Abstract
Objectives: To investigate the precision of weight measurements in critically ill infants in a paediatric intensive care unit (PICU).
Design: Prospective cohort study.
Setting: Royal Children's Hospital PICU.
Participants: Mechanically ventilated infants admitted to the Royal Children's Hospital PICU between September 2020 and February 2021.
Main outcome measures: Mean percentage difference and agreement of consecutive weight measurements.
Results: Thirty infants were enrolled, of which 17 were receiving post-surgical care for congenital heart disease and four were receiving extracorporeal membrane oxygenation (ECMO). The median age was 13 days (interquartile range [IQR], 3.1–52.4 days). The mean difference in weight was 1.3% (standard deviation [SD], 1.0%), and the test–retest agreement intraclass correlation was 0.99 (95% CI, 0.99-0.99; P < 0.01). The percentage difference between measurements was ≤ 2.5% in 26/30 (87%) children, and the range was < 0.1% to 3.6%. In 26 children not receiving ECMO, the mean difference in weight was 1.1% (SD, 1.0%). There were no complications.
Conclusions: Weighing mechanically ventilated, critically ill infants in intensive care can be performed safely, with a mean difference between consecutive weights of 1.3%, making it a potentially useful additional measure of fluid accumulation.
Fluid accumulation is common in critically ill children, and is associated with adverse outcomes.1 It is commonly measured by net difference in fluid intake and output,2 but change in weight is potentially more suitable. Weighing is performed infrequently due to technical difficulties, patient instability, and difficulties in accounting for the weight of medical equipment and its impact on true changes in the patient's bodyweight. Moreover, there are concerns about poor agreement with fluid balance charts.3, 4, 5 Few studies have investigated the precision of weight measurements in mechanically ventilated children. Therefore, we performed a prospective observational study of the precision of consecutive weight measurements in mechanically ventilated children.
Methodology
A prospective cohort study was performed in children admitted to the Royal Children's Hospital paediatric intensive care unit (PICU) between September 2020 and February 2021. Ethics approval was obtained from the Royal Children's Hospital Human Research Ethics Committee (HREC study number QA/66547/RCHM-2020). Mechanically ventilated children nursed in an Atom infant warmer cot (Parker Healthcare, Melbourne, Australia) were included. Previously enrolled, prone positioned, and clinical unstable children were excluded. After parental verbal consent, two consecutive weight measurements were performed.
Weighing technique
The built-in scales in the Atom infant warmer cot were used after testing for accuracy with calibrated weights (Online Appendix, table 1). The weighing procedure is outlined in the Online Appendix (box 1). Each measurement was performed by the principal investigator (BG) with assistance from nursing staff. The first weight was recorded by staff not involved in performing the measurement. Data were entered into a REDCap database V10.7.1 (Vanderbilt University, 2021).
Statistical analysis
Demographic and clinical data were described using frequencies and proportions. Absolute difference (g) and percentage difference (absolute difference ÷ first weight × 100) between weights were calculated. The normality of the data was confirmed using the Shapiro–Wilk test (Online Appendix, figure 1) and the mean (standard deviation [SD]) difference was presented. Test–retest agreement was assessed using intraclass correlation (ICC) and Bland–Altman analysis. Sensitivity analysis was performed excluding children receiving extracorporeal membrane oxygenation (ECMO). Analyses were performed with the “irr”, “lpSolve” and “blandr” packages; R software, version 4.0.2 (R Foundation for Statistical Computing, Vienna, Austria). The ICC estimates with 95% confidence intervals (CIs) were based on single measurements, using a two-way model, and assessed for agreement. A P value < 0.05 was considered statistically significant.
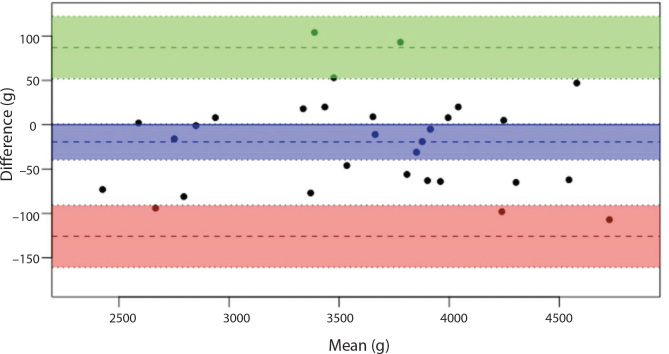
Figure 1.
Frequency of percentage differences between two consecutive weight measurements (n = 30 infants)
Results
Thirty paired weights were performed. The demographic and clinical characteristics of children are shown in the Online Appendix (table 2).
Weight measurements
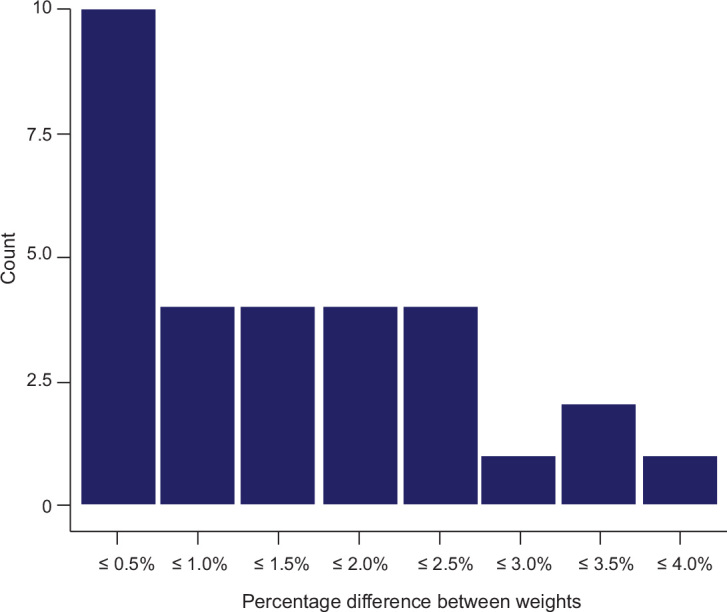
The mean first weight of all children was 3611 g (SD, 621 g). The individual paired weight measurements, absolute and percentage differences, and mean (SD) are shown in the Online Appendix (table 3). The test–retest agreement ICC was 0.99 (95% CI, 0.99–0.99; P < 0.01). The mean proportional weight difference was 1.3% (SD, 1.0%). The percentage difference was ≤ 2.5% in 26/30 children (87%), and the range was < 0.1% to 3.6% or 1 g to 94 g in two children weighing 2849 g and 2619 g respectively. Figure 1 shows the frequency of percentage weight differences. The Bland–Altman analysis, bias, and limits of agreement are shown in Figure 2 and in the Online Appendix (box 2).
Figure 2.
Bland–Altman plot for analysis of agreement between two weights (n = 30)
Sensitivity analysis
In 26 children not receiving ECMO, the mean proportional weight difference was 1.1% (SD, 1.0%). The interobserver agreement ICC was 0.99 (95% CI, 0.99–0.99; P < 0.01).
No complications occurred during weighing.
Discussion
Key findings
In this study, we showed that weighing mechanically ventilated infants can be performed safely with precision. The mean difference between sequential measurements was 1.3%, and when excluding children receiving ECMO, the mean difference was 1.1%. The test–retest agreement was high, and a high proportion of measurements had a mean difference ≤ 2.5%.
Weighing children and adults in intensive care
Measuring weight in critically ill children is uncommonly performed6 due to technical difficulties. In critically ill adults, weight change poorly correlates with recorded measurements of fluid balance,7 (r = 0.34)3 and (r = 0.28).4 In children, the correlation is better (r = 0.63); however, high mean differences challenge its clinical utility.5 Inaccuracies of both weight and recorded measures of fluid balance make their comparison difficult.
Implications of findings
A mean difference in sequential weight measurement of 1.3% is a clinically acceptable margin for assessing fluid accumulation, particularly considering that fluid accumulation is commonly assessed in 5–10% increments2, 8, 9 and even dichotomised at 20%.10 Four weight differences were between 3% and 4%, indicating the need for optimising the technique. But in absolute terms, the peak difference was 94 g — infants are more prone to higher proportional changes.
Strengths and limitations
The strength of this study is the standardisation of weighing technique using accurate scales and consistent operators. The limitations are that we only studied infants weighing up to 5 kg. However, this population has greater proportional margin for difference in weight. We did not subtract the weight of attached devices, but consecutive weights were performed without interval change in the number of devices.
Conclusion
Weighing critically ill infants can be performed safely, with a mean test–retest agreement of 1.3%, making it a potentially useful additional clinical measure of fluid accumulation.
Acknowledgements: The authors would like to acknowledge the families who gave permission for their children to participate and the intensive care nurses Hannah Delahunty, Matthew Van De Velde, James Walker, Zamzam Abdi, Zoe Jamieson, Tabetha White, Artressa Ng, Jamie Palmer, Sarah Johnstone, Cory Bach, Jonathan Read and Courtney Marsden for assisting with weight measurements.
Competing interests
No relevant disclosures.
References
- 1.Alobaidi R., Morgan C., Basu R.K., et al. Association between fluid balance and outcomes in critically ill children: a systematic review and meta-analysis. JAMA Pediatr. 2018;172:257–268. doi: 10.1001/jamapediatrics.2017.4540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alobaidi R., Basu R.K., DeCaen A., et al. Fluid accumulation in critically ill children. Crit Care Med. 2020;48:1034–1041. doi: 10.1097/CCM.0000000000004376. [DOI] [PubMed] [Google Scholar]
- 3.Schneider A.G., Baldwin I., Freitag E., et al. Estimation of fluid status changes in critically ill patients: fluid balance chart or electronic bed weight? J Crit Care. 2012;27(745):e7–12. doi: 10.1016/j.jcrc.2011.12.017. [DOI] [PubMed] [Google Scholar]
- 4.Schneider A.G., Thorpe C., Dellbridge K., et al. Electronic bed weighing vs daily fluid balance changes after cardiac surgery. J Crit Care. 2013;28(1113):e1–e5. doi: 10.1016/j.jcrc.2013.07.056. [DOI] [PubMed] [Google Scholar]
- 5.Bontant T., Matrot B., Abdoul H., et al. Assessing fluid balance in critically ill pediatric patients. Eur J Pediatr. 2015;174:133–137. doi: 10.1007/s00431-014-2372-9. [DOI] [PubMed] [Google Scholar]
- 6.Ahearn M.A., Soranno D.E., Stidham T., et al. Adherence to daily weights and total fluid orders in the pediatric intensive care unit. Pediatr Qual Saf. 2018;3 doi: 10.1097/pq9.0000000000000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.You J.W., Lee S.J., Kim Y.E., et al. Association between weight change and clinical outcomes in critically ill patients. J Crit Care. 2013;28:923–927. doi: 10.1016/j.jcrc.2013.07.055. [DOI] [PubMed] [Google Scholar]
- 8.Akcan-Arikan A., Gebhard D.J., Arnold M.A., et al. Fluid Overload and Kidney Injury Score: a multidimensional real-time assessment of renal disease burden in the critically ill patient. Pediatr Crit Care Med. 2017;18:524–530. doi: 10.1097/PCC.0000000000001123. [DOI] [PubMed] [Google Scholar]
- 9.Sutherland S., Zappitelli M., Alexander S., et al. Fluid overload and mortality in children receiving continuous renal replacement therapy: the Prospective Pediatric Continuous Renal Replacement Therapy Registry. Am J Kidney Dis. 2010;55:316–325. doi: 10.1053/j.ajkd.2009.10.048. [DOI] [PubMed] [Google Scholar]
- 10.Gist K.M., Selewski D.T., Brinton J., et al. Assessment of the Independent and Synergistic Effects of Fluid Overload and Acute Kidney Injury on Outcomes of Critically Ill Children. Pediatr Crit Care Med. 2020;21:170–177. doi: 10.1097/PCC.0000000000002107. [DOI] [PMC free article] [PubMed] [Google Scholar]