Abstract
BACKGROUND
The majority of maternal deaths occur in the postpartum period. We sought to compare postpartum readmission by race and ethnicity to better understand whether there are disparities in maternal health in the postpartum period as indicated by readmission to the hospital.
OBJECTIVE
This study aimed to use state-wide Maryland data to identify postpartum readmission rates by race and ethnicity, as well as the major risk factors, indications, and timing of readmission.
STUDY DESIGN
In this retrospective study (2016–2019), childbirth hospitalizations for patients of childbearing age were identified from the Maryland State Inpatient Database, Healthcare Cost and Utilization Project, Agency for Healthcare Research and Quality. Indication for readmission was described. Multivariable logistic regression models were employed to determine racial and ethnic differences in postpartum readmissions, adjusting for maternal and obstetrical characteristics.
RESULTS
Among total deliveries (n=260,778), 3914 patients (1.5%) were readmitted within 60 days of delivery. The most common primary diagnoses at readmission were hypertension and infection. The prevalence of readmission was 1.2% (1306/111,325) for White patients, 2.3% (1786/79,412) for Black patients, 1.2% (485/40,862) for Hispanic patients and 1.2% (337/29,179) for patients of Other race or ethnicity (P<.0001). Black patients had the highest rates of readmission for hypertensive disorders as compared with all other races (37%, P<.0001). In adjusted models, Black patients were more likely to be readmitted than White patients (odds ratio, 1.64; confidence interval, 1.52–1.77). The majority of all readmissions occurred in the first week after delivery with Black patients having higher rates of readmission in the second week relative to all other groups (P<.0001).
CONCLUSION
Hypertension is a leading cause of postpartum readmission in Maryland. Black patients were more likely to be readmitted for hypertensive disorders of pregnancy and to have delayed readmission relative to other race or ethnic groups. Maryland public health officials should address disparities with interventions targeting racial and ethnic minorities, patients at risk for hypertensive disorders, and barriers to timely care.
Key words: care delay, healthcare disparities, hypertensive disorders of pregnancy, maternal morbidity and mortality, postpartum care, public health
AJOG Global Reports at a Glance.
Why was this study conducted?
This study was conducted to understand indications and risk factors for postpartum readmission in Maryland from 2016 to 2019.
Key findings
Black patients were nearly twice as likely to be readmitted in the postpartum period when compared with White or Hispanic patients and with respect to timing, Black patients were readmitted at a higher rate in the second week following delivery compared with White and Hispanic patients (no differences were found in the first week).
What does this add to what is known?
Hypertension was the leading indication for postpartum readmission and disproportionately affected Black patients and postpartum interventions should target blood pressure control.
Introduction
Postpartum readmissions are maternal hospitalizations occurring during the 60 days following delivery; 90% of these readmissions occur within the first 30 days after delivery.1,2 The study of postpartum readmission has received increasing attention in the context of the high levels of maternal mortality in the United States relative to other well-resourced countries.3 In addition, the maternal death ratio is significantly higher for US Black women when compared with US White women.4 In the United States, over 50% of maternal deaths occur in the postpartum period, with 19% occurring on days 1 to 6 after delivery.5 To address disparities in maternal mortality, we must improve our understanding of postpartum readmission.
In a study of all births in the United States between 2010 and 2014, the incidence of postpartum readmission was found to be 1.6 per 100 deliveries.2 This incidence varies by state, and the overall risk of readmission is increasing.1,6 The most common indications for postpartum readmission are infection, hypertension, and psychiatric illness, and they typically occur in the second week after discharge.1,6,7
Risk factors for postpartum readmission include public insurance status, hypertension, diabetes, postpartum hemorrhage at birth, and cesarean or stillbirth delivery.1,2,6 In addition, Black patients are at a significantly higher risk for postpartum readmission when compared with patients of other races.1 Racial differences in postpartum readmission exist in parallel to those seen in maternal mortality outcomes.4
In Maryland, the pregnancy-related mortality ratio of 18.4 deaths per 100,000 live births in 2013 to 2017 is slightly higher than the national average of 17.3 deaths per 100,000 live births; 81% of maternal deaths in Maryland occur during the postpartum period.8,9 Consistent with national trends, Black women in Maryland have a 2.6 times higher risk of pregnancy-related mortality than White women, and Hispanic women have a 1.6 times higher risk.8 However, there have been no studies on postpartum hospital readmissions in Maryland and how they might differ by race and ethnicity.
This study aimed to examine postpartum readmission rates by race and ethnicity, as well as the major risk factors, indications, and timing of readmission using statewide data as reported in the Maryland State Inpatient Database (SID). Based on Maryland's mortality rates and studies in other states, we hypothesized that Black patients would have higher rates of readmission than those of other races, that the major indications would follow national patterns, and public insurance, comorbidities, and Black race would be significant risk factors.
Materials and Methods
Data source
The 2016 to 2019 Maryland SID was used for this analysis. This is a database developed for the Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality. The database contains discharge data on each of the state's approximate 800,000 annual admissions.10,11 The Johns Hopkins University School of Medicine Institutional Review Board granted exemption due to the deidentified and public nature of this database (Johns Hopkins IRB00320807).
Study population
Delivery discharge records were identified using the International Classification of Diseases 10th Revision, Clinical Modification (ICD-10-CM) diagnosis codes and the International Classification of Diseases 10th Revision Procedure Coding System (ICD-10-PCS) procedure codes. These codes are available on request. Delivery admissions for patients with >1 delivery in the same calendar year were excluded from the analytical sample. Readmissions after delivery were identified using an HCUP unique patient identifier (“visitlink”) that is consistent across admissions and facilities. Deliveries with a missing value for “visitlink” were excluded. Days between the delivery admission and subsequent readmission(s) were calculated using an HCUP timing variable linked to the unique patient identifier (“daystoevent”). Delivery characteristics and primary diagnosis on readmission were categorized using ICD-10-CM diagnosis codes, ICD-10-PCS procedure codes, HCUP Clinical Classifications Software Refined, and Medicare Diagnosis Related Groupings. These codes are available on request.
Statistical analysis
To assess crude associations, categorical variables were analyzed using Pearson chi-square and continuous variables were analyzed using Student t tests or Wilcoxon rank-sum tests. Hierarchical multivariable logistic regression models were used to assess the adjusted relationship between race/ethnicity and 60-day readmission and to identify independent risk factors for readmission while controlling for clinically relevant covariates. Analyses were performed using SAS 9.4 software (SAS Institute, Cary, NC), and statistical significance was set at P<.05.
Results
During the 4-year study period, 260,778 deliveries meeting inclusion criteria occurred in Maryland. The mean age at delivery was 29.8 years, with 16.3% of mothers being of advanced maternal age (age>35 years). Of all patients, 3914 (1.5%) were readmitted within 60 days of delivery; 85% of all readmissions (n=3344) occurred within 30 days of delivery. Among Black patients, 2.3% were readmitted, whereas for other races and ethnicities the proportion of patients readmitted was below 1.5%. Black patients were more likely to be readmitted >1 time, when compared with other races and ethnicities. The median postpartum day of readmission was day 9 for patients of all races and ethnicities, except for Hispanic patients, who were most often readmitted on day 12 (Table 1).
Table 1.
Patient characteristics by race or ethnicity
| Characteristic | Black | White | Hispanic | Other | Total | P value |
|---|---|---|---|---|---|---|
| N (%) | 79,412 (30.5) | 111,325 (42.7) | 40,862 (15.7) | 29,179 (11.2) | 260,778 | |
| Age, mean (SD)a | 29.0 (6.1) | 30.3 (5.3) | 28.8 (6.3) | 31.1 (5.4) | 29.8 (5.8) | <.0001 |
| Age, n, (%)a | ||||||
| <20 | 4306 (5.4) | 2782 (2.5) | 2900 (7.1) | 610 (2.1) | 10,598 (4.1) | <.0001 |
| 20–29 | 38,414 (48.4) | 44,180 (39.7) | 19,088 (46.7) | 10,117 (34.7) | 111,799 (42.9) | |
| 30–39 | 33,333 (42.0) | 60,603 (54.4) | 17,121 (41.9) | 16,919 (58.0) | 127,976 (49.1) | |
| ≥40 | 3355 (4.2) | 3759 (3.4) | 1752 (4.3) | 1532 (5.3) | 10,398 (4.0) | |
| Advanced maternal age (>35 y), n (%)a | 12,524 (15.8) | 17,485 (15.7) | 6564 (16.1) | 5955 (20.4) | 42,528 (16.3) | <.0001 |
| Primary expected payer, n (%) | ||||||
| Medicare/Medicaid | 45,234 (57.0) | 25,693 (23.1) | 30,082 (73.6) | 10,146 (34.8) | 111,155 (42.6) | <.0001 |
| Private | 30,499 (38.4) | 80,697 (72.5) | 8903 (21.8) | 17,816 (61.1) | 137,915 (52.9) | |
| Other | 3679 (4.6) | 4935 (4.4) | 1877 (4.6) | 1217 (4.2) | 11,708 (4.5) | |
| Discharge calendar quarter, n (%) | ||||||
| Q1 | 19,288 (24.3) | 25,806 (23.2) | 9492 (23.2) | 6927 (23.7) | 61,513 (23.6) | <.0001 |
| Q2 | 18,919 (23.8) | 28,717 (25.8) | 9757 (23.9) | 7284 (25.0) | 64,677 (24.8) | |
| Q3 | 21,062 (26.5) | 29,788 (26.7) | 11,081 (27.1) | 7538 (25.8) | 69,469 (26.6) | |
| Q4 | 20,143 (25.4) | 27,014 (24.3) | 10,532 (25.8) | 7430 (25.5) | 65,119 (25.0) | |
| Elixhauser comorbidity index for risk of 30-d, all-cause readmission, median (Q1–Q3) | 0 (0–5) | 0 (0–2) | 0 (0–2) | 0 (0–2) | 0 (0–3) | <.0001 |
| Elixhauser comorbidity index for risk of in-hospital mortality, median (Q1–Q3) | 0 (−7 to 0) | 0 (−7 to 0) | 0 (−4 to 0) | 0 (−3 to 0) | 0 (−7 to 0) | <.0001 |
| Median household income national quartile for patient ZIP code, n, (%) | ||||||
| Unknown | 208 (0.3) | 336 (0.3) | 80 (0.2) | 77 (0.3) | 701 (0.3) | <.0001 |
| Q1 (0th–25th percentile) | 12,361 (15.6) | 7415 (6.7) | 1527 (3.7) | 1214 (4.2) | 22,517 (8.6) | |
| Q2 (26th to 50th percentile (median)) | 10,105 (12.7) | 10,670 (9.6) | 2318 (5.7) | 1883 (6.5) | 24,976 (9.6) | |
| Q3 (51st to 75th percentile) | 27,311 (34.4) | 30,838 (27.7) | 19,628 (48.0) | 8051 (27.6) | 85,828 (32.9) | |
| Q4 (76th to 100th percentile) | 29,427 (37.1) | 62,066 (55.8) | 17,309 (42.4) | 17,954 (61.5) | 126,756 (48.6) | |
| LOS at delivery, median (IQR) | 2 (2–3) | 2 (2–3) | 2 (2–3) | 2 (2–3) | 2 (2–3) | <.0001 |
| Readmitted within 30 d, n (%) | 1564 (2.0) | 1108 (1.0) | 383 (1.0) | 289 (1.0) | 3344 (1.3) | <.0001 |
| Readmitted within 60 d, n (%) | 1786 (2.3) | 1306 (1.2) | 485 (1.2) | 337 (1.2) | 3914 (1.5) | <.0001 |
| >1 Readmission | 106 (0.1) | 81 (0.1) | 32 (0.1) | 16 (0.1) | 235 (0.1) | <.0001 |
| Days to first readmission, median (Q1–Q3) | 9 (6–17) | 9 (6–19) | 12 (6–27) | 9 (5–18) | 9 (6–19) | <.0001 |
Age was available for 260,771 patients; not available for 7 patients. Therefore N = 260,771.
Hamilton. Maryland postpartum readmission. Am J Obstet Gynecol Glob Rep 2023.
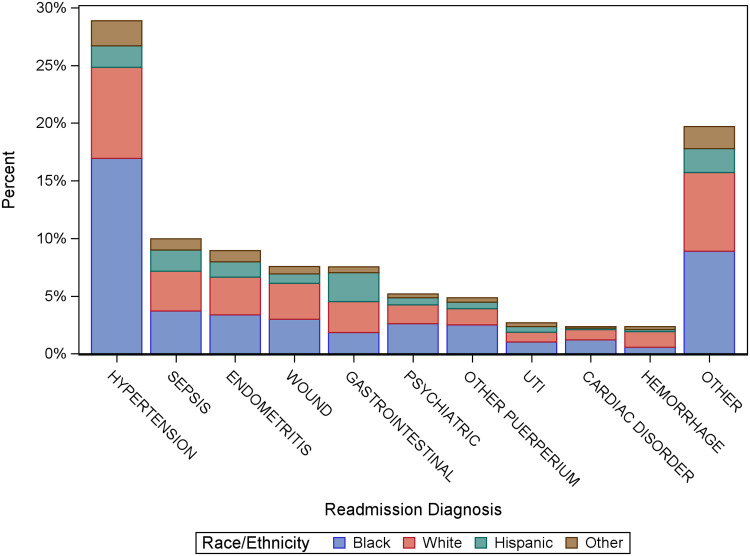
The most common indications for readmission were hypertensive disorders (28.9%), sepsis (10.0%), genital tract infections (8.9%), and wound complications (7.6%) (Table 2). Analysis shows a higher proportion of Black patients readmitted with hypertensive disorders when compared with patients of all other races. Black patients were also more likely to be readmitted with a primary diagnosis of depression or other psychiatric disorders (Figure 1).
Table 2.
First readmission primary diagnosis by race or ethnicity, n (%)
| Diagnosis | Black | White | Hispanic | Other | Total | P value |
|---|---|---|---|---|---|---|
| Preeclampsia/eclampsia/hypertensive disorder of pregnancy | 663 (37.1) | 85 (25.2) | 309 (23.7) | 73 (15.1) | 1130 (28.8) | <.0001 |
| Sepsis and infection | 145 (8.1) | 38 (11.3) | 135 (10.3) | 72 (14.9) | 390 (10.0) | 0.0260 |
| Endometritis and other infection of the genital tract | 132 (7.4) | 38 (11.3) | 128 (9.8) | 52 (10.7) | 350 (8.9) | 0. 2779 |
| Wound complications (Including SS infection and disruption) | 117 (6.6) | 25 (7.4) | 122 (9.3) | 32 (6.6) | 296 (7.6) | 0. 0239 |
| Cholelithiasis, cholecystitis and other diseases of the digestive system | 72 (4.0) | 20 (5.9) | 105 (8.0) | 98 (20.2) | 295 (7.5) | <.0001 |
| Depression and other psychiatric disorders | 102 (5.7) | 13 (3.9) | 64 (4.9) | 24 (5.0) | 203 (5.2) | <.0001 |
| Other complications of the puerperium, not elsewhere classified | 98 (5.5) | 15 (4.5) | 55 (4.2) | 22 (4.5) | 190 (4.9) | <.0001 |
| Urinary tract infections | 40 (2.2) | 13 (3.9) | 33 (2.5) | 19 (3.9) | 105 (2.7) | 1 |
| Heart failure and other cardiac and cardiovascular disorders | 47 (2.6) | 5 (1.5) | 35 (2.7) | 5 (1.0) | 92 (2.4) | 0.0006 |
| Hemorrhage | 22 (1.2) | 10 (3.0) | 53 (4.1) | 7 (1.4) | 92 (2.4) | 0.2123 |
| Other | 348 (19.5) | 75 (22.3) | 267 (20.4) | 81 (16.7) | 771 (19.7) | <.0001 |
Key: reporting adjusted P values after applying Bonferroni correction for multiple comparisons.
Hamilton. Maryland postpartum readmission. Am J Obstet Gynecol Glob Rep 2023.
Figure 1.
Proportion of primary diagnosis on readmission by patient race and ethnicity
The most common indications for readmission were hypertensive disorders (“HTN Disorders”), infection, reproductive tract infection, and wound complications. Black patients were overrepresented in readmissions for hypertensive disorders of pregnancy and depression and other psychiatric disorders. Asterisk denotes P<.05.
Hamilton. Maryland postpartum readmission. Am J Obstet Gynecol Glob Rep 2023.
The median length of stay during the original delivery admission was 2 days, consistently across groups (Table 1). On readmission, the median length of stay was 2 days. Hispanic women had a longer length of stay on readmission (interquartile range [IQR], 2–4 days vs IQR, 1–3 days for patients of all other groups readmitted (Supplemental Table 1). The majority of patients (75.1%) were initially readmitted to the same hospital where they delivered, with 24.9% readmitted to a different hospital. Pairwise comparisons of the proportion of patients readmitted to a different hospital by race indicate Black patients were more likely to be readmitted to a different hospital than White patients (P=.02) and patients of Other races (P=.03). Notably, across all races and ethnicities, length of stay tended to be longer when patients were readmitted at a different hospital (IQR, 2–4 days vs IQR, 1–3 days for those readmitted to the same hospital where delivery occurred).
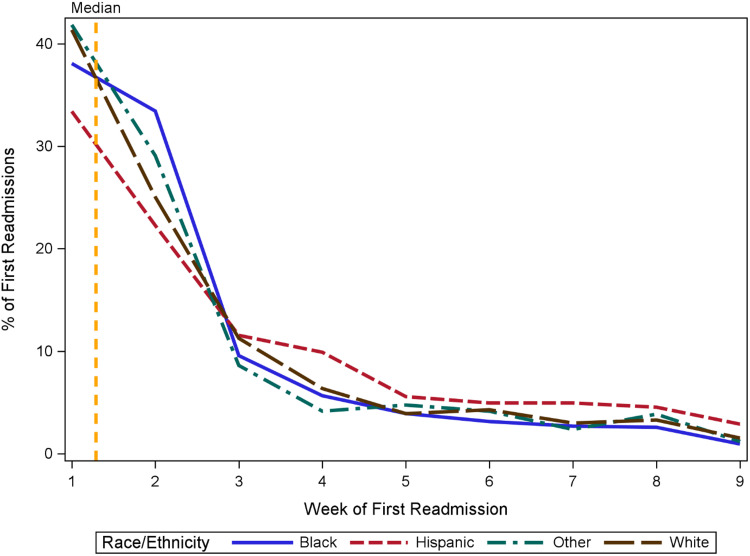
For patients of all races and ethnicities, readmission rates were highest in the first week after discharge. However, after the first week Black patients experienced a less precipitous decline compared with all other race groups (Figure 2). The reduction in proportion of readmissions from week 1 to week 2 among Black patients was 4.7% whereas the reduction in other groups ranged from 11.1% to 16.3%. This resulted in Black patients experiencing more readmissions than all other race groups during week 2 after discharge (33.4% vs 25.1%, respectively; P<.0001) (Supplemental Table 2). Pairwise comparisons further confirmed higher rates of readmission among Black patients in week 2 as compared with White (33.4% vs 25.0%; P<.0001) and Hispanic patients (33.4% vs 22.3%; P<.0001). A similar trend was seen in the fourth week postpartum, when Hispanic patients experienced a slower decline in the proportion of readmissions from week 3 to week 4 as compared with all other races (4.3% vs 1.2%, respectively) resulting in a significantly higher rate of readmission in week 4 as compared with all other races (9.9% vs 5.8%; P=.004) (Figure 2; Supplemental Table 2). Pairwise comparisons also confirmed higher rates of readmission among Hispanic patients in week 4 as compared with Black patients (9.9% vs 5.6%; P=.005) and those of Other races (9.9% vs 4.2%; P=.013) but not White patients (9.9% vs 6.4%; P=.063).
Figure 2.
Week of first readmission by race and ethnicity
The majority of readmissions for patients of all races occurred in week 1, with Black patients experiencing a slower decline in readmission from week 1 to week 2 than patients of other races, and Hispanic patients experiencing a slower decline in readmission from week 3 to week 4 than patients of other races.
Hamilton. Maryland postpartum readmission. Am J Obstet Gynecol Glob Rep 2023.
In multivariate logistic regression models, Black race, when compared with White race, was found to be a significant risk factor for readmission. This was first seen in unadjusted analyses (95% confidence interval [CI], 1.80–2.08) and remained true in models that adjusted for maternal age, income quartile, insurance payor, comorbidities, and delivery characteristics, where Black patients were still more likely to be readmitted than White patients (95% CI, 1.52–1.77). Other independent risk factors identified in this analysis were advanced maternal age (95% CI, 1.24–1.46), government insurance (Medicare or Medicaid) as compared with private insurance (95% CI, 1.01–1.17), Elixhauser comorbidity score (95% CI, 1.03–1.05), induction of labor (95% CI, 1.11–1.31), delivery by cesarean mode (95% CI, 1.82–2.11), and the presence of a placental disorder (95% CI, 1.09–1.50), intrauterine infection (95% CI: 1.21–1.68), or hypertensive disorder of pregnancy (95% CI 1.97–2.27). (Figure 3; Supplemental Table 3).
Figure 3.
Multivariate modeling for readmission risk factors
On multivariate logistic regression analyses, factors found to independently increase risk for readmission were Black race when compared with White race, advanced maternal age, income quartile 2 when compared with income quartile 4, income quartile 3 when compared with income quartile 4, government insurance when compared with private insurance, Elixhauser comorbidity score, current cesarean delivery, placental disorder, hypertensive disorders of pregnancy, and intrauterine infection. Gray fill indicates nonsignificant factors. Purple fill indicates significant risk factors. Error bars represent 95% confidence intervals.
Hamilton. Maryland postpartum readmission. Am J Obstet Gynecol Glob Rep 2023.
After stratification by income quartile, we found that higher odds for readmission of Black patients when compared with White patients persisted across all income quartiles. This is in contrast to Hispanic patients, who had higher odds for readmission when compared with White patients only if they were in the lowest income quartile (95% CI, 1.05–2.57). In addition to Black race, other risk factors such as advanced maternal age, comorbidity score, cesarean delivery, and hypertensive disorders of pregnancy increased the risk for readmission regardless of income (Table 3).
Table 3.
Adjusted odds of readmission by race/ethnicity, stratified by income quartile
| Maternal Race/Ethnicity | Income Q1 |
Income Q2 |
Income Q3 |
Income Q4 |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |||||
| Black vs White | 1.83a | 1.42a | 2.37a | 1.43a | 1.16a | 1.77a | 1.59a | 1.39a | 1.82a | 1.74a | 1.55a | 1.95a |
| Hispanic vs White | 1.65a | 1.06a | 2.57a | 1.17 | 0.81 | 1.70 | 0.91 | 0.77 | 1.09 | 1.09 | 0.91 | 1.29 |
| Other vs White | 1.26 | 0.75 | 2.12 | 1.46a | 1.02a | 2.09a | 0.95 | 0.75 | 1.19 | 0.99 | 0.83 | 1.16 |
Key: Odds ratio estimates shown are adjusted for advanced maternal age, insurance, and maternal characteristics (Elixhauser readmission score, induction, prior c-section, placental disorder, hypertensive disorder(s) of pregnancy, intrauterine infection).
CI, confidence interval; OR, odds ratio; Q, quartile.
P<0.05.
Hamilton. Maryland postpartum readmission. Am J Obstet Gynecol Glob Rep 2023.
Comment
Principal findings
In this analysis of 260,778 patients with a singleton birth in Maryland between 2016 and 2019, 1.5% of patients were readmitted within 60 days. Black patients had the highest rates of readmission (2.3%), compared with 1.2% for other racial and ethnic groups. Hypertension and infection were the most common indications for readmission, with Black patients having the highest rates of readmission for hypertensive disorders. After adjusting for maternal age, insurance status, and comorbidities, Black patients were more likely to be readmitted than White patients regardless of income. Black patients had a higher proportion of readmission occur in the second week after discharge, relative to all other groups.
Results in the context of what is known
The 60-day readmission rate of 1.5% seen in this study is similar to rates seen both in nationwide and other state-specific studies.1,12,13 Hypertension has been previously identified as a leading cause for postpartum readmission, along with infection, gallbladder disease, and psychiatric illness.1,7,14,15 Similar studies have also found Black race to be a significant risk factor for readmission, even when adjusting for other characteristics.1,16,17 Although our study did not find Hispanic ethnicity alone to be a risk factor for postpartum readmission, others have.16,17 On further analyses, we found Hispanic ethnicity to be a significant risk factor for patients in the lowest income quartile but not for those in quartiles 2, 3, or 4. This is in contrast with Black race, which affected risk regardless of the patient's income. Moving forward, more research is needed to better understand the interplay between income and race and ethnicity.
The comorbidities and maternal characteristics we found to increase risk for readmission corroborate those seen in the existing literature, particularly cesarean delivery and hypertensive disorders of pregnancy.1,12, 13, 14, 15,17 We found Maryland patients with government insurance to have a slightly higher risk of readmission than those with private insurance. Other studies have found public insurance to confer an even higher risk for postpartum readmission.15, 16, 17 This might be explained by the Maryland all-payer model, and its emphasis on ensuring quality care for patients who use government insurance.18
Wen et al found that 15% of nationwide postpartum readmissions occurred at a different hospital from where delivery occurred, and this fragmented care was associated with longer lengths-of-stay (LOS) in unadjusted analysis.19 Our results also showed a longer LOS when readmission occurred in a different hospital, but a larger proportion of patients (24.9%) had this fragmentation of care in Maryland. In addition, our findings indicated that Black patients were more likely to experience fragmented care than White patients or those of Other race. This may be due to sicker patients requiring transfer to a higher level of care concomitantly requiring a longer length of stay due to severity of illness. Further study is needed to determine the reason for these discrepancies and whether they worsen outcomes in Maryland.
There is consensus about most readmissions occurring in the first 30 days after delivery.1,15 Our study provides a closer analysis of the week-to-week timing of readmissions by race and ethnicity.
Clinical implications
The American College of Obstetricians and Gynecologists describes the postpartum period as a “fourth trimester” of pregnancy, in which care should be ongoing and individualized.20 The findings of our study provide structure for this individualized care. They indicate that hypertensive disorders are a major risk factor for postpartum readmission. Even after controlling for these conditions, Black race remained a significant risk factor for readmission. Therefore, in addition to targeting patients with hypertensive disorders, public health interventions in Maryland should focus on the needs of racial and ethnic minority patients. This could include promotion of postdelivery care for hypertension control such as in-home blood pressure control services. Other factors shown to increase the risk of readmission, such as advanced maternal age, public insurance, preexisting comorbidities, and specific delivery characteristics should also be taken into consideration when formulating follow-up protocols and recommendations.
Research implications
Our study's findings about the nuances in the timing of readmission showed more Black patients being readmitted in the second week postpartum than those of other races, and more Hispanic patients readmitted in the fourth week postpartum. This raises interesting directions for future studies to investigate the explanations for these findings. Future research should explore barriers to timely care in the postpartum period, to elucidate whether there are issues with access, quality of care, or trust in the medical system, and what can be done to ensure timely care for all.
Strengths and limitations
A primary strength of this study was its large sample size and breadth because the SID allowed for the identification of all hospitalizations and subsequent readmissions in the state of Maryland within the 4 years studied. It must be noted that this study used retrospective data, which has several limitations. Hospitals may incorrectly assign a patient's race or ethnicity. We could also not study the intersections of race and ethnicity, as patients were only assigned 1 identifier. In this study, 11.19% of patients included in the analysis were described with a race or an ethnicity of “Other,” that is, not White, Hispanic, or Black. The study, therefore, did not distinguish between groups such as Asians or Indigenous Americans or reach any conclusions about these patients’ rates or reasons for postpartum readmission.
Finally, 60-day readmissions were more easily probed within the same calendar year, therefore, deliveries between October 31 and December 31 were likely to have underestimated readmission rates.
Conclusions
In Maryland between 2016 and 2019, Black patients were more likely to be readmitted to the hospital in the postpartum period than White patients. Hypertension, the leading indication for postpartum readmission in Maryland, was also the most frequent reason that Black patients were readmitted. Black patients had delayed readmissions relative to patients of other races and ethnicities. Physicians and public health officials should address disparities with interventions designed to serve the needs of racial and ethnic minorities, patients at risk for hypertensive disorders, and patients facing barriers to timely care.
Acknowledgments
The authors would like to thank Hyonoo Joo, BS for his assistance with figure design.
Footnotes
The authors report no conflict of interest.
Patient consent was not required because no personal information or details were included.
This study was presented at the 72nd Annual Clinical and Scientific Meeting of the American College of Obstetricians and Gynecologists, Baltimore MD, May 19-21, 2023.
Cite this article as: Hamilton S, Olson S, Voegtline K, et al. Postpartum readmission in Maryland by race and ethnicity, 2016–2019. Am J Obstet Gynecol Glob Rep 2023;3:100278.
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.xagr.2023.100278.
Appendix. Supplementary materials
References
- 1.Clapp MA, Little SE, Zheng J, Robinson JN. A multi-state analysis of postpartum readmissions in the United States. Am J Obstet Gynecol. 2016;215 doi: 10.1016/j.ajog.2016.01.174. 113.e1–10. [DOI] [PubMed] [Google Scholar]
- 2.Fein A, Wen T, Wright JD, et al. Postpartum hemorrhage and risk for postpartum readmission. J Matern Fetal Neonatal Med. 2021;34:187–194. doi: 10.1080/14767058.2019.1601697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kassebaum NJ, Bertozzi-Villa A, Coggeshall MS, et al. Global, regional, and national levels and causes of maternal mortality during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:980–1004. doi: 10.1016/S0140-6736(14)60696-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Declercq E, Zephyrin L. Maternal mortality in the United States: a primer. 2020. Available at: https://www.commonwealthfund.org/publications/issue-brief-report/2020/dec/maternal-mortality-united-states-primer. Accessed February 30, 2023.
- 5.McKinney J, Keyser L, Clinton S, Pagliano C. ACOG Committee Opinion No. 736: optimizing postpartum care. Obstet Gynecol. 2018;132:784–785. doi: 10.1097/AOG.0000000000002849. [DOI] [PubMed] [Google Scholar]
- 6.Wall-Wieler E, Butwick AJ, Gibbs RS, et al. Maternal health after stillbirth: postpartum hospital readmission in California. Am J Perinatol. 2021;38:e137–e145. doi: 10.1055/s-0040-1708803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clapp MA, Little SE, Zheng J, Kaimal AJ, Robinson JN. Hospital-level variation in postpartum readmissions. JAMA. 2017;317:2128–2129. doi: 10.1001/jama.2017.2830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maryland Maternal Health Innovation Program. Maternal mortality in Maryland 2020. Available at: https://mdmom.org/data. Accessed February 24, 2023.
- 9.Centers for Disease Control and Prevention. Pregnancy mortality surveillance system. Maternal and infant health. 2022. Available at: https://www.cdc.gov/reproductivehealth/maternal-mortality/pregnancy-mortality-surveillance-system.htm. Accessed February 24, 2023.
- 10.Overview of the State Inpatient Databases (SID). Available at https://hcup-us.ahrq.gov/sidoverview.jsp#about. Accessed December 28, 2022.
- 11.The Maryland Health Services Cost Review Commission. Clinical data submission requirements & production schedule. 2020. Available at: https://hscrc.maryland.gov/Pages/hsp_info1.aspx. Accessed December 28, 2022.
- 12.Lydon-Rochelle M, Holt VL, Martin DP, Easterling TR. Association between method of delivery and maternal rehospitalization. JAMA. 2000;283:2411–2416. doi: 10.1001/jama.283.18.2411. [DOI] [PubMed] [Google Scholar]
- 13.Liu S, Heaman M, Joseph KS, et al. Risk of maternal postpartum readmission associated with mode of delivery. Obstet Gynecol. 2005;105:836–842. doi: 10.1097/01.AOG.0000154153.31193.2c. [DOI] [PubMed] [Google Scholar]
- 14.Mogos MF, Salemi JL, Spooner KK, McFarlin BL, Salihu HH. Hypertensive disorders of pregnancy and postpartum readmission in the United States: national surveillance of the revolving door. J Hypertens. 2018;36:608–618. doi: 10.1097/HJH.0000000000001594. [DOI] [PubMed] [Google Scholar]
- 15.Reddy R, James KE, Mauney LC, Kaimal AJ, Daw JR, Clapp MA. Postpartum readmission and uninsurance at readmission for Medicaid vs privately insured births. Am J Obstet Gynecol MFM. 2022;4 doi: 10.1016/j.ajogmf.2021.100553. [DOI] [PubMed] [Google Scholar]
- 16.Aseltine RH, Yan J, Fleischman S, Katz M, DeFrancesco M. Racial and ethnic disparities in hospital readmissions after delivery. Obstet Gynecol. 2015;126:1040–1047. doi: 10.1097/AOG.0000000000001090. [DOI] [PubMed] [Google Scholar]
- 17.Wagner JL, White RS, Tangel V, Gupta S, Pick JS. Socioeconomic, racial, and ethnic disparities in postpartum readmissions in patients with preeclampsia: a multi-state analysis, 2007-2014. J Racial Ethn Health Disparities. 2019;6:806–820. doi: 10.1007/s40615-019-00580-1. [DOI] [PubMed] [Google Scholar]
- 18.Rajkumar R, Patel A, Murphy K, et al. Maryland's all-payer approach to delivery-system reform. N Engl J Med. 2014;370:493–495. doi: 10.1056/NEJMp1314868. [DOI] [PubMed] [Google Scholar]
- 19.Wen T, Krenitsky NM, Clapp MA, et al. Fragmentation of postpartum readmissions in the united states. Am J Obstet Gynecol. 2020;223 doi: 10.1016/j.ajog.2020.01.022. 252.e1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.ACOG Committee Opinion No. 736: optimizing postpartum care. Obstet Gynecol. 2018;131 doi: 10.1097/AOG.0000000000002633. e140–50. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.