Abstract
Objectives: To investigate the prevalence and features of self-reported burnout among intensivists working in Australia and New Zealand, and evaluate potentially modifiable workplace stressors associated with increased risk of self-reported burnout.
Methods: We performed an electronic survey among registered intensivists in Australia and New Zealand. Burnout and professional quality of life were measured using the Professional Quality of Life Scale version 5 (ProQOL-5). Socio-organisational factors were defined a priori and assessed using a five-point Likert scale. Thematic analysis was conducted on an open-ended question on workplace stressors.
Results: 261 of 921 estimated intensivists responded (response rate, 28.3%). Overall, few participants (0.8%) demonstrated high scores (> 75th centile) for burnout, and 70.9% of participants scored in the average range for burnout. Of note, 98.1% of participants scored in the average to high range for compassion satisfaction. No association was found between sex, age, or years of practice with the level of burnout or compassion satisfaction. Seven themes emerged regarding intensivists' most stressful aspects of work: interpersonal interactions and workplace relationships (25.5%), workload and its impact (24.9%), resources and capacity (22.6%), health systems leadership and bureaucracy (16.1%), end-of-life issues and moral distress (8.4%), clinical management (4.9%), and job security and future uncertainty (1.3%).
Conclusion: Fewer Australian and New Zealand intensivists experienced burnout than previously reported. Many self-reported work stressors do not relate to clinical work and are due to interpersonal interactions with other colleges and hospital administrators. Such factors are potentially modifiable and could be the focus of future interventions.
Burnout is a state of mental or emotional exhaustion resulting from persistent exposure to workplace stressors1 and was first described in occupational psychology literature in the 1970s.2 Maslach and colleagues describe burnout as a syndrome characterised by emotional exhaustion, cynicism or depersonalisation, and reduced personal accomplishment.3, 4, 5, 6 Doctors, particularly those in critical care environments, are reported to be at increased risk of experiencing burnout.5, 7, 8, 9, 10
Burnout has been associated with suboptimal care, medical errors,9, 11 job turnover, absenteeism, low morale, self-reported measures of personal distress, increased use of alcohol and drugs, and relationship and family problems.3 There is an important link between burnout and organisational culture and quality of care.12
Limitations of previous studies evaluating burnout include the use of different tools and methodologies, and the variable use of arbitrary cut-offs to define the presence or absence of burnout (usually the 75th centile) as a binary (yes/no) outcome. Despite 20 years of study on burnout, there is a lack of evidence-based research on potentially modifiable workplace factors.13, 14 Furthermore, there is a paucity of studies exploring the potential positive mental health outcomes for staff working in intensive care.
Increasing interest among medical training bodies, colleges and peak organisations in Australia and New Zealand15, 16, 17 in burnout and physician wellbeing has resulted in position statements and framework development.18, 19, 20, 21 In response to such concerns, the Professional Activities and Welfare Committee of the Australian and New Zealand Intensive Care Society (ANZICS) commissioned this survey to assess the frequency of burnout among intensive care physicians practising in Australia and New Zealand. An additional aim was to evaluate workplace stressors associated with an increased risk of self-reported burnout to inform future strategies to prevent or mitigate the effects of workplace stress and burnout on the intensive care specialist medical workforce.
Methods
Study design and research questions
We conducted an electronic survey to evaluate the frequency of burnout, self-reported professional quality of life, and self-reported workplace stressors experienced by intensivists in Australia and New Zealand. Burnout was assessed using the Professional Quality of Life Scale version 5 (ProQOL-5).22 Two previous studies influenced the methodology for our research. A systematic review on the prevalence of compassion fatigue and burnout in the intensive care unit (ICU) reported that burnout has been oversimplified and future research needed to incorporate intensivist work and communication practices and emotional distress.23 The Critical Care Societies Collaborative Statement on burnout in 2016 identified two interventions to mitigate burnout in critical care, enhancing the ICU environment and assisting individuals to cope with the ICU.10 Simpson and Knott recommended a multilevel and holistic approach to the investigation of the ICU clinician.24 To build on current findings and address recent critiques, we adopted a mixed methodology. The ProQOL-5 measurement was used in addition to several work environment questions and an open-ended question on wellbeing, which was analysed thematically.
Socio-organisational variables were evaluated using a Likert agreement scale within a priori defined factors previously associated with workplace stress and burnout,4, 12, 25, 26, 27 including interpersonal interactions and workplace relationships, leadership and governance, and self-determination and control. Finally, we used open-ended responses to seek intensivists' perspectives about the aspects of their work they perceived to be the most stressful.
Ethics
Ethics approval was provided by the University of Queensland School of Medicine, Low and Negligible Risk Ethics SubCommittee (clearance No. 2017001 103).
Participant eligibility and recruitment
Recruitment occurred over a 6-week period (August and September 2018). Participants were registered medical professionals acting in the role of a consultant intensivist, working primarily in an ICU in Australia and New Zealand. Participants were not required to be ANZICS members or Fellows of the College of Intensive Care Medicine of Australia and New Zealand (CICM). An estimated 921 intensivists were eligible to participate.28, 29
The survey was administered electronically (SurveyMonkey; San Mateo, CA, USA). Invitations were distributed via the ANZICS distribution list, and weekly reminders were sent during the 6-week study period. The survey was also promoted in the CICM e-newsletter and via social media. The study focused on specialists to reduce the heterogeneity of the cohort and increase the ease of contacting potential participants because the focus of the Professional Activities and Welfare Committee is the wellbeing of specialists.
Survey development
The survey was developed, conducted and reported in accordance with published guidelines.30 A draft survey was piloted in a sample of vocational paediatric ICU trainees who were ineligible to participate in the survey and was revised to improve the understanding of the questions. It was divided into four parts (Online Appendix, section 1):
-
•
part 1 — ProQOL-5 instrument;
-
•
part 2 — demographic information;
-
•
part 3 — 16 questions addressing socio-organisational factors; and
-
•
part 4 — open-ended text response to the question “What are the three most stressful aspects of your work?”.
The Professional Quality of Life Scale version 5
ProQOL-5 is an open-access, validated psychometric research tool used to measure the positive and negative aspects of the work for employees in helping or caring professions.22 It contains 30 items, with responses given on a 1-5 Likert scale where 1 corresponds to "never” and 5 with "very often”. Responses to these items generate scores for three separate subscales:
-
•
The burnout subscale quantifies negative feelings associated with difficulties in performing work effectively and the sense of hopelessness related to this.
-
•
The secondary traumatic stress subscale measures the negative effects experienced when caring for individuals who have themselves experienced traumatic events. The ProQOL-5 instrument combines burnout and secondary traumatic stress and considers them both as compassion fatigue.
-
•
Compassion satisfaction subscale is defined as the pleasure derived from doing work well and provides a counter to compassion fatigue.
The ProQOL tool developers maintain a registry of studies using various versions of the tool from which scores indicating the 25th and 75th centiles have been published.22 The raw total scores of the ProQOL are categorised as < 22, 23-41 and > 42 and correspond with “low”, “moderate” and “high” for each construct, respectively.
Statistical analysis
Descriptive analyses of demographic data and ProQOL-5 scores were performed. Categorical data are presented as frequencies and percentages, and continuous data are and interquartile range (IQR), as appropriate. Associations and interquartile range (IQR), as appropriate. Associations between the ProQOL-5 burnout subscale (ProQOL-5: burnout) and demographic characteristics were investigated using analysis of variance. Statistical analyses were conducted using Stata/IC 14.2 (StataCorp, College Station, TX, USA). A P value < 0.05 was taken to indicate statistical significance.
Thematic analysis
Open-ended responses to the question “What are the three most stressful aspects of your work?” was analysed through an iterative process using principles based on grounded theory.31, 32, 33, 34 Data were compiled, disassembled and open- coded independently by two investigators (LC and SM). Emergent themes were compared to assess intercoder reliability, and a coding framework was devised. Data were recoded and reassembled into key themes and subthemes to build a visual representation of the data and then rereviewed by four research team members (LC, SM, MN and DJ) to ensure consensus and increase rigour.
Results
Details of participants
From 921 eligible participants, 261 submitted surveys (response rate 28.3%). Males comprised 75.1% of participants, 82.8% practised primarily in Australia, and 57.8% were aged between 41 and 55 years (Table 1). There were minimal missing data, with three surveys missing demographic data, four missing clinical hours in the ICU, and less than ten missing for each of the occupational and environmental factors.
Table 1.
Characteristics of respondents to survey exploring burnout among intensivists in Australia and New Zealand
| Characteristics | n (%) |
|---|---|
| Total number of participants | 261 |
| Age (years) | |
| ≤ 35 | 6 (2.3%) |
| 36-40 | 39 (14.9%) |
| 41-45 | 60 (23.0%) |
| 46-50 | 46 (17.6%) |
| 51-55 | 45 (17.2%) |
| 56-60 | 34 (13.0%) |
| 61-65 | 21 (8.0%) |
| ≥ 66 | 7 (2.7%) |
| Unknown | 3 (1.1%) |
| Sex | |
| Male | 196 (75.1%) |
| Female | 62 (23.8%) |
| Unknown | 3 (1.1%) |
| Primary place of practice | |
| Australia | 214 (82.8%) |
| New Zealand | 43 (16.5%) |
| Other | 1 (0.4%) |
| Unknown | 3 (1.1%) |
| Number of years as intensivist | |
| 0-5 | 62 (23.8%) |
| 6-10 | 52 (19.9%) |
| 11-15 | 36 (13.8%) |
| 16-20 | 53 (20.3%) |
| ≥ 21 | 55 (21.1%) |
| Unknown | 3 (1.2%) |
Details of ProQOL-5 scores
The distribution of participants’ scores on the ProQOL-5 subscales (scale 10-50) are demonstrated in Figure 1 and in the Online Appendix, section 2. Scores in the domain of compassion satisfaction ranged from 16 to 50 (higher scores suggest greater satisfaction). The mean score was 36.1 (SD, 6.5), with 22.6% demonstrating high compassion satisfaction, 1.9% showing low levels of compassion satisfaction, and 75.5% demonstrating moderate compassion satisfaction.
Figure 1.
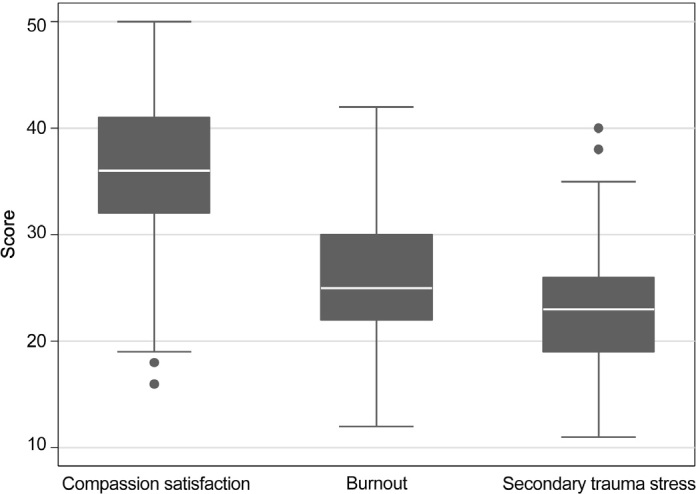
Box plot of Professional Quality of Life Scale version 5 (ProQOL-5) subscales showing median and interquartile range
Participants’ scores for burnout ranged between 12 and 42 (higher scores suggest greater burnout), with a mean score of 26.1 (SD, 6.0). Most participants (70.9%) demonstrated moderate levels of burnout, 28.4% demonstrated low levels of burnout, and only 0.8% had high burnout. There were no associations between burnout score and age, sex, primary place of practice and duration of work as a consultant intensivist (Online Appendix, section 3).
Scores for secondary traumatic stress ranged from 11 to 40 (higher scores suggest more secondary traumatic stress), and the mean score was 22.7 (SD, 5.4). Almost half (46.4%) of participants had low scores in the domain of secondary traumatic stress. The remaining 53.6% had scores between the 25th and 75th centiles (moderate), and none had scores demonstrating high levels of secondary traumatic stress.
Self-reported socio-organisational stressors
Two-hundred and fifty-two participants (96.6%) responded to the 16 questions assessing the impact of socio- organisational factors in the ICU workplace (Table 2). A summary of findings includes:
-
•
Interpersonal interactions and workplace relationships: Most participants reported collegial or effective working relationships “often” or “very often” with their ICU medical colleagues (74.7%), nursing colleagues (81.7%), and other medical specialties (65.1%).
-
•
Leadership and governance: 58.6% of participants reported feeling supported “often” or “very often” by those in leadership positions within their ICU. In contrast, 37.6% reported “never” or “rarely” feeling supported by their hospital executive. Similarly, participants felt the needs of their ICU or specialty were “never” or “rarely” adequately advocated for within their hospital (32.6%) or within their health system (34.5%).
-
•
Self-determination and control: 75.9% responded that they needed to “fight” to get things done at work at least “some of the time”. The majority of participants (86.2%) identified they are working in their job of choice.
Table 2.
Details of level of agreement to questions regarding socio-organisational factors associated with intensivist wellbeing and burnout
| Question | N | Never | Rarely | Sometimes | Often | Very often |
|---|---|---|---|---|---|---|
| Interpersonal interactions and workplace relationships | ||||||
| I enjoy collegial relationships with my ICU medical colleagues | 252 | 4 (1.5%) | 9 (3.5%) | 44 (16.9%) | 120 (46.0%) | 75 (28.7%) |
| I enjoy collegial relationships with my nursing colleagues | 253 | 1 (0.4%) | 4 (1.5%) | 35 (13.4%) | 127 (48.7%) | 86 (33.0%) |
| I enjoy effective working relationships with other medical specialties within my hospital | 253 | 0 | 11 (4.2%) | 72 (27.6%) | 135 (51.7%) | 35 (13.4%) |
| When I am experiencing difficulties at work, I have someone to talk it over with | 254 | 13 (5.0%) | 39 (14.9%) | 70 (26.8%) | 85 (32.6%) | 47 (18.5%) |
| Leadership and governance | ||||||
| I am supported by those in leadership positions within my unit | 254 | 10 (3.8%) | 25 (9.6%) | 66 (25.3%) | 88 (33.7%) | 65 (24.9%) |
| I am supported by the hospital executive | 254 | 25 (9.6%) | 73 (28.0%) | 96 (36.8%) | 54 (20.7%) | 6 (2.3%) |
| I feel as though the needs of my unit are adequately advocated for within my hospital | 254 | 11 (4.2%) | 74 (28.4%) | 93 (35.6%) | 60 (23.0%) | 16 (6.1%) |
| I feel as though the needs of my specialty are adequately advocated for within my health system | 254 | 14 (5.4%) | 76 (29.1 %) | 111 (42.5%) | 43 (16.5%) | 10 (3.8%) |
| I feel that there is a clear and widely understood vision for how the unit I work in is developing | 253 | 14 (5.4%) | 53 (20.3%) | 98 (37.6%) | 68 (26.1 %) | 20 (7.7%) |
| The clinical workload in my unit is managed well | 252 | 5 (1.9%) | 31 (11.9%) | 81 (31.0%) | 114 (43.7%) | 21 (8.1%) |
| Control and self-determination | ||||||
| I find I have to "fight" in order to get things done at work | 252 | 2 (0.8%) | 52 (19.9%) | 116 (44.4%) | 56 (21.5%) | 26 (10.0%) |
| I am concerned about my future in the specialty I have trained in | 254 | 40 (15.3%) | 77 (29.5%) | 71 (27.2%) | 38 (14.6%) | 28 (10.7%) |
| I feel that I can influence the working of my unit | 254 | 5 (1.9%) | 51 (19.5%) | 90 (34.5%) | 7 (28.0%) | 35 (13.4%) |
| I am currently working in the job(s) I want to work in | 253 | 6 (2.3%) | 22 (8.4%) | 64 (24.5%) | 111 (42.5%) | 50 (19.2%) |
| I have adequate access to rostered non-clinical time | 252 | 9 (3.5%) | 20 (7.7%) | 72 (27.6%) | 111 (42.5%) | 40 (15.3%) |
| I have adequate ability to select when I have time away from work | 252 | 2 (0.8%) | 32 (12.3%) | 80 (30.7%) | 105 (40.2%) | 33 (12.6%) |
ICU = intensive care unit.
Thematic analysis of open-ended responses
A total of 228 participants (87.4%) provided 638 free text responses for the open-ended question “What are the three most stressful aspects of your work?”. Individuals who duplicated the same response only had one answer recorded.
Seven themes emerged from the thematic analysis (Online Appendix, section 4) with an overarching major theme of mismatch of expectations between intensivists and their colleagues and trainees, societal expectations, and the system in which they are employed.
-
•
Interpersonal interactions and workplace relationships (163/638 responses, 25.5%): The most frequently perceived poor behaviour included bullying, incivility, conflict and politics. Less dominant themes included dealing with difficult patients and families or issues pertaining to supervision of junior medical staff and trainees. Comments regarding sexist and racist behaviour were very infrequent.
-
•
Workload (159/638 responses, 24.9%): The dominant finding in this theme related to the intrusiveness of shift work, after-hours rostering, and the impact on intensivists' lives, with frequent responses including “on call”, “night call”, “lack of sleep”, “tiredness”, “fatigue” and “after-hours work”. Time management, balancing competing demands, and managing administrative workload and non-clinical portfolios were cited as adversely affecting the participants' personal lives, relationships and their families.
-
•
Resources and capacity (144/638 responses, 22.6%): Perceived resource constraints and inadequate ICU capacity was the third most frequently cited cause of concern, as well as bed management issues and their impact on patient flow.
-
•
Health systems governance, leadership and bureaucracy (103/638 responses, 16.1%): Interactions with members of the organisational hierarchy were listed as a cause of stress and expressed in responses such as “dealing with management” and “dealing with executives”. Common responses included simply “administration”, “bureaucracy” and “leadership”. Less commonly, participants raised concerns regarding leadership within the ICU.
-
•
End-of-life issues and moral distress (54/638 responses, 8.4%): Stress related to end-of-life decision making related mainly to a perceived mismatch of expectations with medical specialties outside of the ICU (“Mismatch of expectations with some non-ICU colleagues over patient care goals”), patient relatives (“Inappropriate continuation of curative care in the dying”), as well as a failure of hospital leadership to address setting of goals of care (“Hospital-wide failure to consider end- of-life planning”).
-
•
Clinical management (31/638 responses, 4.9%): Less frequent sources of stress included the burden of responsibility for the deteriorating or critically unwell patient (“Hoping that I haven’t missed anything clinically”, “Being responsible for the wellbeing of very acutely unwell patients with high incidence of morbidity and mortality”). Concerns on how to remain engaged in ongoing professional development and research were also notable (“Keeping up with the rapidly expanding knowledge”).
-
•
Job security and future uncertainty (8/638 responses, 1.3%): Eight responses related to job security, future uncertainty and the need to constantly move to secure work and training, which was stressful for themselves, their relationships and their families.
Discussion
Summary of major findings
This cross-sectional survey of ICU specialists working in Australia and New Zealand revealed that high levels of burnout and compassion fatigue were relatively uncommon, and levels of compassion satisfaction were moderate. Unlike previous studies on burnout among critical care physicians, there was no significant association between the measures of burnout and age, sex, or duration of work as a consultant intensivist.35, 36
Although most intensivists reported satisfaction with interpersonal interactions and workplace relationships for staff within the ICU, the most common theme identified as affecting wellbeing was interpersonal interactions and workplace relationships. Thus, major reported sources of workplace stressors included adverse interactions with colleagues and administrators outside of the ICU, the burdensome nature and quantity of out-of-hours rostering, administrative work, and issues pertaining to end-of- life care. We identified an overarching theme regarding mismatch of expectations across most of the themes.
Comparison with previous studies
In 2017, Highfield and Parry-Jones surveyed 799 members (34.7%) of the Faculty of Intensive Care Medicine in the United Kingdom using the ProQOL-5 tool37 and found remarkably similar results to our study for each of the subscales. In contrast, in 2007, Shehabi and colleagues8 explored the frequency of burnout among 115 ANZICS members (36%) using the modified Maslach Burnout Inventory. They found a high incidence of burnout and self-reported underachievement in terms of personal accomplishment. However, the authors similarly found that mediation and conflict management were areas where intensivists required assistance.
It is difficult to assess the prevalence of burnout in our study population as there are no widely accepted criteria of what constitutes burnout.38, 39, 40, 41 A recently published systematic review concluded that “there was substantial variability in prevalence estimates of burnout among physicians and marked variation in burnout definitions, assessment methods, and study quality ... [which] preclude definitive conclusions about the prevalence of burnout”.38 The Maslach Burnout Inventory and other tools frequently report burnout as a binary diagnosis (burnout yes or no), whereas burnout needs to be viewed as a spectrum that exists in a dynamic state in response to work environments.42 A review of other studies using the ProQOL-5 to examine the wellbeing of doctors or nurses in various settings revealed marked variation on how the results were presented (Online Appendix, section 5). The developers of the ProQOL-5 tool state that it is best used in its continuous form.22 However, most authors report the prevalence of participants in each arbitrarily defined category, and many do not acknowledge the continuous nature of the scoring system.37, 43, 44, 45
While our study did not find high risk associations for Australian and New Zealand intensivists in relation to burnout, secondary traumatic stress, or compassion fatigue, it did find concerning systemic issues that were having a significant impact on the working relationships, levels of stress, and risks to wellbeing for Australian and New Zealand intensivists.
One of the reasons for the low frequency of reported burnout may relate to the relatively low mortality seen in Australian and New Zealand ICUs. ICU mortality has previously been shown to be an independent determinant of burnout.46
Study strengths and limitations
This study is the first known research using the ProQOL-5 tool with intensivists in Australia and New Zealand, allowing investigation of negative associations such as burnout, secondary traumatic stress and compassion fatigue and the positive association of compassion satisfaction. This study also explored professional quality of life, socio-organisational stressors and sources of stress that may be amenable to modification. The study included a comparatively large sample size of intensivists.
Our respondents were relatively representative of the population of intensivists in Australia and New Zealand at the time of the study. Unpublished data from the CICM revealed that, in 2019, 80% of active Fellows were from Australia, 77% were male, and 45% were aged between 41 and 55 years. In an era when intensive care clinicians are reported to have high levels of burnout,47 this study found positive associations with reports of moderate compassion satisfaction. Such findings are important to attract trainees to this field.
A limitation of our study is that we cannot state why over 70% of intensivists chose not to participate, creating a risk of non-responder bias. We made a conscious decision to use the ProQOL-5 in favour of other psychometric tools used to measure burnout. The ProQOL-5 captures the incidence of compassion satisfaction and secondary traumatic stress and enables a more comprehensive understanding of the issues facing Australian and New Zealand intensive care specialists. The associations revealed in our analysis do not imply causation. The Australian and New Zealand health care system differs from those in the United States and Europe and our findings may not be applicable to other countries.
Our participants self-identified by responding to communications from distributions lists from ANZICS and CICM and self-identified as intensivists. They survey was also promoted at conferences and on social media platforms. It is possible that some additional intensivists could have been identified using distribution lists from the regional colleges for anaesthetists or emergency physicians.
Our findings represent the perspective of intensivists from 2018. The delay in compiling and reporting our data was the result of the unprecedented clinical demand of the coronavirus disease 2019 (COVID-19) pandemic. It is likely that the COVID-19 pandemic has been associated with novel workplace stressors affecting clinician wellbeing. However, our study will provide an important baseline to allow comparison with such changes. In addition, as clinical care and workplace practices return to a pre-COVID-19 state, we believe it is likely that the themes we have identified will remain relevant for strategies to improve workplace conditions and clinician wellbeing. Indeed, it is probably that the anxiety, depression and stress recently reported in association with the COVID-19 pandemic48 may have exacerbated such workplace stressors.
The findings of our study represent the perspectives and workplace stressors of specialists. It is likely that the factors affecting nurses, allied health and ICU trainees will differ from those reported here and may be the subject of future studies. The prevalence of burnout among other intensive care health care professionals remains poorly understood, with a wide variance in measurement tools and results making definitive conclusions difficult.23, 38, 49 Previous studies have reported high levels of burnout among ICU nurses.50 Our study did not include other health care professionals due to the challenges of accessing email distributions lists and the anticipated heterogeneity of workplace stressors within each professional group.
We collected a small amount of demographic characteristics in our study to reduce the length of the survey to improve response rate. Inclusion of data on ethnicity, country of origin, sexual orientation, or balance of private and public practice may have provided additional information. As our cohort contained mostly men, this may affect our findings, particularly in relation to the reporting of sexist behaviour.
Implications for clinicians, researchers and policymakers
Our study suggests that severe burnout was relatively uncommon among intensivists in Australia and New Zealand. This study found that concerns related to burnout and stress were less associated with clinical issues than they were with systemic processes and structures beyond the control of individual intensive care specialists. The wellbeing of health care professionals is dependent on engagement, autonomy, connection, contribution and being appreciated and respected.51, 52, 53, 54 Several findings in this study demonstrate how health authorities can build on the commitment and job satisfaction for intensivists and what interventions could occur to negate the negative aspects of the job and culture. Managing interpersonal conflict and challenging communication is highlighted throughout the study and is an important skill set for intensivists.
Conclusion
Burnout and compassion fatigue is relatively uncommon among Australian and New Zealand intensive care specialists, and few participants report negative interactions with other ICU colleagues. Factors adversely affecting selfreported professional quality of life for Australian and New Zealand intensivists were more likely to be interactions with hospital administrators and colleagues outside the ICU than stressors relating to clinical work.
Competing interests
All authors declare that they do not have any potential conflict of interest in relation to this manuscript.
Acknowledgements
The authors wish to thank Jennifer Holmes (ANZICS) for the administration and support of the survey. We also thank David Rigg (ANZICS Professional Activities and Welfare Committee) and Mark Coulthard (Faculty of Medicine, University of Queensland) for their contribution to the development of this project.
Data sharing statement
Individual participant data that underlie the results in this article is deidentified and available. The data will be immediately available following publication and ending five years following publication. Investigators who proposed to use the data should obtain approval by an independent review committee. The data are available for meta-analysis. Proposals should be directed to mark.nicholls@svha.org.au.
Supplementary Information

References
- 1.World Health Organization . 2018. ICD-11 for mortality and morbidity statistics: QD85 burnout.https://icd.who.int/browse11/l-m/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f129180281 (viewed June 2022) [Google Scholar]
- 2.Freudenberger H.J. Staff burnout. Journal of Social Issues. 1974;30:159–165. [Google Scholar]
- 3.Maslach C., Jackson S.E. The measurement of experienced burnout. J Organ Behav. 1981;2:99–113. [Google Scholar]
- 4.Maslach C., Schaufeli W.B., Leiter M.P. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 5.Embriaco N., Azoulay E., Barrau K., et al. High level of burnout in intensivists: prevalence and associated factors. Am J Respir Crit Care Med. 2007;175:686–692. doi: 10.1164/rccm.200608-1184OC. [DOI] [PubMed] [Google Scholar]
- 6.Maslach C., Jackson S.E., Leiter M.P. In: Evaluating stress: a book of resources. Scarecrow Education. 3rd ed. Zalaquett C.P., Wood R.J., editors. 1996. The Maslach Burnout Inventory manual; pp. 191–218. [Google Scholar]
- 7.Balch C.M., Freischlag J.A., Shanafelt T.D. Stress and burnout among surgeons: understanding and managing the syndrome and avoiding the adverse consequences. Arch Surg. 2009;144:371–376. doi: 10.1001/archsurg.2008.575. [DOI] [PubMed] [Google Scholar]
- 8.Shehabi Y., Dobb G., Jenkins I., et al. Burnout syndrome among Australian intensivists: a survey. Crit Care Resusc. 2008;10:312–315. [PubMed] [Google Scholar]
- 9.Shanafelt T.D., Bradley K.A., Wipf J.E., Back A.L. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136:358–367. doi: 10.7326/0003-4819-136-5-200203050-00008. [DOI] [PubMed] [Google Scholar]
- 10.Moss M., Good V.S., Gozal D., et al. An official Critical Care Societies Collaborative Statement: burnout syndrome in critical care healthcare professionals: a call for action. Crit Care Med. 2016;44:1414–1421. doi: 10.1097/CCM.0000000000001885. [DOI] [PubMed] [Google Scholar]
- 11.West C.P., Huschka M.M., Novotny P.J., et al. Association of perceived medical errors with resident distress and empathy: a prospective longitudinal study. JAMA. 2006;296:1071–1078. doi: 10.1001/jama.296.9.1071. [DOI] [PubMed] [Google Scholar]
- 12.Montgomery A., Todorova I., Baban A., Panagopoulou E. Improving quality and safety in the hospital: the link between organizational culture, burnout, and quality of care. Br J Health Psychol. 2013;18:656–662. doi: 10.1111/bjhp.12045. [DOI] [PubMed] [Google Scholar]
- 13.Bresesti I., Folgori L., De Bartolo P. Interventions to reduce occupational stress and burn out within neonatal intensive care units: a systematic review. Occup Environ Med. 2020;77:515–519. doi: 10.1136/oemed-2019-106256. [DOI] [PubMed] [Google Scholar]
- 14.Young J.L., Derr D.M., Cicchillo V.J., Bressler S. Compassion satisfaction, burnout, and secondary traumatic stress in heart and vascular nurses. Crit Care Nurs Q. 2011;34:227–234. doi: 10.1097/CNQ.0b013e31821c67d5. [DOI] [PubMed] [Google Scholar]
- 15.College of Intensive Care Medicine of Australia and New Zealand. CICM welfare [website]. https://www.cicm.org.au/Fellows/Special-Interest-Groups/Welfare (viewed June 2020).
- 16.Australian and New Zealand College of Anaesthetists. ANZCA welfare of anaesthetists SIG [website]. https://www.anzca.edu.au/about-us/doctors-health-and-wellbeing. (viewed June 2020).
- 17.WRaP EM. Wellness, resilience, and performance: emergency medicine [website]. https://wrapem.org/ (viewed June 2020).
- 18.New Zealand Medical Association Doctor's health, wellbeing and vitality: position statement. NZMA. 2013 https://www.nzma.org.nz/assets/Uploads/Documents/Doctors-Health-and-Wellbeing-2013.pdf (viewed June 2022) [Google Scholar]
- 19.Australian Medical Association Health and wellbeing of doctors and medical students — position statement [website] AMA. 2020 https://www.ama.com.au/position-statement/health-and-wellbeing-doctors-and-medical-students-2020 (viewed June 2022) [Google Scholar]
- 20.Royal Australasian College of Physicians. Health of doctors: position statement [website]RACP. 2017 https://www.racp.edu.au/news-and-events/all-news/news-details?id=101c60af-bbb2-61c2-b08b-ff00001c3177 (viewed June 2022) [Google Scholar]
- 21.Australian and New Zealand College of Anaesthetists. Doctors' Health and Wellbeing Framework [website]ANZCA. 2019 http://www.anzca.edu.au/resources/doctors-welfare/draft-interim-framework (viewed June 2020) [Google Scholar]
- 22.Stamm B.H. 2nd ed. ProQOL; Pocatello, ID: 2010. The Concise ProQOL manual.https://proqol.org/proqol-manual (viewed June 2022) [Google Scholar]
- 23.van Mol M.M.C., Kompanje E.J.O., Benoit D.D., et al. The prevalence of compassion fatigue and burnout among healthcare professionals in intensive care units: a systematic review. PloS ONE. 2015;10:e0136955. doi: 10.1371/journal.pone.0136955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Simpson N., Knott C.I. Stress and burnout in intensive care medicine: an Australian perspective. Med J Aust. 2017;206:107–108. doi: 10.5694/mja16.00626. [DOI] [PubMed] [Google Scholar]
- 25.Shanafelt T.D., Noseworthy J.H. Executive leadership and physician well-being: nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92:129–146. doi: 10.1016/j.mayocp.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 26.Montgomery A., Panagopoulou E., Kehoe I., Valkanos E. Connecting organisational culture and quality of care in the hospital: is job burnout the missing link? J Health Organ Manag. 2011;25:108–123. doi: 10.1108/14777261111116851. [DOI] [PubMed] [Google Scholar]
- 27.Lee R.T., Seo B., Hladkyj S., et al. Correlates of physician burnout across regions and specialties: a meta-analysis. Hum Resourr Health. 2013;11:48. doi: 10.1186/1478-4491-11-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Medical Council of New ZealandThe New Zealand Medical Workforce in. 2016 https://www.mcnz.org.nz/assets/Publications/Workforce-Survey/d57ff59857/Workforce-Survey-2016.pdf (viewed June 2022) [Google Scholar]
- 29.Medical Board of Australia. Medical Board of Australia Registrant data: reporting period: 1 October 2016 - 31 December 2016. https://www.medicalboard.gov.au/Search.aspx?f.Format%7Cf=pdf&f.Date%7Cd=d%3D2017+%3A%3A+2017&f.Date%7Cd=d%3D2019+%3A%3A+2019&f.date%7Cd=dgrt14jul2016lst16jul2017&query=&fformat%7Cf=word%2Ftext+file&f.Content+type%7Ccontent=reports&f.website%7Cboard=ahpra&start_rank=11 (viewed June 2022).
- 30.Jones D., Story D.A., Clavisi O., Jones R. Peyton P An introductory guide to survey research in anaesthesia. Anaesth Intensive Care. 2006;34:245–253. doi: 10.1177/0310057X0603400219. [DOI] [PubMed] [Google Scholar]
- 31.Yin R.K. In: Qualitative research from start to finish. 2nd ed. Yin R.K., editor. Guilford Publications; 2015. Analyzing qualitative data, I: compiling, disassembling, and reassembling; pp. 184–217. [Google Scholar]
- 32.Yin R. In: Qualitative research from start to finish. 2nd ed. Yin R.K., editor. Guilford Publications; 2015. Analyzing qualitative data, II: interpreting and concluding; pp. 218–243. [Google Scholar]
- 33.Castleberry A., Nolen A. Thematic analysis of qualitative research data: is it as easy as it sounds? Curr Pharm Teach Learn. 2018;10:807–815. doi: 10.1016/j.cptl.2018.03.019. [DOI] [PubMed] [Google Scholar]
- 34.Lingard L., Albert M., Levinson W. Grounded theory, mixed methods, and action research. BMJ. 2008;337:a567. doi: 10.1136/bmj.39602.690162.47. [DOI] [PubMed] [Google Scholar]
- 35.Teixeira C., Ribeiro O., Fonseca A.M., Carvalho A.S. Burnout in intensive care units — a consideration of the possible prevalence and frequency of new risk factors: a descriptive correlational multicentre study. BMC Anesthesiol. 2013;13:38. doi: 10.1186/1471-2253-13-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vandevala T., Pavey L., Chelidoni O., et al. Psychological rumination and recovery from work in intensive care professionals: associations with stress, burnout, depression and health. J Intensive Care. 2017;5:16. doi: 10.1186/s40560-017-0209-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Highfield J., Parry-Jones J. Professional quality of life in intensive care medicine: the 2018 Faculty of Intensive Care Medicine Workforce survey. J Intensive Care Soc. 2020;21:299–304. doi: 10.1177/1751143719877102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rotenstein L.S., Torre M., Ramos M.A., et al. Prevalence of burnout among physicians a systematic review. JAMA. 2018;320:1131–1150. doi: 10.1001/jama.2018.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bianchi R. Is the “burnout epidemic” an academic fiction? BMJ. 2017;358:j4389. doi: 10.1136/bmj.j4389. [DOI] [PubMed] [Google Scholar]
- 40.Bianchi R., Schonfeld I.S., Vandel P., Laurent E. On the depressive nature of the "burnout syndrome": a clarification. Eur Psychiatry. 2017;41:109–110. doi: 10.1016/j.eurpsy.2016.10.008. [DOI] [PubMed] [Google Scholar]
- 41.Dyrbye L.N., West C.P., Shanafelt T.D. Defining burnout as a dichotomous variable. J Gen Intern Med. 2009;24:440. doi: 10.1007/s11606-008-0876-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Maslach C., Leiter M.P. In: The handbook of stress and health. Cooper C.L., Quick J.C., editors. John Wiley and Sons; 2017. Understanding burnout. [Google Scholar]
- 43.Flanders S., Hampton D., Missi P., et al. Effectiveness of a staff resilience program in a pediatric intensive care unit. J Pediatr Nurs. 2020;50:1–4. doi: 10.1016/j.pedn.2019.10.007. [DOI] [PubMed] [Google Scholar]
- 44.Dasan S., Gohil P., Cornelius V., Taylor C. Prevalence, causes and consequences of compassion satisfaction and compassion fatigue in emergency care: a mixed-methods study of UK NHS Consultants. Emerg Med J. 2015;32:588–594. doi: 10.1136/emermed-2014-203671. [DOI] [PubMed] [Google Scholar]
- 45.McCain R.S., McKinley N., Dempster M., et al. A study of the relationship between resilience, burnout and coping strategies in doctors. Postgrad Med J. 2018;94:43–47. doi: 10.1136/postgradmedj-2016-134683. [DOI] [PubMed] [Google Scholar]
- 46.Merlani P., Verdon M., Businger A., et al. Burnout in ICU caregivers: a multicenter study of factors associated to centers. Am J Respir Crit Care Med. 2011;184:1140–1146. doi: 10.1164/rccm.201101-0068OC. [DOI] [PubMed] [Google Scholar]
- 47.Sanfilippo F., Palumbo G.J., Noto A., et al. [Prevalence of burnout among intensive care physicians: a systematic review] [Prevalência de burnout entre médicos atuantes em terapia intensiva: uma revisão sistemática] [Portuguese] Rev Bras Ter Intensiva. 2020;32:458–467. doi: 10.5935/0103-507X.20200076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hammond N.E., Crowe L., Abbenbroek B., et al. Impact of the coronavirus disease 2019 pandemic on critical care healthcare workers' depression, anxiety, and stress levels. Aust Crit Care. 2021;34:146–154. doi: 10.1016/j.aucc.2020.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chuang C.H., Tseng P.C., Lin C.Y., et al. Burnout in the intensive care unit professionals: a systematic review. Medicine (Baltimore) 2016;95:e5629. doi: 10.1097/MD.0000000000005629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bakker A.B., Le Blanc P.M., Schaufeli W.B. Burnout contagion among intensive care nurses. J Adv Nurs. 2005;51:276–287. doi: 10.1111/j.1365-2648.2005.03494.x. [DOI] [PubMed] [Google Scholar]
- 51.Babenko O. Professional well-being of practicing physicians: the roles of autonomy, competence, and relatedness. Healthcare (Basel) 2018;6:12. doi: 10.3390/healthcare6010012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rimmer A., Chatfield C. What organisations around the world are doing to help improve doctors' wellbeing. BMJ. 2020;369 doi: 10.1136/bmj.m1541. [DOI] [PubMed] [Google Scholar]
- 53.Shapiro D.E., Duquette C., Abbott L.M., et al. Beyond burnout: a physician wellness hierarchy designed to prioritize interventions at the systems level. Am J Med. 2019;132:556–563. doi: 10.1016/j.amjmed.2018.11.028. [DOI] [PubMed] [Google Scholar]
- 54.Walsh J. Gender, the work-life interface and wellbeing: a study of hospital doctors. Gend Work Organ. 2013;20:439–453. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials



