.5 [IQR, 33.6-105.6] v 4.0 hours [IQR, 0.9-17.0]; P < 0.001) (Figure 2), as 97.1% (169/174) of non-RRT-related admissions were done directly from the ED (P < 0.001). In addition, based on the worst vital signs in the first 24 hours of ICU stay, the patients admitted after an RRT review had a higher median temperature (median, 38.5°C [IQR, 37.7-39.1] v 38.1°C [IQR, 37.3-38.8]; P = 0.004) but a lower respiratory rate (median, 28 min-1 [IQR, 23-34] v 30 min-1 [IQR, 24-38]; P = 0.004), and were less likely to be obese (31.1% [85/273] v 20.8% [25/120]; P = 0.04) than patients without a prior RRT review. Treatment limitations were present in 6.8% (n = 28) of patients and were similar in both groups.
Figure 1.
Flow diagram of the eligible study cohort from the Australian and New Zealand Intensive Care Society Adult Patient Database between 25 January and 31 October 2020
ICU = intensive care unit; IHCA = in-hospital cardiac arrest; RRT = rapid response team. * This IHCA occurred in the emergency department setting, and the patient had an RRT review, which is likely related to the rapid response system set-up of that particular hospital.
Figure 2.
Hours until intensive care unit (ICU) admission based on prior rapid response team (RRT) review
Secondary outcomes
Interventions, organ support, and development of complications based on prior RRT review
There were no significant differences in drug prescriptions for patients between the groups (Table 2). A greater proportion of patients in the RRT group received high flow nasal oxygen (72% [85/118] v 55% [154/280]; P = 0.002) and renal replacement therapy (15.3% [18/118] v 7.9% [22/277]; P = 0.04), and were more likely to develop bacterial pneumonia (25.7% [29/113] v 15.5% [41/264]; P = 0.03) during their ICU stay. There were no differences in the provision of invasive or non-invasive ventilation or rescue therapies (prone positioning, inhaled nitric oxide, and extracorporeal membrane oxygenation) between the groups. Although arrhythmia (14.4%), venous thromboembolic disease (10.8%), bacteraemia (10.7%) and myocarditis (9.9%) were common, they were similar between the groups.
Table 2.
Interventions and complications of patients admitted to the intensive care unit (ICU) with coronavirus disease 2019 (COVID-19)
| Interventions and complications | Overall | RRT call | No RRT call | P |
|---|---|---|---|---|
| Total number of patients | 413 | 126 | 287 | |
| Drugs | ||||
| Antibiotics | 356/394 (90.4%) | 112/118 (94.9%) | 244/276 (88.4%) | 0.06 |
| Steroids | 257/397 (64.7%) | 83/120 (69.2%) | 174/277 (62.8%) | 0.25 |
| Hydroxychloroquine | 33/395 (8.4%) | 13/120 (10.8%) | 20/275 (7.3%) | 0.24 |
| Oseltamivir | 1/396 (0.3%) | 0/120 (0.0%) | 1/276 (0.4%) | 0.99 |
| Lopinavir-ritonavir | 11/396 (2.8%) | 2/120 (1.7%) | 9/276 (3.3%) | 0.52 |
| Remdesivir | 121 (29.3%) | 43/126 (34.1%) | 78/287 (27.2%) | 0.16 |
| Organ support* | ||||
| High flow nasal oxygen | 239/398 (60.1%) | 85/118 (72.0%) | 154/280 (55.0%) | 0.002 |
| Non-invasive ventilation | 46/394 (11.7%) | 13/117 (11.1%) | 33/277 (11.9%) | 0.87 |
| Mechanical ventilation | 218/407 (53.6%) | 74/124 (59.7%) | 144/283 (50.9%) | 0.11 |
| Inotropic or vasopressor | 201/394 (51.0%) | 66/117 (56.4%) | 135/277 (48.7%) | 0.19 |
| Neuromuscular blocking agent | 157/395 (39.7%) | 53/118 (44.9%) | 104/277 (37.5%) | 0.18 |
| Prone positioning | 140/395 (35.4%) | 50/118 (42.4%) | 90/277 (32.5%) | 0.07 |
| Renal replacement therapy | 40/395 (10.1%) | 18/118 (15.3%) | 22/277 (7.9%) | 0.043 |
| Other cardiac procedures | 19/395 (4.8%) | 6/118 (5.1%) | 13/277 (4.7%) | 0.80 |
| Tracheostomy | 31/394 (7.9%) | 5/118 (4.2%) | 26/276 (9.4%) | 0.10 |
| Inhaled nitric oxide | 23/395 (5.8%) | 10/118 (8.5%) | 13/277 (4.7%) | 0.16 |
| ECMO | 9/395 (2.3%) | 3/118 (2.5%) | 6/277 (2.2%) | 0.73 |
| Complications during hospital stay | ||||
| Viral pneumonitis | 251/387 (64.9%) | 71/116 (61.2%) | 180/271 (66.4%) | 0.35 |
| Bacterial pneumonia | 70/377 (18.6%) | 29/113 (25.7%) | 41/264 (15.5%) | 0.029 |
| Bacteraemia | 41/383 (10.7%) | 13/114 (11.4%) | 28/269 (10.4%) | 0.86 |
| Stroke | 3/388 (0.8%) | 2/117 (1.7%) | 1/271 (0.4%) | 0.22 |
| Arrhythmia | 56/388 (14.4%) | 22/117 (18.8%) | 34/271 (12.5%) | 0.12 |
| Barotrauma† | 16/387 (4.1%) | 5/117 (4.3%) | 11/270 (4.1%) | 0.99 |
| Cardiac arrest | 7/388 (1.8%) | 1/117 (0.9%) | 6/271 (2.2%) | 0.68 |
| Pulmonary embolism | 16/371 (4.3%) | 5/115 (4.3%) | 11/256 (4.3%) | 0.99 |
| Deep vein thrombosis | 24/372 (6.5%) | 10/115 (8.7%) | 14/257 (5.4%) | 0.26 |
| Myocarditis | 37/372 (9.9%) | 11/116 (9.5%) | 26/256 (10.2%) | 0.99 |
ECMO = extracorporeal membrane oxygenation; RRT = rapid response team. Percentages may not total 100 because of rounding. Where the denominator does not match the total number of patients at the head of the table, this is due to missing data.
Assessed daily until ICU discharge.
Defined as pneumothorax or pneumomediastinum or subcutaneous emphysema on chest x-ray or chest computed tomography scan.
Outcome data based on prior RRT review
Overall ICU and hospital mortality rates were 12.3% (51/413) and 13.6% (56/411) respectively, with no significant difference between the groups. Even though the ICU length of stay was similar between the two groups (median, 6 days; IQR, 3-16 days), patients in the RRT review group had a longer hospital length of stay (median, 18 [IQR, 11-33] v 13 days [IQR, 7-24]; P < 0.001). The hospital readmission rate was 16.2%, which was similar between the groups (Table 3)
Table 3.
Clinical outcomes of patients depending on prior rapid response team (RRT) review
| Clinical outcomes | Overall | RRT call | No RRT call | P |
|---|---|---|---|---|
| Total number of patients | 413 | 126 | 287 | |
| In-hospital cardiac arrest | 8/386 (2.1%) | 2/116 (1.7%) | 6/270 (2.2%) | 0.99 |
| Duration of ventilation, days, median (IQR) | 10 (5-16) | 10 (6-15) | 10 (5-16) | 0.84 |
| ICU LOS, days, median (IQR) | ||||
| All patients | 6 (3-16) | 9 (3-16) | 6 (2-16) | 0.06 |
| Survivors | 6 (3-15) | 8 (3-16) | 5 (2-14) | 0.07 |
| Hospital LOS, days, median (IQR) | ||||
| All patients | 15 (8-26) | 18 (11-33) | 13 (7-24) | < 0.001 |
| Survivors | 15 (8-27) | 19 (11-34) | 13 (8-24) | 0.001 |
| ICU mortality | 51 (12.3%) | 17 (13.5%) | 34 (11.8%) | 0.63 |
| Hospital mortality | 56/411 (13.6%) | 19/126 (15.2%) | 37/286 (12.9%) | 0.54 |
| Hospital readmission | 16/99 (16.2%) | 6/26 (23.1%) | 10/73 (13.7%) | 0.35 |
| ICU-acquired weakness | 68/174 (39.1%) | 21/57 (36.8%) | 47/117 (40.2%) | 0.74 |
ICU = intensive care unit; IQR = interquartile range; LOS = length of stay. Percentages may not total 100 because of rounding. Where the denominator does not match the total number of patients at the head of the table, this is due to missing data.
IHCA rate
Only 1.9% (8/413) of ICU patients with COVID-19 had an IHCA. Most of these (6/8) occurred after ICU admission, and most (6/8) were male. The patients who had an IHCA had a median age of 70 years (IQR, 64.8-72.2 years); however, this was not statistically different from the patients who did not have an IHCA (median age, 62 years; IQR, 50-70 years; P = 0.11). The frequency of IHCA was similar between the two groups (1.7% [2/116] v 2.2% [6/270]; P = 0.99) (Figure 1). Only one patient survived to hospital discharge, and the five patients who died after ICU discharge were recorded as having had treatment withdrawn due to poor prognosis.
Sensitivity analysis
A total of 199 patients were admitted to the ICU from the ward. Of these, 120 ward patients (60.3%) were admitted after an RRT review. There were no differences in the baseline characteristics between the groups, except that more patients with obesity (body mass index ≥ 30 kg/m2) were admitted to the ICU without a prior RRT review (20% [23/120] v 33.3% [26/79]; P = 0.04), and patients in the RRT review group were more likely to have tachycardia (Online Appendix, table 1). No patients admitted from the ward had a cardiac arrest in the preceding 24 hours, and only two went on to have an IHCA. There were no differences between interventions, organ support, development of complications, and clinical outcomes between the groups (Online Appendix, table 2).
Discussion
Summary of major findings
This study, which included 413 patients with COVID-19 admitted to Australian ICUs, revealed three important findings. Firstly, the RRT review group comprised one-third of all ICU admissions and nearly two-thirds of ward-based admissions. Secondly, having had a prior RRT review did not affect the rates of IHCA, ICU or hospital mortality, although such patients had a longer hospital length of stay. Thirdly, among patients with COVID-19 admitted to the ICU, IHCA was infrequent, although only one of the eight patients with IHCA survived.
Comparisons with previous studies
A single-centre, retrospective, observational study from Wuhan, China, reported 761 hospital admissions with severe COVID-19 pneumonia, of whom 17.9% (136/761) received cardiopulmonary resuscitation for an IHCA.3 This study investigated IHCA for all hospitalised patients regardless of ICU admission status. In contrast, given that ANZICS APD does not capture pre-ICU data, our study included only patients with COVID-19 who were admitted to the ICU. It is therefore possible that an IHCA could have occurred and that the patient was not admitted to the ICU for various reasons, such as palliation. However, our study showed that no patient admitted from the ward had an IHCA in the preceding 24 hours. Another multicentre cohort study across 68 hospitals in the United States reported 5019 ICU admissions with severe COVID-19 pneumonia, of whom 8% (400/5019) received cardiopulmonary resuscitation for an IHCA.4 A recent systematic review reported a pooled IHCA event incidence of between 1.5% and 5.8% among patients admitted to hospital with COVID-19 and between 8.0% and 11.4% among patients in the ICU.8 Our study demonstrated a significantly lower IHCA rate (1.9%) for ICU patients with COVID-19 than that reported in these studies.
In the pre-COVID-19 era, the rate of ICU admissions from the ward following an RRT review was 56.7% in Australia10 and 51.2% in the United States.20 Our findings of 60.3% ICU admissions following an RRT review was similar to the pre-COVID-19 era. Additionally, the ANZROD scores for patients admitted to the ICU following an RRT review in the pre-COVID-19 era of 13.4%,10 was similar to that found in our study (12.7%). Furthermore, the baseline characteristics of patients in our study were also comparable to those in the pre-COVID-19 era, suggesting that the nature of deteriorating patients on the ward and thresholds for ICU admission in our region is representative. Moreover, outcome measures for patients admitted after RRT reviews in the COVID-19 era, including ICU and hospital mortality, were also comparable to the pre-COVID-19 era (13.5% v 12.3% and 15.2% v 20.8% respectively).10
Discussion of major findings
The lower rates of IHCA reported in our study are likely due to several factors. Firstly, the health care system in Australia was not overwhelmed because of the country's geographic isolation and very strict public health measures.21 This allowed patients to have better access to the ICU early in the course of their illness and to interventions that might have prevented clinical deterioration to cardiac arrest. Secondly, the main source of COVID-19 in Australia in the first wave of the pandemic was international travel (56% of patients), a population who may have been healthier than those infected via community spread.18 In contrast, in the United Kingdom, locally acquired infections predominated and affected an older and more vulnerable population.18,22 Differences in goals of care and not for resuscitation documentation earlier in the course of hospital admission may have also contributed to the lower IHCA rates. Additionally, it is possible that a coordinated approach between the ED, ICU and ward teams may have accounted for the decreased IHCA rate compared with that seen internationally through earlier recognition of high risk patients and better triage. Furthermore, it is possible that many patients with COVID-19 admitted to the ward were not candidates for cardiopulmonary resuscitation, and not eligible for admission to the ICU due to their comorbid conditions or frailty. These treatment limitation orders for patients remaining on the ward were not captured in our data. Finally, as COVID-19-related IHCA mortality is high, the lower IHCA rate in our study may in part explain the lower observed overall mortality.9
We found that more obese patients with COVID-19 were admitted to the ICU without an RRT review, which might reflect the greater number of comorbid conditions associated with obesity,23 and greater concern for how such patients would fare on the ward, resulting in earlier ICU referral before meeting RRT review criteria. Patients admitted following an RRT review had fewer days between symptom onset and hospital admission, which may suggest a rapidly worsening trajectory, highlighting the merits of RRT reviews.
We also found that patients in the RRT review group had a longer stay in hospital before ICU admission compared with the non-RRT group. This reflects that patients in the non-RRT review group were mostly admitted from the ED, where RRT reviews are uncommon in Australia and where patients usually only spend a short period of time in order to meet the National Emergency Access Target of 90% of ED patients being admitted or discharged in under 4 hours.24
The longer hospital length of stay of RRT review patients may reflect patients on the ward who presented later in the course of their illness, with marked inflammatory responses or hospital-acquired infections. These patients may be expected to have a longer hospital stay than those admitted from the ED, who may be at an earlier stage in their illness, and whose illness may resolve more rapidly.
The sensitivity analysis of patients admitted from the ward also revealed that most patients were admitted to the ICU following an RRT review, and none had an IHCA in the preceding 24 hours, again highlighting the benefit of earlier ICU admission because of RRT reviews. Interestingly, there were no significant differences in hospital length of stay or clinical outcomes for patients with COVID-19 admitted to the ICU from the ward depending on prior RRT review, which is a novel and relevant finding.
Study strengths and limitations
Our study has several notable strengths. Firstly, the multicentre design incorporated high quality data and a larger sample size than many other studies. Secondly, this was an Australia-wide study that included data from all eight states and territories over our study period. To our knowledge, it is the only study to explore the use of RRT in the COVID-19 pandemic.
A few limitations should be acknowledged. Firstly, our study lacks a comparator group to ascertain whether our findings are different for patients with COVID-19 or simply a reflection of the way an RRT functions within the Australian health care system. The set-up of a rapid response system often varies widely between hospitals and may explain the difference in numbers of patients admitted from different sources. Secondly, there were no international comparators to explore if our findings reflected intrinsic differences in health care as opposed to resource availability or cultural differences in the provision of supportive care. Thirdly, this was a retrospective design. Fourthly, although there were only a small proportion of patients with treatment limitations and a lower proportion of frail patients compared with non-frail patients, we did not have data on pre-ICU triage following an RRT review that limited ICU admissions. Finally, a wide range of statistical significance tests were carried out with no adjustment for the multiple comparisons, which may increase the likelihood of false positive results.
Conclusion
This multicentre, retrospective, observational cohort study of patients with COVID-19 in Australia revealed that RRT reviews were a common pathway for deteriorating ward patients to be admitted to the ICU, and that IHCA was infrequent. The well established RRTs along with the non-overwhelmed Australian health care system may have resulted in early detections of clinical deterioration permitting earlier ICU admissions and prevention of IHCAs.
Acknowledgments
Acknowledgements:
The authors and the ANZICS CORE Management Committee thank clinicians, data collectors and researchers at the following contributing sites: Alfred Hospital, Austin Hospital, Ballarat Health Services, Bendigo Health Care Group, Box Hill Hospital, Bundaberg Base Hospital, Caboolture Hospital, Cabrini Hospital, Calvary Mater Newcastle, Campbelltown Hospital, Canberra Hospital, Concord Hospital (Sydney), Dandenong Hospital, Epworth Richmond Hospital, Fiona Stanley Hospital, Footscray Hospital, Frankston Hospital, Gold Coast University Hospital, Ipswich Hospital, John Hunter Hospital, Joondalup Health Campus, Launceston General Hospital, Lismore Base Hospital, Liverpool Hospital, Maroondah Hospital, Monash Medical Centre Clayton, Nepean Hospital, Princess Alexandra Hospital, Redcliffe Hospital, Rockingham General Hospital, Royal Adelaide Hospital, Royal Brisbane and Women's Hospital, Royal Darwin Hospital, Royal Melbourne Hospital, Royal North Shore Hospital, Royal Perth Hospital, Royal Prince Alfred Hospital, Sir Charles Gardiner Hospital, South West Healthcare Warrnambool, St George Hospital (Sydney), St Vincent's Hospital (Melbourne), St Vincent's Hospital (Sydney), Sunshine Hospital, The Northern Hospital, The Prince Charles Hospital, University Hospital Geelong, Westmead Hospital, and Wollongong Hospital.
Competing interests
All authors declare that they do not have any potential conflict of interest in relation to this manuscript.
Supplementary Information

References
- 1.World Health Organization. Weekly epidemiological update on COVID-19 — 8 March 2022. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---8-march-2022 (viewed Mar 2022).
- 2.Nishiga M., Wang D.W., Han Y., et al. COVID-19 and cardiovascular disease: from basic mechanisms to clinical perspectives. Nat Rev Cardiol. 2020;17:543–558. doi: 10.1038/s41569-020-0413-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shao F., Xu S., Ma X., et al. In-hospital cardiac arrest outcomes among patients with COVID-19 pneumonia in Wuhan. China. Resuscitation. 2020;151:18–23. doi: 10.1016/j.resuscitation.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hayek S.S., Brenner S.K., Azam T.U., et al. In-hospital cardiac arrest in critically ill patients with covid-19: multicenter cohort study. BMJ. 2020;371 doi: 10.1136/bmj.m3513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shirazi S., Mami S., Mohtadi N., et al. Sudden cardiac death in COVID-19 patients, a report of three cases. Future Cardiol. 2021;17:113–118. doi: 10.2217/fca-2020-0082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Du Y., Tu L., Zhu P., et al. Clinical features of 85 fatal cases of COVID-19 from Wuhan. A retrospective observational study. Am J Respir Crit Care Med. 2020;201:1372–1379. doi: 10.1164/rccm.202003-0543OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ippolito M., Catalisano G., Marino C., et al. Mortality after inhospital cardiac arrest in patients with COVID-19: A systematic review and meta-analysis. Resuscitation. 2021;164:122–129. doi: 10.1016/j.resuscitation.2021.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lim Z.J., Ponnapa Reddy M., Curtis J.R., et al. A systematic review of the incidence and outcomes of in-hospital cardiac arrests in patients with coronavirus disease 2019. Crit Care Med. 2021;49:901–911. doi: 10.1097/CCM.0000000000004950. [DOI] [PubMed] [Google Scholar]
- 9.Biddle N, Edwards B, Gray M, Sollis K: Tracking outcomes during the COVID-19 pandemic (August 2020) — divergence within Australia. https://csrm.cass.anu.edu.au/sites/default/files/docs/2020/9/Tracking_wellbeing_outcomes_during_the_COVID-19_pandemic_February_to_August_2020.pdf (viewed May 2021).
- 10.Orosz J., Bailey M., Udy A., et al. Unplanned ICU admission from hospital wards after rapid response team review in Australia and New Zealand. Crit Care Med. 2020;48:e550–e556. doi: 10.1097/CCM.0000000000004353. [DOI] [PubMed] [Google Scholar]
- 11.Buist M., Harrison J., Abaloz E., Van Dyke S. Six year audit of cardiac arrests and medical emergency team calls in an Australian outer metropolitan teaching hospital. BMJ. 2007;335:1210–1212. doi: 10.1136/bmj.39385.534236.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jones D., Bellomo R., Bates S., et al. Long term effect of a medical emergency team on cardiac arrests in a teaching hospital. Crit Care. 2005;9:R808–R815. doi: 10.1186/cc3906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Santamaria J., Tobin A., Holmes J. Changing cardiac arrest and hospital mortality rates through a medical emergency team takes time and constant review. Crit Care Med. 2010;38:445–450. doi: 10.1097/CCM.0b013e3181cb0ff1. [DOI] [PubMed] [Google Scholar]
- 14.Australian Commission on Safety and Quality in Health Care. National consensus statement: essential elements for recognising and responding to acute physiological deterioration, second edition. https://www.safetyandquality.gov.au/sites/default/files/migrated/National-Consensus-Statement-clinical-deterioration_2017.pdf (viewed July 2021).
- 15.Department of Health and Human Services, Victoria State Government. Factsheet rapid response call management for known or suspected COVID-19 patients. https://www.health.vic.gov.au/factsheet-rapid-response-call-management-known-or-suspected-covid-19-patients (viewed Aug 2021).
- 16.Australian and New Zealand Intensive Care Society. COVID-19 guidelines, version 3. https://www.anzics.com.au/wp-content/uploads/2020/10/ANZICS-COVID-19-Guidelines_V3.pdf (viewed July 2021).
- 17.International Society for Rapid Response Systems. Recommendations for rapid response teams (RRTs) and critical care outreach (CCO) services in the context of the COVID-19 pandemic. https://www.baccn.org/static/uploads/resources/RRT_and_CCO_COVID-19_Version_1.pdf (viewed Aug 2021).
- 18.Burrell A.J.C., Pellegrini B., Salimi F., et al. Outcomes for patients with COVID-19 admitted to Australian intensive care units during the first four months of the pandemic. Med J Aust. 2021;214:23–30. doi: 10.5694/mja2.50883. [DOI] [PubMed] [Google Scholar]
- 19.Department of Health and Human Services, Victoria State Government. COVID-19 hospital-acquired infections among patients in Victorian health services (25 January 2020-15 November 2020). https://www.coronavirus.vic.gov.au/sites/default/files/2021-06/Attachment%201_Full%20Report%20%281%29.pdf (viewed Aug 2021).
- 20.Jäderling G., Bell M., Martling C.R., et al. ICU admittance by a rapid response team versus conventional admittance, characteristics, and outcome. Crit Care Med. 2013;41:725–731. doi: 10.1097/CCM.0b013e3182711b94. [DOI] [PubMed] [Google Scholar]
- 21.Chin K.L., Ofori-Asenso R., Jordan K.A., et al. Early signs that COVID-19 is being contained in Australia. J Infect. 2020;81:318–356. doi: 10.1016/j.jinf.2020.04.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Docherty A.B., Harrison E.M., Green C.A., et al. Features of 20,133 UK patients in hospital with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ. 2020;369 doi: 10.1136/bmj.m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aghili S.M., Ebrahimpur M., Arjmand B., et al. Obesity in COVID-19 era, implications for mechanisms, comorbidities, and prognosis: a review and meta-analysis. Int J Obes (Lond) 2021;45:998–1016. doi: 10.1038/s41366-021-00776-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sullivan C., Staib A., Khanna S., et al. The National Emergency Access Target (NEAT) and the 4-hour rule: time to review the target. Med J Aust. 2016;204:354. doi: 10.5694/mja15.01177. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials